
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 16 September 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.933981
 Merna Attia1†
Merna Attia1† Fatma A. Ibrahim1†
Fatma A. Ibrahim1† Mohamed Abd-Elfatah Elsady1†
Mohamed Abd-Elfatah Elsady1† Mohamed Khaled Khorkhash1†
Mohamed Khaled Khorkhash1† Marwa Abdelazim Rizk1†
Marwa Abdelazim Rizk1† Jaffer Shah2*
Jaffer Shah2* Samar A. Amer3,4,5†
Samar A. Amer3,4,5†Background: Stress is manifested by different physical, cognitive, emotional, and behavioral stress-related symptoms, and everyone experiences it uniquely. The COVID-19 Pandemic has tremendously affected university students' lives. So, we conducted this study to determine the stress frequency, causes, determinants, and related symptoms involving physical, cognitive, emotional, and behavioral traits and coping strategies among university students in Egypt during the third wave of the COVID-19 pandemic, 2021.
Methods: Cross-sectional study targeted 1,467 randomly selected undergraduate university students, representing all colleges from 30 universities in Egypt, through a validated self-administrated questionnaire.
Results: The total stress-related symptom score was statistically significant (p < 0.05), higher among females, married, living on campus, with a (B) GPA, and those who had both organic and psychological disorders. The top 10 prevalent physical symptoms were headaches, chronic fatigue, hair loss, low back pain, neck pain, shoulders and arm pain, ophthalmological symptoms, acne, shakiness of extremities, and palpitations, respectively. The most reported symptoms regarding the cognitive, emotional, and behavioral aspects were anxiety and racing thoughts, moodiness and irritability, and excessive sleeping, respectively. Nine hundred and thirty-seven (63.9%) reported that the COVID-19 pandemic badly affected their lives, either directly or indirectly. The study showed that the prevalence of stress among university students is more than 97%. One thousand and five (68.5%) preferred isolation as a relieving technique.
Conclusion: Stress and its related physical, cognitive, emotional, and behavioral symptoms are prevalent among university students. Most of the university students who were recruited reported that the COVID-19 pandemic badly affected their lives and used negative ways to deal with stress, like staying alone and sleeping too much. Positive ways to deal with stress, like seeing a therapist or meditating, were less common.
Stress is the physiologic response in which various defensive mechanisms come into play to deal with a threatening or challenging situation (1). During stress, the nervous system releases stress hormones that trigger a fight or flight state. Stress can be positive, as the stress response helps people stay alert when needed. After the stressors have passed, the body returns to normal and relaxes. But experiencing stress frequently or constantly can cause wear and tear on different body systems. So, both mental and physical health can be badly affected (2).
Stress and its related symptoms can be triggered or exaggerated by many risk factors, including age, gender, marital status, personal characteristics, grade level, academic performance (3, 4), nature of the study, living conditions, financial problems (5), work environment (6), quality of sleep (7), chronic illness (8), facing massive life changes (9), and facing a pandemic like COVID-19 (10).
Worldwide, academic stress is very prevalent among university students, negatively affecting their mental health (11–14). Medical students are the most affected by stress and depression (15–17). Academic stress occurs due to the requirements of college life, such as frequent examinations, deadlines, poor time management, delayed assignments, poor housing, noise, overcrowding, working while studying, adjustment to a new environment or even country, the imbalance between academic and personal life, and many other personal problems (18).
The COVID-19 Pandemic has tremendously affected people's lives. University students were also affected physically and psychologically (19). Recognizably, college students had a higher prevalence of stress and other mental health issues during the pandemic (10). Many risk factors are implicated in increasing perceived stress during the pandemic, such as quarantine for more than 14 days, inadequate access to supplies, having a chronic medical illness, fear of infection, getting infected, or the death of a relative or loved one (20–22).
Stress is manifested by different symptoms, as everyone experiences stress uniquely. It may involve physical, cognitive, emotional, and behavioral symptoms (23, 24). Physical symptoms include musculoskeletal pain, chronic fatigue, breathing problems, palpitations, bloating, abdominal pain, and changes in bowel habits (25). Some other physical symptoms include headaches and migraines (23) and hair loss (26), as well as acne (27–29) and eye problems (30, 31).
Cognitive aspects include the following symptoms: poor concentration, memory problems, constant worrying and anxiety, and seeing the negatives only. Emotional symptoms include depression, agitation, irritability, and loneliness. Behavioral symptoms include: neglecting responsibilities, appetite changes, sleep disturbances, smoking, using alcohol or drugs, and various nervous acts such as nail biting (23).
Ignoring ongoing, chronic stress and its related symptoms can cause or worsen many serious health problems, including mental health problems, such as depression, anxiety, and personality disorders, which would reflect on their social and academic lives. It can also cause cardiovascular diseases, including heart disease, high blood pressure, abnormal heart rhythms, heart attacks, and strokes; obesity and other eating disorders; menstrual problems; sexual dysfunction, such as impotence and premature ejaculation in men and loss of sexual desire in men and women; skin and hair problems, such as acne, psoriasis, and eczema; and permanent hair loss; and gastrointestinal problems, such as GERD, gastritis, ulcerative colitis, and irritable colon (32).
People face stress with various coping strategies to reduce the pressure of stress. These strategies can be positive or negative. Positive techniques include: exercise as a positive strategy to divert attention from unfavorable thoughts and stop the stress cycle; hormones that reduce stress can be released while you are in a face-to-face interaction with a friend or relative; By triggering the body's relaxation response, relaxation techniques lower tension and increase emotions of joy; Getting enough sleep helps with fatigue relief and stress reduction; eating a healthy diet rich in fresh fruit and vegetables, omega-3 fatty acids, and high-quality protein helps to cope better with ups and downs (23, 33); and A psychiatric consultation can help you customize the most effective stress management techniques for your needs and lifestyle.
Negative stress-coping techniques include social isolation and loneliness that raise health risks comparable to those associated with alcohol use disorders or smoking 15 cigarettes a day, increasing the risk of premature mortality. Additionally, they are twice as detrimental to both physical and mental health as obesity (34, 35). Some people might believe that smoking or alcohol temporarily lessens stress. But over time, they can exacerbate stress, increasing the likelihood of mental and psychological issues in addition to alcohol dependence (36). Overeating processed and convenience foods, refined carbs, and sugary snacks can exacerbate the effects of stress on the body and have a negative impact (23).
Worldwide, COVID-19's spread is uncontrollable, and it has already had an impact on people and countries. Holmes et al. called for multidisciplinary scientific research to be at the forefront of the international response to the COVID-19 pandemic in order to provide evidence-based guidance on how to promote people's health and well-being during the pandemic (37). In response to this call, we're focusing on university students as a vulnerable group to age-related, academic, and COVID-19 related stressors during the third wave of the COVID-19 pandemic to learn more about their stress and health problems. So, we conducted this study to improve the overall health status and reduce the impact of stress among university students through determining and studying the stress prevalence, causes, determinants, stress-related symptoms (physical, cognitive, emotional, and behavioral symptoms) and stress coping strategies among undergraduate university students in Egypt during the COVID-19 pandemic, 2021.
The cross-section study targeted randomly selected undergraduate university students in Egypt who fulfilled the selection criteria that included undergraduate students, aged between 17 and 26, from public and private universities in Egypt and resident in Egypt during the study period, excluding students who had chronically complicated medical or psychological disorders that interfered with their participation such as complicated diabetes (Retinal detachment, diabetic foot, diabetic nephropathy), and complicated cardiovascular diseases e.g., chronic heart failure.
Egypt currently has 20 public universities (with about two million students) and 23 private universities (about 60,000 students). The sample size was calculated to be 489 by using the Epi–info program, which used the total number of 2,442,000 university students in Egypt, and due to a lack of data on the frequency of stress-related symptoms, we assumed that it was 50% based on the average prevalence of perceived stress scale in other studies in Egypt [62.3% in Fayoum, in 2017, and 54% in Ain Shams University in 2016] (38). As a multistage cluster sample, after considering the effect design, the sample size was tripled to increase the power of the study and to represent all targeted strata, which totaled 1,467 students.
A multistage sampling technique was used to recruit a representative sample through the following stages: (1) A random selection of two or three faculties from the 20 Egyptian governorates that contain universities, with the exception of Cairo (Egypt's capital, which contains more than 260,000 students and more than 43 faculties, and home to the majority of private universities in Egypt), from which we target 10 universities. (2) The sample was stratified by college or faculty type (13 practical and 13 theoretical) within each college. (3) The sample is then stratified by grade level for each college. (4) A simple random sample obtained from each university's most popular official social media platforms or websites for these colleges and classes (Facebook, WhatsApp, and Telegram groups). Students completed and submitted the self-administered online questionnaire after providing informed written consent. Reminder messages and reposting of the questionnaire's link were used to increase the response rate until the required sample is completed (see Supplementary materials 1, 2).
The Google form of the Arabic questionnaire, as it is the main language in Egypt, was designed to achieve the objectives of the study based on previous studies (23, 25–31, 33, 39), and was prepared as a well-structured, pretested, pre-coded, Arabic, self-administrated questionnaire. It was originally created in English before being translated into Arabic, except Section 4 (the Perceived Stress Scale), which had an Arabic validation in another study (39). The English version of the questionnaire was translated into Arabic by a bilingual panel consisting of two healthcare professionals and one externally qualified medical translator. Two translators who spoke English did a back translation, and if there were any questions, the original panel was asked.
A validating schedule was developed by six experts (three psychiatrists, one family medicine, and two public health and community medicine) for the questionnaire, after which it was tested for clarity and comprehension through a pilot study, which was conducted on 25 students. Their results were included in our study results. The calculated Cronbach's alpha was 0.79. It is composed of five main sections (see Supplementary material 3).
There were 11 questions (Q) that asked about their gender, age, nationality, marital status, residence, university name, college name, study nature, academic level, GPA, and if they had any health problems.
It is composed of 54 questions, that were well structured from the following studies (23, 25–31) to assess the four main domains (symptoms);
• Physical symptoms are assessed through 36 questions to evaluate the affection of eight systems as follows: the neuro-musculoskeletal system (5 Q). The gastrointestinal system (10 Q). The cardiovascular system (3 Q). Cutaneous system (skin and hair symptoms) (3 Q). The respiratory system (2 Q). The ophthalmological system (1 Q). The gynecological system (1 Q) (See Section 2 of the questionnaire).
• Cognitive symptoms are assessed through five Qs about concentration, memory problems, anxiety and overthinking, pessimism, and decision-making.
• Emotional symptoms are assessed through five Qs about depression and unhappiness, anxiety and agitation, feeling loneliness and isolation, moodiness, irritability, and anger, and if there are any other mental or emotional health problems.
• Behavioral symptoms are measured by answering eight questions about appetite, excessive sleeping, insomnia, withdrawing from groups and preferring to be alone, not doing their jobs, smoking, and biting their nails.
• Each question measured the occurrence rate of each symptom on the Likert Scale.
• The Likert scale has four points (never = zero, rarely = one, frequently or occasionally = two, and always = three).
• The total score of stress-related symptoms was 162; the physical symptom score was 108, the cognitive symptom score was 15, the emotional score was 15, and the behavioral score was 24.
• The top 10 symptoms were calculated by the sum of (often, sometimes, and always).
Exposure or infection history (themselves or their families), and students were allowed to select more than one answer (See Section 3 of the questionnaire).
Studying effects, such as isolation at home with suspension of study for a period of time, studying online, delayed exams, and exams replaced with research. All these options were introduced to participants as Egypt considered all these options as mitigation measures for students during the pandemic, and they differed according to the college and the nature of the study.
It's a 10-question validated scale (with the internal consistency of the PSS-10 and its positive and negative subscales were acceptable (coefficient alpha = 0.67, 0.79, and 0.89), to assess the severity of the perceived stress on a 4-point Likert Scale (never = zero, almost never = one, sometimes = two, often = three, and very often = four). Based on the PSS-10, the stress scale was classified into three categories: (0–13) low perceived stress, (14–26) moderate perceived stress, and (27–40) high-perceived stress (39).
University students were allowed to select more than one answer from many suggested coping strategies, such as isolation, sleeping, eating, praying, etc., and others, and write down their other coping strategies if they had them (see Section 5 of the questionnaire below). From articles by the Anxiety and Depression Association of America (ADAA) and the CDC, we came up with these choices (40, 41).
After the Exempt No. 6925-14-7-2021, IRP ethical approval was obtained from the institutional review board at Zagazig University, Egypt. The official college classrooms' online social media portals, such as Facebook, WhatsApp, and Telegram, were used to distribute the online Google form. The data was collected during May, 2021. To increase the response rate, we asked the admins to share, repost, and invite them to do so after they signed a written agreement that their identities would not be revealed and a weekly reminder until they finished the sample.
The collected data was coded and analyzed using the SPSS program version 23.0. The categorical variables were expressed as frequency (F) and percentage (%), and the chi-square test (X2) was used for analysis. Quantitative variables were presented as mean ± standard deviation (SD) or median according to the data distribution. The Kolmogorov-Smirnov test was used to determine whether continuous data was considered skewed or not normally distributed. A t-test was used to confirm this. The normally distributed variables were analyzed using ANOVA and Post-Hoc tests, while non-parametric variables were analyzed using the Mann-Whitey U test, with statistical significance set at p 0.05. To test the association between two continuous variables persons correlation coefficient test was used. A simple logistic regression analysis within A generalized linear model technique was used to examine the association of each potential factor. With the binary outcome of vaccination adverse effects (no or mild stress, and moderate or severe stress).
Out of the 1,467 students, 1,157 (78.9%) were females, with a mean age of 23.0 years (SD = 21.2 ± 1.7), 1,431 (97.6%) were Egyptians, 1,262 (86.0%) were single, 653 (44.5%) living in urban areas, and 991 (76.6%) in practical colleges, with a (B) GPA of 593 (40.4%), and 761 (51.9%) were without comorbidities (Table 1).
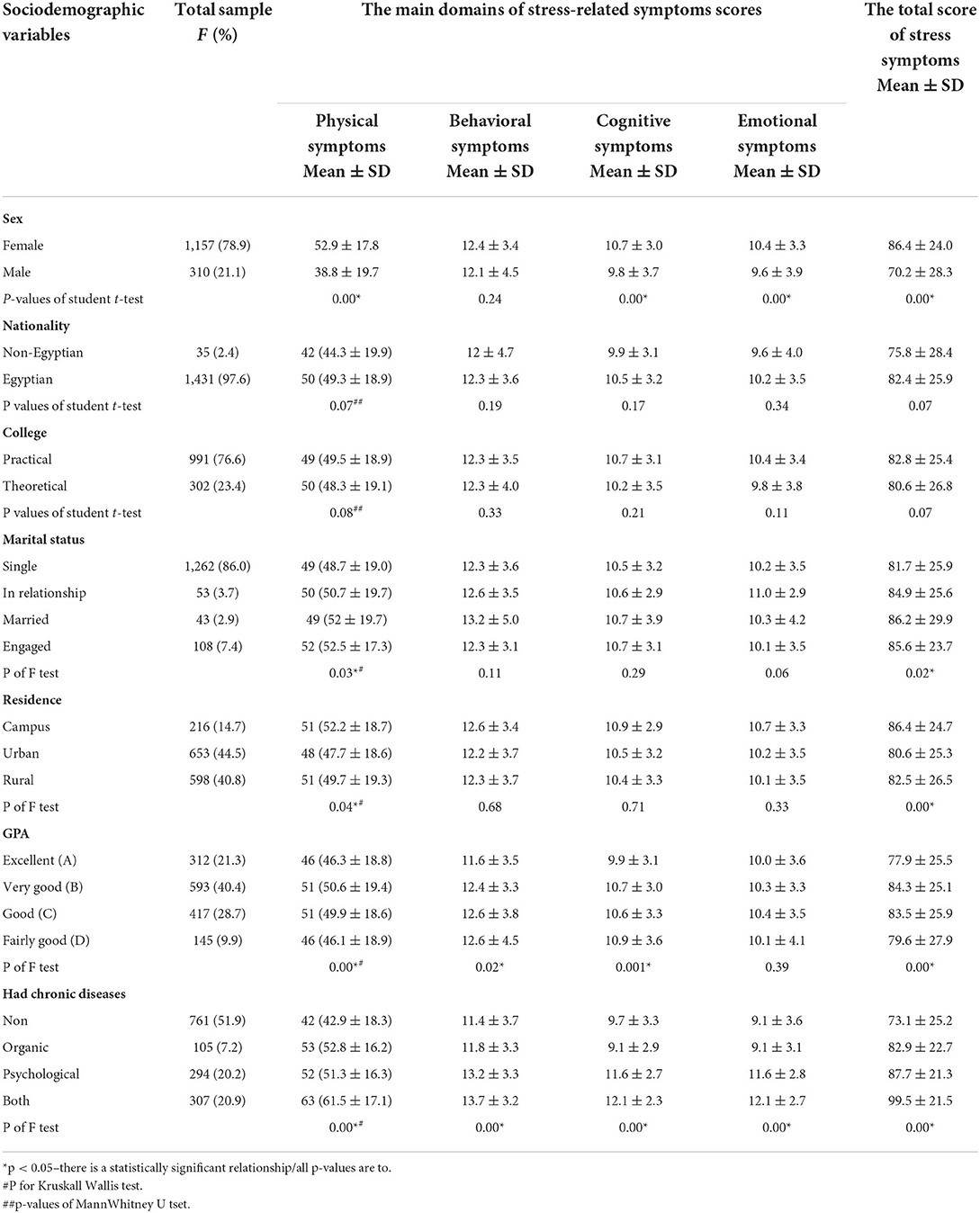
Table 1. The Sociodemographic Characteristics, and its relationship with the stress-related symptoms score (per domains and total score).
As regards the stress-related physical symptoms, the top 10 symptoms in descending order were: headache 1,225 (83.5%), chronic fatigue 1,212 (82.6%), hair loss 1,104 (75.3%), low back pain 1,036 (70.6%), neck pain 994 (67.8%), shoulders and arms pain 929 (63.3%), ophthalmology related symptoms 889 (60.6%), acne 883 (60.2%), shakiness of extremities such as hands 879 (59.9%), and palpitations 866 (59%). On the other hand, the following symptoms were experienced as never before: difficulty swallowing, painful oral ulcers, and increased body temperature, by 695 (47.4%), 664 (45.3%), and 594 (40.5%), respectively (Table 2; Figure 1).
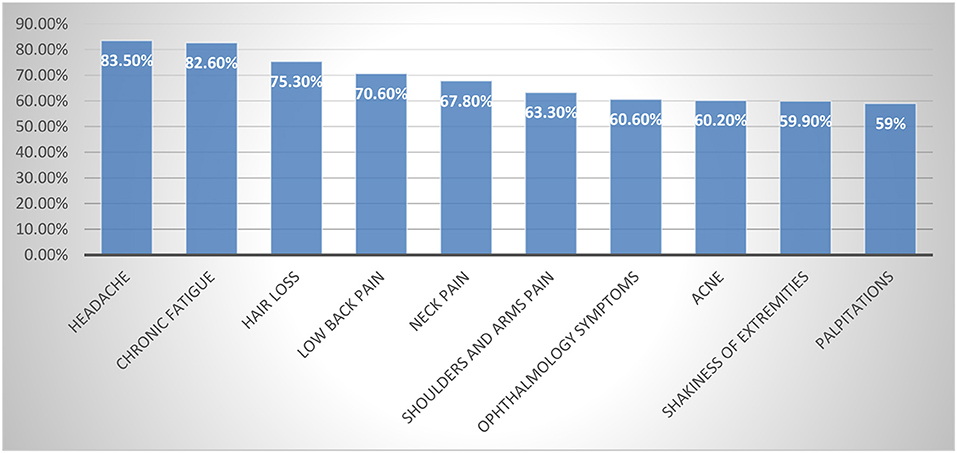
Figure 1. The frequency of the top 10 stress-related physical symptoms among the studied university students. Top ten symptoms were calculated by the sum of (often or sometimes and always).
As regards cognitive, emotional, and behavioral stress-related symptoms, university students reported that the most common cognitive symptoms were anxiety and racing thoughts 1,313 (89.5%), followed by poor concentration 1,274 (86.8%). Emotional symptoms including moodiness, irritability, or anger were 1,288 (87.8%), and depression and unhappiness were 1,232 (84%). Behavioral symptoms were excessive sleeping 1,142 (77.8%), followed by avoiding gatherings and preferring isolation 1,131 (77%) (Table 3).
The stress-related symptom score: The mean score of total stress-related symptoms was significantly (p < 0.05) higher in females (86.4 ± 24.0), married (86.2 ± 29.9), living on campus (86.4 ± 24.7), B GPA (84.3 ± 25.1), and students who had both organic and psychological disorders (99.5 ± 21.5). The total number of stress-related symptoms had no statistically significant (p > 0.05) relationship with either nationality or faculty type (Table 1).
Stress-related symptoms were significantly higher among females (p = 0.001). Cognitive and emotional symptoms were significantly higher among females. Stress symptoms were significantly associated with stressed married students (p = 0.02), particularly the physical symptoms (p = 0.03). They were significantly higher among students living on campus (p = 0.00), particularly physical symptoms (p = 0.04). Students with a B GPA showed a significant prevalence of stress symptoms (p = 0.001), particularly physical (p = 0.001), cognitive (p = 0.001), and behavioral (p = 0.02). Students who suffered from organic and psychological disorders revealed significantly prevalent stress symptoms involving the four domains (p = 0.001).
Nine hundred thirty-seven university students (63.9%) reported that COVID-19 affected their lives directly and/or indirectly. As regards the exposure/infection history, 708 (72.8%) got mild COVID-19 symptoms, 842 (57.4%) were isolated at home, and 377 (38.5%) had one of their relatives die after infection. As regards the effect of the COVID-19 Pandemic on their studies, 783 (53.4%) studied online, and 664 (45.3%) of their exams were delayed. There was a moderate to good (r > 0.76) positive or direct statistically significant association (p = 0.001) between the effects of COVID-19 on students' health status or their relatives among the students whose lives were negatively affected (T = 937) and the total PSS-10 and the total stress-related symptoms and its four (emotional, cognitive, physical, and behavioral) domains (Table 4).
The majority of the studied university students suffered from moderate and severe stress, 960 (65.4%) and 474 (32.3%), respectively. The mean ±SD) of the PSS was significantly (p < 0.05) higher among females (24.5 ± 5.7), non-Egyptians (32.2 ± 6.5), students with low GPA (25.1 ± 6.1), and students who suffered from both organic and psychological disorders (26.6 ± 4.9). On the other hand, it showed no statistically significant relationship (p > 0.05) with the type of study, residence, and relationship status. The total PSS score was significantly (p < 0.05) correlated with the coping strategies. The more the positive adapted coping strategies, the lower the PSS (r = −0.23), and positively correlated with the adapted negative coping strategies (Table 5).
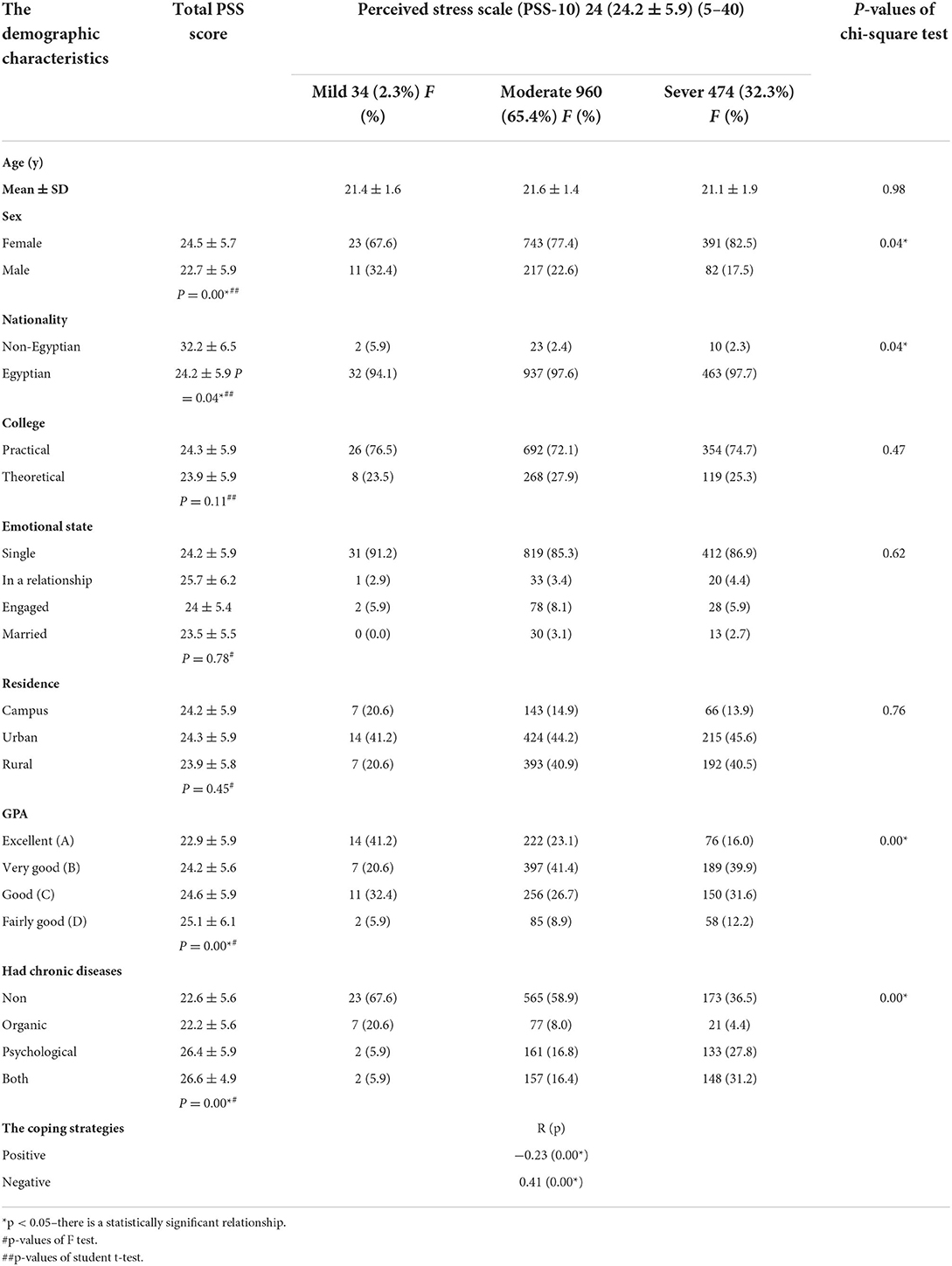
Table 5. The Perceived Stress Scale (PSS-10) and its relationship with the demographic characteristics.
Females OR [95% C.I] 2.65 [1.61–11.5], lower GPA OR [95% C.I] 3.36 [1.5–14.9], those with psychological disorders OR [95% C.I] 4.58 [4.07–19.6], and those with both (organic and psychological disorders) OR [95% C.I] 4.79 [1.12–20.4] were factors (predictors) that increased the risk of being under moderate to severe stress (Table 6).
As regards coping strategies during stressful times, the recruited university students 1,005 (68.5%) preferred isolation, 913 (66.5%) excessive sleeping, and praying (912, 62.2%). The least common strategies reported were 46 (3.1%) consulting a psychiatrist and 0.2% meditating (Figure 2).
During the third wave of the COVID-19 pandemic, the majority of university students in Egypt reported that the pandemic affected their lives in either direct or indirect ways. The majority suffered from moderate to severe perceived stress that was manifested by many physical, emotional, behavioral, and cognitive stress-related symptoms. Both students' perceived stress scales and stress-related symptoms had many determinants that we discussed in detail later.
In terms of nonspecific stress-related symptoms, we reported that 1212 (82.6%) of university students experienced stress-related fatigue, also known as “adrenal fatigue,” as revealed by (42–44). Stress impairs adrenal gland function, which has an impact on energy levels via 16 different mechanisms in the brain, gut, immune system, endocrine system, and mitochondria (the cellular energy generators of your body). e.g., It depletes the endocannabinoid system, changes the balance of neurotransmitters in the brain (serotonin, dopamine, and acetylcholine), disrupts the hypothalamus-pituitary-adrenal (HPA) axis, and reduces thyroid hormone levels (45). While 853 people (58.2%) reported stress-related dizziness, this was consistent with the stress effect on the vestibular system. This proved the causal association between stress and dizziness (46–48).
As regards the stress-related neuromusculoskeletal system, it is significantly impacted by stress, with low back pain accounting for 1,036 (70.6%), neck pain accounting for 994 (67.8%), and shoulders and arms pain accounting for 929 (63.3%) of university students. This is consistent with the findings of numerous studies conducted in a variety of workplaces in a variety of countries that demonstrated a link between stress and musculoskeletal pain complaints (49–52).
In terms of stress-related neurological symptoms, 879 (59.9%) of university students reported shakiness in their extremities, such as their hands. In conformity with the information provided in (53). When the body prepares to deal with a stressor, it perceives anxiety as a signal that there is a need to evacuate from danger, thus muscles become ready to respond, resulting in trembling, twitching, and even shaking (54). Additionally, stress can exacerbate psychogenic tremors [underlying psychiatric problems like depression or post-traumatic stress disorder (PTSD)], but these psychogenic tremors can be reduced or eliminated when people are preoccupied (53).
Tension-type headaches (TTH) and tightness around the head were reported by 1,225 (83.5%) of university students consistently with (55–57). Although the fundamental causes are currently unclear, Simultaneously, research in healthy humans is beginning to shed light on the link between stress and pain processing in the central nervous system, particularly in the central pain systems that are thought to be dysfunctional in TTH. Moreover, 861 (58.7%) of students suffered from stress migraine (a debilitating, throbbing, and severe pain present only on one side of the head) similar to (58, 59). Stress and anxiety can also trigger TTH and migraine and contribute to its chronicity (60). But stress headaches and migraine attacks mess with your head differently.
In terms of stress-related dermatological symptoms, 1,104 (75.3%) of university students experienced hair loss during stressful situations, making it the third most common symptom after headaches and chronic fatigue. According to (26), corticosterone (stress hormone) is a systemic inhibitor of hair follicle stem cell function. Chronic stress disrupts tissue homeostasis, resulting in hair loss. While 883 (60.2%) of those surveyed had acne, acne is strongly linked to stress, according to (27–29). Acne in stressed females may be due to associated menstrual disturbances, which 667 female university students (61–65) reported having.
Ophthalmology stress-related symptoms were reported by 889 (60%) students in the form of blurred vision, double vision, fogginess, and any other eye-related complaints. Consistently with (30), who found that symptomatic vitreous floater patients showed substantial levels of psychological distress and that the severity of floater symptoms was significantly associated with that distress. They agreed with (31) that dry eye disease is more common in those who are depressed, anxious, or stressed.
As regards stress-related respiratory symptoms, Similar to (66, 67), in this study we reported shortness of breath among 668 (45.5%) and rapid breathing among 581 (39.6%) university students, known as psychogenic or anxiety dyspnea, or dyspnea catastrophizing (dyspnea that is not related to effort). These difficulties in filling the lung are correlated with the anterior cingulate cortex (ACC) in the brain. The ACC's role is to process negative affective states such as anxiety (68–70).
Stress-related cardiovascular diseases (CVD) were palpitations of 866 (59%), chest pain of 532 (36.3%), and increased blood pressure of 424 (28.9%), respectively. Musey et al. (71, 72), Redina and Markel (73), Damtie et al. (74) found similar results. Because the sympathetic nervous system and the hypothalamus-pituitary-adrenal (HPA) axis are engaged, more catecholamines, glucocorticoids, and inflammatory cytokines are produced, resulting in increased cardiac output, skeletal muscle blood flow, salt retention, and cutaneous vasoconstriction (75).
Stress-related gastrointestinal (GIT) symptoms included bloating sensation and abdominal discomfort as the most reported symptoms by 861 (58.7%), and abdominal pain was reported by 822 (56%). According to prior research (76–79), negative emotional stress both increases and exacerbates IBD symptoms. Catecholamines and cortisol are both released by the brain in stressful situations, and the digestive system can't get away from the combined effects of both hormones on the body, which reduce intestinal motility (80).
In agreement with (61–65), we found that 667 (57.6%) of female participants had menstrual disturbances, such as irregular and/or heavy menses. This is due to stress's role in lowering circulating gonadotropins and gonadal steroid hormones; consequently, persistent stress can result in full reproductive function impairment (80).
The main complaints were anxiety and racing thoughts, followed by poor concentration, memory issues, poor judgment, and only perceiving the negative. It was in line with (81–84). Stress can shut down many centers in the prefrontal cortex, which orchestrates the brain's activity for intelligent regulation of behavior, thought, and emotion and allows the primitive brain to take over, causing mental paralysis and panic. In addition to losing self-control, they are likely to make poor lifestyle choices, including bad decisions (85).
Moodiness, irritability, or rage are the most commonly reported symptoms, followed by depression and unhappiness, loneliness and isolation, anxiety, and agitation. These findings are in accordance with others (86–89). This is the body's hormonal stress-response mechanism, whereby stress activates the hypothalamic-pituitary-adrenal (HPA) axis, and glucocorticoids, including the cortisol hormone, are released into the bloodstream, increasing the risk of depression. Stress also decreases the volume of the hippocampus (the brain part that affects emotional reactions). This could result in depressive symptoms (90).
Excessive sleeping, withdrawing from gatherings, and preferring isolation were the most commonly reported symptoms, respectively. While smoking was the least reported behavioral change. These findings are consistent with outcomes from previous studies (91–94).
Seven hundred twenty-five (49.54%) students reported an increase in appetite, while 854 reported a reduction (58.2%). This depends on the type of stress, because stress alters food intake, raising or decreasing it (95, 96). In the short term, stress can reduce appetite as the nervous system sends signals to the adrenal glands to secrete epinephrine, which triggers the body's fight-or-flight response that temporarily puts eating on hold. But if stress persists, the adrenal glands release cortisol, which increases appetite and increases the motivation to eat (97).
Stress activates the sympatho-adreno-medullary (SAM) and HPA systems. Hormones like melatonin and others from the HPA axis modulate the sleep-wake cycle, while its dysfunction can disrupt sleep (98).
We found that 937 (63.9%) reported that the COVID-19 pandemic badly affected their lives, either directly or indirectly. Consistently with (99) which proved that COVID-19 confinement directly caused moderate to severe stress among university students. And agreeing with (76), stated that COVID-19 anxiety was significantly related to Crohn's disease symptom severity and social dysfunction. There were many reported causes of this stress, including infection with COVID-19, which was reported by a total of 828 students with different severities. Three hundred and seventy-seven (38.8%) of students experienced a relative's death with COVID-19, and 842 (57.4%) experienced home isolation. This was because on May 31st, the total number of confirmed cases was 267,171 cases, and 15,309 deaths by default affected all inhabitants in Egypt, including university students (100), and stress related to the high level of widespread vaccine hesitancy and worries about the COVID-19 vaccine, that only around one million citizens have been vaccinated out more than 100 million (101). In addition to the effect of the pandemic on their study, 783 (53.4%) studied online, 664 (45.3%) delayed exams, and 239 (30.2%) replaced. Even though Egypt thought these strategies would help stop the spread of the pandemic, all of these new experiences in learning and exams could be stressful and difficult for both the universities and students at this time (102). Furthermore, there are other factors like family responsibilities, personal health concerns, health problems that affected the family, and the economy that played a role.
In the students whose lives were adversely affected (T = 937) during the pandemic, there was a moderate to good (r > 0.76), positive or direct statistically significant association (p = 0.001) between the effects of COVID-19 on students' health status or that of their relatives, and the overall stress-related symptoms and its four subtypes. In addition to COVID-19-related stress, the post-COVID-19 condition may be to blame for this. Additionally, as many as 828 (88.4%) of the population may have post-COVID-19 syndrome. Although there are many different, changing, and fluctuating clinical symptoms, fatigue and neurocognitive impairments are the most common. Post-COVID-19 syndrome, which manifests as a variety of emotional symptoms like depression and anxiety; physical symptoms like headaches, fatigue, and menstrual changes; behavioral symptoms like appetite and sleep disturbance; and post-COVID-19 cognitive impairment. Although post-COVID-19 syndrome is not well understood, its diagnostic criteria have not undergone adequate psychometric evaluation (103, 104). It is critical to distinguish it from stress-related symptoms.
In May 2021, our study showed that the frequency of moderate to severe stress among university students was more than 97% (65.4% moderate and 32.3% severe). This can be attributed to a variety of factors, including the fact that 937 (63.9%) of them reported that the COVID-19 pandemic had a negative impact on their lives, either directly or indirectly. Furthermore, during stressful times, the majority of recruited university students adopted negative coping strategies, preferring isolation and excessive sleeping. Positive coping strategies, consulting a psychiatrist, and meditation were the least reported.
The frequency of moderate-to-severe stress varied in different years and countries, but all were lower than ours. For example, 92.5% in Pakistan in 2013, 88.9% in Minia, Egypt in April 2017, 71.9% in Saudi Arabia in 2012, 62.3% in Fayoum, Egypt in 2017, and 54% in Ain Shams University in 2016 (38). This may be attributed to the challenges of the COVID-19 pandemic because more than 78.0% of the recruited students were females, who are more susceptible to stress than males, and 377 (38.8) of them experienced the death of a family member as a result of COVID-19 (death of a loved one is the number two of the top five stress drivers).
In terms of gender, many studies (16, 105, 106) found a significantly higher PSS in females, consistent with our finding; OR [95% C.I] was 2.65 [1.61–11.5] (p = 0.00). Numerous neurobiological and behavioral factors may contribute to this gender disparity in stress response. Acute HPA, ACTH, and autonomic response levels in adult women have been found to be lower. Additionally, women's sexual hormones lower HPA and sympathoadrenal reactivity. As a result, the brain receives slow cortisol feedback, has a harder time controlling its stress response, and is more likely to experience depression in women. They are also vulnerable to the depressive impacts of interpersonal problems. When women engage in “tend-and-befriend” behaviors, their right prefrontal brain activity, cortisol levels, and left orbitofrontal cortex activity are all reduced. It involves lowering cortisol levels, the stress response, and attachment-related caregiving mechanisms that usually control sympathetic and HPA arousal, as well as the limbic system, which is made up of the ventral striatum, putamen, insula, and cingulate cortex (107).
Other research (108) showed no discernible difference in stress levels between men and women. Others claimed that male students had higher stress levels than female students. However, this might be due to the cultural, religious, and female obligations of certain groups. Cultural factors including relationship issues with parents and instructors (such as unfairness, mistreatment, and severe criticism) and substance abuse—most commonly using mild tranquilizers—were noted more frequently by Egyptian women. Mule and Barthel (16) addressed the societal changes in Egypt, where there has been an increase in women's engagement in the labor market and, to some extent, in politics. Additionally, globalization and exposure to Western culture have steered this traditionally Islamic nation toward alternate gender values. The lack of gender differences may also be attributed to the student body's extremely selectivity and homogeneity as well as its particular personal attributes that are valued in the competitive environment of medical school (17). In addition to their regular tasks, which include taking care of the home.
In terms of nationality, Non-Egyptians had significantly (p = 0.04) higher levels of stress (moderate to severe) than Egyptians, and being Egyptian was a protective factor OR 0.55, and 95% C.I [0.27–1.14], consistent with previous research that found international students to be more stressed than domestic students, which is described as acculturative stress, which is attributed mainly to the unfamiliar cultural and environmental changes, the different educational systems, and limited language proficiency (109, 110).
In terms of academic performance, students with low GPA were significantly more stressed than the others OR 3.36, and 95% C.I [1.5–14.9], (p = 0.00), which is in line with the results of other studies that have found that students with high academic performance experience less stress (105, 106). Similar studies have demonstrated that clinical outcomes like suicidality are influenced by academic stress. Subjects who are at risk for poor clinical outcomes frequently approach suicide by searching online for news and information about self-harm and suicidal behaviors, even if they are good ethical leaders (111). Additionally, affective temperament-types were more strongly and independently associated with poor clinical outcomes than were major depressive disorder diagnoses or other variables that might be linked to academic stress and poor clinical outcomes (112).
In terms of comorbidity, we found that university students with psychological disorders OR 4.58, 95% C.I [4.07–19.6] and those with both organic and psychological disorders OR 4.79, 95% C.I [1.12–20.4] had a significantly higher prevalence of stress (p = 0.00). That was also related to vaccination hesitancy as vaccination priority was given to patients with chronic diseases. In addition to the higher perceived severity and susceptibility (101).
In terms of coping strategies, the total PSS score was significantly (p < 0.05) correlated with the coping strategies. The more the positive adapted coping strategies, the lower the PSS (r = −0.23) and it was positively correlated with the adapted negative coping strategies. This explains why (we advise reading Doing What Matters in Times of Stress: An Illustrated Guide). The need to give people useful tools to help them manage stress is emphasized in the stress management book Coping with Distress. Self-help techniques can be practiced every day for as little as a few minutes (113). Consequently, it is crucial to create and implement health education programmes for college students.
According to the various coping techniques described by (40, 41). Coping strategies for stress are different from one another. Students resorted to the following ways to relieve stress: One thousand and five (68.5%) preferred isolation, while 913 (66.5%) preferred excessive sleeping as the most common coping method, although these coping strategies may be symptoms of stress (23). That is in line with the fact that, when things are stressful, students tend to avoid social situations by hiding or sleeping more than usual.
More than four hundred university students (31.3%) try eating as a way to emit the angry or stressful energy contained within. This can be attributed to the fact that stress increases appetite and a hunger sensation, in addition to sugar cravings, which serve as a symptom as well as a coping mechanism. Cravings lead to poor eating habits, such as eating highly processed foods that are low in protein and fiber but high in glycemic load. This causes inflammation, which suppresses the neurotransmitter orexin directly (which is key in regulating wakefulness and energy levels). Energy drinks, ironically, deplete your energy levels the most. Clinical studies also revealed high food consumption, specifically of palatable foods, during periods of psychological stress (95). Glucocorticoids make people eat more food that they find tasty. This is linked to reward-based eating as a way to lessen the stress response (92, 96).
Referring to the religious background of the Egyptian society, 912 (62.2%) university students were praying to relieve their stress. Five hundred four (34.4%) preferred speaking with a friend over talking with family. Three hundred forty-six (23.6%), because speaking with others can trigger hormones that relieve stress (23). Logically, students would share similar stressors based on their age and study nature. Therefore, they would understand each other more than their families. Only 11.02% adapted exercise that serve as a distraction from negative thoughts and pause the negative cycle of stress (114).
While the least followed coping method was smoking, 66 (4.5%), this is attributed to the fact that some people smoke as self-medication to ease feelings of stress. As nicotine creates an immediate and temporary sense of relaxation, people falsely think that smoking reduces stress and anxiety. But actually, smoking increases anxiety and tension, plus there its negative effects on health (115). This small percentage may be attributed to the fact that 78.9% of the recruited students were females, and smoking is not acceptable among females in Egypt due to cultural factors besides religious factors.
Coping strategies employed by students in dealing with academic stress vary among different studies. For example, in Nigeria, for example, the top six coping strategies were as follows: adopt a positive attitude; yell and scream; exercise; talk to friends; think about their goals to put things in perspective; and go shopping or to a place of worship (114). Students at the UEW Winneba Campus preferred the emotion-focused style to the problem-focused style in dealing with stress (116). A survey of undergraduate pharmacy students at the University of Khartoum revealed that the most frequent strategies were praying (84.4%) and maintaining some control over the situation (61.9%) (117). In Hong Kong, Chinese university students seemed to prefer positive coping strategies (namely, “Problem Solving” and “Seek Social Support”), especially “Problem Solving” (118), while in Poland, there are various coping strategies which are preferred by different categories of students (119).
Unfortunately, only 46 (3.1%) went to a psychiatrist, which helped to personalize the best healthy strategies to deal with stress according to everyone's needs and lifestyle (34). That may be attributed to the lack of students' awareness of their mental health, fearing stigma, the cost, and their tight timetable. There were also other ways with a minimal percent described by students. Only 3 (0.2%) of the recruited university students said they adopted relaxation techniques such as meditation, yoga, and deep breathing to reduce stress and boost feelings of joy through activation of the body's relaxation response, which increases concentration, reduces stress and anxiety, alleviates depression, and enhances our overall mental health (23).
Lastly, stress, according to our research, manifests itself not just as psychological distress but also as a variety of physical, cognitive, emotional, and behavioral manifestations. Moank of factors that affected by stress, appeared to increase during covid (120–122).
The study was conducted on a large sample. The sample was randomly stratified to represent all the university students in Egypt. It included students from 20 governorates, 30 public and private universities, 13 practical and 13 theoretical colleges, and from all the academic grades.
The questionnaire used to get the data was well-structured, validated, and detailed. It asked 54 questions about stress-related symptoms and how often people said they had them, on a scale of one to four (never, rarely, often, sometimes, and always).
The study didn't just look at the common psychological stress-related symptoms. It also looked at the physical, cognitive, emotional, and behavioral aspects of stress, which haven't been talked about as much in the literature before.
Data was collected at the end of the semester in May 2021, during the 3rd wave of the COVID-19 pandemic. Students are typically stressed during this time as they prepare for finals, which gives an idea of the current associated symptoms. This decreases the recall bias in this cross-section study.
First, our study has all the limitations of observational studies, such as bias and confounding issues. Second, the study depended on an online self-administered questionnaire, which reduced the accuracy of collected data because of recall and availability bias. Furthermore, it was a self-administered questionnaire without a complete clinical examination to exclude other organic causes. Third, the poor response rate from some groups, such as males and theoretical college students. Fourth, when we talk about new types of stress that haven't been studied before, it's hard to tell which of the findings about stress are caused by the end of the semester or COVID problems. Also, the students used a variety of coping techniques to deal with their stress, which we don't know about. Fifth, we couldn't prove the associations as a cross-sectional study. Finally, there is no baseline or pre-pandemic assessment.
More than half of the recruited students reported that the COVID-19 pandemic badly affected their lives, either directly or indirectly. Perceived stress and stress-related symptoms were prevalent among university students during the third wave of the COVID-19 pandemic, which was manifested with many physical, cognitive, emotional, and behavioral stress-related symptoms. The top 10 prevalent physical symptoms were headaches, chronic fatigue, hair loss, low back pain, neck pain, shoulders and arm pain, ophthalmological symptoms, acne, shakiness of extremities, and palpitations, respectively. The most reported symptoms regarding the cognitive, emotional, and behavioral aspects were anxiety and racing thoughts, moodiness, and excessive sleeping, respectively. Perceived stress is significantly higher among females, international students, those with low GPA, and students who have organic and psychological diseases. The majority of recruited university students during stressful times adopted negative coping strategies (preference for isolation and excessive sleep), while positive coping strategies (consulting a psychiatrist and meditation) were the least reported.
(1) In order to raise awareness of students' mental health, we propose that the results of this study, which demonstrate how demanding academic life can be, be communicated with stakeholders at every university. Ours emphasizes the stresses of academic life, calling for increased attention to and support for students' mental health while also urging universities to provide funded psychiatric visits and other stress-reduction measures.
(2) Developing and implementing health education programs for college students, particularly risky groups (females, international students, students with low GPA, and students with organic and psychological diseases), about the various aspects of stress that can affect them in order to avoid unnecessary investigations; reducing student drug abuse because they frequently use over-the-counter drugs to relieve pain or other unexplained physical symptoms; and early detection with a better diagnosis. Furthermore, educating students on the physical symptoms of stress will reduce the number of times they visit unnecessary specialists to explain the effects of academic stress on their health; increase awareness of stress-related symptom, and offer the best coping mechanisms in order to improve their mental health and well-being.
(3) Providing affordable, accessible, and confidential mental health support services in all colleges and universities through well-trained social workers, life coaches, and psychiatrists for the rapid and effective management of all related stress and mental and psychological disorders among university students.
(4) Governments and the media should try to get rid of the old-fashioned stigma of mental disorders and make it more common for people to go to a psychiatrist.
(5) (Doing What Matters in Times of Stress) is based on informed evidence and extensive field testing for anyone who experiences stress, wherever they live and whatever their circumstances. An Illustrated Guide that we recommend: Coping with Distress is a stress management book for dealing with adversity. The goal of the handbook is to provide people with practical tools to assist them in managing stress. Self-help approaches can be practiced in as little as a few minutes per day. The guide can be used alone or in conjunction with the audio exercises, which are available in 17 languages (113).
(6) Additional research would be conducted on different populations in different countries to prove and strengthen these findings, to focus on each reported symptom, to try to clarify the mechanisms of these associations because many symptoms occur with unknown mechanisms; to improve diagnosis with early detection and proper management through referral to a psychiatrist; to study and compare the effectiveness of each coping strategy, and to provide recommendations for people.
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
The studies involving human participants were reviewed and approved by Institutional Review Board at Zagazig University (#6925). The patients/participants provided their written informed consent to participate in this study.
Conceptualization: MA and SA. Methodology: MA and SA. Software: JS. Supervision: MA, SA, and JS. Validation: MA, MR, and SA. Formal analysis and supervision: SA. Data curation: MA, FI, ME, MK, MR, and SA. Writing—review and editing and visualization: MA and SA. All authors writing—original draft preparation and have read and agreed to the published version of the manuscript.
We would like to thank all students who accepted to participate in our survey. We also appreciate the role of colleges' official online groups that welcomed sharing the survey's link.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.933981/full#supplementary-material
Q, Questions; F, Frequency; %, Percentage; SD, Standard deviation; PSS, Perceived Stress Scale; fig, Figures; ANOVA, Analysis of Variance; HPA, Hypothalamus-pituitary-adrenal axis; PTSD, Post-Traumatic Stress Disorder; TTH, Tension-Type Headaches; ACC, Anterior cingulate cortex; CVD, Cardiovascular Diseases; GIT, Gastrointestinal Tract; SAM, Sympatho-Adreno-Medullary.
1. Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: a review. EXCLI J. (2017) 16:1057. doi: 10.17179/excli2017-480
2. Mental Health Foundation. Stress (2021). Available online at: https://www.mentalhealth.org.uk/a-to-z/s/stress (accessed June 2, 2021).
3. Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. (2015) 141:354. doi: 10.4103/0971-5916.156571
4. Ta VP, Gesselman AN, Perry BL, Fisher HE, Garcia JR. Stress of singlehood: marital status, domain-specific stress, and anxiety in a national US sample. J Soc Clin Psychol. (2017) 36:461–85. doi: 10.1521/jscp.2017.36.6.461
5. Hayes A, Hoover JN, Karunanayake CP, Uswak GS. Perceived causes of stress among a group of western Canadian dental students. BMC Res Notes. (2017) 10:1–9. doi: 10.1186/s13104-017-2979-9
6. Bhui K, Dinos S, Galant-Miecznikowska M, de Jongh B, Stansfeld S. Perceptions of work stress causes and effective interventions in employees working in public, private and non-governmental organisations: a qualitative study. BJPsych Bull. (2016) 40:318–25. doi: 10.1192/pb.bp.115.050823
7. Alotaibi AD, Alosaimi FM, Alajlan AA, Abdulrahman KAB. The relationship between sleep quality, stress, and academic performance among medical students. J Family Community Med. (2020) 27:23. doi: 10.4103/jfcm.JFCM_132_19
8. Vancampfort D, Koyanagi A, Ward PB, Veronese N, Carvalho AF, Solmi M, et al. Perceived stress and its relationship with chronic medical conditions and multimorbidity among 229,293 community-dwelling adults in 44 low-and middle-income countries. Am J Epidemiol. (2017) 186:979–89. doi: 10.1093/aje/kwx159
9. Chiang YC, Chu M, Zhao Y, Li X, Li A, Lee CY, et al. Influence of subjective/objective status and possible pathways of young migrants' life satisfaction and psychological distress in China. Front Psychol. (2021) 12:1956. doi: 10.3389/fpsyg.2021.612317
10. Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2025591. doi: 10.1001/jamanetworkopen.2020.25591
11. Abebe AM, Kebede YG, Mengistu F. Prevalence of stress and associated factors among regular students at Debre Birhan governmental and nongovernmental health science colleges North Showa zone, Amhara region, Ethiopia 2016. Psychiatry J. (2018) 2018:7534937. doi: 10.1155/2018/7534937
12. Jia YF, Loo YT. Prevalence and determinants of perceived stress among undergraduate students in a Malaysian University. J Health Transl Med. (2018) 21.
13. Asif S, Mudassar A, Shahzad TZ, Raouf M, Pervaiz T. Frequency of depression, anxiety and stress among university students. Pak J Med Sci. (2020) 36:971. doi: 10.12669/pjms.36.5.1873
14. Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. (2017) 255:186–94. doi: 10.1016/j.psychres.2017.05.027
15. Pacheco JP, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry. (2017) 39:369–78. doi: 10.1590/1516-4446-2017-2223
16. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. (2016) 50:456–68. doi: 10.1111/medu.12962
17. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
18. Managing, Stress (n,.d.). University of St Andrews. Available online at: https://www.st-andrews.ac.uk/students/advice/leaflets/stress/ (accessed June 3, 2021).
19. Hamaideh SH, Al-Modallal H, Tanash MA, Hamdan-Mansour A. Depression, anxiety and stress among undergraduate students during COVID-19 outbreak and “home-quarantine”. Nursing Open. (2021) 9:1423–31. doi: 10.1002/nop2.918
20. Kassir G, El Hayek S, Zalzale H, Orsolini L, Bizri M. Psychological distress experienced by self-quarantined undergraduate university students in Lebanon during the COVID-19 outbreak. Int J Psychiatry Clin Pract. (2021) 25:1–8. doi: 10.1080/13651501.2021.1900872
21. Moayed MS, Vahedian-Azimi A, Mirmomeni G, Rahimi-Bashar F, Goharimoghadam K, Pourhoseingholi MA, et al. Depression, anxiety, and stress among patients with COVID-19: a cross-sectional study. Clinical, Biological and Molecular Aspects of COVID-19. (2021) 1321:229. doi: 10.1007/978-3-030-59261-5_19
22. Tang S, Xiang Z. Who suffered most after deaths due to COVID-19? Prevalence and correlates of prolonged grief disorder in COVID-19 related bereaved adults. Glob Health. (2021) 17:1–9. doi: 10.1186/s12992-021-00669-5
23. Segal J, Smith M, Segal R, Robinson L. Stress symptoms, signs, and causes. HelpGuideorg International (2016). Available online at: https://www.helpguide.org/articles/stress/stress-symptoms-signs-and-causes.htm (accessed June 14, 2021).
24. Halbreich U. Stress-related physical and mental disorders: a new paradigm. BJPsych Adv. (2021) 27:145–52. doi: 10.1192/bja.2021.1
25. American Psychological Association. Stress effects on the body (2018). Available online at: http://www.apa.org/topics/stress/body (accessed June 14, 2021).
26. Choi S, Zhang B, Ma S, Gonzalez-Celeiro M, Stein D, Jin X, et al. Corticosterone inhibits GAS6 to govern hair follicle stem-cell quiescence. Nature. (2021) 592:428–32. doi: 10.1038/s41586-021-03417-2
27. Jusuf NK, Putra IB, Sutrisno AR. Correlation between stress scale and serum substance P level in acne vulgaris. Int J Gen Med. (2021) 14:681. doi: 10.2147/IJGM.S294509
28. Markovic M, Soldatovic I, Bjekic M, Sipetic-Grujicic S. Adolescents' self perceived acne-related beliefs: from myth to science ⋆, ⋆⋆. Anais brasileiros de dermatologia. (2020) 94:684–90. doi: 10.1016/j.abd.2019.02.005
29. Wen L, Jiang G, Zhang X, Lai R, Wen X. Relationship between acne and psychological burden evaluated by ASLEC and HADS surveys in high school and college students from central China. Cell Biochem Biophys. (2015) 71:1083–8. doi: 10.1007/s12013-014-0312-y
30. Kim YK, Moon SY, Yim KM, Seong SJ, Hwang JY, Park SP. Psychological distress in patients with symptomatic vitreous floaters. J Ophthalmol. (2017) 2017:3191576. doi: 10.1155/2017/3191576
31. Yilmaz U, Gokler ME, Unsal A. Dry eye disease and depression-anxiety-stress: A hospital-based case control study in Turkey. Pak J Med Sci. (2015) 31:626. doi: 10.12669/pjms.313.7091
32. Marks H. Stress Symptoms. WebMD (2021). Available online at: https://www.webmd.com/balance/stress-management/stress-symptoms-effects_of-stress-on-the-body (accessed June 14, 2021).
33. How, do you cope? (n,.d.). Available online at: https://www.semel.ucla.edu/dual-diagnosis-program/News_and_Resources/How_Do_You_Cope (accessed June 14, 2021).
34. Good Therapy. Getting help for stress (2018). Available online at: https://www.goodtherapy.org/learn-about-therapy/issues/stress/get-help (accessed June 14, 2021).
35. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
36. The link between stress and alcohol. (n.d.). Available online at: pubs.niaaa.nih.gov/publications/AA85/AA85.htm
37. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
38. Seedhom AE, Kamel EG, Mohammed ES, Raouf NR. Predictors of Perceived Stress among Medical and Nonmedical College Students, Minia, Egypt. Int J Prev Med. (2019) 10:107. doi: 10.4103/ijpvm.IJPVM_6_18
39. Ali AM, Hendawy AO, Ahmad O, Al Sabbah H, Smail L, Kunugi H. The Arabic version of the Cohen perceived stress scale: factorial validity and measurement invariance. Brain Sci. (2021) 11:419. doi: 10.3390/brainsci11040419
40. ADAA. Tips to manage anxiety and stress (2021). Available online at: adaa.org/tips-manage-anxiety-and-stress (accessed June 3, 2021).
41. National Center for Injury Prevention and Control Division Division of Violence Prevention (2021). Available online at: https://www.cdc.gov/violenceprevention/about/copingwith-stresstips.html (accessed June 14, 2021).
42. Kop WJ, Kupper HM. Fatigue and stress. In Stress: Concepts, cognition, emotion, and behavior. Academic Press (2016). p. 345–50.
43. Mcbeth J, Tomenson B, Chew-Graham CA, Macfarlane GJ, Jackson J, Littlewood A, et al. Common and unique associated factors for medically unexplained chronic widespread pain and chronic fatigue. J Psychosom Res. (2015) 79:484–91. doi: 10.1016/j.jpsychores.2015.10.004
44. Smartt C, Medhin G, Alem A, Patel V, Dewey M, Prince M, et al. Fatigue as a manifestation of psychosocial distress in a low-income country: a population-based panel study. Trop Med Int Health. (2016) 21:365–72. doi: 10.1111/tmi.12658
45. Wurtman RJ, Wurtman JJ. Brain serotonin, carbohydrate-craving, obesity and depression. Obes Res. (1995) 3(Suppl 4):477S−80S. doi: 10.1002/j.1550-8528.1995.tb00215.x
46. Laura Morris O Dizziness Related to Anxiety and Stress. Academy Of Neurologic Physical Therapy (2015). Available online at: https://www.neuropt.org/docs/default-source/vsig-english-pt-fact-sheets/anxiety-and-stress-dizziness4ca035a5390366a68a96ff00001fc240.pdf?sfvrsn=80a35343_0andsfvrsn=80a35343_0 (accessed June 14, 2021).
47. Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience. (2009) 164:1579–87. doi: 10.1016/j.neuroscience.2009.09.034
48. Saman Y, Bamiou DE, Gleeson M, Dutia MB. Interactions between stress and vestibular compensation-a review. Front Neurol. (2012) 3:116. doi: 10.3389/fneur.2012.00116
49. Yazdi M, Zeverdegani SK, MollaAghaBabaee AH. Association of derived patterns of musculoskeletal disorders with psychological problems: a latent class analysis. Environ Health Prev Med. (2019) 24:1–9. doi: 10.1186/s12199-019-0784-x
50. Vargas-Prada Figueroa S, Coggon D. Psychological and psychosocial determinants of musculoskeletal pain and associated disability. Best Pract Res Clin Rheumatol. (2015) 29:374–90. doi: 10.1016/j.berh.2015.03.003
51. Babaei AHMA, Yazdi M, Zeverdegani SK, Barakat S. Prevalence of musculoskeletal disorders and its relationship with occupational stress among workers at a steel industry. Iran Occup Health. (2016) 13:59–69. Available online at: https://www.sid.ir/en/journal/ViewPaper.aspx?id=645586
52. Taban E, Shokri S, YazdaniAval M, RostamiAghdamShendi M, Kalteh HO, Keshizadeh F. Impact of job stress on the prevalence of musculoskeletal disorders among computer users of hospitals in Gorgan, Iran, in 2014. J Public Health Epidemiol. (2015) 4:139–45. doi: 10.18869/acadpub.johe.4.3.139
53. NINDS. “Tremor Fact Sheet” (2021). Available online at: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Tremor-Fact-Sheet (accessed June 14, 2021).
54. Watson K. Anxiety Shaking: What Causes It? (2018). Available online at: https://www.healthline.com/health/anxiety-shaking (accessed June 14, 2021).
55. NINDS. “Headache: Hope Through Research” (2016). Available online at: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Headache-Hope-Through-Research (accessed June 14, 2021).
56. Chowdhury D. Tension type headache. Ann Indian Acad Neurol. (2012) 15(Suppl 1):S83. doi: 10.4103/0972-2327.100023
57. Cathcart S, Winefield AH, Lushington K, Rolan P. Stress and tension-type headache mechanisms. Cephalalgia. (2010) 30:1250–67. doi: 10.1177/0333102410362927
58. Al-Hayani M, AboTaleb H, Bazi A, Alghamdi B. Depression, anxiety and stress in Saudi migraine patients using DASS-21: local population-based cross-sectional survey. Int J Neurosci. (2021) 1−9. doi: 10.1080/00207454.2021.1909011
59. Radat F. Stress et migraine [Stress and migraine]. Rev Neurol. (2013) 169:406–12. doi: 10.1016/j.neurol.2012.11.008
60. Liu TH, Wang Z, Xie F, Liu YQ, Lin Q. Contributions of aversive environmental stress to migraine chronification: research update of migraine pathophysiology. World J Clin Cases. (2021) 9:2136. doi: 10.12998/wjcc.v9.i9.2136
61. Rafique N, Al-Sheikh MH. Prevalence of menstrual problems and their association with psychological stress in young female students studying health sciences. Saudi Med J. (2018) 39:67. doi: 10.15537/smj.2018.1.21438
62. Gilbrech KI,. The Impact of Stress on the Menstrual Cycle. The Eleanor Mann School of Nursing Undergraduate Honors Theses. (2020). Available online at: https://scholarworks.uark.edu/nursuht/102
63. Jha N, Bhadoria AS, Bahurupi Y, Gawande K, Jain B, Chaturvedi J, et al. Psychosocial and stress-related risk factors for abnormal menstrual cycle pattern among adolescent girls: a case-control study. J Educ Health Promot. (2020) 9:313. doi: 10.4103/jehp.jehp_419_20
64. Singh R, Sharma R, Rajani H. Impact of stress on menstrual cycle: a comparison between medical and non medical students. Saudi J Med Med Sci. (2015) 4:115. doi: 10.4103/2278-0521.157886
65. Ansong E, Arhin SK, Cai Y, Xu X, Wu X. Menstrual characteristics, disorders and associated risk factors among female international students in Zhejiang Province, China: a cross-sectional survey. BMC Women's Health. (2019) 19:1–10. doi: 10.1186/s12905-019-0730-5
66. Leander M, Lampa E, Rask-Andersen A, Franklin K, Gislason T, Oudin A, et al. Impact of anxiety and depression on respiratory symptoms. Respir Med. (2014) 108:1594–600. doi: 10.1016/j.rmed.2014.09.007
67. Elmer J. How Anxiety Can Cause Shortness of Breath and What You Can Do. Healthline (2018). Available online at: https://www.healthline.com/health/shortness-of-breath-anxiety (accessed June 14, 2021).
68. Sahasrabudhe TR. Psychogenic dyspnea. Medical Journal of Dr. DY Patil University. (2013) 6:14. doi: 10.4103/0975-2870.108627
69. Weiner D, Weiner P, Beckerman M. [Anxiety dyspnea]. Harefuah. (2014) 153:147–50. Available online at: https://pubmed.ncbi.nlm.nih.gov/24791552/
70. Stoeckel MC, Esser RW, Gamer M, Buchel C, Leupoldt A. Dyspnea catastrophizing and neural activations during the anticipation and perception of dyspnea. Psychophysiology. (2018) 55. doi: 10.1111/psyp.13004
71. Musey Jr PI, Schultebraucks K, Chang BP. Stressing out about the heart: a narrative review of the role of psychological stress in acute cardiovascular events. Acad Emerg Med. (2020) 27:71–79. doi: 10.1111/acem.13882
72. Musey Jr PI, Patel R, Fry C, Jimenez G, Koene R, Kline JA. Anxiety associated with increased risk for emergency department recidivism in patients with low-risk chest pain. Am J Cardiol. (2018) 122:1133–41. doi: 10.1016/j.amjcard.2018.06.044
73. Redina OE, Markel AL. Stress, genes, and hypertension. Contribution of the ISIAH rat strain study. Curr Hypertens Rep. (2018) 20:1–10. doi: 10.1007/s11906-018-0870-2
74. Damtie D, Bereket A, Bitew D, Kerisew B. The prevalence of hypertension and associated risk factors among secondary school teachers in Bahir Dar City administration, Northwest Ethiopia. Int J Hypertens. (2021) 2021:11. doi: 10.1155/2021/5525802
75. Krantz DS, Helmers KF, Bairey CN, Nebel LE, Hedges SM, Rozanski A. (1991). Cardiovascular reactivity and mental stress-induced myocardial ischemia in patients with coronary artery disease. Psychosom Med. (1991) 53:1–12. doi: 10.1097/00006842-199101000-00001
76. Nass BY, Dibbets P, Markus CR. Impact of the COVID-19 pandemic on inflammatory bowel disease: the role of emotional stress and social isolation. Stress Health.? (2021) 38:222–33. doi: 10.1002/smi.3080
77. Han CJ, Jarrett ME, Heitkemper MM. Relationships between abdominal pain and fatigue with psychological distress as a mediator in women with irritable bowel syndrome. Gastroenterol Nurs. (2020) 43:28. doi: 10.1097/SGA.0000000000000383
78. Popa SL, Dumitrascu DL. Anxiety and IBS revisited: ten years later. Clujul Med. (2015) 88:253. doi: 10.15386/cjmed-495
79. Kasemy ZA, Sakr AA, EL Shebiny EM, Elbasyouny HA, El Dalatony M. Psychological status and irritable bowel syndrome among healthcare workers. Egypt J Occup Med. (2020) 44:605–20. doi: 10.21608/ejom.2020.109590
80. Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. (2011) 15:18–22. doi: 10.4103/2230-8210.77573
81. Carmen S. Stress and cognition. Wiley Interdiscip Rev Cogn Sci. (2013) 4:245–61. doi: 10.1002/wcs.1222
82. Cibrian-Llanderal T, Melgarejo-Gutierrez M, Hernandez-Baltazar D. Stress and cognition: psychological basis and support resources. Health and Academic Achievement. (2018) 11. doi: 10.5772/intechopen.72566
83. Leng Y, Wainwright NWJ, Hayat S, Stephan BCM, Matthews FE, Luben R, et al. The association between social stress and global cognitive function in a population-based study: the European Prospective Investigation into Cancer (EPIC)-Norfolk study. Psychological Med. (2013) 43:655–66. doi: 10.1017/S0033291712001316
84. Lin YF, Wang LY, Chen CS, Li CC, Hsiao YH. Cellular senescence as a driver of cognitive decline triggered by chronic unpredictable stress. Neurobiol Stress. (2021) 15:100341. doi: 10.1016/j.ynstr.2021.100341
85. Debiec J, LeDoux JE. Noradrenergic signaling in the amygdala contributes to the reconsolidation of fear memory: treatment implications for PTSD. Ann NY Acad Sci. (2006) 1071:521–4. doi: 10.1196/annals.1364.056
86. Yang L, Zhao Y, Wang Y, Liu L, Zhang X, Li B, et al. The effects of psychological stress on depression. Curr Neuropharmacol. (2015) 13:494–504. doi: 10.2174/1570159X1304150831150507
87. Pimple P, Shah A, Rooks C, Bremner JD, Nye J, Ibeanu I, et al. Association between anger and mental stress–induced myocardial ischemia. Am Heart J. (2015) 169:115–21. doi: 10.1016/j.ahj.2014.07.031
88. Yanguas J, Pinazo-Henandis S, Tarazona-Santabalbina FJ. The complexity of loneliness. Acta Bio Med. (2018) 89:302. doi: 10.23750/abm.v89i2.7404
89. Fan LB, Blumenthal JA, Watkins LL, Sherwood A. Work and home stress: associations with anxiety and depression symptoms. Occup Med. (2015) 65:110–16. doi: 10.1093/occmed/kqu181
90. Emotional symptoms of stress: What are they and how are they treated? Available online at: medicalnewstoday.com (accessed April 26, 2022).
91. Grafe LA, Bhatnagar S. Orexins and stress. Front Neuroendocrinol. (2018) 51:132–45. doi: 10.1016/j.yfrne.2018.06.003
92. Chao AM, Jastreboff AM, White MA, Grilo CM, Sinha R. Stress, cortisol, and other appetite-related hormones: prospective prediction of 6-month changes in food cravings and weight. Obesity. (2017) 25:713–20. doi: 10.1002/oby.21790
93. Siddiqui JA, Qureshi SF, Marei WM, Mahfouz TA. Onychophagia (nail biting): a body focused repetitive behavior due to psychiatric co-morbidity. Psychiatry Behav Sci. (2017) 7:47. doi: 10.5455/jmood.20170204031431
94. Choi D, Ota S, Watanuki S. Does cigarette smoking relieve stress? Evidence from the event-related potential (ERP). Int J Psychophysiol. (2015) 98:470–6. doi: 10.1016/j.ijpsycho.2015.10.005
95. Ely DR, Dapper V, Marasca J, Correa JB, Gamaro GD, Xavier MH. Effect of restraint stress on feeding behavior of rats. Physiol Behav. (1997) 61:395–8. doi: 10.1016/S0031-9384(96)00450-7
96. Varma M, Chai JK, Meguid MM, Gleason JR, Yang ZJ. Effect of operative stress on food intake and feeding pattern in female rats. Nutrition. (1999) 15:365–72. doi: 10.1016/S0899-9007(99)00033-7
97. Harvard Health Publishing. Why stress causes people to overeat (2021). Available online at: https://www.health.harvard.edu/staying-healthy/why-stress-causes-people-to-overeat (accessed April 17, 2022).
98. Han KS, Kim L, Shim I. Stress and sleep disorder. Exp Neurobiol. (2012) 21:141–50. doi: 10.5607/en.2012.21.4.141
99. Husky MM, Kovess-Masfety V, Swendsen JD. Stress and anxiety among university students in France during Covid-19 mandatory confinement. Compr Psychiatry. (2020) 102:152191. doi: 10.1016/j.comppsych.2020.152191
100. WHO COVID-19 Dashboard. Available online at: https://covid19.who.int/region/emro/country/eg (accessed April 17, 2022).
101. Omar DI, Hani BM. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J Infect Public Health. (2021) 14:1481–8. doi: 10.1016/j.jiph.2021.06.019
102. Ehab Tahaand Samih Talaat (2020). Available online at: https://www.tamimi.com/law-update-articles/impact-of-covid-19-on-education-in-egypt-a-new-world-order-in-the-education-realm/ (accessed April 20, 2021).
103. Amer AA, Amer SA, Alrufaidi KM, Abd-Elatif EE, Alafandi BZ, Yousif DA, et al. Menstrual changes after COVID-19 vaccination and/or SARS-CoV-2 infection and their demographic, mood, and lifestyle determinants in Arab women of childbearing age, 2021. Front Reprod Health. (2022) 4:927211. doi: 10.3389/frph.2022.927211
104. Carod-Artal FJ. Post-COVID-19 syndrome: epidemiology, diagnostic criteria and pathogenic mechanisms involved. Rev Neurol. (2021) 72:384–96. doi: 10.33588/rn.7211.2021230
105. Halboub E, Alhajj MN, AlKhairat AM, Sahaqi AAM, Quadri MFA. Perceived stress among undergraduate dental students in relation to gender, clinical training and academic performance. Acta Stomatologica Croatica. (2018) 52:37–45. doi: 10.15644/asc52/1/6
106. Nahar VK, Davis RE, Dunn C, Layman B, Johnson EC, Dascanio JJ, et al. The prevalence and demographic correlates of stress, anxiety, and depression among veterinary students in the Southeastern United States. Res Vet Sci. (2019) 125:370–3. doi: 10.1016/j.rvsc.2019.07.007
107. Verma R, Balhara YP, Gupta CS. Gender differences in stress response: Role of developmental and biological determinants. Ind Psychiatry J. (2011) 20:4–10. doi: 10.4103/0972-6748.98407
108. Gao W, Ping S, Liu X. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J Affect Disord. (2020) 263:292–300. doi: 10.1016/j.jad.2019.11.121
109. Yu B, Chen X, Li S, Liu Y, Jacques-Tiura AJ, Yan H. Acculturative stress and influential factors among international students in China: a structural dynamic perspective. PloS ONE. (2014) 9:e96322. doi: 10.1371/journal.pone.0096322
110. Karaman MA, Watson JC. Examining associations among achievement motivation, locus of control, academic stress, life satisfaction: a comparison of U.S. and international undergraduate students. Personality and Individual Differences. (2017) 111:106–10. doi: 10.1016/j.paid.2017.02.006
111. Solano P, Ustulin M, Pizzorno E, Vichi M, Pompili M, Serafini G, et al. A Google-based approach for monitoring suicide risk. Psychiatry Res. (2016) 246:581–6. doi: 10.1016/j.psychres.2016.10.030
112. Baldessarini RJ, Innamorati M, Erbuto D, Serafini G, Fiorillo A, Amore M, et al. Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. J Affect Disord. (2017) 210:19–21. doi: 10.1016/j.jad.2016.12.003
113. Doing What Matters in Times of Stress. World Health Organization. Available online at: https://www.who.int/publications/i/item/9789240003927?gclid=CjwKCAjwsJ6TBhAIEiwAfl4TWGWTMGEzv7q8J6oh5DB-GoPI0qe3op-MgOj8gmGq1yAkP2FwLGF1QhoCC7cQAvD_B (acessed April 26, 2022).
114. Dada JO, Babatunde SO, Adeleye RO. Assessment of academic stress and coping strategies among built environment undergraduate students in Nigerian higher education. J Appl Res High Educ. (2019) 11:367–378. doi: 10.1108/JARHE-06-2018-0100
115. Mental Health Foundation. Smoking and mental health (2021). Available online at: https://www.mentalhealth.org.uk/explore-mental-health/a-z-topics/smoking-and-mental-health (accessed April 20, 2021).
116. Esia-Donkoh K, Yelkpieri D, Esia-Donkoh K. Coping with Stress: Strategies Adopted by Students at the Winneba Campus of University of Education, Winneba, Ghana. US-China Education Review. (2011) 2:290–9.
117. Yousif MA, Arbab AH, Yousef BA. Perceived academic stress, causes, and coping strategies among undergraduate pharmacy students during the COVID-19 pandemic. Adv Med Educ Pract. (2022) 13:189–97. doi: 10.2147/AMEP.S350562
118. Lo C-F. Stress and coping strategies among University Freshmen in Hong Kong: validation of the coping strategy indicator. Psychology. (2017) 8:1254–66. doi: 10.4236/psych.2017.88081
119. Babicka-Wirkus A, Wirkus L, Stasiak K, Kozłowski P. University students' strategies of coping with stress during the coronavirus pandemic: data from Poland. PLoS ONE. 16:e0255041. doi: 10.1371/journal.pone.0255041
120. Santangelo OE, Provenzano S, Giordano D, Alagna E, Armetta F, Gliubizzi C, et al. Nursing students and depressive symptomatology: an observational study in University of Palermo. Mental Illness.? (2019). doi: 10.1108/MIJ-10-2019-0006
121. Sredniawa A, Drwiła D, Krotos A, Wojtaś D, Kostecka N, Tomasik T. Insomnia and the level of stress among students in Krakow, Poland. Trends Psychiatry Psychother. (2019) 41:60–8. doi: 10.1590/2237-6089-2017-0154
122. Most Stressful Life Events—Handling the 5 Top Stressors in Life. University Hospitals (uhhospitals.org).
Keywords: stress, stress-related symptoms, coping strategies, university students, the COVID-19 pandemic, Egypt
Citation: Attia M, Ibrahim FA, Elsady M-E, Khorkhash MK, Rizk MA, Shah J and Amer SA (2022) Cognitive, emotional, physical, and behavioral stress-related symptoms and coping strategies among university students during the third wave of COVID-19 pandemic. Front. Psychiatry 13:933981. doi: 10.3389/fpsyt.2022.933981
Received: 06 May 2022; Accepted: 18 August 2022;
Published: 16 September 2022.
Edited by:
Hironobu Fujiwara, Kyoto University Hospital, JapanReviewed by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyCopyright © 2022 Attia, Ibrahim, Elsady, Khorkhash, Rizk, Shah and Amer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jaffer Shah, amFmZmVyLnNoYWhAa2F0ZWIuZWR1LmFm
†ORCID: Merna Attia orcid.org/0000-0002-6457-4252
Fatma A. Ibrahim orcid.org/0000-0001-7020-5843
Mohamed Abd-Elfatah Elsady orcid.org/0000-0003-1141-1510
Mohamed Khaled Khorkhash orcid.org/0000-0003-0038-5409
Marwa Abdelazim Rizk orcid.org/0000-0003-4294-9655
Samar A. Amer orcid.org/0000-0002-9475-6372
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.