- 1Department of Public Health, Xinjiang Medical University, Urumqi, China
- 2Obstetrics Department, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
Objective: To investigate the relationship between pregnancy stress and prenatal anxiety in pregnant women in Urumqi, Xinjiang, and the mediating effect of mental resilience level on the relationship between pregnancy stress and prenatal anxiety.
Method: The investigation involved 750 pregnant women at a tertiary hospital in Urumqi, and included a questionnaire eliciting general demographic information, a pregnancy stress scale (Pregnancy Pressure Scale, PPS), generalized anxiety disorder scale (Generalized Anxiety Disorder-7, GAD-7), and a mental resilience scale (Connor—Davidson resilience scale, CD-RISC). The Bootstrap mediation effect test was used to test the effect relationship between variables, and Amos was used to establish the structural equation model.
Results: Among the 750 participants, 122 (16.2%) had moderate or greater pregnancy stress (PPS > 1), 372 (49.6%) had mild or greater anxiety symptoms (GAD-7 > 5), and 241 (32.1%) had good or higher mental resilience score. Pregnancy stress negatively affected resilience (β = −0.37, p < 0.01), and resilience also negatively affected prenatal anxiety (β = −0.12, p < 0.01). The mediating effect value of resilience was 8.3%.
Conclusion: Pregnancy stress, mental resilience, and prenatal anxiety were significantly correlated, and mental resilience played a partial mediating role in the influence of pregnancy stress on prenatal anxiety. It is recommended that pregnant women exercise their mental resilience to reduce the incidence of prenatal anxiety and promote physical and mental health.
Introduction
Anxiety disorder during pregnancy mainly refers to pregnant women during pregnancy feel panic, tension as the main feature of mental health disorders (1, 2). With the emergence of adverse emotions in pregnant women, other negative psychological aspects associated with pregnancy also appear, such as pregnancy pressure. Pregnancy pressure refers to the pressure that pregnant women feel from the environment and work during pregnancy, and it is an inducing factor that aggravates anxiety and depression in pregnant women (3, 4). In recent years, many researchers have paid attention to the mental health of pregnant women, especially anxiety and depression. Studies have shown that excessive pregnancy pressure had a negative impact on the health of pregnant women and the growth of their offspring (5–7). One study showed that low anxiety and cortisol levels and reduced work-life conflicts could prevent fetal complications (6, 7). Besides, research indicated that serious psychological problems during pregnancy can make pregnant women suicidal (8). The response to the new coronavirus in recent years has increased public panic and anxiety, affecting people's mental health (9). Many studies focus on epidemiological investigation and infection prevention measures, but pay little attention to mental health problems (10, 11).
Pregnant womens' ability to self-regulate and adapt well by using their own positive qualities and external environmental resources are called psychological resilience (12, 13). The psychological resilience scale includes 25 self-reported questions and covers five factors: personal competence; high standards and tenacity; trust in one's instincts, tolerance of negative effect, and strengthening effects of stress; positive acceptance of change and secure relationships; control; and spiritual influences (14, 15). Studies have shown that if pregnant women have a high level of resilience they can actively face negative situations and various maladaptive behaviors during pregnancy (16–18). In this study, 750 pregnant women were investigated to study the correlations between pregnancy stress, resilience and prenatal anxiety, and to explore the mediating effect of resilience between pregnancy stress and prenatal anxiety.
Methods
Study participants
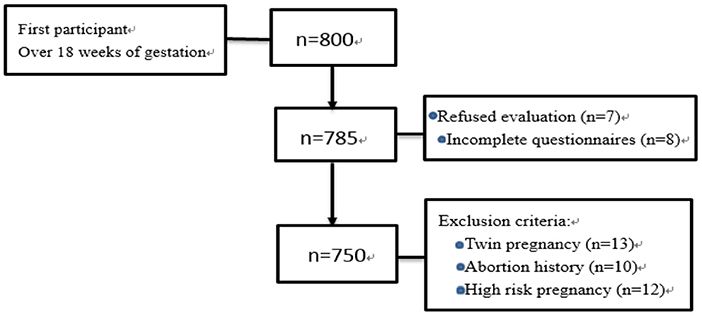
This study was carried out in the Department of Obstetrics and Gynecology of A tertiary hospital in Urumqi city, starting from December 2020 to May 2021. The study participants come from districts of Xinjiang, and they were pregnant women who underwent labor examination and we used random sampling methods to randomly distribute questionnaires to the women who came for a prenatal examination on the same day, so as to ensure that the probability of each pregnant woman being selected was equal. Inclusion criteria: clear diagnosis of pregnancy, informed consent, gestational weeks over 18. Exclusion criteria: no informed consent, incomplete data collection, twin pregnancy, have a history of abortion, severe mental disorders, cognitive disorders, hearing disorders, language communication disorders, severe pregnancy complications, and high risk pregnancies. The investigators conducted on-site questionnaire surveys for those women who met the inclusion and exclusion criteria, and the questionnaires were completed independently. If a questionnaire was found to be incomplete, it was not used. We invited 800 women to join this research, and exclude 50 people who do not meet the inclusion criteria. Finally, 750 valid questionnaires were collected, with an effective success rate of 93.7%, as shown in Figure 1.
General demographic questionnaires included general demographic data such as maternal age, educational level, monthly family income, place of residence, and occupation, as well as maternal family environment and living conditions, marital relations, exercise, psychological preparation for pregnancy, and pregnancy knowledge.
Pregnancy pressure scale
This scale contains three dimensions with a total of 30 entries. Dimension 1 “parent role” contains 15 items, and was the scale of the top 15 entries; dimension 2 “mother and child health and safety” contained eight items, and scaled 16–23; dimension 3 “body shape and physical activity change” contained four entries, namely items 24–27 in the inventory. There were also three items not included in the dimensions: the last three items of the scale (19). The Likert 4 grade scoring method was adopted foe this scale, and the score is the actual total score of the scale divided by the total items of the scale, where 0 points represents no pressure, 0.001–1 points represents mild pressure, 1.001–2 points represents moderate pressure and 2.001–3 points represents severe pressure (3). The higher the score, the greater the pregnancy pressure for a women, and the Cronbach's α coefficient was 0.953.
Generalized anxiety disorder-7
The Generalized Anxiety Scale, which consist of seven items, used a 4-level scoring system. Each part was scored on a scale of 0–3, with an overall score of 0–4 representing normal, 5–9 representing mild anxiety, 10–14 representing moderate anxiety, and 15–21 representing severe anxiety (20). Out of a total of 21 points, the higher the score, the higher the anxiety level; the Cronbach's α coefficient was 0.885.
Connor-Davidson resilience scale
This scale includes 3 dimensions of tenacity (13 items), strength (8 items) and optimism (4 items), with a total of 25 items (21). The Likert 5 score is used, and 0–4 points indicate almost never, rarely, sometimes, often and almost always. The total score of the scale was 0–100 points. A score of < 60 indicates poor resilience, 60–70 indicates normal resilience, a score of 70–80 indicates good resilience, and ≥80 indicates excellent resilience (22). The Cronbach's α coefficient is 0.972.
Statistical methods
The data from the questionnaire were collected, and the information was input into Statistical Package for Social Sciences (SPSS) for Windows version 25.0 for analysis, the enumeration data were expressed as the number of cases and percentage, and the measurement data that obeyed the normal distribution were statistically described. Normally distributed data between groups were analyzed using an independent sample t-test or analysis of ANOVA. Pregnancy stress, prenatal anxiety and resilience scores were in line with a normal distribution using Shapiro-Wilk Test (P > 0.05). The study also measured the corresponding Cronbach's αs. The mediating effect of resilience between pregnancy stress and prenatal anxiety was tested by non-parametric percentile Bootstrap method (23), the non-parametric percentile method of deviation correction, and N = 5,000. Mediation effect analysis proposes to determine whether a mediation effect exists and the type of mediation's corresponding parameters. Parameter refers to influence effect value. When the Bootstrap 95% confidence interval does not include 0, the mediating effect is considered to be statistically significant (24, 25). A mediating effect path analysis chart was produced using Amos23.0 modeling and analysis.
Results
General demographic data
Among the 750 pregnant women who met the criteria and were included in this study, 613 (81.7%) were of Han nationality and 137 (18.3%) were of ethnic minorities. Sixty-four (8.5%) were younger than 25-years-old, 601 (80.1%) were between 25- and 35-years-old, and 85 (11.3%) were older than 35-years-old. Among them, 62 (8.3%) had less than high school education, 206 (27.5%) had high school education, 357 (47.6%) had a bachelor's degree, 115 (15.3%) had a master's degree or above, and 10 (1.3%) had others degree. In total, 573 (76.4%) were employed and 177 (23.6%) were housewives; 33 (4.4%) live in rural areas, and 717 (95.6%) live in urban areas.
Pregnancy stress, prenatal anxiety, and mental resilience level
The data were analyzed statistically using SPSS 25.0. In this study, the prenatal anxiety score of the pregnant women was (4.98 ± 3.38), the pregnancy stress score was (0.60 ± 0.48), and its' three dimension scores are (0.18 ± 0.21; 0.24 ± 0.17; 0.11 ± 0.10); the mental resilience score was (60.17 ± 19.44), and its' three dimension scores are (30.31 ± 10.47; 20.36 ± 6.39; 9.50 ± 3.46); In this study, 122 participants (16.2%) had moderate or greater pregnancy stress (PPS>1), 372 (49.6%) had mild or greater anxiety symptoms (GAD-7>5), and 241 (32.1%) had a good or higher mental resilience score of 70. There were statistically significant differences in the score of the GAD-7 scale among pregnant women with different educational levels and monthly family incomes, and statistically significant differences in the score for the PPS scale among pregnant women with different ages, monthly family incomes, and occupations. Except for ethnicity resilience scores were statistically significant in different demographic data, as shown in Table 1.
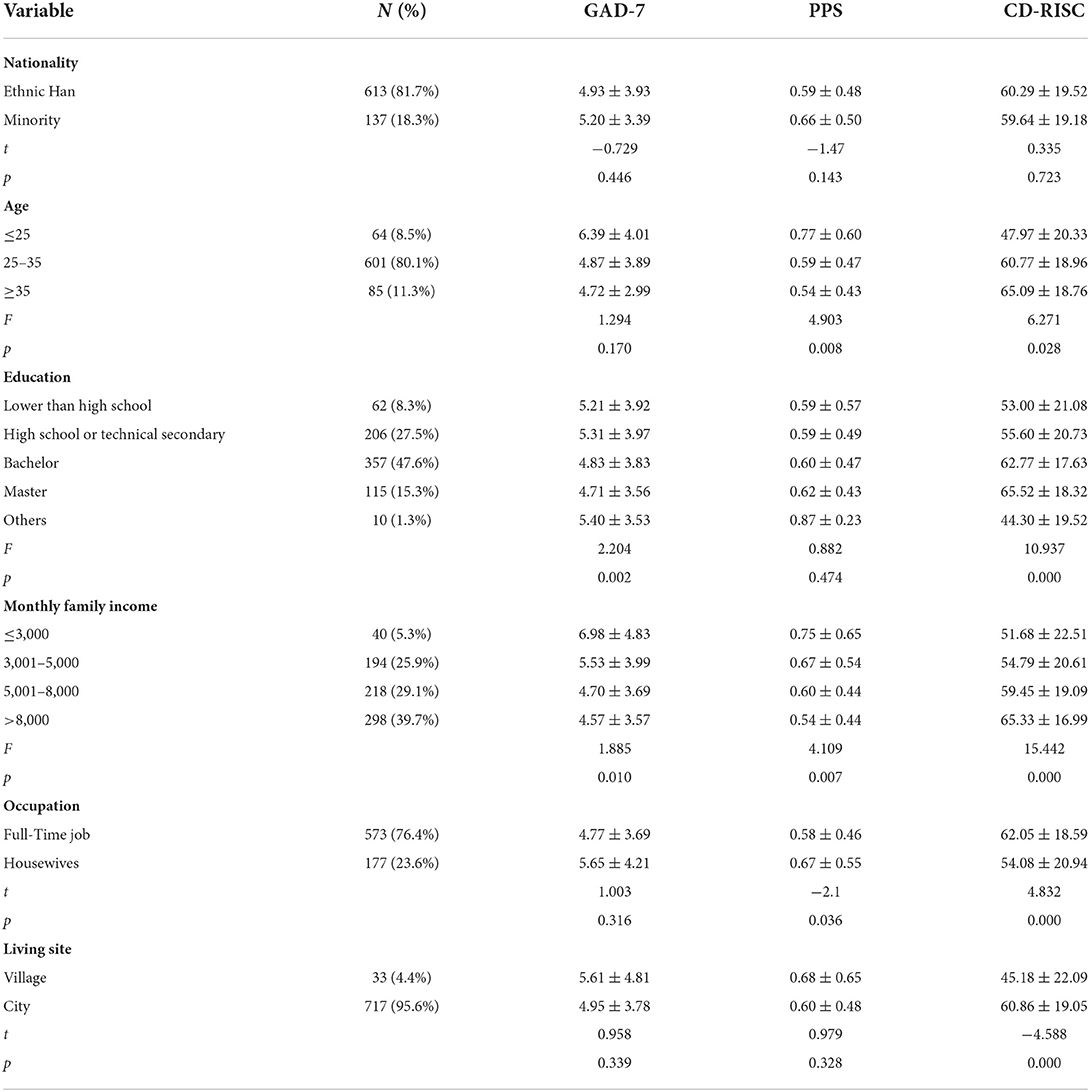
Table 1. GAD-7, PPS, and CD-RISC scores of pregnant women with different demographic characteristics.
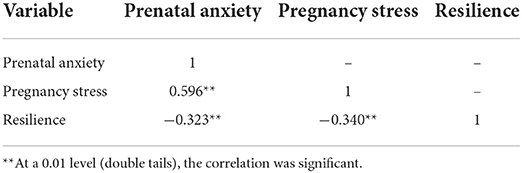
Correlation analysis of pregnancy stress, resilience, and prenatal anxiety
The data of this study conform to normality by Shapiro-Wilk Test (p > 0.05). According to Pearson's correlation analysis, prenatal anxiety was significantly positively correlated with pregnancy stress (p < 0.01), resilience was significantly negatively correlated with prenatal anxiety (p < 0.01), and resilience was significantly negatively correlated with pregnancy stress (p < 0.01), as shown in Table 2.
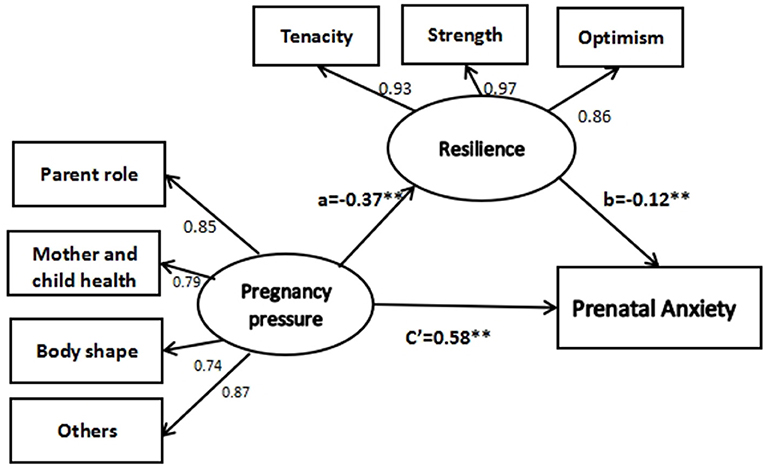
The mediating effect of resilience between pregnancy stress and prenatal anxiety
Using the Bootstrap mediating effect test, this study assumes that resilience plays a mediating role between pregnancy stress and prenatal anxiety. After the analysis of the mediating effect, it was found that the total effect and indirect effect of pregnancy stress on prenatal anxiety were significant (p < 0.01). The confidence interval of the mediating effect of resilience as a mediating variable between pregnancy stress and prenatal anxiety was [0.024–0.074], as shown in Table 3.
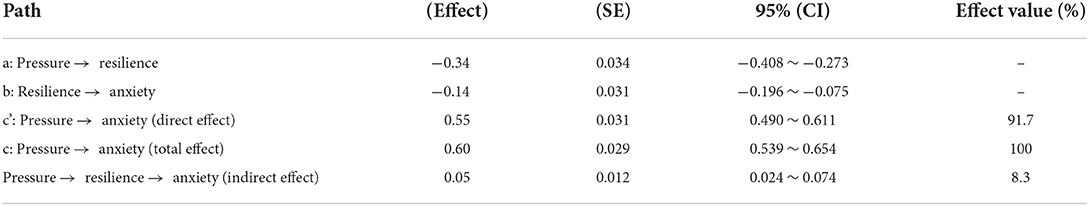
Table 3. Bootstrap analysis of the mediating effect of resilience between pregnancy stress and prenatal anxiety.
With resilience as the mediating variable, pregnancy pressure as the independent variable, and prenatal anxiety as the dependent variable, Amos was introduced to develop a result equation model. The results showed that the path coefficients of the model were statistically significant (p < 0.01). The fitting indexes of the structural equation model were as follows: CMIN/DF = 4.042, RMSEA = 0.064, GFI = 0.977, AGFI = 0.954, CFI = 0.987, and TLI = 0.980. The results showed that pregnancy pressure negatively affected resilience (β = −0.37, p < 0.01), and resilience negatively affected prenatal anxiety (β = −0.12, p < 0.01). According to the path analysis chart, the intermediary effect a*b = c–c', namely −0.37 × −0.12 = 0.60–0.55, indicating that the intermediary effect is exists (see Figure 2). The mediating effect (a*b = 0.05) accounted for 8.3% of the total effect (0.60), indicating that resilience partially mediated the relationship between pregnancy stress and prenatal anxiety.
Discussion
In this study, it was found that the overall pregnancy stress level in pregnant women was below the level of mild stress, and the score for the stressors (mother–child health and safety) was the highest. It appeared that worrying about mother-child health was the main stressor, which was inconsistent with the results of a previous study that the main stressor was the stress caused by the parenting role (26). The analysis of the reasons for this difference showed that the gestational age of the sample studied by Guo et al. was ≥37 weeks, while the pregnant women in our study had no limit on gestational age. The closer to the birth, the more fearful the pregnant woman is about changing her role (19, 27). Most of the pregnant women in our group had mild prenatal anxiety. The prenatal anxiety score was positively correlated with family monthly income, which was consistent with the previous research showing that the higher the family monthly income, the lower the prenatal anxiety level (28). Less than half of the pregnant women were at high or higher levels of resilience. Resilience is negatively correlated with maternal prenatal anxiety, indicating that maternal resilience can alleviate maternal prenatal anxiety (29, 30).
Pregnancy pressure, prenatal anxiety, and resilience were significantly correlated. Pregnancy pressure was positively correlated with prenatal anxiety, indicating that the greater the pregnancy pressure, the higher the degree of prenatal anxiety, which is consistent with the results of other research (31, 32). Therefore, pregnant women should be given care during pregnancy, which can reduce their pressure and anxiety (33). There was a negative correlation between resilience and prenatal anxiety, indicating that the level of resilience is a protective factor for prenatal anxiety: the higher the level of resilience, the lower the degree of prenatal anxiety, which is consistent with the results of previous studies (34). Pregnant womens' resilience will affect their ability to cope with major life events. The physiological changes caused by pregnancy itself also exert stress, and for pregnant women who cannot follow positive strategies to manage their emotions effectively and adapt to the state of pregnancy, it is difficult to maintain mental health, thus affecting their overall health (35, 36).
In this study, the score for the resilience optimism dimension of pregnant women was high, and 63.8% of pregnant women exceeded the average score of this dimension. However, the score for the tenacity dimension was lowest, which is consistent with the results of previous studies (37). This result suggests that we should focus on helping pregnant women to improve their resilience (38). This study concluded that the psychological resilience of pregnant women had an intermediary role in regulating pregnancy stress and prenatal anxiety. Emotion can be regulated by psychological resilience (39, 40). Good psychological resilience can produce positive emotions, so that pregnant women can effectively reduce the impact of stress on negative emotions (41, 42).
To summarize, resilience, as an intermediary, can affect both maternal pregnancy stress and maternal prenatal anxiety, as a protective factor against both (43). The higher the level of resilience of pregnant women, the lower the pregnancy pressure and the milder the symptoms of prenatal anxiety (44). In addition, resilience played a partial mediating effect in the relationship between pregnancy stress and prenatal anxiety in pregnant women, that is, pregnancy stress could directly affect prenatal anxiety, or indirectly affect prenatal anxiety through resilience (45, 46).
This study explored the relationship between pregnancy stress and prenatal anxiety in pregnant women, and verified the mediating effect of resilience between them. However, this study had certain limitations. First, the study used a cross-sectional study design, which cannot accurately determine causal relationships, when compared with a cohort study. Second, the study did not limit the gestational age of pregnant women during sample selection, although previous studies have shown that gestational age was one of the important factors affecting prenatal depression and pregnancy pressure (47). Therefore, the influence of gestational age on prenatal depression and pregnancy stress was not examined in this study. Last but not least, this study participants did not exclude pregnant women conceived through assisted reproductive techniques.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Xinjiang Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XT and LL processing data. WZ and GW are participate in writing articles. BS and TJ making tables and figures. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Thirteen Five Key Science—Public Health and Preventive Medicine (Grant No. 11091121204) and the Nature Science Foundation of Xinjiang autonomous region (Grant No. 2018D01C146).
Acknowledgments
The authors thank all the people who completed the questionnaire. We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Demircan S, Bor ED. Knowledge, perception, and protective measures of Turkish pregnant women towards COVID-19 pandemic and their effects on anxiety levels. J Obstet Gynaecol. (2022) 5:1018–22. doi: 10.1080/01443615.2021.1990232
2. Zou Y, Hui S, Demei X, Haihui M, Juan W, Rongming X, et al. Anxiety, depression and sleep status of pregnant women in Beijing during the prevalence of new corona pneumonia. Chin J Ment Health. (2020) 3:267–72. doi: 10.3969/j.issn.1000-6729.2022.03.014
3. Kim Y, Chung CW. Development of the Korean pregnancy stress scale. Jpn J Nurs Sci. (2018) 15:113–24. doi: 10.1111/jjns.12175
4. Luong TC, Pham TTM, Nguyen MH, Do AQ, Pham LV, Nguyen HC, et al. Fear, anxiety and depression among pregnant women during COVID-19 pandemic: impacts of healthy eating behaviour and health literacy. Ann Med. (2021) 1:2120–31. doi: 10.1080/07853890.2021.2001044
5. Mei H, Li N, Li JW, Zhang D, Cao ZQ, Zhou YJ, et al. Depression, anxiety, and stress symptoms in pregnant women before and during the COVID-19 pandemic. J Psychosom Res. (2021) 2021:110586. doi: 10.1016/j.jpsychores.2021.110586
6. Ramiro-Cortijo D, de la Calle M, Benitez V, Gila-Diaz A, Moreno-Jimenez B, Arribas SM. Maternal psychological and biological factors associated to gestational complications. J Pers Med. (2021) 11:183. doi: 10.3390/jpm11030183
7. Ramiro-Cortijo D, de la Calle M, Gila-Diaz A, Moreno-Jimenez B, Martin-Cabrejas MA, Arribas SM. Maternal resources, pregnancy concerns, and biological factors associated to birth weight and psychological health. J Clin Med. (2021) 10:695. doi: 10.3390/jcm10040695
8. Legazpi PCC, Rodriguez-Munoz MF, Le HN, Balbuena CS. Suicidal ideation: prevalence and risk factors during pregnancy. Midwifery. (2022) 106:103226. doi: 10.1016/j.midw.2021.103226
9. Awad-Sirhan N, Simó-Teufel S, Molina-Muñoz Y, Cajiao-Nieto J, Izquierdo-Puchol MT. Factors associated with prenatal stress and anxiety in pregnant women during COVID-19 in Spain. Enferm Clin. (2021) 32:S5–13. doi: 10.1016/j.enfcle.2021.10.003
10. Xiang YT, Zhao YJ, Liu ZH, Li XH, Zhao N, Cheung T, et al. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. (2020) 16:1741–4. doi: 10.7150/ijbs.45072
11. Shen X, Li YT, Feng J, Lu ZX, Tian KM, Gan Y. Current status and associated factors of psychological among the Chinese residents during the coronavirus disease 2019 pandemic. Int J Soc Psychiatry. (2022) 68:34–43. doi: 10.1177/0020764020980779
12. Wu Z, Huan L, Yaling F. Study on the correlation between maternal fear of childbirth and family care and resilience. J Shenyang Med Coll. (2020) 22:59–62. doi: 10.1016/j.ijnss.2020.09.003
13. Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. (2020) 266:113348. doi: 10.1016/j.socscimed.2020.113348
14. Jung YE, Min JA, Shin AY, Han SY, Lee KU, Kim KS, et al. The Korean version of the connor-davidson resilience scale: an extended validation. Stress Health. (2012) 28:319–26. doi: 10.1002/smi.1436
15. Yu XN, Lau JTF, Mak WWS, Zhang JX, Lui WWS. Factor structure and psychometric properties of the connor-davidson resilience scale among Chinese adolescents. Compr Psychiatry. (2011) 52:218–24. doi: 10.1016/j.comppsych.2010.05.010
16. Ren J. Path analysis of psychological resilience and its influencing factors of threatened premature pregnant women. Nurs J. (2019) 34:426–9. doi: 10.16821/j.cnki.hsjx.2019.05.011
17. Ma RQ, Yang FZ, Zhang LJ, Sznajder KK, Zou CQ, Jia YJ, et al. Resilience mediates the effect of self-efficacy on symptoms of prenatal anxiety among pregnant women: a nationwide smartphone cross-sectional study in China. BMC Pregn Childb. (2021) 21:430. doi: 10.1186/s12884-021-03911-5
18. Oviedo Diana C, Sofia PM, Sofia RA, Tratner Adam E, Elianne PQ, Carlos C, et al. Psychosocial response to the COVID-19 pandemic in panama. Front Public Health. (2022) 10:919818. doi: 10.3389/fpubh.2022.919818
19. Chen W, Nahong S, Weifei L. Analysis of influencing factors of late pregnancy pressure in second-child pregnant women. China Mater Child Health Care. (2021) 36:3791–4. doi: 10.19829/j.zgfybj.issn.1001-4411.2021.16.042
20. Jiang L, Sujun Z, Zhonghua P, Zhonghua P, Dizi Y. PHQ-9 and GAD-7 are used to analyze the mental health survey results of pregnant women. China Mater Child Health Res. (2021) 32:1172–7. doi: 10.3389/fpsyg.2021.701629
21. Kuiper H, van Leeuwen CCM, Stolwijk-Swuste JM, Post MWM. Measuring resilience with the connor-davidson resilience scale (CD-RISC): which version to choose? Spinal Cord. (2019) 57:360–6. doi: 10.1038/s41393-019-0240-1
22. Li L, Yufeng Y, Xuyan L, Yuan Y, Yurui W. Study on the level of resilience and its influencing factors in patients with early threatened abortion. Mod Med Health. (2020) 36:996–9. doi: 10.1002/pon.5485
23. Jiang C, Shu L. Intermediary analysis and bootstrap program application. Psychol Explorat. (2015) 35:458–63. doi: 10.16719/j.cnki.1671-6981.20210431
24. Wen Z, Ye B. Mediating effect analysis: method and model development. Prog Psychol Sci. (2014) 22:731–45. doi: 10.3724/SP.J.1042.2014.00731
25. Zhao L, Fang L, Jinfang H, Tingting Z, Chunfei W. Mediation effect testing procedures and their applications. Biotechnol World. (2014) 11:216. doi: 10.1080/00273171.2018.1528542
26. Guo W, Yang G, Lin B. Investigation on the influencing factors of psychological stress in pregnant women in late pregnancy. Chin Med Sci. (2018) 8:139–41. doi: 10.3969/j.issn.2095-0616.2018.06.043
27. Perez-Aranda A, Garcia-Campayo J, Gude F, Luciano Juan V, Feliu-Soler A, Gonzalez-Quintela A, et al. Impact of mindfulness and self-compassion on anxiety and depression: the mediating role of resilience. Int J Clin Health Psychol. (2021) 21:100229. doi: 10.1016/j.ijchp.2021.100229
28. Jin X, Xu X, Qiu J, Xu Z, Sun L, Wang Z, et al. Psychological resilience of second-pregnancy women in China: a cross-sectional study of influencing factors. Asian Nurs Res. (2021) 15:121–8. doi: 10.1016/j.anr.2021.01.002
29. Lubian Lopez DML, Hinojo CAB, Bernal JEA, Laiz MF, Santiago JA, Vilches VG, et al. Resilience and psychological distress in pregnant women during quarantine due to the COVID-19 outbreak in Spain: a multicentre cross-sectional online survey. J Psychosom Obstet Gynaecol. (2021) 42:115–22. doi: 10.1080/0167482X.2021.1896491
30. Li GP, Kong LH, Zhou HY, Kang XF, Fang YY, Li P. Relationship between prenatal maternal stress and sleep quality in Chinese pregnant women: the mediation effect of resilience. Sleep Med. (2016) 25:8–12. doi: 10.1016/j.sleep.2016.02.015
31. Liu L, Mingyuan T, Weiwei X. Correlation analysis of anxiety, pregnancy stress and mental health in pregnant women with gestational diabetes mellitus. Mod Med Health Res Electro Mag. (2020) 4:1–3.
32. Stanhope KK, Comeau DL, Ulloa M, Leon JS, Suglia SF, Hogue CJ, et al. Perceptions of stress and resilience among Latina women enrolled in prenatal care in Metro Atlanta through an ecosocial lens. Health Soc Care Community. (2021) 29:e348–58. doi: 10.1111/hsc.13359
33. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
34. Shang N, Huafu Z, Shengwen D. Correlation between resilience and anxiety of pregnant women in late pregnancy. Tianjin Nurs. (2019) 27:509–13. doi: 10.3969/j.issn.1006-9143.2019.05.002
35. Huang J, Longqiong W, Xinyang Y, Bizhen L. Understanding the mediating role of social support and childbirth self-efficacy between resilience and FOC of pregnant women. Chongqing Med. (2022) 1–10. Available online at: http://kns.cnki.net/kcms/detail/50.1097.R.20220209.0908.004.html
36. Luo Z, Yaqing S, Jiajia Y, Yifan Z, Zhengkui L, Fangfang S. Perceived stress, resilience, and anxiety among pregnant Chinese women during the COVID-19 pandemic: latent profile analysis and mediation analysis. Front Psychol. (2021) 12:696132. doi: 10.3389/fpsyg.2021.696132
37. Tu C. Correlation analysis between resilience and family care of pregnant women with severe preeclampsia. Mod Diag Treat. (2021)32:3490–2.
38. Liu JH, Yan XX, Chu LL, Li CE, Hu JM, Zou SQ. Mediating role of mental resilience between sleep quality and mindfulness level of pregnant women screened by prenatal diagnosis. J Healthc Eng. (2022) 2022:7011836. doi: 10.1155/2022/7011836
39. Elmas B, Vatansever M, Civan KA, Salman OB, Asut G, Cakmak IB, et al. Evaluation of psychological resilience and anxiety levels of patients with hyperemesis gravidarum diagnosis and comparison with healthy pregnant women. Turk J Obstet Gynecol. (2021) 18:115–23. doi: 10.4274/tjod.galenos.2021.05994
40. Ladekarl M, Olsen NJ, Winckler K, Brodsgaard A, Nohr EA, Heitmann BL, et al. Early postpartum stress, anxiety, depression, and resilience development among Danish first-time mothers before and during first-wave COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:11734. doi: 10.3390/ijerph182211734
41. Lv L. Analysis of psychological pressure and resilience of pregnant women with pernicious placenta previa. Chin Rural Med. (2020) 27:25–6. doi: 10.19542/j.cnki.1006-5180.004094
42. Magnusson FL, Rogathi JJ, Sigalla GN, Manongi R, Rasch V, Gammeltoft T, et al. Does resilience moderate the effect of intimate partner violence on signs of depression among Tanzanian pregnant women: a cross-sectional study. Acta Obstetr Gynecol Scand. (2021) 100:768–74. doi: 10.1111/aogs.14062
43. Bien A, Rzonca E, Grzesik-Gasior J, Pieczy kolan A, Humeniuk E, Michalak M, et al. Determinants of psychosocial resilience resources in obese pregnant women with threatened preterm labor-A cross-sectional study. Int J Environ Res Public Health. (2021) 18:10590. doi: 10.3390/ijerph182010590
44. Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, et al. Depression, anxiety, resilience, and coping: the experience of pregnant and new mothers during the first few months of the COVID-19 pandemic. J Womens Health. (2021) 30:654–64. doi: 10.1089/jwh.2020.8866
45. La Marca-Ghaemmaghami P, Zimmermann R, Haller M, Ehlert U. Cortisol and estriol responses to awakening in the first pregnancy trimester: associations with maternal stress and resilience factors. Psychoneuroendocrinology. (2021) 125:105120. doi: 10.1016/j.psyneuen.2020.105120
46. Brunton R, Wood T, Dryer R. Childhood abuse, pregnancy-related anxiety and the mediating role of resilience and social support. J Health Psychol. (2022) 27:868–78. doi: 10.1177/1359105320968140
Keywords: pregnant women, pregnancy stress, prenatal anxiety, mental resilience, the mediating effect
Citation: Tuxunjiang X, Li L, Wumaier G, Zhang W, Sailike B and Jiang T (2022) The mediating effect of resilience on pregnancy stress and prenatal anxiety in pregnant women. Front. Psychiatry 13:961689. doi: 10.3389/fpsyt.2022.961689
Received: 05 June 2022; Accepted: 16 September 2022;
Published: 14 October 2022.
Edited by:
Robert James Wickham, Lafayette College, United StatesReviewed by:
Marco Garzitto, University of Udine, ItalyDavid Ramiro-Cortijo, Autonomous University of Madrid, Spain
Copyright © 2022 Tuxunjiang, Li, Wumaier, Zhang, Sailike and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ting Jiang, NzA3NTc5MDE1QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiabidan Tuxunjiang
Xiabidan Tuxunjiang Ling Li2†
Ling Li2† Gulijianati Wumaier
Gulijianati Wumaier Ting Jiang
Ting Jiang