
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 28 February 2023
Sec. Aging Psychiatry
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1077665
This article is part of the Research Topic Resilience in Chronic Disease, volume II View all 8 articles
Background: At the intersection of old age and illness, older adults with life-threatening illnesses (LTI) are a group who often show resilience and seek validation of life, acceptance, and integration of past and now, even under the fear of loss, suffering, and dying evoked by life adversities. Life review has been widely conducted to help older adults enhance well-being and cope with burdens. Spirituality is an important part of an older adult’ overall well-being, especially for those with LTI. However, few review studies examined the effectiveness of life review interventions on psychospiritual outcomes among this population. The aim of the study was to examine the effectiveness of life review on psychospiritual well-being among older adults with LTI.
Methods: A systematic review with meta-analysis following the recommendations of the Cochrane Collaboration was conducted. Database searches included PubMed, PsycINFO, the Cochrane Library, the Campbell Library, EBSCO, CNKI, and the Airiti Library up to March 2020. Gray literature and reference lists from relevant articles were also searched and reviewed.
Results: In total, 34 studies were included in the systematic review and the meta-analysis for outcomes of depression (n = 24), quality-of-life (QOL) (n = 10), anxiety (n = 5), life satisfaction (n = 3), mood (n = 3), apathy (n = 2), and general well-being (n = 2). Other psychospiritual outcome measures included spirituality, self-esteem, meaning in life, hope, and some multi-dimensional instruments. The studies greatly varied in program design, content, format, length, and more. Although with high heterogeneity, meta-analysis results demonstrated standardized mean differences in favor of life review in decreasing depression, anxiety, negative mood, and increasing positive mood and QOL compared with the control group.
Conclusion: This review calls for including more psycho-spiritual well-being measures among interventions for older adults with LTI, as well as studies with rigorous designs in future research.
As age increases, people are more likely to have one or more health-related problems, including life-threatening illnesses (LTI), such as cancer and heart diseases (1). Living with LTI causes pain and distress and transitions in one’s physical, psychological, social, and spiritual aspects of life (2, 3). Many people living with LTI show remarkable resilience and gradually yearn for a life larger than illness and one’s physical conditions (4), indicating the importance of exploring this population’s psychospiritual well-being.
Gleig (5) defined psychospiritual well-being as the integration of psychological and spiritual well-being. It includes embracing a spiritual dimension of the human being as fundamental to psychic health and full human development, and using methods in both fields in a holistic approach for inner growth. Researchers further pointed out that such outcomes could include self-awareness, coping and adjusting effectively to stress and loss, having satisfying relationships and connectedness with others, a sense of faith, a sense of empowerment and confidence, and living with meaning and hope, etc. (2, 4, 6, 7); Lin and Bauer-Wu (8). The key to understand one’s psychospiritual well-being is to hold a holistic, integrated view of healing and inner growth.
To enhance the overall well-being of people facing challenges associated with LTI, pharmacological and non-pharmacological interventions have been increasingly developed and delivered. One of the non-pharmacological interventions is life review (9, 10). Life review has been widely used among different populations to achieve therapeutic benefits such as enhancing one’s quality-of-life (QOL) and decreasing anxiety and depression (11). Older adults are very likely to experience various types of adversities, such as deteriorating health, worsening financial security, and illness or death of a family member. In the phase of coping (or not coping), some older individuals fail to adapt to the aging process, while others embrace opportunities and actively engage themselves in challenges, viewing their lives and health as satisfactory (12). According to Luthar et al. (13), it may be easier to detect resilient attitudes, activities, and behaviors in later life, as compared to younger individuals, older adults have acquired more life experiences to perform certain coping strategies to achieve positive outcomes; among these strategies, life review is a promising one (14).
Although sometimes used interchangeably with reminiscence by researchers and practitioners, life review and reminiscence bear significant differences: reminiscence involves recalling a memory, and thus the main goal is to stimulate one’s cognitive functioning, while life review involves reflecting and evaluating what the memory means to the person, and the main goal is usually to improve QOL and achieve ego-integrity (15–17). Some systematic review and meta-analysis studies separated the two [e.g., (18)], while others included both [e.g., (19)]. Life review definitions used by researchers were inconsistent. For example, in Ning et al. (20), although called group reminiscence, stroke patients participated in structured conversations on “First Met,” “Unforgettable Youth,” “My Other Half,” “My Favorite Entertainments,” “My Pride,” and “My Late-Life” with a main purpose to alleviate depressive symptoms, instead of focusing on cognition training. In the current study, we included studies that delivered an intervention of recalling and/or reflecting on memories, no matter how the authors named the intervention. Together we call this type of intervention “life review.”
Several systematic review and meta-analysis studies have been conducted to evaluate the effects of life review. Most of these studies focused on general older adult populations [e.g., (21, 22)] and people with cognitive impairments [e.g., (23, 24)]; the outcome measures focused on QOL, depression, and cognition [e.g., (11, 19)]. Not enough attention was paid to how life review could benefit older adults with LTI on other psychospiritual outcomes (e.g., hope, self-esteem). At the intersection of old age and illness, older adults with LTI are a group who often seek validation of life and acceptance and integration of past and now, even under the fear of loss, suffering, and dying evoked by LTI (4, 25). This process of seeking inner strength is highly consistent with the goals and procedures of life review. Thus, examining how life review could psychospiritually benefit older adults with LTI is essential and urgent.
In a previous study, Chen et al. (26) conducted a systematic review of the effects of life review on psychospiritual well-being among patients with LTI. However, they only included patients with cardiovascular disease, cancer, acquired immune deficiency syndrome (AIDS), and organ failure. Additionally, with 11 studies included, they only included depression, QOL, and self-esteem in the meta-analysis; nor did they clearly define what psychospiritual well-being is. The current systematic review and meta-analysis study aimed to thoroughly examine the effects of life review interventions on psychospiritual outcomes among older adults with LTI.
This systematic review and meta-analysis study was conducted following the guidelines outlined by the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Group (27).
Older adults with at least one diagnosed LTI or condition were included. In this study, we defined LTI based on the top 10 causes of death recorded by the World Health Organization (28) for upper-middle- and high-income countries (as based on literature review for regions of potentially included studies). After combining different types of cancer, these include cancer, ischemic heart disease, stroke, chronic obstructive pulmonary disease, lower respiratory infection, diabetes mellitus, kidney disease, and Alzheimer’s disease and related dementias (ADRD). Additionally, we included studies on palliative or hospice older adult patients, as having a life-threatening condition is one criterium to receive such service. If a study contains participants with more than one disease or in more than one age group, only those that separate participants’ conditions and age groups for analysis were included.
Interventions needed to meet our definition of life review: an intervention of recalling and/or reflecting on memories, no matter how the authors named the intervention. There was no requirement for minimum or maximum intervention duration, location, or interventionist. However, multi-component interventions where life review was only part of the intervention were excluded.
There was no requirement for control: a control could be no treatment, treatment as usual, waitlist, passive control (social contacts and conversations unrelated to life review, such as on social security income, diet), and active control (counseling about one’s life but not structured life review sessions; also could be another psychosocial intervention). However, for the meta-analysis, considering the huge effects an active control can have on the outcome, it was not included in the meta-analysis. In other words, only groups of no treatment, treatment as usual, waitlist, and passive control were used for meta-analysis.
Studies that assessed any psychospiritual effect of a life review intervention were included in the systematic review, provided that standardized assessments, rating scales, or questionnaires were used. These outcomes included but not limiting to anxiety, depression, QOL, life satisfaction, mood, hope, dignity, meaning in life, spiritual well-being, etc. Outcomes measured at post-intervention and additional follow-up were considered. Outcomes that were measured in at least two studies were included in the meta-analysis.
Studies that used random assignment with pre- and post-intervention assessments were considered for this review. These included RCTs, defined as studies in which individual participants are randomly assigned to either an intervention group or to a control group (29). Although some studies did not explicitly used the term “RCT,” we still included them if they could not be ruled out using a randomized controlled design (e.g., authors did not explicitly use the term “RCT” but mentioned “randomized” and “controlled.” An example description is: “Participants were randomized into two groups”).
Study was written in English or Chinese with full-text available.
The following academic databases were searched in March 2020: PubMed; PsycINFO; the Cochrane Library; the Campbell Library; EBSCO; CNKI; and the Airiti Library. Search terms were: (“old*” OR “elder*” OR “age*” OR “aging” OR “geriatric*” OR “senior” OR “late life”) AND (“life review” OR “reminiscence” OR “dignity therapy” OR “meaning-centered therapy” OR “life story” OR “storybook” OR “memoir” OR “life history” OR “life experience” OR “autobiograph*” OR “life album” OR “memory book” OR “memory album” OR “narrative therapy”) AND “random*” OR “rct”). Search terms were customized to each database.
The following websites were searched for gray literature: Google Scholar, ProQuest Dissertations & Theses Database (PQDT), and Duxiu. Authors of relevant conference abstracts were reached out for possible information sharing.
We searched the reference lists of included articles (i.e., articles eligible for further analysis) for additional relevant studies.
Reviewers ML and YW each screened half of the titles and abstracts. For abstracts with no full-text, authors’ correspondence information was searched online, and emails were sent to request the full-text of the study, if one existed. After that, full-text was retrieved for articles passing the abstract screening stage for further screening. Four reviewers were divided into two groups, with each group screening half of full-text articles using a pre-designed Google form with inclusion and exclusion criteria such as illness and outcome measures. Any uncertainties concerning suitability were discussed at weekly group meetings with all four investigators: Before a weekly group meeting, the first author compared the results and informed the whole group of each pair’s inconsistencies, and then asked the other pair to screen those articles again, so that all four of us could discuss inconsistencies in the group meeting. Full-text of all articles can be provided per request.
Four reviewers, again in two groups, independently extracted data using a pre-designed Google form, which was pilot tested with four articles. Each group extracted data from half of included studies. The following data were extracted, and where necessary, additional information was requested from authors:
(1) Basic study information: authors, reference, country/region.
(2) Participant characteristics: illness/condition, total number and number in each group, age, gender, race/ethnicity.
(3) Intervention characteristics: intervention content, individual or group format, in-person or virtual, setting, length (e.g., number of weeks), number of sessions, duration per session, control/comparison.
(4) Intervention assessment information: time point (e.g., pretest, posttest, follow-up), measures, outcomes with screenshots (including the mean and standard deviation of final values, and number of participants in each group at each time point), outcome raters (e.g., patients, caregivers, staff).
After comparing results within a group, any uncertainties that could not be solved were discussed in weekly meetings with all four reviewers: Before a weekly group meeting, the first author compared the results and informed the whole group of each pair’s inconsistencies, and then asked the other pair to read the relevant part of the articles, so that all four of us could discuss inconsistencies in the meeting.
RevMan 5.4 was used for meta-analysis. Outcomes measured in at least two studies were included in the meta-analysis. Heterogeneity was assessed using an I2 statistic. To interpret heterogeneity, reviewers followed Cochrane guidance (i.e., 0–40% might not be important; 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity; and 75–100% is considerable heterogeneity) (30). Where there were high levels of heterogeneity of the treatment effect between studies, a random-effects model and the standardized mean difference were used. If one study used more than one instrument to measure the same outcome variable, the team used the more commonly used instrument for the analysis. Subgroup and sensitivity analysis were performed if the heterogeneity was high. Where necessary, we performed subgroup analyses with various possible reasons for heterogeneity, including study quality (one analysis included studies with low random allocation risk, and another analysis excluded studies with four or more “high” plus “unclear” ratings in ROB appraisal), cognition (only included ADRD patients), measurement tool (compared meta-analysis results of studies that used different measurement tools for the same outcome), outcome rater (compared results of studies where outcomes were rated by older adults themselves or by caregivers), control group (compared results of studies that used different control groups, such as usual care vs. no intervention), country/region (compared results of studies that were conducted in different countries/regions), intervention weeks (>10 weeks vs. ≤10 weeks), number of intervention sessions (>10 sessions vs. ≤10 sessions).
Four reviewers independently assessed the risk of bias using the Cochrane “Risk of Bias” tool (31), classifying each category as low, high, or unclear ROB. Any disagreements regarding ROB ratings were discussed at weekly meetings until a consensus was reached.
Figure 1 shows the PRISMA flowchart of the study review and selection process. A total of 34 studies, representing a total of 2,752 participants, were included in the review and the meta-analysis.
Table 1 presents the characteristics of included studies. Among 34 studies, 19 were conducted in Asia (13 in mainland China, three in Taiwan, two in Japan, one in Hong Kong), 11 in Europe (five in the United Kingdom, three in Turkey, two in Belgium, one in Portugal), three in the United States, and one in Argentina. Eighteen were RCT, 14 were randomized studies, and two were “quasi-experimental” studies, as claimed by authors, in which the randomization could not be ruled out.
In terms of the intervention details, apart from five studies that did not provide the information on the intervention length (35–37, 41, 42), the length ranged from 4 weeks to 10 months, with more than half (n = 23) fell between six to 12 weeks. The number of sessions ranged from 4 to 24. Sixteen interventions were conducted individually with an older adult; 12 were in groups of older adults; three were attended by older adults together with their caregivers (24, 34, 37); one study did not specify (43). For the remaining two studies, in Thorgrimsen et al. (38), caregivers first participated in the intervention for 11 weeks, followed by 7-week older adult-caregiver dyads participating together; in 39, there were two intervention groups, with the content being the same but in the individual and the group format, respectively.
Researchers claimed the reminiscence was used in 27 studies, including one that used the reminiscence gaming on a device (39), and one that used the “spiritual reminiscence” (44). For others, three used life review (42, 45, 46), three used narrative therapy (35, 36, 47), and one used life-story book (48). Control groups received usual care in 20 studies (including one waitlist, (39)), passive control activities in three studies such as weekly calls and conversations on topics not related to life review (37, 49, 50), no intervention in three studies (38, 42, 51), and other activities relevant to the interventions in two studies (46, 52). Three studies did not provide control group information (44, 53, 54). In the remaining three studies, two control groups were used. In Lai and Kayser-Jones (55), one group received passive control and the other did not receive any treatment; in Mei et al. (34), one group was the reminiscence received only by caregivers, and the other was usual care group; in Serrani Azcurra (43), one was the active control (i.e., counseling) and the other was the passive control.
Eleven psychospiritual outcomes were measured. Depression was measured in more than half of studies (n = 24), QOL measured in 11, and anxiety in five. Life satisfaction was measured in three studies. Mood, apathy, spirituality, and general well-being were measured in two studies. Self-esteem, meaning in life, and hope were measured in one study. Please see Table 1 for detailed information.
Additionally, four multi-dimensional measurement tools were used in several studies. They were not included in the meta-analysis, either because only a total score was calculated, or because the same concept was measured in the study using a more widely used scale. These tools included Neuropsychiatric Inventory Questionnaire (NPI-P) (measured in four studies), which measures a variety of symptoms such as delusions and hallucinations but also psychospiritual outcomes such as depression and anxiety; Multidimensional Observation Scale for Elderly Subjects (MOSES) (two studies), which includes five domains: self-care, disorientation, depression, irritability, and withdrawal; Nurses’ Observation Scale for Inpatient Evaluation (NOSIE) (one study); and Memorial Symptom Assessment Scale – Short Form (MSAS-SF) (one study), which includes four parts: physical symptoms, physical bother, emotional symptoms, and emotional bother.
A majority of studies (n = 24) had pre- and post-intervention assessments; others had during-intervention, or follow-up assessments, or both. However, the follow-up assessments were conducted at a variety of different time points (e.g., 1 month, 6 weeks, and 3 months after the intervention), which made it difficult to conduct meta-analyses for results of follow-up assessments.
Regarding participants’ diseases/conditions, participants in most studies (n = 27) were ADRD patients, four were stroke patients (20, 32–34), two were patients with ischemic heart disease (35, 36), and one were general palliative care patients (37). The number of participants ranged from 11 to 488, with most studies (n = 29) had fewer than 100 participants. Participants in most studies (n = 28) were recruited from certain types of institutions, including hospitals, nursing homes/old age homes/care homes or long-term care facilities in general, assisted living facilities, and medical centers. Participants in three studies were community-dwelling older adults (20, 38, 39). Participants in two studies were recruited from multiple sources (37, 40), and one study unclear (34).
Most studies (n = 29) reported significant between-group results in at least one outcome domain at one time point. For outcomes measured only in one study, Wu and Koo (44) found that the interaction term between group and time for hope was significant (P < 0.001), indicating the changes over time in hope was different between the intervention and the control group. No significant differences were found for self-esteem in Morgan (42) or for meaning in life in Allen et al. (37). Meta-analysis results for other outcomes are reported in one section below.
Risks of bias were summarized in Figure 2. Regarding random sequence generation, 17 studies were judged to be at low risk, which used drawing lots, random numbers (using a table or envelopes), and randomization software. Four studies were judged to be at high risk in this domain. Specifically, in Duru Aşiret and Kapucu (49); Van Bogaert et al. (40), and Wang (54), odd-number participants were assigned into the control group and even numbers into the intervention group. In Morgan (42), the initial participants were randomly assigned alternatively to the groups, while subsequent participants were allocated to groups using randomization by minimization.
For allocation concealment, six studies were judged to be at low risk, including five that used sealed envelopes (38, 39, 51, 53, 56), and one study in which the whole randomization process was conducted by an accredited clinical trials unit (46). A majority of studies (n = 24) did not report information on allocation concealment, and the remaining four studies (40, 42, 49, 54) were judged to be at high risk.
Regarding blinding participants and interventionists, 14 studies were rated as high risk and 20 studies as unclear, with no studies judged to be at low risk. Meanwhile, 13 studies were judged as low risk for blinding outcome assessment, by using personnel not included in the intervention process. In four studies (42, 50, 51, 57), evaluators were not blind to group assignment. Seventeen studies did not provide information in this domain.
One study (37) was judged to be at high risk for incomplete outcome data because of a high dropout rate at the baseline assessment (41% dropped out), and the dropout rate was higher in intervention group than in control group. One study (44) did not provide information for dropouts and thus rated as unclear. The remaining studies were all rated as low risk in this domain. Lastly, two studies were judged as high risk for selective reporting. Allen et al. (37) did not report results for follow-up assessments, and Serrani Azcurra (43) did not report anxiety and depression scores that were stated to have been measured, based on the article’s methods section.
We performed meta-analysis with outcomes that were measured in at least two studies. We found that most of our meta-analyses showed considerable heterogeneity, and further performed sensitivity and subgroup analyses. However, heterogeneity was not improved. We reported sensitivity and subgroup analyses for depression as an example. Subgroup analyses for other outcomes are available upon request.
Twenty-four studies representing 1,756 participants reported data on depression and were pooled for a meta-analysis using the random-effects model. Considerable heterogeneity was identified (I2 = 94%, P < 0.00001), while results showed that there were significant standardized mean differences in favor of life review intervention compared with controls for depression [SMD = −1.07, 95% CI (−1.52, −0.63), P < 0.00001] (Figure 3). Sensitivity analysis was performed but high heterogeneity still existed. Based on the forest plot, there were two outliers. After removing Li et al. (47), I2 was 92% [SMD = −0.84, 95% CI (−1.22, −0.45)]; after removing Li (33), I2 was 92% [SMD = −0.88, 95% CI (−1.27, −0.49)].
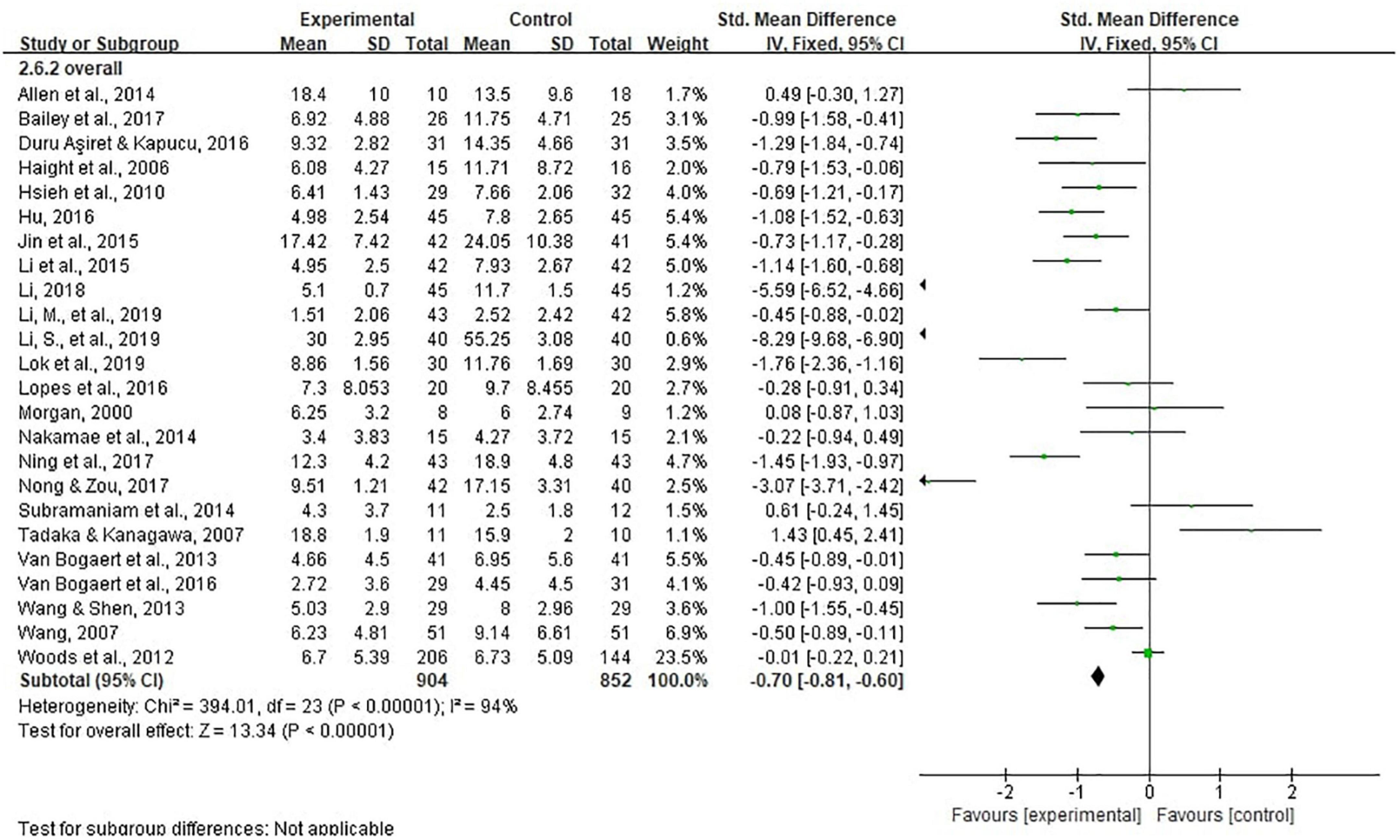
Figure 3. Effect size of the intervention group versus the control group on depression rating scores.
We also performed subgroup analyses with various possible reasons for heterogeneity (e.g., study quality, cognition, measurement tool, outcome rater, control group, country/region, intervention weeks, number of intervention sessions) (Table 2). However, heterogeneity remained high in subgroups except for two studies in UK [I2 = 53%, SMD = −0.05, 95% CI (−0.51, 0.41), P = 0.83], and two studies in Taiwan [I2 = 0%, SMD = −0.57, 95% CI (−0.88, −0.26), P = 0.0004]. Meanwhile, a significant difference (P = 0.0005) was found in terms of country/region where the study was conducted. Although with considerable heterogeneity (I2 = 97%), pooled results of eight studies in China showed a SMD of −2.39 [95% CI (−3.37, −1.42), P < 0.00001], an absolute value much larger than those in other countries and regions.
Five studies representing 624 participants reported data on anxiety and were pooled for a meta-analysis using the random-effects model. Considerable heterogeneity was identified (I2 = 98%, P < 0.00001), while results showed that there were significant standardized mean differences in favor of life review intervention compared with controls for anxiety [SMD = −3.54, 95% CI (−5.52, −1.56), P = 0.0005] (Figure 4).
Eleven studies representing 936 participants reported data on QOL. Random-effects model showed considerable heterogeneity (I2 = 92%, P < 0.00001) and significant standardized mean differences was in favor of life review intervention [SMD = 0.87, 95% CI (0.34, 1.41), P = 0.001] (Figure 5).
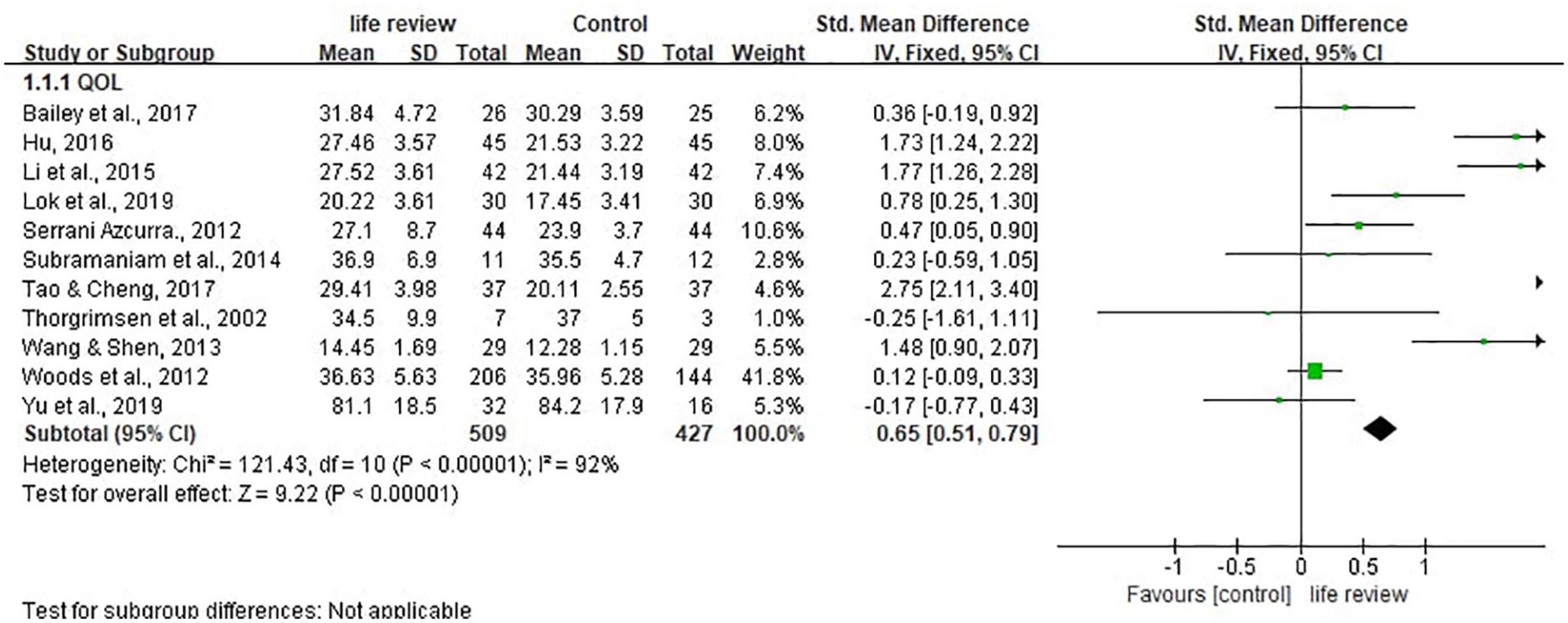
Figure 5. Effect size of the intervention group versus the control group on quality-of-life rating scores.
Three studies (34, 42, 44) with a total of 164 participants were pooled using the random-effects model. Results showed considerable heterogeneity (I2 = 95%, P < 0.00001) and no significant differences between the intervention and the control groups in life satisfaction (P = 0.16) (Figure 6A).
Mood was measured in two studies (39, 45) using the Alzheimer’s Disease and Related Dementia Mood Scale, with five domains (i.e., hostile, apathetic, sad, contented, and spirited) that are categorized into positive (including contended and spirited) and negative moods (including hostile, apathetic, and sad). Meta-analyses with 78 participants showed low heterogeneity and significant standardized mean differences in favor of life review intervention in increasing one’s positive moods and decreasing negative moods [positive: I2 = 0%, SMD = 0.97, 95% CI (0.49, 1.46), P < 0.0001; negative: I2 = 0%, SMD = −1.00, 95% CI (−1.49, −0.51), P < 0.0001] (Figures 6B, C).
Two studies (50, 58) with a total of 93 measured the apathy outcome, an indicator of motivation to get things done. Due to different score directions, scores in Manav and Simsek (50) were reversed to make them comparable to the other study. Results showed considerable heterogeneity (I2 = 97%, P < 0.00001) and no significant differences between the intervention and the control groups in apathy (P = 0.48) (Figure 6D).
Two studies (37, 44) measured spirituality well-being; however, results could not be pooled for the meta-analysis. In Allen et al. (37), four subscales (daily spiritual experience, forgiveness, meaning, abandonment by God) with different score directions of Brief Multidimensional Measure of Religiousness and Spirituality (BMMRS) were used. As the instrument’s development teams did not suggest combining the subscale scores (59), we did not generate a combined score to perform the meta-analysis. Regarding the results, Allen et al. (37) reported that, compared to the control group, intervention group expressed more forgiveness [F(1,25) = 5.24, P = 0.031; partial eta-squared = 0.17] and less abandonment by God [F(1,25) = 4.88, P = 0.037; partial eta-squared = 0.16]. While for Wu and Koo (44), spirituality well-being score increased in the intervention group but decreased in the control group, with a significant time x group interaction term (P < 0.001).
Two studies (43, 55) with 154 participants measured participants’ general well-being and results were pooled for meta-analysis. With a low heterogeneity (I2 = 0), no significant differences were found between the intervention and control groups in general well-being (P = 0.45) (Figure 6E).
Publication bias was assessed for depression and QOL through visually inspecting asymmetry in the funnel plots. The funnel plot showed asymmetry indicating potential publication bias was present in this review, which might have influenced the results (Figures 7, 8).
This systematic review and meta-analysis study examined the effects of life review on psychospiritual outcomes among older adults with LTI. A total of 34 studies representing 2,752 participants were identified. Our results indicated that life review could benefit older adults with LTI in decreasing anxiety, depression, and negative mood, and enhancing their positive mood and QOL. Meanwhile, many other psychospiritual outcomes were measured less frequently, and high-quality studies were lacking.
Previous meta-analyses for older adults also showed the effects of life review on decreasing depression (15, 16). However, the effects of life review on QOL were not significant in Lan et al. (16). It could be because of the small number of studies included for meta-analyses in Lan et al. (16): only two studies were pooled for the effects of QOL. It could also be because, while their study focused on the general older adult population, our study focused on older adults with LTI, which is a group of individuals who have been undergoing great distress because of their physical and psychological conditions (3), and thus the therapeutic benefits of life review could be more likely to manifest among this population. Life review interventions encourage older people to remember and talk about their life histories. In doing so, older adults with LTI recognize their strengths and resilience and feel satisfaction from knowing that their lives have meaning. In other words, life review brings the resilience, hardiness, and wisdom of life experiences and lessons learned; the more, the less vulnerability and risk of illnesses. It is noteworthy that during the life review sessions, both positive and negative life experiences may be brought about. While positive experiences make participants feel delighted and fulfilled, adverse life events also have meanings. By reviewing negative ones, older adults with LTI may re-evaluate the experience and come to peace with the past and the present, thus increasing their resilience to cope with difficult, stressful, and traumatic situations.
In addition to depression, anxiety, and QOL, measured in at least five studies, other psychospiritual outcomes included life satisfaction, mood, apathy, spirituality, self-esteem, meaning in life, hope, and general well-being. Only a small number of studies measured them; thus, it is less possible to draw a firm conclusion about the effectiveness of life review. However, these concepts were hugely important for older adults living with LTI: even with a heightened awareness of mortality, people living with LTI would try to have a positive outlook on life and tend to focus more on family and relationships (7). They would also respond to loss and suffering by becoming certain and taking control of the uncontrollable (4). Additionally, many people with LTI reported relying on religion to cope with their illnesses (2). Thus, we call for more research on interventions for older adults living with LTI to include more psychospiritual outcome measures, such as hope and self-esteem, to understand better this population’s remarkable story of growth and transformation through adversity. Life review, by its name, could be a valuable tool to discuss their life experiences and solicit their thoughts and feelings for the past, present, and future.
In this review, high-quality evidence is lacking, and only a few studies were judged to be at low risk in at least five risk of bias domains. Although half studies were rated as low risk in the random sequence generation, only a few reported adequate allocation concealment. No study was rated as low risk in blinding of participants and personnel; however, this is indeed difficult to achieve in psychosocial interventions, as interventionists and participants are naturally aware of the intervention activities. However, more than half of the studies did not report blinding of outcome assessment, or outcome assessors were not blinded. This could generate bias as unblinded assessors might exaggerate the intervention effects. In the future, studies with a more rigorous study design should be implemented, paying special attention to random sequence generation, allocation concealment, and blinding of outcome assessment.
This study has several limitations. First, we only included English and Chinese literature due to the team’s language capacity, and thus excluded potentially useful information written in other languages. Second, we used the WHO’s list of leading causes of death as criteria for LTI. However, people could undergo different stages of an illness, and patients with certain illnesses or in specific stages (such as early stages of cancer) do not face impending death. Third, studies that used four multi-dimensional measurement tools were not included in the meta-analysis. This could bring a risk of bias due to missing results in synthesis. Fourth, this study might be limited by the selected databases. Although the investigators included the most widely used English and Chinese databases, it remains possible that some works, particularly unpublished studies conducted in other countries, were not located and examined. Finally, our meta-analysis results also showed considerable heterogeneity, which could be because of great variations in terms of intervention format, length, setting, study quality, and other study characteristics; however, we believe this study serves as one of the first steps for the team to go deeper into researching the intervention effects on psychospiritual outcomes, and thus in the current stages, studies including this one are still exploratory.
Future research implications are as follows. First, more well-designed RCT studies are warranted to evaluate the psychospiritual effects of life review interventions among older adults with LTI. The outcome should include not only depression, anxiety, and QOL, but also other psychospiritual outcomes crucial to one’s holistic well-being. We also call for more rigorous design, especially high-quality designs that minimize biases in domains of random sequence generation, allocation concealment, and blinding of outcome assessment. In addition, studies with larger sample sizes are necessary to clarify the efficacy. Finally, future research can include qualitative studies to obtain the opinions of participants with different backgrounds on the optimal time, length, number of sessions, and other characteristics of life review interventions.
Despite some limitations, the study findings support a positive effect of life review on psychospiritual outcomes among older adults with LTI. Healthcare providers in different settings should continue to utilize life review for this population. They should measure and monitor their effects on different psychospiritual outcomes, to investigate how these interventions help them cope with challenges, increase resilience, and maintain hope and a deeply experienced sense of self-identity in the intersection of old age and life-threatening illness.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
ML, YW, and IC designed the study. ML and YW conducted the title and abstract screening. ML drafted the manuscript. All authors extracted the data and attended the group meetings to reach a consensus, critically reviewed it and provided the feedback, and contributed to the article and approved the submitted version.
This study was supported by the Fundamental Research Funds for the Central Universities (JBK22YJ07).
We want to thank researchers from the following two projects for their assistance in meta-analysis methods: Lanzhou University Research and Interpretation of the Spirit of the 20th National Congress of the Communist Party of China: The Research on the Digital Transformation of Social Work for Chinese older adults Based on the Healthy China Strategy (2023lzdxjbkyzx006); and the Major Project of the National Social Science Fund of China: Research on the Theoretical System, International Experience and Chinese Path of Evidence-based Social Science (19ZDA142).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National Institute on Aging. Geroscience: The Intersection of Basic Aging Biology, Chronic Disease, and Health. (2021). Available online at: http://www.nia.nih.gov/research/dab/geroscience-intersection-basic-aging-biology-chronic-disease-and-health (accessed January 12, 2021).
2. Hong EPW, Margaret O, Leng CY, Kannuasamy P. The lived experience of older Chinese Singaporeans with life-threatening illnesses in an inpatient hospice. Prog Palliat Care. (2012) 20:19–26. doi: 10.1179/1743291X12Y.0000000004
3. Kasiram M, Sartori P. Positive living strategies that can be learned from studies on near-death experiences and life-threatening illnesses. Soc Work. (2015) 51:456–66. doi: 10.1080/09540129650125704
4. Bruce A, Sheilds L, Molzahn A, Beuthin R, Schick-Makaroff K, Shermak S. Stories of liminality: living with life-threatening illness. J Holist Nurs. (2014) 32:35–43. doi: 10.1177/0898010113498823
5. Gleig A. Psychospiritual. In: DA Leeming, K Madden, S Marlan editors. Encyclopedia of Psychology and Religion. (Boston, MA: Springer) (2010).
6. Ellis J. Thinking beyond rupture: continuity and relationality in everyday illness and dying experience. Mortality. (2013) 18:251–69. doi: 10.1080/13576275.2013.819490
7. Holder GN, Young WC, Nadarajah SR, Berger AM. Psychosocial experiences in the context of life-threatening illness: the cardiac rehabilitation patient. Palliat Support Care. (2015) 13:749–56. doi: 10.1017/S1478951514000583
8. Lin H-R, Bauer-Wu SM. Psycho-spiritual well-being in patients with advanced cancer: an integrative review of the literature. J Adv Nurs. (2003) 44:69–80. doi: 10.1046/j.1365-2648.2003.02768.x
9. Keall RM, Clayton JM, Butow PN. Therapeutic life review in palliative care: a systematic review of quantitative evaluations. J Pain Symptom Manage. (2015) 49:747–61. doi: 10.1016/j.jpainsymman.2014.08.015
10. Zhang X, Xiao H, Chen Y. Effects of life review on mental health and well-being among cancer patients: a systematic review. Int J Nurs Stud. (2017) 74:138–48. doi: 10.1016/j.ijnurstu.2017.06.012
11. Huang H, Chen Y, Chen P, Huey-Lan Hu S, Liu F, Kuo Y, et al. Reminiscence therapy improves cognitive functions and reduces depressive symptoms in elderly people with dementia: a meta-analysis of randomized controlled trials. J Am Med Dir Assoc. (2015) 16:1087–94. doi: 10.1016/j.jamda.2015.07.010
12. Fowler SN, Pruthi R. Resilience: definitions, ambiguities, and applications. In: B Resnick, LP Gwyther, KA Roberto editors. Resilience in Aging: Concepts, Research, and Outcomes. (New York, NY: Springer) (2011). p. 1–14.
13. Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. (2000) 71:543–62. doi: 10.1111/1467-8624.00164
14. Birren JE, Kenyon GM, Ruth J-E, Schroots JJF, Svensson T editors. Aging and Biography: Explorations in Adult Development. New York, NY: Springer (1996).
15. Bohlmeijer E, Smit F, Cuijpers P. Effects of reminiscence and life review on late-life depression: a meta-analysis. Int J Geriatr Psychiatry. (2003) 18:1088–94. doi: 10.1002/gps.1018
16. Lan X, Xiao H, Chen Y. Effects of life review interventions on psychosocial outcomes among older adults: a systematic review and meta-analysis. Geriatr Gerontol Int. (2017) 17:1344–57. doi: 10.1111/ggi.12947
17. Nall R. Life Review Therapy. (2018). Available online at: https://www.healthline.com/health/life-review-therapy (accessed January 11, 2021).
18. Gil I, Costa P, Parola V, Cardoso D, Almeida M, Apostolo J. Efficacy of reminiscence in cognition, depressive symptoms and quality of life in institutionalized elderly: a systematic review. Rev Esc Enferm USP. (2019) 53:e03458. doi: 10.1590/S1980-220X2018007403458
19. Westerhof GJ, Slatman S. In search of the best evidence for life review therapy to reduce depressive symptoms in older adults: a meta-analysis of randomized controlled trials. Clin Psychol Sci Pract. (2019) 26:e12301.
20. Ning X, Wang Y, Sha S, Zheng Y, Zhao D, Xie T, et al. The effect of structured group reminiscence therapy on the elderly patients with post stroke depression in community [Jiegouhua tuanti huaijiu liaofa dui shequ laonian cuzhong hou yiyu huanzhe de yingxiang]. J Chengdu Med Coll. (2017) 12:510–3. doi: 10.3969/j.issn.1674-2257.2017.04.033
21. Hsieh H-F, Wang J-J. Effect of reminiscence therapy on depression in older adults: a systematic review. Int J Nur Stud. (2003) 40:335–45. doi: 10.1016/S0020-7489(02)00101-3
22. Istvandity L. Combining music and reminiscence therapy interventions for wellbeing in elderly populations: a systematic review. Complement Ther Clin Pract. (2017) 28:18–25. doi: 10.1016/j.ctcp.2017.03.003
23. Subramaniam P, Woods B. The impact of individual reminiscence therapy for people with dementia: systematic review. Expert Rev Neurother. (2012) 12:545–55. doi: 10.1586/ern.12.35
24. Woods B, O’Philbin L, Farrell EM, Spector AE, Orrell M. Reminiscence therapy for dementia. Cochrane Database Syst Rev. (2018) 3:CD001120. doi: 10.1002/14651858.CD001120.pub3
25. Cengage. Life Review. Encyclopedia.com. (2021). Available online at: https://www.encyclopedia.com/social-sciences-and-law/sociology-and-socialreform/sociology-general-terms-and-concepts/life-review (accessed January 11, 2021).
26. Chen Y, Xiao H, Yang Y, Lan X. The effects of life review on psycho-spiritual well-being among patients with life-threatening illness: a systematic review and meta-analysis. J Adv Nurs. (2017) 73:1539–54. doi: 10.1111/jan.13208
27. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed1000097
28. World Health Organization. The Top 10 Causes of Death. (2020). Available online at: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed January 11, 2021).
29. Ryan R, Hill S, Broclain D, Horey D, Oliver S, Prictor M. Study Design Guide. London: The Cochrane Collaboration (2013).
30. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ editors, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (updated September 2020). London: Cochrane (2020).
31. Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928–5928. doi: 10.1136/bmj.d5928
32. Jin Y, Tu W, Chen C. Nostalgic therapy for elderly patients with Alzheimer’s disease [Huaijiu liaofa zai laonian chidai huanzhe zhong de zuoyong]. Zhejiang Med. (2016) 38:717–21. doi: 10.3928/0098-9134-19920101-03
33. Li H. Effect of nostalgic therapy on depressive symptoms and quality of life in elderly patients with stroke [Huaijiu liaofa dui laonian naocuzhong huanzhe yiyu zhengzhuang ji shenghuo zhiliang de yingxiang]. Jilin Med. (2018) 39:1368–70.
34. Mei Y, Lin B, Li Y, Ding C, Zhang Z. Effects of modified 8-week reminiscence therapy on the older spouse caregivers of stroke survivors in Chinese communities: a randomized controlled trial. Int J Geriatr Psychiatry. (2018) 33:633–41. doi: 10.1002/gps.4833
35. Li J, Yang Q, Li L, Wang A, Bian L, Yin N, et al. The effect of narrative therapy on elderly patients with coronary heart disease, constipation, and anxiety [Xushi huli dui laonian guanxinbing bianmi hebing jiaolv huanzhe de yingxiang fenxi]. J Clin Nurs Pract. (2017) 2:18–9.
36. Wang L. Application of narrative nursing to older patients with coronary heart disease, constipation, and anxiety [Xushi huli dui laonian guanxinbing binami hebing jiaolv huanzhe de yingyong]. Our Health. (2019) 6:244–5.
37. Allen RS, Harris GM, Burgio LD, Azuero CB, Miller LA, Shin HJ, et al. Can senior volunteers deliver reminiscence and creative activity interventions? Results of the legacy intervention family enactment randomized controlled trial. J Pain Symptom Manage. (2014) 48:590–601. doi: 10.1016/j.jpainsymman.2013.11.012
38. Thorgrimsen L, Schweitzer P, Orrell M. Evaluating reminiscence for people with dementia: a pilot study. Arts Psychother. (2002) 29:93–7. doi: 10.1016/S0197-4556(01)00135-6
39. Yu F, Mathiason MA, Johnson K, Gaugler JE, Klassen D. Memory matters in dementia: efficacy of a mobile reminiscing therapy app. Alzheimers Dement (N Y). (2019) 5:644–51. doi: 10.1016/j.trci.2019.09.002
40. Van Bogaert P, Van Grinsven R, Tolson D, Wouters K, Engelborghs S, Van der Mussele S. Effects of SolCos model-based individual reminiscence on older adults with mild to moderate dementia due to Alzheimer disease: a pilot study. J Am Med Dir Assoc. (2013) 14:528.e9–13. doi: 10.1016/j.jamda.2013.01.020
41. Hu P. Application of nostalgic therapy in nursing of Alzheimer’s patients [Huaijiu liaofa zai laonian chidai huanzhe huli zhong de yingyong yanjiu]. J Clin Med Pract. (2016) 20:15–7. doi: 10.7619/jcmp.201622005
42. Morgan S. The Impact of a Structured Life Review Process on People With Memory Problems Living in Care Homes (Publication No. U126001). Ann Arbor, MI: ProQuest Dissertations Publishing (2000).
43. Serrani Azcurra D. A reminiscence program intervention to improve the quality of life of long-term care residents with Alzheimer’s disease: a randomized controlled trial. Braz J Psychiatry. (2012) 34:422–33. doi: 10.1016/j.rbp.2012.05.008
44. Wu LF, Koo M. Randomized controlled trial of a six-week spiritual reminiscence intervention on hope, life satisfaction, and spiritual well-being in elderly with mild and moderate dementia. Int J Ger Psychiatry. (2016) 31:120–7. doi: 10.1002/gps.4300
45. Haight BK, Gibson F, Michel Y. The Northern Ireland life review/life storybook project for people with dementia. Alzheimers Dement. (2006) 2:56–8. doi: 10.1016/j.jalz.2005.12.003
46. Subramaniam P, Woods B, Whitaker C. Life review and life story books for people with mild to moderate dementia: a randomised controlled trial. Aging Ment Health. (2014) 18:363–75. doi: 10.1080/13607863.2013.837144
47. Li S, Yu G, Chen J, Zhang R. Application of personalized narrative nursing in elderly patients with chronic obstructive pulmonary disease [Gexinghua xushi huli zai laonian manxing zusexing feijibing bingren zhong de yingyong]. Chin Nurs Res. (2019) 33:2903–5. doi: 10.12102/j.issn.1009-6493.2019.16.043
48. Wang Y, Shen C. An intervention of life story book on older adults with dementia [Jiyu shenghuo gushi shu de laonian chidai d ganyu yanjiu]. Chin J Gerontol. (2013) 33:5239–41. doi: 10.3969/j.issn.1005-9202.2013.21.007
49. Duru Aşiret G, Kapucu S. The effect of reminiscence therapy on cognition, depression, and activities of daily living for patients with Alzheimer disease. J Geriatr Psychiatry Neurol. (2016) 29:31–7. doi: 10.1177/0891988715598233
50. Manav A, Simsek N. The effect of reminiscence therapy with internet-based videos on cognitive status and apathy of older people with mild dementia. J Geriatr Psychiatry Neurol. (2019) 32:104–13. doi: 10.1177/0891988718819864
51. Lok N, Bademli K, Selcuk-Tosun A. The effect of reminiscence therapy on cognitive functions, depression, and quality of life in Alzheimer patients: randomized controlled trial. Int J Geriatr Psychiatry. (2019) 34:47–53. doi: 10.1002/gps.4980
52. Nakamae T, Yotsumoto K, Tatsumi E, Hashimoto T. Effects of productive activities with reminiscence in occupational therapy for people with dementia: a pilot randomized controlled study. Hong Kong J Occup Ther. (2014) 24:13–9. doi: 10.1016/j.hkjot.2014.01.003
53. Van Bogaert P, Tolson D, Eerlingen R, Carvers D, Wouters K, Paque K, et al. SolCos model-based individual reminiscence for older adults with mild to moderate dementia in nursing homes: a randomized controlled intervention study. J Psychiatr Ment Health Nurs. (2016) 23:568–75. doi: 10.1111/jpm.12336
54. Wang J-J. Group reminiscence therapy for cognitive and affective function of demented elderly in Taiwan. Int J Geriatr Psychiatry. (2007) 22:1235–40. doi: 10.1002/gps.1821
55. Lai CKY, Kayser-Jones J. Randomized controlled trial of a specific reminiscence approach to promote the well-being of nursing home residents with dementia. Int Psychogeriatr. (2004) 16:33–49. doi: 10.1017/s1041610204000055
56. Li M, Lyu J-H, Zhang Y, Gao M-L, Li R, Mao P-X, et al. Efficacy of group reminiscence therapy on cognition, depression, neuropsychiatric symptoms, and activities of daily living for patients with Alzheimer disease. J Geriatr Psychiatry Neurol. (2019):1–10. doi: 10.1177/0891988719882099
57. Tadaka E, Kanagawa K. Effects of reminiscence group in elderly people with Alzheimer disease and vascular dementia in a community setting. Geriatr Gerontol Int. (2007) 7:167–73. doi: 10.1111/j.1447-0594.2007.00381.x
58. Hsieh C-J, Chang C, Su S-F, Hsiao Y-L, Shih Y-W, Han W-H, et al. Reminiscence group therapy on depression and apathy in nursing home residents with mild-to-moderate dementia. J Exp Clin Med. (2010) 2:72–8.
59. Fetzer Institute. Multidimensional Measurement of Religiousness/Spirituality for use in Health Research. Kalamazoo, MI: Fetzer Institute (1999).
60. Bailey EM, Stevens AB, LaRocca MA, Scogin F. A randomized controlled trial of a therapeutic intervention for nursing home residents with dementia and depressive symptoms. J Appl Gerontol. (2017) 36:895–908. doi: 10.1177/0733464815627956
61. Li L, Ge Z, Deng X. The effect of reminiscence therapy on patients with Alzheimer’s disease [Huaijiu liaofa zai laonian chidai huanzhe zhong de yingyong]. Chin J Nurs. (2015) 30:1–4. doi: 10.3870/j.issn.1001-4152.2015.19.001
62. Lopes TS, Afonso RMLBM, Ribeiro ÓM. A quasi-experimental study of a reminiscence program focused on autobiographical memory in institutionalized older adults with cognitive impairment. Arch Gerontol Geriatr. (2016) 66:183–92. doi: 10.1016/j.archger.2016.05.007
63. Nong D, Zou X. The effect of nostalgia therapy on the cognition and depression of older dementia patients [Huaijiu liaofa dui laonian chidai huanzhe renzhi gongneng ji yiyu qingxu de yingxiang]. J Clin Nurs Pract. (2017) 2:135–8.
64. Tao R, Cheng Q. Effects of reminiscence nursing therapy on cognitive function and quality of life in elderly patients with dementia [Huaijiu huli liaofa dui laonian chidai huanzhe renzhi gongneng ji shenghuo zhiliang de yingxiang]. China Contin Med Educ. (2017) 9:263–4. doi: 10.3969/j.issn.1674-9308.2017.22.139
Keywords: life review, psychospiritual well-being, life-threatening illness, quality-of-life, older adult, anxiety, depression
Citation: Liu M, Wang Y, Du Y and Chi I (2023) Life review on psychospiritual outcomes among older adults with life-threatening illnesses: A systematic review and meta-analysis. Front. Psychiatry 14:1077665. doi: 10.3389/fpsyt.2023.1077665
Received: 23 October 2022; Accepted: 03 February 2023;
Published: 28 February 2023.
Edited by:
Zeng-Jie Ye, Guangzhou University of Chinese Medicine, ChinaReviewed by:
Yajing Zhong, Katholieke Universiteit Leuven, BelgiumCopyright © 2023 Liu, Wang, Du and Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Wang,  d2FuZ3lpbmdldmVyQGx6dS5lZHUuY24=
d2FuZ3lpbmdldmVyQGx6dS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.