
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry, 28 July 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.961538
This article is part of the Research TopicMental-Health-Related Stigma and Discrimination: Prevention, Role, and Management StrategiesView all 16 articles
Introduction: The stigma of mental illness has a negative impact on the diagnosis and treatment of these disorders. Considering the high prevalence of mental illness, the attitude of medical specialists toward mental disorders, who are front liners in diagnosing and treating these patients, is critical. Therefore, we examined the attitude of Iranian medical specialty trainees toward providing health care services for patients with mental illness.
Methods: We included 143 residents in the fields that have the most interactions with patients with mental disorders, including internal medicine, surgery, neurology, cardiovascular diseases, and psychiatry. A demographic checklist, as well as the opening minds scale for health care providers stigma assessment questionnaire, was provided, which measures five dimensions of improvement, social responsibility, social distance, exposure, and other (such as risk) in health care providers toward delivering the healthcare services to patients with mental disorders.
Results: The mean score of stigma for mental illness in medical specialty trainees was 61.36 ± 4.83 out of 100. Psychiatric residents have the least stigmatizing attitude (58.38 ± 3.54), and internal medicine and cardiology residents have the highest score, respectively, (62.96 ± 6.05, 62.45 ± 3.80). As for comparing subscales between specialties, only the social responsibility subscale showed a significant difference, with psychiatry having less stigma toward social responsibility (12.93 ± 2.01) than cardiology (15.09 ± 1.50) trainees.
Conclusion: The attitude of medical specialty trainees toward providing health care services for patients with mental illness is not uniform; internal medicine and cardiology residents have more stigmatizing attitude, while psychiatric residents have less stigmatizing attitude. It seems that not every contact could be useful in making a better attitude toward mental illness, but it needs preconditions, like a structured contact that leads to positive outcomes. Anti-stigma interventions are needed to improve the attitude of medical specialty trainees toward providing health care services to patients with mental illness.
Stigma is described as a trait that society considers undesirable and distinguishes the stigmatized person from other members of the community to which they belong. Stigma persists today in attitudes toward patients with some medical and mental disorders. This is more obvious than in the medical profession (1–4). Mental illness stigma is a serious problem that affects patients and those around them, as well as health care institutions and staff working with people with mental illness. The more a person with a mental illness feels stigmatized, the lower his or her self-esteem, social adjustment, and quality of life (5, 6). Stigma also affects access to care, as people may not be willing to seek help despite mental or emotional problems, as it may be seen as a weakness or a failure (7, 8).
In addition, people with a mental disorder diagnosis suffer from the effects of discrimination in health care. Not only do people with mental illness benefit less from access to primary care, but there is evidence that physicians perform fewer physical examinations, laboratory tests, prevention, and treatment interventions on this population (9–11). For instance, general practitioners may feel less comfortable having a patient with schizophrenia than a patient with depression or diabetes. They may have a pessimistic view of the effectiveness of psychiatric treatment (12). Although stigmatization of mental illness among health care professionals has been studied less than the general population, existing evidence suggests that medical practitioners also hold a range of attitudes toward individuals with a psychiatric diagnosis like those held by the public (13). In some studies, professional experience has been associated with a more favorable attitude. Therefore, physicians who interact more with patients may understand diversity, and the point of view toward the stigmatized group members is essential for strengthening the positive attitudes (14, 15).
In Iran, studies have shown that roughly 1 out of 4 people suffer from at least one mental disorder (16). As with most other countries, a significant number of patients with mental disorders feel that they are humiliated, discriminated against, and socially rejected. This affects the patients and their families, who often experience unpleasant stigma. It is also observed that there is a correlation between the number of hospitalizations, duration of the disorder, and the type of the mental illness with the stigma that patients and their families encounter (17, 18).
Due to the high prevalence of mental disorders in the community and the negative impact of stigmatizing attitude toward this group of patients in the treatment and diagnosis of these disorders, we decided to implement the following study to use the results to help the process of diagnosis and treatment of patients with mental disorder and to uncover where more anti-stigma interventions are needed. It is a fact that, for many patients, particularly in low- and middle-income countries like Iran, the primary choice is to use a university medical health center. Knowing that medical specialty trainees carry out a large volume of the workload of these centers, this study examined the attitude of these health care providers who have the most direct interaction with patients with mental illness in Iran toward providing services for these vulnerable groups.
This cross-sectional study was conducted at the Iran University of Medical Sciences, one of the three largest public medical universities in Tehran, Iran, in 2020 and 2021. We enrolled all medical specialty trainees of specialties that frequently are in direct contact with the patients with mental disorders, including internal medicine, surgery, neurology, cardiovascular disorders, and psychiatry. Inclusion criteria were ongoing studying at one of the courses mentioned above at Iran University of Medical Sciences, consent for participation, and a lack of a previous degree in a mental health-related major like psychology.
An online survey package containing two questionnaires was sent to participants via an online link by email and/or social media. The participants were reminded for the first time within a week and a second time a month later.
A personal demographic information checklist, including the following (age, gender, residency program, marital status, number of shifts per month, and self-report of personal experience with mental illness, family history of psychiatric disorder, and history of violence or serious personal problems), and the stigma assessment questionnaire.
Opening minds scale for health care providers (OMS-HC) is a self-report questionnaire that evaluates attitudes and behavioral intentions toward people with mental illness. The main questionnaire was first confirmed with the Cronbach’s alpha coefficient of 0.82. The full OMS-HC contains 20 items. Each item is responded as strongly agree, agree, neither agree nor disagree, disagree, strongly disagree, and scored from 1 to 5. The total score ranges from 20 (least stigmatizing) to 100 (most stigmatizing). Items 3, 8, 9, 10, 11, 15, and 19 require reverse coding. This questionnaire consists of five dimensions: social distance (Items 1, 3, 16, 17, and 19), other concepts (overshadow of detection and dangerous; Items 2 and 15), detection (Items 4, 5, 6, 7, and 10), recovery (Items 8, 9, and 14), and social responsibility (Items 11, 12, 13, 18, and 20; 19, 20).
The OMS-HC questionnaire has been translated and validated by two groups in Iran, with the Cronbach’s alpha: 0.76 and 0.87, respectively. While the translation of Kordloo et al. contains only ten items, we considered Vaghee et al.’s translation more suitable and used it in the study (21).
The study protocol was reviewed by the Iran University of Medical Science Ethics Committee and approved with the IR license.IUMS.FMD.REC.1399.228. The participants filled out the questionnaire voluntarily and anonymously after online consent for participation.
The collected data were analyzed using the statistical software analysis tool SPSS (version 16). For describing demographic information of the participants, results were expressed as mean and standard deviation (Mean ± SD) for quantitative variables and as a percentage for categorical qualitative variables. We used ANOVA for comparing the groups of trainees. The significance level was considered less than 0.05.
A total of 143 medical specialty trainees were enrolled in the study, with a completion rate of about 70%, 58.7% female, and 41.3% male. The mean age was 30.72 (SD: 4.22). The average night shift per month for residents was 7.97 (SD: 3.51) nights. Other demographic features are presented in Table 1.
The correlation between the total stigma score and the demographic features was analyzed. Among the demographic variables, having a personal history of mental illness was the only associated and significantly meaningful with the total stigma score (P-value = 0.007, r = 0.150).
The mean total stigma score for mental illness in the participants was 61.36 ± 4.83 out of 100, ranging from 51 to 75 (95% C.I. 60.56–62.16). The mean score for each group is presented in Table 2. When comparing the total stigma score between different specialties, the ANOVA results showed a significant difference between other groups (P-value = 0.002). A further post hoc test was done to express the differences in detail, shown in Table 2. Psychiatric trainees have the least stigmatizing score compared to internal medicine and cardiology trainees, having the most stigmatizing score, respectively.
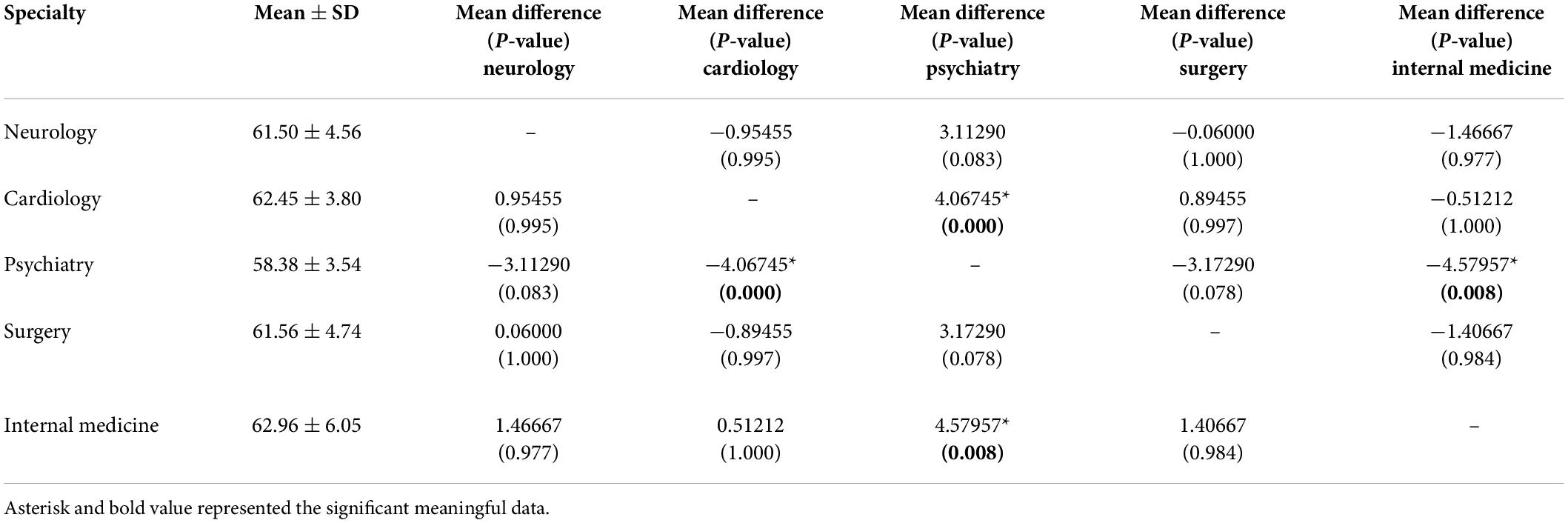
Table 2. Data descriptive: The mean total stigma score for mental illness among different medical residents and their comparison with one another.
As for comparing different subscales of the scale within other specialties, it was only in the social responsibility subscale that there was a significant difference in different groups, with psychiatry having less stigma toward social responsibility (12.93 ± 2.01) than cardiology (15.09 ± 1.50) trainees (P-value < 0.001) as shown in Table 3.
The mean total stigma score for mental illness in the participants in our study is 61.36 ± 4.83 out of 100, ranging from 51 to 75. Previous studies using the same 20-item OMS-HC questionnaire have shown fewer total stigma scores. For instance, a 2012 study by Kassam et al. showed that the mean total score among health care providers/trainees in Canada was 57.5 (95% C.I. 57.2–57.9). Scores ranged from 41 to 96, and the standard deviation was 4.8 (22). In another study, the median score among healthcare trainees other than medical students in Italy was 27, IQR [21;30] for the 20 items version (theoretical range, 0–80; 23). Similar studies on pharmacy students and medical students in Canada had total stigma scores of 46.7 (95% C.I. 44.5–48.4) and 48.6 (95% C.I., 47.5–49.8), respectively, (24, 25).
Being part of the middle eastern community, higher stigma scores in our study could be due to various factors such as different answering styles or sociocultural backgrounds. Cross-cultural differences, such as the importance of public opinion and conventional viewpoints, and religious environment, are significant and need further studies (26, 27).
The result of our study shows that psychiatric trainees have a less stigmatizing attitude toward patients with mental disorders compared to internal medicine and cardiology trainees. However, this finding was insignificant for surgery and neurology trainees.
Some specialties, such as cardiology and internal medicine, have higher workloads and burnout (28, 29). Increased workload and burnout may be associated with a more stigmatizing attitude toward mental health. This could be one reason for lower stigmatizing attitudes in psychiatric residents.
It is believed that patients with mental disorders are more frequently visited in cardiology and internal medicine clinics than in surgery (30–32). This finding is controversial with previous theories that more contact with patients with mental illness will reduce the stigma. One explanation could be that, in fields such as internal medicine and cardiology, the mental disorder of the patients is not systematically diagnosed and treated. As a result, patients remain unwell, and the unsatisfied doctor would keep the negative attitude that patients with mental illness can never get better and cannot have a normal life. Whereas in fields such as psychiatry, with proper treatment of patients, longitudinal assessment, and routine follow-ups, achievements are vividly seen. The response to treatment leads to recovery, balanced work, life, and a social environment. Thus, these exclusive preconditions may be the reason for the less stigmatizing attitude of psychiatric trainees (14, 15).
In other words, not every contact could help make a better attitude toward mental illness, but it needs preconditions.
When comparing the different stigma subscales, our study only shows that psychiatric trainees are less stigmatized toward social responsibility than other groups. Previous studies have shown that stigma toward social responsibility negatively affects empathy (20). An integrated relationship model has been proposed: physicians with a better experience, more excellent patient-to-physician contact, and more empathy toward them feel less uneasy with patients with mental disorders; thus, they tend to reduce their social distance from them (33).
Age, gender, marital status, and the number of shifts seem to have no meaningful relationship with stigma toward mental disorders. Our findings are consistent with previous and similar studies in Iran (34). Our results indicate that medical trainees with a personal history of medical illness have a less stigmatizing attitude toward patients with mental disorders. This finding is similar to previous studies (35, 36). Overall, it seems like personal contact has a protective factor toward manifesting less stigma toward mental disorders, such as those with personal experience, or psychiatrist trainees who work with patients with mental disorders daily. This finding is supported by similar previous results (37, 38). As discussed previously, contact does not seem to be enough. Perhaps, in these categorized groups, once they see the long-term effect of treatment on people closest to them, they feel less stigmatized toward them and people with mental illness.
To the best of our knowledge, our study is among the very first studies in Iran on the attitude toward providing healthcare for patients with mental disorders. Iran University of Medical Sciences is one of the largest medical universities in Iran, and so the findings may be generalized to Iranian trainees. Nevertheless, the small sample size, particularly for between-group analyses, limits the interpretation of our findings. In addition, the lack of longitudinal study for observation of participants over time and using anti-stigma interventions is another limitation of our study.
The development of anti-stigma programs can simultaneously target the attitudes of medical specialty trainees toward mental disorders, help-seeking, and their social behaviors toward patients with a mental disorder. These strategies can target different observations in this study. Different anti-stigma strategies, such as educational workshops, showing a movie about a patient with a mental disorder, close contact with patients with mental disorders, and group free discussion, were suggested by previous studies (4).
Future studies on larger sample sizes, among other specialties and universities, other health care community members, and qualitative methods are suggested, particularly in the medical staff with the most interaction with patients with mental disorders. In addition, the efficacy and effectiveness of anti-stigma strategies in well-designed trials among this group of healthcare providers should be evaluated in future trials.
The attitude of medical specialty trainees toward providing health care services for patients with mental illness is not uniform; internal medicine and cardiology residents have more stigmatizing attitude, while psychiatric residents have less stigmatizing attitude. It seems that not every contact could be useful in making a better attitude toward mental illness, but it needs preconditions, like a structured contact that leads to positive outcomes. Personal experience with mental illness also has a positive effect on the attitude. Anti-stigma interventions to improve the attitude of medical specialty trainees toward providing health care services for patients with mental illness should be considered.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Iran University of Medical Science. The patients/participants provided their written informed consent to participate in this study.
SM, SS, and MS: conceptualization and design. SM and MS: data collection and initial draft preparation. SM and SS: data analyses. All authors editing and review.
We must appreciate the participants for their helpful collaboration.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Goffman E. Asylums: Essays on the Social Situation of Mental Patients and Other Inmates. Garden City, NY: Anchor Books (1968).
2. Ransing R, Ramalho R, de Filippis R, Ojeahere MI, Karaliuniene R, Orsolini L, et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brain Behav Immun. (2020) 89:555–8. doi: 10.1016/j.bbi.2020.07.033
3. Adiukwu F, Bytyçi DG, Hayek SE, Gonzalez-Diaz JM, Larnaout A, Grandinetti P, et al. Global perspective and ways to combat stigma associated with COVID-19. Indian J Psychol Med. (2020) 42:569. doi: 10.1177/0253717620964932
4. Rezvanifar F, Shariat SV, Shalbafan M, Salehian R, Rasoulian M. Developing an educational package to improve attitude of medical students toward people with mental illness: a delphi expert panel, based on a scoping review. Front Psychiatry. (2022) 13:860117. doi: 10.3389/fpsyt.2022.860117
5. Hankir A, Northall A, Zaman R. Stigma and mental health challenges in medical students. BMJ Case Rep. (2014) 2014:bcr2014205226.
6. Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: the consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. (2001) 52:1621–6.
7. Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. (2005) 20:529–39.
8. Schomerus G, Matschinger H, Angermeyer MC. The stigma of psychiatric treatment and help-seeking intentions for depression. Eur Arch Psychiatry Clin Neurosci. (2009) 259:298–306.
9. Miller CL, Druss BG, Dombrowski EA, Rosenheck RA. Barriers to primary medical care among patients at a community mental health center. Psychiatr Serv. (2003) 54:1158–60. doi: 10.1176/appi.ps.54.8.1158
10. Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. (2006) 86:15–22. doi: 10.1016/j.schres.2006.06.026
11. Kisely S, Smith M, Lawrence D, Cox M, Campbell LA, Maaten S. Inequitable access for mentally ill patients to some medically necessary procedures. CMAJ. (2007) 176:779–84.
12. Lawrie SM, Martin K, McNeill G, Drife J, Chrystie P, Reid A, et al. General practitioners’ attitudes to psychiatric and medical illness. Psychol Med. (1998) 28:1463–7.
13. Chin SH, Balon R. Attitudes and perceptions toward depression and schizophrenia among residents in different medical specialties. Acad Psychiatry. (2006) 30:262–3.
14. Couture SM, Penn DL. Interpersonal contact and the stigma of mental illness: a review of the literature. J Ment Health. (2003) 12:291–305. doi: 10.1176/appi.ps.201100529
15. Björkman T, Angelman T, Jönsson M. Attitudes towards people with mental illness: a cross-sectional study among nursing staff in psychiatric and somatic care. Scand J Caring Sci. (2008) 22:170–7. doi: 10.1111/j.1471-6712.2007.00509.x
16. Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian mental health survey, 2011. Arch Iran Med. (2015) 18:76–84.
17. Rezayat F, Mohammadi E, Fallahi-khoshknab M. The process of responding to stigma in people with schizophrenia spectrum disorders and families: a grounded theory study. Perspect Psychiatr Care. (2020) 56:564–73. doi: 10.1111/ppc.12468
18. Rezayat F, Mohammadi E, Fallahi-khoshknab M, Sharifi V. Experience and the meaning of stigma in patients with schizophrenia spectrum disorders and their families: a qualitative study. Jpn J Nurs Sci. (2019) 16:62–70. doi: 10.1111/jjns.12212
19. Modgill G, Patten SB, Knaak S, Kassam A, Szeto ACH. Opening minds stigma scale for health care providers (OMS-HC): examination of psychometric properties and responsiveness. BMC Psychiatry. (2014) 14:120. doi: 10.1186/1471-244X-14-120
20. Vagheei S, Hashemi BM, Kashani Lotfabadi M, Salarhaji A, vagheei N, Feizi M. The relationship between empathy and stigma towards psychiatric disorders among nursing students. Future Med Educ J. (2018) 8:38–43. doi: 10.1016/j.nedt.2017.11.019
21. Rezvanifar F, Shariat SV, Amini H, Rasoulian M, Shalbafan M. A scoping review of questionnaires on stigma of mental illness in Persian. Iranian J Psychiatry Clin Psychol. (2020) 26:240–59.
22. Kassam A, Papish A, Modgill G, Patten S. The development and psychometric properties of a new scale to measure mental illness related stigma by health care providers: the opening minds scale for health care providers (OMS-HC). BMC Psychiatry. (2012) 12:62. doi: 10.1186/1471-244X-12-62
23. Destrebecq A, Ferrara P, Frattini L, Pittella F, Rossano G, Striano G, et al. The Italian version of the opening minds stigma scale for healthcare providers: validation and study on a sample of bachelor students. Commu Ment Health J. (2018) 54:66–72. doi: 10.1007/s10597-017-0149-0
24. Patten SB, Remillard A, Phillips L, Modgill G, Szeto AC, Kassam A, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ. (2012) 12:120.
25. Papish A, Kassam A, Modgill G, Vaz G, Zanussi L, Patten S. Reducing the stigma of mental illness in undergraduate medical education: a randomized controlled trial. BMC Med Educ. (2013) 13:141.
26. Mohammadzadeh M, Awang H, Mirzaei F. Mental health stigma among Middle Eastern adolescents: a protocol for a systematic review. J Psychiatr Ment Health Nurs. (2020) 27:829–37. doi: 10.1111/jpm.12627
27. Sewilam AM, Watson AMM, Kassem AM, Clifton S, McDonald MC, Lipski R, et al. Roadmap to reduce the stigma of mental illness in the Middle East. Int J Soc Psychiatry. (2015) 61:111.
28. Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. (2004) 28:240–2.
30. Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB. Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med. (2000) 15:381–8. doi: 10.1046/j.1525-1497.2000.12088.x
31. Mitake T, Iwasaki S, Deguchi Y, Nitta T, Nogi Y, Kadowaki A, et al. Relationship between burnout and mental-illness-related stigma among nonprofessional occupational mental health staff. BioMed Res Int. (2019) 2019:5921703. doi: 10.1155/2019/5921703
32. Seyedmoharrami I, Atif K, Tatari M, Abbaspour S, Zandi A, Teimori-Boghsani G, et al. Accomplices of job burnout among employees of a medical university. Russian Open Med J. (2019) 8:e0105.
33. Méndez Fernández AB, Lombardero Posada X, Aguiar Fernández FX, Murcia Álvarez E, González Fernández A. Professional. preference for mental illness: the role of contact, empathy, and stigma in Spanish social work undergraduates. Health Soc Care Commu. (2022) 30:1492–1503.
34. Ebrahimi H, Namdar H, Vahidi M. Mental illness stigma among nurses in psychiatric wards of teaching hospitals in the north-west of Iran. Iran J Nurs Midwifery Res. (2012) 17:534–8.
35. Rodríguez-Almagro J, Hernández-Martínez A, Rodríguez-Almagro D, Quiros-García JM, Solano-Ruiz MDC, Gómez-Salgado J. Level of stigma among Spanish nursing students toward mental illness and associated factors: a mixed-methods study. Int J Environ Res Public Health. (2019) 16:4870. doi: 10.3390/ijerph16234870
36. Foster K, Withers E, Blanco T, Lupson C, Steele M, Giandinoto J, et al. Undergraduate nursing students’ stigma and recovery attitudes during mental health clinical placement: a pre/post-test survey study. Int J Ment Health Nurs. (2019) 28:1068–80. doi: 10.1111/inm.12634
37. Saif FA, Shakhoori HA, Nooh S, Jahrami H. Association between attitudes of stigma toward mental illness and attitudes toward adopting evidence-based practice within health care providers in Bahrain. PLoS One. (2019) 14:e0225738. doi: 10.1371/journal.pone.0225738
Keywords: social stigma, community psychiatry, mental illness, medical students, medical education
Citation: Movahedi S, Shariat SV and Shalbafan M (2022) Attitude of Iranian medical specialty trainees toward providing health care services to patients with mental disorders. Front. Psychiatry 13:961538. doi: 10.3389/fpsyt.2022.961538
Received: 04 June 2022; Accepted: 01 July 2022;
Published: 28 July 2022.
Edited by:
Morteza Shamsizadeh, Hamadan University of Medical Sciences, IranReviewed by:
Fahimeh Afzaljavan, Mashhad University of Medical Sciences, IranCopyright © 2022 Movahedi, Shariat and Shalbafan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammadreza Shalbafan, Shalbafan.mr@iums.ac.ir
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.