
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry , 18 October 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.998888
This article is part of the Research Topic Community Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic - Volume II View all 11 articles
 Salmi Razali1,2,3
Salmi Razali1,2,3 Jo Anne Saw1*
Jo Anne Saw1* Nurul Azreen Hashim1
Nurul Azreen Hashim1 Nor Jannah Nasution Raduan1
Nor Jannah Nasution Raduan1 Dina Tukhvatullina4
Dina Tukhvatullina4 Daria Smirnova5,6
Daria Smirnova5,6 Konstantinos N. Fountoulakis7
Konstantinos N. Fountoulakis7During the COVID-19 pandemic, numerous social and life changes were implemented to curb the spread of the disease. The effect of lockdown and isolation predisposes the general population to various psychological health concerns. The existing determinants of suicidal behaviour were further added with social isolation, financial stress, depression, and other pandemic-related stressors. Hence, our study aimed to investigate suicidal behaviour and the associated factors among Malaysians during the COVID-19 pandemic. It is a cross-sectional online questionnaire survey that used convenient sampling, where the survey was disseminated to the public via Google Forms through social media during the first wave of the COVID-19 pandemic in Malaysia. This study is also part of a large international COVID-19 mental health international study for the general population (COMET-G). This research revealed concerns about issues related to suicidal behaviours during the beginning of the COVID-19 pandemic. Suicidal behaviours were associated with depression, sex, marital status, educational level, employment type, residential area, number of people living together, number of children, and family dynamics. The pandemic effects from psychological, social, and economic perspectives will definitely take more time for recovery. Future prevention and protection are needed especially for the highly at-risk group on top of the general population in any future unforeseen circumstances of the pandemic.
The COVID-19 infection leaves long-term neuropsychiatric symptoms, including sleep problems, anxiety, depressed mood, and irritability, making them more vulnerable to mental health disturbances. Furthermore, the effects of lockdown, isolation, and quarantine predisposed the general population to psychological and emotional burdens, putting them at risk of mental health disorders (1). Although COVID-19 had its outbreak in China in December 2019, Malaysia only had the first COVID-19 case in February 2020. Due to this threat, Malaysia had its first movement control order (MCO) on 18 March 2020 (2). During this time, travelling across districts and states was to be avoided, and mass gatherings were postponed, especially in religious houses. These continued in a few separate episodes until the end of 2021 (3).
There was heterogeneous nomenclature for definitions of suicidal behaviour according to literature. Suicidal behaviour is defined as suicide attempts, which are self-directed injurious acts with at least some intent to end one’s own life, which range from completed suicide to highly lethal and failed suicide attempts to low-lethality, usually impulsive attempts due to social crisis (4). Factors affecting suicidal behaviour are complex and variable. These factors can generally be divided into sociodemographic, socioeconomic, socio-political, geographical, cultural, lifestyle, and health- or clinical-related factors (5). Personality and individual differences, cognitive factors, social aspects, and adverse life events are the main psychological factors contributing to the suicidal behaviour (6). The Malaysian data collected before the COVID-19 pandemic showed that the determinants of suicidal behaviour were income, age, gender, ethnicity, education, marital status, self-rated health, and being diagnosed with diabetes and hypercholesterolemia (7).
During the COVID-19 pandemic, the existing determinants of suicidal behaviour were added to social isolation, financial stress, depression, limited or variable access to healthcare services, and other pandemic-related stressors (8). Studies done during the COVID-19 pandemic found that suicidal ideation was associated with loneliness, anxiety, depression, insomnia, impaired family functioning, a history of mental health issues, alcohol misuse, COVID-19-related stress symptoms, concerns over COVID-19, having tested positive for COVID-19, a younger age, an unmarried or divorced marital status, living alone, being a military veteran, previous homelessness, financial strain, housing instability, unemployment, poor perceived quality of physical health, disability, and living with an individual with frail health (9–12). A study in Italy showed that 14% of respondents were at higher risk of having suicidal ideation after being unemployed due to the pandemic (13). While another study among healthcare workers (HCW) in Malaysia during the COVID-19 pandemic discovered that suicidal ideation was linked to depression and early career status of less than 10 years in service (14).
Our study investigated suicidal behaviour and the associated factors among Malaysians during the COVID-19 pandemic. This study is part of a large international COVID-19 mental health international study for the general population (COMET-G).
This study is part of the global joint project of more than 40 countries worldwide initiated by the Aristotle University of Thessaloniki and the Mental Health Sector of the Scientific Research Institute of the Pan-Hellenic Medical Association, Greece. It is a cross-sectional online questionnaire survey that used convenient sampling.
In Malaysia, the survey was disseminated to the public using Google Forms through social media (e.g., Facebook and Twitter) during the first wave of the COVID-19 pandemic. The distribution of the survey was done from 1 July 2020 (average of six cases per week) to 6 October 2020 (average of 338 cases per week) during the initial wave of the COVID-19 pandemic in Malaysia.
The selection criteria were participants aged 18 years and above, who could read Malay or English, and who had access to the internet to receive the online form. All potential participants were provided with an explanation regarding the risk and benefits of the study on the introductory page of the online questionnaire. Participants who agreed to participate were invited to answer the questionnaires. Implied consent was gathered when the participant proceeded to the next page, where the actual survey began. This study was approved by the local institutional research ethics committee, REC/06/2020 (MR/109).
Embedded in the survey was Pro Forma questionnaire for sociodemographic data, including sex, age, marital status, residential areas, educational status, employment, and status of being a HCW status, living condition (including the number of people living together, number of children, and status of living with a vulnerable family member), and their background medical disease. The detailed categorisation of independent variables followed the main COMET-G study, which include sex statuses (female, male, and other/do not want to declare), age (years old) (≤ 21, 22–45, 46–60, and ≥ 61), marital status [single or married (or in a civil partnership), divorced (or estranged), co-habitant, widower, or other], educational level (elementary school or less, high school degree or equivalent, bachelor’s degree, master’s degree, and doctorate), residential area [capital city, city > 1 million population, city (100,000–1 million population), town (20,000–100,000 inhabitants), town (< 20,000 inhabitants), rural area to village and other], number of people living together (one, two, three, four, and five or more), number of children (zero, one, two, three, and four or more), living with vulnerable people (No or Yes), employment status (working at the public sector, working at private sector, self-employed, retired, unemployed, housekeeper, college or university students, not working by choice, and other), status as HCW (doctor, nurse, other HCW with direct contacts to clinical work, administrative employee at a hospital, other hospital staff, and do not work in the health sector), and status of the chronic medical illness (No or Yes).
For mental health status, the presence of depression and anxiety were assessed with the Center for Epidemiologic Studies Depression Scale (CES-D) and the State-Trait Anxiety Inventory (STAI-Y). The English version of these questionnaires was prepared by the lead collaborating centre, while the Malay version was prepared after translation and discussion between local researchers with reference to the Malay version of the questionnaires (15). The total scores of those questionnaires were used to indicate depression when the CES-D score was above the cut-off score of 23/24 and the algorithm score was above 9.03 as per the categorisation in COMET-G (16) and anxiety, respectively. Furthermore, statements assessing the emotional changes (joy and melancholy) were also included in the survey. Spirituality was also assessed using a Likert score ranging from 0 to 3.
Participants were also asked about the family dynamics during the lockdown due to the pandemic. Using Likert scores ranging from “−2 = much less,” “−1 = less,” “0 = same,” “1 = more,” and “2 = much more,” the participants were asked about their needs to communicate with other members of their family, receive emotional support from other members of the family, and the presence of any conflicts with the rest of your family members during the period of lockdown due to the pandemic. They were also asked about changes in the overall quality of relationships with the other members of their family compared to the one before the quarantine by choosing the score: “−2 = much worse,” “−1 = worse,” “0 = it has not changed,” “1 = a little bit better,” and “2 = much better.” Similar scoring was used for the status of the participant’s financial status. Furthermore, a question was also given about managing to maintain a basic daily routine (such as waking up in the morning, regular meals, sleeping hours, and routine activities) both for participants and their families, the scores ranged from “0 = not at all,” “1 = a little,” “2 = most of the times,” and “3 = always.” Finally, the level of difficulty managing their children’s daily life and behaviour was also asked, and the scores ranged from “−2 = much more difficult than before,” “−1 = somehow more difficult but not always,” “0 = same as always (also if the participant does not have children),” “1 = somehow easier but not always,” and “2 = much easier than before.” The overall family dynamics are represented by the total scores of all domains of the family dynamic scores.
Suicidal behaviour was measured with the Risk Assessment Suicidality Scale (RASS) (17). The English version of the survey was prepared by the lead collaborating centre, while the Malay version was prepared after translation and discussion between local researchers. The overall suicidal behaviour was indicated by the total score of RASS, while the suicidal intention, lifetime suicidal behaviour, and history of suicidal behaviour were assessed using the RASS subscales of “intention,” “life,” and “history,” respectively (17). The full protocol can be found elsewhere (16).
Descriptive statistics were calculated for the independent variables: key sociodemographic variables (including sex, age, marital status, educational level, residential area, number of people living together, number of children, employment, status as HCW, and the status of living with vulnerable people), health status (status of chronic medical illness, depression, and anxiety), family dynamics, and spirituality. All independent variables that are significant (p < 0.05) in bivariate analyses were included in the model. Multiple forward stepwise linear regression analyses were performed to investigate variables that could be the contributing factors for overall suicidal behaviour. Two-tailed p-value and 95% confidence intervals (95% CI) were provided. Statistical analyses were performed using IBM SPSS version 26.
The study sample included 963 participants; the majority were women (578; 60.0%) and a small proportion refused to declare their sex identity or chose “other” (74; 7.7%). The mean age of the participants was 40.1 ± 12.0 years, and about two-thirds (662; 68.7%) were between 22 and 45 years old. The majority (725; 75.3%) had tertiary education such as bachelor, master, or doctoral degree. Participants came from all types of residential areas, from rural areas (156; 16.2%) to towns (265; 27.5%) and city centres (517; 53.7%). Most of the participants were living with at least someone (916; 95.1%), less than one-third had no children (298; 30.9%), and about one-third were living with someone vulnerable (311; 32.3%). In terms of employment, about one-third were working in the public sector (357; 37.1%), and 129 (13.4%) of the participants were college or university students. The majority (817; 84.8%) did not work in the health sector. Table 1 shows further details of the sociodemographic background of the participants.
Of the total participants, 180 (18.7%) had chronic medical diseases as tabulated in Table 1. For depression, the mean ± SD of CESD scores was 21 ± 10.51 and the scores ranged from 3 to 56. For anxiety, the mean ± SD of STAI scores was 45.92 ± 9.60 and the scores ranged from 20 to 78. The mean ± SD for the total score of family dynamic parameters was −0.59 ± 3.70 and the scores ranged from −12.00 to 11.00. The spirituality score ranged from 0 to 3, with a mean ± SD of 1.74 ± 1.05.
Table 2 summarises the bivariate analyses of the associations between suicidal behaviours and the possible contributing factors. The tests showed that overall suicidal behaviours were associated with sex (F = 10.278, p < 0.001), marital status (F = 8.074, p < 0.001), educational level (F = 3.567, p = 0.003), employment type (F = 8.747, p < 0.001), residential area (F = 5.481, p < 0.001), number of people living together (F = 4.048, p = 0.003), number of children (F = 2.556, p = 0.038), depression (r = 0.440, p < 0.001), anxiety (r = 0.311, p < 0.001), and family dynamic (r = –0.088, p = 0.009). Overall suicidal behaviours and each domain of RASS (intention, lifetime, and history) were associated with sex, employment type, educational level, number of people living together, number of children, anxiety, and depression. On the contrary, none of the suicidal behaviour domains was associated with the existence of chronic medical diseases.
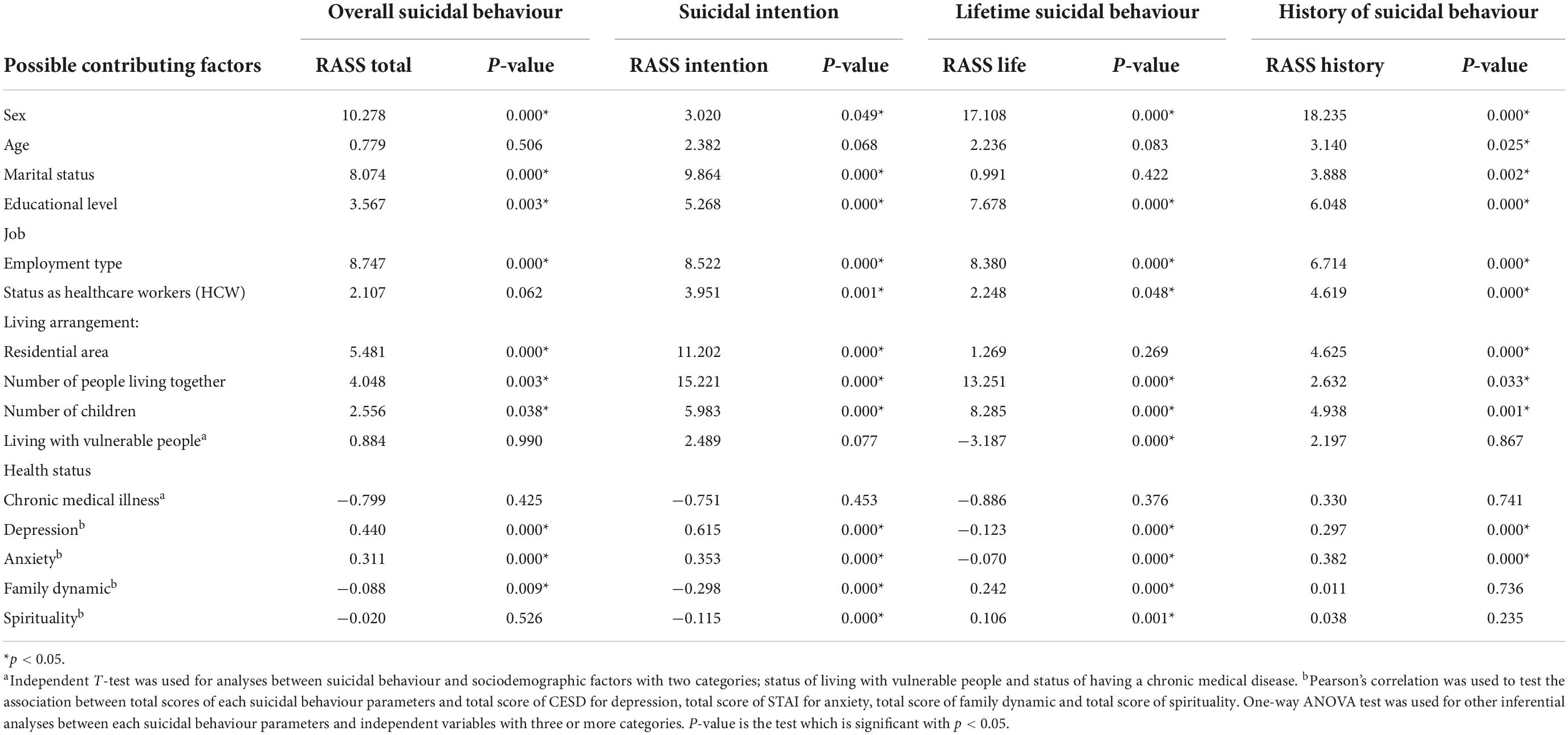
Table 2. The bivariate analyses of associations between suicidal behaviours and the possible contributing factors.
Table 3 summarises the multivariate forward linear regressions of three proposed models. All three models are statistically significant with low adjusted R2 and low collinearity scores. The first model includes depression, sex, family dynamic, and the number of people living together as the significant contributing factors to suicidal behaviours. The second model includes the number of children as another additional factor (a protective factor). The third model shows that depression, sex, family dynamics, number of people living together, the number of children, and marital status changes are significant contributing factors to suicidal behaviours.
Due to MCO during the COVID-19 pandemic, psychological effects were evident among the general population. Suicidal behaviour was one of the main outcomes of this study. We found that suicidal behaviour was highly associated with sex, marital status, educational level, employment type, residential area, number of people living together, number of children, and family dynamics. Most participants in this study were educated; therefore, they had better access to the internet and participated in this study. WHO found women to have a higher risk of suicidal behaviour, although they have lower rates of suicide compared to men. Knowledge of the importance of gender factors shows the importance of paying attention to each gender when suicidal behaviour is identified.
A straightforward explanation may be that women expressed suicidal behaviour more than men, probably due to higher emotional sensitivity toward stress, especially during adverse life events (18). A few other local studies found a higher prevalence of depression and anxiety among Malaysian women (19) and a higher rate of suicidal ideation among female HCW during the MCO (14).
According to a systematic review by Mamun (1), loneliness and social isolation caused by MCO during COVID-19 affected more those who are alone, such as those divorced, separated, widows, or those with no children or staying alone. These findings matched our findings that these sociodemographic factors had a higher risk of suicidal behaviour during the pandemic. Our study found that higher educational status was linked to suicidal behaviour during the pandemic. This could be explained by the fact that high educational attainment leads to stability in employment, and the pandemic causes a sudden loss of jobs, hence causing high frustration and distress. This is in line with other studies that found that a high educational level was associated with a higher risk of suicidal behaviours (20, 21). Those with unemployment were found to be associated with suicidal behaviours, and financial constraints may precipitate economic stunting during the pandemic (22).
This study found that suicidal behaviour during the COVID-19 pandemic was associated with depression and anxiety. This finding was similar to other studies done during the same time (1, 8, 10, 11). This finding was expected, as suicidal behaviour could be a manifestation of depression and anxiety and also the consequence of these psychological problems. Depression and anxiety are known risk factors for suicidal behaviour, and during the COVID-19 pandemic, people may develop depressive symptoms and anxiety following reports of deaths, increased media communications, and an escalating number of new cases (23). Another study found an association between depressive symptoms, COVID-19 preventive practice measures, daily activities in home quarantine, and suicidal behaviours (24). Another review of sociocultural risk and predisposing factors for suicidal behaviour in developing countries revealed that the fear of being infected with COVID-19, growing economic pressure, and lack of resources due to lockdown were significant (25).
Surprisingly, in our study, having a chronic medical illness was not a significant contributing factor to suicidal behaviour. This is contrary to findings by other studies, which demonstrated that the presence of comorbid medical illnesses like diabetes, cerebrovascular diseases, heart diseases, and other chronic conditions would increase the risk of developing mental health problems, including suicidal behaviour (9–11, 26, 27). We were unable to demonstrate the association between suicidal behaviour and having chronic medical illness because this study did not take into account the severity and types of the chronic medical illness. Another explanation was that a previous study showed the effect that medical illness has on a person’s life in terms of disruption to daily activity rather than the number of medical conditions that predict suicide risk (28), which could explain the lack of association in our study.
However, from an ethnocultural point of view, illness perception differs between different religions in Malaysia. Malay Muslims believed suffering and diseases were trials from God for a better life in the everlasting world, while Chinese Taoists perceived illnesses to be an imbalance of forces in the body system. On the contrary, Christians may believe illnesses are due to personal sins and are a form of cleansing (29).
There were some practical strategies for reducing and managing suicidal behaviours during the COVID-19 pandemic. The government needs to address COVID-19-related unemployment and financial insecurity through financial provisions like tax deferral, wage subsidy, and investment in the labour market programme, as well as support for employers, to help them retain their workers (30). In Malaysia, the government used fiscal policy to allocate a huge budget from the lowest income individuals to the highest international trade to reduce the economic implications caused by the outbreak of COVID-19 (31). Other suicide prevention strategies include improving access to mental healthcare; responsible media reporting with information about available support; preventing increased alcohol intake; and limiting access to lethal means of suicide (32).
Since this was a cross-sectional study, we were unable to demonstrate a causal-effect relationship. The data collection was fully online and distributed via social media, therefore this study was limited to participants with internet access and social media. There was also selection bias due to the convenience sampling method, which may affect the generalizability of the results to the general population. There were also other confounding factors not studied, like the history of suicidal attempts, life events, and family history of suicide. We would like to recommend a future prospective study to investigate this topic in more detail, to include other factors that could influence suicidal behaviours using randomised sampling and both online and physical data collection.
This study revealed that depression, sex, family dynamics, the number of people living together, the number of children, and marital status are significant contributing factors to suicidal behaviours. With an understanding of the related variables associated with suicidal behaviours among the general population, which is supported by data, future mental health support can be provided for intervention, prioritising the at-risk group. This will also help in future preparedness for an unforeseen pandemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Research Ethics Committee Research Management Centre Universiti Teknologi MARA. The patients/participants provided their written informed consent to participate in this study.
SR, JS, NH, and NR were the primary authors in analyzing and writing the manuscript. DT, DS, and KF were involved in the design and conceptualization of the whole research project. All authors contributed to the article and approved the submitted version.
We would like to thank the leading investigators from the Aristotle University of Thessaloniki and the Mental Health Sector of the Scientific Research Institute of the Pan-Hellenic Medical Association, Greece, for the opportunity to collaborate in this study. We also thank the Faculty of Medicine, Universiti Teknologi MARA, for sponsoring the cost of the publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Mamun MA. Suicide and suicidal behaviors in the context of COVID-19 pandemic in Bangladesh: a systematic review. Psychol Res Behav Manage. (2021) 2021:695–704. doi: 10.2147/PRBM.S315760
2. Shah AUM, Safri SNA, Thevadas R, Noordin NK, Rahman AA, Sekawi Z, et al. COVID-19 outbreak in Malaysia: actions taken by the Malaysian government. Int J Infect Dis. (2020) 97:108–16. doi: 10.1016/j.ijid.2020.05.093
3. World Health Organization [WHO]. COVID-19 in Malaysia Situation Report 01. (2020). Available online at: https://www.who.int/malaysia/internal-publications-detail/covid-19-in-malaysia-situation-report-01* accessed qu
4. Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. (2003) 4:819–28. doi: 10.1038/nrn1220
5. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. (2015) 2015:1–13. doi: 10.1016/S0140-6736(15)00234-2
6. O’Connor RC, Nock MK. The psychology of suicidal behavior. Lancet Psychiatry. (2014) 1:73–85. doi: 10.1016/S2215-0366(14)70222-6
7. Cheah YK, Azahadi M, Phang SN, Manaf NH. Sociodemographic, lifestyle and health determinants of suicidal behaviour in Malaysia. Psychiatry Res. (2018) 12:1–21. doi: 10.1016/j.psychres.2017.12.086
8. Efstathiou V, Stefanou M-I, Siafakas N, Makris M, Tsivgoulis G, Zoumpourlis V, et al. Suicidality and COVID-19: suicidal ideation, suicidal behaviors and completed suicides amidst the COVID-19 pandemic (Review). Exp Ther Med. (2022) 23:1–8. doi: 10.3892/etm.2021.11030
9. Elbogen EB, Lanier M, Blakey SM, Wagner HR, Tsai J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: the role of COVID-19-related stress, social isolation, and financial strain. Dep Anxiety. (2021) 38:739–48. doi: 10.1002/da.23162
10. Papadopoulou A, Efstathiou V, Yotsidi V, Pomini V, Michopoulos I, Markopoulou E, et al. Suicidal ideation during COVID-19 lockdown in greece: prevalence in the community, risk and protective factors. Psychiatry Res. (2021) 297:1–8. doi: 10.1016/j.psychres.2021.113713
11. Efstathiou V, Michopoulos I, Yotsidi V, Smyrnis N, Zompola C, Papadopoulou A, et al. Does suicidal ideation increase during the second COVID-19 lockdown? Psychiatry Res. (2021) 2021:1–3. doi: 10.1016/j.psychres.2021.113990
12. Antonelli-Salgado T, Monteiro GM, Marcon G, Roza TH, Zimerman A, Hoffmann MS, et al. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: a longitudinal study. J Affect Dis. (2021) 2021:52–60. doi: 10.1016/j.jad.2021.04.044
13. Pompili M, Innamorati M, Sampogna G, Albert U, Carmassi C, Carrà G, et al. The impact of covid-19 on unemployment across Italy: consequences for those affected by psychiatric conditions. J Affect Disord. (2022) 1:59–66. doi: 10.1016/j.jad.2021.09.035
14. Sahimi HM, Daud TI, Chan LF, Shah SA, Rahman FH, Jaafar NR. Depression and suicidal ideation in a sample of Malaysian healthcare workers: a preliminary study during the COVID-19 pandemic. Front Psychiatry. (2021) 12:1–9. doi: 10.3389/fpsyt.2021.658174
15. Ghazali SR, Elklit A, Balang RV, Ameenudeen Sultan M, Chen Y. Determining the cut-off score for a malay language version of the centre for epidemiologic studies depression scale (CESD). ASEAN J Psychiatry. (2014) 15:146–52.
16. Fountoulakis KN, Karakatsoulis G, Abraham S, Adorjan K, Ahmed HU, Alarcón RD, et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur Neuropsychopharmacol. (2022) 54:21–40.
17. Fountoulakis KN, Pantoula E, Siamouli M, Moutou K, Gonda X, Rihmer Z, et al. Development of the risk assessment suicidality scale (RASS): a population-based study. J Affect Dis. (2012) 138:449–57. doi: 10.1016/j.jad.2011.12.045
18. World Health Organization [WHO]. Suicide in the World: Global Health Estimates. (2019). Available oline at: https://apps.who.int/iris/bitstream/handle/10665/326948/WHO-MSD-MER-19.3-eng.pdf?* accessed qu.
19. Wong LP, Alias H, Md Fuzi AA, Omar IS, Mohamad Nor A, Tan MP, et al. Escalating progression of mental health disorders during the COVID-19 pandemic: evidence from a nationwide survey. PLoS One. (2021) 16(3):e0248916. doi: 10.1371/journal.pone.0248916
20. Rahman ME, Zubayer AA, Bhuiyan MR, Jobe MC, Khan MK. Suicidal behaviors and suicide risk among Bangladeshi people during the COVID-19 pandemic: an online cross-sectional survey. Heliyon. (2021) 2020:1–6. doi: 10.1016/j.heliyon.2021.e05937
21. Pompili M, Vichi M, Qin P, Innamorati M, Leo DD, Girardi P. Does the level of education influence completed suicide? A nationwide register study. J Affect Dis. (2013) 147:437–40. doi: 10.1016/j.jad.2012.08.046
22. Mamun M, Sakib N, Gozal D, Bhuiyan A, Hossain S, Bodrud-Doza M, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Dis. (2021) 279:462–72. doi: 10.1016/j.jad.2020.10.036
23. Lahav Y. Psychological distress related to COVID-19 – the contribution of continuous traumatic stress. J Affect Dis. (2020) 277:129–37.
24. Islam MS, Tasnim R, Sujan MS, Ferdous MZ, Sikde MT, Masud JH, et al. Depressive symptoms associated with COVID-19 preventive practice measures, daily activities in home quarantine and suicidal behaviors: findings from a large-scale online survey in Bangladesh. BMC Psychiatry. (2021) 273:1–12. doi: 10.1186/s12888-021-03246-7
25. Shoib S, Buitrago JG, Shuja K, Aqeel M, Filippise RD, Abbas J, et al. Suicidal behavior sociocultural factors in developing countries during COVID-19. L’Encéphale. (2022) 48:78–82. doi: 10.1016/j.encep.2021.06.011
26. Özdin S, Özdin ÜB. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. (2020) 2020:505–11. doi: 10.1177/0020764020927051
27. Chen N, Lee G, Tan B, Jing M, Goh Y, Ngiam N, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
28. Onyeka IN, Maguire A, Ross E, O’Reilly D. Does physical ill-health increase the risk of suicide? A census-based follow-up study of over 1 million people. Epidemiol Psychiatr Sci. (2020) 29:1–10. doi: 10.1017/S2045796020000529
29. Ting RS, Aw Yong YY, Tan MM, Yap CK. Cultural responses to covid-19 pandemic: religions. illness perception, and perceived stress. Front Psychol. (2021) 23:634863. doi: 10.3389/fpsyg.2021.634863
30. McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. (2020) 19:250–1. doi: 10.1002/wps.20767
31. Azmi FAM, Zainudin AZ, Yunus NM, Jaafar MN, Wan Ismail WI, Amdan MA. Towards stabilizing the economic impact of COVID-19 through fiscal policy in malaysia. Geopoli Quart. (2021) 17:90–107.
Keywords: suicidal behaviour, COVID-19, Malaysia, mental health, pandemic
Citation: Razali S, Saw JA, Hashim NA, Raduan NJN, Tukhvatullina D, Smirnova D and Fountoulakis KN (2022) Suicidal behaviour amid first wave of COVID-19 pandemic in Malaysia: Data from the COVID-19 mental health international (COMET-G) study. Front. Psychiatry 13:998888. doi: 10.3389/fpsyt.2022.998888
Received: 20 July 2022; Accepted: 12 September 2022;
Published: 18 October 2022.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Gaia Sampogna, University of Campania “L. Vanvitelli,” ItalyCopyright © 2022 Razali, Saw, Hashim, Raduan, Tukhvatullina, Smirnova and Fountoulakis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jo Anne Saw, YW5uZWpvc2F3QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.