- 1Department of Nosocomial Infection Management, Xi’an Central Hospital, College of Medicine, Xi’an Jiaotong University, Xi’an, China
- 2Health Management and Policy Institute, School of Public Policy and Administration, Xi’an Jiaotong University, Xi’an, China
- 3Department of Public Health, Medical College, Qinghai University, Xining, China
- 4Division for Mental and Physical Health, Norwegian Institute of Public Health, Oslo, Norway
- 5Department of Clinical Medicine, Qinghai Institute of Health Sciences, Xining, China
- 6Department of Public Education, Xining Urban Vocational & Technical College, Xining, China
- 7School of Pharmacy, Qinghai Nationalities University, Xining, China
Purpose: University freshmen are particularly vulnerable as they are undergoing the transition from high school to university with a range of changes. Sleep problems among this group in the Qinghai–Tibet Plateau of China were barely studied. This study aimed to explore sleep disturbance, and its association with quality of life (QoL) and demographic and clinical characteristics among university freshmen in Qinghai–Tibet Plateau, China.
Methods: A multistage stratified cluster random sampling method was performed to recruit student participants with a structured questionnaire to collect sociodemographic and clinical characteristics, and lifestyle behaviors. Sleep disturbance including three aspects of sleep disturbance (i.e., difficulty initiating sleep (DIS), difficulty maintaining sleep (DMS), and early morning awakening (EMA)) was assessed using standardized measurement. Multiple logistic regression models were applied to analyze the data.
Results: Among included 2,769 freshmen, the prevalence of sleep disturbance was 14.8% (95% CI: 14.2–15.5%), and corresponding prevalence of DIS, DMS, and EMA was 8.2% (95% CI: 7.7–8.7%), 8.3% (95% CI: 7.8–8.8%), and 4.2% (95% CI: 3.8–4.6%), respectively. Freshmen with sleeping disturbance had significantly lower QoL in physical [F (1, 2769) = 60.23, p < 0.001], psychological [F (1, 2769) = 46.18, p < 0.001], social [F (1, 2769) = 23.04, p < 0.001], and environment [F (1, 2769) = 6.07, p = 0.01] domains. Multiple logistic regression analyses revealed that having breakfast five times a week or less (less than three times, OR = 1.79, 95% CI: 1.34–2.40; 3–5 times, OR = 1.40, 95% CI: 1.09–1.79), self-perceived severe Internet dependence (OR = 1.71, 95% CI: 1.11–2.65), self-perceived poor health status (OR = 3.44, 95% CI: 2.06–5.74), high academic stress (OR = 1.42, 95% CI: 1.13–1.78), poor relationship with classmates (OR = 3.44, 95% CI: 1.53–7.71), and severe ADHD symptoms (OR = 1.08, 95% CI: 1.05–1.12) were positively associated with sleeping disturbance.
Conclusion: Sleep disturbance was common among freshmen and is associated with poorer QoL. Prevention and intervention strategies should be developed and implemented, especially among the vulnerable university freshman groups.
Introduction
Sleep disturbance is one of the most common health problems among university students (1), and the corresponding prevalence varies greatly worldwide. For instance, the prevalence of sleep disturbance among university students ranged between 27.0% in the United States and as high as 70.0% in Iran (2, 3). One meta-analysis including 76 studies revealed that the prevalence of sleep disturbance among Chinese university students was 25.7% (4). Sleep disturbance among students is found to be negatively associated with both mental and physical health, such as academic failure, depression, and poor quality of life (5–7), but also adverse health behaviors, such as Internet addiction, sedentary, and binge-eating behavior (8–10). Individuals with sleep disturbance are characterized by being insufficiently physically active, having poor social relationships and economic status, and reporting greater academic stress (11–14). It was demonstrated that students with unhealthy lifestyle behaviors like cigarette smoking had a high risk of several types of sleep disturbance, such as longer latency to fall asleep and short total sleep duration (15). Previous research found females to be 2.6 times as likely as males to suffer from sleep disturbance (16).
University freshmen are in particularly vulnerable position, as they are undergoing the transition from high school to college or university, with a range of changes including experience lifestyle and social behavior changes (17, 18), for example, being away from home and families, which could help them to casting off the shackles of parents and engage in more social activities (19). It was evidenced that university freshmen are at higher risk of sleep disturbance as compared to senior students (OR = 1.52, 95% CI: 1.17–1.99) (20). Despite the extensive number of studies focusing on sleep disturbance among university students, those specifically paid close attention to the freshmen group were limited.
Sleep disturbances pose great challenges at high altitude (i.e., Qinghai province). Qinghai Province is located in the eastern part of the Qinghai–Tibet Plateau, with 84.1% of the total area above 3,000 m above sea level. Qinghai Province has a unique climatic environment, with multiethnic communities (Han 52.29%, Tibetan 25.23%, Hui 14.78%, Tu 3.55%, and others 4.15% in 2019). There are only few studies on the relationship between sleep and multiethnic group.
We, therefore, conducted this study to explore the prevalence of sleep disturbance among freshmen in Qinghai–Tibet Plateau and compare the quality of life between freshmen with and without sleep disturbance. Then, we examine the association between sleep disturbance and a range of sociodemographic and clinical characteristics. Based on the previous study suggesting the increased risk of sleep disturbance among freshmen on mental health (21), we hypothesized that freshmen university students with sleep disturbances would have a poor quality of life (QoL).
Materials and methods
Study design and participants
This cross-sectional study is a school-based mental health survey. It was conducted in December 2019 in Qinghai province, China, which is a plateau region with an average altitude of 2,300 m. A multistage stratified cluster random sampling method was performed to recruit student participants. Four universities (Qinghai University, Qinghai Nationalities University, Qinghai Institute of Health Sciences, and Xining Urban Vocational & Technical College) were selected from twelve universities or colleges in this region based on affiliation levels and classifications. A stratified (majors were taken as the indicator) random sampling method was used to select the classes among the freshmen in each university or college, and cluster sampling was then used in each class. The details concerning the study design have been previously described (22, 23). Those who were fully enrolled were included in this study. Participants with chronic diseases or tumors that can strongly associate with sleep were excluded. The study was approved by the Ethics Committee of the Medical College of Qinghai University, and all participants provided informed consent. This survey was proceeded by following the principles of anonymity and voluntariness.
Measures
Sociodemographic and clinical characteristics including age, sex (female/male), ethnic Han [yes (The Han represent the majority of China’s people)/no], weight, height, residence areas prior to the enrollment (plateau/non-plateau areas), family economic level (low/general/high), weekly breakfast intake (six–seven times/three–five times/less than three times), self-perceived Internet dependence (no or mild/moderate/severe), academic stress (low/general/high), relationship with classmates, teachers, and families (good/general/poor), and self-perceived health status (good/fair/poor) were collected. Body mass index (BMI) was computed as BMI=weight(kg)/height2(m). BMI was divided into four categories according to the modified criteria for the Chinese population, that is, underweight (<18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24.0–27.9 kg/m2), and obesity (≥28 kg/m2) (24, 25).
Sleep disturbances in the past month were measured by asking the following questions (26): “Do you have difficulties in falling asleep at night (DIS)?”; “Do you have difficulties in maintaining sleep and wake up often (DMS)?”; and “Do you wake up in the midnight or early morning and have difficulties getting back to sleep (EMA)?”. Each question was answered in three options (never, sometimes, and often). The presence of at least one type of sleep disturbance (answer with “often”) was considered as having possible sleep disturbance.
The six-item Adult Attention-Deficit/Hyperactivity Disorder (ADHD) Self-Report Screening Scale for DSM-5 (ASRS-5) was used to measure ADHD symptom. Each item was answered from 0 (never) to 4 (very often). The total score ranges from 0 to 24, and higher total scores indicate severe ADHD (Cronbach’s α = 0.83) (27).
Chinese version of the World Health Organization Quality of Life brief version (WHOQOL-BREF) (28) was used to measure quality of life, which has 26 items and covers physical, psychological, social, and environmental domains. The scores for each domain were transformed on a special 4- to 20-point scale, and higher scores indicate greater QoL (Cronbach’s α = 0.70–0.91) (29).
Data analyses
All data were imputed into EpiData 3.1 with double-entry method. We excluded participants with 20% or more missing values, and multiple imputation (MI) approach was employed to handle missing data. The Shapiro–Wilk test and Q–Q plot were applied to assess whether continuous variables were normally distributed. The number (n) and percentage (%) or the mean and standard deviation (MSD) were used to describe the sociodemographic and clinical characteristics, as appropriate. Differences in sociodemographic and clinical characteristics between students with and without sleep disturbance were compared with the independent t-test, the Mann–Whitney U-test, and the chi-square test. Analysis of covariance (ANCOVA) was separately conducted to compare the four domains of QoL between the two groups after controlling the variables with significant differences in univariate analysis. Four multiple logistic analyses were applied to explore the association between potential characteristics and sleeping disturbance and its three aspects, by, respectively, setting sleep disturbance and its three types as dependent variables, and factors with significant difference in univariate analysis (sleep disturbance and its three aspects) as independent variables. We used the Hosmer–Lemeshow test to evaluate the goodness of each model and took advantage of R “forestplot” package (30) to draw forest plot to visually display the results. SPSS 25.0 was used to analyze data, and the significant level was set at 0.05 (two-tailed).
Results
A total of 3,000 questionnaires were sent, among which 2,899 were returned giving a response rate of 96.6%. By excluding participants with 20% or more missing values, data from 2,769 freshmen (age:19.16 ± 1.40, 1,835 female students) were analyzed in the current study. Of these participants, 41.4% are Han ethnic and 58.6% are ethnic minorities. The prevalence of sleep disturbance among freshmen was 14.8% (95% CI: 14.2–15.5%; n = 411), and the corresponding prevalence of DIS, DMS, and EMA was 8.2% (95% CI: 7.7–8.7%; n = 227), 8.3% (95% CI: 7.8–8.8%; n = 229), and 4.2% (95% CI: 3.8–4.6%; n = 116), respectively. Of the students with sleep disturbance, 13.1% (54/411) of them reported having taken hypnotics.
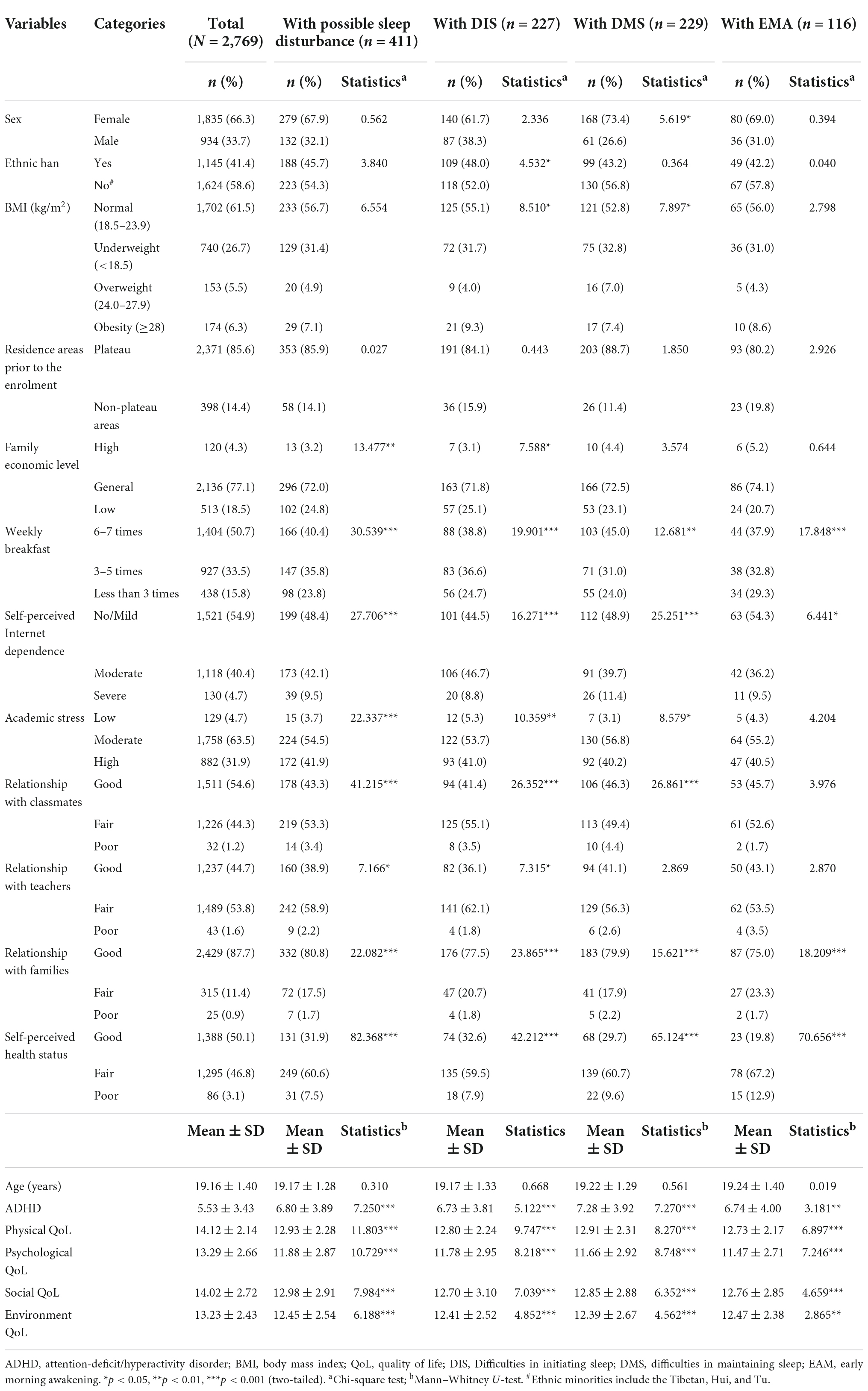
The Shapiro–Wilk test showed that age, ADHD score, and QoL in physical, psychological, environment, and social domains were not normally distributed. Table 1 displays the comparisons of sociodemographic and clinical characteristics between freshmen with and without sleep disturbance, DIS, DMS, and EMA. The QoL among freshmen without sleep disturbance was 14.33 ± 2.05, 13.54 ± 2.54, 14.20 ± 2.65, and 13.36 ± 2.39 in physical, psychological, social, and environment domains, respectively. The corresponding index among freshmen with sleep disturbance was 12.93 ± 2.28, 11.88 ± 2.87, 12.98 ± 2.91, and 12.45 ± 2.54.
ANCOVA analyses showed that, after controlling for BMI, family economic level, weekly breakfast, self-perceived Internet dependence, academic stress, ADHD, and interpersonal relationships (relationship with classmates, teachers, and families), participants with sleep disturbance had significantly lower QoL as compared to those without sleep disturbance in physical domain [F (1, 2769) = 60.23, p < 0.001], psychological domain [F (1, 2769) = 46.18, p < 0.001], social domain [F (1, 2769) = 23.04, p < 0.001], and environment domain [F (1, 2769) = 6.07, p = 0.01].
Multiple logistic regression showed that having breakfast five times a week or less (less than three times, OR = 1.79, 95% CI: 1.34–2.40; three–five times, OR = 1.40, 95% CI: 1.09–1.79), a self-perceived severe Internet dependence (OR = 1.71, 95% CI: 1.11–2.65), high academic stress (OR = 1.42, 95% CI: 1.13–1.78), poor relationship with classmates (OR = 3.44, 95% CI: 1.53–7.71), self-perceived poor health status (OR = 3.44, 95% CI: 2.06–5.74), and severe ADHD symptoms (OR = 1.08, 95% CI: 1.05–1.12) were positively associated with sleeping disturbance (Figure 1).
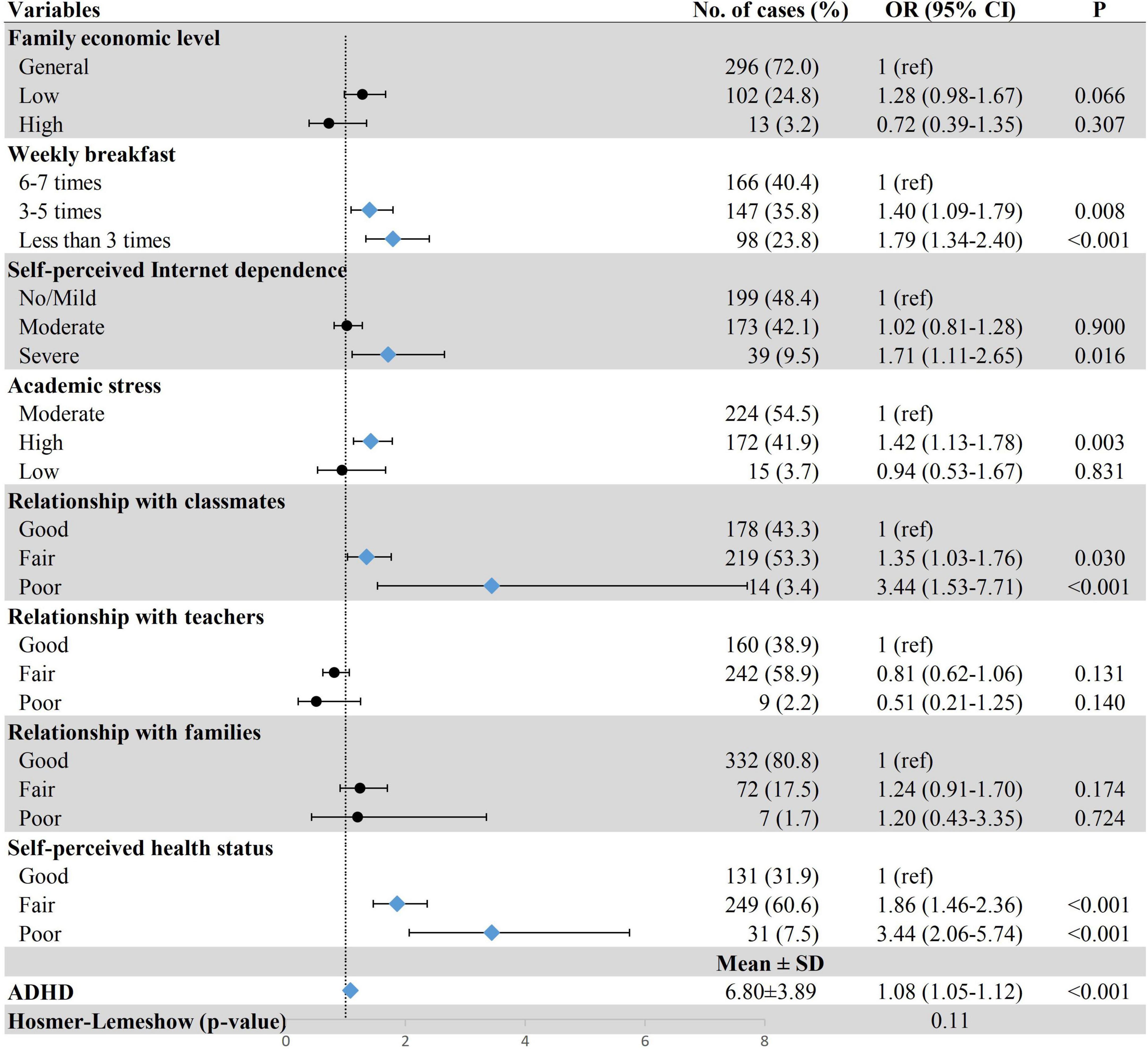
Figure 1. Association between demographic and clinical characteristics and possible sleep disturbance. Row with blue diamond indicates statistical significance. ADHD, attention-deficit/hyperactivity disorder; OR, odds ratio; 95% CI, 95% confidence interval.
Figures 2–4 show the results of multiple logistic regression analyses for the three patterns of sleep disturbances. Students having breakfast less than three times a week (DIS, OR = 1.77, 95% CI: 1.22–2.56; DMS, OR = 1.45, 95% CI: 1.01–2.11; EMA, OR = 1.97, 95% CI: 1.22–3.18), with self-perceived poor health status (DIS, OR = 2.68, 95% CI: 1.44–4.99; DMS, OR = 4.31, 95% CI: 2.38–7.81; EMA, OR = 9.67, 95% CI: 4.71–19.80), and severe ADHD symptoms (DIS, OR = 1.06, 95% CI: 1.02–1.10; DMS, OR = 1.12, 95% CI: 1.08–1.16; EMA, OR = 1.06, 95% CI: 1.01–1.11) were more likely to have different types of sleep disturbance. Poor relationship with classmates was positively associated with DIS (OR = 2.87, 95% CI: 1.12–7.31) and DMS (OR = 2.78, 95% CI: 1.13–6.81); yet due to a small number of individuals in these groups, the results should be interpreted with caution. The results also showed that freshmen with high academic stress (OR = 1.40, 95% CI: 1.04–1.89) were susceptible to DIS. Female freshmen (OR = 1.47, 95% CI: 1.07–2.03) and underweight students (OR = 1.41, 95% CI: 1.03–1.93) were more prone to have DMS.
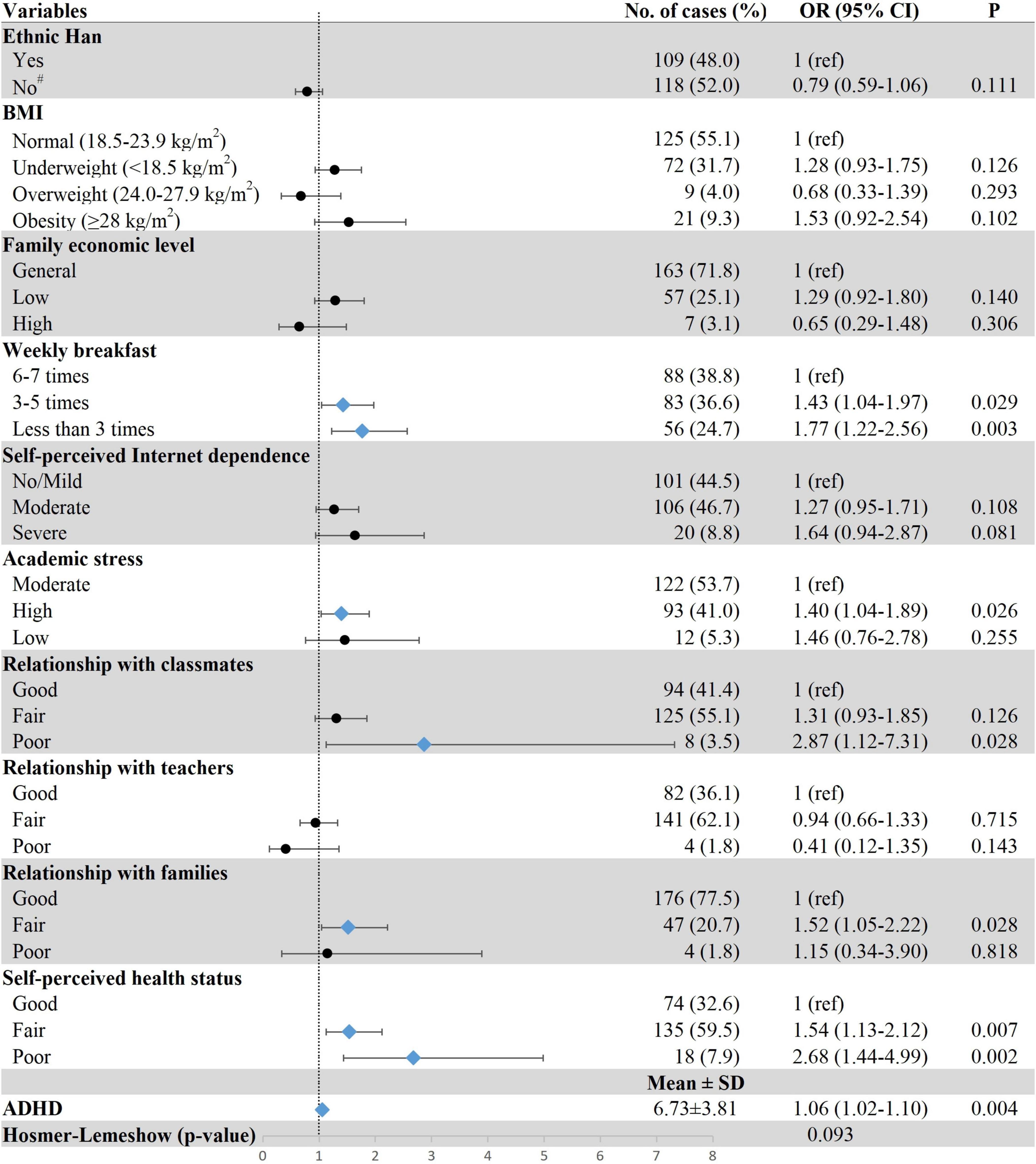
Figure 2. Associations between demographic and clinical characteristics and DIS. Row with blue diamond indicates statistical significance. #Ethnic minorities including the Tibetan, Hui, and Tu. ADHD, attention-deficit/hyperactivity disorder; BMI, body mass index; DIS, difficulties initiating sleep; OR, odds ratio; 95% CI, 95% confidence interval.
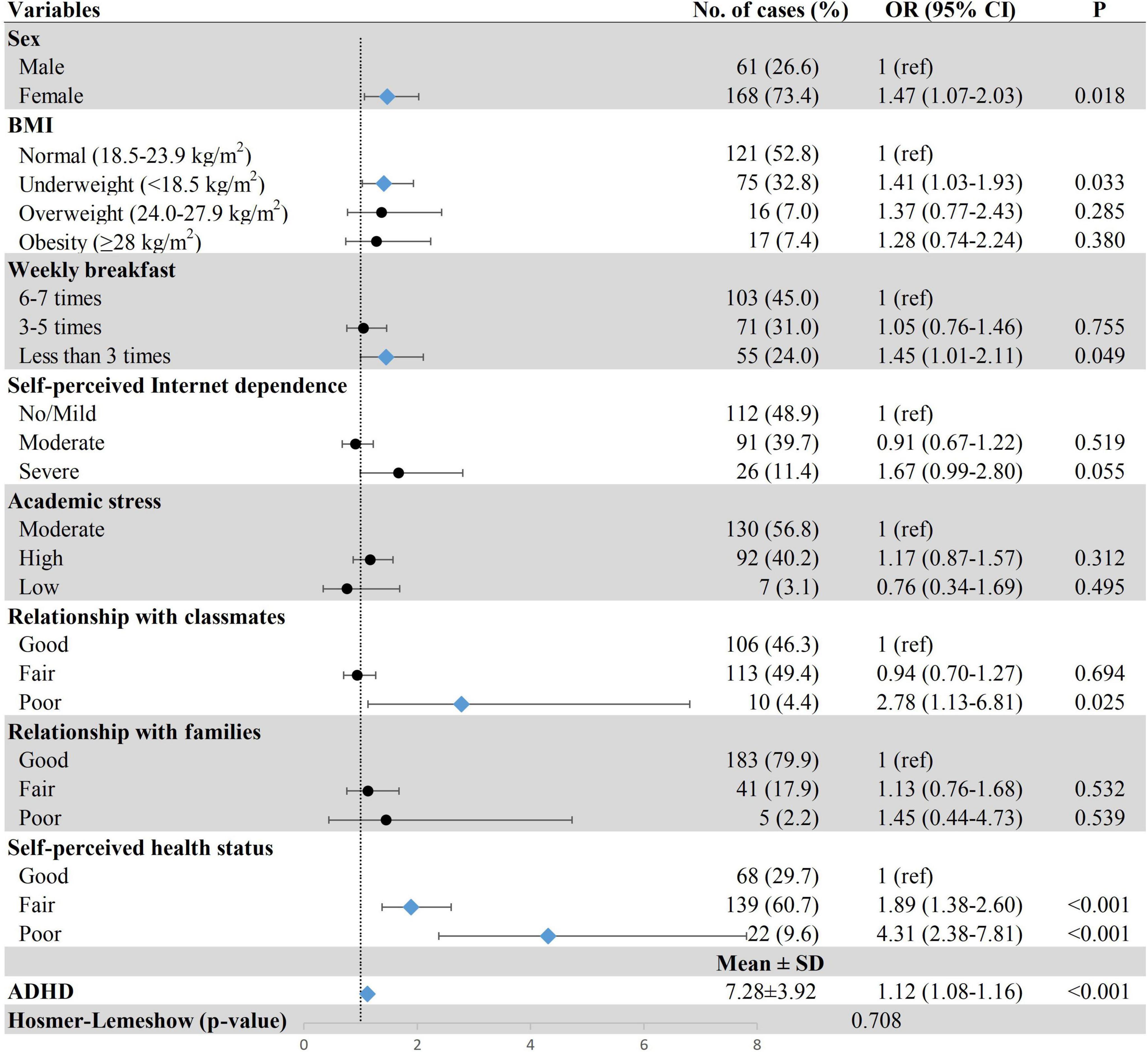
Figure 3. Associations between demographic and clinical characteristics and DMS. Row with blue diamond indicates statistical significance. ADHD, attention-deficit/hyperactivity disorder; BMI, body mass index; DMS, difficulties in maintaining sleep; OR, odds ratio; 95% CI, 95% confidence interval.
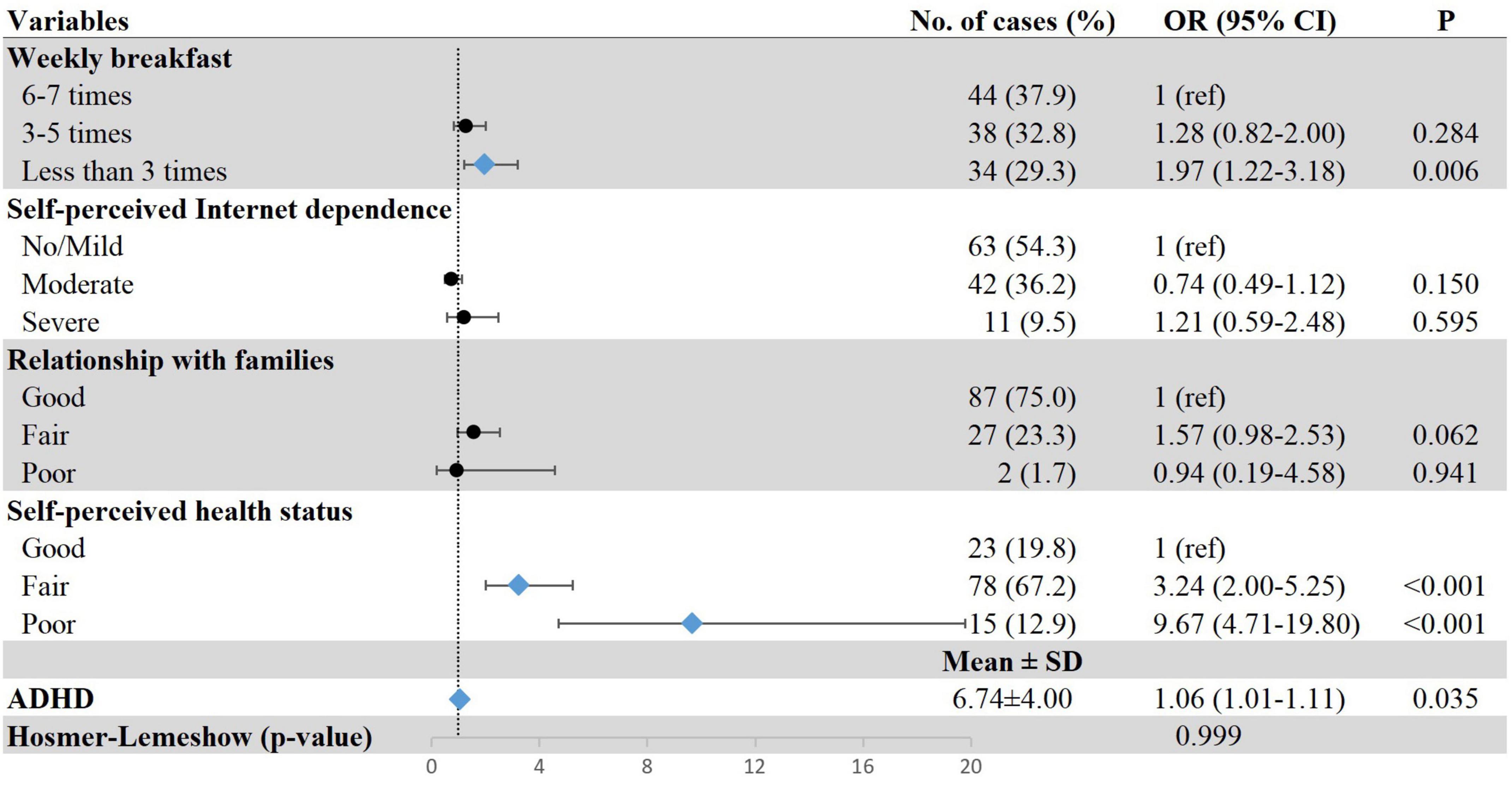
Figure 4. Associations between demographic and clinical characteristics and EMA. Row with blue diamond indicates statistical significance. ADHD, attention-deficit/hyperactivity disorder; EMA, early-morning awakening with inability to return to sleep; OR, odds ratio; 95% CI, 95% confidence interval.
Discussion
We found that the prevalence of sleep disturbance among freshmen in Qinghai–Tibet plateau was 14.8%, which was higher than the corresponding global figure of 10.4% measured in 20,222 undergraduate students from 26 countries (31). However, it was lower than the figure among freshmen in the United States (42.0%) (32), Saudi Arabia (75.4%) (33), Japan (33.3%) (21), and another study of China (37.9%) (34). The discrepancies could be explained by the following aspects. First, freshmen were more likely to suffer from sleep disturbance given the fact that they have fewer experiences than students in other grades in dealing with new pattern of life and academic pressure (20). It should also be noticed that the study was performed in December, and the academic pressure could also have partially explained the effects of final examination. Second, sleep is associated with varying socioeconomic factors. For example, people living in countries with high economic pressure and poor healthcare are susceptible to sleep disturbance (35). Third, racial differences in sleep quality were common (36), even within the same race (37). In addition, the definition, assessment tools, and investigative method used are not consistent across studies. Therefore, the direct comparisons of these rates should be made with caution.
As hypothesized, freshmen with sleep disturbance reported poorer QoL in physical, psychological, social, and environmental domains than those without sleep disturbance. Furthermore, we found breakfast consumption less than five times a week being positively associated with sleep disturbance. Skipping breakfast is relatively common among university students, with a range of 40.0% to 70.0% (38, 39). A cross-sectional study showed that having breakfast five or more days a week is a probable protective factor of sleep (40). Except for circadian rhythm, the association of breakfast intake and sleep disturbance was also related to a lack of daytime routine (41, 42). The association between Internet dependence and sleep disturbance was also reported among Japanese adolescents (43) and another large-scale study among Chinese adolescents (44). Another study found using the Internet as an unstructured activity with no fixed start and ending points can take up sleep time and cause sleep disturbance (45, 46). Another possible mechanism is that the screen light of Internet-using devices inhibits the secretion of melatonin, which will reduce subjective and objective sleep signals resulting in syndrome sleep phase delay (47, 48).
According to previous studies, negative relationship with family, teacher, or classmate may produce harmful emotion and behavior (49, 50), which could further lead to sleep disturbance. In our study, only poor relationship with classmates was significantly associated with sleep disturbance. The relationship with classmates is one of the most essential interpersonal contact when freshmen involve in university life. Studies have proven that students’ harmonious interpersonal relationships would benefit their sleep (51, 52); students with high-level interpersonal relationships experience less interpersonal pressure and mood swings which is propitious to sleep (53). Notably, fair relationship with families was associated with DIS. Previous findings suggested that under the context of outside pressure, cohesive relationship with families serves as a “safety signal” and may provide sense of stability which is necessary for healthy sleep (54). However, we found no association between poor relationship with families and DIS as only 25 participants had poor relationship with families which is less than one % of the total sample size.
We also found that about half of the students in this study reported good self-perceived health status and there is a strong independent association between self-perceived health status and sleep disturbance, which was consistent with the previous study (55). In this sample, the odds of suffering from sleep disturbance among freshmen with ADHD are higher than those who are not having ADHD. The previous study indicated that the odds of experiencing sleep disturbance for adolescents with ADHD were more than six times of those without (56). A meta-analysis revealed that youth have worse sleep quality after taking stimulants (57), and the psychostimulant use among participants with higher ADHD symptoms was not assessed in this study. Besides, it has been reported that untreated ADHD patients had melatonin onset delay at night which was related with circadian rhythm disorder (58).
Deviation from normal weight (BMI = 18.5–24.9) is found to be significantly associated with sleep disturbance in epidemiological studies conducted in European countries (59, 60). We only found association between underweight and DIS. The prevalence of underweight was obviously higher than the prevalence of obesity and overweight in our study. In addition, females were more likely to develop DIS, which is consistent with prior research indicating that females have 50% higher risk to develop DIS than males (61). These sex differences may be partially explained by changes in hormones during menstruation among females, which increase the risk of sleep disturbance (62).
High-altitude environments were also found to have an adverse effect on the physiological function of people who are used to living at low altitude (63). However, we did not ascertain the significant association between residence areas prior to the enrollment (plateau or non-plateau areas) and sleep disturbance. This may be related to the fact that this investigation was conducted three months after the start of academic year and they may have adapted to the plateau environment. It should be noted that Qinghai province is a plateau region with an average altitude of 2,300 m, but previous surveys revealed that stress responses to high altitude are usually limited to over 3,000 m above sea level (64, 65).
Our study results suggested that university freshmen suffered from sleep disturbance, which was associated with poor QoL. School-based preventions and interventions should be considered and implemented to prevent sleep disturbance and hence the reduced QoL of those potentially affected (66). For instance, psychological counseling services through face-to-face care and telehealth should be both adopted. Helping the establishment of exceptional self-regulation in freshmen also contributes to a series of positive health consequences with long-term implications (67).
However, the results of this study should be interpreted considering several limitations. The first one related to the cross-sectional study design and self-report data failed to help us report any causal relationship between sleep disturbance and related factors. Second, the measurement of independent variables, such as self-perceived Internet dependence, which is single item measures and may lower the reliability and validity. Third, this study intends to research the sleep disturbance of freshmen in Qinghai–Tibet plateau, but only Qinghai province is included. Further studies should include more provinces in Qinghai–Tibet plateau to validate the results. However, our study benefited greatly from the sample size that ensured the statistical power and a detailed assessment of sleep disturbance including three dimensions (i.e., DIS, DMS, and EMA).
Conclusion
This study highlighted that sleep disturbance is common among university freshmen in Qinghai–Tibet plateau and is associated with poorer QoL of those affected. Students with poor relationship with classmates, irregularly breakfast intake, self-perceived Internet dependence, self-perceived poor health status, high academic stress, and ADHD symptom were more likely to have sleep disturbance. The focus on development and implementation of preventive measures targeted toward freshmen and their sleep problems could not only promote healthy sleep but also improve students’ academic performance. Improving consciousness of freshmen about the modifiable lifestyle factors having adverse effect on their sleep is also of great importance.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved and reviewed by the Ethics Committee of the Medical College of Qinghai University. Written informed consent to participate was obtained from all participants.
Author contributions
TZ, SL, and LL: study design. TZ, LL, Y-YL, JG, H-RC, H-YS, X-YG, Y-MR, and Z-CD: data collection, analysis, and interpretation. TZ, LL, SL, and KH: drafting of the manuscript. All authors approved the final version for publication.
Funding
This study was supported by the National Natural Science Foundation of China (81860606) and the Natural Science Foundation of Qinghai Province (2019-ZJ-906).
Acknowledgments
We thank all the participants and research investigators for their supports on this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Putilov AA, Sveshnikov DS, Bakaeva ZB, Yakunina EB, Starshinov YP, Torshin VI, et al. Differences between male and female university students in sleepiness, weekday sleep loss, and weekend sleep duration. J Adolesc. (2021) 88:84–96. doi: 10.1016/j.adolescence.2021.02.006
2. Becker SP, Jarrett MA, Luebbe AM, Garner AA, Burns GL, Kofler MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health. (2018) 4:174–81. doi: 10.1016/j.sleh.2018.01.001
3. Sarbazvatan H, Amini A, Aminisani N, Shamshirgaran SM. Sleep quality and academic progression among students of tabriz university of medical sciences, northwest of iran. Res Dev Med Educ. (2017) 6:29–33. doi: 10.15171/rdme.2017.006
4. Li L, Wang YY, Wang SB, Zhang L, Li L, Xu DD, et al. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res. (2018) 27:e12648. doi: 10.1111/jsr.12648
5. Titova OE, Hogenkamp PS, Jacobsson JA, Feldman I, Schioth HB, Benedict C. Associations of self-reported sleep disturbance and duration with academic failure in community-dwelling Swedish adolescents: sleep and academic performance at school. Sleep Med. (2015) 16:87–93. doi: 10.1016/j.sleep.2014.09.004
6. Matsui K, Kuriyama K, Yoshiike T, Nagao K, Ayabe N, Komada Y, et al. The effect of short or long sleep duration on quality of life and depression: an internet-based survey in Japan. Sleep Med. (2020) 76:80–5. doi: 10.1016/j.sleep.2020.10.012
7. Xu YM, Pu SS, Li Y, Zhong BL. Possible avoidant personality disorder magnifies the association between bullying victimization and depressive symptoms among chinese university freshmen. Front Psychiatry. (2022) 13:822185. doi: 10.3389/fpsyt.2022.822185
8. Chen YL, Gau SS. Sleep problems and internet addiction among children and adolescents: a longitudinal study. J Sleep Res. (2016) 25:458–65. doi: 10.1111/jsr.12388
9. Yang Y, Shin JC, Li D, An R. Sedentary behavior and sleep problems: A systematic review and meta-analysis. Int J Behav Med. (2017) 24:481–92. doi: 10.1007/s12529-016-9609-0
10. Allison KC, Spaeth A, Hopkins CM. Sleep and eating disorders. Curr Psychiatry Rep. (2016) 18:92. doi: 10.1007/s11920-016-0728-8
11. Kovacevic A, Mavros Y, Heisz JJ, Fiatarone Singh MA. The effect of resistance exercise on sleep: A systematic review of randomized controlled trials. Sleep Med Rev. (2018) 39:52–68. doi: 10.1016/j.smrv.2017.07.002
12. Gordon AM, Carrillo B, Barnes CM. Sleep and social relationships in healthy populations: A systematic review. Sleep Med Rev. (2021) 57:101428. doi: 10.1016/j.smrv.2021.101428
13. Zhang W, Ohira T, Maeda M, Nakano H, Iwasa H, Yasumura S, et al. The association between self-reported sleep dissatisfaction after the Great East Japan Earthquake, and a deteriorated socioeconomic status in the evacuation area: the Fukushima Health Management Survey. Sleep Med. (2020) 68:63–70. doi: 10.1016/j.sleep.2019.09.004
14. Liu B, Gao F, Zhang J, Zhou H, Sun N, Li L, et al. Sleep quality of students from elementary school to university: A cross-sectional study. Nat Sci Sleep. (2020) 12:855–64. doi: 10.2147/NSS.S266493
15. Costa M, Esteves M. Cigarette smoking and sleep disturbance. Addict Disord Their Treatment. (2018) 17:40–8. doi: 10.1097/ADT.0000000000000123
16. Ahmed AE, Al-Jahdali H, Fatani A, Al-Rouqi K, Al-Jahdali F, Al-Harbi A, et al. The effects of age and gender on the prevalence of insomnia in a sample of the Saudi population. Ethn Health. (2017) 22:285–94. doi: 10.1080/13557858.2016.1244624
17. Kim M, Cardinal BJ. Psychological state and behavioural profiles of freshman enrolled in college and university instructional physical activity programmes under different policy conditions. Montenegrin J Sports Sci Med. (2019) 8:13–20. doi: 10.26773/mjssm.190902
18. Zhang CL, Xu YM, Zhong BL. The association between smoking and loneliness among Chinese university freshmen. Ann Transl Med. (2020) 8:649. doi: 10.21037/atm-20-3523
19. Griggs S, Crawford SL. Differences in hope, core self-evaluations, emotional well-being, and health risk behaviors in freshman university students. Nurs Forum. (2019) 54:505–12. doi: 10.1111/nuf.12364
20. Li Y, Bai W, Zhu B, Duan R, Yu X, Xu W, et al. Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual Life Outcomes. (2020) 18:210. doi: 10.1186/s12955-020-01465-2
21. Supartini A, Honda T, Basri NA, Haeuchi Y, Chen S, Ichimiya A, et al. The impact of sleep timing, sleep duration, and sleep quality on depressive symptoms and suicidal ideation amongst japanese freshmen: The EQUSITE Study. Sleep Disord. (2016) 2016:8737654. doi: 10.1155/2016/8737654
22. Lu L, Jian S, Dong M, Gao J, Zhang T, Chen X, et al. Childhood trauma and suicidal ideation among Chinese university students: the mediating effect of Internet addiction and school bullying victimisation. Epidemiol Psychiatr Sci. (2020) 29:e152. doi: 10.1017/S2045796020000682
23. Lu L, Dong M, Jian S, Gao J, Ye L, Chen HR, et al. Sex differences in the factors associated with sleep duration in university students: A cross-sectional study. J Affect Disord. (2021) 290:345–52. doi: 10.1016/j.jad.2021.04.025
24. Cai J, Ma A, Wang Q, Han X, Zhao S, Wang Y, et al. Association between body mass index and diabetes mellitus in tuberculosis patients in China: a community based cross-sectional study. BMC Public Health. (2017) 17:228. doi: 10.1186/s12889-017-4101-6
25. He W, Li Q, Yang M, Jiao J, Ma X, Zhou Y, et al. Lower BMI cutoffs to define overweight and obesity in China. Obesity (Silver Spring). (2015) 23:684–91. doi: 10.1002/oby.20995
26. Liu S, Chow IHI, Lu L, Ren YM, Yang HL, Jian SY, et al. Comparison of sleep disturbances between older nursing home residents in high- and low-altitude areas. J Geriatr Psychiatry Neurol. (2020) 33:370–6. doi: 10.1177/0891988719892335
27. Ustun B, Adler LA, Rudin C, Faraone SV, Spencer TJ, Berglund P, et al. The world health organization adult attention-deficit/hyperactivity disorder self-report screening scale for DSM-5. JAMA Psychiatry. (2017) 74:520–7. doi: 10.1001/jamapsychiatry.2017.0298
28. Felce D, Perry J. Quality of life: Its definition and measurement. Res Dev Disabil. (1995) 16:51–74. doi: 10.1016/0891-4222(94)00028-8
29. Lin CY, Lee TY, Sun ZJ, Yang YC, Wu JS, Ou HT. Development of diabetes-specific quality of life module to be in conjunction with the World Health Organization quality of life scale brief version (WHOQOL-BREF). Health Qual Life Outcomes. (2017) 15:167. doi: 10.1186/s12955-017-0744-3
31. Peltzer K, Pengpid S. Nocturnal sleep problems among university students from 26 countries. Sleep Breath. (2015) 19:499–508. doi: 10.1007/s11325-014-1036-3
32. Chen W-L, Chen J-H. Consequences of inadequate sleep during the college years: Sleep deprivation, grade point average, and college graduation. Prev Med. (2019) 124:23–8. doi: 10.1016/j.ypmed.2019.04.017
33. Aldhawyan AF, Alfaraj AA, Elyahia SA, Alshehri SZ, Alghamdi AA. Determinants of subjective poor sleep quality in social media users among freshman college students. Nat Sci Sleep. (2020) 12:279–88. doi: 10.2147/NSS.S243411
34. Ma C, Zhou L, Xu W, Ma S, Wang Y. Associations of physical activity and screen time with suboptimal health status and sleep quality among Chinese college freshmen: A cross-sectional study. PLoS One. (2020) 15:e0239429. doi: 10.1371/journal.pone.0239429
35. Chen WC, Chen SJ, Zhong BL. Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in wuhan, china, during the COVID-19 Pandemic. J Geriatr Psychiatry Neurol. (2022) 35:215–22. doi: 10.1177/08919887221078564
36. George KM, Peterson RL, Gilsanz P, Mungas DM, Glymour MM, Mayeda ER, et al. Racial/Ethnic differences in sleep quality among older adults: kaiser healthy aging and diverse life experiences (KHANDLE) Study. Ethn Dis. (2020) 30:469–78. doi: 10.18865/ed.30.3.469
37. Takahashi M, Wang G, Adachi M, Jiang F, Jiang Y, Saito M, et al. Differences in sleep problems between Japanese and Chinese preschoolers: a cross-cultural comparison within the Asian region. Sleep Med. (2018) 48:42–8. doi: 10.1016/j.sleep.2017.11.1145
38. Mansouri M, Sharifi F, Shokri A, Varmaghani M, Yaghubi H, Moghadas-Tabrizi Y, et al. Breakfast consumption is inversely associated with primary headaches in university students: The MEPHASOUS study. Complement Ther Med. (2021) 57:102663. doi: 10.1016/j.ctim.2021.102663
39. Ojieabu CE, Sholeye O, Ojieabu W, Onabajo B. Breakfast consumption and associated factors among students in olabisi onabanjo university, ogun state, nigeria. Value in Health. (2017) 20:A683–4. doi: 10.1016/j.jval.2017.08.1719
40. Gomez-Chiappe N, Lara-Monsalve PA, Gomez AM, Gómez DC, González JC, González L, et al. Poor sleep quality and associated factors in university students in Bogota D.C., Colombia. Sleep Sci. (2020) 13:125–30. doi: 10.5935/1984-0063.20190141
41. Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Insufficient sleep duration is associated with dietary habits, screen time, and obesity in children. J Clin Sleep Med. (2018) 14:1689–96. doi: 10.5664/jcsm.7374
42. Villa-Gonzalez E, Huertas-Delgado FJ, Chillon P, Ramirez-Velez R, Barranco-Ruiz Y. Associations between active commuting to school, sleep duration, and breakfast consumption in Ecuadorian young people. BMC Public Health. (2019) 19:85. doi: 10.1186/s12889-019-6434-9
43. Tokiya M, Itani O, Otsuka Y, Kaneita Y. Relationship between internet addiction and sleep disturbance in high school students: a cross-sectional study. BMC Pediatr. (2020) 20:379. doi: 10.1186/s12887-020-02275-7
44. Guo L, Luo M, Wang WX, Huang GL, Xu Y, Gao X, et al. Association between problematic Internet use, sleep disturbance, and suicidal behavior in Chinese adolescents. J Behav Addict. (2018) 7:965–75. doi: 10.1556/2006.7.2018.115
45. Yang J, Guo Y, Du X, Jiang Y, Wang W, Xiao D, et al. Association between Problematic Internet Use and Sleep Disturbance among Adolescents: The Role of the Child’s Sex. Int J Environ Res Public Health. (2018) 15:2682. doi: 10.3390/ijerph15122682
46. Luo W, Zhong BL, Chiu HF. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
47. Petit A, Karila L, Estellat C, Moisan D, Reynaud M, D’Ortho MP, et al. Sleep disorders in Internet addiction. Presse Med. (2016) 45(12 Pt 1):1170–7. doi: 10.1016/j.lpm.2016.04.025
48. Royant-Parola S, Londe V, Trehout S, Hartley S. The use of social media modifies teenagers’ sleep-related behavior. Encephale. (2018) 44:321–8. doi: 10.1016/j.encep.2017.03.009
49. Bannon SM, Greenberg J, Goldson J, O’Leary D, Vranceanu AMA. Social Blow: The role of interpersonal relationships in mild traumatic brain injury. Psychosomatics. (2020) 61:518–26. doi: 10.1016/j.psym.2020.04.003
50. Dietz LJ. Family-Based interpersonal psychotherapy: An intervention for preadolescent depression. Am J Psychother. (2020) 73:22–8. doi: 10.1176/appi.psychotherapy.20190028
51. Jin Y, Ding Z, Fei Y, Jin W, Liu H, Chen Z, et al. Social relationships play a role in sleep status in Chinese undergraduate students. Psychiatry Res. (2014) 220:631–8. doi: 10.1016/j.psychres.2014.08.029
52. Wang PY, Lin PH, Lin CY, Yang SY, Chen KL. Does interpersonal interaction really improve emotion, sleep quality, and self-efficacy among junior college students? Int J Environ Res Public Health. (2020) 17:4542. doi: 10.3390/ijerph17124542
53. Gunn HE, Troxel WM, Hall MH, Buysse DJ. Interpersonal distress is associated with sleep and arousal in insomnia and good sleepers. J Psychosom Res. (2014) 76:242–8. doi: 10.1016/j.jpsychores.2013.11.010
54. Tsai KM, Dahl RE, Irwin MR, Bower JE, McCreath H, Seeman TE, et al. The roles of parental support and family stress in adolescent sleep. Child Dev. (2018) 89:1577–88. doi: 10.1111/cdev.12917
55. Mangrio E, Zdravkovic S, Sjogren Forss K. The association between self-perceived health and sleep-quality and anxiety among newly arrived refugees in sweden: A quantitative study. J Immigr Minor Health. (2020) 22:82–6. doi: 10.1007/s10903-019-00871-z
56. Becker SP, Langberg JM, Eadeh HM, Isaacson PA, Bourchtein E. Sleep and daytime sleepiness in adolescents with and without ADHD: differences across ratings, daily diary, and actigraphy. J Child Psychol Psychiatry. (2019) 60:1021–31. doi: 10.1111/jcpp.13061
57. Kidwell KM, Van Dyk TR, Lundahl A, Nelson TD. Stimulant medications and sleep for youth with ADHD: A Meta-analysis. Pediatrics. (2015) 136:1144–53. doi: 10.1542/peds.2015-1708
58. Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep Med. (2010) 11:652–8. doi: 10.1016/j.sleep.2010.02.012
59. Mullane N, Bradley C. An investigation into the association between demographic and morbidity factors, and sleep disturbance. Ir J Med Sci. (2018) 187:163–75. doi: 10.1007/s11845-017-1640-x
60. Sivertsen B, Pallesen S, Sand L, Hysing M. Sleep and body mass index in adolescence: results from a large population-based study of Norwegian adolescents aged 16 to 19 years. BMC Pediatr. (2014) 14:204. doi: 10.1186/1471-2431-14-204
61. Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. (2006) 29:85–93. doi: 10.1093/sleep/29.1.85
62. Pengo MF, Won CH, Bourjeily G. Sleep in women across the life Span. Chest. (2018) 154:196–206. doi: 10.1016/j.chest.2018.04.005
63. Kabel AM, Al Thumali AM, Aldowiala KA, Habib RD, Aljuaid SS, Alharthi HA. Sleep disorders in adolescents and young adults: Insights into types, relationship to obesity and high altitude and possible lines of management. Diabetes Metab Syndr. (2018) 12:777–81. doi: 10.1016/j.dsx.2018.04.029
64. Hill CM, Bucks RS, Cellini N, Motamedi S, Carroll A, Heathcote K, et al. Cardiac autonomic activity during sleep in high-altitude resident children compared with lowland residents. Sleep. (2018) 41:181. doi: 10.1093/sleep/zsy181
65. Bian SZ, Zhang L, Jin J, Zhang J-H, Li Q-N, Chen J-F, et al. The onset of sleep disturbances and their associations with anxiety after acute high-altitude exposure at 3700 m. Transl Psychiatry. (2019) 9:175. doi: 10.1038/s41398-019-0510-x
66. Li HM, Xu YM, Zhong BL. Relationship between childhood left-behind experience and quality of life among chinese university freshmen: place of origin matters. Front Psychiatry. (2021) 12:789622. doi: 10.3389/fpsyt.2021.789622
Keywords: China, quality of life, Qinghai-Tibet Plateau, sleep disturbance, university freshmen
Citation: Zhang T, Lu L, Ren Y-M, Liu Y-Y, Hynek KA, Gao J, Chen H-R, Shen H-Y, Gai X-Y, Dang Z-C and Liu S (2022) Sleep disturbance and quality of life among university freshmen in Qinghai–Tibet Plateau of China. Front. Psychiatry 13:996996. doi: 10.3389/fpsyt.2022.996996
Received: 11 August 2022; Accepted: 12 October 2022;
Published: 08 November 2022.
Edited by:
Bao-Liang Zhong, Wuhan Mental Health Center, ChinaReviewed by:
Wen-Wang Rao, Shantou University, ChinaShi-Bin Wang, Guangdong Mental Health Center, China
Copyright © 2022 Zhang, Lu, Ren, Liu, Hynek, Gao, Chen, Shen, Gai, Dang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Lu, bGlzZXJAb3V0bG9vay5jb20=; Shou Liu, bGl1c2hvdTIwMDRAYWxpeXVuLmNvbQ==
 Tiantian Zhang
Tiantian Zhang Li Lu
Li Lu Yan-Ming Ren3
Yan-Ming Ren3 Yu-Ying Liu
Yu-Ying Liu Kamila Angelika Hynek
Kamila Angelika Hynek Shou Liu
Shou Liu