- 1Research Division, Institute of Mental Health, Singapore, Singapore
- 2Early Psychosis Intervention Programme, Department of Psychosis, Institute of Mental Health, Singapore, Singapore
- 3Saw Swee Hock School of Public Health, National University of Singapore, Singapore, Singapore
Background: Needs define the capacity of a patient to benefit from health care services and a systematic assessment of needs allows planning and delivery of effective treatment to suit patients. This study aimed to understand the (a) needs felt by patients and those perceived by the care providers (CPs), (b) agreement between patients and CPs in the identified needs and (c) factors associated with unmet needs.
Methods: Participants (N = 215) were recruited through convenience sampling from the Early Psychosis Intervention Programme (EPIP). Data was captured from patients and CPs using the Camberwell Assessment of Needs Short Appraisal Schedule (CANSAS).
Results: Patients and CPs identified an average of 4.06 and 3.84 needs, respectively. The highest number of unmet needs were identified for the social (50% of patients and CPs) and health domains (31.13% of patients’ vs. 28.30% of CPs). Company, intimate relationships, psychotic symptoms, money, sexual expression and psychological distress, information and benefits were the unmet needs identified by patients, whereas company, intimate relationships, physical health, and daytime activities were identified by CPs. The concordance between patients and CPs was low with majority of the items scoring slight to fair agreement (Cohen’s kappa = 0–0.4). Older age, depression, severe anxiety and having Obsessive-Compulsive Disorder (OCD) were positively associated with unmet needs in patients.
Conclusion: While there was an overall consensus on the total needs and met needs between patients and CPs, the level of agreement between the two groups on various items were low. Different perceptions regarding unmet needs were noted between the groups. A holistic approach that takes into account different facets of the needs of patients together with strategic planning to address unmet needs might improve treatment outcomes and satisfaction.
Introduction
Schizophrenia and other psychotic disorders are among the top 25 causes of disability worldwide with sufferers recording 13.4 million years of life lived with disability (1, 2). Despite the relatively low prevalence (0.28% in 2016; 1), the disease has tremendous health, social and economic impact. Patients have a higher risk of premature mortality compared to the general population with the gap widening over the years (3). Schizophrenia is also associated with other psychiatric comorbidities, poorer social functioning, and unemployment (4).
Needs are means by which an individual can attain physical, mental, and social wellbeing (5). Maslow described needs through a 5-tier hierarchical pyramidal model where he classified needs as deficiency needs (physiological needs (food, home, sleep, and clothing), need for safety, love and belonging (friendship), and esteem), and growth needs (self-actualization). The model proposed that when a person fulfills his basic needs (deficiency needs), the focus turns toward achieving the higher-level growth needs where they find their meaning in life and life satisfaction (6). In healthcare, needs are described as the capacity of an individual to benefit from the services they receive (7). They get maximum benefit when their needs are met during the treatment process. Healthcare organizations have a key role in this process as they can address and resolve unmet needs and facilitate a smooth reintegration of patients back to their premorbid lives. However, to achieve this aim, organizations need to know what the needs of patients are. This information should be gathered through a systematic needs assessment process that will help identify non-recipients of service, and recipients of ineffective or inappropriate care (7). Such an assessment will allow effective utilization of resources and delivery of patient centric care.
Assessing the needs of patients with chronic mental illnesses is complicated as it varies based on many illness-related factors viz. type of disease, duration, severity, as well as individual psychosocial factors. Patients with schizophrenia have a higher burden of psychiatric comorbidities that are associated with unmet needs and adverse treatment outcomes (8). Depression, anxiety and Obsessive-Compulsive Disorder (OCD) are common psychiatric comorbidities in this group (8). The prevalence of depression varies from 30 to 80% in those with schizophrenia (9). Nearly 38% of patients suffer from anxiety disorder (10) and 12.3% from OCD (11). Given that patients with schizophrenia have diverse needs contributed by the disease characteristics and comorbidities, utmost attention should be paid to various growth and deficiency needs domains to ensure that they get maximum benefit from health care services.
Uygur and Danaci (12) studied the needs of patients with schizophrenia and found that among various health and social needs, those related to psychotic symptoms were unmet in the group. Housework, daily activities, psychological distress, and relationships were also identified as needs. Several studies (13–16) have shown that the needs felt by patients and those perceived by care providers (CPs) often differ. Slade et al. (13) noted that agreement for service satisfaction, as well as help given and received were low between CPs and patients. This has significant implications including treatment non-adherence due to patients’ dissatisfaction with services that fail to address their needs. Joska and Flisher (17) confirmed this by showing that higher fulfilled (met) needs and treatment satisfaction were correlated with better treatment adherence.
Healthcare providers often perceive the needs of their patients based on their clinical expertise and prior training received which may not be reflective of the actual needs of the population. This often leads to a top-down approach in the delivery of care where the patient’s perspective and needs are unintentionally ignored, leading to disengagement from services and unfavorable treatment outcomes (18). Clinicians and policy makers are increasingly acknowledging the treatment gap and social disparities in those with serious mental illnesses and reaching a consensus that a patient centric approach focusing on meeting the needs of patients should be prioritized to achieve better treatment adherence and outcomes (19).
Moreover, there were discrepancies in the social and health needs identified in various studies conducted among those with schizophrenia across the globe. Physical health and money were identified as unmet needs in a Swedish sample of 32 patients (15) while information on conditions/treatment and benefits were identified in a study conducted in Israel [n = 52; (19)]. Ochoa et al. (16) investigated a Spanish sample of patients with schizophrenia (n = 231) and showed that the unmet needs were mostly related to domains involving psychotic symptoms, company, daytime activities, house upkeep, food, and information. McCrone et al. (20) evaluated the unmet needs in patients with schizophrenia across different countries and showed that unmet needs vary across different countries. The authors reported that unmet needs were high in urban settings which is probably related to the nature of the care delivered and cultural differences. Besides, sociodemographic characteristics influence the perception of unmet needs for mental health care. A study conducted in 2,564 individuals with mental illness showed that unmet needs and contributing factors varied among different sociodemographic groups (21). Women, those with university education and individuals with “white” ethnicity had higher odds of cost related unmet needs while “blacks” tend to report lack of time, information, and transportation (21). The study also identified age as a major determinant of unmet needs. Yang et al. (22) confirmed this observation by showing that age, gender, ethnicity, and education has a role in reporting unmet needs. This calls for more studies in different cultural and geographical contexts to understand the variations in needs among patients with schizophrenia to effectively deliver patient centric care and improve treatment outcomes.
In Singapore, the prevalence of schizophrenia spectrum and other psychotic disorders was 2.3% in the adult population, with an early age of onset (23.1 years) and low treatment gap [80.4% sought treatment, (23)]. The Early Psychosis Intervention Programme (EPIP), a multidisciplinary nationwide program aims to diagnose and manage psychosis at an early stage to improve treatment outcomes and long-term prognosis (24). A program evaluation of EPIP conducted 2 years post implementation showed that 71.1% of patients achieved remission, and 76.5% of patients were employed/admitted to educational programs (25). Improving treatment outcomes and quality of life of patients is a core focus of the program (24) and thus a systematic needs assessment complements the program’s aims. To the best of our knowledge, no studies have been conducted in an Asian early psychosis population to understand the different facets of patient needs. Such a study could be informative in improving patients’ care experience.
This study aimed to understand the (a) needs felt by patients and those perceived by CPs, (b) agreement between patients and CPs in the identified needs, and (c) factors associated with unmet needs.
Materials and methods
Participants and setting
The study recruited patients from the outpatient clinics of EPIP. Eligible patients were aged 18–40 years, had a diagnosis of schizophrenia spectrum and other psychotic disorder, had sufficient mental capacity to participate in the study as assessed by the clinician or trained study team member, and were able to read and converse in English. The language of the survey was restricted to English as the majority of EPIP patients are young adults or adolescents who can speak English. The patients were asked to nominate three CPs who according to them knew their care needs well. The CPs were approached in the order of preference, as indicated by the patient. Patients who were in the acute phase (within 3 months from the first visit to EPIP), with a diagnosis other than schizophrenia spectrum and other psychotic disorder, unable to provide consent [and parental consent for minors (below 21 years)] were excluded. Those in the acute phase (3 months of their first visit to EPIP) were excluded as they are clinically unstable which affects their capacity to provide informed consent and answer the questions in a thoughtful manner.
Patients were recruited through referrals by their attending care teams. A trained team member explained the study and took written informed consent from the patient (and parent, for minors), before administering the survey either face to face or through videoconferencing. All, except the need assessment questionnaire were self-administered. The study followed procedures approved by the Institutional Research Review Committee and Domain Specific Review Board (DSRB Ref: 2020/01112).
Sample size
The sample size was estimated based on the results from Uygur and Danaci (12). To estimate the needs of patients with schizophrenia spectrum and other psychotic disorders using similar instruments with a desired width of the confidence interval or precision set at 1 and confidence level set at 95%, a sample size from 53 to 87 was required. After considering a withdrawal rate of approximately 20%, the study required a total sample size of 104 patients and their CPs. The patients and the CPs were recruited in 1:1 dyad and thus, the desirable total sample size of 208 was estimated.
Measures
Sociodemographic information
Age, gender, ethnicity, marital status, income, and employment status were captured through a structured questionnaire.
Clinical variables
Number of hospital admissions (“In the past 12 months have you been admitted to the hospital for mental health issues”?) and psychiatric medications over the past 12 months (Yes/No) were captured through self-report while Positive and Negative Syndrome Scale (PANSS), treatment adherence [medication adherence: assessed by the CP as non-adherent (0–49%; partial adherence: 50–74%; adherent: 75–100%)], duration of untreated psychosis (onset of symptoms to first visit to EPIP, dichotomized as more than 1 year or less than 1 year), and treatment duration which was calculated based on the duration from first visit to the date of interview (dichotomized as less than 1 year or more than 1 year), were captured from the EPIP clinical database.
Needs assessments
Camberwell Assessment of Need Short Appraisal Version (CANSAS) assessed needs in 5 domains corresponding to 22 different areas/subdomains including (a) basic needs (accommodation, food, daytime activities) (b) health [physical health (needs help with physical health conditions), psychotic symptoms (needs care to alleviate psychotic symptoms), psychological distress (feeling sad, anxious or frightened), safety to self and others, alcohol, (abuse of) drugs), (c) functioning (self-care, looking after the home, child care, education, and money) (d) social (company (social life), intimate relationships (relationship with partner), and sexual expression (sexual practices and contraception)] (e) services [information on the conditions and its treatment, transportation, telephone, and benefits (other entitlements)]. The responses were captured on a 4-point scale (“no need,” “met need,” “unmet need” and “unknown need”). The ratings were captured by trained study team members as per the guidelines (26). The scale had been previously validated in mental health populations (16, 27).
Depression
Depressive symptoms were assessed using Patient Health Questionnaire-9 (PHQ-9), a validated 9-item scale scored on a 4-point scale [Not at all (0), several days (1), more than half the days (2), nearly every day (3)]. A score of 0–4 indicates no/minimal depression, 5–9 is mild, 10–14 is moderate, 15–19 is moderately severe and 20–27 indicates severe depression (28). Due to the small frequencies within the categories, regrouping was done as follows for the regression analysis: none to minimal, mild, moderate, and moderately severe to severe.
Anxiety
Generalized Anxiety Disorder (GAD-7) scale is a validated tool to assess Generalized anxiety disorder in clinical practice and research. The 7- items scale captures the responses on a 4-point scale (“not at all,” “several days,” “more than half the days,” and “nearly every day”). The total score ranges from 0 to 21. A score of 5 represents a mild level of anxiety and 10 and 15 represents moderate, and severe levels, respectively (29). The categories were regrouped as minimal, mild-moderate, and severe for the regression analysis due to the small sample within the categories.
Obsessive-compulsive disorder
Obsessive-Compulsive Inventory-Revised (OCI-R) was used to capture OCD. It is an 18 items tool where responses are captured on a 5-point scale (“not at all,” “a little,” “moderately,” “a lot,” “extremely”) to evaluate 6 groups of OCD symptoms (washing, checking, ordering, obsessing, hoarding, and neutralizing). The total score ranges from 0 to 72. A cut-off score of 21 identifies 66% of OCD cases while a cut-off score of 5 identifies 99.5% cases. The scale has been validated in several studies (30, 31).
Analysis
A descriptive analysis was performed on categorical variables such as sociodemographic information which is expressed as frequency and percentages. The CANSAS scores between the groups (patient vs. CP) were compared using paired t-test. The agreement between CP and patients were assessed using Cohen’s Kappa coefficients. Kappa values above 0.80 were considered strong agreement while 0.61–0.80 indicates substantial agreement, 0.41–0.60 indicate moderate agreement, 0.21 to 0.40 indicates fair agreement and below 0.20 indicate slight agreement (32). Differences in the ratings of unmet needs between patients and CPs were calculated using paired sample t-test. Factors associated with unmet needs in patients were calculated using linear regression using unmet needs as outcome variable and sociodemographic and clinical variables as independent variables. A univariate analysis was initially performed and the variables that showed significant differences were included in the linear regression. All the analyses were done using IBM SPSS statistics version 25 (IBM SPSS statistics for Windows, Version 23.0, Armonk, NY: IBM Corp.).
Results
Sociodemographic characteristics of the participants
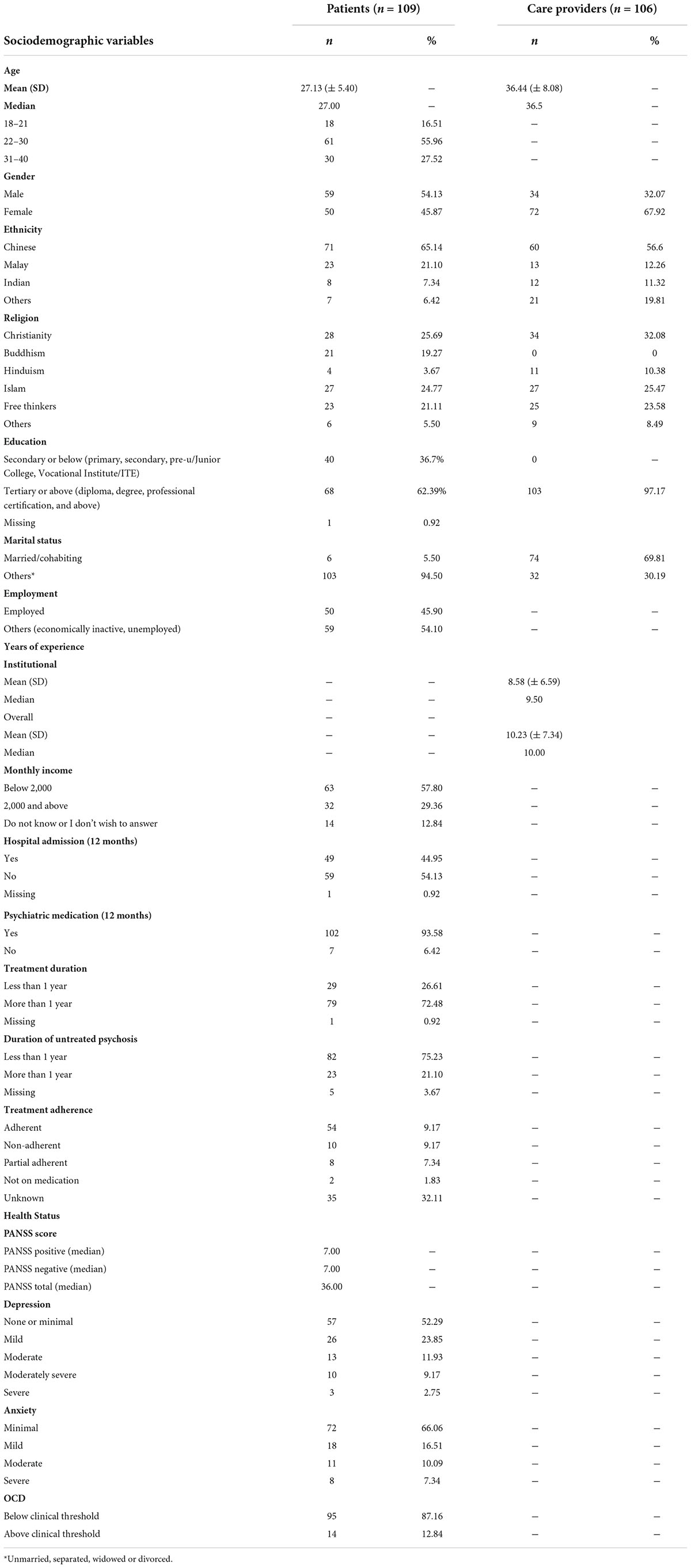
Table 1 shows the sociodemographic characteristics of the participants. A total of 109 patients and 106 CPs were recruited leading to 106 pairwise comparison of needs. The mean age of patients and CPs were 27.13 (±5.4) and 36.44 (±8.08) years, respectively. Around 65% of patients were Chinese, 62.39% had an education status of tertiary or above and 45.9% were employed, whilst 67.92% of CPs were females and had 9.5 years (median) of work experience in the current setting. Around 54% of patients were not admitted to the hospital in the past year and 93.58% were on medications (past 12 months). Around 72.48% were attending treatment for more than a year and 75.23% reported a duration of less than a year of untreated psychosis. Around 49.54% were adherent to treatment, 47.7% had depression (mild to severe), 33.9% had anxiety (mild to severe), and 12.8% met the clinical threshold of OCD.
Needs identified by patients and care providers
The average number of total needs identified were 4.06 and 3.84 for patients and CPs, respectively. Overall patients rated 0.3 more needs (out of 22) than CPs. The average unmet needs identified were 1.26 and 1.02 by patients and CPs, respectively (p ≥ 0.05).
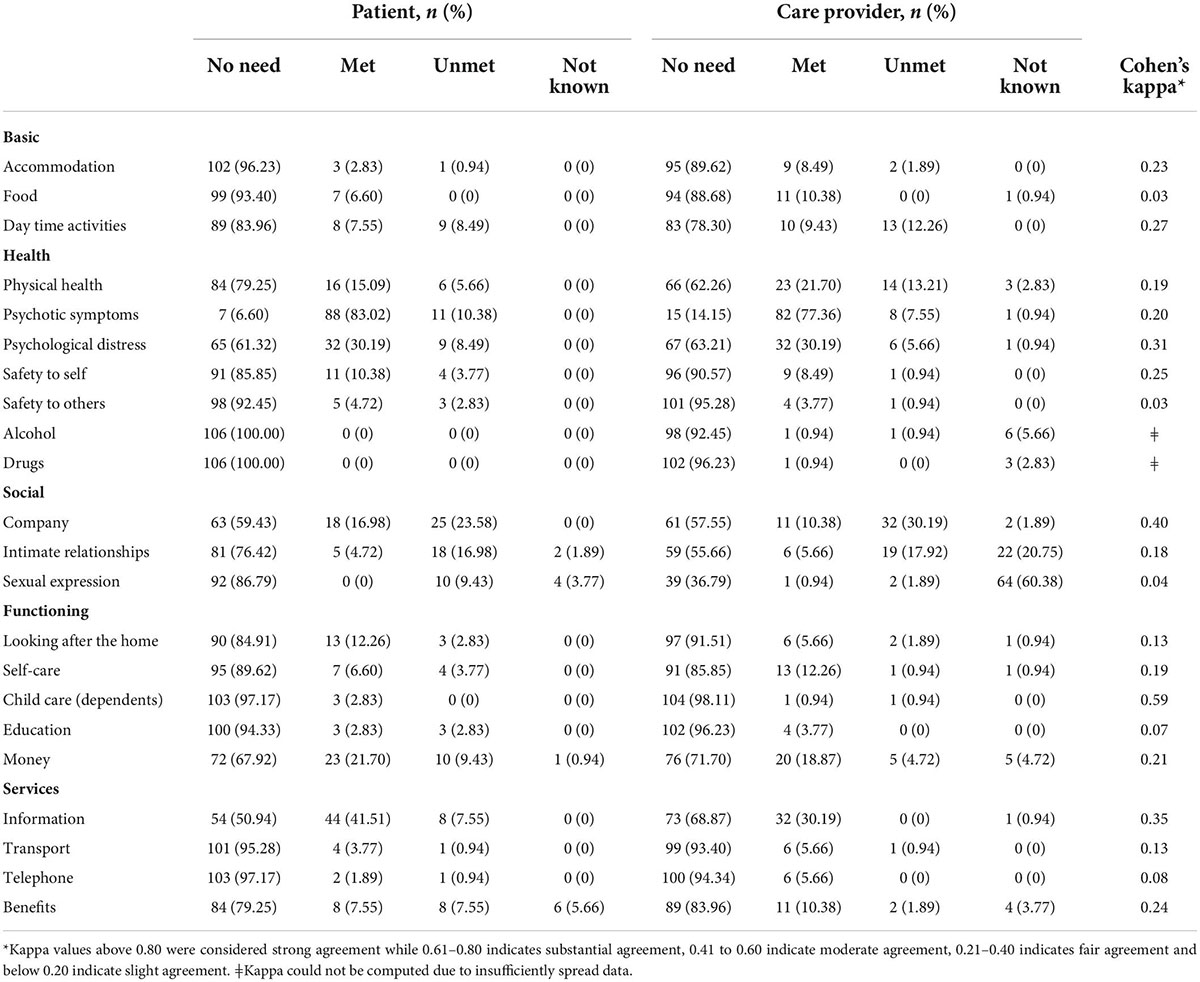
The majority of patients reported absence of needs on all items, except the needs regarding psychotic symptoms, under the “health” domain (Table 2, 6.6%; n = 7 for patients compared to 14.15%; n = 15 for CPs), and on information about the disease and treatment under the “services” domain (50.94%; n = 54 of patient vs. 68.87%; n = 73 of CPs). For “psychotic symptoms,” the majority of patients who reported a need indicated the need as “met” (83.02%; n = 88 of patients compared to 77.36%; n = 82 of CPs). For “information on disease and treatment,” 41.51% (n = 44) and 7.55% (n = 8) of the patients had met and unmet needs, whilst 30.19% (n = 32) and 0% of CPs identified a met and unmet need, respectively. The highest number of unmet needs were identified for the social (50% of patients and CP) and health domains (31.13% of patients vs. 28.30% by CP).
While the number of participants (patients and CPs) who identified unmet needs were similar for “social” and “health” domains, a higher number of CPs (14.15%; n = 15) when compared to the patients (9.43%; n = 10) identified unmet needs in “basic” needs domain. On the contrary, a higher number of patients identified unmet needs for “functioning” (18.87%; n = 20 vs. 8.49%; n = 9) and “services” (16.98%; n = 18 vs. 2.83%; n = 3) when compared to the CPs. CPs perceived higher number of unmet needs on 4 specific items under various domains when compared to the patients: accommodation (1.89% vs. 0.94%), company (30.19% vs. 23.58%), alcohol (0.94% vs. 0%) and intimate relationships (17.92% vs. 16.98%). Company, intimate relationships, psychotic symptoms, money, sexual expression, psychological distress, information, and benefits were the most frequent unmet needs identified by the patients. On the other hand, company, intimate relationships, physical health, and daytime activities were the unmet needs identified by CPs.
Highest number of needs were identified (met or unmet needs) for health, social and services domain (Supplementary Table 1).
Concordance between patients and care providers
Moderate agreement (k = 0.41–0.6, Table 2) was noted only for the childcare/dependents needs (k = 0.59). Fair agreement (k = 0.21–0.4) was noted for basic needs (accommodation, daytime activities), health (psychological distress, safety to self), social (company), functioning (money) and for services (information, benefits). Slight agreement (k = 0–0.2) was noted for services (transport, telephone) functioning (looking after home, self-care and education), health (physical health, psychotic symptoms, safety to others) and basic needs (food). The lowest level of agreement was noted for needs for food (k = 0.03), safety to others (k = 0.03), sexual expression (k = 0.04), education (k = 0.07) and telephone (k = 0.08). Among the items identified as unmet needs, company and intimate relationship were the top 2 items endorsed by the patients and CPs in agreement which each other.
Factors influencing unmet needs felt by the patients
Duration of untreated psychosis, PANSS score, treatment adherence, hospital admissions, psychiatric medication and treatment duration showed no significant relationship with total unmet needs. Age, depression, anxiety, and OCD showed a positive association with unmet needs. Compared to minors (18–21 years old), adults (aged 31–40 years) tend to endorse significantly more unmet needs (B: 1.10; 95% CI: 0.15–2.05; p = 0.03; Table 3). Those with moderate severity of depression tend to report higher number of unmet needs (B: 1.35; 95% CI: 0.35–2.35; p = 0.01) compared to those with no or minimal depressive symptoms. Similarly, those with severe anxiety (B: 2.18; 95% CI: 0.52–43.84; p = 0.01), and OCD (B: 1.69; 95% CI: 0.61–2.76; < p = 0.01) reported more unmet needs than those with minimal anxiety and below clinical threshold OCD, respectively.
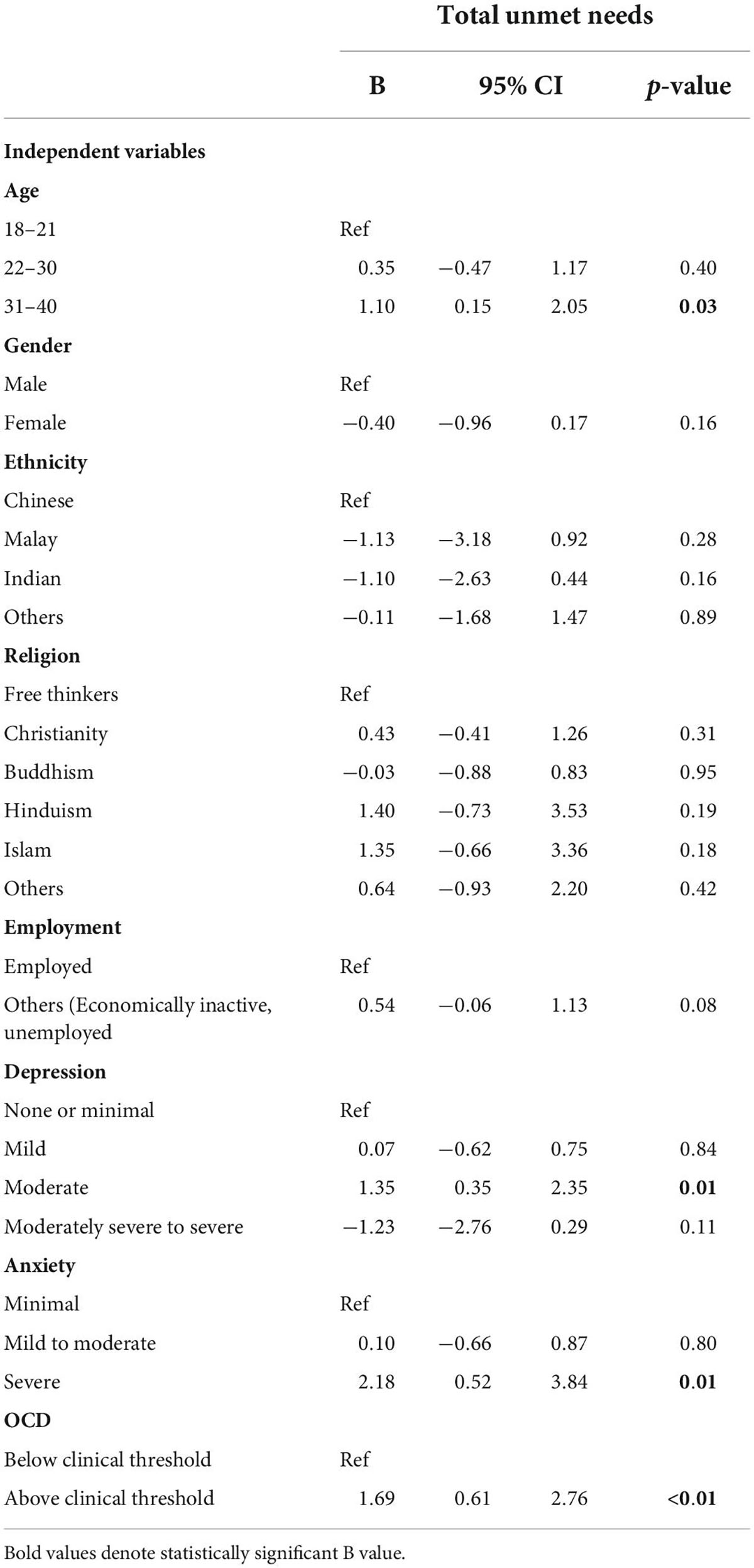
Table 3. Results of linear regression examining the sociodemographic and clinical correlates of needs felt by patients.
Discussion
In the current study, patients and CPs identified similar need domains with an average of 4.06 and 3.84, needs, respectively. Both the groups identified health and social domains to have a higher number of unmet needs. The agreement between patients and CPs were, however, low. Age, depression, anxiety, and OCD were positively associated with unmet needs felt by patients.
In the current study, patients and CPs identified an average of 4.06 and 3.84 needs, respectively. Patients endorsed 1.26 unmet needs compared to 1.02 by CPs. This is lower than what was reported by Slade et al. (27) who reported 6.7 and 6.1 needs for patients and CPs, respectively. However, it is similar to Lasalvia et al. (33) who observed an average need endorsement of 3.64 in a sample of patients with psychosis in Italy. However, the authors did not analyze the average unmet needs in their study. Jorquera et al. (34) identified an average of 1.0 unmet needs per patients which is in agreement with our results. Fleury et al. (35) compared the needs endorsed by participants from different areas in Quebec and showed that metropolitan areas were vulnerable to unmet needs. The authors also compared the mental health needs endorsed by various studies and showed a varying level of need endorsements ranging from 3.07 to 9.5 by patients and 2.4–10.9 by CPs. McCrone et al. (20) compared the needs of schizophrenia patients across the world and concluded that the needs are different across countries. These observed differences were proposed to be due to area specific factors, interviewer characteristics (interviewers who are clinicians are well acquainted to the needs and thus will identify more problems) or cultural differences (20, 35). Contrary to that reported in developed nations, studies conducted in developing nations showed different domains of unmet needs (26). A study conducted in Brazil among patients with early psychosis identified transportation and benefits as domains of unmet needs (36). This was attributed to the lack of awareness of the participants regarding their benefit entitlements. A similar study in Ethiopia among individuals with psychosis identified higher unmet needs on basic (accommodation, food, daytime activities) and social life domains (37). Thus, the needs of the patients could be different based on the economic status, infrastructure, and healthcare policies. The lower endorsement of needs in the current study could be attributed to the local services. Singapore being a developed country that has an efficient healthcare system and community level outreach could have addressed the basic growth and deficiency needs through strong policies that support the needs of the population.
The majority of participants endorsed having no need for most of the items on the scale except for specific items (psychotic symptoms and information on condition and treatment), for which a substantial proportion from both the groups endorsed that the needs are met (psychotic symptoms: 83.02%; information: 41.51%). This is probably because the treatment is delivered specifically for the psychotic symptoms and thus the treatment needs for psychotic symptoms and need for information is fulfilled for the majority of patients who are seeking treatment for first episode psychosis 39). This agrees with previous reports (12, 34, 38). Endorsement of a fulfilled need (met need) is captured as the presence of a need for which the patient has received help from the health care system, family/friends, or community partners to fulfill the need. Thus, it can be considered as a positive outcome of treatment. EPIP Singapore has an efficient patient management system that involves a multidisciplinary team assessing and taking care of the needs of the patients. Thus, the low endorsement of unmet needs could be a reflection of care provided by the program. Nonetheless, Jorquera et al. (34) have warned that emphasis on clinical elements alone often leads to the unintentional neglect of other domains that are of paramount importance in achieving the desired treatment outcomes.
Needs (met or unmet) were reported for “social,” “health” and “services” domains by both patients and CPs with the former two being the domains of most of the unmet needs. In particular, company (social interaction), intimate relationships, psychotic symptoms, money, sexual expression and psychological distress, information and benefits were identified to have an unmet need in descending order with the former three being the most prominent unmet needs felt by the patients. EPIP offers a system which addresses the basic, social, services, functioning and healthcare needs of the patients. Nonetheless, the pandemic had a tremendous impact on the care delivery during the past 2 years where social distancing measures and healthcare burden of the pandemic had affected group therapy sessions and face to face consultations that were meant to address these aspects. The data was captured during this period where there were ongoing restrictions that prevented social interactions between CPs and patients or among patients. Thus, the unmet needs reflected in the social and services domains could reflect the pandemic induced barriers to care that included inability to hold face to face sessions such as group activities or group therapy, psychoeducation and other social activities which are a part of the treatment. It could also be attributed to illness specific factors such as negative symptoms e.g., avolition and social withdrawal which are commonly observed in schizophrenia. Furthermore, as the needs of the patients change at different stages of their life/disease (39, 40) it is possible that the needs emerged during the course of their treatment journey. Therefore, an ongoing evaluation of the needs must be integrated to the psychoeducation programs to address emerging needs. It is also possible that the patients often forget the information on their treatment and disease given by their care team and thus continued education/communication as a part of the existing program would be a useful strategy to mitigate the unmet needs. We also noted unmet needs in sexual expression (sexual life and contraception) and intimate relationships. In Asian culture, sexual expression and relationships are considered as extremely private topics which are not often discussed between patients and CPs due to embarrassment, cultural influences, or lack of training of the CPs to handle these sensitive topics. Nonetheless, unmet needs in these domains requires attention and the care team should work toward identifying the causes of the unmet needs to take effective steps to resolve them.
A few of the studies have reported similar domains of unmet needs (41), however, the domains and items identified in various studies tend to differ. Psychological distress was a common unmet need identified in most of the studies (12, 27, 34, 35), as it is a common occurrence in recovering patients who understand the reality of their condition once their symptoms stabilize. They feel the stress, worry, grief, or anxiety with their social situation and reintegration which stems from their social exclusion due to the mental illness or lack of social skills. Other studies conducted in schizophrenia patients identified mostly different unmet needs (12, 27, 34, 35). A systematic review of 20 studies showed that social relationships, information about disease and psychological distress were the main sources of unmet needs in people with mental illness (5). The source of these discrepancies is multifactorial and could be attributed to the sociocultural context/characteristics of the sample and the differences in the care systems (8). Socioeconomic status, social contact, family relationship and stigmatization in the community influences the type of needs felt by the patients (8). Another factor that could play a key role in the observed discrepancy among studies is the severity and stage of the disease. A study conducted in Australia among people with mental illness showed higher unmet needs for company, daytime activity and intimate relationship in community and inpatient samples (42). The authors noted that the need was higher for inpatient samples. In contrast, long stay patients with a psychotic disorder reported unmet needs on domains for accommodation, social and care (43). Also, the needs of the patients evolve with time and are different at different time points (39, 40). Unmet needs are also dependent on the stage of the disease. Although the available evidence in early psychosis patients is scarce, it was noted that psychotic symptoms, psychological distress, daily activities and social relationships were the needs endorsed by the patients with early psychosis, which is similar to our observation (34, 40). These reports thus emphasize the importance of needs assessments at regular intervals in specific subpopulations of diagnoses to capture the evolving needs of the patients in the context of the limitations in applying the results across populations.
We noted low levels of agreement ranging from slight to fair between the CP and patients in the majority of domains (19 out of 22). This could be due to various reasons which include staff characteristics where CPs with different professional expertise focus on specific needs thus some needs are inadvertently ignored. The underpinnings of this omission could be the differences in the perception of necessity, convenience, lack of knowledge or inability to reach a consensus even after the discussion (32). Our CPs identified by the patients included psychiatrists (n = 24), case managers (n = 77), psychologists (n = 3) and peer support specialist (n = 2) who have different level of expertise and interactions with the patients. Similar results were recorded in previous studies (32). While the staff might be aware of the clinical care needs, they might not have sufficient knowledge on other domains, leading to a low concordance (27, 32, 35, 44). Fleury et al. (35) looked at CP specific characteristics and showed its influence on the needs identified. Psychiatrists tend to identify only clinical issues while social workers and other professionals endorse problems in other social, functioning and service-related domains Nonetheless, the lack of a substantial concordance between the patients and CPs has clinical implications as it reflects a lack of understanding of actual unmet needs which would have an impact on the treatment process and its outcome. Thus, an approach that involves training of the CPs to identify various areas of needs of their patients beyond the clinical elements and effective planning to monitor the unmet needs observed in areas with slight agreement (services, functioning and health domains) along with strategies to fulfill the needs could achieve favorable outcomes.
We have also noted that sociodemographic and clinical characteristics of the patients were associated with the unmet needs. Older adults (31–40 years) when compared to young adults (18–21 years) reported significantly higher number of unmet needs. This could be attributed do their family environment, socioeconomic status, and comorbidities. It is possible that the older age group had higher commitments than the younger age group and thus report higher unmet needs. Also, it is well known that older patients are more prone to chronic conditions that could add on to their unmet needs. Similar results were reported previously (45, 46). We have noted that those with moderate depressive symptoms, OCD and severe anxiety tend to report significantly higher number of unmet needs. Other studies have also noted similar findings (12, 47). Depression, anxiety, and OCD are highly prevalent in those with schizophrenia spectrum and other psychotic disorders. Our previous studies have noted a prevalence of 16.5% for depression and 5.1% for OCD in the EPIP population (48) which could lead to unmet needs, especially in psychiatric and psychosocial domains in patients with early psychosis (20, 49, 50). We did not observe a relationship between the treatment duration, adherence to medication and duration of untreated psychosis with unmet needs. While our results corroborate the findings by Landolt et al. (40) who studied the correlates of unmet needs in early psychosis and reported no relationship between these variables, it contradicts the findings from Jorquera et al. (34). This could be attributed to the same characteristics that were discussed earlier.
This study was conducted in a sample of patients receiving care for first episode psychosis and thus adds value to the knowledge gaps on the needs of this population. We have also considered the treatment duration, adherence, duration of untreated psychosis, use of medication and hospitalization to account for the factors that could affect the unmet needs. The sample was drawn from the outpatient clinic of the EPIP and thus the results cannot be generalized without reservation. Also, we have employed the kappa coefficients to deduce the concordance between patients and CPs. While kappa coefficients were calculated due to its advantage of controlling for expected agreement levels occurring by chance, it should still be interpreted with caution, especially when obvious disparity in needs are observed between parties of interest. Finally, the low coefficient is not exclusively an indication of the low agreement but could also be due to the skewed distribution of the values across the categories. Future research should focus on gaining an in depth understanding of the reasons for unmet needs reported in specific domains and patients’ perspective/suggestions to overcome these unmet needs. A qualitative study would shed light on this unknown aspect and give directions for improving the consensus of unmet needs between patients and CPs. Furthermore, additional domains of needs that are relevant in early psychosis patients such as, cognitive functions (memory), and needs for occupational/role functioning (attaining goals/aspiration, independent work/studies) should be explored to ensure holistic care.
Conclusion
Highest number of unmet needs were identified by patients and CPs in social, health and functioning domain with patients identifying highest unmet needs in functioning and services domain. The items that scored the highest proportion of unmet needs were company, intimate relationships (social domain) followed by psychotic symptoms (health domain). The agreement between patients and CPs were slight to-fair. Low concordance could reflect the lack of knowledge of the CPs in that particular domain stemming from lack of expertise, or disagreements between patients and CPs and should be improved through effective discussion and resolution of the problems. Older age, having depressive symptoms, OCD and severe anxiety were associated with unmet needs felt by the patients. Treatment of psychiatric comorbidities could alleviate some of the unmet needs. Routine monitoring of the needs of patients could reveal changing perspectives and dynamics that will enable CPs to work toward fulfilling the unmet needs through effective communication and goal setting. Such arrangements could improve treatment outcomes and quality of life of patients.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the National Healthcare Group’s Domain Specific Review Board (DSRB Ref:2020/01112). Written informed consent to participate in this study was provided by the participant or his/her legal guardian (if minor) legal guardian/next of kin.
Author contributions
PA and MS conceptualized the study. PA, MS, ES, SV, CT, SK, and LZ contributed to study methodology. PA, PS, PW, YT, SV, CT, JH, LC, and ES were involved in the data collection. ES and PA performed data validation and quality checks. PA, MS, and YT performed data analysis and interpretation. PA wrote the first draft of the manuscript. All authors revised the manuscript and approved the final manuscript.
Funding
The study was funded by the Institute of Mental Health’s Research Fund (Ref No: 733-2020).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.952666/full#supplementary-material
References
1. Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. (2018) 44:1195–203. doi: 10.1093/schbul/sby058
2. Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. (2016) 12:357. doi: 10.2147/NDT.S96649
3. Oakley P, Kisely S, Baxter A, Harris M, Desoe J, Dziouba A, et al. Increased mortality among people with schizophrenia and other non-affective psychotic disorders in the community: a systematic review and meta-analysis. J Psychiatr Res. (2018) 102:245–53. doi: 10.1016/j.jpsychires.2018.04.019
4. Crespo-Facorro B, Such P, Nylander AG, Madera J, Resemann HK, Worthington E, et al. The burden of disease in early schizophrenia–a systematic literature review. Curr Med Res Opin. (2021) 37:109–21. doi: 10.1080/03007995.2020.1841618
5. Tuncer G, Duman ZÇ. Needs of individuals with chronic mental disorders: a systematic review. Psikiyatride Guncel Yaklasimlar. (2020) 12:155–67. doi: 10.18863/pgy.530945
7. Stevens A, Gillam S. Needs assessment: from theory to practice. BMJ. (1998) 316:1448–52. doi: 10.1136/bmj.316.7142.1448
8. Torres-González F, Ibanez-Casas I, Saldivia S, Ballester D, Grandón P, Moreno-Küstner B, et al. Unmet needs in the management of schizophrenia. Neuropsychiatr Dis Treat. (2014) 10:97. doi: 10.2147/NDT.S41063
9. Krynicki CR, Upthegrove R, Deakin JF, Barnes TR. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr Scand. (2018) 137:380–90. doi: 10.1111/acps.12873
10. Temmingh H, Stein DJ. Anxiety in patients with schizophrenia: epidemiology and management. CNS Drugs. (2015) 29:819–32. doi: 10.1007/s40263-015-0282-7
11. Swets M, Dekker J, van Emmerik-van Oortmerssen K, Smid GE, Smit F, de Haan L, et al. The obsessive compulsive spectrum in schizophrenia, a meta-analysis and meta-regression exploring prevalence rates. Schizophr Res. (2014) 152:458–68. doi: 10.1016/j.schres.2013.10.033
12. Uygur AB, Esen Danaci A. Needs of patients with schizophrenia and their predictors. Turk Psikiyatri Dergisi. (2019) 30:180–90.
13. Slade M, Phelan M, Thornicroft G, Parkman S. The camberwell assessment of need (CAN): comparison of assessments by staff and patients of the needs of the severely mentally ill. Soc Psychiatry Psychiatr Epidemiol. (1996) 31:109–13. doi: 10.1007/BF00785756
14. Grinshpoon A, Friger M, Orev E, Shvarts S, Kaplan ZE, Abramowitz MZ, et al. Relative perceptions of the needs of inpatients with schizophrenia and schizoaffective disorders. Isr J Psychiatry Relat Sci. (2008) 45:201–9.
15. Foldemo A, Ek AC, Bogren L. Needs in outpatients with schizophrenia, assessed by the patients themselves and their parents and staff. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:381–5. doi: 10.1007/s00127-004-0750-8
16. Ochoa S, Haro JM, Autonell J, Pendas A, Teba F, Marquez M. NEDES group. Met and unmet needs of schizophrenia patients in a Spanish sample. Schizophr Bull. (2003) 29:201–10. doi: 10.1093/oxfordjournals.schbul.a006998
17. Joska J, Flisher AJ. The assessment of need for mental health services. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:529–39. doi: 10.1007/s00127-005-0920-3
18. Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. BMJ. (1998) 316:1310–3. doi: 10.1136/bmj.316.7140.1310
19. Morgan C, Fearon P, Lappin J, Heslin M, Donoghue K, Lomas B, et al. Ethnicity and long-term course and outcome of psychotic disorders in a UK sample: the ÆSOP-10 study. Br J Psychiatry. (2017) 211:88–94. doi: 10.1192/bjp.bp.116.193342
20. McCrone P, Leese M, Thornicroft G, Schene A, Knudsen HC, Vázquez-Barquero JL, et al. EPSILON study group. A comparison of needs of patients with schizophrenia in five European countries: the EPSILON Study. Acta Psychiatr Scand. (2001) 103:370–9. doi: 10.1034/j.1600-0447.2001.00207.x
21. Alang SM. Sociodemographic disparities associated with perceived causes of unmet need for mental health care. Psychiatr Rehabil J. (2015) 38:293–9. doi: 10.1037/prj0000113
22. Yang JC, Roman-Urrestarazu A, McKee M, Brayne C. Demographic, socioeconomic, and health correlates of unmet need for mental health treatment in the United States, 2002–16: evidence from the national surveys on drug use and health. Int J Equity Health. (2019) 18:1–1. doi: 10.1186/s12939-019-1026-y
23. Subramaniam M, Abdin E, Vaingankar JA, Sambasivam R, Zhang YJ, Shafie S, et al. Lifetime prevalence and correlates of schizophrenia and other psychotic disorders in Singapore. Front Psychiatry. (2021) 12:249. doi: 10.3389/fpsyt.2021.650674
24. Chong SA, Verma S, Mythily S, Poon LY, McGorry PD. The early psychosis intervention programme in Singapore: a balanced scorecard approach to quality care. J Ment Health. (2008) 17:79–91. doi: 10.1080/09638230701530200
25. Verma S, Poon LY, Subramaniam M, Abdin E, Chong SA. The Singapore early psychosis intervention programme (EPIP): a programme evaluation. Asian J Psychiatr. (2012) 5:63–7. doi: 10.1016/j.ajp.2012.02.001
26. Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, et al. The camberwell assessment of need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry. (1995) 167:589–95. doi: 10.1192/bjp.167.5.58931
27. Slade M, Phelan M, Thornicroft G. A comparison of needs assessed by staff and by an epidemiologically representative sample of patients with psychosis. Psychol Med. (1998) 28:543–50. doi: 10.1017/s0033291798006564
28. Kroenke K, Spitzer RL, Williams JB. The PHQ−9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
30. Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The obsessive-compulsive inventory: development and validation of a short version. Psychol Assess. (2002) 14:485–96.
31. Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB, et al. The OCI-R: validation of the subscales in a clinical sample. J Anxiety Disord. (2007) 21:394–406. doi: 10.1016/j.janxdis.2006.05.006
32. Houtjes W, van Meijel B, Deeg DJ, Beekman AT. Unmet needs of outpatients with late-life depression; a comparison of patient, staff and carer perceptions. J Affect Disord. (2011) 134:242–8. doi: 10.1016/j.jad.2011.05.052
33. Lasalvia A, Ruggeri M, Mazzi MA, Dall’Agnola RB. The perception of needs for care in staffand patients in community−based mental health services. The south−verona outcome project 3. Acta Psychiatr Scand. (2000) 102:366–75. doi: 10.1034/j.1600-0447.2000.102005366.x
34. Jorquera N, Alvarado R, Libuy N, de Angel V. Association between unmet needs and clinical status in patients with first episode of schizophrenia in Chile. Front Psychiatry. (2015) 6:57. doi: 10.3389/fpsyt.2015.00057
35. Fleury MJ, Grenier G, Lesage A. Agreement between staff and service users concerning the clientele’s mental health needs: a quebec study. Can J Psychiatry. (2006) 51:281–6. doi: 10.1177/070674370605100503
36. Schlithler AC, Scazufca M, Busatto G, Coutinho LM, Menezes PR. Reliability of the Brazilian version of the camberwell assessment of needs (CAN) in first-episode psychosis cases in São Paulo. Brazil. Braz J Psychiatry. (2007) 29:160–3. doi: 10.1590/s1516-44462006005000026
37. Fekadu A, Hanlon C, Gebre-Eyesus E, Agedew M, Solomon H, Teferra S, et al. Burden of mental disorders and unmet needs among street homeless people in Addis Ababa. Ethiopia. BMC Med. (2014) 12:1–2. doi: 10.1186/s12916-014-0138-x
38. Ganesh K, Gupta S. Comparison of unmet needs of patients on treatment of schizophrenia perceived by patients and their family caregivers. Indian J Soc Psychiatry. (2017) 33:181. doi: 10.4103/ijsp.ijsp_31_16
39. Killaspy H, Rambarran D, Bledin K. Mental health needs of clients of rehabilitation services: a survey in one trust. J Ment Health. (2008) 17:207–18.
40. Landolt K, Rössler W, Burns T, Ajdacic-Gross V, Galderisi S, Libiger J, et al. Unmet needs in patients with first-episode schizophrenia: a longitudinal perspective. Psychol Med. (2012) 42:1461–73. doi: 10.1017/S0033291711002406
41. Hosáková J, Hosák L. Needs of hospitalized schizophrenic patients in the north moravia and the czech part of silesia. Acta Medica (Hradec Kralove). (2015) 58:104–7. doi: 10.14712/18059694.2015.102
42. Cleary M, Freeman A, Hunt GE, Walter G. Patient and carer perceptions of need and associations with care-giving burden in an integrated adult mental health service. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:208–14.
43. Chopra P, Herrman HE. The long-term outcomes and unmet needs of a cohort of former long-stay patients in melbourne. Australia. Community Ment Health J. (2011) 47:531–41. doi: 10.1007/s10597-010-9351-z
44. MacCarthy B, Benson J, Brewin CR. Task motivation and problem appraisal in long-term psychiatric patients. Psychol Med. (1986) 16:431–8. doi: 10.1017/s0033291700009260
45. Hickie IB, Davenport TA, Scott EM, Hadzi−Pavlovic D, Naismith SL, Koschera A. Unmet need for recognition of common mental disorders in Australian general practice. Med J Aust. (2001) 175:S18–24. doi: 10.5694/j.1326-5377.2001.tb143785.x
46. Guillén Andrés AI, Muñoz López M. Variables related to psychosocial needs among people with severe mental illness using community services and their informal caregivers. Anuario de Psicol Clin de La Salud Ann Clin Health Psychol. (2011) 7:15–23.
47. Parslow RA, Parslow RA, Jorm AF. Predictors of partially met or unmet need reported by consumers of mental health services: an analysis of data from the Australian national survey of mental health and wellbeing. Aust N Z J Psychiatry. (2001) 35:455–63. doi: 10.1046/j.1440-1614.2001.00924.x
48. Sim K, Swapna V, Mythily S, Mahendran R, Kua EH, McGorry P, et al. Psychiatric comorbidity in first episode psychosis: the early psychosis intervention program (EPIP) experience. Acta Psychiatr Scand. (2004) 109:23–9. doi: 10.1111/j.0001-690x.2004.00196.x
49. DeVylder JE, Oh HY, Corcoran CM, Lukens EP. Treatment seeking and unmet need for care among persons reporting psychosis-like experiences. Psychiatr Serv. (2014) 65:774–80. doi: 10.1176/appi.ps.201300254
Keywords: need assessment, treatment need, care provider, unmet needs, Camberwell Assessment of Needs
Citation: AshaRani PV, Tan YWB, Samari E, Wang P, Cetty L, Satghare P, Ho J, Koh SA, Zhong Yi L, Tang C, Verma S and Subramaniam M (2022) Needs of patients with early psychosis: A comparison of patient’s and mental health care provider’s perception. Front. Psychiatry 13:952666. doi: 10.3389/fpsyt.2022.952666
Received: 27 May 2022; Accepted: 26 August 2022;
Published: 20 September 2022.
Edited by:
Roy Abraham Kallivayalil, Pushpagiri Medical College, IndiaReviewed by:
Sudhir Bhave, DR NKP Salve Institute of Medical Sciences and Research Centre, IndiaJoice Geo, Pushpagiri Medical College, India
Copyright © 2022 AshaRani, Tan, Samari, Wang, Cetty, Satghare, Ho, Koh, Zhong Yi, Tang, Verma and Subramaniam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: P. V. AshaRani, QXNoYXJhbmlfUEVaSFVNTU9PVFRJTF9WQVNVREVWQU5fTkBpbWguY29tLnNn
 P. V. AshaRani
P. V. AshaRani Yeow Wee Brian Tan
Yeow Wee Brian Tan Ellaisha Samari
Ellaisha Samari Peizhi Wang1
Peizhi Wang1 Laxman Cetty
Laxman Cetty Pratika Satghare
Pratika Satghare Lee Zhong Yi
Lee Zhong Yi Charmaine Tang
Charmaine Tang Swapna Verma
Swapna Verma Mythily Subramaniam
Mythily Subramaniam