- 1BrainPark, Turner Institute for Brain and Mental Health and School of Psychological Sciences, Monash University, Clayton, VIC, Australia
- 2Monash Business School, Monash University, Caulfield, VIC, Australia
- 3Department of Psychiatry, Faculty of Medicine, University of Southampton, Southampton, United Kingdom
- 4Southern Health NHS Foundation Trust, Southampton, United Kingdom
- 5Department of Psychiatry and Behavioral Neuroscience, University of Chicago, Chicago, IL, United States
Objective: Problematic drinking is highly prevalent among the general population, oftentimes leading to significant negative consequences, including physical injury, psychological problems and financial hardship. In order to design targeted early interventions for problematic drinking, it is important to understand the mechanisms that render individuals at risk for and/or maintain this behavior. Two candidate drivers of problematic drinking are distress-driven impulsivity and trait compulsivity, with recent research suggesting these constructs may interact to enhance risk for addictive behaviors. The current study examined whether individual differences in distress-driven impulsivity and trait compulsivity interact in relation to problematic drinking.
Method: Distress-driven impulsivity (indexed by the S-UPPS-P negative urgency subscale), trait compulsivity (indexed by the CHIT scale) and problematic drinking (indexed by the BATCAP alcohol scale) were assessed in two independent online samples (Sample 1, n = 117; Sample 2, n = 474). Bootstrapped moderation analysis was conducted to examine whether trait compulsivity moderated the relationship between distress-driven impulsivity and problematic drinking.
Results: In both samples, there was a significant interaction between distress-driven impulsivity and trait compulsivity in relation to problematic drinking. Follow-up tests revealed that, in both samples, higher distress-driven impulsivity was associated with more problematic drinking behaviors among participants with high trait compulsivity only.
Conclusions: The current findings add to the growing literature supporting an interactive relationship between impulsivity and compulsivity-related traits in relation to addictive behaviors and have implications for informing early detection of risk and targeted early interventions.
Introduction
Problematic drinking [heavy and/or harmful drinking patterns (1)] is highly prevalent among the general population and may have a significant negative impact on individuals' physical and psychological health, as well as social and financial conditions (2). According to the World Health Organization report (3), alcohol use disorder causes three million deaths every year (accounting for 5.3% of all deaths) and contributes to the development and/or progression of more than 200 types of injuries and illnesses. For instance, a meta-analysis found that alcohol use disorders were strongly associated with major depression and anxiety disorders (4). Additionally, people experiencing problems with alcohol have significantly higher odds ratios for suicide attempts compared to those who did not consume alcohol (5). Other frequently reported issues resulting from problematic drinking include legal problems, impaired social functioning and financial hardship (2, 6). Given that problematic drinking is associated with a broad range of negative consequences, both personally and socially, it is important to understand the risk factors and underlying mechanisms that drive and maintain this behavior. This knowledge may help develop targeted prevention and early interventions for people experiencing problems with alcohol use.
Previous studies have suggested that certain personality traits, such as trait impulsivity [i.e., the tendency to act rashly without proper consideration of potential consequences (7)], may drive problematic drinking behaviors (8, 9). As a multi-faceted trait, impulsivity includes features such as the tendency to take rash action when distressed (distress-driven impulsivity), difficulties in remaining focused on a task (lack of preservation), the tendency to act without forethought (lack of premeditation), inability to stay focused on tasks (lack of perseverance), the tendency to seek novel, exciting experience (sensation seeking) and the tendency to act rashly under strong positive emotions (positive urgency). Among various facets of impulsivity, distress-driven impulsivity has been found to be consistently associated with alcohol use disorder and considered as a potential endophenotype for alcohol-related problems (8–10).
While impulsivity is a well-established risk factor for addictive behaviors and disorders (11), addictive behaviors and disorders can also be compulsive (12); that is, they feature repetitive behaviors that persist despite negative consequences (13, 14). Different accounts exist to explain compulsivity in addictive behaviors [e.g., (15–17)]. One line of thinking posits that there are individual differences in one's propensity to repetitive actions that persist despite negative consequences [e.g., trait compulsivity, (18)], which predispose individuals toward addictive behaviors. This idea is supported by studies showing that trait compulsivity is associated with a range of addictive behaviors, including problematic internet use and problematic drinking (19–21).
Despite distress-driven impulsivity and compulsivity both being associated with addictive behaviors, they are separable dimensional constructs and underlie distinct patterns of behavior (13, 22). Importantly, the proposed mechanisms through which distress-driven impulsivity and compulsivity influence addictive behaviors are different. For instance, individuals characterized by high distress-driven impulsivity may engage in a range of (potentially) addictive behaviors, with tendencies considered to reflect reduced control over impulses in the context of negative emotion (23, 24). On the other hand, individuals characterized by high trait compulsivity may repetitively engage in an addictive behavior despite that behavior being associated with adverse consequences, with such tendencies considered to reflect cognitive inflexibility and related processes (17, 25, 26).
An increasing number of studies suggest that distress-driven impulsivity- and compulsivity- related factors may interact to drive risk for problematic/addictive behaviors (24, 27). That is, while either factor alone might be related to engagement in addictive behaviors, when both co-exist at high levels, the addictive behaviors appear to be most problematic (24, 27). Importantly, findings of this interaction have led to explanations that offer mechanistic insights into the development of problematic addictive behaviors (27). Specifically, the interaction has been explained as reflecting inflexibility of a learned coping strategy. Briefly, as individuals high in distress-driven impulsivity are more likely to engage in problematic behaviors in the context of negative emotions [due to impaired cognitive control (28)], they are more likely to experience the stress-reducing consequences of the behavior (29, 30), which in turn can promote learning (31, 32) of that response as a coping strategy for the individual. Over time, engaging in addictive behaviors to cope with negative affect can lead to negative consequences. At this point, individuals high on trait compulsivity might be more likely to persist in engaging in these behaviors despite negative consequences, owing to inflexibility. In contrast, individuals with low trait compulsivity may find it easier to adjust their behavior in response to the changed circumstances (i.e., the onset of negative consequences) and engage in alternative coping strategies, owing to their greater flexibility.
To date, findings of this interaction have involved cognitive tasks to examine the moderating influence of inflexibility [a central component of compulsivity; (24, 27)]. Although cognitive tasks can be informative with respect to neurocognitive mechanisms, they can be time-consuming and difficult to administer. For these findings to be translated into practice, translatable, it would be ideal to replicate the interaction that has been shown to exist at a cognitive level, at a self-report level. Thus, to advance the understanding of mechanisms driving the persistence of problematic behaviors and determine whether the previously found interaction at the cognitive level (24) may be extended to the trait (self-report) level, the current study examined whether trait compulsivity interacts with (i.e., moderates) the relationship between distress-driven impulsivity and problematic drinking. We hypothesized that trait compulsivity will moderate the relationship between distress-driven impulsivity and problematic drinking. Specifically, in line with past research (24), we expect that distress-driven impulsivity will be related to problematic drinking among individuals with high trait compulsivity, whereas no such relationship will be seen among individuals with low trait compulsivity. Finally, to examine the robustness of this effect, the current study adopted a two-sample design. We examined the interaction between trait compulsivity and distress-driven impulsivity in two independent samples (i.e., a general community sample and a student sample).
Method
Sample 1 consisted of 117 participants from the general community. Participants were recruited via the Mechanical Turk crowdsourcing platform. A brief description, including research purpose and survey design, was provided in the recruitment advertisement. Participants were included in the study if they were 18 years of age or older and provided informed consent. Eligible participants proceeded to an online survey. Participants who completed the survey received a USD $9 compensation.
Sample 2 consisted of 474 students. Participants were recruited through a student research participation pool at Monash Business School, Monash University, Australia. Course credit compensation was given for completing the study. Participants were included in the study if they were 18 years of age or older and provided informed consent.
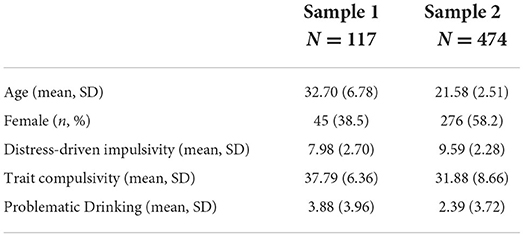
For both study samples, the recruitment protocol followed the Declaration of Helsinki and was approved by the Monash University Human Research Ethics Committee. Descriptive statistics of study variables are presented in Table 1.
Measures
The Cambridge-Chicago compulsivity trait scale
This is a 15-item self-report scale assessing trait compulsivity. The CHIT scale covers reward drive, perfectionism and, most pertinent to the current study, inflexibility/rigidity (33). According to a recent review on measurements of impulsivity and compulsivity (34), the CHIT was recommended as a self-report compulsivity measure for future research. Participants were asked to rate how much they agree with the description from the scale ranging from strongly disagree (0) to agree /strongly agree (3). CHIT total score was the moderator of interest. Higher scores indicate higher levels of trait compulsivity.
The short version of the Urgency, premeditation (lack of), perseverance (lack of), sensation seeking, and Positive Urgency impulsivity behavior scale
This is a 20-item self-report scale assessing trait impulsivity. Subscales include Negative Urgency (4 items); Positive Urgency (4 items); Lack of Perseverance (4 items); Lack of Premeditation (4 items); and Sensation Seeking (4 items). Sample items for each subscale include “When I feel bad, I will often do things I later regret in order to make myself feel better now,” “I tend to lose control when I am in a great mood,” “Once I get going on something I hate to stop,” “I like to stop and think things over before I do them” and “I quite enjoy taking risks.” Participants were asked to rate how much they agree with the description from the scale ranging from agree strongly (1) to disagree strongly (4). Distress-driven impulsivity (Negative Urgency) subscale score was the independent variable of interest. The Negative Urgency subscale reflects the tendency to act rashly under negative emotions (35) and has been found to correlate with deficits in both general inhibitory control and specific response inhibition to negative emotional stimuli (28, 36). Higher scores indicate higher levels of distress-driven impulsivity.
Brief assessment tool of compulsivity associated problems
Problematic drinking was measured by the BATCAP alcohol use scale. This is a 6-item self-report scale assessing compulsivity-related problems associated with a given behavior (in this study, alcohol use). Individuals who reported having consumed alcohol in the past month were asked to complete the BATCAP for alcohol use. The BATCAP was developed to assess the severity of problems associated with any specified potentially compulsive or problematic behavior (34, 37). The six items in the BATCAP cover time lost, distress, loss of control, functional impact, anxiety if prevented from doing the behavior, and strongest urges in the past week. Participants were asked to rate how much they agree with the description on a Likert scale ranging from 0 to 4. The BATCAP alcohol total score was used to index problematic drinking. Higher scores indicate higher levels of problematic drinking. The BATCAP scale has been shown to be positively correlated to the Alcohol Use Disorders Identification Test [rs = 0.53, p < 0.01, (37)], indicating sufficient concurrent validity.
Data analysis
To examine the interactive effect of distress-driven impulsivity and trait compulsivity on problematic drinking, as well as determine the moderating role of trait compulsivity in distress-driven impulsivity-alcohol use association, moderation analysis was conducted via PROCESS (38) in both samples. The PROCESS macro used a bias-corrected bootstrap method, which was suitable for analyzing non-normal distributed data (38). Negative urgency subscale score was entered as the independent variable, CHIT score was entered as the moderator, BATCAP alcohol score was entered as the dependent variable. Age, gender, and the other four S-UPPS-P subscales scores were set as covariates due to their potential confounding effect (37). Following the recommendations by Hayes (38), all continuous variables included in the analysis were mean centered. We applied 5,000 bootstrap samples for the current analysis. A significant interaction effect was identified when the 95% confidence interval did not contain zero. Simple slope tests were used to plot the interaction effect. The interaction was plotted at two levels of CHIT scores (high CHIT group: scored 1 SD above mean; low CHIT group: scored 1 SD below mean). The Johnson-Neyman regions of significance is included in the Supplementary material.
Results
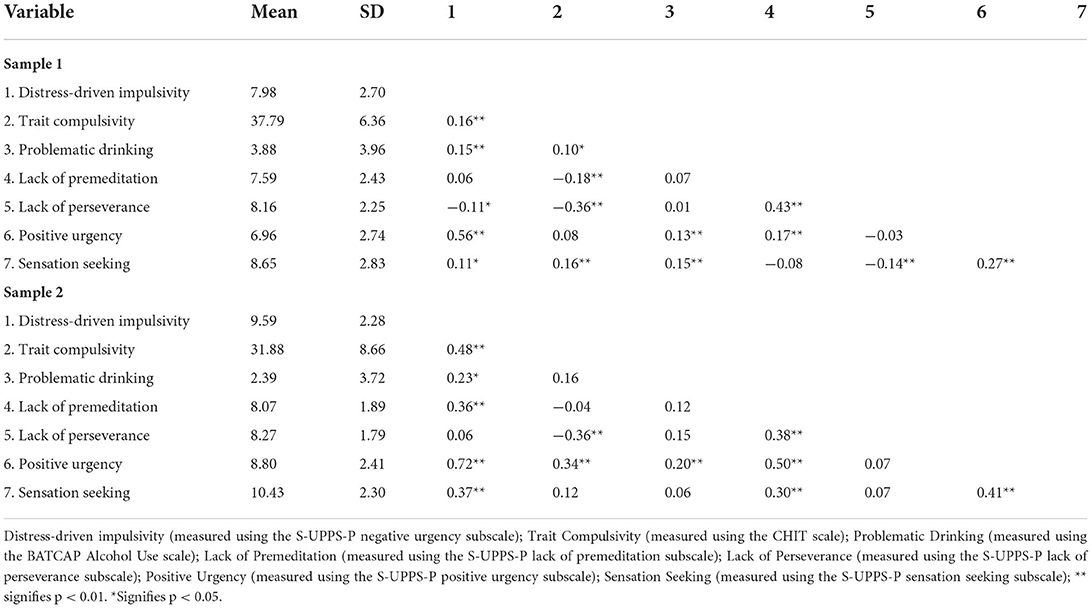
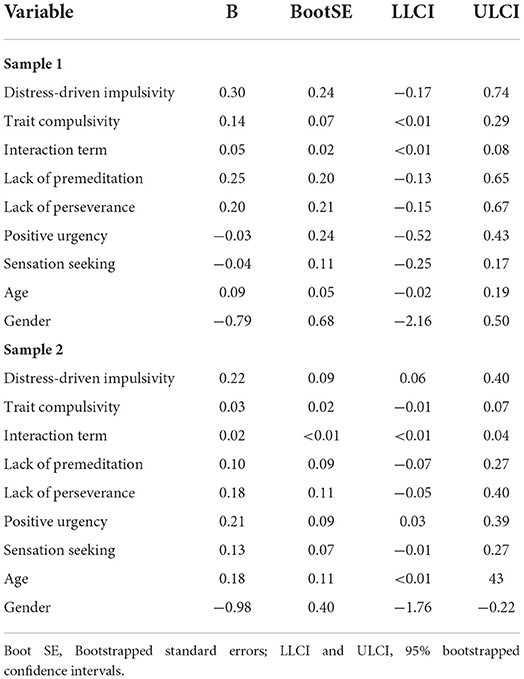
Sample 1 included 117 participants (38.5% female, n = 45), aged 18–50 (mean = 32.68, SD = 6.74). Sample 2 included 474 participants (58.2% female, n = 276), aged 18–44 years (mean = 21.58, SD = 2.51). Spearman's correlations across study variables are presented in Table 2. The results for moderation analysis are presented in Table 3. In Sample 1, we found a significant interaction effect between distress-driven impulsivity and trait compulsivity in predicting BATCAP alcohol score (b = 0.05, Boot SE = 0.02, CI = [<0.01, 0.08]). A similar interaction effect was also observed in Sample 2 (b = 0.02, Boot SE = 0.01, CI = [<0.01, 0.03]).
Follow-up analysis in Sample 1 showed that the effect of distress-driven impulsivity the BATCAP alcohol score was significant in the high CHIT group only (b = 0.61, SE = 0.21, CI = [0.20, 1.02]). Similar results were observed in Sample 2 (b = 0.38, SE = 0.11, CI = [0.16, 0.60]). Specifically, in both samples, higher distress-driven impulsivity traits were associated with elevated problematic drinking among participants with high trait compulsivity only (Figure 1). No such association was found among participants with low trait compulsivity in both samples.

Figure 1. Effect of distress-driven impulsivity on problematic drinking at different levels of trait compulsivity in Sample 1 (A) and Sample 2 (B).
Discussion
The current study aimed to examine whether there is an interaction effect between distress-driven impulsivity and compulsivity on problematic drinking and whether this effect could be replicated across two independent samples. Consistent with our hypothesis, we found that trait compulsivity moderated the association between distress-driven impulsivity and problematic drinking. Further, this effect was seen in both samples. Specifically, distress-driven impulsivity traits were associated with elevated problematic drinking among participants with high trait compulsivity only. No such association was found among participants with low trait compulsivity in both samples.
Impulsivity and compulsivity have long been viewed as risk drivers for problematic behaviors (11, 12, 18, 39). Growing evidence supports an interactive effect between impulsivity- and compulsivity-related cognition in driving addictive behaviors [e.g., (24)]. The current study extends previous research by showing that the interaction exists at the trait level. In line with previous interpretations [e.g., in relation to addiction-like eating; (27)], the current findings may be interpreted as: individuals with high distress-driven impulsivity levels are more prone to engage in problematic behaviors (e.g., alcohol consumption) under negative emotional states due to their deficits in cognitive control. Constantly engaging in drinking when distressed may increase individuals' likelihood of experiencing the stress-relieving effect of this behavior, leading individuals to acquire alcohol consumption as a coping strategy. Over time, such coping-motivated drinking may become maladaptive and lead to negative consequences. In view of negative consequences associated with drinking, individuals with low trait compulsivity may adjust their behaviors and engage in alterative coping strategies. Meanwhile, individuals with high trait compulsivity persist with the maladaptive option (i.e., alcohol consumption) due to impaired flexibility.
The current findings have important implications for the early identification of individuals at risk for problematic drinking. Specifically, by replicating the high-risk neurocognitive profile using self-report trait measures, the current findings highlight the potential of using a 5-min self-report trait screener to detect risk (a) simply (i.e., using measures that are easier to administer and less time-consuming than most cognitive tests) and (b) independently of drinking behaviors. This latter point has critical implications for early detection. Owing to the focus on traits as criteria to identify risk, such measures could be used to detect risk before drinking has even begun. In terms of developing targeted interventions, both impulsivity and compulsivity have been linked to impaired cognitive functioning (20, 24). Existing studies show that cognitive training provided promising outcomes for substance use disorders both in function improvement and symptom reduction (40, 41). Specifically, cognitive control training shows efficacy in reducing distress-driven impulsivity (42). Another potential type of intervention for reducing impulsivity and compulsivity could be personality change interventions. Digital personality change interventions (43) have been found effective in helping participants increase/decrease unwanted personality traits (indexed by the short Big Five Inventory-2) over 3 months, with medium- to large- effect sizes (43). Such interventions may be similarly effective in reducing trait impulsivity and compulsivity.
One key strength of the current study is utilizing a two-sample design. Specifically, the proposed relationship between distress-driven-impulsivity and trait compulsivity was examined in two different samples from two different countries with different demographics (e.g., general sample vs. student sample). The results were consistent in both samples, indicating the robustness of our findings. Despite its strength, several limitations should be noted when interpreting current findings. Firstly, the current study utilized cross-sectional samples, which restricted us from drawing any causal conclusions. Secondly, the generalizability of our results may be impacted due to the overall subclinical nature of our samples. Further, the utilization of the online crowdsourcing sample (i.e., the Mechanical Turk sample) with self-report measures may introduce potential issues of no verification of alcohol use compared to in-lab settings. Future studies should consider replicating our findings in clinical samples with structured clinical interviews. Finally, longitudinal studies are needed to examine the predictive effects of the impulsivity-compulsivity interaction.
In conclusion, the current study suggested that distress-driven impulsivity and trait compulsivity interactively determine the severity of problematic drinking. Trait compulsivity moderated the impulsivity-problematic drinking association. This is consistent with previous findings reporting the impulsivity-compulsivity interaction effect at the cognitive level was associated with increased problematic drinking behaviors. The current findings have important implications for future assessment and intervention efforts. Specifically, the short self-report measures used in the current study may be utilized to identify individuals at risk for problematic drinking, possibly even prior to the onset of symptoms. In turn, earlier identification of risk can help direct the appropriate support and early interventions to the people who would benefit most from them. Finally, the current findings highlight the potential of an emerging class of interventions (i.e., personality change interventions) for targeting trait impulsivity and compulsivity and, in turn, reducing risk for problematic drinking.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Monash University Ethical Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
CL wrote the first draft of this manuscript. CL, KR, and LA designed the major components of the study. All authors contributed to the selection of study measures and revising subsequent versions of the paper.
Funding
MY has received funding from Monash University, the National Health and Medical Research Council 302 (NHMRC; including Fellowship #APP1117188), the Australian Research Council (ARC), Australian Defense Science and Technology (DST), and the Department of Industry, Innovation and Science (DIIS). MY has also received philanthropic donations from the David Winston Turner Endowment Fund, Wilson Foundation. SC’s role in this study was funded by a Wellcome Trust Clinical Fellowship (110049/Z/15/Z & 110049/Z/15/A). RL was funded by a National Health and Medical Research Council project grant (APP1162031).
Acknowledgments
We are extremely grateful to the Wilson Foundation and David Winston Turner Endowment Fund whose generous philanthropic investment in the BrainPark research team and facility made this research possible.
Conflict of interest
Author MY has received payment from law firms in relation to court and/or expert witness reports. Author SC consults for Promentis and receives a stipend/honoraria from Elsevier for editorial work. Author JG has received research grants from Biohaven, Promentis, and Otsuka Pharmaceuticals. He also receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.938275/full#supplementary-material
References
1. Reid MC, Fiellin DA, O'Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med. (1999) 159:1681–9. doi: 10.1001/archinte.159.15.1681
2. Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, et al. Prevalence of 12-month alcohol use, high-risk drinking, and dsm-iv alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. (2017) 74:911–23. doi: 10.1001/jamapsychiatry.2017.2161
4. Lai HM, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990-2014: a systematic review and meta-analysis. Drug Alcohol Depend. (2015) 154:1–13. doi: 10.1016/j.drugalcdep.2015.05.031
5. Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I, et al. meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med. (2017) 47:949–57. doi: 10.1017/S0033291716002841
6. Hingson RW, Zha W, White AM. Drinking beyond the binge threshold: predictors, consequences, and changes in the US. Am J Prev Med. (2017) 52:717–27. doi: 10.1016/j.amepre.2017.02.014
7. Rømer Thomsen K, Callesen MB, Hesse M, Kvamme TL, Pedersen MM, Pedersen MU, et al. Impulsivity traits and addiction-related behaviors in youth. J Behav Addict. (2018) 7:317–30. doi: 10.1556/2006.7.2018.22
8. Berg JM, Latzman RD, Bliwise NG, Lilienfeld SO. Parsing the heterogeneity of impulsivity: a meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychol Assess. (2015) 27:1129. doi: 10.1037/pas0000111
9. Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res. (2013) 37:1441–50. doi: 10.1111/acer.12131
10. Cyders MA, Coskunpinar A, VanderVeen JD. Urgency: A Common Transdiagnostic Endophenotype For Maladaptive Risk Taking. (2016). doi: 10.1037/14854-009
11. Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehav Rev. (2008) 32:777–810. doi: 10.1016/j.neubiorev.2007.11.003
12. Yucel M, Oldenhof E, Ahmed SH, Belin D, Billieux J, Bowden-Jones H, et al. A transdiagnostic dimensional approach towards a neuropsychological assessment for addiction: an international Delphi consensus study. Addiction. (2019) 114:1095–109. doi: 10.1111/add.14424
13. Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci. (2012) 16:81–91. doi: 10.1016/j.tics.2011.11.009
14. Luigjes J, Lorenzetti V, de Haan S, Youssef GJ, Murawski C, Sjoerds Z, et al. Defining compulsive behavior. Neuropsychol Rev. (2019) 29:4–13. doi: 10.1007/s11065-019-09404-9
15. Everitt BJ, Robbins TW. From the ventral to the dorsal striatum: devolving views of their roles in drug addiction. Neurosci Biobehav Rev. (2013) 37:1946–54. doi: 10.1016/j.neubiorev.2013.02.010
16. Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the 'dark side' of drug addiction. Nat Neurosci. (2005) 8:1442–4. doi: 10.1038/nn1105-1442
17. Albertella L, Chamberlain SR, Fontenelle LF, Westbrook RF. Linking addictive and obsessive-compulsive behaviours. In: Patel VB, Preedy VR, editors. Handbook of Substance Misuse and Addictions: From Biology to Public Health. Cham: Springer International Publishing (2021). p. 1–18. doi: 10.1007/978-3-030-67928-6_5-1
18. Chamberlain SR, Stochl J, Redden SA, Grant JE. Latent traits of impulsivity and compulsivity: toward dimensional psychiatry. Psychol Med. (2018) 48:810–21. doi: 10.1017/S0033291717002185
19. Albertella L, Chamberlain SR, Le Pelley ME, Greenwood L-M, Lee RSC, Den Ouden L, et al. Compulsivity is measurable across distinct psychiatric symptom domains and is associated with familial risk and reward-related attentional capture. CNS Spectr. (2020) 25:519–26. doi: 10.1017/S1092852919001330
20. Chamberlain SR, Grant JE. Initial validation of a transdiagnostic compulsivity questionnaire: the Cambridge–chicago compulsivity trait scale. CNS Spectr. (2018) 23:340–6. doi: 10.1017/S1092852918000810
21. Kidd M, Kilic Z, Ioannidis K, Grant JE, Yücel M, Stein DJ, et al. The COVID-19 pandemic and problematic usage of the internet: Findings from a diverse adult sample in South Africa. J Psychiatr Res. (2022) 153:229–235. doi: 10.1016/j.jpsychires.2022.06.035
22. Chamberlain SR, Tiego J, Fontenelle LF, Hook R, Parkes L, Segrave R, et al. Fractionation of impulsive and compulsive trans-diagnostic phenotypes and their longitudinal associations. Aust N Z J Psychiatry. (2019) 53:896–907. doi: 10.1177/0004867419844325
23. Kalanthroff E, Henik A, Derakshan N, Usher M. Anxiety, emotional distraction, and attentional control in the Stroop task. Emotion. (2016) 16:293. doi: 10.1037/emo0000129
24. Albertella L, Le Pelley ME, Chamberlain SR, Westbrook F, Lee RS, Fontenelle LF, et al. Reward-related attentional capture and cognitive inflexibility interact to determine greater severity of compulsivity-related problems. J Behav Ther Exp Psychiatry. (2020) 69:101580. doi: 10.1016/j.jbtep.2020.101580
25. Albertella L, Watson P, Yücel M, Le Pelley ME. Persistence of value-modulated attentional capture is associated with risky alcohol use. Addict Behav Rep. (2019) 10:100195. doi: 10.1016/j.abrep.2019.100195
26. Lee RS, Hoppenbrouwers S, Franken I. A systematic meta-review of impulsivity and compulsivity in addictive behaviors. Neuropsychol Rev. (2019) 29:14–26. doi: 10.1007/s11065-019-09402-x
27. Liu C, Rotaru K, Lee RS, Tiego J, Suo C, Yücel M, et al. Distress-driven impulsivity interacts with cognitive inflexibility to determine addiction-like eating. J Behav Addict. (2021) 10:534–9. doi: 10.1556/2006.2021.00027
28. Zorrilla EP, Koob GF. Impulsivity derived from the dark side: neurocircuits that contribute to negative urgency. Front Behav Neurosci. (2019) 13:136. doi: 10.3389/fnbeh.2019.00136
29. Dallman MF, Pecoraro NC, la Fleur SE. Chronic stress and comfort foods: self-medication and abdominal obesity. Brain Behav Immun. (2005) 19:275–80. doi: 10.1016/j.bbi.2004.11.004
30. Goeders NE. The impact of stress on addiction. Eur Neuropsychopharmacol. (2003) 13:435–41. doi: 10.1016/j.euroneuro.2003.08.004
31. Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. (2004) 111:33–51. doi: 10.1037/0033-295X.111.1.33
32. Jacobs DF. A general theory of addictions: a new theoretical model. J Gambl Behav. (1986) 2:15–31. doi: 10.1007/BF01019931
33. Hampshire A, Hellyer P, Soreq E, Mehta MA, Ioannidis K, Trender W, et al. Dimensions and modulators of behavioural and mental-health change during the Covid-19 pandemic. MedRxiv. (2020). doi: 10.1101/2020.06.18.20134635
34. Hook RW, Grant JE, Ioannidis K, Tiego J, Yücel M, Wilkinson P, et al. Trans-diagnostic measurement of impulsivity and compulsivity: a review of self-report tools. Neurosci Biobehav Rev. (2021) 120:455–69. doi: 10.1016/j.neubiorev.2020.10.007
35. Cyders MA, Littlefield AK, Coffey S, Karyadi KA. Examination of a short english version of the UPPS-P impulsive behavior scale. Addict Behav. (2014) 39:1372–6. doi: 10.1016/j.addbeh.2014.02.013
36. Allen KJD, Hooley JM. Negative emotional action termination (NEAT): support for a cognitive mechanism underlying negative urgency in nonsuicidal self-injury. Behav Ther. (2019) 50:924–37. doi: 10.1016/j.beth.2019.02.001
37. Albertella L, Le Pelley ME, Chamberlain SR, Westbrook F, Fontenelle LF, Segrave R, et al. Reward-related attentional capture is associated with severity of addictive and obsessive-compulsive behaviors. Psychol Addict Behav. (2019) 33:495–502. doi: 10.1037/adb0000484
38. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications (2017).
39. Hampshire A, Hellyer PJ, Soreq E, Mehta MA, Ioannidis K, Trender W, et al. Associations between dimensions of behaviour, personality traits, and mental-health during the COVID-19 pandemic in the United Kingdom. Nat. Commun. (2021) 12:4111. doi: 10.1038/s41467-021-24365-5
40. Dhir S, Teo W-P, Chamberlain SR, Tyler K, Yücel M, Segrave RA. The effects of combined physical and cognitive training on inhibitory control: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 128:735–48. doi: 10.1016/j.neubiorev.2021.07.008
41. Verdejo-Garcia A. Cognitive training for substance use disorders: neuroscientific mechanisms. Neurosci Biobehav Rev. (2016) 68:270–81. doi: 10.1016/j.neubiorev.2016.05.018
42. Peckham AD, Johnson SL. Cognitive control training for emotion-related impulsivity. Behav Res Ther. (2018) 105:17–26. doi: 10.1016/j.brat.2018.03.009
Keywords: distress-driven impulsivity, negative urgency, compulsivity, alcohol use disorder, problematic drinking
Citation: Liu C, Rotaru K, Chamberlain SR, Yücel M, Grant JE, Lee RSC, Wulandari T, Suo C and Albertella L (2022) Distress-driven impulsivity interacts with trait compulsivity in association with problematic drinking: A two-sample study. Front. Psychiatry 13:938275. doi: 10.3389/fpsyt.2022.938275
Received: 07 May 2022; Accepted: 04 August 2022;
Published: 15 September 2022.
Edited by:
Henry W. Chase, University of Pittsburgh, United StatesReviewed by:
Kyung-Hyun Suh, Sahmyook University, South KoreaMassimo Bardi, Randolph–Macon College, United States
Copyright © 2022 Liu, Rotaru, Chamberlain, Yücel, Grant, Lee, Wulandari, Suo and Albertella. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chang Liu, Y2hhbmcubGl1NUBtb25hc2guZWR1
 Chang Liu
Chang Liu Kristian Rotaru
Kristian Rotaru Samuel R. Chamberlain3,4
Samuel R. Chamberlain3,4 Murat Yücel
Murat Yücel Jon E. Grant
Jon E. Grant Rico S. C. Lee
Rico S. C. Lee Chao Suo
Chao Suo Lucy Albertella
Lucy Albertella