
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 September 2022
Sec. Sleep Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.940741
This article is part of the Research Topic Interaction Between Neuropsychiatry and Sleep Disorders: from Mechanism to Clinical Practice View all 19 articles
 Qianqian Xin1,2†
Qianqian Xin1,2† Dhirendra Paudel3†
Dhirendra Paudel3† Kai An4
Kai An4 Youran Ye1,2
Youran Ye1,2 Shuqiong Zheng1,2
Shuqiong Zheng1,2 Lei Chen5
Lei Chen5 Bin Zhang1,2*
Bin Zhang1,2* Honglei Yin1,2*
Honglei Yin1,2*Objective: To find publications trend about cognitive behavior therapy for insomnia (CBTI) using bibliometric and visualization analysis. In this study, the authors sought to identify the publication trends of peer-reviewed articles about CBTI.
Materials and methods: Analyses were focused on the past 18 years from 2004 to 2021. All searches were performed on the Web of Science Core Collection database. The search was repeated to include structural cognitive behavior therapy for insomnia. Quantitative analysis was assessed using the bibliometric tool. Visualization analysis was carried out using VOSviewer.
Results: In the 736 articles reviewed, the number of publications has been increasing every year for the past 18 years. Behavioral sleep medicine and sleep were the most active journals published on CBTI. The United States and Canada had the highest scientific publications in the field. Morin CM and Espie CA were the most active authors. The study type mostly observed were randomized controlled trials, meta-analyses, and epidemiological. Publications on digital-based cognitive behavior therapy and accessibility to primary care settings represent the future trends of research on CBTI.
Conclusion: Possible explanations for CBTI publication trends were discussed, including the emergence of the evidence-based therapy, feasibility, and scalability. Potential CBTI publications trends in the future and clinical implications were also discussed.
Cognitive Behavior Therapy for Insomnia (CBTI) is a psychotherapeutic approach to treating insomnia that includes cognitive, behavioral, and educational components (1). Cognitive content in CBTI attempts to change dysfunctional beliefs about sleep often termed cognitive restructuring. Behavioral content in CBTI consist of relaxation training (such as deep breathing exercises, progressive muscle relaxation, hypnosis, and/or meditation), stimulus control (changing the association of bedtime habit making sleep difficulties, like eating, watching TV, or using a cell phone or computer) (2), and sleep restriction (limits time spent in bed during the day and/or night to reestablish a consistent sleep schedule). Psychoeducation about the connection between feelings, thoughts, behaviors, and sleep is central to CBTI which is often aided by a sleep diary. Although CBTI lasts between 6–8 sessions (3), the length may vary according to the provider and person’s needs. Treatment may be as short as two sessions when given by a primary care provider (4), furthermore, there were reports of single-shot CBTI and its effectiveness in literature. Although cognitive therapy and behavioral therapy alone are effective, patients will experience the greatest benefit when all components of CBTI are combined with an 8-week course (5).
Insomnia is a major public health concern with a prevalence of about 10–20% (6). There are both pharmacological (such as benzodiazepines, z-drugs, melatonin, antidepressants, antipsychotics, and antihistamines) and non-pharmacological treatments (sleep hygiene, cognitive behavior therapy, relaxation therapy, multicomponent therapy, and paradoxical intention) available for insomnia (7). CBTI is one of the effective non-pharmacological treatments which can be applied to primary insomnia or comorbid insomnia in chronic conditions without the fear of drug interaction. However, due to the lack of trained clinicians, the uneven geographic distribution of knowledgeable professionals, and high costs, CBTI is an effective but underutilized treatment for insomnia (8).
Bibliometrics is a statistical method which provides researchers with qualitative and quantitative characteristics of literature by analyzing measurement indicators such as countries, journals, institutions, authors, and keywords, to describe current trends and discover the field hotspots. Bibliometric analysis has made a great contribution to the development of treatment and clinical guidelines (9). Therefore, this study intends to use bibliometrics to analyze the research status and research hotspots of CBTI, to lead the direction for related fields in the future.
The criteria for considering studies for this bibliometric analysis are described below.
The papers published between the years 2004 and 2021 relevant to cognitive behavior therapy for insomnia were included. A detailed search strategy was developed for this study, and two researchers (QX and DP) in the field conducted article screening. Having more than one screener ensures the elimination of bias and errors in methodology resulting in data of high quality. The bibliometric and visualization analysis was done.
The current study aimed to examine possible trends in the volume of peer-reviewed publications on cognitive behavioral interventions for insomnia across time and to assess the evolution of such trends.
Data retrieval for this study was conducted on March 30, 2022. Data are drawn from the Web of Science Core Collection (WOSCC) using the Science Citation Index Expanded, the Social Science Citation Index, the Arts, and Humanities Citation Index, and the Emerging Sources Citation Index (SCIE, SSCI, AHCI, and ESCI) for the period of 18 years (2004–2021). Documents for analysis were restricted to original academic journal contributions (i.e., articles and reviews) which we will refer to as “papers.” Figure 1 shows the adapted Prisma flow diagram for the study (10).
After multiple iterations and using wildcards the following 2 concepts were used as topic search terms: concept 1, Cognitive Behavior Therapy (TS = (“cogniti* behavio* therap*”) OR Behavior Therapy (TS = (“behavio* therap*” OR “behavio* psychotherap*”) AND Cognitive Therapy (TS = (“cogniti* therap*” OR “cogniti* psychotherap*”) AND concept 2, insomnia (TS = (insomnia OR sleep Initiation and maintenance disorder* OR disorder* of initiating and maintaining sleep OR primary insomnia OR transient insomnia OR chronic insomnia OR secondary insomnia OR sleeplessness OR insomnia disorder* OR sleep wake disorder* OR sleep initiation dysfunction)).
Criteria for inclusion of a paper were as follows: (a) the main problem statement was insomnia (primary or comorbid), (b) the type of study was empirical, replication or review, and (c) the treatment condition used or main theme of the review was therapy consisting of both cognitive and behavioral in content.
As such the final included papers are relevant to cognitive behavior therapy for insomnia (CBTI). And those articles comparing behavior therapy and cognitive therapy for insomnia populated with boolean search strategies were excluded.
Papers on Cognitive Behavior Therapy for insomnia.
Number of publications, distribution of journals, the contribution of authors, institutions, and countries, top-cited papers, and keyword co-occurrences.
The Bibliometrix (11), an R package for bibliometric analysis was used to analyze the annual scientific productions, citation counting, journal, author, institution, and country distribution. The VOSviewer is visualization software that constructs a visualization network map from the co-occurrence of keywords (12).
The study included a total of 736 papers on CBTI. The number of annual publication papers increased every year, from 11 papers in 2004 to 138 in 2021. The study included papers on randomized clinical/controlled trials (RCT) (307), original research other than RCT (234), meta-analysis with systematic reviews (32), meta-analyses (19), systematic reviews (31) and reviews other than systematic reviews and meta-analysis (113). Figure 2 shows yearly trends and top 10 journals publishing CBTI papers from 2004 to 2021.
Cognitive behavior therapy for insomnia papers were distributed in 236 journals. Sleep published the most papers (62/736, 8.42%), followed by Behavioral Sleep Medicine (52/736, 7.07%). The highest impact factors (IF) and h-index were observed with Sleep (IF: 5.849, h-index: 35) and Sleep Medicine Reviews (IF:11.609, h-index:21) (Table 1). Table 1 listed the top 10 journals according to volumes of publications on CBTI.
There were 957 institutions that participated in the CBTI papers. Table 2 presented the top 10 institutions that contributed papers on CBTI. The University of Laval published the most papers (79/736, 10.73%), followed by the University of Pennsylvania (68/736, 9.24%) (Table 3).
Only 33 countries around the globe contributed to papers on CBTI. Table 3 shows the top 10 countries that published papers on CBTI. The United States published the most articles (296/736,40.22%), followed by Canada (62/736,8.42%) (Table 3).
The study identified 2,783 authors contributing to CBTI papers. Table 2 presented the top 10 authors with the highest yields of CBTI studies. Morin CM had the most papers (38/736, 5.16%), followed by Espie CA (34/736, 4.62%). Espie CA and Morin CM had the highest h-index of 21 and 19, respectively (Table 2).
Out of the top 10 cited papers in this study (Table 4), four were practical recommendations for the management of insomnia. One was a pilot study done on depression co-morbidity. One was a review on the relationship between sleep and pain. Two were meta-analyses on cognitive behavior therapy for insomnia. And two were a randomized controlled trial on CBT vs. z-drug (viz Zopiclone and Zolpidem) for insomnia.
The research directions of CBTI publications collected by WoS were divided into five clusters (Figure 3). The top ten keywords as detected by VOSviewer were insomnia (n = 460), cognitive behavioral therapy (n = 358), sleep (n = 227), depression (n = 174), meta analysis (n = 167), efficacy (n = 161), validation (n = 131), older-adults (n = 121), severity index (n = 114) and randomized controlled trial (n = 102).
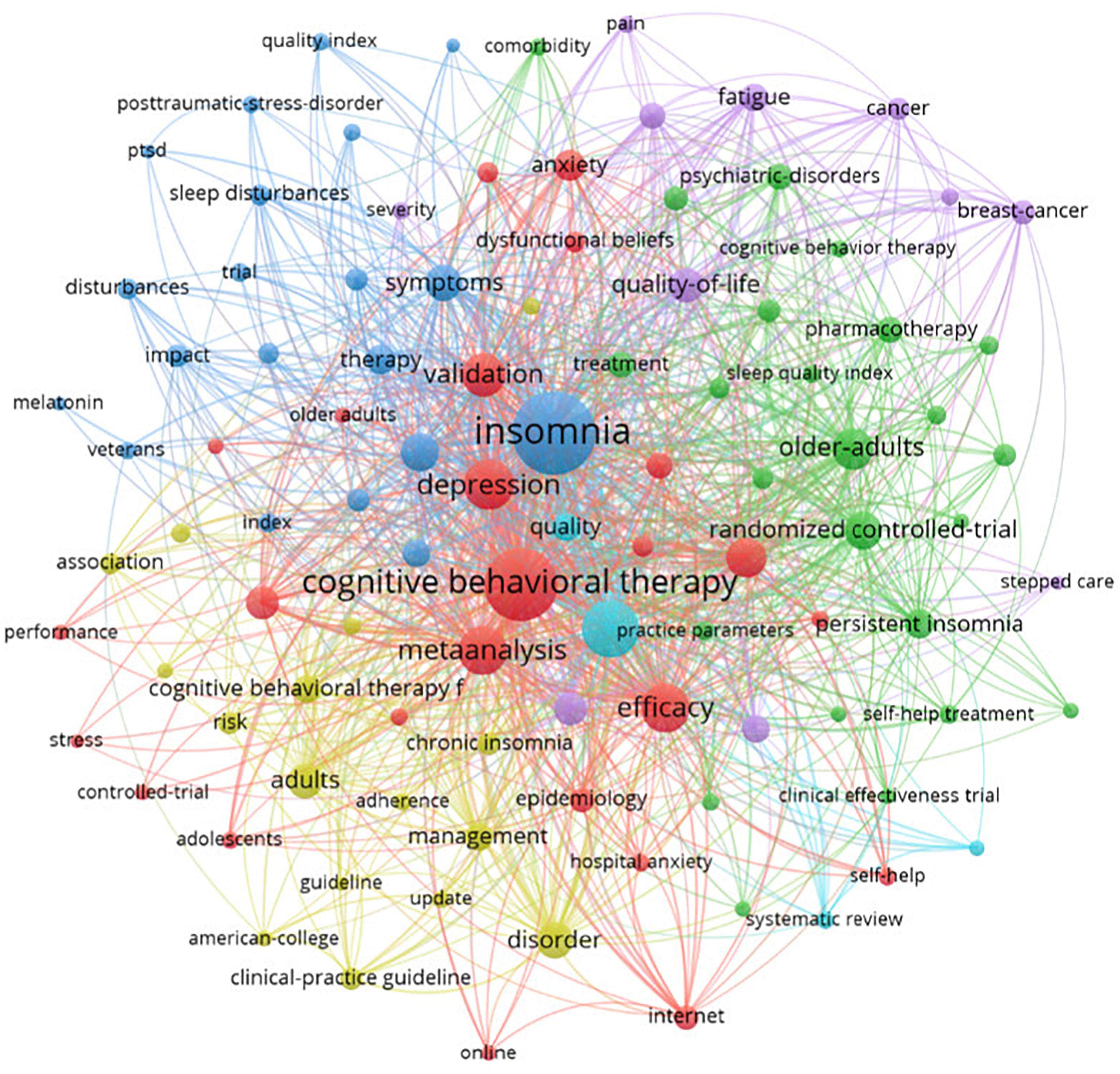
Figure 3. Network visualization map of co-occurrence on top 100 keywords. Each node is represented by a circle with labels for different words. Larger circles represent more frequently used words. The thickness and length of the lines linked between nodes represent the strength of the association between the corresponding nodes.
The visual analysis shows the research trends. Most of the participants were adolescents, adults, older adults, veterans, and women. The study type mostly observed were randomized controlled trials, meta-analyses, and epidemiological. CBTI has been used in comorbid conditions both physical and psychiatric conditions such as stress, post-traumatic stress disorder, anxiety, depression, pain, fatigue, and cancer. It can be drawn that measurement tools used to test the effectiveness of CBTI were insomnia severity index, sleep quality index, hospital anxiety depression scale, quality of life, polysomnography, and actigraphy. The appearance of words like the internet and online shows the digital adoption of cognitive behavior therapy in recent years.
Most of the papers excluded were about Cognitive behavior therapy for other disorders, notably CBT for tinnitus, cancer, pain, hypertension, and psychiatric disorders. The pharmacological management articles were also excluded.
This study found that the number of annual publication papers on CBTI increased every year. Sleep and Behavioral Sleep Medicine were the top journals of CBTI publications, among the top 10 authors who published CBTI papers, four are from the United States and three are from Canada. The University of Laval and the University of Pennsylvania were the top institutions that published papers on CBTI, and the United States and Canada were the top countries that published papers on CBTI.
This study found that the authors in an institution from countries in North America and Europe contribute more to CBTI research. China, Japan, and Korea taking a lead in Asian Continent. In the identified publications, the United States, Canada, Australia, and China were currently leaders in CBTI. And the study found that, among the top 10 authors who published CBTI papers, four are from the United States and three are from Canada. Four of the top 10 institutions on CBTI papers were from the United States, and another five were from Canada, Sweden, the United Kingdom, Australia, and Holland. This might be due to the better economic and scientific status of each country or territory and better communication among them similar to another bibliometric analysis study (13).
The changes in the number of scholarly publications in a field were an important indicator of trends in the field (14). The journal with higher publication frequency provides researchers with guidelines for paper publication. The study found that Sleep and Behavioral Sleep Medicine had a high frequency of CBTI publications. Nowadays, researchers are probing on metabolic, hormonal, genetic, cellular, and subcellular effects of sleep disturbances (15). However, CBTI research is still in the early stage, and the cooperation between authors is still limited. Facilitating collaboration between authors, institutions and countries will increase the number of authors who regularly publish in the field and contribute to a more effective exchange of experiences on CBTI research to improve the quality of treatment methods for insomnia.
The study found that CBTI has been widely used in comorbid conditions both physical and psychiatric conditions such as stress, post-traumatic stress disorder, anxiety, depression, pain, fatigue, and cancer. Co-occurrence can be drawn that the study type mostly observed were randomized controlled trials, meta-analyses, and epidemiological, and measurement tools used to test the effectiveness of CBTI were insomnia severity index, sleep quality index, polysomnography among others.
Cognitive behavior therapy for insomnia has been accepted as a first-line treatment, and American Academy of Sleep Medicine (AASM) guidelines also recommend CBTI as standard psychological and behavioral therapy for chronic insomnia. In addition, The National Institute for Health and Care Excellence (NICE) guidelines and the latest European Sleep Research Association guidelines also recommend CBTI as an initial treatment for chronic insomnia in any age group (16). Numerous previous studies have shown that CBTIs were effective in reducing the severity of insomnia, also in primary care settings (17). Results from previous studies on the effectiveness of CBTI have shown response rates over 60%, with good initial responses maintained after 6 months (18). Silversten et al. compared CBTI, Zopiclone (a drug treatment), and placebo in a sample of 46 older adults diagnosed with chronic insomnia. They found that over just 6 weeks, patients who received CBTI reported more improvements in sleep efficiency, slow-wave sleep, middle of the night awakenings, compared with patients who received the drug or a placebo. These results persisted even at 6 months, with patients receiving CBTI reporting greater improvements in sleep efficiency than those receiving Zopiclone (19).
Cognitive behavior therapy for insomnia also has a good effect on insomnia with comorbid conditions, especially depression and anxiety. Anxiety disorders are the most common mental health disorder worldwide, with a prevalence of 25%, and people with anxiety disorders often experience poor sleep quality, and further exacerbate anxiety. Molecular imaging evidence also suggests that there are specific neurotransmitter mechanisms of sleep-wake regulation associated with anxiety (20). It is known that there is a benefit of CBTI not only for insomnia but also for comorbid anxiety disorder (20). A report of ten studies examining the effect of CBTI on depressive outcomes in patients with co-occurring depression and insomnia reported that CBTI may be an appropriate stand-alone treatment for co-occurring depression and insomnia, or in combination with antidepressants (21). Several other meta-analyses have similar results (22). Apart from anxiety and depression, CBTI has been applied to the treatment of comorbid insomnia in pain, migraine, fatigue, chronic obstructive pulmonary disease, asthma, Parkinson’s disease, and other neurological as well as psychiatric disorders (23).
Subjective-objective sleep differences have long been a difficult problem in sleep medicine practice, which is because sleep is a subjective perceptual experience of a person, so subjective sleep parameters are often inconsistent with objective sleep parameters measured by polysomnography or actigraphy. The measurement tools or indicators like polysomnography, actigraphy, and insomnia severity index (ISI) are being widely used in the field of sleep (24). Polysomnography was considered the “gold standard” for assessing sleep characteristics and stages. An advantage of actigraphy is that it can assess sleep outcomes over multiple nights, allowing an assessment of sleep patterns and variability (25). ISI is particularly useful in population and clinical settings where more than one condition needs to be measured at a time without overburdening the patient (26). With the help of psychometric tools and technologies available, studies have found that CBTI is effective regardless of whether the subjective-objective sleep differences are large or small (27).
With keywords co-occurrence, it can be drawn that digital CBTI is a research hotspot in recent years. CBTI is recommended as a first-line treatment. However, some doctors were difficult to carry out CBTI due to a lack of professional knowledge, sufficient time, qualified psychologists, high cost, and other reasons (28).
The number of trained CBTI practitioners is scarce. Most patients learn about sleeping tablets than CBTI due to prescribing physicians and advertisements and misconceptions about CBTI (8). Health care workers and physicians play an important role in the dissemination of CBTI (8). In addition, there is an optimistic view regarding CBTI utilization. Even primary healthcare workers can deliver 6-session CBT to insomnia patients without the involvement of physicians and with minimal supervision (29). Furthermore, reports showed that brief CBT can be delivered with teleconsultation and self-help materials (30). These findings suggest that brief and effective CBTI can be developed to suit primary care settings. In primary care settings, with limited resources, various modifications of CBTI have been investigated such as group CBTI, and brief CBTI (4). Several CBTI modifications are effective and comparative to standard CBTI in routine care settings (31).
Furthermore, the application of digital CBTI may bridge the gap. Digital CBTI can be divided into different types including internet, phone, email, and mobile app-based CBTI. Compared with face-to-face CBTI, online CBTI is a cost-effective and time-effective, scalable, and accessible, meanwhile interactive web design, animation technology, automated multimedia web applications coupled with effective clinical support can greatly improve patient motivation and outcomes (32). Espied et al. (33) found that the online CBT was related to adherence to some therapists’ guidance in patients with co-morbid insomnia and depression. The results of sleep onset latency and sleep efficiency of verbally contacted telephone-based CBTI were suboptimal, possibly because therapist-patient interaction may play a key role in the success of digital CBTI. Online CBTI with therapists significantly improved several sleep metrics, including self-reported total sleep time (compared to phone-based CBTI), wake after sleep onset (compared to mobile app-based CBTI, phone-based CBTI, and web-based CBTI without a therapist), and sleep efficiency (compared to online CBTI without a therapist). In addition, a meta-analysis of assessment methods analyzing digital CBTI found that compared with face-to-face therapy, digital CBTI prolonged self-reported total sleep time, shortened sleep onset latency, shortened wake after sleep onset, and better sleep efficiency (32). Online CBTI combined with virtual therapists is preferred considering better treatment outcomes, offering promising results, scalability, and addressing the lack of real therapists in the future (32). At the same time, future research should focus on raising the awareness of primary care providers (general practitioners, primary care nurses, etc.) about CBTI, optimizing CBTI online courses (for example, doing some preparation before each CBTI meeting, having a specific agenda, and schedule the meeting at a time when the primary care provider is less tiring), increased training of primary care providers (such as more thorough discussion of the different components of CBTI treatment, negotiate with the patient on the goals of each session, regular phone calls to actively follow up with the patient) and providing patients with some relevant paper materials (34), and explore other new behavioral treatments such as population-specific CBTI or combination therapy. Digital CBTI will help provide immediate evidence-based care to individuals in rural/remote areas during the current COVID-19 pandemic and social distancing in the future (35).
There are some limitations of our bibliometric study. Firstly, the data was searched from the database of WOSCC and only papers published in the English language were selected. The strategy might have missed some important literature in the field. Secondly, the citation of the same paper in different databases is different, and the citation of WOSCC is different than that of google scholar. Although the variable contributions of authors include co-authors, the possibility of co-authorship and their contribution to the field could not be ascertained. These issues should be addressed in future studies.
This research systematically and comprehensively analyzes the research characteristics and trends of the CBTI paper. The field of CBTI is maturing, with great potential and broad prospects. The quality of research in this field is high. The top journals can be used by researchers as target journals for publications on CBTI. Additionally, the topics of special interest and novel studies in this field are indicative of the future directions in CBTI research. Over the past 18 years, CBTI has dominated the professional literature. CBTI was applied to insomnia as well as comorbid conditions with insomnia. New approaches like digital-based CBTI have emerged, likely influenced by the increase in the use of digital platforms. Future research should focus on creating new delivery models for CBTI that emphasize the prevention of insomnia and the scalability of treatments.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
QX and DP worked with KA to formulate the search formula, identify the search library, literature search, and data analysis. LC, YY, and SZ helped draft the manuscript and screen the data. DP visualized and revised the manuscript. HY and BZ helped with the conception and revision of the full text. All authors contributed to the article and approved the submitted version.
This research was funded by the National Natural Science Foundation of China (NSFC) (Grant number: 81801351, PI: HY).
DP was employed by the company Mental Health and Yoga Pvt., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed are those of the author(s) and not necessarily those of the NSFC.
1. Edinger JD, Arnedt JT, Bertisch SM, Carney CE, Harrington JJ, Lichstein KL, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med. (2021) 17:255–62. doi: 10.5664/jcsm.8986
2. Bootzin RR, Epstein DR. Understanding and treating insomnia. Annu Rev Clin Psychol. (2011) 7:435–58. doi: 10.1146/annurev.clinpsy.3.022806.091516
3. Pigeon WR. Treatment of adult insomnia with cognitive-behavioral therapy. J Clin Psychol. (2010) 66:1148–60. doi: 10.1002/jclp.20737
4. Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep. (2003) 26:177–82. doi: 10.1093/sleep/26.2.177
5. Davidson JR, Dickson C, Han H. Cognitive behavioural treatment for insomnia in primary care: a systematic review of sleep outcomes. Br J Gen Pract. (2019) 69:e657–64. doi: 10.3399/bjgp19X705065
7. Cunnington D, Junge MF, Fernando AT. Insomnia: prevalence, consequences and effective treatment. Med J Aust. (2013) 199:S36–40. doi: 10.5694/mja13.10718
8. Rossman J. Cognitive-behavioral therapy for insomnia: an effective and underutilized treatment for insomnia. Am J Lifestyle Med. (2019) 13:544–7. doi: 10.1177/1559827619867677
9. Avcu G, Sahbudak Bal Z, Duyu M, Akkus E, Karapinar B, Vardar F. Thanks to Trauma: a delayed diagnosis of pott disease. Pediatr Emerg Care. (2015) 31:e17–8. doi: 10.1097/PEC.0000000000000637
10. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
11. Aria M, Cuccurullo C. bibliometrix : an R-tool for comprehensive science mapping analysis. J Inform. (2017) 11:959–75. doi: 10.1016/j.joi.2017.08.007
13. Fei X, Wang S, Zheng X, Liu K, Liang X. Global research on cognitive behavioural therapy for schizophrenia from 2000 to 2019: a bibliometric analysis via CiteSpace. Gen Psychiatr. (2021) 34:e100327. doi: 10.1136/gpsych-2020-100327
14. Peng C, He M, Cutrona SL, Kiefe CI, Liu F, Wang Z. Theme trends and knowledge structure on mobile health apps: bibliometric analysis. JMIR Mhealth Uhealth. (2020) 8:e18212. doi: 10.2196/18212
15. Worley SL. The extraordinary importance of sleep: the detrimental effects of inadequate sleep on health and public safety drive an explosion of sleep research. P T. (2018) 43:758–63.
16. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
17. Cheung JMY, Jarrin DC, Ballot O, Bharwani AA, Morin CM. A systematic review of cognitive behavioral therapy for insomnia implemented in primary care and community settings. Sleep Med Rev. (2019) 44:23–36. doi: 10.1016/j.smrv.2018.11.001
18. Harvey AG, Bélanger L, Talbot L, Eidelman P, Beaulieu-Bonneau S, Fortier-Brochu É, et al. Comparative efficacy of behavior therapy, cognitive therapy, and cognitive behavior therapy for chronic insomnia: a randomized controlled trial. J Consult Clin Psychol. (2014) 82:670–83. doi: 10.1037/a0036606
19. Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. (2006) 295:2851–8. doi: 10.1001/jama.295.24.2851
20. Hohoff C, Kroll T, Zhao B, Kerkenberg N, Lang I, Schwarte K, et al. ADORA2A variation and adenosine a receptor availability in the human brain with a focus on anxiety-related brain regions: modulation by ADORA1 variation. Transl Psychiatry. (2020) 10:406. doi: 10.1038/s41398-020-01085-w
21. Cunningham JEA, Shapiro CM. Cognitive behavioural therapy for insomnia (CBT-I) to treat depression: a systematic review. J Psychosom Res. (2018) 106:1–12. doi: 10.1016/j.jpsychores.2017.12.012
22. Ye YY, Zhang YF, Chen J, Liu J, Li XJ, Liu YZ, et al. Internet-based cognitive behavioral therapy for insomnia (ICBT-i) improves comorbid anxiety and depression-a meta-analysis of randomized controlled trials. PLoS One. (2015) 10:e0142258. doi: 10.1371/journal.pone.0142258
23. Hertenstein E, Trinca E, Wunderlin M, Schneider CL, Züst MA, Fehér KD, et al. Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: a systematic review and meta-analysis. Sleep Med Rev. (2022) 62:101597. doi: 10.1016/j.smrv.2022.101597
24. Sivertsen B, Omvik S, Havik OE, Pallesen S, Bjorvatn B, Nielsen GH, et al. A comparison of actigraphy and polysomnography in older adults treated for chronic primary insomnia. Sleep. (2006) 29:1353–8. doi: 10.1093/sleep/29.10.1353
25. Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: a systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med Rev. (2016) 28:108–24. doi: 10.1016/j.smrv.2015.06.003
26. Kraepelien M, Blom K, Forsell E, Hentati Isacsson N, Bjurner P, Morin CM, et al. A very brief self-report scale for measuring insomnia severity using two items from the insomnia severity index - development and validation in a clinical population. Sleep Med. (2021) 81:365–74. doi: 10.1016/j.sleep.2021.03.003
27. Ahn JS, Bang YR, Jeon HJ, Yoon IY. Effects of subjective-objective sleep discrepancy on the response to cognitive behavior therapy for insomnia. J Psychosom Res. (2021) 152:110682. doi: 10.1016/j.jpsychores.2021.110682
28. Everitt H, McDermott L, Leydon G, Yules H, Baldwin D, Little P. GPs’ management strategies for patients with insomnia: a survey and qualitative interview study. Br J Gen Pract. (2014) 64:e112–9. doi: 10.3399/bjgp14X677176
29. Espie CA, Brindle S, Tessier S, Dawson S, Hepburn T, McLellan A, et al. Chapter 5 - supervised cognitive-behavior therapy for insomnia in general medical practice—preliminary results from the West of Scotland program. In: E Sanavio editor. Behavior and Cognitive Therapy Today. Pergamon: Oxford (1998). p. 67–75. doi: 10.1016/B978-008043437-7/50006-5
30. Mimeault V, Morin CM. Self-help treatment for insomnia: bibliotherapy with and without professional guidance. J Consult Clin Psychol. (1999) 67:511–9. doi: 10.1037/0022-006X.67.4.511
31. Koffel E, Bramoweth AD, Ulmer CS. Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): a narrative review. J Gen Intern Med. (2018) 33:955–62. doi: 10.1007/s11606-018-4390-1
32. Hasan F, Tu YK, Yang CM, James Gordon C, Wu D, Lee HC, et al. Comparative efficacy of digital cognitive behavioral therapy for insomnia: a systematic review and network meta-analysis. Sleep Med Rev. (2022) 61:101567. doi: 10.1016/j.smrv.2021.101567
33. Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry. (2019) 76:21–30. doi: 10.1001/jamapsychiatry.2018.2745
34. Torrens I, Esteva M, Vicens C, Pizá-Portell MR, Vidal-Thomàs MC, Vidal-Ribas C, et al. Assessing the feasibility and acceptability of a cluster-randomized study of cognitive behavioral therapy for chronic insomnia in a primary care setting. BMC Fam Pract. (2021) 22:77. doi: 10.1186/s12875-021-01429-5
Keywords: cognitive behavior therapy, insomnia, visualization, psychotherapy, bibliometric
Citation: Xin Q, Paudel D, An K, Ye Y, Zheng S, Chen L, Zhang B and Yin H (2022) Thematic trends and knowledge structure on cognitive behavior therapy for insomnia: A bibliometric and visualization analysis. Front. Psychiatry 13:940741. doi: 10.3389/fpsyt.2022.940741
Received: 10 May 2022; Accepted: 23 August 2022;
Published: 15 September 2022.
Edited by:
Laura Verga, Max Planck Institute for Psycholinguistics, NetherlandsReviewed by:
Vincenza Castronovo, San Raffaele Hospital (IRCCS), ItalyCopyright © 2022 Xin, Paudel, An, Ye, Zheng, Chen, Zhang and Yin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Honglei Yin, eWluaG9uZ2xlaTE5ODFAMTYzLmNvbQ==; Bin Zhang, emhhbmc3M2JpbkBob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.