
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry , 14 July 2022
Sec. Mood Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.936009
This article is part of the Research Topic Women in Psychiatry 2022: Mood Disorders View all 6 articles
Background: Premenstrual syndrome/premenstrual dysphoric disorder is a serious condition affecting women worldwide, causing clinically significant distress or interference. Therefore, solving these diseases has become the utmost concern worldwide, culminating in numerous studies. In this study, we performed bibliometric analysis on the 100 most cited papers with the aim of identifying research hot spots and trends in this field.
Methods: We screened the Science Citation Index Expanded (SCIE) of Web of Science (WOS) to identify the top 100 cited studies on PMS/PMDD. Next, we analyzed relevant literature from various journals, countries/regions, institutions, authors, and keywords. Finally, we used VOSviewer and Citespace software to generate knowledge maps and identify hot spots and trends.
Results: The top 100 highly cited studies were published in 55 journals, between 1999 and 2017, across 24 countries/regions around the world. Most articles were published in Obstetrics and Gynecology, whereas Psych neuroendocrinology had the largest average number of citations per paper. The United States had the highest number of publications, followed by England, Canada, and Sweden. The top three institutions that published the highly cited literature were the University of Pennsylvania, Yale University, and National Institute of Mental Health (NIMH). Obstetrics, Gynecology, Psychiatry, and Reproductive Biology were the main research directions, whereas the top 10 Co-occurrence of Keywords included double-blind, fluoxetine, efficacy, prevalence, epidemiology, phase sertraline treatment, depression, progesterone, placebo, and placebo-controlled trial. Results from cluster analysis indicated that more comprehensive epidemiology and steroid pathogenesis have gradually become the hot spots and trends.
Conclusion: These findings demonstrated that bibliometric analysis can intuitively and rapidly reveal the frontiers and hot spots of research in PMS/PMDD. Notably, epidemiology, steroid pathogenesis, GABAA receptor delta subunits, and double-blind placebo-controlled trials are potential areas of focus for future research.
Premenstrual dysphoric disorder (PMDD), a severe form of premenstrual syndrome (PMS), refers to a condition in which women of childbearing age exhibit periodic symptoms of discomfort, emotion, and physical disorders in the luteal phase, which deeply affect the patients' ability to study, and work as well as quality of life (1–5). Clinically, PMS/PMDD not only brings a substantial burden on both physical and mental aspects of life (6, 7) but also predisposes affected individuals to depression and bipolar disorders (8–10). Recent studies have demonstrated that some PMDD patients are suicidal, as evidenced by the fact that nearly 40% of PMDD women reported suicidal ideation (11, 12).
Published articles on PMS/PMDD date back to 1950 (13). In the past 60 years, researchers have made significant progress on PMS/PMDD, a phenomenon that is still ongoing (14). However, It is difficult to grasp the development overview and trend of PMS/PMDD research field, and scientific analysis of bibliometrics is urgently needed.
Knowledge on the top 100 cited papers may generate an understanding into the current focus of researchers. Bibliometric analysis, an effective method for analyzing literature, enhances researchers' understanding of a particular research area (15). In this study, we adopted bibliometric analysis to identify the top 100 cited papers on PMS/PMDD, and determined the trends in research on this topic from a perspective different from the previous research (14), which will promote the development of this research field and promote the basic research to gain new discoveries.
Data were obtained from the Science Citation Index Expanded (SCI-E) database in the Web of Science Core Collection (WOSCC) (1). The literature search was framed as follows: [TI = (Premenstrual Syndrome) OR TI = (Premenstrual Dysphoric Disorder) OR TI = (late luteal phase dysphoric disorder) referring to related retrieval strategy (16). The range of article publication dates range was set from inception of the database to April 8th, 2022. No limitations were applied with regards to either the year of publication or language.
Papers were displayed in descending order, based on the number of citations. Where necessary, two independent researchers identified the 100 most-cited papers after reading the titles, abstracts, and full texts. Conference papers and studies in which PMS/PMDD was not the central topic were excluded. Any disagreement, between the researchers, was resolved through discussion and consensus with a third researcher.
The top 100 articles were selected, then imported into Endnote X9, where several study characteristics, including title, keywords, document type, citation number, publication date, country, institutions, journals, and the 2020 impact factor of journals, were extracted. Next, we combined the online platform https://bibliometric.com, with VOSviewer 1.6.17, and Citespace R 5.8 to determine potential research hot spots and trends in this field by visualizing the aforementioned characteristics in the top 100 articles.
A total of 1,135 documents were initially retrieved from WoSCC. The list was arranged in descending order of citations, and the top 100 cited papers selected as listed in Table 1. The total number of citations for these 100 papers was 9,675 (median = 96.75) and frequency distribution of citations by year could been seen in Figure 1. The top 100 papers had 3821 references, with an h-index of 68. The most frequently cited articles included “The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD)” (17) by Halbreich, U (431 citations), followed by “Prevalence, incidence, and stability of premenstrual dysphoric disorder in the community” (355 citations) (18), “Cortical gamma-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder—A proton magnetic resonance spectroscopy study” (257 citations) (19), “Efficacy of a new low-dose oral contraceptive with drospirenone in premenstrual dysphoric disorder” (226 citations) (20) and “Efficacy of selective serotonin-reuptake inhibitors in premenstrual syndrome: a systematic review” (218 citations) (21). The abovementioned articles have been cited more than 200 times.
The distribution of publications by year is illustrated using a histogram in Figure 2. The top 100 cited papers on PMS/PMDD were published between 1999 and 2017, although articles published between 2018 and 2022 were not included in the list. Additionally, 13 papers published in 2007 had the most significant impact on research in this field. Among the selected papers, 67 and 33 were original research articles and reviews, respectively. Furthermore, the 23 papers published in 2003 had the most significant impact on research in this field (Figure 2).
We generated a citation network of journals, based on the average published year, to depict interaction among the top 100 cited articles published in 55 journals (Figure 3). Notably, Obstetrics and Gynecology published the largest number of papers (7 papers), followed by the American journal of psychiatry (6 papers). On the other hand, Psych neuroendocrinology had the largest average number of citations per paper (1 paper, 917 citations).
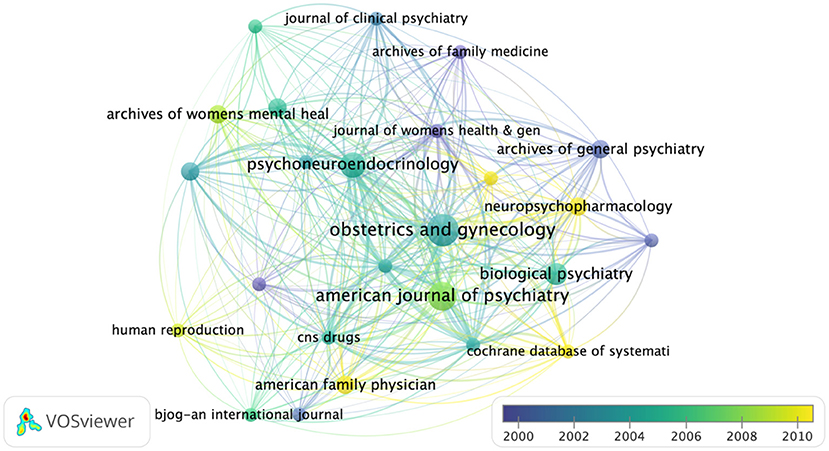
Figure 3. Network-based visualization of journals that published the 100 most cited articles according to average publication year. The size of the circles represents the number of articles in the 100 most cited list, whereas the width of the curved line denotes link strength. The distance between 2 journals indicates the approximate relatedness of the nodes.
A total of 360 authors contributed to the top 100 cited papers, although some of the 386 items in the network were not connected. The largest set of connected items comprised 83 items. Notably, Freeman EW was at the core of this network, although Halbreich U and Yonkers KA emerged as new authors in recent years. Freeman EW had the highest number of papers (11, with 956 citations), followed by Halbreich U and Yonkers KA who had 645 and 894 citations, respectively (Figure 4).
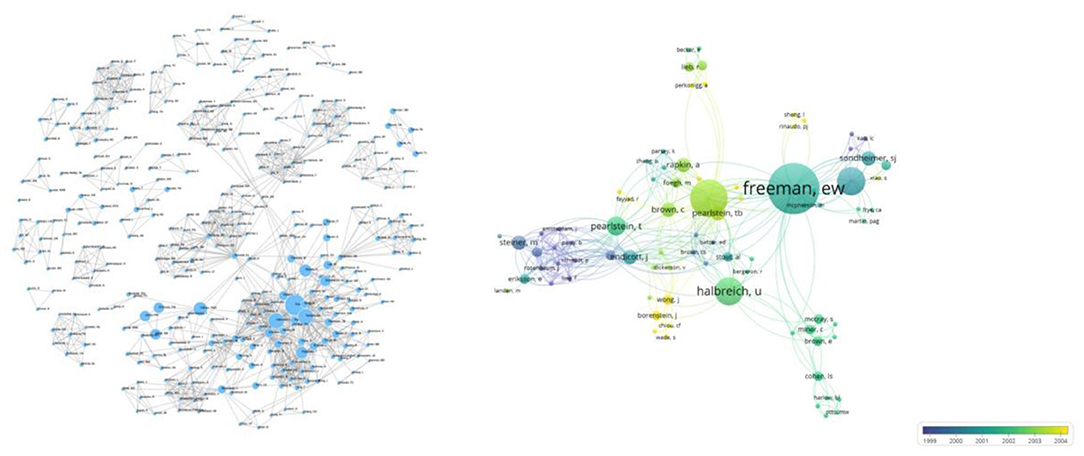
Figure 4. Networks showing interconnectivity among co-authors across the 100 most cited articles according to the average published year. Size of the circles indicate the number of articles in the 100 most cited list, while the width of the curved line represents the link strength. The distance between two authors indicates approximate relatedness among the nodes.
The selected top 100 cited papers were published across 24 countries or regions (Figure 5). Among them, the United States had the highest contribution (68 articles), followed by England (13 papers). Among the 24 countries, the United States formed the largest national cooperation network, covering 17 countries. In terms of research institutions, the 100 most cited papers were published by 153 institutions, with the largest set of connected items comprising 107 institutions. Specifically, the University of Pennsylvania contributed the most papers (15 papers), followed by Yale University and NiMH which accounted for 13 and 10 papers, respectively (Figure 6).
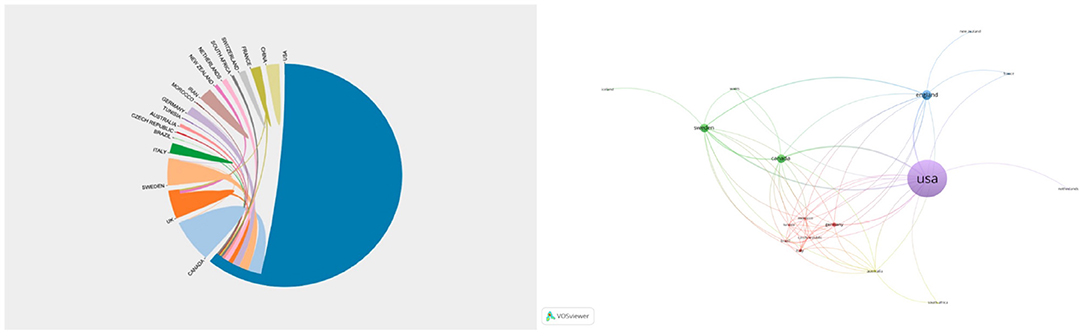
Figure 5. Networks showing the collaboration among countries/regions in the top 100 cited papers. Circle size represents the number of papers in the top 100 cited articles.
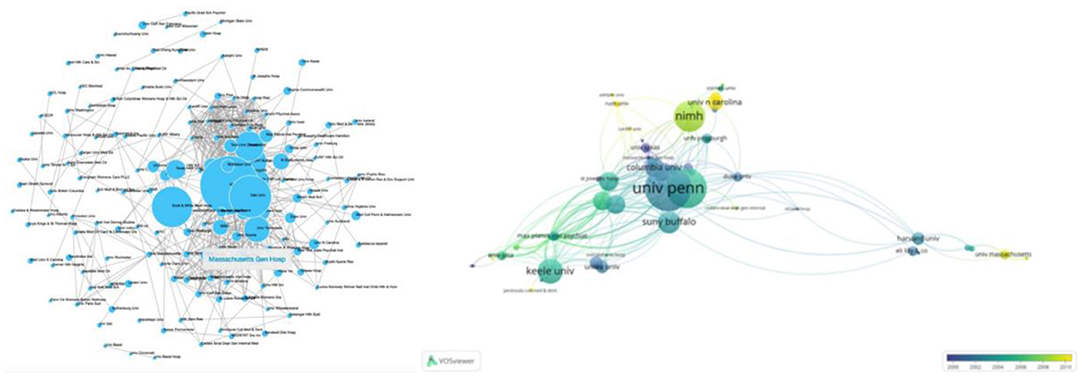
Figure 6. Network visualization of the institutions that contributed to the top 100 cited articles. The size of the circle represents the number of papers in the top 100 list.
The top 100 cited papers on PMS/PMDD were stratified into various study directions based on WOS categories as shown in Table 2. Among them, “Obstetrics Gynecology” (98 papers) was the topmost research direction, followed by “Psychiatry” (63 papers), and “Reproductive Biology” (61 papers), among others (Table 2).
A total of 477 keywords were identified across the top 100 cited papers. We excluded 10 keywords, such as women, menstrual cycle, premenstrual dysphoric disorder, and premenstrual syndrome, among others. Further analysis revealed cooccurring keywords, with the following forming the top 10; double-blind, fluoxetine, efficacy, prevalence, epidemiology, phase sertraline treatment, depression, progesterone, placebo, and placebo-controlled trial (Table 3). These keywords were further classified into 11 clusters as follows: cluster 1 (epidemiology), cluster 2 (placebo-controlled trial), cluster 3 (steroid), cluster 4 (late luteal phase), cluster 5(premenstrual syndrome), cluster 6 (emotional perception), cluster 7 (dysmenorrhea), cluster 8 (therapeutic use), cluster 9 (brain-derived neurotrophic factor), cluster 10 (delta) and cluster 11 (Japanese women) (Figure 7, Table 4).
Women's menstrual cycle-related disorders, such as premenstrual syndrome and dysmenorrhea, predispose many women to various diseases which subsequently adversely affect their health (22).
The top 100 cited papers were selected from papers titled “Premenstrual Syndrome,” “Premenstrual Dysphoric Disorder,” or “late luteal phase dysphoric disorder” referring to its citations, which represent the concerns of researchers. Analysis of the selected top 100 cited articles resulted in a total of 9,676 citations, with an average of 96.76 citations per article. Among them, the earliest paper entitled “Randomized controlled trial of the management of premenstrual syndrome and premenstrual mastalgia using luteal phase-only danazol,” was published in 1999 (23), whereas the most recent one was “Premenstrual Dysphoric Disorder Symptoms Following Ovarian Suppression: Triggered by Change in Ovarian Steroid Levels but Not Continuous Stable Levels” published in 2017 (24). Moreover, “The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD)” (17) by Halbreich was the most cited article.
Analysis of the 100 most cited papers revealed contribution by 386 authors. Among them, Freeman EW, Halbreich U, and Yonkers KA were the highest contributors to the most influential articles, suggesting that their researches are a potential hotspot in this field. Particularly, Freeman EW's s newest paper, entitled “Are there differential symptom profiles that improve in response to different pharmacological treatments of premenstrual syndrome/premenstrual dysphoric disorder?” revealed possible well-defined subgroups of PMDD. It is evident that overall treatment response rates may improve if treatments are targeted at subtypes (25). On the other hand, Yonkers KA's paper, entitled “Premenstrual Dysphoric Disorder: Evidence for a New Category for DSM-5,” discussed DSM-5 for premenstrual dysphoric disorder (26), whereas Halbreich U's article “Clinical diagnostic criteria for premenstrual syndrome and guidelines for their quantification for research studies,” revealed updated diagnostic criteria for PMS/PMDD and guidelines for clinical and research applications (27). A total of 83 items showed an interaction, of which Freeman EW was at the core of this network, although new scholars, such as Halbreich U and Yonkers KA have emerged in recent years. These authors are distributed across 24 countries or regions and 153 institutions. Among them, the University of Pennsylvania and the United States contributed the highest number of publications. This indicated that American institutions and authors play a leading role in research on PMDD, this may guide future research activities.
Epidemiological research is the primary and critical approach for exploring development and progression of PMS/PMDD. Notably, 11 out of the 100 most cited articles described prevalence of PMS/PMDD between 2000 and 2014 (17, 18, 28–35), while 29 focused on epidemiology. Collectively, these articles provide reliable data sources to better our understanding of PMS/PMDD, including incidence rate. In recent years, numerous studies have evaluated childhood body size and premenstrual disorders in young adulthood (36), comorbid bipolar disorder (37), prevalence, and associated factors among different groups (38). For instance, studies showed that the prevalence of PMS among Academics at a University in Midwest Brazil was 46.9% (38), and 21.1% for university students (39), which are higher than ever before. Moreover, risk factors for PMS/PMDD include childhood abuse and neglect (40), childhood maltreatment (41), and perinatal depression (42), among others.
At present, the pathogenesis of PMDD remains unclear. However, steroid pathogenesis such as progesterone and allopregnanolone in PMS/PMDD has always been research hotspots. New findings have suggested that progesterone exerts a different effect on the metabolic profiles of women with PMDD compared to controls (43). In addition, a change in estradiol/progesterone levels from low to high, and not the steady-state level, was associated with onset of PMDD symptoms (24). Gradually, researchers have found that allopregnanolone is the provoking factor behind the negative mood symptoms in PMDD, a disease whose pathophysiology is significantly correlated with impaired GABAA-R response to dynamic ALLO fluctuations across the menstrual cycle, manifesting in affective symptoms (44–46). It is possible that GABAA-R response to allopregnanolone, alpha4 and delta subunits of GABAA-R may be playing an essential role in mood swings (47). Recent studies have also associated copy number variations in GABRB2 with PMDD (48, 49). Future studies are expected to elucidate GABAA-R's susceptibility to ALLO.
Treatment is a crucial step in management of PMS/PMDD. The clusters of co-occurrent keywords suggest that prospecting for effective treatment therapies for PMS/PMDD, such as use of fluoxetine (50), and vitex agnus castus (51), is a promising research hotspot. However, placebo-controlled trials are needed to generate more reliable data.
This study had several limitations. After consulting numerous literature, we used the Web of Science to identify relevant datasets. Although this is the most commonly used database for literature searches, some early publications may be missing. For an accurate econometric analysis, we referred to previous studies (16) and adopted a Title keyword rather than Topic keyword retrieval approach. Although our search results were accurate, they may not be extensive enough.
To the best of our knowledge, this is the first bibliometric analysis of the most frequently cited papers on PMS/PMDD. Our results indicate that most essential studies on PMS/PMDD have been published in the Journal of Obstetrics and Gynecology. American authors and institutions have played a leading role in research on PMDD, thus represent a future research direction. Moreover, epidemiology for prevalence and risk factors, steroid pathogenesis, such as progesterone, allopregnanolone, and placebo-controlled trial for the treatment represent future trends in this field of research.
MG designed the study and wrote and revised the draft manuscript. MG, HZ, CW, and XM performed literature search, retrieval, and data collection. MG and HZ carried out data visualization and graphical interpretation. QZ, DG, and JW provided critical assistance or funding. All authors contributed to and approved the final draft of the manuscript before submission.
This study was supported by funds from the Key Project of Natural Science Foundation of Shandong Province (No. ZR2020ZD17), National Natural Science Foundation of China (Nos. 81001484 and 81473558), Natural Science Foundation of Shandong Province (No. ZR202102270167), Shandong medical and health science and technology development plan project (No. 202105010467) and 20 articles for colleges and universities funded project in Jinan (No. 2020GXRC002).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to acknowledge the support of the Team of Research and Innovation Focusing on Emotional Diseases and Syndromes in Shandong University of Traditional Chinese Medicine, Team of Young Scientific Research and Innovation Focusing on Pharmacology Mechanism of Emotional Diseases and Syndromes in Ganzangxiang.
1. Mishra S, Elliott H, Marwaha R. Premenstrual Dysphoric Disorder. StatPearls: Treasure Island (FL) (2022).
2. Yonkers KA, Simoni MK. Premenstrual disorders. Am J Obstet Gynecol. (2018) 218:68–74. doi: 10.1016/j.ajog.2017.05.045
3. Albsoul-Younes A, Alefishat E, Farha RA, Tashman L, Hijjih E, AlKhatib R. Premenstrual syndrome and premenstrual dysphoric disorders among Jordanian women. Perspect Psychiatr Care. (2018) 54:348–53. doi: 10.1111/ppc.12252
4. Di Giulio G, Reissing ED. Premenstrual dysphoric disorder: prevalence, diagnostic considerations, and controversies. J Psychosom Obstet Gynaecol. (2006) 27:201–10. doi: 10.1080/01674820600747269
5. Hofmeister S, Bodden S. Premenstrual syndrome and premenstrual dysphoric disorder. Am Fam Physician. (2016) 94:236–40.
6. Yang M, Wallenstein G, Hagan M, Guo A, Chang J, Kornstein S. Burden of premenstrual dysphoric disorder on health-related quality of life. J Womens Health. (2008) 17:113–21. doi: 10.1089/jwh.2007.0417
7. Slyepchenko A, Frey BN, Lafer B, Nierenberg AA, Sachs GS, Dias RS. Increased illness burden in women with comorbid bipolar and premenstrual dysphoric disorder: data from 1 099 women from STEP-BD study. Acta Psychiatr Scand. (2017) 136:473–82. doi: 10.1111/acps.12797
8. Slyepchenko A, Minuzzi L, Frey BN. Comorbid premenstrual dysphoric disorder and bipolar disorder: a review. Front Psychiatry. (2021) 12:719241. doi: 10.3389/fpsyt.2021.719241
9. Sepede G, Brunetti M, Di Giannantonio M. Comorbid premenstrual dysphoric disorder in women with bipolar disorder: management challenges. Neuropsychiatr Dis Treat. (2020) 16:415–26. doi: 10.2147/NDT.S202881
10. Cirillo PC, Passos RB, Bevilaqua MC, Lopez JR, Nardi AE. Bipolar disorder and premenstrual syndrome or premenstrual dysphoric disorder comorbidity: a systematic review. Braz J Psychiatry. (2012) 34:467–79. doi: 10.1016/j.rbp.2012.04.010
11. Wikman A, Sacher J, Bixo M, Hirschberg AL, Kopp Kallner H, Epperson CN, et al. Prevalence and correlates of current suicidal ideation in women with premenstrual dysphoric disorder. BMC Womens Health. (2022) 22:35. doi: 10.1186/s12905-022-01612-5
12. Yan H, Ding Y, Guo W. Suicidality in patients with premenstrual dysphoric disorder-A systematic review and meta-analysis. J Affect Disord. (2021) 295:339–46. doi: 10.1016/j.jad.2021.08.082
13. Morton JH. Premenstrual tension. Am J Obstet Gynecol. (1950) 60:343–52. doi: 10.1016/0002-9378(50)90475-3
14. Gao M, Gao D, Sun H, Cheng X, An L, Qiao M. Trends in research related to premenstrual syndrome and premenstrual dysphoric disorder from 1945 to 2018: a bibliometric analysis. Front Public Health. (2021) 9:596128. doi: 10.3389/fpubh.2021.596128
15. Ahmad P, Slots J. A bibliometric analysis of periodontology. Periodontol 2000. (2021) 85:237–40. doi: 10.1111/prd.12376
16. Liu Y, Li J, Cheng X, Zhang X. Bibliometric analysis of the top-cited publications and research trends for stereotactic body radiotherapy. Front Oncol. (2021) 11:795568. doi: 10.3389/fonc.2021.795568
17. Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology. (2003) 28(Suppl. 3):1–23. doi: 10.1016/S0306-4530(03)00098-2
18. Wittchen HU, Becker E, Lieb R, Krause P. Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychol Med. (2002) 32:119–32. doi: 10.1017/S0033291701004925
19. Epperson CN, Haga K, Mason GF, Sellers E, Gueorguieva R, Zhang W, et al. Cortical gamma-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder: a proton magnetic resonance spectroscopy study. Arch Gen Psychiatry. (2002) 59:851–8. doi: 10.1001/archpsyc.59.9.851
20. Yonkers KA, Brown C, Pearlstein TB, Foegh M, Sampson-Landers C, Rapkin A. Efficacy of a new low-dose oral contraceptive with drospirenone in premenstrual dysphoric disorder. Obstet Gynecol. (2005) 106:492–501. doi: 10.1097/01.AOG.0000175834.77215.2e
21. Dimmock PW, Wyatt KM, Jones PW, O'Brien PM. Efficacy of selective serotonin-reuptake inhibitors in premenstrual syndrome: a systematic review. Lancet. (2000) 356:1131–6. doi: 10.1016/S0140-6736(00)02754-9
22. Kenda M, Glavac NK, Nagy M, Dolenc MS. Herbal products used in menopause and for gynecological disorders. Molecules. (2021) 26:7421. doi: 10.3390/molecules26247421
23. O'Brien PMS, Abukhalil IEH. Randomized controlled trial of the management of premenstrual syndrome and premenstrual mastalgia using luteal phase–only danazol. Am J Obstet Gynecol. (1999) 180:18–23. doi: 10.1016/S0002-9378(99)70142-0
24. Schmidt PJ, Martinez PE, Nieman LK, Koziol DE, Thompson KD, Schenkel L, et al. Premenstrual dysphoric disorder symptoms following ovarian suppression: triggered by change in ovarian steroid levels but not continuous stable levels. Am J Psychiatry. (2017) 174:980–9. doi: 10.1176/appi.ajp.2017.16101113
25. Halbreich U, O'Brien PM, Eriksson E, Backstrom T, Yonkers KA, Freeman EW. Are there differential symptom profiles that improve in response to different pharmacological treatments of premenstrual syndrome/premenstrual dysphoric disorder? CNS Drugs. (2006) 20:523–47. doi: 10.2165/00023210-200620070-00001
26. Epperson CN, Steiner M, Hartlage SA, Eriksson E, Schmidt PJ, Jones I, et al. Premenstrual dysphoric disorder: evidence for a new category for DSM-5. Am J Psychiatry. (2012) 169:465–75. doi: 10.1176/appi.ajp.2012.11081302
27. Halbreich U, Backstrom T, Eriksson E, O'Brien S, Calil H, Ceskova E, et al. Clinical diagnostic criteria for premenstrual syndrome and guidelines for their quantification for research studies. Gynecol Endocrinol. (2007) 23:123–30. doi: 10.1080/09513590601167969
28. Tolossa FW, Bekele ML. Prevalence, impacts and medical managements of premenstrual syndrome among female students: cross-sectional study in college of health sciences, mekelle university, mekelle, northern Ethiopia. BMC Womens Health. (2014) 14:52. doi: 10.1186/1472-6874-14-52
29. Tschudin S, Bertea PC, Zemp E. Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch Womens Ment Health. (2010) 13:485–94. doi: 10.1007/s00737-010-0165-3
30. Potter J, Bouyer J, Trussell J, Moreau C. Premenstrual syndrome prevalence and fluctuation over time: results from a French population-based survey. J Womens Health. (2009) 18:31–9. doi: 10.1089/jwh.2008.0932
31. Gehlert S, Song IH, Chang CH, Hartlage SA. The prevalence of premenstrual dysphoric disorder in a randomly selected group of urban and rural women. Psychol Med. (2009) 39:129–36. doi: 10.1017/S003329170800322X
32. Takeda T, Tasaka K, Sakata M, Murata Y. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in Japanese women. Arch Womens Ment Health. (2006) 9:209–12. doi: 10.1007/s00737-006-0137-9
33. Cohen LS, Soares CN, Otto MW, Sweeney BH, Liberman RF, Harlow BL. Prevalence and predictors of premenstrual dysphoric disorder (PMDD) in older premenopausal women. The harvard study of moods and cycles. J Affect Disord. (2002) 70:125–32. doi: 10.1016/S0165-0327(01)00458-X
34. Golding JM, Taylor DL, Menard L, King MJ. Prevalence of sexual abuse history in a sample of women seeking treatment for premenstrual syndrome. J Psychosom Obstet Gynaecol. (2000) 21:69–80. doi: 10.3109/01674820009075612
35. SveindÓTtir H, BÄCkstrÖM T. Prevalence of menstrual cycle symptom cyclicity and premenstrual dysphoric disorder in a random sample of women using and not using oral contraceptives. Acta Obstet Gynecol Scand. (2000) 79:405–13. doi: 10.1034/j.1600-0412.2000.079005405.x
36. Lu D, Aleknaviciute J, Kamperman AM, Tamimi RM, Ludvigsson JF, Valdimarsdottir UA, et al. Association between childhood body size and premenstrual disorders in young adulthood. JAMA Netw Open. (2022) 5:e221256. doi: 10.1001/jamanetworkopen.2022.1256
37. El Dahr Y, de Azevedo Cardoso T, Syan SK, Caropreso L, Minuzzi L, Smith M, et al. Investigating biological rhythms disruptions across the menstrual cycle in women with comorbid bipolar disorder and premenstrual dysphoric disorder. Arch Womens Ment Health. (2022) 25:345–53. doi: 10.1007/s00737-022-01220-0
38. Rezende APR, Alvarenga FR, Ramos M, Franken DL, Dias da Costa JS, Pattussi MP, et al. Prevalence of premenstrual syndrome and associated factors among academics of a university in midwest Brazil. Rev Bras Ginecol Obstet. (2022) 44:133–41. doi: 10.1055/s-0041-1741456
39. Eldeeb SM, Eladl AM, Elshabrawy A, Youssef AM, Ibrahim MH. Prevalence, phenomenology and personality characteristics of premenstrual dysphoric disorder among female students at Zagazig University, Egypt. Afr J Prim Health Care Fam Med. (2021) 13:e1–9. doi: 10.4102/phcfm.v13i1.2924
40. Yang Q, Thornorethardottir EB, Hauksdottir A, Aspelund T, Jakobsdottir J, Halldorsdottir T, et al. Association between adverse childhood experiences and premenstrual disorders: a cross-sectional analysis of 11,973 women. BMC Med. (2022) 20:60. doi: 10.1186/s12916-022-02275-7
41. Younes Y, Hallit S, Obeid S. Premenstrual dysphoric disorder and childhood maltreatment, adulthood stressful life events and depression among lebanese university students: a structural equation modeling approach. BMC Psychiatry. (2021) 21:548. doi: 10.1186/s12888-021-03567-7
42. Pereira D, Pessoa AR, Madeira N, Macedo A, Pereira AT. Association between premenstrual dysphoric disorder and perinatal depression: a systematic review. Arch Womens Ment Health. (2022) 25:61–70. doi: 10.1007/s00737-021-01177-6
43. Di Florio A, Alexander D, Schmidt PJ, Rubinow DR. Progesterone and plasma metabolites in women with and in those without premenstrual dysphoric disorder. Depress Anxiety. (2018) 35:1168–77. doi: 10.1002/da.22827
44. Hantsoo L, Epperson CN. Allopregnanolone in premenstrual dysphoric disorder (PMDD): evidence for dysregulated sensitivity to GABA-A receptor modulating neuroactive steroids across the menstrual cycle. Neurobiol Stress. (2020) 12:100213. doi: 10.1016/j.ynstr.2020.100213
45. Timby E, Backstrom T, Nyberg S, Stenlund H, Wihlback AN, Bixo M. Women with premenstrual dysphoric disorder have altered sensitivity to allopregnanolone over the menstrual cycle compared to controls-a pilot study. Psychopharmacology. (2016) 233:2109–17. doi: 10.1007/s00213-016-4258-1
46. Bixo M, Johansson M, Timby E, Michalski L, Backstrom T. Effects of GABA active steroids in the female brain with a focus on the premenstrual dysphoric disorder. J Neuroendocrinol. (2018) 30:10.1111/jne.12553. doi: 10.1111/jne.12553
47. Smith SS, Shen H, Gong QH, Zhou X. Neurosteroid regulation of GABA(A) receptors: focus on the alpha4 and delta subunits. Pharmacol Ther. (2007) 116:58–76. doi: 10.1016/j.pharmthera.2007.03.008
48. Ullah A, Long X, Mat WK, Hu T, Khan MI, Hui L, et al. Highly recurrent copy number variations in GABRB2 associated with schizophrenia and premenstrual dysphoric disorder. Front Psychiatry. (2020) 11:572. doi: 10.3389/fpsyt.2020.00572
49. Barki M, Xue H. GABRB2, a key player in neuropsychiatric disorders and beyond. Gene. (2022) 809:146021. doi: 10.1016/j.gene.2021.146021
50. Fluoxetine. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (2012).
Keywords: bibliometric analysis, citations, premenstrual syndrome, trends, PMDD
Citation: Gao M, Zhang H, Wang C, Mou X, Zhu Q, Wang J and Gao D (2022) Top 100 Cited Papers on Premenstrual Syndrome/Premenstrual Dysphoric Disorder: A Bibliometric Study. Front. Psychiatry 13:936009. doi: 10.3389/fpsyt.2022.936009
Received: 04 May 2022; Accepted: 14 June 2022;
Published: 14 July 2022.
Edited by:
Karen Tabb, University of Illinois at Urbana-Champaign, United StatesReviewed by:
Jian Huang, Zhejiang University School of Medicine, ChinaCopyright © 2022 Gao, Zhang, Wang, Mou, Zhu, Wang and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongmei Gao, Z2N5XzExMkAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.