- 1LVR-Institute for Healthcare Research, Cologne, Germany
- 2Medical Faculty, Heinrich Heine University Düsseldorf, Düsseldorf, Germany
- 3LVR Clinic Cologne, Cologne, Germany
Background: During the first phase of the Coronavirus-19 disorder (COVID-19) pandemic in the spring of 2020, utilization of inpatient mental healthcare was significantly reduced. We now report on a long-term observational study of inpatient mental healthcare in a large psychiatric hospital association in North Rhine-Westphalia, Germany, covering the second and third pandemic waves of autumn and winter 2020 followed up until June 2021.
Objectives: Analysis of the changes of inpatient and day patient mental healthcare utilization in an association of psychiatric hospitals during the COVID-19 pandemic from January 2020 until June 2021.
Materials and methods: We used the statistics database of the association of the nine psychiatric hospitals of the Rhineland Regional Council (Landschaftsverband Rheinland, LVR). We compared the case numbers of the pandemic period with previous years and analyzed changes in the diagnostic spectrum, rates of coercion and therapeutic outcomes. We also analyzed age, gender, diagnoses and coercive measures of patients tested positive for COVID-19 during inpatient psychiatric healthcare.
Results: Case rates were reduced during and after the COVID-19 pandemic episodes of 2020 and the following months of spring and summer 2021. Changes varied between diagnostic groups, and there were even increases of case numbers for acute psychotic disorders. Coercive measures increased during the pandemic, but therapeutic outcomes were maintained at the pre-pandemic level. Women and patients of higher ages were overrepresented among psychiatric inpatients with COVID-19.
Conclusion: The COVID-19 pandemic led to over during reductions of inpatient psychiatric hospital admissions and changes of the diagnostic spectrum accompanied by increased rates of coercive measures. These effects may reflect an overall increased severity of mental disorders during the COVID-19 pandemic, deferrals of inpatient admissions or a lack of outpatient mental healthcare services utilization. To differentiate and quantitate these potential factors, further studies in the general population and in the different mental healthcare sectors are needed. In order to reduce the number of COVID-19 cases in psychiatric hospitals, vaccination of people of higher ages and with dementias seem to be the most needed strategy.
Introduction
The coronavirus-19 (COVID-19) pandemic had an overall negative impact on the mental health of the general population (1, 2). Due to its medical and social consequences, the COVID pandemic has been traumatizing the general population for long time periods and increased the need of mental healthcare (3, 4). However, the individual mental health responses were heterogenous with a subgroup of approximately one third of the population showing increasing levels of anxiety and/or depression during the first year of the pandemic (5). Ahrens and coworkers (6) described marked interindividual differences in perceived stress between subgroups. In vulnerable groups, psychological state deteriorated over time, putting them at risk for mental disorder development. Consequently, health services should especially identify and allocate resources to vulnerable individuals (6).
Analyzing the time pattern of service utilization during a pandemic is of central importance to prepare services for future pandemics. For example, in a recent UK survey, Bu and coworkers (7) found that mostly friends and families were approached when people in lockdown faced mental health problems. Until now, there have been few reports about the utilization of inpatient mental healthcare during the pandemic. In an earlier study, we showed a reduction of overall inpatient psychiatric admission rates accompanied by a shift toward more acute cases during the initial pandemic phase of early 2020 in Germany (8). Some mental health services were reorganized to include telepsychiatry (9–11). An Italian study indicated an increased demand for urgent psychiatric consultations predominantly for vulnerable groups like people living in psychiatric facilities (12). Following the first pandemic wave in early 2020, two more waves developed in the course of 2020 and 2021. Emergency psychiatric admissions increased even after lockdown measures were curtailed, indicating over during effects of the pandemic and lockdown measures on mental healthcare services (13, 14). Therefore, we were interested in performing a follow-up study of psychiatric hospital admission rates spanning the subsequent pandemic phases in 2020 and 2021. Besides admission rates, we analyzed the long-term numbers and diagnoses of inpatients with mental disorders and COVID-19 comorbidity. These analyses should help to assess the impact of the COVID-19 pandemic on psychiatric inpatient utilization and to clinically characterize psychiatric inpatients with mental disorders who develop COVID-19 infections. Such analyses are expected to be helpful to prepare mental healthcare systems for future virus pandemics.
We studied admission rates and admission diagnoses of adult psychiatry departments of nine psychiatric hospitals of the hospital association of the Rhineland Regional Council [Landschaftsverband Rheinland (LVR)], which have approximately 2,835 beds and 750 day patient places. These hospitals provide mental healthcare services to approximately half of the population of the Rhineland (4.4 million inhabitants) and are representative of mental healthcare services in Germany as shown by their typical day mix indices (8).
Materials and methods
The observation period for this study was 1 January 2018 until 30 June 2021. This observation period covered the first minor phase of the COVID-19 pandemic in Germany in spring 2020, which was followed by a period of low COVID case numbers in summer 2020 and then by a two more pronounced waves of COVID 19 cases from fall 2020 until early spring 2021. Numbers of COVID-19 cases then again decreased in summer of 2021. We therefore compared the time period 1 January 2018 until 30 June 2019, with the time period 1 January 2020 until 30 June 2021.
Clinical routine data were obtained from the LVR statistics database. These data are documented for clinical routine purposes of quality insurance and remuneration. They included age and sex, diagnoses, length of stay, frequency of coercive measures (involuntary admission, restraint and seclusion) and COVID-19 test results. The clinical routine data of the nine psychiatric hospitals are transferred on a daily basis to an anonymized statistics database, which serves quality assurance purposes. We analyzed the anonymized aggregated data of the departments of general psychiatry, addiction medicine, geriatric psychiatry and psychosomatic medicine by means of time series analysis of the monthly inpatient and day patient admission rates, frequencies of diagnoses of mental disorders, gender and age of patients. We also studied the number, age and gender of inpatients with COVID-19 as identified by the corresponding ICD-10-codes in the statistics database. Additional analyses addressed measures of coercion as identified by the rates of involuntary hospitalizations under the auspices of the North Rhine-Westphalia Mental Health Act, and the case-based rates of coercive measures (seclusion and restraint). For statistical analyses, we calculated odds ratios to assess the risk of COVID-19 infection in different groups of patients. We used Chi-square tests to compare rates of categorical variables between groups and used Student’s t-test to compare the age distributions of people with and without COVID-19. Statistical analyses were performed using standard statistical software (SPSS 26, Konstanz Information Miner and GraphPad Version 9.3.1). We performed this retrospective epidemiological study following the principles of the Helsinki Declaration.
Results
Comparing the monthly inpatient and day patient admission rates for two 18-months observation periods, there was a decline of 12.5% in inpatients and 25.9% in outpatients (Figure 1). Numbers decreased already in March 2020, when the first COVID 19 pandemic wave occurred in Germany, and similarly so in summer 2020 coincidentally with the second wave. Admission rates never fully recovered to the pre-pandemic values throughout the observation period. The decline of case numbers affected nearly all diagnostic groups, but was different between diagnostic groups. Table 1 shows the changes for the 10 most frequent diagnoses of 2018/2019. The decline was most pronounced among those with affective and substance related disorders. Delirium superimposed on dementia (ICD-10 diagnostic group F05.1) increased slightly and a relatively large increase of 18% was observed for patients with acute polymorphic psychotic disorders (ICD-10 diagnostic group F23.1 from 539 to 636 cases).
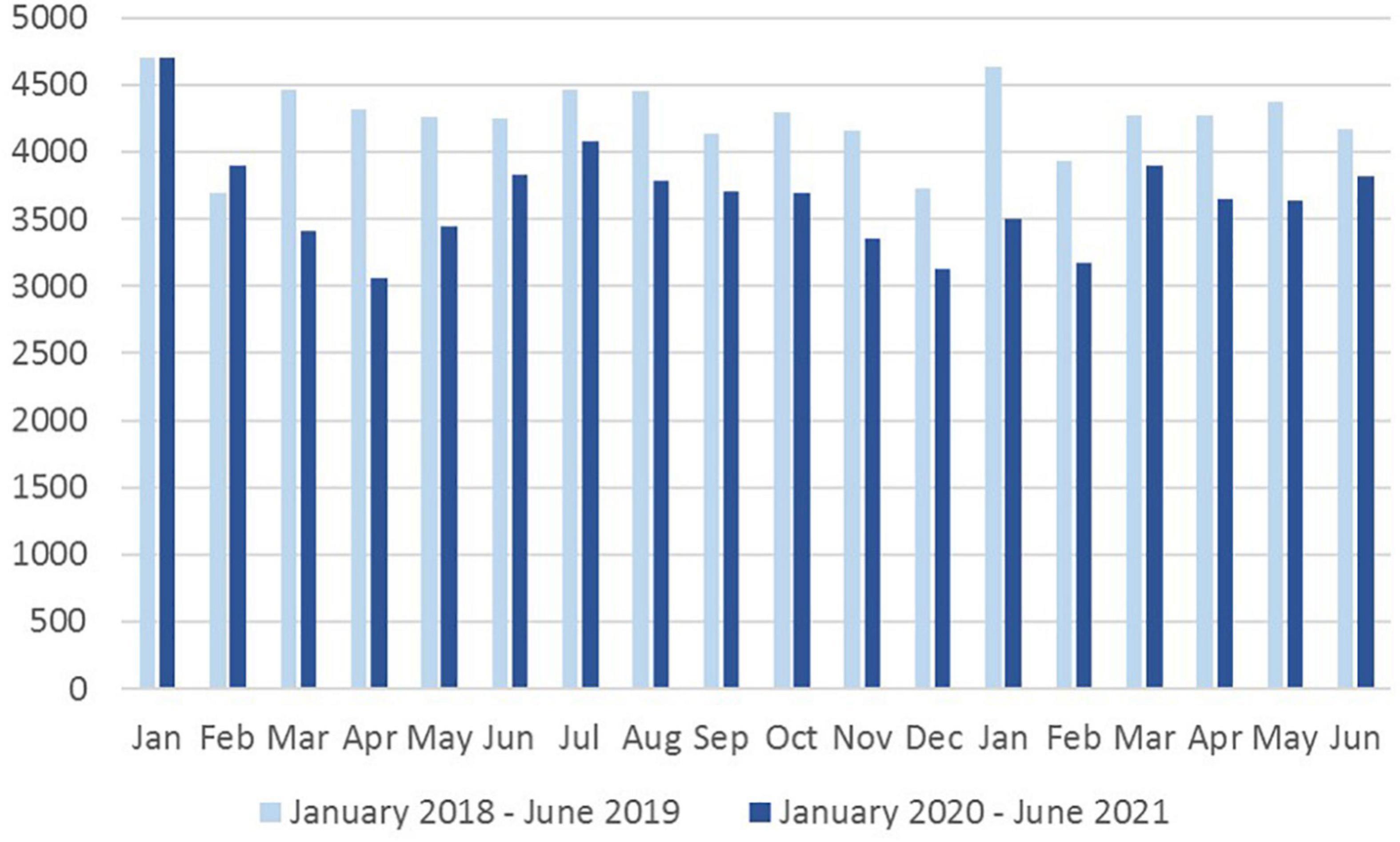
Figure 1. Monthly admission rates. Shown are the monthly admission rates in the adult psychiatric departments of nine psychiatric hospitals of the Rhineland region in Germany in the time periods 1 January 2018 until 30 June 2019 (light blue bars) and 1 January 2020 until 30 June 2021 (dark blue bars).
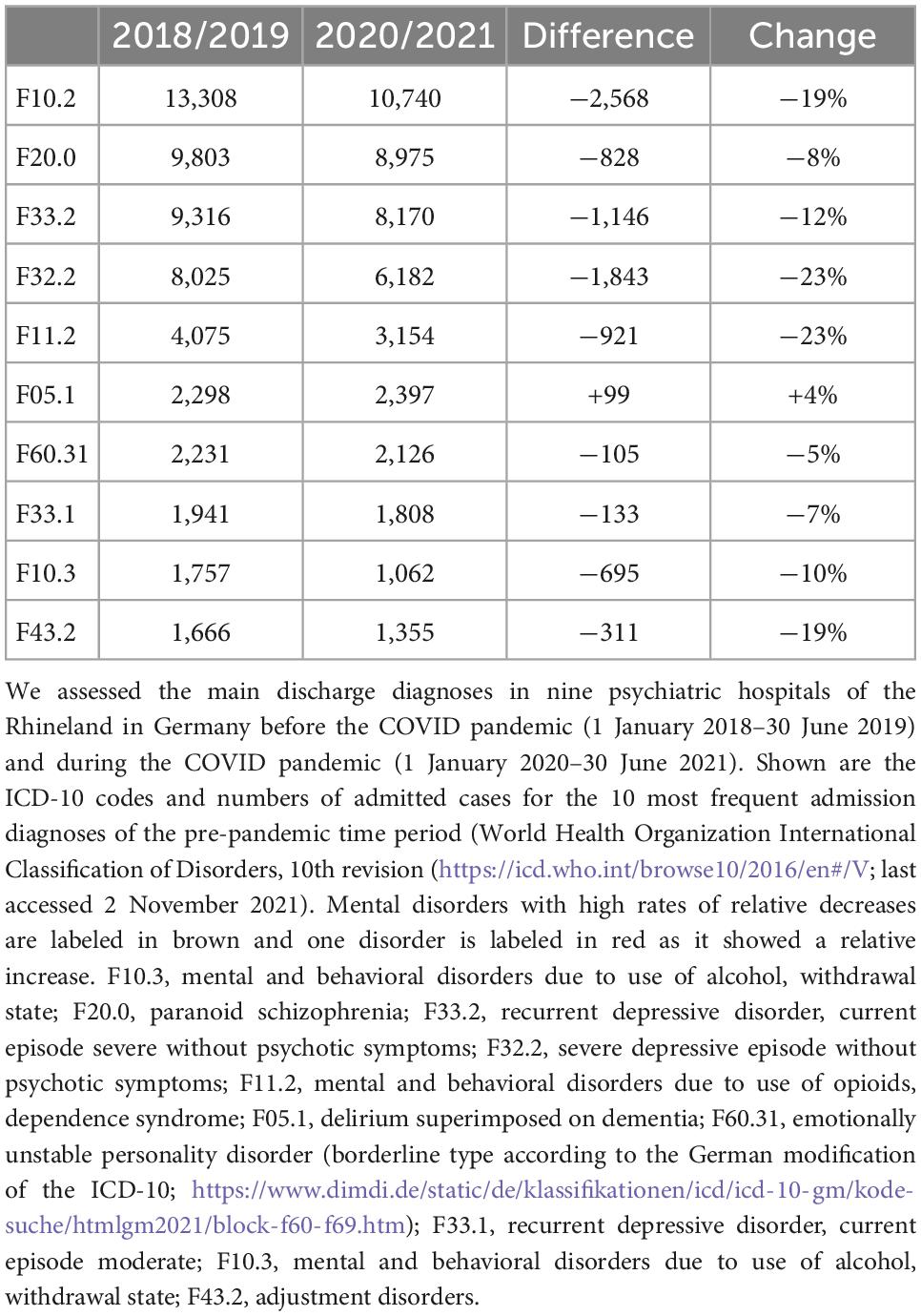
Table 1. Change in the frequency of the 10 most frequent admission diagnoses of the 2018/2019 period.
We observed increased rates of involuntary admission and involuntary inpatient treatment accompanied by increased rates of coercive measures (restraint and seclusion) in 2020 compared to 2019 (Table 2). Rates were significantly different between the two observation periods for all three variables (two-sided Chi-square-test for all three comparisons p < 0.0001 and df = 1; PsychKG Chi-square = 280.3; restraint Chi-square = 172.8; seclusion Chi-square = 21.93).
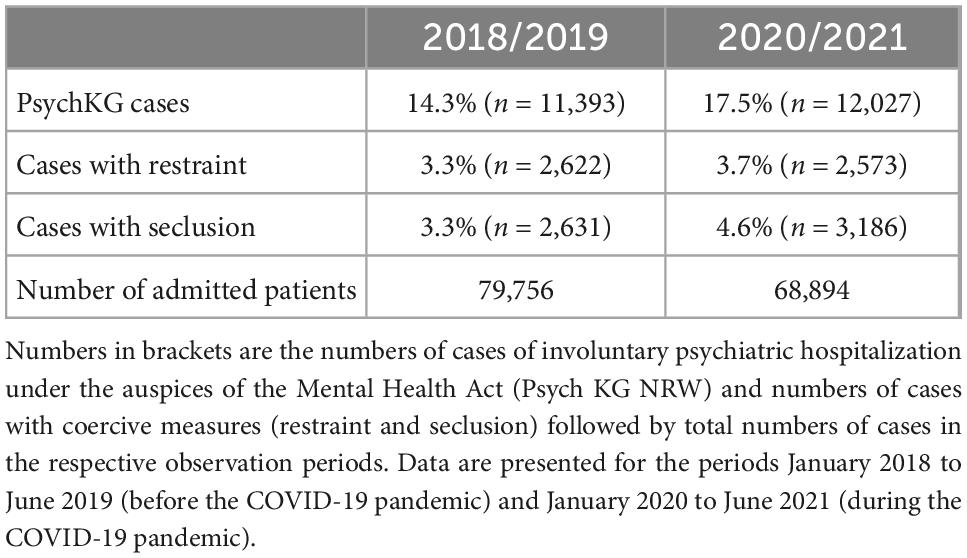
Table 2. Rates of involuntary psychiatric hospitalization under the auspices of the Mental Health Act (Psych KG NRW) and rates of coercive measures in the nine LVR psychiatric hospitals.
During the reporting period January 2020 until June 2021, 475 cases of COVID-19 were documented among inpatients of the nine psychiatric hospitals. These cases occurred mainly in the fall and winter months of 2020 and early in 2021 (Figure 2). All COVID-19 cases occurred in inpatients, no cases were observed in day patients. In total, 145 cases were identified between 0 and 4 days after inpatient admission, 97 cases were identified within 5–14 days after admission, and 233 cases were identified later during the course of psychiatric inpatient treatment. Allowing for an incubation period of several days, these figures indicate that the majority of COVID-19 infections (330/475 = 70%) occurred during the inpatient stay. Most psychiatric COVID-19 patients (n = 128) were diagnosed with an organic mental disorder including Alzheimer’s dementia (Figure 3). For affective disorders and disorders of the group of schizophrenias, we found similar rates of both infected and non-infected inpatient psychiatric cases. In the group of addiction disorders, COVID-19 cases were relatively underrepresented. The odds ratios for finding a COVID-19 patient in the diagnostic group of the organic mental disorders including the dementias was as high as 4.25 [95%CI 3.44; 5.24], while in the group of addiction disorders, it was only 0.37 [95% CI 0.28; 0.49].
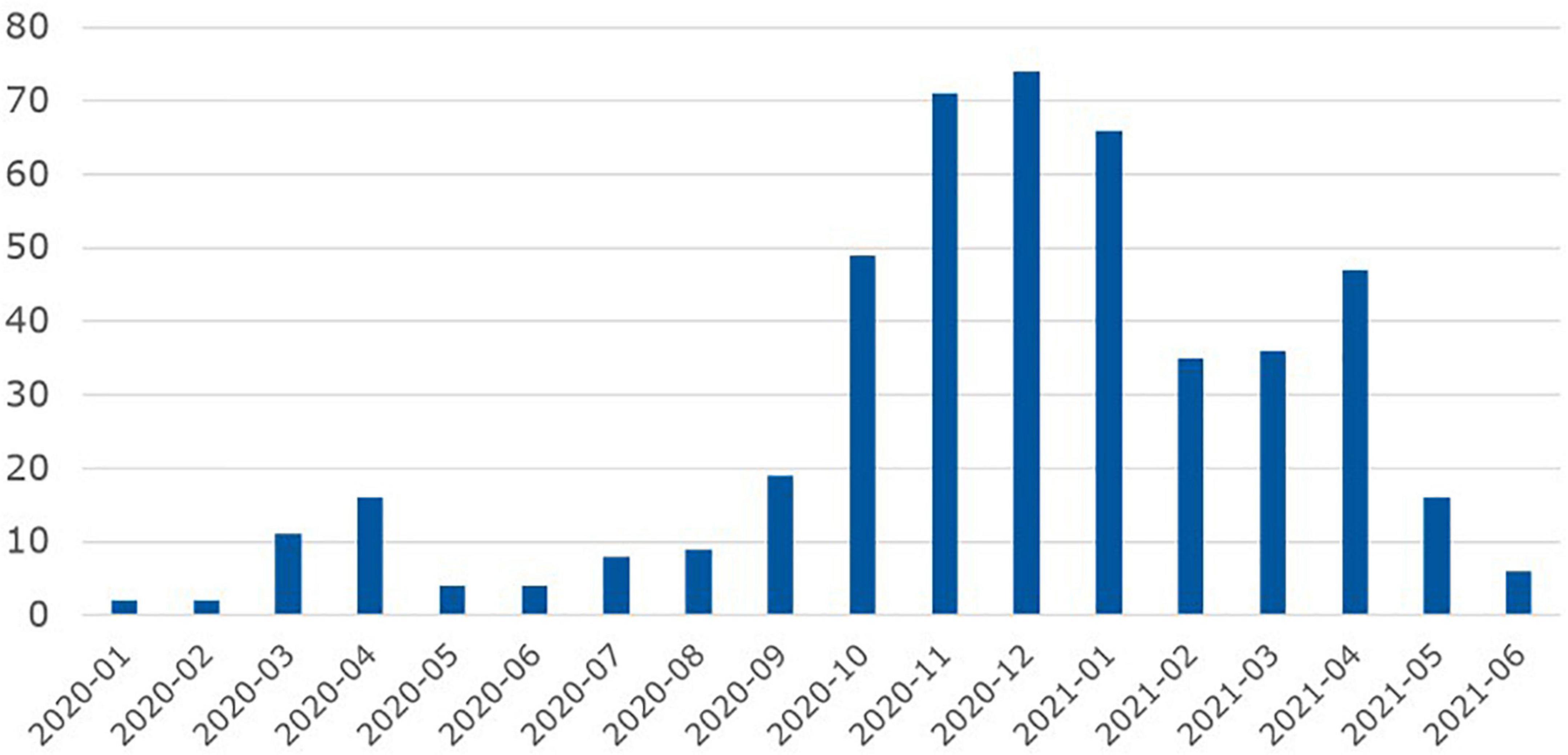
Figure 2. Monthly case numbers of COVID-19 among psychiatric inpatients of the nine psychiatric LVR-hospitals. Observation period: 1 January 2020 until 30 June 2021.
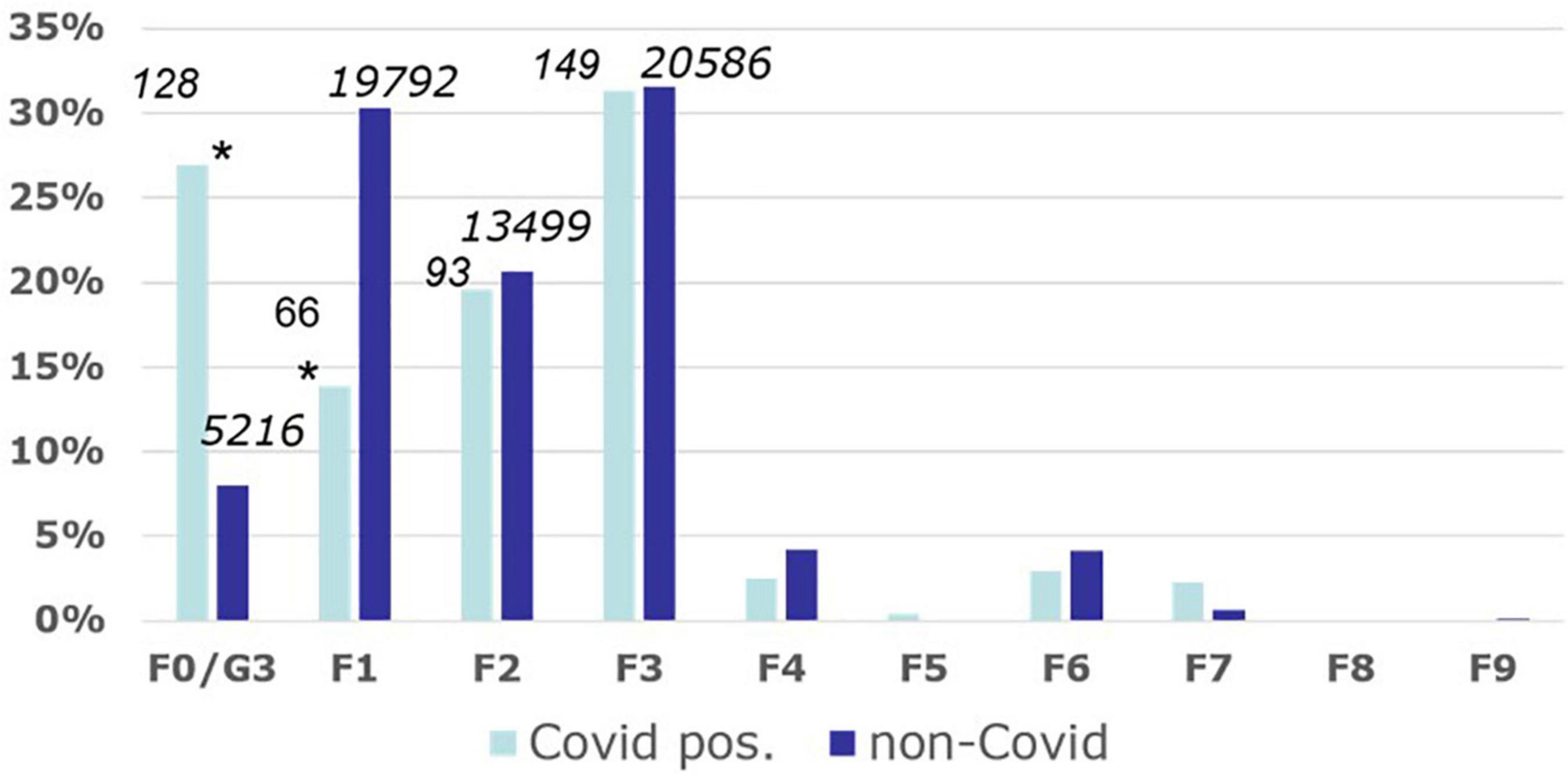
Figure 3. Spectrum of mental disorders of COVID-19-infected psychiatric inpatients. Frequency of COVID-19-cases in different diagnostic groups of psychiatric inpatients of the LVR psychiatric hospitals as differentiated by the World Health Organization International Classification of Disorders, 10th revision (https://icd.who.int/browse10/2016/en#/V; last accessed 2 November 2021). The figures above each bar indicate absolute case numbers during the observation period 1 January 2020 until 30 June 2021. Asterisks indicate that the group differences were significant in Chi square tests (p < 0.001). For example: The bars for the diagnostic group F0/G3 (organic mental disorders including dementias) indicate that 27% of all COVID-19-cases, but only 9% of the non-COVID-19-cases, were diagnosed with an F0/G3 disorder. F1, mental and behavioral disorders due to psychoactive substance use; F2, schizophrenia, schizotypal and delusional disorders; F3, mood (affective) disorders; F4, neurotic, stress-related and somatoform disorders; F5, behavioral syndromes associated with physiological disturbances and physical factors; F6, disorders of adult personality and behavior; F7, mental retardation; F8, disorders of psychological development; F9, behavioral and emotional disorders with onset usually occurring in childhood and adolescence.
Psychiatric inpatients with COVID-19-infections were significantly older (median 58 years, mean ± SD 57 ± 21 years) compared to non-COVID-19 patients (median 46 years, mean ± SD 47 ± 18 years; t-test double-sided p < 0.0001, T = 10.1507; df = 479.02). The relative risk of COVID-19 infection of psychiatric inpatients was significantly increased in women compared to men (relative risk for women 1.32 95% confidence interval 1.100–1.587; Chi-square test p < 0.00225; df = 1; Chi-Square 9.3374). We found significantly higher rates of involuntary admissions and coercive measures among psychiatric inpatient cases with COVID-19 as compared to non-COVID-19 patient cases (Figure 4).
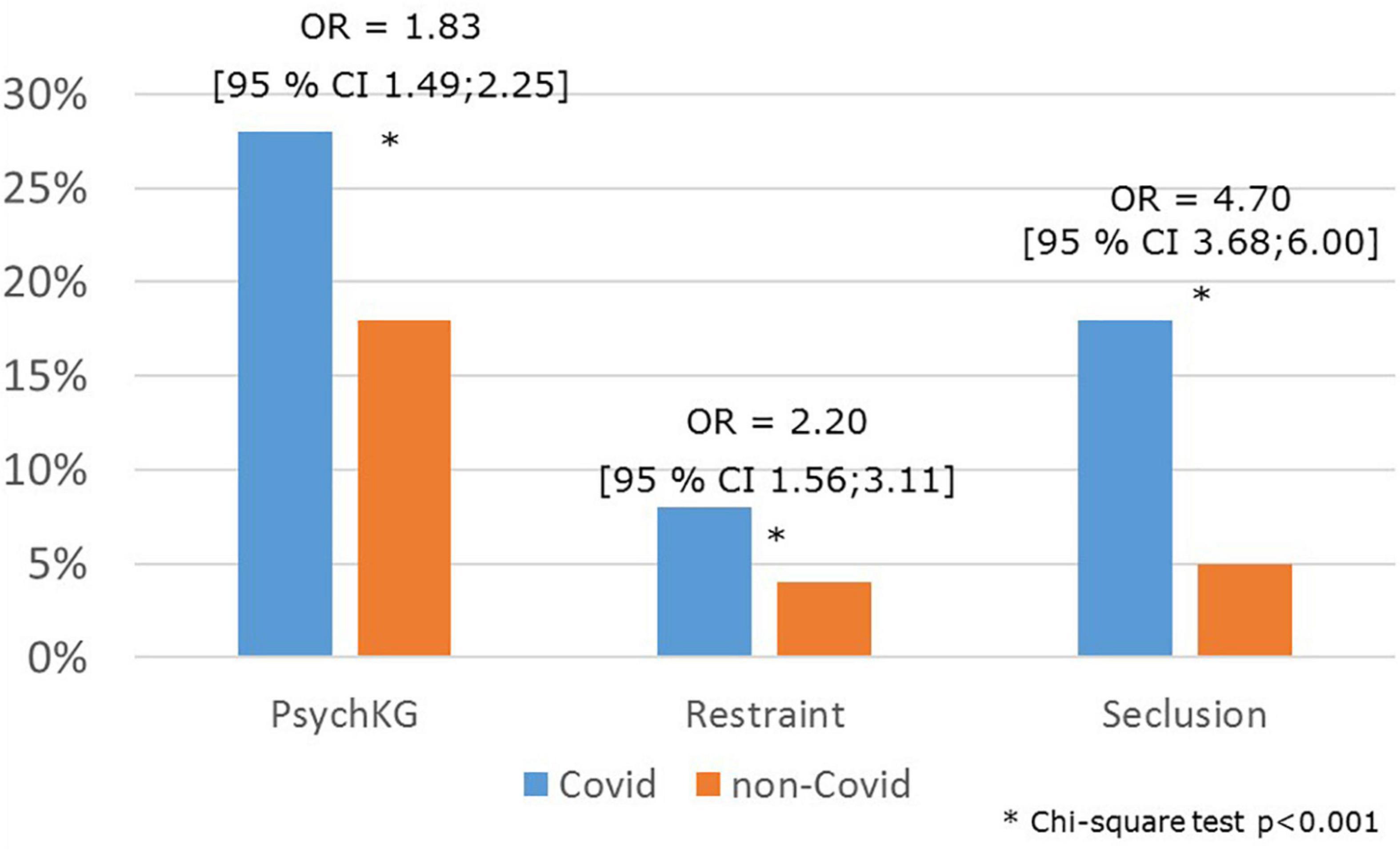
Figure 4. Rates of coercion among psychiatric inpatients with COVID-19. Given are the rates of cases of involuntary hospitalization [Psych KG, indicating the North-Rhine Westphalia Mental Health Act (Psychisch Kranke Gesetz NRW)], and rates of cases with seclusion and restraint in psychiatric inpatients with COVID-19 infections compared to patients without COVID-19 infection. Observation period: 1 January 2020 until 30 June 2021.
Discussion
In this follow up study, we confirm our findings obtained during the first wave of COVID-19 infections in Germany in spring 2020, in which we had shown a reduction of case numbers of psychiatric inpatients (8), which mostly in patients with affective and addiction disorders. We confirm the previously observed trend toward more acute cases, as indicated by diagnostic shifts toward more acute mental illnesses like Acute polymorphic psychotic disorder with symptoms of schizophrenia (ICD-10 F23.1) and increased rates of coercive measures. We further extend our initial findings by showing that these changes were over during beyond the second wave of COVID-19 in late 2020 and early 2021. In addition, we show that the admission rates did not recover during the periods of decreased COVID-19 cases in the summers of 2020 and 2021. This may be due to over during pandemic effects on outpatient consultation rates, which may have led to under assignment of patients to psychiatric inpatient care. Similar findings of an overall decrease of total numbers of unplanned psychiatric hospital admissions were reported from another large German hospital network in 2020 (15, 16). Of note, the diagnostic spectrum was somehow different in that Fasshauer et al. reported that the decrease of unplanned admissions was less pronounced for cases with substance use disorders. This may have been due to a focus on emergency admissions in the studies by Fasshauer et al. compared to all types of hospital admissions in our study.
In addition, we extend our previous findings by showing increased rates of involuntary admissions and coercive measures, which may be due to a relative increase of more severe psychiatric cases during the pandemic and/or the impact of the need to enforce hygiene measures in acute psychiatric wards. In line with our findings, Fasshauer et al. (16) also reported increased rates of involuntary psychiatric admissions and coercive measures in their sample from a large German wide hospital network. Flammer et al. (17), who used the case registry for coercive measures of the state of Baden-Wuerttemberg. Germany, reported similar trends. In contrast, one international study reported declining rates of seclusion and restraint in a Canadian psychiatric hospital during the COVID-19-pandemic (18). Further detailed studies focusing on patient characteristics associated with coercive measures are warranted to identify explanations for such divergent findings.
Especially older people with dementia are a particularly vulnerable group for contracting COVID-19 and the pandemic led to increased mental strains and depression also in caretakers, as was shown in a recent German questionnaire survey of caretakers (19). As in our previous study, there was an overrepresentation of women, people of higher ages and patients with organic mental disorders including dementias among the psychiatric inpatient cases with COVID-19. This finding is now on a firmer empirical basis given the longer observation period and the high number of cases in our present study.
The strengths of our analysis lie in the large numbers of observed cases, the long observation period covering several phases of the pandemic, the new analysis of psychiatric COVID-19 cases and the representativeness of the studied psychiatric hospitals for general psychiatry in Germany. Limitations are the use of routine data documented for clinical and remuneration purposes and the retrospective nature of the study.
Taken together, our study and results from other studies indicate that while psychiatric inpatient case numbers decreased, case severity and disease acuity increased in psychiatric outpatient emergency units (20, 21) and inpatient mental healthcare during the COVID-19 pandemic in Germany. Similar trends were reported from Denmark (9), France (22), Italy (23, 24), Portugal (25), Switzerland (13, 14), and the United Kingdom (26–29) suggesting that these trends are not specific to national mental healthcare services, but reflect more general effects of the pandemic on mental healthcare in Europe. This may have been due to a reduction of mild cases referred to psychiatric services during the pandemic or a reduced rate of use of outpatient services, but it may also indicate that referrals to psychiatric hospitals were deferred until a higher than usual case severity was reached, or that the COVID-19 pandemic led to an increased rate of acute and severe mental disorders in the general population.
An Italian study during the initial COVID-19 pandemic phase showed that the utilization of mental healthcare services increased and was modulated by individual psychosocial factors like the type of coping strategy, indicating that such factors need to be taken into account when preparing mental healthcare services for future pandemics (30). Further large scale follow-up studies in the general population are needed to address these issues. Hence, in response to the experiences during the COVID-19 pandemic the role of psychiatrists and psychiatry are changing with increased responsibilities for ascertaining adequate mental and somatic healthcare for vulnerable people with mental disorders (31, 32).
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The study was based on anonymized hospital records which cannot be transferred to others due to data protection regulations. Requests to access aggregated statistical analyses should be directed to JZ, ✉ anVlcmdlbi56aWVsYXNla0BsdnIuZGU=.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
JZ and EG-M designed the study. JZ and JV analyzed the data. All authors interpreted the results and wrote the manuscript.
Funding
This study was supported by institutional funds of the LVR Hospital Association.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vindegaard N, Benros M. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
2. Xiong J, Lipsitz O, Nasri F, Lui L, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
3. Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of CO-VID-19 response. World Psychiatry. (2020) 19:129–30. doi: 10.1002/wps.20768
4. Unützer J, Kimmel R, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. (2020) 19:130–1. doi: 10.1002/wps.20766
5. Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman T, et al. Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol Med. (2021): Epub ahead of print. doi: 10.1017/S0033291721001665
6. Ahrens K, Neumann R, Kollmann B, Brokelmann J, von Werthern N, Malyshau A, et al. Impact of COVID-19 lockdown on mental health in Germany: longitudinal observation of different mental health trajectories and protective factors. Transl Psychiatry. (2021) 11:392. doi: 10.1038/s41398-021-01508-2
7. Bu F, Mak H, Fancourt D. Rates and predictors of uptake of mental health support during the COVID-19 pandemic: an analysis of 26,720 adults in the UK in lockdown. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:2287–97. doi: 10.1007/s00127-021-02105-w
8. Zielasek J, Vrinssen J, Gouzoulis-Mayfrank E. Utilization of inpatient mental health care in the Rhineland during the COVID-19 pandemic. Front Public Health. (2021) 9:593307. doi: 10.3389/fpubh.2021.593307
9. Hansen J, van Sas T, Fløjstrup M, Brabrand M, Hvolby A. The effect of the march 2020 COVID-19 lockdown on national psychiatric contacts in Denmark: an interrupted time series analysis. Brain Behav. (2021) 11:e2264. doi: 10.1002/brb3.2264
10. Markowitz J, Milrod B, Heckman T, Bergman M, Amsalem D, Zalman H, et al. Psychotherapy at a distance. Am J Psychiatry. (2021) 178:240–6. doi: 10.1176/appi.ajp.2020.20050557
11. Schaub A, Michel C, Beck P, Falkai P. [Inpatient psychiatric treatment in the corona-crisis by psychologists and psychiatrists in home-office and in the clinic]. Fortschr Neurol Psychiatr. (2021) 89:424–32. doi: 10.1055/a-1483-9904
12. Di Lorenzo R, Pinelli M, Bertani D, Cutino A, Dragone D, Elia C, et al. The impact of COVID-19 pandemic on psychiatric emergencies in two different settings: emergency room and community mental health service. Front Psychiatry. (2022) 13:894939. doi: 10.3389/fpsyt.2022.894939
13. Ambrosetti J, Macheret L, Folliet A, Wullschleger A, Amerio A, Aguglia A, et al. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatry. (2021) 21:465. doi: 10.1186/s12888-021-03469-8
14. Ambrosetti J, Macheret L, Folliet A, Wullschleger A, Amerio A, Aguglia A, et al. Impact of the COVID-19 pandemic on psychiatric admissions to a large Swiss emergency department: an observational study. Int J Environ Res Public Health. (2021) 18:1174. doi: 10.3390/ijerph18031174
15. Fasshauer J, Bollmann A, Hohenstein S, Hindricks G, Meier-Hellmann A, Kuhlen R, et al. Emergency hospital admissions for psychiatric disorders in a German-wide hospital network during the COVID-19 outbreak. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1469–75. doi: 10.1007/s00127-021-02091-z
16. Fasshauer J, Bollmann A, Hohenstein S, Mouratis K, Hindricks G, Meier-Hellmann A, et al. Impact of COVID-19 pandemic on involuntary and urgent inpatient admissions for psychiatric disorders in a German-wide hospital network. J Psychiatr Res. (2021) 142:140–3. doi: 10.1016/j.jpsychires.2021.07.052
17. Flammer E, Eisele F, Hirsch S, Steinert T. Increase in coercive measures in psychiatric hospitals in Germany during the COVID-19 pandemic. medRxiv. (2022) [Preprint]. doi: 10.1101/2022.02.03.22270373
18. Martin K, Arbour S, McGregor C, Rice M. Silver linings: observed reductions in aggression and use of restraints and seclusion in psychiatric inpatient care during COVID-19. J Psychiatr Mental Health Nurs. (2021): Epub ahead of print. doi: 10.1111/jpm.12752
19. Dominke C, Wie G, Piguet O, Kumfor F, Diehl-Schmid J. Auswirkungen der COVID-19-pandemie auf neuropsychiatrische symptome von menschen mit demenz und die psychische gesundheit ihrer pflegenden angehörigen. Eine online-studie. Impact of the COVID-19 pandemic on neuropsychiatric symptoms of patients with dementia and the mental health of their caregivers. An online survey. Nervenheilkunde. (2021) 40:861–9. doi: 10.1055/a-1548-4602
20. Aly L, Sondergeld R, Hölzle P, Frank A, Knier B, Pausch E, et al. Die COVID-19-pandemie veränderte nicht die zahl, aber die art psychiatrischer notfälle: versorgungsdaten aus vergleichszeiträumen von 2019 und 2020 [The COVID-19 pandemic has not changed the number but the type of psychiatric emergencies: a comparison of care data between 2019 and 2020]. Nervenarzt. (2020) 91:1047–9. doi: 10.1007/s00115-020-00973-2
21. Hoyer C, Ebert A, Szabo K, Platten M, Meyer-Lindenberg A, Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2021) 271:377–9. doi: 10.1007/s00406-020-01151-w
22. Pignon B, Gourevitch R, Tebeka S, Dubertret C, Cardot H, Dauriac-Le Masson V, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin Neurosci. (2020) 74:557–9. doi: 10.1111/pcn.13104
23. Beghi M, Brandolini R, Casolaro I, Beghi E, Cornaggia C, Fraticelli C, et al. Effects of lockdown on emergency room admissions for psychiatric evaluation: an observational study from the AUSL Romagna, Italy. Int J Psychiatry Clin Pract. (2020) 2:1–5. doi: 10.1080/13651501.2020.1859120
24. Boldrini T, Girardi P, Clerici M, Conca A, Creati C, Di Cicilia G, et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 110:110304. doi: 10.1016/j.pnpbp.2021.110304
25. Gonçalves-Pinho M, Mota P, Ribeiro J, Macedo S, Freitas A. The impact of COVID-19 pandemic on psychiatric emergency department visits—A descriptive study. Psychiatr Q. (2020): Epub ahead of print. doi: 10.1007/s11126-020-09837-z
26. Abbas M, Kronenberg G, McBride M, Chari D, Alam F, Mukaetova-Ladinska E, et al. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatr Serv. (2021) 72:242–6. doi: 10.1176/appi.ps.202000467
27. Chen S, Jones P, Underwood B, Moore A, Bullmore E, Banerjee S, et al. The early impact of COVID-19 on mental health and community physical health services and their patients’ mortality in Cambridgeshire and Peterborough, UK. J Psychiatr Res. (2020) 131:244–54. doi: 10.1016/j.jpsychires.2020.09.020
28. Chen S, She R, Qin P, Kershenbaum A, Fernandez-Egea E, Nelder J, et al. The medium-term impact of COVID-19 lockdown on referrals to secondary care mental health services: a controlled interrupted time series study. Front Psychiatry. (2020) 11:585915. doi: 10.3389/fpsyt.2020.585915
29. Tromans S, Chester V, Harrison H, Pankhania P, Booth H, Chakraborty N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych Open. (2020) 6:e117. doi: 10.1192/bjo.2020.104
30. Menculini G, Tortorella A, Albert U, Carmassi C, Carrà G, Cirulli F, et al. Access to mental health care during the first wave of the COVID-19 pandemic in Italy: results from the comet multicentric study. Brain Sci. (2021) 11:1413. doi: 10.3390/brainsci11111413
31. Stewart D, Appelbaum P. COVID-19 and psychiatrists’ responsibilities: a WPA position paper. World Psychiatry. (2020) 19:406–7. doi: 10.1002/wps.20803
Keywords: COVID-19, pandemic, psychiatric services utilization, mental healthcare, inpatient
Citation: Zielasek J, Lehmann I, Vrinssen J and Gouzoulis-Mayfrank E (2022) Analysis of the utilization, processes, and outcomes of inpatient mental healthcare during the first three waves of the COVID-19 pandemic in the federal state of North Rhine-Westphalia, Germany. Front. Psychiatry 13:957951. doi: 10.3389/fpsyt.2022.957951
Received: 31 May 2022; Accepted: 30 November 2022;
Published: 22 December 2022.
Edited by:
Elke Van Hoof, Vrije University Brussels, BelgiumReviewed by:
Gaia Sampogna, University of Campania “L. Vanvitelli”, ItalyChristiane Montag, Charité – Universitätsmedizin Berlin, Germany
Copyright © 2022 Zielasek, Lehmann, Vrinssen and Gouzoulis-Mayfrank. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jürgen Zielasek, ✉ anVlcmdlbi56aWVsYXNla0BsdnIuZGU=
 Jürgen Zielasek
Jürgen Zielasek Isabell Lehmann1
Isabell Lehmann1 Jürgen Vrinssen
Jürgen Vrinssen Euphrosyne Gouzoulis-Mayfrank
Euphrosyne Gouzoulis-Mayfrank