
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 28 September 2022
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.925462
Introduction: Research on borderline personality disorder (BPD) has shown that less intensive care is especially effective when patients have been told about their condition. However, problems with diagnosing the disorder are also described in the literature. This study thus aims to explore the factors associated with the challenges of identifying and then communicating a BPD diagnosis to patients.
Methods: We analyzed a database of 202 patients of Toulouse University Hospital (France) who had a CIM−10 F60.3 diagnosis. This data was used to identify the sociodemographic and clinical benchmarks associated with patients who had received an established BPD diagnosis prior to their attendance at the hospital's emergency department (ED) in the study period.
Results: Sixty-three percentage of the patients admitted to our psychiatric ED had been given an earlier diagnosis of BPD. Those who had not been diagnosed were more likely to: not have undergone any psychiatric follow-up; not have been hospitalized in the psychiatry department; and not have previously attended at the ED. Patients with BPD and a comorbidity of MDD were also less likely to have received a BPD diagnosis before their ED admission.
Conclusion: This study found that patients without an established BPD diagnosis who present at the ED are more likely to not be known to the psychiatric care system. This suggests that EDs have a specific role to play in making a diagnosis and the subsequent orientation of care.
Borderline personality disorder (BPD) is described in DSM-5 as being characterized by the impairment and pervasive dysregulation of affects, self-image, interpersonal relationships, and behavior (1). It has been found to be present in approximately 2% to 6% of the adult population (2–4) and in 3% of adolescents aged 12–14 years (5).
The prognosis for the disorder has recently changed from untreatable to treatable thanks to psychotherapy, which is now considered to be the primary treatment (6). Many comprehensive types of psychotherapy have been found to be effective at treating those with BPD (7–10). In addition, recent research has shown that less intensive, easier-to-undertake therapies may be almost as effective, with an example being the good psychiatric management (GPM) approach developed by Gunderson (11). This treatment is now recommended as the primary intervention, but its use makes it essential to obtain information about the diagnosis and for therapists to have undertaken relevant psychological training.
Patients with BPD are frequent attenders at psychiatric EDs, presenting with complaints related to their disorder almost five times as often as the general population (12), amounting to approximately 10 % of all attendances (12–14). The psychiatric ED has become a crucial part of the mental healthcare system, acting as a bridge between inpatient and outpatient services and as a third treatment setting, particularly for regular attendees. Data on patients suffering from BPD suggest that the use of crisis services can be linked to a risk of suicide, but psychotherapy, including dialectical behavioral therapy, can lower this risk (13). Hospitalization is also a risk factor, with a higher number of prior admissions associated with an increased likelihood of completed suicide (14).
In view of the above, it is important to integrate ED admissions into stepped-care interventions as a way to ensure there is a pathway to specialist outpatient care (15–17). Nonetheless, we have previously described a gap in the treatment of BPD patients who present at the ED between official recommendations and their incorporation in clinical practice (18). This is partly explained by the organization of care, in particular the failure of community resources like crisis lines or other therapy, which has also been identified as an issue by patients (19).
This is unfortunate, because ED admissions are an opportunity to reinforce GPM principles and bolster outpatient treatment, potentially leading to a reduction in the number of future ED attendances, suicidal behavior, and hospitalizations (20). The first step of GPM is clearly the establishment of a BPD diagnosis, if appropriate, but a failure to do so is commonly described in the literature. An example is a survey carried out among a psychiatric population which found that 57% of psychiatrists had failed to identify BPD and 37% did not document it in their patients' records (21). It is acknowledged that the diagnosis can be difficult to make, as patients with the disorder frequently consult physicians about other issues (somatic complaints, depressive symptoms, substance use) (11), potentially leading to alternative diagnoses being made (22).
Nevertheless, establishing and communicating a BPD diagnosis is critical, enabling: therapeutic follow-ups to be put in place; expectations to be managed; symptoms to be distinguished from voluntary behaviors; the anticipation of emergencies and crises; and the avoidance of negative reactions.
In order to clarify the role of the ED in the course of care provided to patients suffering from BPD, including the importance of making the diagnosis, this study compared the characteristics of patients who had and had not been diagnosed with the disorder at the time of their attendance at our ED. We expected to find that the BPD patients who had not been diagnosed would be those who had also not benefited from any psychiatric follow-up and/or had not previously been admitted to the ED.
We conducted a retrospective study involving patients who attended at the psychiatric ED of Toulouse University Hospital (France) during the period 1.1.20–7.31.21. The department provides care for those who only require outpatient treatment, albeit following a brief period (typically 24–48 h) of inpatient care to stabilize their emotional distress, enable clinicians to meet relatives, and coordinate subsequent follow-ups. The duration of this short-term hospitalization is also adaptable to the clinical condition, with some patients being admitted to the department for up to 5 days. Patients admitted to the short-term psychiatry ward benefit from specific psychiatric evaluations and examinations (including clinical observations and interviews with relatives), enabling any diagnoses to be refined.
We adopted a retrospective chart review method to conduct this study of the patients admitted to the short-term psychiatry ward described above (23). The data used were extracted from the psychiatric assessments recorded in the patients' medical files. These files are organized using a standard framework, which makes data extraction possible. In this study, we consulted the medical files contained in the database of patients whose BPD diagnosis had been assigned a CIM−10 F60.3 code as part of a primary or secondary diagnosis (Orbis® software).
We extracted the following data from the medical files:
1. The Medical History That led to a Recorded BPD Diagnosis Made Before the Latest ED Admission. This Was Achieved Using Data Collected From a Patient's General Practitioner (GP), Psychiatrist (if the Patient Was Being Followed up), and Reports of Previous Hospitalizations or ED Admissions.
2. Sociodemographic Data: age, Gender, Level of Education, and Professional and Personal Status. Clinical Data: Reason for ED Attendance, Current Follow-up With a GP, Current Psychiatric Follow-up, History of Attempted Suicide, and Number of ED Admissions in the Previous 12 Months. As the Study's Inclusion Period Coincided With the COVID-19 Pandemic, Data Relating to Its Impact Were Also Collected, Including any Consequential Crises Recorded in the Medical Files (e.g., Arising From Social Restrictions, Financial Concerns, Worries About Health).
The extracted data were then analyzed by a psychiatrist who was able to consult the practitioner who made the diagnosis if there was any confusion about the information contained in the medical files.
The diagnoses recorded in the database were based on the DSM-5 criteria (1) and had been made by the ED's experienced psychiatrists (mean of 3 years working in the ED) during a patient's short-term hospitalization. This particular cohort of patients was used because they all underwent the same evaluations, which were conducted by the department's psychiatrists. To avoid the possibility of any overestimation of symptoms, we also met the patients' relatives and investigated their biographies (from pregnancy to date) during the short-term hospitalization to clarify the trajectory of symptoms. A BPD diagnosis was treated as not confirmed if the symptoms began during the latest crisis period. A large proportion (54%) of the patients in the cohort had been referred to an outpatient crisis service after their hospitalization. This aimed to both help them to resolve the factors behind their latest crisis and confirm their BPD diagnosis (the SCID II was used for this purpose). The follow-up support provided by the service was in place for about 2 months. The service uses the same medical files as the ED, enabling us to track the evolution of symptoms and identify the diagnosis made during this follow-up period. This revealed that 93% of the patients diagnosed with BPD in the ED had their BPD diagnosis confirmed by the crisis service. The 7% of patients whose BPD diagnosis was not confirmed were removed from our sample.
Our goal was to compare the social and clinical characteristics of patients with an established diagnosis of BPD to those of patients who had not previously been diagnosed with the condition. Patients were assigned to these two groups based on their medical history (see above) relating to the BPD diagnosis.
Our use of the data was approved by the Commission Nationale de l'Information et des Libertés (CNIL) in accordance with the French legislation: MR-004.
The continuous and categorical variables are described in terms of the mean (+/- standard deviation) and/or the median (+/- interquartile range), based on their distributions, numbers, and percentages, respectively. Associations between the patients' categorical characteristics and having a previously established BPD diagnosis were tested using the chi-squared or Fischer exact tests (when the expected values were <5.0). A multivariable logistic regression model was employed to assess any link between the sociodemographic and clinical characteristics and having an earlier-established BPD diagnosis or the absence thereof. The results are presented in terms of odds ratios (ORs). The variables found to be significantly associated in the p < 0.05 bivariate analyses were included in the initial regression model. The analysis was controlled for gender, age, and level of education. We then performed a backwards, step-by-step manual selection to produce our final model, controlling for confounding variables at each stage. The statistical analyses were performed using the RStudio software, version 1.3.1093©, 2009-2020.
Two hundred and two patients were included in the sample (Figure 1). Of these, 55% were referred to the ED by the French 911 service (SAMU), 31% attended spontaneously, 10% were referred by health professionals, and 4% by other means. The reasons for their attendance at the ED were: suicidal ideation (43%), a suicide attempt (37%), alcohol or other narcotic intoxication (5.5%), non-psychiatric issues (various somatic complaints; 8%), anxiety (5%), and depressive symptoms (1.5%). The treatments the patients received were: no psychotropic treatment (23%), one form of psychotropic treatment (22%), two or more psychotropic treatments (56%), SSRI anti-depressants (25%), benzodiazepines (25%), mood stabilizers (10%), antipsychotics (second generation; 21%), antipsychotics (first generation; 13%), and antidepressants other than SSRIs (2%). In terms of age, 60% of the patients were aged between 15 and 25, 23% between 26 and 35, 6% between 36 and 45, 8% between 46 and 55, and 2% older than 56. Of the patients aged between 15 and 25, 22 of them (10%) were younger than 18, with 50% being 17 years old and 50% 16. Additionally, 45% of the patients were employed, 31% were students, and 24% were unemployed; 65% were single, 30% had a partner, and 5% were divorced. A crisis relating to the COVID-19 pandemic was noted in the medical files of 13 patients. Finally, women made up 80% of the sample; 50% of the cohort had received an earlier diagnosis of BPD, 60% had already been hospitalized in the psychiatry department, 41% had previously attended at the ED, and 50% had an addiction comorbidity.
One hundred and twenty-eight patients (63%) had received a previous BPD diagnosis. In this group, the patients were more likely to: be employed (55 vs. 35% in the unknown diagnosis group; p = 0.01); currently have a psychiatric follow-up in place (77 vs. 55%; p < 0.001); have already been hospitalized on a psychiatric ward (85 vs. 44%; p < 0.001); have a history of attempting suicide (80 vs. 52%; p < 0.001); and have had a higher number of ED admissions in the previous 12 months (0.97 admissions on average vs. an average of 2.7; p < 0.001). Conversely, the patients who had not received an earlier BPD diagnosis were more likely to have been diagnosed with a major depressive disorder (MDD) (41% in the unknown diagnosis group vs. 26% in the group of patients with a BPD diagnosis; p < 0.001). The details of the comparisons are presented in Table 1.
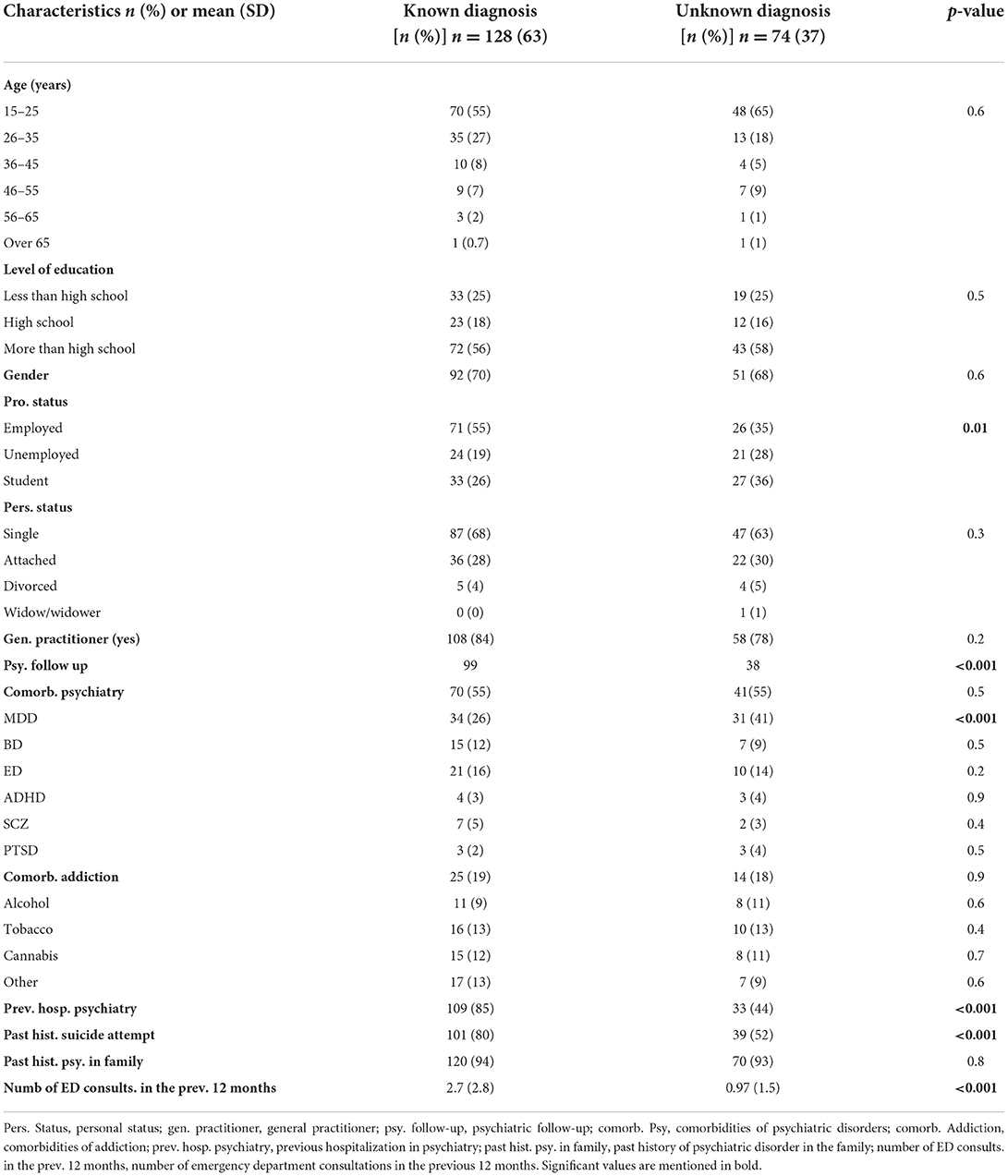
Table 1. Comparison between sociodemographic and clinical characteristics based on knowledge of a BPD diagnosis.
Four factors were identified as being associated with an earlier BPD diagnosis: a history of hospitalization on a psychiatric ward [OR = 4.1; 95% CI = (1.8–9.3)]; an MDD comorbidity [OR = 0.4; 95% CI = (0.1–0.9)]; the number of admissions to the ED in the previous 12 months [OR = 1.25; 95% CI = (1.07–1.5)]; and a previous suicide attempt [OR = 2.2; 95% CI = (1.01–4.6)]. There were no significant links between having an earlier BPD diagnosis and having a current psychiatric follow-up in place, a history of attempting suicide, or a patient's professional status.
The results of this regression analysis are presented in Figure 2.
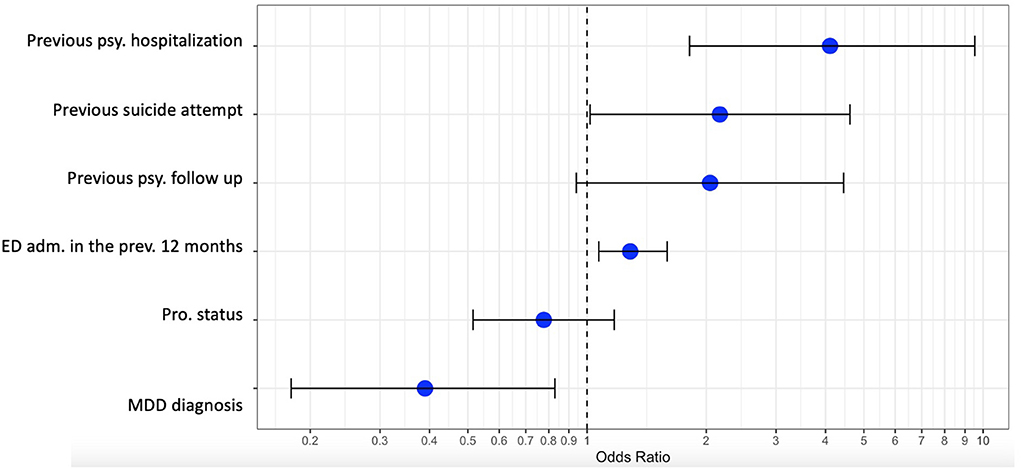
Figure 2. Multimodal regression analysis. Previous psy. hospitalization, previous psychiatric hospitalization; previous psy follow up, previous psychiatric follow up; ED adm. in the previous 12 months, ED admission in the previous 12 months; pro. status, professional status; MDD diagnosis, major depressive disorder diagnosis.
Knowledge of their BPD diagnosis is a crucial part of the care patients receive. Our study thus had the goal of identifying the factors associated with having received such a diagnosis before the latest ED attendance.
Our cohort's patients were mainly admitted to the ED due to a suicidal crisis, as is also reflected in the literature concerning the reasons for ED referrals among patients with BPD (24, 25). In terms of their psychiatric diagnosis, 55% of our patients had been diagnosed with a condition other than BPD, with the most common being mood disorders. These included MDD in 33% of the patients, which is relatable to the existing literature (26, 27), and bipolar disorder in 10%, which is lower than the 20% figure in previous reports (27, 28). About 20% of the patients had an addiction, as is also commonly described in the literature (27, 29).
As expected, the patients diagnosed with BPD were significantly more often followed-up by a psychiatrist and were more often hospitalized in the psychiatry department. This suggests that those who had not received a BPD diagnosis were more likely to enter the care system via the ED. However, 51% of the patients with a psychiatric follow-up in place and 44% of those who had previously been hospitalized in the psychiatry department had not been diagnosed with BPD. This is surprising, given that questionnaires to assist clinicians in identifying the disorder are available and could be used in outpatient care (30–32).
Interestingly, the patients diagnosed with MDD were less likely to have received a BPD diagnosis, irrespective of whether they had any psychiatric follow-ups in place, although this finding was still significant in the group that was being followed up. This suggests that an MDD diagnosis may mask a determination that a patient has BPD. Indeed, previous studies have also highlighted that diagnosing BPD can be a difficult task for clinicians and the disorder is liable to be confused with other conditions (33). There were no differences in terms of the presence of other psychiatric comorbidities or addictive behaviors between the patients with or without an earlier BPD diagnosis, suggesting that having one of these conditions is not a complicating factor.
Our analysis also identified that the patients who had already been diagnosed with BPD were six times more likely to have previously been hospitalized on the psychiatric ward. This is striking, as treatment guidelines recommend that these patients should, as far as possible, not be admitted. It may be the case that a period of hospitalization improves the diagnostic process because of the opportunity it provides to make additional clinical observations. There was no evidence in our study that the absence of a BPD diagnosis was linked to the complexity of the psychiatric presentation, including when there were comorbid diagnoses of other psychiatric disorders or addiction; the exception to this was an MDD diagnosis. It may be the case that clinicians are more confident about communicating the diagnosis during inpatient care. Indeed, it has previously been reported that psychiatrists are more uncomfortable about delivering a BPD diagnosis than any other psychiatric condition (21). This is despite the fact that both patients and their relatives describe a sense of relief when the diagnosis is made and communicated to them (34).
We also found that the number of ED attendances was associated with an earlier BPD diagnosis. This is relevant to the hypothesis that a previous ED admission has enabled the diagnosis to be made. On the other hand, our patients without a BPD diagnosis had also attended at the ED an average of once in the previous 12 months, again suggesting that there are diagnosis delays, even though there is strong evidence of the benefits of making an early diagnosis and implementing treatment guidelines (35, 36). Indeed, the identification of BPD symptoms is fundamental to providing prompt and adequate access to intervention programs that can improve the natural life-course trajectory of the disorder (37). This is also relevant for adolescents, with Greenfield et al., for example, identifying baseline predictors for direct patient care in this age group (38). Nevertheless, the literature also attests that factors, including the fear of stigmatization, are a barrier to early diagnosis in clinical practice, especially in adolescents (39, 40). Our study found that 50% of the patients in our cohort under the age of 18 had been diagnosed with BPD before attending at the ED. Among those without an established diagnosis, 27% had been to the ED in the previous 12 months and 90% had a psychiatric follow-up in place.
The interaction between the factors examined in the multiple regression analysis revealed that previous suicide attempts and attendance at the ED were associated with having a BPD diagnosis. This correlates with the hypothesis that presenting at the ED could lead to a diagnosis being established. This data does not, however, identify who made the diagnosis, which could even have been established by the post-ED outpatient care service. Moreover, a previous suicide attempt appears to be an independent factor, suggesting that the diagnosis may be made for patients who attend at the ED for reasons other than a suicide attempt.
Our research has some weaknesses. First, a major limitation is that we did not employ standardized tools for establishing a BPD diagnosis. In particular, previous studies have shown that clinical judgments tend to underestimate the presence of the disorder compared to the use of structured clinical interviews (41). Questionnaires have been publishing earlier (42). Nevertheless, at the time the study was performed, only two questionnaires were available for this purpose in French (43) that demonstrated imitated psychometric qualities (44). Moreover, although the “Borderline Personality Questionnaire” has recently been produced, this was not in time for use in our study (43). Nonetheless, all the psychiatrists who made the BPD diagnoses in our research had been trained to do so and used the DSM-5 criteria. Additionally, we also monitored the evolution of symptoms in the patients referred to the outpatient crisis service to ensure that the diagnosis was confirmed. Unfortunately, however, 46% of patients were not referred to and followed up by the service, meaning that such data was unavailable for them. It should, nevertheless, be noted that the prevalence of BPD (9% of patients) identified reflects the outcomes of previous research (12, 13).
A further possible limitation is the study's use of a retrospective chart review, which can have methodological limitations (45), although an attempt was made to limit these by structuring the research and standardizing the data collection. Moreover, the absence of standardized reviewing process is another limitation, indeed data were not independently collected, with no inter-rater agreement and no validated standardized instrument for chart review. In addition, although we did not monitor practitioners' BPD knowledge, the team of psychiatrists is composed of a small pool of physicians who had all undergone the same training on detecting the disorder. An additional limitation arises from the cross-sectional design, which only enabled us to identify associations and not test the explicative hypotheses. Moreover, the fact that this is a monocentric study may make it difficult to generalize the results, although our cohort presented with similar clinical characteristics to those in BPD populations in general.
Despite the possible issues identified above, the study also has particular strengths, since there is limited research available concerning BPD patients in the ED.
In conclusion, this study suggests that patients without an established BPD diagnosis who are seen in the ED are more likely to be unknown to the psychiatric care system more generally. This indicates that the ED has a specific role to play in diagnosing the disorder and orientating the care required.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was performed in line with the principles of the Declaration of Helsinki and was approved by the Regional Ethics Committee in Uppsala (Ref. no. 2014/252). Written informed consent was obtained from all the individual participants included in the study.
JS and MA wrote the article. EB, MA, and JS designed the study. MA collected the data. JS performed the statistical analysis. All authors contributed to the article and approved the submitted version.
We are grateful to the team working in the Psychiatric Emergency Department at Toulouse University Hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
BPD, Borderline personality disorder; CIM, Classification Internationale des Maladies; ED, Emergency department; MDD, Major depressive disorder; OR, Odds ratio.
1. Association AP. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5. 5th ed. Washington, DC: American Psychiatric Publishing (2013). p. 1.
2. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. (2008) 69:533–45. doi: 10.4088/JCP.v69n0404
3. Lenzenweger MF, Loranger AW, Korfine L, Neff C. Detecting personality disorders in a nonclinical population. Application of a 2-stage procedure for case identification. Arch Gen Psychiatry. (1997) 54:345–51. doi: 10.1001/archpsyc.1997.01830160073010
4. Ellison WD, Rosenstein LK, Morgan TA, Zimmerman M. Community and clinical epidemiology of borderline personality disorder. Psychiatr Clin North Am. (2018) 41:561–73. doi: 10.1016/j.psc.2018.07.008
5. Guilé JM, Zavaglia E, Berthiaume C, Bergeron L. Prevalence and comorbidity of borderline personality traits in the Quebec general population aged 12-14 years. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:2053–62. doi: 10.1007/s00127-021-02067-z
6. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. Am J Psychiatry. (2001) 158(Suppl. 10):1–52.
7. Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. (2017) 74:319–28. doi: 10.1001/jamapsychiatry.2016.4287
8. Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guilford Press (1993). p. 558.
9. Dobson KS. Handbook of Cognitive-Behavioral Therapies. 3rd ed. New York, NY: Guilford Press. (2009). p. 497.
10. BATEMAN A, FONAGY P. Mentalization based treatment for borderline personality disorder. World Psychiatry. (2010) 9:11–5. doi: 10.1002/j.2051-5545.2010.tb00255.x
11. Gunderson JG. Handbook of Good Psychiatric Management for Borderline Personality Disorder. Washington, DC: American Psychiatric Pub. (2014).
12. Brennan JJ, Chan TC, Hsia RY, Wilson MP, Castillo EM. Emergency department utilization among frequent users with psychiatric visits. Acad Emerg Med Off J Soc Acad Emerg Med. (2014) 21:1015–22. doi: 10.1111/acem.12453
13. Coyle TN, Shaver JA, Linehan MM. On the potential for iatrogenic effects of psychiatric crisis services: the example of dialectical behavior therapy for adult women with borderline personality disorder. J Consult Clin Psychol. (2018) 86:116–24. doi: 10.1037/ccp0000275
14. Temes CM, Frankenburg FR, Fitzmaurice GM, Zanarini MC. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. (2019) 80:4039. doi: 10.4088/JCP.18m12436
15. Huxley E, Lewis KL, Coates AD, Borg WM, Miller CE, Townsend ML, et al. Evaluation of a brief intervention within a stepped care whole of service model for personality disorder. BMC Psychiatry. (2019) 19:341. doi: 10.1186/s12888-019-2308-z
16. Laporte L, Paris J, Bergevin T, Fraser R, Cardin JF. Clinical outcomes of a stepped care program for borderline personality disorder. Personal Ment Health. (2018) 12:252–64. doi: 10.1002/pmh.1421
17. Paris J. Stepped care: an alternative to routine extended treatment for patients with borderline personality disorder. Psychiatr Serv Wash DC. (2013) 64:1035–7. doi: 10.1176/appi.ps.201200451
18. Cases C, Lafont Rapnouil S, Gallini A, Arbus C, Salles J. Evidence of practice gaps in emergency psychiatric care for borderline personality disorder: how can this be explained? BMC Psychiatry. (2020) 20:476. doi: 10.1186/s12888-020-02892-7
19. Vandyk A, Bentz A, Bissonette S, Cater C. Why go to the emergency department? Perspectives from persons with borderline personality disorder. Int J Ment Health Nurs. (2019) 28:757–65. doi: 10.1111/inm.12580
20. Hong V. Borderline personality disorder in the emergency department: good psychiatric management. Harv Rev Psychiatry. (2016) 24:357–66. doi: 10.1097/HRP.0000000000000112
21. Sisti D, Segal AG, Siegel AM, Johnson R, Gunderson J. Diagnosing, disclosing, and documenting borderline personality disorder: a survey of psychiatrists' practices. J Personal Disord. (2016) 30:848–56. doi: 10.1521/pedi_2015_29_228
22. Ruggero CJ, Zimmerman M, Chelminski I, Young D. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. (2010) 44:405–8. doi: 10.1016/j.jpsychires.2009.09.011
23. Worster A, Haines T. Advanced statistics: understanding medical record review (MRR) studies. Acad Emerg Med Off J Soc Acad Emerg Med. (2004) 11:187–92. doi: 10.1111/j.1553-2712.2004.tb01433.x
24. Borschmann R, Henderson C, Hogg J, Phillips R, Moran P. Crisis interventions for people with borderline personality disorder. Cochrane Database Syst Rev. (2012) 6:CD009353. doi: 10.1002/14651858.CD009353.pub2
25. Shaikh U, Qamar I, Jafry F, Hassan M, Shagufta S, Odhejo YI, et al. Patients with borderline personality disorder in emergency departments. Front Psychiatry. (2017) 8:136. doi: 10.3389/fpsyt.2017.00136
26. Links PS, Heslegrave RJ, Mitton JE, van Reekum R, Patrick J. Borderline psychopathology and recurrences of clinical disorders. J Nerv Ment Dis. (1995) 183:582–6. doi: 10.1097/00005053-199509000-00004
27. Shah R, Zanarini MC. Comorbidity of borderline personality disorder: current status and future directions. Psychiatr Clin North Am. (2018) 41:583–93. doi: 10.1016/j.psc.2018.07.009
28. Fornaro M, Orsolini L, Marini S, De Berardis D, Perna G, Valchera A, et al. The prevalence and predictors of bipolar and borderline personality disorders comorbidity: Systematic review and meta-analysis. J Affect Disord. (2016) 195:105–18. doi: 10.1016/j.jad.2016.01.040
29. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biol Psychiatry. (2002) 51:936–50. doi: 10.1016/S0006-3223(02)01324-0
30. Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). J Personal Disord. (2003) 17:568–73. doi: 10.1521/pedi.17.6.568.25355
31. Zimmerman M, Balling C. Screening for borderline personality disorder with the mclean screening instrument: a review and critique of the literature. J Personal Disord. (2021) 35:288–98. doi: 10.1521/pedi_2019_33_451
32. Greenfield B, Henry M, Lis E, Slatkoff J, Guilé JM, Dougherty G, et al. Correlates, stability and predictors of borderline personality disorder among previously suicidal youth. Eur Child Adolesc Psychiatry. (2015) 24:397–406. doi: 10.1007/s00787-014-0589-9
33. Zimmerman M, Galione JN, Ruggero CJ, Chelminski I, Young D, Dalrymple K, et al. Screening for bipolar disorder and finding borderline personality disorder. J Clin Psychiatry. (2010) 71:1212–7. doi: 10.4088/JCP.09m05161yel
34. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. (2011) 364:2037–42. doi: 10.1056/NEJMcp1007358
35. National Collaborating Centre for Mental Health (UK). Borderline Personality Disorder: Treatment and Management. Leicester: British Psychological Society (UK) (2009).
36. Zanarini MC, Temes CM, Frankenburg FR, Reich DB, Fitzmaurice GM. Description and prediction of time-to-attainment of excellent recovery for borderline patients followed prospectively for 20 years. Psychiatry Res. (2018) 262:40–5. doi: 10.1016/j.psychres.2018.01.034
37. Bozzatello P, Bellino S, Bosia M, Rocca P. Early detection and outcome in borderline personality disorder. Front Psychiatry. (2019) 10:710. doi: 10.3389/fpsyt.2019.00710
38. Greenfield B, Jolicoeur-Martineau A, Brown M, Kandiyoti A, Henry M, Sasson T, et al. Frequent follow-up of suicidal youth assessed in the emergency room: Long-term trajectory and predictors of suicidality. Prev Med. (2021) 152:106737. doi: 10.1016/j.ypmed.2021.106737
39. Kaess M, Brunner R, Chanen A. Borderline personality disorder in adolescence. Pediatrics. (2014) 134:782–93. doi: 10.1542/peds.2013-3677
40. Chanen A, McCutcheon L. Personality disorder in adolescence: The diagnosis that dare not speak its name. Personal Ment Health. (2008) 2:35–41. doi: 10.1002/pmh.28
41. Zimmerman M, Mattia JI. Psychiatric diagnosis in clinical practice: is comorbidity being missed? Compr Psychiatry. (1999) 40:182–91. doi: 10.1016/S0010-440X(99)90001-9
42. Armelius BA, Kullgren G, Renberg E. Borderline diagnosis from hospital records. Reliability and validity of Gunderson's Diagnostic Interview for Borderlines (DIB). J Nerv Ment Dis. (1985) 173:32–4. doi: 10.1097/00005053-198501000-00005
43. Larivière Erg N, Pérusse F, David P. Traduction et validation du questionnaire de dépistage Borderline Personality Questionnaire. Can J Psychiatry Rev Can Psychiatr. (2021) 66:306–12. doi: 10.1177/0706743720944079
44. Bouvard M, Fontaine-Buffe M, Cungi C, Adeleine P, Chapoutier C, Durafour E, et al. Etude préliminaire d'un entretien structuré des troubles de la personnalité: Le SCID II. [Preliminary study of the structured diagnostic interview for personality disorders: The SCID II.]. Encéphale Rev Psychiatr Clin Biol Thérapeutique. (1999) 25:416–21.
Keywords: borderline personality disorder, diagnosis, emergency department, brief intervention, short-term hospitalization
Citation: Artioli M, Bougon E, Mathur A and Salles J (2022) Factors associated with a borderline personality disorder diagnosis in the emergency department. Front. Psychiatry 13:925462. doi: 10.3389/fpsyt.2022.925462
Received: 21 April 2022; Accepted: 29 August 2022;
Published: 28 September 2022.
Edited by:
Alexandra Philipsen, University Hospital Bonn, GermanyReviewed by:
Jean Marc Guile, University of Picardie Jules Verne, FranceCopyright © 2022 Artioli, Bougon, Mathur and Salles. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juliette Salles, anVsaWV0dGUuc2FsbGVzQGhvdG1haWwuZnI=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.