
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 05 October 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.946383
 Zhuo-Ran Chen1†
Zhuo-Ran Chen1† Li Zhang2†
Li Zhang2† Ya-Wei Chen3
Ya-Wei Chen3 Meng-Yang Xu4
Meng-Yang Xu4 Hang Jia5
Hang Jia5 Meng-Ying Li6
Meng-Ying Li6 Yu-Han Lou7,8,9
Yu-Han Lou7,8,9 Ling Lan7,8,9*
Ling Lan7,8,9*Shared decision-making (SDM) is a scientific and reasonable decision-making model. However, whether physicians choose SDM is usually influenced by many factors. It is not clear whether the strained doctor–patient relationship will affect physicians' willingness to choose SDM. Through a survey by questionnaire, 304 physicians' evaluations of doctor–patient relationship (DPR) were quantified by the difficult DPR questionnaire-8. Their preferences for SDM and the reasons were also evaluated. The correlation between physicians' evaluations of DPR and their preferences for SDM were analyzed. 84.5% physicians perceived DPR as poor or strained, 53.3% physicians preferred SDM, mainly because of the influences of medical ethics and social desirability bias. Their preferences for SDM were not significantly correlated with their evaluations of DPR (P > 0.05). Physicians with different evaluations of DPR (good, poor, and strained) all had similar preferences for SDM (42.6, 56.4, and 42.9%), with no significant difference (P > 0.05). There was no correlation between physicians' evaluations of DPR and their preferences for SDM. Physicians' evaluations of poor DPR did not affect their preferences for SDM. This may be influenced by the medical ethics and social desirability bias.
Shared decision-making (SDM) is an advocated clinical decision-making model in which physicians and patients work together to decide on clinical diagnoses and treatment plans. In SDM, a physician informs a patient about the efficacy, benefits and risks of a treatment plan; the patient informs the physician about his/her views and concerns about the disease and related risks; and finally, the physician and patient make right and reasonable choice together regarding issues related to diagnosis and treatment during the medical process (1–5). SDM requires physicians to consider the best scientific evidence and the values, goals and propensities of patients (6). As a good clinical decision-making model, SDM reflects the patient-centered approach, which is more conducive to ensuring individualized diagnosis and treatment, reducing medical risks and improving patient compliance and therapeutic effects (2, 3, 7–15) than the traditional informational model (in which physicians inform patients of the pros and cons of the available treatment options and let the patients make the final decision alone) and the paternalistic model (in which physicians make all decisions on behalf of the patients). Therefore, SDM has received increasing attention from both physicians and patients in various specialties in many countries including psychiatrists (16, 17). Salyers and Zisman-Ilani (17) pointed out that SDM required patient involvement in mental health service delivery and in promoting mental well-being. In recent years, patient decision aid (PDA) has become one of the effective ways of SDM. It can take many forms, such as tables, movies, or applications. For example, Ottawa Personal Decision Guide, Annalisar software, etc. (18).
On the other hand, good DPR is the necessary foundation for the smooth development of medical activities, which can not only promote patients' recovery, but also be very important for physicians' mental health. However, in China, the tense doctor–patient relationship (DPR) has become a general problem. A data published in 2019 by China Medical Association showed that there were 90,000 medical disputes in China in 2016, in which there were above 50% of medical staff subjected to verbal violence and 15% of the medical staff suffered physically hurt (19). Under the influence of tense DPR, physicians are prone to develop a sense of identity and alertness, increase psychological pressure and subjectively cause a poor evaluation of DPR. The constant deterioration of DPR in recent years has manifested as a lack of understanding and trust between physicians and patients (20–26).
As one of the key subjects who choice SDM, physicians' preference for SDM is crucial to promoting its development. However, under the current tense situation of DPR in China, physicians' evaluations of DPR might affect their diagnosis and treatment behaviors, such as fear of responsibility, conservative treatment and unwillingness to communicate, which should also include the impact on whether they are willing to choose SDM. In the context of increasingly strained DPR, what are physicians' preferences for SDM? Whether is there correlation between physicians' evaluations of DPR and their preferences for SDM? No relevant research has been reported. Therefore, this study analyzed physicians' preferences for SDM and reasons, and the correlation between physicians' evaluations of DPR and their preferences for SDM.
329 clinical physicians were selected randomly as study participants from 22 clinical departments in a general hospital in China. A total of 329 questionnaires were distributed, and 312 questionnaires were recovered on site. A total of 304 (92.4%) valid questionnaires were included in this study. All participants gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Zhengzhou University in China.
The Difficult DPR Questionnaire-10 (DDPRQ-10) (27, 28) was widely used to quantitatively evaluate physicians' evaluations of DPR. Yang H et al. revised it to form a Chinese-specific DDPRQ-8, which had good reliability and validity (29). The contents and scoring methods of DDPRQ-8 was respectively shown as Table 1. The evaluations of DPR were classified into three levels based on the DDPRQ-8 score: good (0–16 points), poor (17–32 points), and strained (33–48 points).
The open ended questions in questionnaires were used. Physicians' preferences for SDM were classified into three levels and five categories as followed: high propensity (including considerably high propensity and relatively high propensity), neutral propensity, and low propensity (including relatively low propensity and extremely low propensity). Additionally, the reasons of physicians' preferences for SDM were investigated, including the influence of medical ethics (presence or absence), social desirability bias (presence or absence), DPR (good or poor), patients' willingness to participate in decision-making (strong or weak), patients' level of medical knowledge (high or low), and whether SDM is necessary for patient's conditions (yes or no). Three levels, five categories and six reasons of SDM preference were listed on the questionnaire. Data was collected by allowing physicians to self-evaluate and choose an appropriate level, category and reason respectively.
The sample size was calculated by a formal power analysis. The significance level of α was set to 0.05. Fisher's exact test showed that the sample size was at least 200, which can provide >80% potency to detect the differences. SPSS 24.0 was used for data analysis. Chi-square test was used to compare the physicians' evaluations of DPR under the demographic information, and analyze the difference of the reasons of physicians' preferences for SDM. Spearman's rank correlation coefficient and Fisher's exact test were used to analyze the correlation between physicians' evaluations of DPR and their preferences for SDM. P < 0.05 was considered statistically significant.
The demographic information of physicians included department, age, gender, educational level, and professional title. 304 physicians came from 22 clinical departments including neurology, psychiatry, gastroenterology, hepatology, respiratory and pediatrics, etc. (Table 2). There were 64.5% male and 35.5% female participants, with an average age of 38.8 ± 8.9 years (range: 24–60 years). They included 36 (11.8%) resident physicians, 126 (41.4%) attending physicians, 68 (22.4%) associate chief physicians, and 74 (24.3%) chief physicians. The educational backgrounds of participants were as followed: 55 Bachelors (18.1%), 166 Masters (54.6%) and 83 Doctors (27.3%) (Table 3).
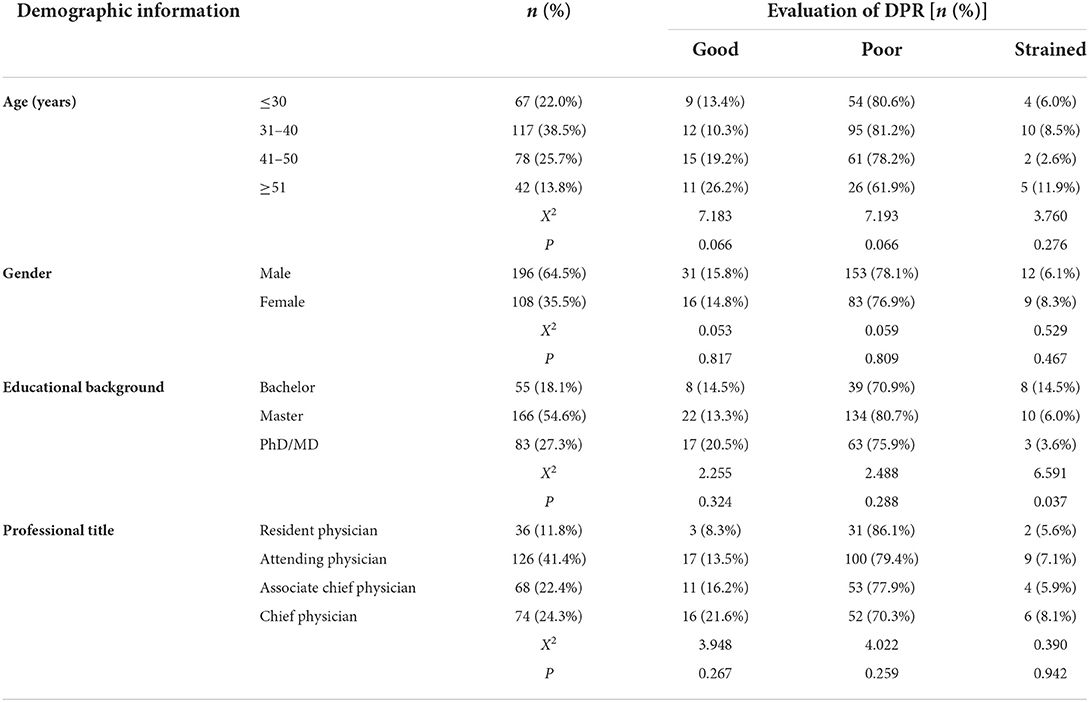
Table 3. Physicians' evaluations of doctor–patient relationship (DPR) under the demographic information.
Physicians generally had a negative attitude toward DPR and perceived DPR as poor. A total of 84.5% (257/304) of physicians had a DDPRQ-8 score of 17 or higher, suggesting that they perceived DPR as poor or strained; this group included the 6.9% (21/304) of physicians with a DDPRQ-8 score of 33 or higher, suggesting that they perceived DPR as strained (Table 4).
Physicians generally perceived DPR as poor under different demographic information, including age, gender, educational level and professional title (Table 2). There were no significant different of physicians' evaluations of good, poor or strained DPR, among different levels of age, gender, educational level and professional title, respectively (The values of χ2 and P were shown in Table 3).
A total of 53.3% (162/304) of physicians preferred SDM, while 21.1% (64/304) did not prefer SDM (Table 5).
An investigation of the possible reasons for physicians' preferences indicated that physicians preferred SDM mainly because of the influences of medical ethics and social desirability bias, with medical ethics accounting for 60.5% of the responses. The leading reasons for a neutral propensity were the same as above, with medical ethics accounting for 30.8% and social desirability bias accounting for 39.7%. The leading reasons for low propensity were poor DPR and low levels of medical knowledge among patients, with medical ethics accounting for 34.4% and social desirability bias accounting for 28.1% of the responses. The results of the chi-square test showed that the differences among physicians with different preferences for SDM were statistically significant (χ2 = 124.445, P < 0.001) (Table 6).
Spearman's rank correlation coefficient showed that physicians' evaluations of poor DPR and their preferences for SDM were independent of each other. There was no significant correlation between the two (r = −0.082, P = 0.155).
Fisher's exact test showed that similar proportions of physicians preferred SDM regardless of whether they perceived DPR as good, poor or strained; the respective proportions were 42.6, 56.4 and 42.9%. The preferences for SDM were not significantly different among physicians who perceived good, poor or strained DPR (P = 0.073) (Table 7).
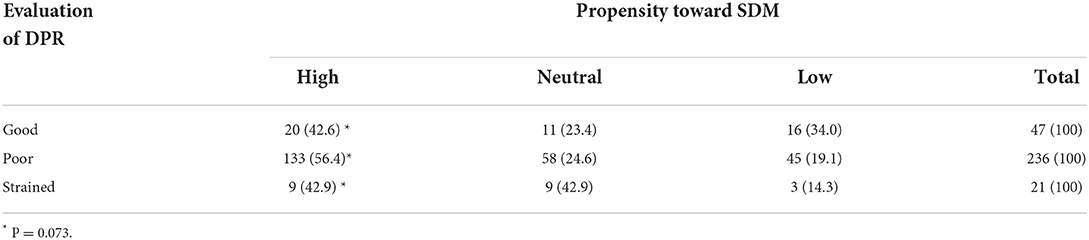
Table 7. Preferences for shared decision-making (SDM) among physicians with different evaluations of doctor–patient relationship (DPR) [n (%)].
As a good clinical decision-making model, SDM has the following characteristics compared with the traditional informational mode and parental mode: physicians and patients both participate in decision-making, equally share information about disease diagnosis and treatment, establish consensus through continuous communication, and, on this basis, reach an agreement regarding the diagnosis and treatment plans (1, 30–33). SDM aims to reduce the differences and discrepancies between physicians and patients, create optimal treatment plans, reduce medical costs, conserve social resources, eliminate doubts, promote enthusiasm for compliance and self-management in patients, and facilitate mutual empathy (2, 4, 7, 34–43), which is of great significance and is the best way to build a medical service system in which physicians and patients act in accord (33, 44–46). Therefore, SDM should be the preferred decision-making model among physicians.
The frequency of medical disputes and violent acts against doctors in recent years deteriorated the DPR (25, 26), making doctors feel insecure and causing them to perceive poor DPR in their medical practice (47). The results of this study showed that physicians generally hold a negative attitude toward DPR, with up to 84.5% of physicians perceiving poor or strained DPR. As one of the main actors in DPR, physicians' evaluations of poor DPR will reduce their sense of professional identity and pride and will cause anxiety, depression, and other negative emotions (48); compromise their occupational satisfaction, sense of self-accomplishment, and subjective well-being; and reduce their investment in their daily work (49, 50). When patients feel that they are being neglected or treated indifferently, they inevitably become dissatisfied and resent their doctors, which exacerbates the already strained DPR and can even result in disputes, thus forming a vicious cycle (51–56). If the situation continues, it is bound to greatly frustrate the orientation of doctors and patients to each other and may affect patients' participation in SDM. To reduce medical risks, avoid medical disputes, and strengthen self-protection, doctors may engage in defensive medical behaviors (57–59), such as performing a wide range of laboratory tests, examinations and treatments; avoiding high-risk surgery and the admission of high-risk patients; providing unnecessary referral options and consultations to pass the buck; concealing the patient's true condition or exaggerating the conditions and the risk of treatment; and intentionally choosing conservative treatments for patients.
In this context, do physicians' evaluations of DPR affect their propensities for SDM in medical practice? A study of physicians' preferences and experiences in clinical decision-making showed that approximately 75% of physicians preferred SDM and that 87% believed that they applied preferred decision-making models (60). The results of this study also showed no overall correlation between physicians' evaluations of poor DPR and their preferences for SDM. Regardless of whether physicians perceived DPR as good or bad, their strong willingness to practice SDM was unaffected. This shows that physicians are fully aware of the importance of SDM; even if they were not optimistic about current DPR, most of them were willing to practice SDM. In the current situation of strained DPR, the strong propensity of physicians toward SDM strongly reflects their high awareness of medical ethics, strong sense of responsibilities and socially desirable behavior, and positive subjective intentions. This finding was validated by the analysis of the reasons why physicians prefer SDM. This result is in line with the principle of respect in medical ethics, which means that physicians and patients should respect each other sincerely in their communication and emphasizes that medical staff should respect patients and their families. That is to say, physicians are required to respect patients' personality rights and autonomy, so as to ensure patients' autonomy to make rational treatment decisions. The essence of independent choice is to respect and maintain the patients' independent rights. Respecting the principle is the necessary condition and reliable foundation to establish a harmonious DPR (61, 62). Poor DPR are the leading reason why physicians are unwilling to practice SDM; given the generally strong propensity toward SDM, poor DPR might affect the choice of only a small number of physicians.
Some scholars believe that the use of SDM can alleviate strained DPR (63–65). This study also found that among the 44 physicians with considerably high preferences for SDM, only 3 (6.8%) believed that DPR were strained, while among the 14 physicians who had extremely low preferences for SDM, 2 (14.3%) believed that DPR were strained, a proportion that was higher than that of the former group. Although a larger sample size is needed to verify this finding, the above data may suggest that SDM is conducive to building harmonious DPR. In future studies, we will expand the sample size, further investigate patients' evaluations of DPR, comprehensively evaluate the evaluations of DPR among physicians and patients and explore whether physicians' adoption of SDM will improve DPR.
Of course, it is worth mentioning that physicians' willingness to practice SDM is not the only factor in this decision-making model that is decisive in achieving desired results and reaching a consensus on diagnosis and treatment in clinical practice. Effective communication between physicians and patients is also a decisive factor, since patients are an important actor involved in SDM. Pollard et al. and Aoki et al. found that although physicians prefer SDM in clinical practice, physicians ultimately make decisions alone (34, 66). This finding indicates that in the clinical decision-making process, the decision-making model that physicians adopt is not always the one they claim to prefer. Although Chinese patients have a stronger intention to participate in decision-making, they are restricted by their educational levels, economic conditions, and medical knowledge (67). Moreover, patients' family members participate in decision-making regarding diagnosis and treatment more frequently than the patients do. Even though Chinese physicians prefer SDM, it is often difficult for them to engage in SDM in actual clinical practice due to the limited participation of patients.
The late start on protecting patients' right to informed consent and the slow promotion of the SDM concept in China is partially responsible for the current situation, while the lack of effective communication between physicians and patients is the leading factor. The modern medical model has changed from the traditional biomedical model to the biopsychosocial medical model. Patients' demands for medical healthcare are diverse, and their willingness to participate in treatment decisions has become increasingly strong. Physicians also perceive the strong willingness of patients and their families to participate in decision-making regarding diagnosis and treatment. Therefore, physicians are willing to practice SDM in their communications with patients. However, the high workload of physicians, insufficient time for communication, and the generally high expectations and requirements of diagnosis and treatment results among patients and their families impose enormous pressure on physicians. Therefore, physicians may fail to communicate with patients harmoniously and effectively in their attempts to practice SDM. Moreover, the rapid development and wide application of high-end medical technology in clinical practice enables physicians to obtain important objective information on patients' conditions using highly sensitive instruments and equipment. As a result, physicians may not be fully aware of patients' information needs. These problems are obstacles to SDM (68). Ineffective outcomes of SDM will result in information asymmetry between physicians and patients. Patients lack information on the efficacy, benefits, and risks of diseases and relevant treatment regimens, and their partial understanding results in unrealistic expectations regarding efficacy and prognosis. Physicians do not fully understand the values, preferences, and family conditions of patients. Under such situations, it is difficult for patients and physicians to cooperatively make the most suitable decisions for patients, which raises the potential risk of doctor–patient conflicts.
Therefore, although strained DPR generally did not affect physicians' preferences for SDM, it may reduce the willingness of some physicians to practice SDM and may affect the final outcomes of SDM. We will expand the sample size and conduct an in-depth investigation and analysis of this issue. Moreover, this study did not include the investigation of patients' evaluations of DPR. The unilateral physicians' evaluations could reflect the true psychological states of physicians DPR, but it might lead to less objective evaluation of DPR tension. We will investigate and compare the evaluations of physicians and patients of DPR in future research, so as to improve the real evaluation of DPR tension. In addition, quantitative assessment such as scores may be used to identify the possible reasons for physicians' evaluations of SDM instead of qualitative evaluation. We will quantify the evaluation method in future research.
Most of physicians have poor evaluations of DPR, but it does not affect their choice tendency for SDM, which may be because of the influence of professional ethics and social desirability bias. Under the current environment of tense DPR, physicians have a strong willingness to make SDM to determine the treatment plan along with the participation of patients and their families.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
LL and Y-WC: conceptualization. Z-RC and Y-HL: data curation. LZ, M-YX, and Y-HL: formal analysis. LZ and Y-WC: investigation. LZ, Y-WC, M-YX, and HJ: project administration. LL: supervision and writing—review and editing. Y-WC: visualization. Z-RC and LZ: writing—original draft. All authors contributed to the article and approved the submitted version.
Author Y-WC was employed by the company Genecast Biotechnology Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (Or it takes at least two to tango). Soc Sci Med. (1997) 44:681–92. doi: 10.1016/S0277-9536(96)00221-3
2. Stiggelbout AM, Pieterse AH, De Haes JC. Shared decision making: concepts, evidence, and practice. Patient Educ Couns. (2015) 98:1172–9. doi: 10.1016/j.pec.2015.06.022
3. Hoffmann TC, Montori VM, Del Mar C. The connection between evidence-based medicine and shared decision making. JAMA. (2014) 312:1295–6. doi: 10.1001/jama.2014.10186
4. Faiman B, Tariman JD. Shared decision making: improving patient outcomes by understanding the benefits of and barriers to effective communication. Clin J Oncol Nurs. (2019) 23:540–2. doi: 10.1188/19.CJON.540-542
5. Zisman-Ilani Y, Roth RM, Mistler LA. Time to support extensive implementation of shared decision making in psychiatry. JAMA Psych. (2021) 78:1183–4. doi: 10.1001/jamapsychiatry.2021.2247
6. Kon AA, Davidson JE, Morrison W, Danis M. American College of Critical Care Medicine, American Thoracic Society. Shared decision making in ICUs: An American College of Critical Care Medicine and American Thoracic Society Policy Statement. Crit Care Med. (2016) 44:188–201. doi: 10.1097/CCM.0000000000001396
7. Dy SM, Purnell TS. Key concepts relevant to quality of complex and shared decision-making in health care: a literature review. Soc Sci Med. (2012) 74:582–7. doi: 10.1016/j.socscimed.2011.11.015
8. Weston WW. Informed and shared decision-making: the crux of patient-centred care. CMAJ. (2001) 165:438–9.
9. Santhirapala R, Moonesinghe R. Primum non nocere: is shared decision-making the answer? Perioper Med. (2016) 5:16. doi: 10.1186/s13741-016-0042-3
10. Gulbrandsen P, Clayman ML, Beach MC, Han PK, Boss EF, Ofstad EH, et al. Shared decision-making as an existential journey: aiming for restored autonomous capacity. Patient Educ Couns. (2016) 99:1505–10. doi: 10.1016/j.pec.2016.07.014
11. Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Légaré F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. (2012) 344:e256. doi: 10.1136/bmj.e256
12. Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor–patient communication about drugs: the evidence for shared decision making. Soc Sci Med. (2000) 50:829–40. doi: 10.1016/S0277-9536(99)00376-7
13. Politi MC, Wolin KY, Légaré F. Implementing clinical practice guidelines about health promotion and disease prevention through shared decision making. J Gen Intern Med. (2013) 28:838–44. doi: 10.1007/s11606-012-2321-0
14. Ruiz Yanzi MV, Barani MS, Franco JVA, Vazquez Peña FR, Terrasa SA, Kopitowski KS. Translation, transcultural adaptation, and validation of two questionnaires on shared decision making. Health Expect. (2019) 22:193–200. doi: 10.1111/hex.12842
15. Ramon S, Quirk AD, Zisman-Ilani Y. Shared decision making in mental health: international perspectives on implementation. Front Psych. (2021) 12:793284. doi: 10.3389/fpsyt.2021.793284
16. Zisman-Ilani Y, Obeidat R, Fang L, Kim YS, Hsieh S, Berger Z. Shared decision making and patient-centered care in Israel, Jordan, and the US: an exploratory and comparative study of physician perceptions. JMIR Format Res. (2020) 4:e18223. doi: 10.2196/18223
17. Salyers MP, Zisman-Ilani Y. Shared decision-making and self-directed care. In: Goldman, H., Frank, R., Morrissey, J. (eds) The Palgrave Handbook of American Mental Health Policy. (2019) pp. 197–228. Palgrave Macmillan, Cham. doi: 10.1007/978-3-030-11908-9_8
18. Patient Decision Aids. Available online at: https://decisionaid.ohri.ca (accessed September 12, 2022).
19. Chinese Medical Doctor Association. Data from: White paper on the practice status of Chinese doctors. (2019). Available online at: www.cmt.com.cn/detail/1331701.html (accessed September 12, 2022).
20. Qiao T, Fan Y, Geater AF, Chongsuvivatwong V, McNeil EB. Factors associated with the doctor–patient relationship: doctor and patient perspectives in hospital outpatient clinics of Inner Mongolia Autonomous Region, China. Patient Prefer Adherence. (2019) 13:1125–43. doi: 10.2147/PPA.S189345
21. Li J, Qi F, Guo S, Peng P, Zhang M. Absence of humanities in China's medical education system. Lancet. (2012) 380:648. doi: 10.1016/S0140-6736(12)61368-3
22. Hou X, Xiao L. An analysis of the changing doctor–patient relationship in China. J Int Bioethique. (2012) 23:83–94. doi: 10.3917/jib.232.0083
23. Zhang X, Sleeboom-Faulkner M. Tensions between medical professionals and patients in mainland China. Camb Q Healthc Ethics. (2011)20:458–465. doi: 10.1017/S0963180111000144
24. Jie L. New generations of Chinese doctors face crisis. Lancet. (2012) 379:1878. doi: 10.1016/S0140-6736(12)60774-0
25. The Lancet. Violence against doctors: Why China? Why now? What next? Lancet. (2014) 383:1013. doi: 10.1016/S0140-6736(14)60501-8
26. The Lancet. Protecting Chinese doctors. Lancet. (2020) 395:90. doi: 10.1016/S0140-6736(20)30003-9
27. Hahn SR. Physical symptoms and physician-experienced difficulty in the physician-patient relationship. Ann Intern Med. (2001) 134:897–904. doi: 10.7326/0003-4819-134-9_Part_2-200105011-00014
28. Wu H, Zhao X, Fritzsche K, Leonhart R, Schaefert R, Sun X, et al. Quality of doctor–patient relationship in patients with high somatic symptom severity in China. Complement Ther Med. (2015) 23:23–31. doi: 10.1016/j.ctim.2014.12.006
29. Yang H. Development and Evaluation of Chinese Version PDRQ/DDPRQ Scale: Quantitative Study of Doctor–patient Relationship (dissertation). Jinzhong: Shanxi Medical University (2011).
30. Charles C, Gafni A, Whelan T. Decision-making in the physician–patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. (1999) 49:651–61. doi: 10.1016/S0277-9536(99)00145-8
31. Pavlo AJ, O'Connell M, Olsen S, Snyder MK, Davidson L. Missing ingredients in shared decision-making? Psychiatr Q. (2019) 90:333–8. doi: 10.1007/s11126-019-9624-9
32. Tonelli MR, Sullivan MD. Person-centred shared decision making. J Eval Clin Pract. (2019) 25:1057–62. doi: 10.1111/jep.13260
33. Korger S, Eggeling M, Cress U, Kimmerle J, Bientzle M. Decision aids to prepare patients for shared decision making: Two randomized controlled experiments on the impact of awareness of preference-sensitivity and personal motives. Health Expect. (2021) 24:257–68. doi: 10.1111/hex.13159
34. Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: a systematic review. Patient Educ Couns. (2015) 98:1046–57. doi: 10.1016/j.pec.2015.05.004
35. Oshima Lee E, Emanuel EJ. Shared Decision Making to Improve Care and Reduce Costs. N Engl J Med. (2013) 368:6–8. doi: 10.1056/NEJMp1209500
36. Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. (2000) 50:892–9.
37. Arab-Zozani M, Moynihan RN, Pezeshki MZ. Shared decision making: How can it be helpful in reducing medical overuse due to medical misinformation mess? J Eval Clin Pract. (2020) 26:602–3. doi: 10.1111/jep.13358
38. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients' preferences matter. BMJ. (2012) 345:e6572. doi: 10.1136/bmj.e6572
39. Kennedy AD, Sculpher MJ, Coulter A, Dwyer N, Rees M, Abrams KR, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes, and costs: a randomized controlled trial. JAMA. (2002) 288:2701–8. doi: 10.1001/jama.288.21.2701
40. Sullivan MD, Leigh J, Gaster B. Brief report: training internists in shared decision making about chronic opioid treatment for non-cancer pain. J Gen Intern Med. (2006) 21:360–2. doi: 10.1111/j.1525-1497.2006.00352.x
41. Sieber W, Newsome A, Lillie D. Promoting self- management in diabetes: efficacy of a collaborative care approach. Fam Syst Health. (2012) 30:322–9. doi: 10.1037/a0030714
42. Hoffman RM, McNaughton-Collins M. The superiority of patient engagement and shared decision-making in noninferiority trials. J Gen Intern Med. (2014) 29:16–7. doi: 10.1007/s11606-013-2593-z
43. Tilburt JC, Wynia MK, Montori VM, Thorsteinsdottir B, Egginton JS, Sheeler RD, et al. Shared decision-making as a cost-containment strategy: US physician reactions from a cross-sectional survey. BMJ Open. (2014) 4:e004027. doi: 10.1136/bmjopen-2013-004027
44. Weiss EM, Clark JD, Heike CL, Rosenberg AR, Shah SK, Wilfond BS, et al. Gaps in the implementation of shared decision-making: illustrative cases. Pediatrics. (2019) 143:e20183055. doi: 10.1542/peds.2018-3055
45. Zisman-Ilani Y, Barnett E, Harik J, Pavlo A, O'Connell M. Expanding the concept of shared decision making for mental health: a systematic and scoping review of interventions. Mental Health Rev J. (2017) 22:191–213. doi: 10.1108/MHRJ-01-2017-0002
46. Zisman-Ilani Y, Chmielowska M, Dixon L, Ramon S. NICE shared decision making guidelines and mental health: challenges for research, practice, and implementation. BJPsych Open. (2021) 7:E154. doi: 10.1192/bjo.2021.987
47. Robinson G. Effective doctor patient communication: building bridges and bridging barriers. Can J Neurol Sci. (2002) 29:30–2. doi: 10.1017/S0317167100001918
48. Zhou X., Pu j, Zhong X, Zhu D, Yin D, Yang L, et al. Burnout, psychological morbidity, job stress, and job satisfaction in Chinese neurologists. Neurology. (2017) 88:1727–35. doi: 10.1212/WNL.0000000000003883
49. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272–81. doi: 10.1016/S0140-6736(16)31279-X
50. Sablik Z, Samborska-Sablik A, Drozdz J. Universality of physicians' burnout syndrome as a result of experiencing difficulty in relationship with patients. Arch Med Sci. (2013) 9:398–403. doi: 10.5114/aoms.2012.28658
51. Montgomery A, Panagopoulou E, Kehoe I, Valkanos E. Connecting organisational culture and quality of care in the hospital: is job burnout the missing link? J Health Organ Manag. (2011) 25:108–23. doi: 10.1108/14777261111116851
52. Shanafelt TD, Gradishar WJ, Kosty M, Satele D, Chew H, Horn L, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. (2014) 32:678–86. doi: 10.1200/JCO.2013.51.8480
53. Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. (2007) 32:203–12. doi: 10.1097/01.HMR.0000281626.28363.59
54. Wen J, Cheng Y, Hu X, Yuan P, Hao T, Shi Y. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci Trends. (2016) 10:27–33. doi: 10.5582/bst.2015.01175
55. Cohen D, Rhydderch M, Reading P, Williams S. Doctors' health: obstacles and enablers to returning to work. Occup Med. (2015) 65:459–65. doi: 10.1093/occmed/kqv056
56. Merrett A, Jones D, Sein K, Green T, Macleod U. Attitudes of newly qualified doctors towards a career in general practice: a qualitative focus group study. Br J Gen Pract. (2017) 67:e253–9. doi: 10.3399/bjgp17X690221
57. Kattel P. Defensive Medicine: Is It Legitimate or Immoral? J Nepal Health Res Counc. (2019) 16:483–5. doi: 10.33314/jnhrc.v16i41.1828
58. Carroll AE. The High Costs of Unnecessary Care. JAMA. (2017) 318:1748–9. doi: 10.1001/jama.2017.16193
59. Brenno LC. Defensible medicine: an effective response to the malpractice liability crisis. Minn Med. (1987) 70:139–41.
60. Murray E, Pollack L, White M, Lo B. Clinical decision-making: physicians' preferences and experiences. BMC Fam Pract. (2007) 8:10. doi: 10.1186/1471-2296-8-10
61. Gillon R. Defending the four principles approach as a good basis for good medical practice and therefore for good medical ethics. J Med Ethics. (2015) 41:111–6. doi: 10.1136/medethics-2014-102282
62. Gillon R. Ethics needs principles—four can encompass the rest–and respect for autonomy should be ‘first among equals'. J Med Ethics. (2003) 29:307–12. doi: 10.1136/jme.29.5.307
63. Carman KL, Dardess P, Maurer M. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff Millwood. (2013) 32:223–31. doi: 10.1377/hlthaff.2012.1133
64. Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. (2007) 335:24–7. doi: 10.1136/bmj.39246.581169.80
65. Charmel PA, Frampton SB. Building the business care for patient-centered care. Healthe Finacnc Manage. (2008) 62:80–5.
66. Aoki A, Ohbu S. Japanese physicians' preferences for decision making in rheumatoid arthritis treatment. Patient Prefer Adherence. (2016) 10:107–13. doi: 10.2147/PPA.S95346
67. Chen JJ, Tian M. Analysis of the problems and solutions for the joint decision-making of doctors and patients. Medicine and Philosophy (Chinese). (2018) 39:10–2. doi: 10.4018/IJDSST.2018010103
Keywords: shared decision-making, doctor–patient relationship, physician, China, patient decision aid
Citation: Chen Z-R, Zhang L, Chen Y-W, Xu M-Y, Jia H, Li M-Y, Lou Y-H and Lan L (2022) Correlation analysis between physicians' evaluations of doctor–patient relationship and their preferences for shared decision-making in China. Front. Psychiatry 13:946383. doi: 10.3389/fpsyt.2022.946383
Received: 17 May 2022; Accepted: 05 September 2022;
Published: 05 October 2022.
Edited by:
Aliya Naheed, International Center for Diarrhoeal Disease Research (icddr,b), BangladeshReviewed by:
Yaara Zisman-Ilani, Temple University, United StatesCopyright © 2022 Chen, Zhang, Chen, Xu, Jia, Li, Lou and Lan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Lan, bGFubGluZzk1QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.