
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 29 August 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.942782
This article is part of the Research Topic Global Excellence in Public Mental Health: Asia and Australasia Volume II View all 13 articles
Background: To date, few empirical studies have examined the clinical characteristics of suicide attempts (SA) in individuals with borderline personality disorder (BPD) in China.
Aims: To examine the prevalence and factors associated with SA in Chinese individuals with BPD.
Methods: In this cross-sectional study, 84 patients with BPD were recruited from a large public psychiatric hospital in Wuhan, China, between 2013 and 2015. Trained experienced psychiatrists interviewed participants to collect clinical data, including demographics, axis I and axis II diagnoses of mental disorders according to the DSM-IV-TR, number of hospitalizations, and history of SA. An interview outline was used to identify the existence of lifetime SA. In addition, the Beck Depression Inventory-II, Buss & Perry Aggression Questionnaire, Child Trauma Questionnaire-Short Form, and Beck Hopelessness Scale were administered to assess respondents’ depressive symptoms, aggression, childhood traumatic experiences, and hopelessness.
Results: Fifty-two (61.9%) patients reported attempting suicide during their lifetime. Univariate logistic regression analysis screened 7 factors associated with SA in individuals with BPD into Multiple logistic regression analysis: female sex, unemployment, major depressive disorder (MDD), hostility, self-aggression, depressive symptoms, and emotional neglect. Multiple logistic regression analysis identified 3 significant and independent correlates of SA: MDD [odds ratio (OR) = 26.773, 95% confidence interval (CI) = 3.914–183.132, P = 0.001], hostility (OR = 1.073, CI = 1.019–1.130, P = 0.007), and self-aggression (OR = 1.056, CI = 0.998–1.119, P = 0.060).
Conclusion: Chinese individuals with BPD have a high risk of suicide. Correlates of SA in this population differ to some extent from those in Western populations as reported in the literature. Paying attention to MDD and some types of aggression in Chinese individuals with BPD may help identify their risk of suicide. Future large-sample cohort study may improve the limitations of this study and further confirm the point of view above.
The main characteristics of borderline personality disorder (BPD) include a pervasive pattern of emotion dysregulation, inconsistent identity, and disturbed interpersonal function, as indicated by five (or more) of the following: fear of abandonment, unstable relationships, unstable self-image, impulsivity, recurrent suicide/self-harm, mood instability, feelings of emptiness, inappropriate anger, dissociation/transient paranoid ideation (1). BPD is the most common personality disorder in both clinical and non-clinical settings in Western countries, with a prevalence of approximately 10–25% (2, 3) and 0.7–5.9% (4–6) in clinical and non-clinical populations, respectively. In China, a multicenter study reported that the prevalence of BPD reached 9.9% in psychiatric treatment settings (7). BPD is a serious personality disorder that can cause severe social function impairments, and it is associated with a high risk of suicide. It has been documented that approximately 50–75% of patients with BPD have attempted suicide (8, 9); in addition, each of these patients has attempted suicide more than three times during their lifetime (10). Repetitive suicidal behaviors in patients with BPD are sometimes misinterpreted as merely a form of threat or manipulation in clinical practice. However, since suicide attempts (SA) lead to a greater risk of completed suicide than expected (11), it is a significant clinical concern in patients with BPD.
Several factors were probably associated with SA in patients with BPD, such as comorbidities of other mental disorders, personality traits, childhood abuse, some demographic characteristics, and other factors; however, studies have shown inconsistent results to some extent (10, 12–20). Many studies on BPD indicated that there were significant associations between SAs and affective disorders, especially depressive disorders (10, 14, 17). However, few found that a comorbid diagnosis of major depression had only a short-term effect or little effect on suicide risk in patients with BPD (18, 19). One study even suggested further that risk factors for SA include state depression (e.g., depressed symptoms), but not comorbid affective disorder (18). Similarly, substance abuse is common among suicide attempters with BPD (13, 14); however, some studies have found no associations between substance abuse and SA in these patients (18, 20). Another possible associated factor is the personality traits of patients with BPD, such as aggression, anger, hostility, and impulsivity (10, 12, 13, 15, 17, 19); but negative results have also been reported (20). Moreover, childhood abuse, especially sexual abuse, was considered correlated with SA in patients with BPD (15, 16). Low socioeconomic status, age, hospitalization, and poor psychosocial functioning have also been classified as risk factors for SA in patients with BPD (16, 19, 20).
As mentioned above, the data for clinical characteristics of suicidal behaviors in individuals with BPD are mainly derived from Western countries, and there are still some inconsistent findings. In China, to the best of our knowledge, few empirical studies have been conducted to examine the clinical epidemiology of SA in patients with BPD in China. From the few research data in China (7), it can be inferred that the number of Chinese patients in with BPD may be huge, and the suicidal behavior of this population is a clinical problem that cannot be ignored. Considering the clinical importance of suicide prevention and management of suicidal risk in patients with BPD, we investigated the prevalence and correlates of SA in patients with BPD from a large public psychiatric hospital in central China.
Participants were selected from patients treated at Wuhan Mental Health Center over a period of 2 years from 2013 to 2015. This center is the largest public psychiatric specialty hospital in Wuhan, central China, with over 1,000 inpatient beds. Patients with confirmed clinical diagnosis of BPD, according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) (21), aged between 18 and 60 years, and received treatments at the hospital during the study period were consecutively invited to join the study. Patients with severe physical diseases, including neurological diseases, such as epilepsy, were excluded. Two experienced psychiatrists assessed their eligibility and invited eligible patients to participate in the study.
Trained investigators interviewed patients in a standardized manner, aiming to collect demographic information (sex, age, educational background, occupation, and marital status), axis I diagnoses of DSM-IV-TR, number of hospitalizations, and the outcome of this study, lifetime SA. An interview outline was used to identify the existence of lifetime SA, which mainly included four questions: (1) Have you ever self-injured or suicided, such as taking medicine or cutting your wrists? (2) How many times? (3) What specific methods were used? (4) How much did you want to die while doing these things? If the patient answered yes to question 1 and was able to describe in detail at least one suicidal behavior with thoughts of death, SA was present; Otherwise, SA was absent.
All participants completed 4 validated Chinese self-rating scales: Buss and Perry Aggression Questionnaire (BP-AQ) (22), Beck Depression Inventory-II (BDI-II) (23), Child Trauma Questionnaire-Short Form (CTQ-SF) (24), and Beck Hopelessness Scale (BHS) (25). BP-AQ was used to assess personality characteristic of aggression. It consisted of 30 items, with five subscales: physical aggression, anger, verbal aggression, hostility, and self-aggression. The CTQ-SF was used to assess childhood abuse and consisted of 28 items in five subscales: emotional abuse, sexual abuse, physical abuse, physical neglect, and emotional neglect. BDI-II and BHS were used to rate the levels of depressive symptoms and hopelessness, respectively.
Descriptive statistics and univariate and multivariate logistic regression analyses were performed. In the univariate logistic regression analysis, the presence or absence of SA was considered as the outcome variable, while the above demographic, psychosocial, and clinical variables were considered as the independent variables. Significant factors identified in the univariate analysis were included into the multivariate logistic regression analysis. Forward stepwise regression based on maximum likelihood estimation was used to identify independent factors associated with SA in patients with BPD. The 95% confidence intervals (CIs) and odds ratios (ORs) were used to quantify the association between the factors and SA. The statistical significance level was set at two-sided P < 0.05. All analyses were performed using IBM SPSS 20.0 (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.).
During the study period, a total of 355 patients with BPD met the inclusion and exclusion criteria, of which 84 patients agreed to participate in the study and completed the questionnaires, and all questionnaires were qualified for the analysis. Among the 84 patients with BPD, the age ranged from 18 to 38 years (mean age, 24.6 ± 5.5 years), and 52 (61.9%) had attempted suicide before the interview. Other clinical characteristics and demographic data are shown in Table 1.
The univariate logistic regression analysis (Table 2) revealed that there were 7 factors associated with SA in patients with BPD, namely female sex, unemployment, major depressive disorder (MDD), hostility, self-aggression, depressive symptoms, and emotional neglect.
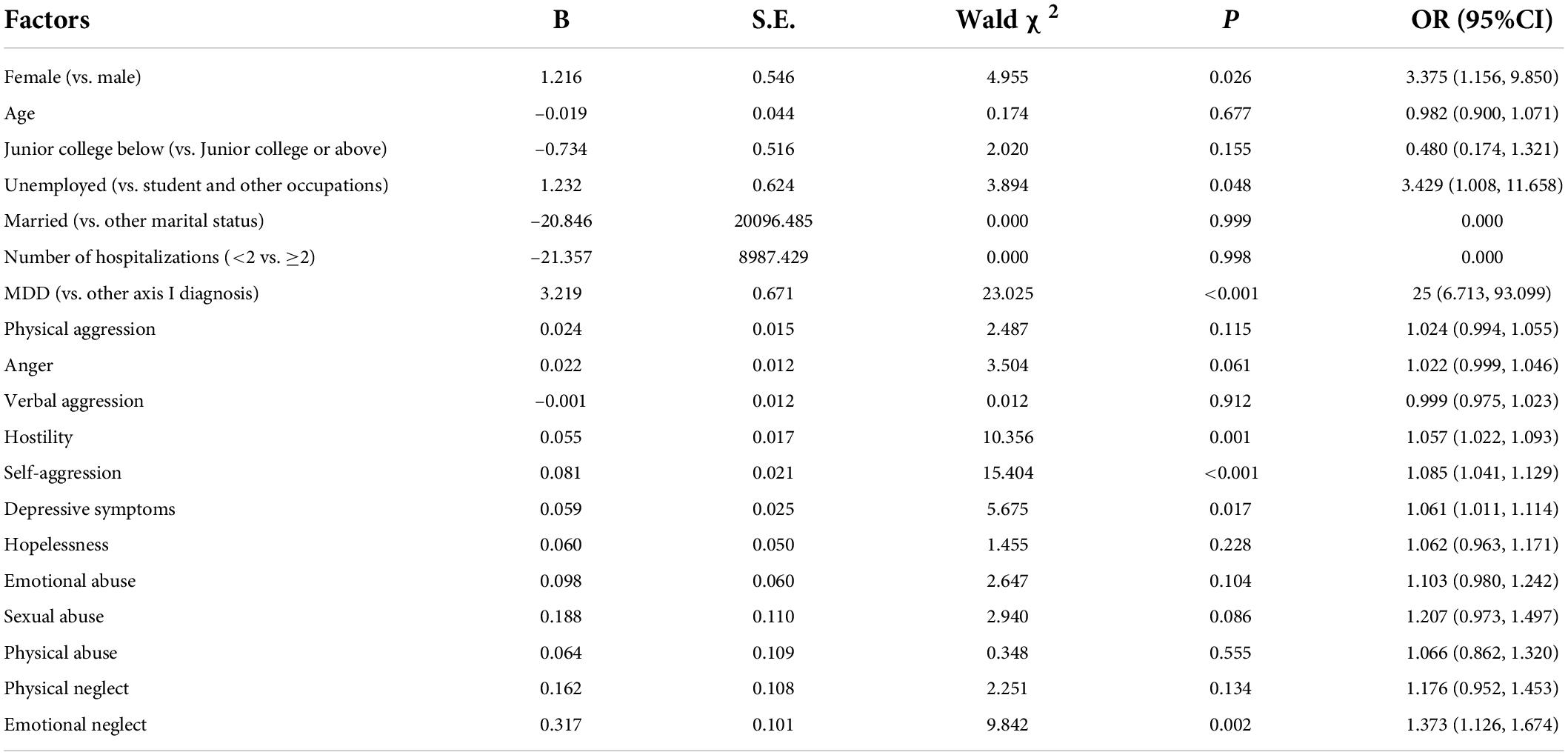
Table 2. Results of the univariate logistic regression analysis on the factors correlated with suicide attempt (SA) in BPD patients.
The final model of multivariate logistic regression analysis (Table 3) identified three correlates significantly and independently associated with SA in BPD patients: MDD (OR = 26.773, CI = 3.914–183.132, P = 0.001), hostility (OR = 1.073, CI = 1.019–1.130, P = 0.007), and self-aggression (OR = 1.056, CI = 0.998–1.119, P = 0.060).
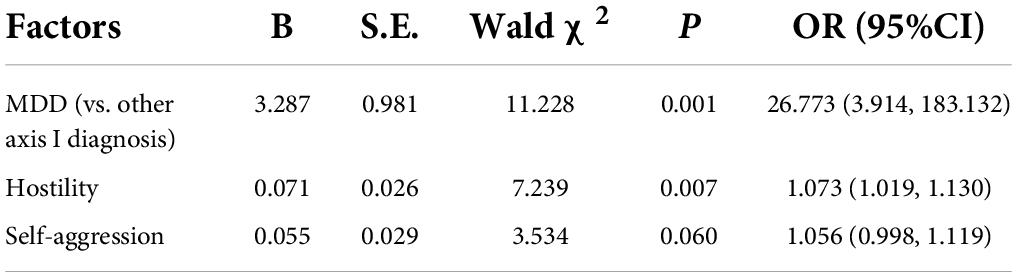
Table 3. Results of the multivariate logistic regression analysis on the factors correlated with SA in BPD patients.
To the best of our knowledge, this is the first study to examine SA and its associated factors in individuals with BPD in China. The results showed that the lifetime prevalence of SA in Chinese patients with BPD was 61.9%, which is consistent with the high rate reported in Western countries (8, 9). The significant correlates of SA in this patient population were MDD and self-aggression, partly replicating the findings from Western studies (10, 12–15, 17, 19). Meanwhile, it was preliminarily speculated from other inconsistent results that some of the differences might be related to different cultures and regions.
MDD, as a typical and severe type of depressive disorder, has been associated with SA in patients with BPD, which was also found in our study (10, 14, 17). Compared with depressive state and temporary psychological symptoms, MDD refers to more profound and persistent mood problems, and patients may eventually assume that suicide is the only way to end their painful lives. This accords with the characteristics of repeated SAs in patients with BPD. They tend not to present only occasionally suicidal impulses or depressive state. Understandably, the correlations of current depressive and hopeless symptoms to SA in this patient population were not found in this study, although previous studies had the opposite results (10, 18). In addition, no association between comorbidities of other mental disorders and SA in patients with BPD was found in this study, which may be partly due to the small number of cases with comorbidities of other mental disorders. Although this is inconsistent with some Western studies (13, 14), it supports the findings of a large sample study in Shanghai, another China city: depressive disorder is the most common axis I disorder in BPD clinical samples, while substance abuse is rare (26). The DSM-IV includes substance abuse in the diagnostic criteria for BPD as one of the self-damaging impulsive behaviors, but many drugs are tightly controlled in China, which greatly limits their availability.
Furthermore, aggression, especially hostility and self-aggression, are also significant correlates of SA in patients with BPD, partly replicating the findings of previous studies (10, 12, 13, 15, 17). From the psychopathology of BPD, the hate for important objects caused by severe psychological trauma in the early years and the symbiotic relationship with those objects leads to frequent no-boundary dissatisfaction and violence against others and oneself, and the extreme result is suicide. Specifically, most items of hostility involved the defense mechanism of projection, a paranoid belief that the outside world is bad, while refusing to acknowledge inner bad feelings. More importantly, self-aggression subscale was all about intentional or unintentional self-harm or self-punishment, which was conceptually related to SA. Therefore, this factor was still retained as a correlate of SA in this study, although its significance was borderline. In contrast, impulsiveness, another personality trait of BPD, was not included in this study on the basis of the possibility of overlap between aggression and impulsiveness (27, 28), and aggression might be more relevant to suicide in patients with BPD (10, 13).
The effect of childhood abuse was not shown in this study, and even sexual abuse, considered by some studies to be the strongest predictor of SA in patients with BPD (15, 16), was not found to be associated. Talking about sex is more of a taboo in Eastern cultures than in Western ones, and this is also true among people with mental disorders (29, 30), which may mask the role sexual abuse plays in such patients. However, why other types of abuse were not associated with SA requires further clarification. In addition, patients’ ages and number of hospitalizations were also not associated with SA in this study, which was not consistent with the results of some other BPD studies (16, 20). Most patients were young (under 38 years), which is in line with a significant decline in the prevalence of patients with BPD over 40 years (31), and most patients were repeatedly hospitalized, which is consistent with some studies (32, 33). This may be explained by repeated hospitalizations as a way to escape from daily life, while symptoms of the personality disorder tend to ease with age. Therefore, it may result in failure to distinguish differences in SA among patients of different ages and hospitalizations in this study.
This study had some limitations. First, the participants were clinical patients from a psychiatric hospital in a city in central China, and the sample size was relatively small, which suggested that the findings should be explained with considerable caution. Second, the cross-sectional nature of the study did not permit an examination of causality. Third, as this was a preliminary study, research tools require improving, and certain data require further collection and analysis, such as using a structured interview to improve the detection rate of BPD, comparing it with the results of a new dimension system in the diagnosis for personality disorders (DSM-5 or ICD-11), and investigating the family history of suicide, psychosocial functioning, frequency of SA and other factors. Future research, conducting a relatively large cohort study to compare suicide risk among patients at different time points, use improved diagnostic tools, collect more clinical variables, and collect patient data in community populations as controls, should address most of the limitations of this study.
The high prevalence of SA in Chinese individuals with BPD suggests a significant risk of suicide in this population in China. The suicidal behavior of Chinese patients with BPD is more likely to accompany with MDD and personality characteristics of hostility and self-aggression, but is not related to substance abuse, childhood sexual abuse and other factors as reported by Western studies. Paying attention to MDD and some types of aggression in Chinese individuals with BPD may help identify their risk of suicide. However, given the small sample size, the results should be interpreted with caution. Future large-sample cohort studies incorporating community population sampling and optimizing research tools may further refine the limitations of this study.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Wuhan Health and Family Planning Commission [approval number (2013)9, 5/12/2013]. The patients/participants provided their written informed consent to participate in this study.
FY and JT contributed to the conceptualization. JZ and S-FZ investigated patients and conducted project administration. B-LZ analyzed and interpreted the data. FY and S-FZ wrote the draft of the manuscript. B-LZ, JZ, and JT revised and edited the manuscript. FY acquired funding. B-LZ and JT provided supervision. All authors contributed to the article and approved the submitted version.
This study was funded by the Wuhan Municipal Health Commission (grant no. WX19Q43), the Health Commission of Hubei Province Scientific Research Project (grant no. WJ2019M015), and the Health Commission of Hubei Province Scientific Research Project (grant no. WJ2019H390).
We thank Editage (www.editage.cn) for English language editing. We also thank Research Square for presenting the preprint (34).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Psychiatric Association. Diagnostic and Statistical Manual Of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596.893619
2. Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. (2011) 377:74–84. doi: 10.1016/S0140-6736(10)61422-5
3. Ellison WD, Rosenstein LK, Morgan TA, Zimmerman M. Community and clinical epidemiology of borderline personality disorder. Psychiatr Clin North Am. (2018) 41:561–73. doi: 10.1016/j.psc.2018.07.008
4. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. (2018) 21:28–32. doi: 10.1016/j.copsyc.2017.09.001
5. Ten Have M, Verheul R, Kaasenbrood A, van Dorsselaer S, Tuithof M, Kleinjan M, et al. Prevalence rates of borderline personality disorder symptoms: a study based on the Netherlands Mental Health Survey and Incidence Study-2. BMC Psychiatry. (2016) 16:249. doi: 10.1186/s12888-016-0939-x
6. Zanarini MC, Horwood J, Wolke D, Waylen A, Fitzmaurice G, Grant BF. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. J Pers Disord. (2011) 25:607–19. doi: 10.1521/pedi.2011.25.5.607
7. Lai CM, Leung F, You J, Cheung F. Are DSM-IV-TR borderline personality disorder, ICD-10 emotionally unstable personality disorder, and CCMD-III impulsive personality disorder analogous diagnostic categories across psychiatric nomenclatures? J Pers Disord. (2012) 26:551–67. doi: 10.1521/pedi.2012.26.4.551
8. Goodman M, Tomas IA, Temes CM, Fitzmaurice GM, Aguirre BA, Zanarini MC. Suicide attempts and self-injurious behaviours in adolescent and adult patients with borderline personality disorder. Pers Ment Health. (2017) 11:157–63. doi: 10.1002/pmh.1375
9. Soloff PH, Chiappetta L. 10-year outcome of suicidal behavior in borderline personality disorder. J Pers Disord. (2019) 33:82–100. doi: 10.1521/pedi_2018_32_332
10. Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry. (2000) 157:601–8. doi: 10.1176/appi.ajp.157.4.601
11. Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. Am J Psychiatry. (2016) 173:1094–100. doi: 10.1176/appi.ajp.2016.15070854
12. Barteček R, Hořínková J, Linhartová P, Kašpárek T. Emotional impulsivity is connected to suicide attempts and health care utilization in patients with borderline personality disorder. Gen Hosp Psychiatry. (2019) 56:54–5. doi: 10.1016/j.genhosppsych.2018.11.008
13. Baus N, Fischer-Kern M, Naderer A, Klein J, Doering S, Pastner B, et al. Personality organization in borderline patients with a history of suicide attempts. Psychiatry Res. (2014) 218:129–33. doi: 10.1016/j.psychres.2014.03.048
14. Black DW, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. (2004) 18:226–39. doi: 10.1521/pedi.18.3.226.35445
15. Ferraz L, Portella MJ, Vállez M, Gutiérrez F, Martín-Blanco A, Martín-Santos R, et al. Hostility and childhood sexual abuse as predictors of suicidal behaviour in borderline personality disorder. Psychiatry Res. (2013) 210:980–5. doi: 10.1016/j.psychres.2013.07.004
16. Rodante DE, Grendas LN, Puppo S, Vidjen P, Portela A, Rojas SM, et al. Predictors of short- and long-term recurrence of suicidal behavior in borderline personality disorder. Acta Psychiatr Scand. (2019) 140:158–68. doi: 10.1111/acps.13058
17. Sher L, Fisher AM, Kelliher CH, Penner JD, Goodman M, Koenigsberg HW, et al. Clinical features and psychiatric comorbidities of borderline personality disorder patients with versus without a history of suicide attempt. Psychiatry Res. (2016) 246:261–6. doi: 10.1016/j.psychres.2016.10.003
18. Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R. Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatry. (1994) 151:1316–23. doi: 10.1176/ajp.151.9.1316
19. Soloff PH, Chiappetta L. Suicidal behavior and psychosocial outcome in borderline personality disorder at 8-year follow-up. J Pers Disord. (2017) 31:774–89. doi: 10.1521/pedi_2017_31_280
20. Soloff PH, Chiappetta L. Prospective predictors of suicidal behavior in BPD at 6 year follow-up. Am J Psychiatry. (2012) 169:484–90. doi: 10.1176/appi.ajp.2011.11091378
21. American Psychiatric Association. Diagnostic and Statistical Manual Of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association (2000). doi: 10.1176/appi.books.9780890423349
22. Li XY, Phillips MR, Zhang YL, Niu YJ, Tong YS, Yang SJ. Development, reliability and validity of the Chinese version of Buss & Perry Aggression Questionnaire. Chin J Nerv Ment Dis. (2011) 37:607–13. doi: 10.3969/j.issn.1002-0152.2011.10.010
23. Wang Z, Yuan CM, Huang J, Li ZZ, Chen J, Zhang HY, et al. Reliability and validity of the Chinese version of Beck Depression Inventory-II among depression patients. Chin Ment Health J. (2011) 25:476–80. doi: 10.3969/j.issn.1000-6729.2011.06.014
24. He J, Zhong X, Gao Y, Xiong G, Yao S. Psychometric properties of the Chinese version of the Childhood Trauma Questionnaire-Short Form (CTQ-SF) among undergraduates and depressive patients. Child Abuse Negl. (2019) 91:102–8. doi: 10.1016/j.chiabu.2019.03.009
25. Zhang WC, Jia CX, Hu X, Qiu HM, Liu XC. Beck hopelessness scale: psychometric properties among rural Chinese suicide attempters and non-attempters. Death Stud. (2015) 39:442–6. doi: 10.1080/07481187.2014.970300
26. Wang L, Ross CA, Zhang T, Dai Y, Zhang H, Tao M, et al. Frequency of borderline personality disorder among psychiatric outpatients in Shanghai. J Pers Disord. (2012) 26:393–401. doi: 10.1521/pedi_2012_26_008
27. Buss AH, Perry M. The aggression questionnaire. J Pers Soc Psychol. (1992) 63:452–9. doi: 10.1037/0022-3514.63.3.452
28. Critchfield KL, Levy KN, Clarkin JF. The relationship between impulsivity, aggression, and impulsive-aggression in borderline personality disorder: an empirical analysis of self-report measures. J Pers Disord. (2004) 18:555–70. doi: 10.1521/pedi.18.6.555.54795
29. Kim D, Park SC, Yang H, Oh DH. Reliability and validity of the Korean version of the childhood trauma questionnaire-short form for psychiatric outpatients. Psychiatry Investig. (2011) 8:305–11. doi: 10.4306/pi.2011.8.4.305
30. Xie P, Wu K, Zheng YJ, Guo YB, Yang YL, He JF, et al. Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. J Affect Disord. (2018) 228:41–8. doi: 10.1016/j.jad.2017.11.011
31. Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K, et al. Borderline personality disorder. Lancet. (2021) 398:1528–40. doi: 10.1016/s0140-6736(21)00476-1
32. Romanowicz M, Schak KM, Vande Voort JL, Leung JG, Larrabee BR, Palmer BA. Prescribing practices for patients with borderline personality disorder during psychiatric hospitalizations. J Pers Disord. (2020) 34:736–49. doi: 10.1521/pedi_2019_33_405
33. Pec O, Bob P, Pec J, Ludvikova I. Psychodynamic day treatment program for borderline personality disorder: factors that predict outcome and dropout. Medicine. (2021) 100:e25186. doi: 10.1097/md.0000000000025186
34. Yang F, Li G, Zhang S, Jun T. Prevalence and Correlates of Suicide Attempt in Chinese Patients With Borderline Personality Disorder. Research Square [Preprint]. (2020). Available online at: https://www.researchsquare.com (accessed December 28, 2020).
Keywords: borderline personality disorder, suicide attempt, prevalence, factors, clinical characteristics
Citation: Yang F, Tong J, Zhang S-F, Zhang J and Zhong B-L (2022) Prevalence and correlates of suicide attempts in Chinese individuals with borderline personality disorder. Front. Psychiatry 13:942782. doi: 10.3389/fpsyt.2022.942782
Received: 09 June 2022; Accepted: 11 August 2022;
Published: 29 August 2022.
Edited by:
Liye Zou, Shenzhen University, ChinaCopyright © 2022 Yang, Tong, Zhang, Zhang and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juan Zhang, anVhbnpoYW5nZGRAMTYzLmNvbQ==; Bao-Liang Zhong, aGFpemhpbGFuQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.