- 1School of Education Research, China University of Geosciences, Wuhan, China
- 2Research Center for Psychological and Health Sciences, China University of Geosciences, Wuhan, China
- 3Wuhan Mental Health Centre, Wuhan, China
Background: Non-suicidal self-injury (NSSI) and suicide attempt (SA) are risk behaviors that lead to physical injury and even death in individuals, and are a very powerful risk factor when both occur together, with individuals presenting with more severe psychological and behavioral problems. Due to the different demographic characteristics of different study subjects, an overall understanding of the incidence and occurrence of this co-occurrence is lacking to clarify the focus of clinical interventions and future research directions.
Methods: A systematic search was conducted for relevant studies in English and Chinese that reported data on co-occurring non-suicidal self-injury and suicide attempts as of May 2022. The incidence of co-occurrence of non-suicidal self-injury and suicide attempt (NSSI + SA) was calculated using Stata version 16.0 software based on a random-effects model, and the differences in incidence in different populations were compared by subgroups of age group, comorbidity, and time of occurrence. The study was written in strict accordance with PRISMA norms and registration was completed on the PROSPERO platform (CRD42022329095).
Results: A total of 37 studies (139,573 individuals) were included for meta-analysis, and the combined incidence of non-suicidal self-injury and suicide attempt co-occurrence was 9.6%. Among different groups, the prevalence of NSSI + SA was 10, 11, 6, and 26% in adolescents and young adults, adults, the general population, and people with mental illness, respectively, and the co-occurrence of NSSI + SA within 12 months was 17%.
Conclusion: There is a significant group with a history of both non-suicidal self-injury and suicide attempts and presenting with more severe symptoms clinically. Targeted prevention and intervention are urgently needed, but the direction of intervention needs further research on the occurrence trajectory of this co-occurrence.
Systematic Review Registration: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42022329095, identifier: CRD42022329095.
Introduction
Non-suicidal self-injury (NSSI) is intentional self-injury to bodily tissue without suicidal intent for socially or culturally unsanctioned purposes (1). A suicide attempt (SA), is a self-destructive act with at least some intent to end one's life (1). Because suicide attempts are one of the strongest predictors of completed suicide in individuals (2), and 10%−15% of patients with prior suicide attempts eventually die by suicide (3), the main focus in previous studies has been on the occurrence of suicide attempts. It is worth noting, however, that NSSI is not a less lethal form of SA, but a coping mechanism to regulate emotions and endure life, SA reflects a desire to end one's life (4).
Although NSSI differs from suicide attempts, the risk of suicide increases over time as habituation to self-harm and physical pain reduces an individual's fear of suicide and death, or as the need for more than what NSSI can provide (5). The literature suggests a strong association between NSSI and SA. Franklin et al. concluded that a history of NSSI is one of the most consistent and powerful predictors of suicidal behavior in studies conducted over a 50-year period (6). Bryan et al. also concluded that a history of NSSI predicted future suicide attempts, and that adolescents with a history of NSSI had a significantly increased risk of suicide attempts in the following 2 years. The risk of suicide attempts was significantly higher among adolescents with a history of NSSI in the following 2 years (7). In a study of community and clinically independent samples, investigations revealed a moderate to high association between NSSI and history of suicide attempts, with the association stronger than many other recognized risk factors for suicide (e.g., depression, anxiety, and borderline personality disorder), and only suicidal ideation was more strongly associated with suicide attempts than NSSI (8). In addition, previous cross-sectional studies of soldiers receiving mental health care (7) and a prospective study of adolescents (9) have found that a history of NSSI is even more predictive of future suicide attempts than a history of previous suicide attempts.
In addition to the exploration of the association between NSSI and suicide attempt as two separate events, many studies have also found considerable overlap between NSSI and SA (10), which can occur not only separately but also and often simultaneously, and are a particularly powerful risk factor (9, 11). Nock et al. (12) found, after clinical interviews with 89 hospitalized adolescent patients, that 70% of adolescents who reported a history of NSSI also reported a history of prior suicide attempts, and this group of patients showed a trend toward more methodologically diverse self-injurious behaviors that require more clinical attention. In other studies, almost 63%−77% of adolescents with psychiatric disorders who reported both NSSI and suicide attempts were also reported (9, 10), a phenomenon that has become increasingly common in clinical practice.
There has been much academic discussion about NSSI and suicide attempt. The controversy has focused on whether NSSI and suicide attempt are distinct concepts or whether they are part of the same set of self-injurious behaviors, and what the connections and differences between the two are (13, 14). Many scholars advocate separating the two concepts in the diagnostic system (15–17), and some studies suggest that this may be more conducive to adequate risk assessment and treatment planning (18).
In light of the available research findings and to encourage further future research, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) included the two as two distinct conditions in the Proposed Criteria collection. Through a literature review, data reanalysis, and field trial results, expert consensus identified recommended diagnostic entries, thresholds, and durations (19). However, because there is insufficient evidence to justify the inclusion of these recommendations in Section II of the formal diagnosis of mental disorders, these recommended criteria are not used for clinical application and remain to be further explored. Although there is some variation in previous studies regarding the association between NSSI and suicide attempt, there is an accepted consensus from these studies that there is an underlying intent to die in the act of suicide attempt and not in the act of NSSI, which is the primary difference between the two behaviors in the recommended diagnostic entries in the DSM-5 (20). In the DSM-5, the proposed criterion for non-suicidal self-injury is five or more days of intentional self-injury in the past year in anticipation of physical harm but without suicidal intent. In contrast, the proposed criterion for Suicidal Behavior Disorder associated with a suicide attempt is that the individual has made a suicide attempt within the past 24 months and must not have involved a repeat (at least five times in the past 12 months) self-injurious event.
In summary, previous studies have suggested that we have a significant number of individuals with a history of both NSSI and suicide attempts, and that this population presents with more severe psychological and behavioral problems that require targeted and timely clinical interventions (21). However, due to the different demographic characteristics of the populations investigated in these studies, there is a lack of an overall understanding of the co-occurrence of NSSI and suicide attempt, as well as a review overview of the specific studies, which makes it difficult to identify the focus of clinical interventions and the direction of future research. In addition, because the proposed diagnostic criteria associated with NSSI and suicide attempt in the DSM-5 are incompatible over time, understanding the co-occurrence of the two events may also inform the development of subsequent modifications to the formal diagnosis.
Method
This study was written in strict accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered with PROSPERO (International Prospective Register of Systematic Reviews) and completed the registration with the registration number CRD42022329095.
Search strategy
This search utilized the literature databases: PubMed, Embase, Cochrane library, CNKI, Wanfang Data, Web of science, PsycINFO (APA PsycNet), ClinicalTrials.gov, and the preprint databases: MedRxiv, ChinaXiv, SSRN, using a combination of search terms (* indicates truncation) including: “non-suicidal self injury,” “non-suicidal self harm,” “NSSI,” “suicide,” “suicide attempt*,” “suicide ideation,” a comprehensive review of relevant articles to date was conducted for the period March 1, 2022 to May 1, 2022. This search had no language or country restrictions and comprehensively considered all potential studies that met the criteria.
Inclusion/exclusion criteria
Two authors (ZY and FX) independently assessed the eligibility of included studies. Studies included in this review had to meet the following inclusion criteria: (1) the study provided cross-sectional data on the prevalence of suicidal behavior and NSSI over 12 months or over a lifetime; (2) the study had a clear definition of suicidal behavior and NSSI. Studies that (1) included only individuals with a history of NSSI or a history of suicide were excluded (22, 23); and (2) the study provided relevant data on the subjects over a 24-h period (24). In case of disagreements, consensus was sought from another author (WL) outside the evaluation.
Data extraction
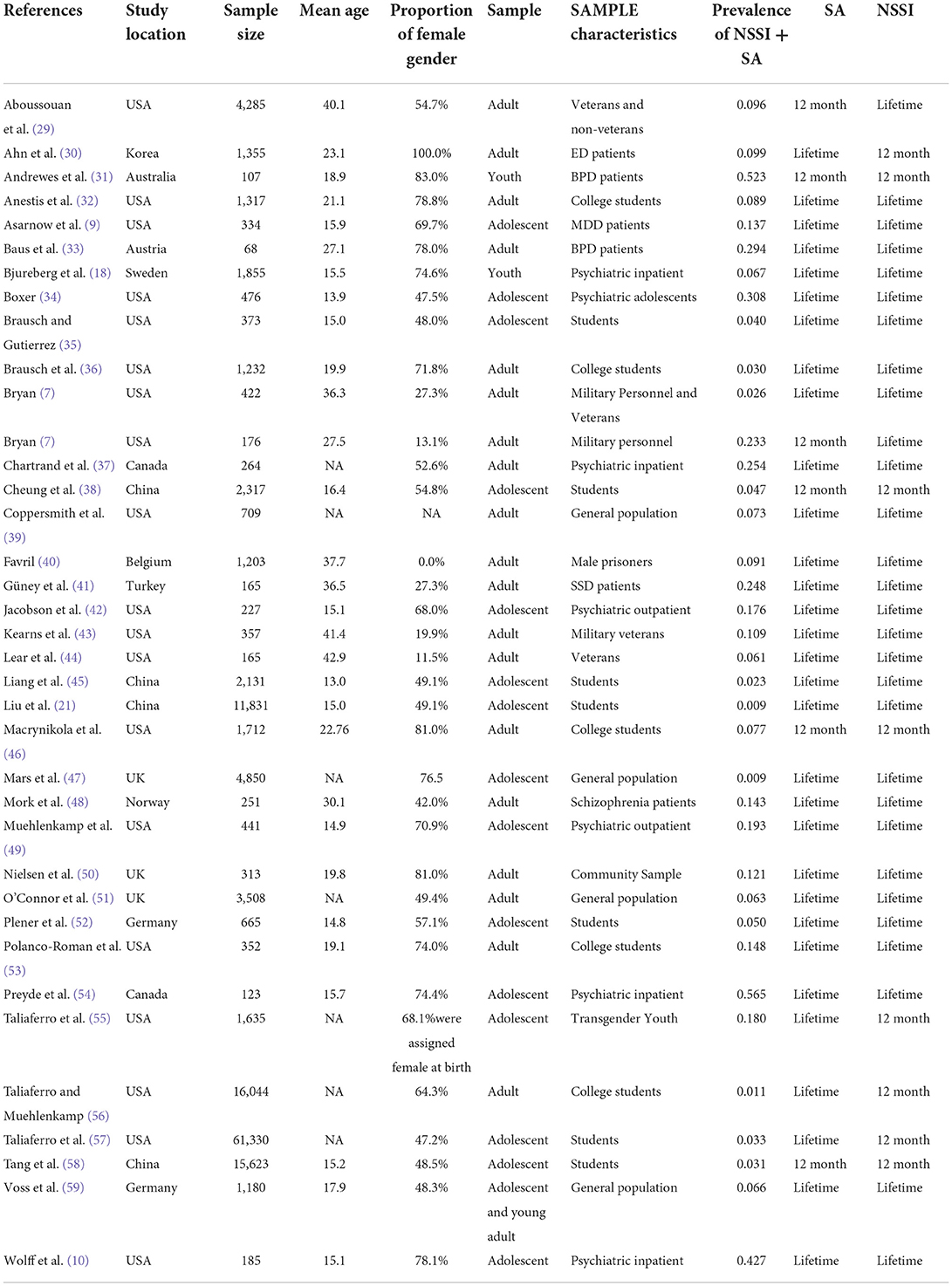
Two reviewers (ZY and FX) independently screened the data; disagreements were resolved by discussion. For each eligible study, the following data were extracted: first author, year of publication, country in which the study was conducted, total sample size, mean age of participants, female sex ratio, sample characteristics, number of participants with a history of suicide attempts and NSSI, and time scale of measurement of history of NSSI or suicide attempts. Data on the characteristics of all studies are shown in Table 1.
Data analysis
All statistical analyses were performed using Stata version 16.0, and the results for the incidence of non-suicidal self-injury and suicide attempts (NSSI +S A) were combined, with 95% confidence intervals used for all results.
Heterogeneity was assessed by the I2 statistic, p-values of the chi-square test for heterogeneity, and visual inspection of forest plots. Higher values of the I2 statistic indicate higher levels of heterogeneity, with 25% being low heterogeneity, 50% being moderate heterogeneity, and 75% being high heterogeneity (25). Given the diversity of participants between studies, the heterogeneity of the combined results was expected to be high, and the combined analysis of incidence was calculated using a random effects model.
To explore possible sources of heterogeneity and to understand the incidence of NSSI + SA among participants with different characteristics so that to determine the focus population for intervention, subgroup analyses were performed for outcomes with sufficient inclusion in the study, with subgroup analyses including: age of the sample (Adolescents & Youths, Adults); psychiatric co-morbidity (yes, no). Time scale of NSSI + SA (12-month NSSI + SA, other); geographic location, and economic and social development status (developed countries, developing countries).
Sensitivity analysis was performed by removing three or more studies with a high risk of bias to determine the effect of risk of bias on the results. Publication bias was assessed by looking at contour-enhanced funnel plots (26) and performing Egger's intercept test (27). A p-value less than or equal to 0.05 was considered a statistically significant value of publication bias, and the trim and fill method (28) was used to adjust for possible bias.
Results
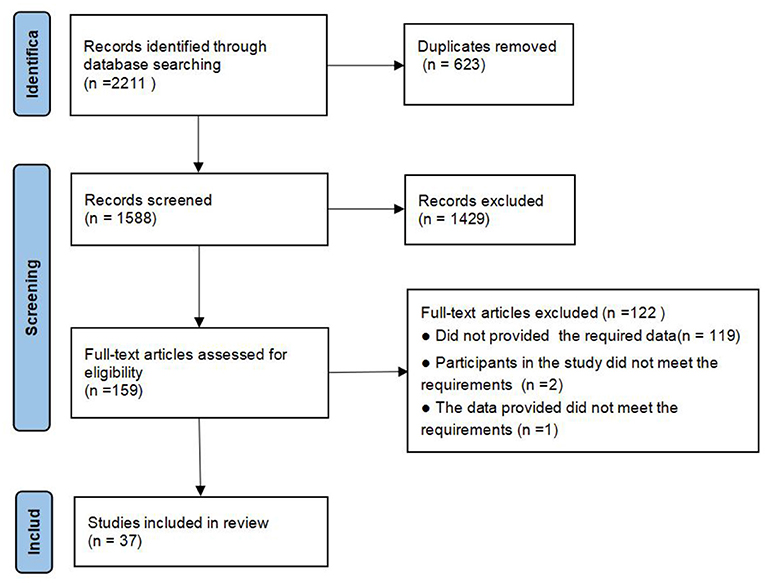
After an extensive literature search of the database, a total of 2,211 potentially relevant citations were collected. After eliminating duplicates, the remaining 1,588 studies were screened for titles and abstracts, 1,429 studies that did not meet the inclusion criteria were excluded, and finally 159 studies were comprehensively reviewed, 37 studies that met the criteria were used in this meta-analysis at last. The detailed process of paper selection and reasons for exclusion are shown in Figure 1.
Study characteristics
In the 37 studies included in the meta-analysis, there were 139,573 participants from 13 countries. The sample size of these studies ranged from N = 68 to 61,330, and the mean age of participants ranged from 13.0 to 42.9 years.
In terms of age group, 18 studies had adolescents and youth as participants, 15 of which had adolescents as participants, two studies had youth as participants, and one study had both adolescents and youth as participants. The remaining 19 studies investigated adult individuals. In terms of co-morbidity, participants in 13 studies were outpatients/inpatients with different types of psychiatric disorders, and participants in 24 studies were in the general population. Regarding the time scales of NSSI and SA measured, seven studies measured participants' history of NSSI within 12 months, 29 studies measured participants' lifetime history of NSSI, and only one study was measured with reference to the definition of NSSI in the DSM5; six studies measured participants' history of suicide attempts within 12 months, and 31 studies measured participants' lifetime suicide attempt history; only four studies measured participants' history of NSSI + SA within 12 months. Detailed study characteristics are shown in Table 1.
Total co-occurrence of NSSI + SA
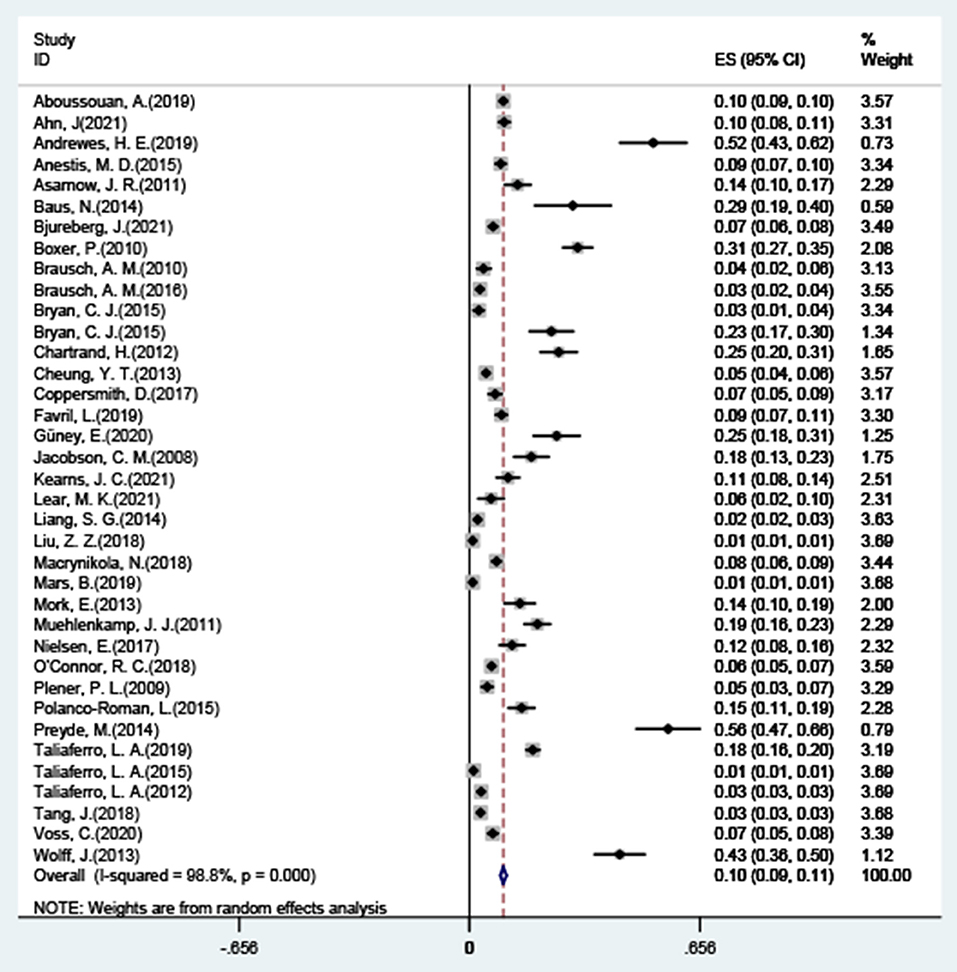
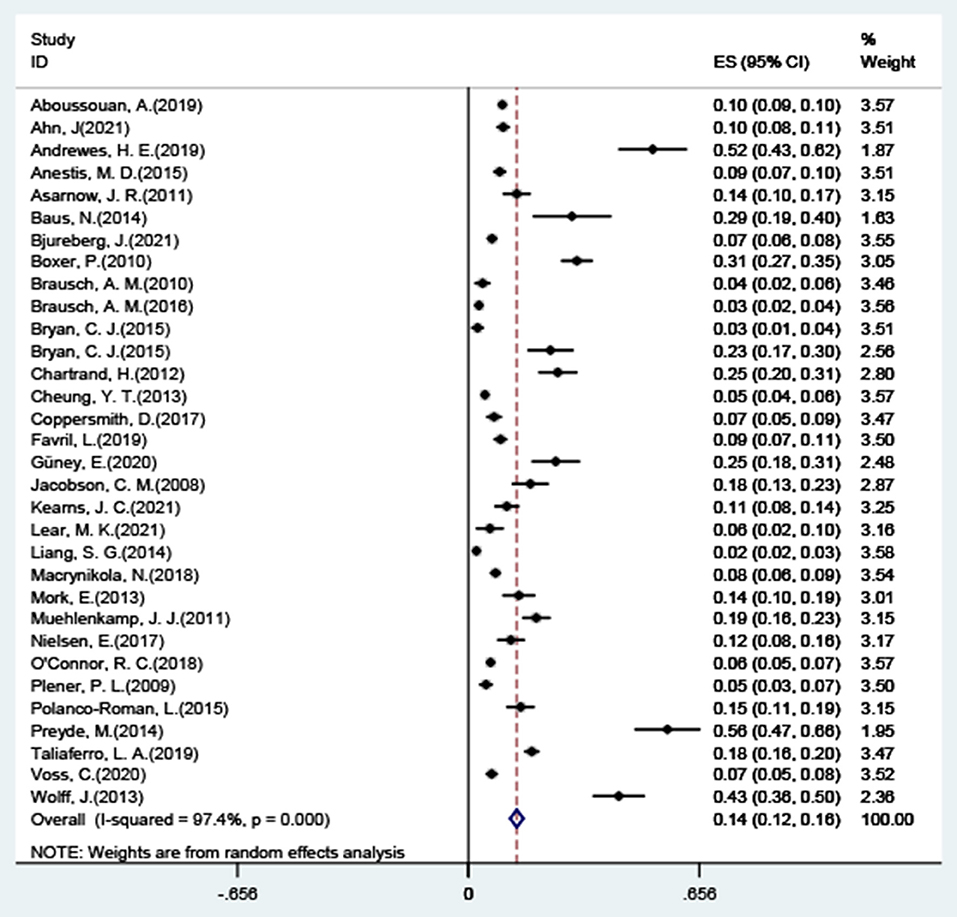
The results of the combined analysis showed that the overall co-occurrence of NSSI and suicide attempts was 9.6% (95% CI: 0.09–0.11), and the forest plot results are shown in Figure 2, with significant high levels of heterogeneity across all included studies (I2 = 98.8%, 95% CI: 98.60–98.91; p < 0.001). After excluding five studies with significant outlier outcomes (21, 47, 56–58), the incidence was 13.7% (95% CI: 0.12–0.16; I2 = 97.4%, 95% CI: 96.92–97.82; p < 0.001), the specific results are shown in Figure 3.
Egger's test suggested some possible publication bias (intercept = 7.96, 95% CI: 5.52–10.40, t = 6.62, df = 36, p < 0.001), and the estimate of the total incidence was 3.3% (95% CI: 0.02–0.04) after correction for publication bias by the cut-and-patch method.
Subgroup analysis
By combining the different subgroups, the results showed that the overall co-occurrence of NSSI + SA was slightly lower in adolescents and young adults (10%, 95% CI: 0.08–0.11; I2 = 98.5%, 95% CI: 98.81–99.16) than in adults (11%, 95% CI: 0.08–0.13; I2 = 99.0%, 95% CI: 98.1–98.76). The total co-occurrence of NSSI + SA was significantly lower in the general population (6%, 95% CI: 0.05–0.07; I2 = 98.8%, 95% CI: 98.58–98.96) than in patients with psychiatric disorders (26%, 95% CI: 0.20–0.32; I2 = 98.8%, 95% CI: 96.66–98.08) within 12 months. The overall concurrent incidence of NSSI events with SA events within 12 months was 17% (95% CI: 0.15–0.18; I2 = 100.0%, 95% CI: 98.08–99.04).
In the general population, the overall incidence of NSSI + SA was lower in adolescents and young adults (5%, 95% CI: 0.03–0.06; I2 = 99.0%, 95% CI: 98.80–99.24) than in adults (8%, 95% CI: 0.06–0.11; I2 = 98.6%, 95% CI: 98.26–98.80). Among patients with psychiatric disorders, the total incidence of NSSI + SA was higher in adolescents and young adults (29%, 95% CI: 0.19–0.40; I2 = 98.3%, 95% CI: 97.69–98.77) than in adults (20%, 95% CI: 0.12–0.28; I2 = 93.0%, 95% CI:86.54–96.32).
In a broader societal context, continent-based subgroup analyses revealed NSSI + SA rates of 12% (95% CI: 0.11–0.14; I2 = 98.9%, 95% CI:98.73-99.08) in North America, 5% (95% CI: 0.03-0.07; I2 = 98.7%, 95% CI:98.17-99.08) in Asia, and 8% (95% CI: 0.05–0.11; I2 = 98.2%, 95% CI:97.61-98.69) in Europe. In addition, the total NSSI + SA rate was higher in developed countries (11%, 95% CI:0.10–0.12; I2 = 98.8%, 95% CI:98.58-98.92) than in developing countries (4%, 95% CI:0.02-0.5; I2 = 98.6%, 95% CI:97.91-99.05).
Discussion
The present study found a concurrent incidence of 9.6% for NSSI and suicide attempt, this suggests that there is a larger group of people presenting with both NSSI and suicide attempts, which requires urgent attention and effective intervention. Given that studies have shown a significant co-occurrence of NSSI and suicidal behavior in adolescents and young adults (12, 60, 61), we analyzed adolescents and young adults as a subgroup in comparison to the adult sample. The results showed that the co-occurrence of NSSI + SA was 10% in adolescents and youth and 11% in adults in the overall sample, with small differences between subgroups. However, after also considering comorbidity, the results showed that the co-occurrence of NSSI + SA was slightly lower in adolescents and youth than in adults in the general population, while the co-occurrence of NSSI + SA was obvious higher in adolescents and youth than in adults in patients with psychiatric disorders. Based on this, it is necessary to take into account the age and comorbidity background of individuals in clinical prevention and intervention of different groups. For the general population, more attention should be paid to adult population about the NSSI + SA related risk factors, while for psychiatric patients, adolescents and young adults are high-risk groups of NSSI + SA. Moreover, NSSI + SA rates vary between countries with different economic and social development status and continents to which they belong, and need to be viewed in the context of different cultural backgrounds.
One way of thinking about why NSSI and suicide attempts co-occur has been suggested by Joiner in his interpersonal psychological theory of suicide (5), where he argues that a person must have both the desire to commit suicide and the ability to inflict fatal self-injury in order to complete a suicide or make a medically serious suicide attempt. In contrast, there are usually two different interpretations of the order in which the two behaviors occur (62). The first conception holds that individuals first develop suicidal desires and then engage in NSSI, and as the repeated behaviors accustom individuals to fear of self-directed violence and gain tolerance for physical pain, this increases their ability to make serious suicidal injuries and thus suicide attempts. That is, NSSI emerges as a mediating step in suicide attempts. The second conception, on the other hand, suggests that individuals first engage in NSSI without suicidal intent, and then gradually develop the desire to commit suicide through the habituation and acquisition of competence described above, which in turn leads to the emergence of suicide attempts. It is not surprising to find that both sets of explanations assume that NSSI occurs prior to a suicide attempt, although this trajectory assumption was unproven at the time.
In fact, in our literature screening, we found two studies that have now investigated the co-occurrence trajectory of NSSI and suicide attempt events by interview. In a study of a non-clinical sample, Bryan et al. found both cases of NSSI occurring first and cases of SA occurring first. NSSI was approximately 10 times more likely to occur prior to the first suicide attempt than the reverse, and the transition time was approximately 4.5 years for individuals who first engaged in NSSI followed by a suicide attempt. They found that a more common pathway for the two behaviors to occur together was to begin with suicidal ideation, followed by NSSI as an intervention step, and finally a suicide attempt, a developmental trajectory that accounted for 37% of all suicide attempt cases (7). This finding is broadly consistent with Joiner's view that NSSI is used as a mediating step in SA. Whereas in the study by Kearns et al. no cases were found in which suicide attempts appeared before NSSI, the results of that study showed that the transition time from NSSI to suicide attempts was about 4.25 years in psychiatric inpatients (43) and about 7.5 years in the community population (44). We can find some differences between the two studies in terms of the time of transition and the group of subjects investigated. It is also important to note that the subjects in both studies were discharged/non-discharged adult military personnel, so further research needs to be conducted as to whether the results can be applied to a broader group.
Regardless of who preceded or followed these two behaviors, it has been clinically found that individuals with a history of both NSSI and a history of suicide attempts are of greater concern. Previous studies have shown that individuals who report the presence of both a history of NSSI and a history of SA will present with more severe symptoms clinically than individuals who report only a history of NSSI or SA (11, 14, 41), and they have been found to have higher rates of psychiatric diagnoses, more severe psychological or behavioral problems (21), more severe psychiatric symptoms and psychosocial disorders, and higher rates of suicide ideation (40). This can be testified to some extent with the results of our study, where we found a 6% co-occurrence of NSSI and suicide attempts in the general population, and up to 26% in patients with psychiatric disorders, where clinical intervention is indeed imminent. As previous studies on the co-occurrence of the two suggest, NSSI may mark a prodromal period of increased risk for suicide attempts, and effective clinical interventions for patients who self-injure may prevent or halt the transition to suicide attempts, thereby reducing the rate of suicide attempts (7). Therefore, it is recommended that clinicians can regularly screen and assess all NSSI to determine if the motivation for the behavior has changed and if the original purpose is still being achieved, thus assessing whether there is an increased risk of suicide attempts (63). In addition, some scholars suggest that when intervening in NSSI, clinicians should avoid making individuals stop self-harming immediately, as this may eliminate their only coping mechanism, cause them to increase distress and turn to more lethal self-harming methods or suicide attempts (56).
In the current DSM-5, the time frame of the diagnosis is five or more days of intentional self-injury in the past year for non-suicidal self-injury, and a suicide attempt within the past 24 months and must not have involved a repeat self-injurious event for Suicidal Behavior Disorder. Most of the existing studies measure the occurrence of NSSI and suicide attempts over a 12-month or lifetime period in individuals, focusing on whether they have a history of the relevant behaviors and less on when and how many times the relevant behaviors occurred. Although the lack of data clearly defining the occurrence of NSSI for more than 5 days in a year does not fully correspond to the criteria in the DSM-5, we know from meta-analysis that the co-occurrence of both NSSI and suicide attempts in a 12-month period is 17%, and this proportion of individuals who co-occur in both behaviors is not negligible in clinical practice. Thus regardless, in the future development of the DSM, if the inclusion of non-suicidal self-injury and suicidal behavior disorder in the formal diagnostic system is to be considered, the definition of these groups with a history of both NSSI and suicide attempts within a year needs to be looked at carefully. Perhaps a new diagnosis that accommodates both behaviors will be needed, or perhaps the incompatible parts of the existing proposed entry will need to be adjusted. In conclusion, the inclusion of a mental disorder diagnosis is a decision that needs to be considered comprehensively, and this decision should take the actual situation into full consideration in order to formulate the corresponding diagnostic threshold indicators.
In addition to the above findings and reflections, there are some limitations in this study. First, because of the great geographical and cultural variability of the subject groups investigated in different studies, and the data on NSSI and SA reported in different studies were not consistent in terms of definition (time of occurrence, number of times, etc.), so the meta-analysis section showed a large heterogeneity of the combined, at the same time the lack of data on specific characteristics of the subjects made it difficult to eliminate the effect of heterogeneity through subgroup analysis. Second, the present study only conducted subgroup analysis on age, psychiatric comorbidity, NSSI + SA time scale, geographical location, economic and social development status, but did not conduct subgroup discussion on gender, emotional temperament type, mainly because the included study did not provide participants' data of NSSI + SA history at these two feature points. However, given that previous studies have shown that gender is an important factor and the relationship between NSSI and suicide attempts may be stronger in females than in males (7), and studies have found significant gender differences in individuals' NSSI + SA histories, at the same time, the measurement of affective temperament type was independently and closely related to the related clinical outcome (64). Therefore, in the future relevant research, further exploration of individuals with different genders and different emotional temperament types can be considered. In addition, considering that there may be some time transition between the occurrence of both NSSI and suicide attempts, it cannot be ruled out that some participants who have not yet attempted suicide in the present but will eventually do so at some point in the future when cross-sectional surveys are conducted, so more prospective studies are needed to control for this limitation.Last but not least, some scholars have found that subjects at risk for suicidal behavior or NSSI usually approached suicide through searching information and news regarding self-harm and suicidal behaviors on Internet (65). Therefore, in future studies, researchers can further verify whether individuals with a history of NSSI experience the process of Internet information search in the process of turning to suicide attempt and are affected accordingly, so as to confirm the direction of clinical intervention in this dimension.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
ZY contributed to the conceptualization, methodology, software, investigation, formal analysis, data curation, and writing—original draft. FX contributed to the investigation, formal analysis, and writing—review and editing. WL contributed to the conceptualization, supervision, validation, and data curation. All authors approved the final version of publication.
Acknowledgments
We are grateful to all authors of the full-text articles.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dong M, Zeng LN, Lu L, Li XH, Ungvari GS, Ng CH, et al. (2019). Prevalence of suicide attempt in individuals with major depressive disorder: a meta-analysis of observational surveys. Psychol Med. (2019) 49:1691–704. doi: 10.1017/S0033291718002301
2. Yoshimasu K, Kiyohara C, Miyashita K. Suicidal risk factors and completed suicide: meta-analyses based on psychological autopsy studies. Environ Health Prev Med. (2008) 13:243–56. doi: 10.1007/s12199-008-0037-x
3. Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, Lönnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. (2004) 161:562–3.
4. American Psychiatric Association. Suggested Criteria for DSM-5 Non-suicidal Self-injury Disorder. (2012). Available online at: http://www.dsm5.org/Pages/Default.aspx (accessed May 1, 2012).
5. Joiner TE, Ribeiro JD, Silva C. Nonsuicidal self-injury, suicidal behavior, and their co-occurrence as viewed through the lens of the interpersonal theory of suicide. Curr Dir Psychol Sci. (2012) 21:342–7. doi: 10.1177/0963721412454873
6. Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. (2017) 143:187–232. doi: 10.1037/bul0000084
7. Bryan CJ, Rudd MD, Wertenberger E, Young-McCaughon S, Peterson A. Nonsuicidal self-injury as a prospective predictor of suicide attempts in a clinical sample of military personnel. Compr Psychiatry. (2015) 59:17. doi: 10.1016/j.comppsych.2014.07.009
8. Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol. (2013) 122:231–7. doi: 10.1037/a0030278
9. Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. (2011) 50:772–81. doi: 10.1016/j.jaac.2011.04.003
10. Wolff J, Frazier EA, Esposito-Smythers C, Burke T, Sloan E, Spirito A, et al. Cognitive and social factors associated with NSSI and suicide attempts in psychiatrically hospitalized adolescents. J Abnorm Child Psychol. (2013) 41:1005–13. doi: 10.1007/s10802-013-9743-y
11. Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. (2012) 32:482–95. doi: 10.1016/j.cpr.2012.05.003
12. Nock MK, Joiner TJ, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. (2006) 144:65–72. doi: 10.1016/j.psychres.2006.05.010
13. Kapur N, Cooper J, O'Connor RC, Hawton K. Non-suicidal self-injury v. attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry. (2013) 202:326–8. doi: 10.1192/bjp.bp.112.116111
14. Grandclerc S, De Labrouhe D, Spodenkiewicz D, Lachal M, Moro JMR. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: a systematic review. PLoS ONE. (2016) 11:e153760. doi: 10.1371/journal.pone.0153760
15. Butler AM, Malone K. Attempted suicide v. non-suicidal self-injury: behaviour, syndrome or diagnosis? Br J Psychiatry. (2013) 202:324–5. doi: 10.1192/bjp.bp.112.113506
16. Oquendo MA, Baca-Garcia E. Suicidal behavior disorder as a diagnostic entity in the DSM-5 classification system: advantages outweigh limitations. World Psychiatry. (2014) 13:128–30. doi: 10.1002/wps.20116
17. Zetterqvist M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adolesc Psychiatry Ment Health. (2015) 9:31. doi: 10.1186/s13034-015-0062-7
18. Bjureberg J, Kuja-Halkola R, Ohlis A, Lichtenstein P, D'Onofrio BM, Hellner C, et al. Adverse clinical outcomes among youths with nonsuicidal self-injury and suicide attempts: a longitudinal cohort study. J Child Psychol Psychiatry. (2021). doi: 10.1111/jcpp.13544
19. Battle D.E. 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM). Codas. 25:191–192. doi: 10.1590/s2317-17822013000200017
20. Hooley JM. Self-harming behavior: introduction to the special series on non-suicidal self-injury and suicide. Appl Prev Psychol. (2008) 12:155–8. doi: 10.1016/j.appsy.2008.08.001
21. Liu ZZ, Chen H, Bo QG, Chen RH, Li FW, Lv L, et al. Psychological and behavioral characteristics of suicide attempts and non-suicidal self-injury in Chinese adolescents. J Affect Disord. (2018) 226:287–93. doi: 10.1016/j.jad.2017.10.010
22. Aouidad A, Cohen D, Mirkovic B, Pellerin H, Garny DLRS, Consoli A, et al. Borderline personality disorder and prior suicide attempts define a severity gradient among hospitalized adolescent suicide attempters. BMC Psychiatry. (2020) 20:525. doi: 10.1186/s12888-020-02930-4
23. Gulbas LE, Hausmann-Stabile C, De Luca D, Tyler SM, Zayas TRLH. An exploratory study of nonsuicidal self-injury and suicidal behaviors in adolescent Latinas. Am J Orthopsychiatry. (2015) 85:302–14. doi: 10.1037/ort0000073
24. Cloutier P, Martin J, Kennedy A, Nixon MK, Muehlenkamp JJ. Characteristics and co-occurrence of adolescent non-suicidal self-injury and suicidal behaviours in pediatric emergency crisis services. J Youth Adolesc. (2010) 39:259–69. doi: 10.1007/s10964-009-9465-1
25. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
26. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. (2007) 61:991–6. doi: 10.1016/j.jclinepi.2007.11.010
27. Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
28. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
29. Aboussouan A, Snow A, Cerel J, Tucker RP. Non-suicidal self-injury, suicide ideation, and past suicide attempts: comparison between transgender and gender diverse veterans and non-veterans. J Affect Disord. (2019) 259:186–94. doi: 10.1016/j.jad.2019.08.046
30. Ahn J, Lee JH, Jung YC. Identifying predictors of non-suicidal self-injuries in individuals with eating disorders. Yonsei Med J. (2021) 62:159–63. doi: 10.3349/ymj.2021.62.2.159
31. Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Relationships between the frequency and severity of non-suicidal self-injury and suicide attempts in youth with borderline personality disorder. Early Interv Psychiatry. (2019) 13:194–201. doi: 10.1111/eip.12461
32. Anestis MD, Khazem LR, Law KC. How many times and how many ways: the impact of number of nonsuicidal self-injury methods on the relationship between nonsuicidal self-injury frequency and suicidal behavior. Suicide Life Threat Behav. (2015) 45:164–77. doi: 10.1111/sltb.12120
33. Baus N, Fischer-Kern M, Naderer A, Klein J, Doering S, et al. Personality organization in borderline patients with a history of suicide attempts. Psychiatry Res. (2014) 218:129–33. doi: 10.1016/j.psychres.2014.03.048
34. Boxer P. Variations in risk and treatment factors among adolescents engaging in different types of deliberate self-harm in an inpatient sample. J Clin Child Adolesc Psychol. (2010) 39:470–80. doi: 10.1080/15374416.2010.486302
35. Brausch AM, Gutierrez PM. Differences in non-suicidal self-injury and suicide attempts in adolescents. J Youth Adolesc. (2010) 39:233–42. doi: 10.1007/s10964-009-9482-0
36. Brausch AM, Williams AG, Cox EM. Examining intent to die and methods for nonsuicidal self-injury and suicide attempts. Suicide Life Threat Behav. (2016) 46:737–44. doi: 10.1111/sltb.12262
37. Chartrand H, Sareen J, Toews M, Bolton JM. Suicide attempts versus nonsuicidal self-injury among individuals with anxiety disorders in a nationally representative sample. Depress Anxiety. (2012) 29:172–9. doi: 10.1002/da.20882
38. Cheung YT, Wong PW, Lee AM, Lam TH, Fan YS, Yip PS, et al. Non-suicidal self-injury and suicidal behavior: prevalence, co-occurrence, and correlates of suicide among adolescents in Hong Kong. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1133–44. doi: 10.1007/s00127-012-0640-4
39. Coppersmith D, Nada-Raja S, Beautrais AL. Non-suicidal self-injury and suicide attempts in a New Zealand birth cohort. J Affect Disord. (2017) 221:89–96. doi: 10.1016/j.jad.2017.06.029
40. Favril L. Non-suicidal self-injury and co-occurring suicide attempt in male prisoners. Psychiatry Res. (2019) 276:196–202. doi: 10.1016/j.psychres.2019.05.017
41. Güney E, Alniak I, Erkiran M. Predicting factors for non-suicidal self-injury in patients with schizophrenia spectrum disorders and the role of substance use. Asian J Psychiatr. (2020) 52:102068. doi: 10.1016/j.ajp.2020.102068
42. Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. (2008) 37:363–75. doi: 10.1080/15374410801955771
43. Kearns JC, Brown SL, Cero I, Gorman KR, Nock MK, Keane TM, et al. Temporal sequences of suicidal and nonsuicidal self-injurious thoughts and behaviors among inpatient and community-residing military veterans. J Affect Disord. (2021) 294:430–40. doi: 10.1016/j.jad.2021.07.088
44. Lear MK, Penzenik ME, Forster JE, Starosta A, Brenner LA, Nazem S, et al. Characteristics of nonsuicidal self-injury among veterans. J Clin Psychol. (2021) 77:286–97. doi: 10.1002/jclp.23027
45. Liang SG, Yan J, Zhu CZ, Situ MJ, Du N, Fu XY, et al. [Personality traits of Chinese adolescents with non-suicidal self injury and suicide attempt]. Sichuan Da Xue Xue Bao Yi Xue Ban. (2014) 45:970–3.
46. Macrynikola N, Miranda R, Soffer A. Social connectedness, stressful life events, and self-injurious thoughts and behaviors among young adults. Compr Psychiatry. (2017) 80:140–9. doi: 10.1016/j.comppsych.2017.09.008
47. Mars B, Heron J, Klonsky ED, Moran P, O'Connor RC, Tilling K, et al. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiat. (2019) 6:327–37. doi: 10.1016/S2215-0366(19)30030-6
48. Mork E, Walby FA, Harkavy-Friedman JM, Barrett EA, Steen NE, Lorentzen S, et al. Clinical characteristics in schizophrenia patients with or without suicide attempts and non-suicidal self-harm–a cross-sectional study. BMC Psychiatry. (2013) 13:255. doi: 10.1186/1471-244X-13-255
49. Muehlenkamp JJ, Ertelt TW, Miller AL, Claes L. Borderline personality symptoms differentiate non-suicidal and suicidal self-injury in ethnically diverse adolescent outpatients. J Child Psychol Psychiatry. (2011) 52:148–55. doi: 10.1111/j.1469-7610.2010.02305.x
50. Nielsen E, Sayal K, Townsend E. Functional coping dynamics and experiential avoidance in a community sample with no self-injury vs. non-suicidal self-injury only vs those with both non-suicidal self-injury and suicidal behaviour. Int J Env Res Public Health. (2017) 14:575. doi: 10.3390/ijerph14060575
51. O'Connor RC, Wetherall K, Cleare S, Eschle S, Drummond J, Ferguson E, et al. Suicide attempts and non-suicidal self-harm: national prevalence study of young adults. BJPsych Open. (2018) 4:142–8. doi: 10.1192/bjo.2018.14
52. Plener PL, Libal G, Keller F, Fegert JM, Muehlenkamp JJ. An international comparison of adolescent non-suicidal self-injury (NSSI) and suicide attempts: Germany and the USA. Psychol Med. (2009) 39:1549–58. doi: 10.1017/S0033291708005114
53. Polanco-Roman L, Jurska J, Quiñones V, Miranda R. Brooding, reflection, and distraction: relation to non-suicidal self-injury versus suicide attempts. Arch Suicide Res. (2015) 19:350–65. doi: 10.1080/13811118.2014.981623
54. Preyde M, Vanderkooy J, Chevalier P, Heintzman J, Warne A, Barrick K, et al. The psychosocial characteristics associated with NSSI and suicide attempt of youth admitted to an in-patient psychiatric unit. J Can Acad Child Adolesc Psychiatry. (2014) 23:100–10.
55. Taliaferro LA, McMorris BJ, Rider GN, Eisenberg ME. Risk and protective factors for self-harm in a population-based sample of transgender youth. Arch Suicide Res. (2019) 23:203–21. doi: 10.1080/13811118.2018.1430639
56. Taliaferro LA, Muehlenkamp JJ. Risk factors associated with self-injurious behavior among a national sample of undergraduate college students. J Am Coll Health. (2015) 63:40–8. doi: 10.1080/07448481.2014.953166
57. Taliaferro LA, Muehlenkamp JJ, Borowsky IW, McMorris BJ, Kugler KC. Factors distinguishing youth who report self-injurious behavior: a population-based sample. Acad Pediatr. (2012) 12:205–13. doi: 10.1016/j.acap.2012.01.008
58. Tang J, Li G, Chen B, Huang Z, Zhang Y, Chang H, et al. Prevalence of and risk factors for non-suicidal self-injury in rural China: results from a nationwide survey in China. J Affect Disord. (2018) 226:188–95. doi: 10.1016/j.jad.2017.09.051
59. Voss C, Hoyer J, Venz J, Pieper L, Beesdo-Baum K. Non-suicidal self-injury and its co-occurrence with suicidal behavior: an epidemiological-study among adolescents and young adults. Acta Psychiatr Scand. (2020) 142:496–508. doi: 10.1111/acps.13237
61. Benjet C, González-Herrera I, Castro-Silva E, Méndez E, Borges G, Casanova L, et al. Non-suicidal self-injury in Mexican young adults: prevalence, associations with suicidal behavior and psychiatric disorders, and DSM-5 proposed diagnostic criteria. J Affect Disord. (2017) 215:1–8. doi: 10.1016/j.jad.2017.03.025
62. Kerr PL, Muehlenkamp JJ, Turner JM. Nonsuicidal self-injury: a review of current research for family medicine and primary care physicians. J Am Board Fam Med. (2010) 23:240–59. doi: 10.3122/jabfm.2010.02.090110
63. Muehlenkamp JJ, Gutierrez PM. Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch Suicide Res. (2007) 11:69–82. doi: 10.1080/13811110600992902
64. Baldessarini RJ, Innamorati M, Erbuto D, Serafini G, Fiorillo A, Amore M, et al. Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. J Affect Disord. (2016) 210:19–21. doi: 10.1016/j.jad.2016.12.003
Keywords: non-suicidal self-injury (NSSI), suicide attempt (SA), co-occurrence, systematic review, meta-analysis
Citation: Ye Z, Xiong F and Li W (2022) A meta-analysis of co-occurrence of non-suicidal self-injury and suicide attempt: Implications for clinical intervention and future diagnosis. Front. Psychiatry 13:976217. doi: 10.3389/fpsyt.2022.976217
Received: 23 June 2022; Accepted: 22 July 2022;
Published: 12 August 2022.
Edited by:
Paul Hoff, University of Zurich, SwitzerlandReviewed by:
Say How Ong, Institute of Mental Health, SingaporeGianluca Serafini, San Martino Hospital (IRCCS), Italy
Copyright © 2022 Ye, Xiong and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wentian Li, bGl3ZW50aWFuMjAxOEAxNjMuY29t
 Zhiyu Ye
Zhiyu Ye Fang Xiong
Fang Xiong Wentian Li
Wentian Li