
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychiatry, 17 June 2022
Sec. Psychological Therapy and Psychosomatics
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.922360
Premenstrual syndrome (PMS) is a common problem for women of reproductive age, affecting various aspects of their lives. While various in-person psychotherapeutic interventions, including Mindfulness therapy, have yielded promising results in reducing PMS symptoms, due to the COVID-19 Pandemic, psychotherapists are providing their services via online methods. Therefore, the present study is the first one worldwide to examine whether smartphone-based Mindfulness training can reduce symptoms of PMS and improve the quality of life in women with PMS. We recruited 80 Iranian women (aged 25–45) with PMS through online advertising who were randomly allocated into two groups of 40. The intervention group underwent two online introductory group sessions followed by 8 weeks of Mindfulness practice, while the control group received no intervention. Before and after the intervention, participants completed the 12-Item Short-Form Health Survey and the Premenstrual Symptoms Screening (PSST) questionnaires. Data were analyzed using the Analysis of Covariance (ANCOVA). Following the intervention, the mean scores of PMS symptoms were significantly lower in the intervention group than in the control group (p < 0.001; η2 = 0.18). Likewise, the quality of life score was significantly higher in the intervention group (p < 0.001; η2 = 0.14). Our results indicated that the smartphone-based Mindfulness training intervention could be an effective treatment modality for women with PMS symptoms, especially during the COVID-19 Pandemic, which has posed limitations for in-person therapies.
Clinical Trial Registration: https://fa.irct.ir/trial/59924, identifier: IRCT20180607040000N2.
Premenstrual syndrome (PMS) is a cyclic phenomenon of somatic and affective symptoms arising during the days preceding menses, disturbing one's regular functioning, followed by a symptom-free interval (1). The American Psychiatric Association (APA) has provided criteria for diagnosing premenstrual dysphoric disorder (PMDD), a severe form of PMS. Accordingly, women are diagnosed with PMDD when seriously impacted by moderate to severe symptoms, as described in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (2). In another definition proposed by the American College of Obstetricians and Gynecologists (ACOG), PMS is a clinical syndrome marked by the cyclic existence of physical and emotional symptoms irrelevant to any organic disease that occur during the 5 days before menses in each of the three prior menstrual cycles and disappear within 4 days of the onset of menses, without recurrence until at least process day (3).
PMS is one of the most common and disturbing health problems among women of childbearing age (4). Recent studies have indicated that more than 75% of women experience some degree of PMS during their reproductive years (5). The prevalence of PMS has been found to be 48% worldwide and 54.9% among the Iranian community sample (6). PMS can affect all age groups; however, the most commonly affected age group includes those 25–45 years old, though the regular treatment-seeking time is the mid or late third decade of life (7–9). Depending on the course of the condition, symptoms can begin from the onset of the first menstrual period and, if left untreated, can often continue from a woman's reproductive years to menopause (10).
More than 200 mild to severe symptoms have been described for PMS, all of which interfere with the daily life of affected women (11, 12). However, the common signs that characterize this syndrome include psychological (e.g., irritability, mood swings, depression, anxiety, and impulsivity), physical (e.g., bloating, breast tenderness, pain, and headache), and behavioral (e.g., lack of coordination, sleep disorders and changes in appetite) symptoms (13, 14). PMS strongly and negatively affects women's quality of life and health, resulting in a significant decrease in mental wellbeing, productivity at work, and academic performance. It also makes the patients more likely to visit a doctor, increasing healthcare costs. Therefore, there is a need for effective treatment for PMS.
Unfortunately, treatment interventions for PMS have remained a significant challenge (15). Over the recent two decades, several studies have been conducted to examine the effectiveness of various pharmacological and non-pharmacological treatment alternatives on PMS (16, 17). While medications effectively relieve PMS syndrome, they have several side effects: nausea, sleep problems, sexual dysfunctions, headache, gastrointestinal problems, vomiting, and drowsiness (18, 19). Since the symptoms of PMS can be chronic and long-lasting, special attention should be paid to the side effects of medical interventions. Most women do not adhere to medical treatments (i.e., using medications) mainly due to side effects or contraindications. Patients often seek non-pharmacological treatment options to deal with the symptoms. Thus, other safe and effective treatment approaches should be considered in the treatment of PMS. In this regard, psychological interventions have produced promising results in the treatment of PMS (20).
The American College of Obstetricians and Gynecologists has identified non-medical interventions as a first-line treatment option for less severe PMS (3). These non-pharmacological approaches include: Lifestyle Changes, Exercise, Diet Change, Stress Management, Biofeedback, Cognitive-Behavioral Therapy, Relaxation Techniques, and Mindfulness (21–23).
Mindfulness therapy is one of the treatment modalities that have produced promising results in the treatment of PMS. The concept of Mindfulness was first examined by Buddhist traditions in philosophical terms unknown to readers nowadays. However, Mindfulness has extended swiftly in Western psychology research and practice, mainly because of the successful standardized Mindfulness-based interventions (24), including Mindfulness-based stress reduction (MBSR) (25) and Mindfulness-based cognitive therapy (MBCT) (26), which assimilate the core of Eastern Mindfulness practices into the Western cognitive-behavioral approach. In one of the most commonly cited definitions, Mindfulness is the awareness that arises through “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally”. Likewise, Baer (27) has defined Mindfulness as “the non-judgmental observation of the ongoing stream of internal and external stimuli as they arise”.
Research on Mindfulness-based interventions (MBIs) has increased exponentially in the past decade. The most common Mindfulness-based interventions include Mindfulness-Based Stress Reduction (MBSR) (25) and Mindfulness-Based Cognitive Therapy (MBCT) (26). MBSR is a model of psychotherapy that combines Mindfulness techniques with stress management techniques (28). At the same time, Mindfulness-Based Cognitive Therapy (MBCT) is a multimodal intervention that integrates training in Mindfulness meditation and the cognitive theory of affective disorders (29).
Several studies have examined the effect of MBIs on PMS. For instance, Blut et al. (30) examined the impact of an 8-week Mindfulness-based intervention on 21 women aged 18–52 years with menstrual-related mood disorders (MRMDs). Results indicated a significant decrease in symptom severity for seven of the 11 (e.g., depression, anxiety, mood swings, and irritability) premenstrual symptoms, increased pain tolerance to the cold pressure, and decreased blood pressure reactivity to mental stress. Likewise, Panahi and Faramarzi (15) investigated the effect of Mindfulness-based cognitive therapy on depression and anxiety in women with PMS in a randomized controlled trial with 60 samples. The results showed that MBCT intervention is acceptable and potentially beneficial in women with PMS symptoms. Psychotherapy should be considered a treatment option for mild to moderate PMS in women with depressive symptoms. In another study, Khaleghi et al. (31) examined the effectiveness of Mindfulness training on inner happiness and non-impulsive behavior with a sample of 40 women with PMS. The results showed that Mindfulness training effectively increased inner satisfaction and reduced non-impulsive behavior in women with PMS.
In recent years, many health services have been severely affected by the COVID-19 Pandemic. Governments took decisive actions to restrict residents' freedom to reduce the contagion, forcing people to avoid unnecessary face-to-face interactions and social gatherings and limiting their movement to the strictly necessary. Like other healthcare treatments, psychotherapy was not subject to entire governmental regulations, and therapists could maintain in-person psychotherapy sessions. However, doing so was practically challenged in private clinics and public health systems, considering that face-to-face meetings could increase the risk of infection for both therapists and patients. Thus, psychotherapists were encouraged to provide their professional services via digital devices to guarantee the continuation of previously active therapeutic interventions. This state of affairs has sparked an unprecedented embrace of virtual healthcare technologies. Therefore, considering the prevalence of PMS and the effectiveness of psychotherapeutic interventions such as MBIs on PMS, it is necessary to develop some smartphone-based interventions to provide psychological services for this group of patients during the COVID-19 epidemic.
Virtual technologies have been widely used to provide mindfulness training (e.g., Mindfulness-based smartphone applications) (32). A meta-analysis indicated that digital Mindfulness training has significant beneficial effects on stress, anxiety, depression, and mental health (33). Likewise, several recent studies showed that Mindfulness training provided through a smartphone app reduced depressive symptoms and improved QOL and wellbeing (34). Also, Friis-Healy et al. (35) found that virtually-delivered psychotherapeutic interventions can increase therapeutic alliance for patients resistant to in-person therapies due to financial constraints or stigma.
To our knowledge, no study has examined the effect of smartphone-based Mindfulness training intervention on reducing the symptoms of PMS. Developing such treatment is necessary given the restrictions that have been raised due to the COVID-19 Pandemic. Besides, this type of intervention will benefit PMS patients who cannot attend in-person therapy because of employment, housekeeping, having a young child, living in remote areas, suffering from physical disabilities, and having heart diseases. Therefore, the present study aimed to examine the effect of smartphone-based Mindfulness training intervention on reducing PMS symptoms and increasing the quality of life (QOL) in a sample of individuals with PMS and a control group using the Persian version of the Mindfulness training mobile app.
A two-group randomized controlled, pretest-posttest design was used. Participants were recruited through online advertising through social media sites and poster advertisements. At first, 460 individuals showed interest in participating in the study and completed the pre-questionnaires after providing online signed informed consent; however, 340 individuals were excluded from the study based on the exclusion/inclusion criteria (Table 1). The G-power program was used to calculate the minimum sample size needed for our study, with an alpha of 0.05, a power of 90%, and an expected medium effect size (r = 0.6). It was determined that a minimum of 72 participants was required to find statistically significant differences, though considering the possibility of dropouts, we included a total of 120 individuals (60 per group) who were randomly assigned to one of the intervention and control groups based on the simple randomization method using the rand function of Excel software (A graphic depiction of the recruitment process is presented in Figure 1). Participants were selected based on exclusion/inclusion from women who completed the online pre-questionnaires shared on social media (Table 1). Of the 60 participants in the intervention group, 20 participants were dropped out before completing the 8-week intervention due to a lack of cooperation for more than 3 days. Likewise, 20 participants dropped out of the control group because they did not respond to the post-study survey. Therefore, data of 80 participants from intervention group (n = 40, M age = 31.42, SD = 4.82) and control group (n = 40, M age = 32.62, SD = 6.15) were analyzed.
This study was first reviewed and approved by the Research Deputy of Iran University of Medical Sciences (Code Number = IR.IUMS.REC.1400.659). The study was registered in the Iranian Registry of Clinical Trials (ID Number = IRCT20180607040000N2, Registration date: 2021-11-28). The 120 participants who met the criteria for participating in the study were asked to complete the remaining pre-questionnaire (i.e., the PSST, GHQ-28, and SF-12). Once the participants completed the measures, we created two groups on WhatsApp. The participants in the control group were told that they were on the waiting list and that their sessions would be held after 2 months. The first author developed the Mindfulness training application (Mindfulness Coach Persian Version; Tehran, Iran) based on the manual by Chaskalson (40). Then, the manual's content was translated to Farsi and reviewed by the authors. First, two 1-h group training sessions were held for the intervention group by the first author through Skype. The participants were familiarized with premenstrual syndrome, the foundations of Mindfulness, and how to use the Mindfulness coach app. Both sessions were recorded and shared on the WhatsApp group of the intervention group so that members could download the video files of the meeting if any of them missed any part of the sessions. Then, the download file of the application (an app file type designed for the Android platform) was shared with participants in the intervention group, and they were asked to install the app on their smartphones. The participants were instructed to perform the exercises specified by the app for at least 20 min per day for 8 consecutive weeks. For 8 weeks, daily notifications were sent to each participant to remind them to perform the exercises. Both groups were asked to complete the post-questionnaires at the end of week eight. Then, we provided the same two 1-h group training sessions for the control group, followed by the same intervention provided for the intervention group. As a reward for participating in the study, both groups' members were granted free 1-year membership for the Mindfulness training application.
First, two 1-h introductory sessions were provided for the intervention group (The content of these sessions with a brief description could be retrieved from Table 2). Next, the Mindfulness-based intervention was carried out using a smartphone app, which included 8 weeks of Mindfulness exercises aimed at alleviating PMS symptoms, including psychological (e.g., irritability, mood swings, depression, anxiety, and impulsivity), physical (e.g., bloating, breast tenderness, pain, and headache), and behavioral (e.g., lack of coordination, sleep disorders, and changes in appetite) symptoms and increase the quality of life. The intervention group performed specific exercises related to each week every day for 8 consecutive weeks (56 days). In each stage, step-by-step instructions and audio/video exercises were provided based on the two approaches of Mindfulness, including Mindfulness-based stress reduction (MBSR) and Mindfulness-based cognitive therapy (MBCT). The content of the sessions with a brief description is provided in Table 3.
The GHQ-28 is a self-report measure designed by Goldberg and Hillier (41) and widely used as a screening tool for mental disorders. It includes four subscales of somatic symptoms, anxiety and sleep disturbance, social dysfunction, and depression (42). Twenty-eight items of the measure are rated on a four-point Likert scoring system (from 0 to 3), with a total maximum score of 84 and a minimum of zero. Psychiatric morbidity is defined as a total score of ≥23, and a score of ≥7 in each subscale is defined as psychiatric morbidity. Studies on the validation of the GHQ-28 have demonstrated its high validity and reliability in different countries (41). The psychometrics of the Persian version of the GHQ28 was supported by Nazif et al. (39). In the current study, the reliability of GHQ-28 based on Chronbach's alpha was 0.85 for the GHQ-28 total score and ranged from 0.65 to 0.74 for the subscales scores.
PSST is a self-report questionnaire developed by Steiner et al. (43). PSST has 19-items loading on two domains. The first domain includes 14 items assessing psychological, physical, and behavioral symptoms; the second domain has five items and evaluates the impact of symptoms on women's functioning. Each item is rated on a four-point Lickert type scale (not at all = 0, mild = 1, moderate = 2, severe = 3). Hariri et al. (37) translated and validated the Persian version of the PSST. In the current study, Chronbach's alpha was 0.89, 0.82, and 0.85 for the PSST total score and subscales of mood symptoms and behavioral and physical symptoms, respectively.
The 12-Item Short-Form Health Survey (SF-12) is a widely used measure to evaluate health-related quality of life (HRQoL). It is a subset of the larger SF-36 and monitors health in general and specific populations. The SF-12 was designed by Ware et al. (44) and measures eight health aspects, including physical functioning, role limitations due to physical health problems, bodily pain, general health, vitality (energy/fatigue), social functioning, role limitations due to emotional issues, and mental health (psychological distress and psychological wellbeing). Two subscales are derived from the SF-12, including the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Montazeri et al. (45) examined the psychometrics of the SF-12 in Iran and concluded that the measure is suitable for use with Iranian samples. Scores of 12–24 indicate poor quality of life, 25–36 indicate average quality of life, and 48–37 show good quality of life. In the current study, Chronbach's alpha was 0.79, 0.72, and 0.74 for the SF-12 total score and subscales of mental and physical health, respectively.
We used SPSS 20 software for data entry and statistical analyses. The normality of the distribution for outcome measures was tested using the Kolmogorov–Smirnov test, and the results supported the normality of the data (p > 0.05). The independent-samples t-test was used to detect initial differences between groups in age. At the same time, the Chi-square test was implemented to compare descriptive variables of the groups, including marital status and level of education. We performed a series of analyses of covariance (ANCOVA) to determine whether the groups differed in their reported levels of behavioral and somatic symptoms of PMS and reported levels of QOL scores using baseline values as covariates. The following rules of thumb are used to interpret values for Partial eta squared: η2 = 0.01 indicates a small effect; η2 = 0.06 indicates a medium effect; η2 = 0.14 indicates a large effect. It was decided beforehand that a p level of <0.05 would be accepted as indicating statistically significant results.
As shown in Tables 4, 5, groups did not differ significantly on demographic variables, including marital status, level of education, and age. Thus, the groups were matched in these variables. To examine if the Mindfulness intervention has resulted in significant differences in PSST and SF-12 total scores (dependent variables), two sets of ANCOVAs with baseline values as covariates were conducted. Results indicated that the intervention group scored significantly lower than the control group in total score of PSST [F(1, 75) = 2.27, p < 0.001, η2 = 0.18] and higher in terms of the SF-12 total score [F(1, 75) = 68.65, p < 0.001, η2 = 0.14]. Further, to examine whether the groups scored significantly different in the subscales scores of PSST and SF-12, we conducted four one-way ANCOVAs, with- baseline values as covariates. Results revealed that the intervention group had significantly lower PSST mood [Wilks' λ = 0.275; F(1, 75) = 17.20; p < 0.001; η2 = 0.17] and behavioral/physical symptoms scores [Wilks' λ = 0.275; F(1, 75) = 89.21; p < 0.001; η2 = 0.15] than the control group. Similarly, the intervention group scored significantly higher in SF-12 physical health [Wilks' λ = 0.331; F(1, 75) = 5.50; p < 0.001; η2 = 0.11] and mental health [Wilks' λ = 0.275; F(1, 75) = 11.15; p < 0.001; η2 = 0.15] scores compared with the control group. Table 6 presents the means and standard deviations of study variables in pre-test and post-test for each group.
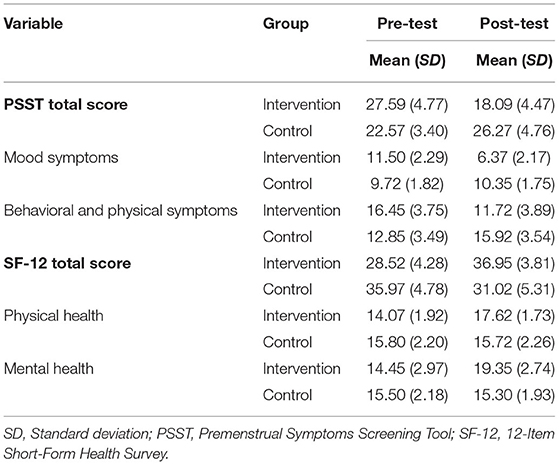
Table 6. Descriptive information about the premenstrual symptoms, quality of life scores in pre-test and post-test.
This study aimed to examine the effectiveness of smartphone-based Mindfulness training intervention in reducing PMS symptoms and increasing the quality of life (QOL) using the Persian version of the Mindfulness training mobile app. Based on the effect size values, these differences were in the strong range for the PMS symptoms and were in the moderate to strong ranges for the QOL scores assessed by SF-12. To the best of our knowledge, very few studies have examined the effectiveness of Mindfulness-based intervention on PMS symptoms. Moreover, our study is the first one worldwide to explore the efficacy of smartphone-based Mindfulness training intervention on PMS symptoms and the quality of life (QOL). Overall, our results indicated that the intervention significantly reduced the PMS' psychological, physical, and behavioral symptoms and also considerably improved the quality of life among PMS patients. We discuss our findings below.
Our findings supported the effectiveness of Mindfulness training using the Persian version of the Mindfulness training app in reducing the physical and behavioral symptoms of PMS, which is in line with a few previous research (46–48). For example, Askari et al. (46) examined the effect of MCBT on PMS symptoms; their results showed that MCBT reduced physical and behavioral symptoms of PMS significantly. Mindfulness is a balanced sense of consciousness that helps- individuals observe and accept emotions and physical experiences as clearly as they occur. Thus, in the case of PMS, Mindfulness intervention can help patients feel and accept their feelings/emotions and physical symptoms such as pain. Consequently, the extent of attention and oversensitivity to reporting these symptoms are reduced (49). Furthermore, Mindfulness helps patients be fully aware of their thoughts and feelings and accept them without judgment, be in a state of calm and concentration, and gain the ability to control their thoughts, anxiety, and emotions. As a result, Mindfulness therapy helps patients develop a remarkable ability to cope with the physical and behavioral symptoms of PMS (50). Mindfulness works exactly like when people consciously turn their awareness to the experiences they are going through here and now. Therefore, Mindfulness treatment could have helped the participants become aware of their cognitive, behavioral, and emotional responses to PMS symptoms, allowing patients to modify their relationship with their painful thoughts and feelings on PMS symptoms and reduce the impact of these thoughts and feelings on their lives (51).
Furthermore, our results indicated a significant reduction in mood symptoms of PMS after the Mindfulness treatment, a finding consistent with previous studies (15, 30, 48). For example, Bluth et al. (30) examined the effect of an 8-week Mindfulness-based intervention on 21 women with menstrually related mood disorders (MRMDs). Results indicated a significant reduction in symptom severity for seven of the 11 (e.g., depression, anxiety, mood swings, and irritability) PMS symptoms. Similarly, Panahi and Faramarzi (15) explored the effect of MBCT on depression and anxiety symptoms in PMS patients, and the results showed that MBCT significantly reduced PMS symptoms and anxiety and depression symptoms. In this regard, it could be said that Mindfulness encourages combining meditation and specific mental orientations toward an experience and awareness of the present in a non-judgmental way by minimizing the conflict in thoughts and feelings. Mindfulness meditation activates an area of the brain that creates positive emotions, has beneficial effects on the body's immune function, and alleviates depression (52). Following Mindfulness training, the person learns to identify stressful situations, become fully aware of them, and consciously control experiences such as depression, anxiety, and stress. As soon as the individuals master their reactions in-depth, they can modify their responses to stressful, anxiety-provoking, and depressive situations and use positive instead of negative ones (53). Given its non-judgmental- approach to internal experiences (feelings and cognitions), Mindfulness allows individuals to reduce their automatic reactions in dealing with stressful experiences. With the passage of time and increased awareness and acceptance of life incidents that can be changed, activation of response systems to stress and physical symptoms decreases (15).
Finally, our findings showed the significant effectiveness of Mindfulness training in improving the physical and mental dimensions of the quality of life in individuals with PMS, which dovetails with the results of prior studies (54–56). For example, van Emmerik et al. (54) examined the effect of Mindfulness-Based Mobile Application intervention on quality of life, general psychiatric symptoms, and self-actualization. The results showed that it is possible to achieve the long-lasting positive impact of Mindfulness intervention on general psychiatric symptoms and several aspects of quality of life at low costs with smartphone apps for Mindfulness. Mindfulness can improve the quality of life in several ways: First, Mindfulness helps individuals notice that cognition, thoughts, and feelings are fleeting thoughts and feelings. This attitude reduces rumination, and automatic thoughts, leading to reduced negative emotions and unpleasant reactions and effective management of these emotions (57). Second, while Mindfulness emphasizes the acceptance of the current situation, individuals with PMS try to change the actual unfavorable situation. Thus, Mindfulness focuses on helping patients be satisfied with the current situation rather than sustained efforts to address the possible future issues. Accepting the recent situation results in an elevated sense of- satisfaction and happiness, which is not conditional on the type of experience. Finally, Mindfulness may improve women's physical and psychological health with PMS by encouraging them to perform muscle relaxation techniques and reducing aggravating physical reactions to stress, resulting in improved quality of life (58).
The results from the current study should be interpreted considering a few limitations. First, due to the lack of access to the intervention group after the post-treatment assessment, we could not perform a follow-up analysis to examine the long-term effects of the intervention. It is suggested that future research include follow-ups to examine the long-term effectiveness of the intervention. Second, we did not use a Mindfulness measure to see if the Mindfulness scores had significantly enhanced after the intervention. Third, using a sample of volunteers is also a limitation, as there may be a reason to self-select, which leads to bias. Fourth, using self-report measures for primary outcomes may be considered a limitation, though this is how PMS is commonly measured. Fifth, analyses in this study followed a per-protocol design but not an intention-to-treat one; the latter type of study design is used to nullify the effects of crossover and dropout, which may break the random assignment to the treatment groups in a study. Sixth, our study sample included highly educated women suffering from moderate to severe PMS; thus, the results should be interpreted only for individuals with high education. Finally, since this study was the first worldwide to examine smartphone-based Mindfulness intervention with a PMS sample, we suggest future studies replicate the results in various cultures. This includes translating the app to other languages and examining the efficacy of the intervention.
Our findings suggested that smartphone-based Mindfulness training intervention is an effective treatment for highly educated individuals suffering from moderate to severe PMS. More specifically, this intervention could be an excellent treatment modality during the COVID-19 Pandemic, wherein therapists prefer online therapies over in-person interventions because of the safety of both parties. Such interventions can increase access to treatment and reduce treatment costs so more patients can benefit from it.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Research Deputy of Iran University of Medical Sciences (Code Number: IR.IUMS.REC.1400.659). The patients/participants provided their written informed consent to participate in this study.
DM designed the Mindfulness coach app, performed the intervention, and prepared the manuscript. KZ and BG supervised the study and reviewed and revised the manuscript. All authors have contributed to the study and agreed to the publication of the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by the Iran University of Medical Sciences (IUMS), Tehran, Iran; Grant Number = IUMS-1400-1-50-20718.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors appreciate all women who voluntarily participated in this study. We also appreciate Mr. Mojtaba Elhami Athar for reviewing and revising the final draft of the current study.
1. Gudipally PR, Sharma GK. Premenstrual Syndrome. StatPearls. Treasure Island, FL: StatPearls Publishing (2022).
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association (2013).
3. Bulletins–Gynecology ACoP. ACOG Practice Bulletin: No 15: premenstrual syndrome. Obstetr Gynecol. (2000) 95(Suppl. 1–9).
4. Banth S, Ardebil MD. Effectiveness of Mindfulness meditation on pain and quality of life of patients with chronic low back pain. Int J Yoga. (2015) 8:128–33. doi: 10.4103/0973-6131.158476
5. Rapkin AJ. Lewis EI. Treatment of premenstrual dysphoric disorder. Womens Health. (2013) 9:537–56. doi: 10.2217/WHE.13.62
6. Ranjbaran M, Omani Samani R, Almasi-Hashiani A, Matourypour P, Moini A. Prevalence of premenstrual syndrome in Iran: a systematic review and meta-analysis. Int J Reprod Biomed. (2017) 15:679–86. doi: 10.29252/ijrm.15.11.679
7. Sharma B, Sharma RK, Agarwal T, Jindal M, Singh K. Study of the effect of 61-point relaxation therapy in premenstrual syndrome. Natl J Physiol Pharm Pharmacol. (2019) 9:155–9. doi: 10.5455/njppp.2019.9.1134212122018
8. Cohen LS, Soares CN, Otto MW, Sweeney BH, Liberman RF, Harlow BL. Prevalence and predictors of premenstrual dysphoric disorder (PMDD) in older premenopausal women. The Harvard study of moods and cycles. J Affect Disord. (2002) 70:125–32. doi: 10.1016/S0165-0327(01)00458-X
9. Giulio G, Reissing E. Premenstrual dysphoric disorder: prevalence, diagnostic considerations, and controversies. J Psychosom Obstetr Gynecol. (2007) 27:201–10. doi: 10.1080/01674820600747269
10. Rapkin AJ, Winer SA. Premenstrual syndrome and premenstrual dysphoric disorder: quality of life and burden of illness. Expert Rev Pharmacoecon Outcomes Res. (2009) 9:157–70. doi: 10.1586/erp.09.14
11. Braverman PK. Premenstrual syndrome and premenstrual dysphoric disorder. J Pediatr Adolesc Gynecol. (2007) 20:3–12. doi: 10.1016/j.jpag.2006.10.007
12. Campagne DM, Campagne G. The premenstrual syndrome revisited. Eur J Obstet Gynecol Reprod Biol. (2007) 130:4–17. doi: 10.1016/j.ejogrb.2006.06.020
13. Katzinger J, Hudson T. 212 - premenstrual syndrome. In: Pizzorno JE, Murray MT, editors. Textbook of Natural Medicine, 5th ed. St. Louis, MO: Churchill Livingstone (2020). p. 1739–47.e3.
14. Freeman EW, Sammel MD, Rinaudo PJ, Sheng L. Premenstrual syndrome as a predictor of menopausal symptoms. Obstet Gynecol. (2004) 103:960–6. doi: 10.1097/01.AOG.0000124804.81095.7f
15. Panahi F, Faramarzi M. The effects of mindfulness-based cognitive therapy on depression and anxiety in women with premenstrual syndrome. Depress Res Treat. (2016) 2016:9816481. doi: 10.1155/2016/9816481
16. Hantsoo L, Epperson CN. Premenstrual dysphoric disorder: epidemiology and treatment. Curr Psychiatry Rep. (2015) 17:87. doi: 10.1007/s11920-015-0628-3
17. Ussher J, Perz J. PMS as a process of negotiation: women's experience and management of premenstrual distress. Psychol Health. (2013) 28:909–27. doi: 10.1080/08870446.2013.765004
18. Shapiro SSJD. Treatment of dysmenorrhoea and premenstrual syndrome with non-steroidal anti-inflammatory drugs. Drugs. (1988) 36:475–90. doi: 10.2165/00003495-198836040-00005
19. Jarvis CI, Lynch AM, Morin AK. Management strategies for premenstrual syndrome/premenstrual dysphoric disorder. Ann Pharmacother. (2008) 42:967–78. doi: 10.1345/aph.1K673
20. Montazeri S. Non-pharmacological treatment of premenstrual syndrome. Afr J Midwifery Women Health. (2011) 5:148–52. doi: 10.12968/ajmw.2011.5.3.148
21. Lafrance MN, McKenzie-Mohr SJF. The DSM and its lure of legitimacy. Psychology. (2013) 23:119–40. doi: 10.1177/0959353512467974
22. Pearlstein TB, Halbreich U, Batzar ED, Brown CS, Endicott J, Frank E, et al. Psychosocial functioning in women with premenstrual dysphoric disorder before and after treatment with sertraline or placebo. J Clin Psychiatry. (2000) 61:101–9. doi: 10.4088/JCP.v61n0205
23. Ussher JM. Premenstrual syndrome: fact, fantasy or fiction?. In: Psychology at the Turn of the Millennium: Congress Proceedings: XXVII International Congress of Psychology, Stockholm, 2000, Volume 2. (2002). (pp. 497—528).
24. Gu J, Strauss C, Bond R, Cavanagh K. How do Mindfulness-based cognitive therapy and Mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. (2015) 37:1–12. doi: 10.1016/j.cpr.2015.01.006
25. Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of Mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. (1982) 4:33–47. doi: 10.1016/0163-8343(82)90026-3
26. Segal ZV, Teasdale JD, Williams JMG. Mindfulness-based cognitive therapy: Theoretical rationale and empirical status. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York, NY: Guilford Press (2004), pp. 45–65.
27. Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol. (2003) 10:125. doi: 10.1093/clipsy.bpg015
29. Segal Z, Dimidjian S, Vanderkruik R, Levy J A. maturing Mindfulness-based cognitive therapy reflects on two critical issues. Curr Opin Psychol. (2019) 28:218–22. doi: 10.1016/j.copsyc.2019.01.015
30. Bluth K, Gaylord S, Nguyen K, Bunevicius A, Girdler S. Mindfulness-based stress reduction as a promising intervention for amelioration of premenstrual dysphoric disorder symptoms. Mindfulness. (2015) 6:1292–302. doi: 10.1007/s12671-015-0397-4
31. Khaleghi F, Asgari P, Heydari A. The effectiveness of mindfulness of internal happiness, impulsive behavior in women with premenstrual syndrome. MJMS. 61(supplment1), 38–49.
32. Plaza I, Demarzo MMP, Herrera-Mercadal P, García-Campayo J. Mindfulness-based mobile applications: literature review and analysis of current features. JMIR Mhealth Uhealth. (2013) 1:e2733. doi: 10.2196/mhealth.2733
33. Economides M, Martman J, Bell MJ, Sanderson B. Improvements in stress, affect, and irritability following brief use of a mindfulness-based smartphone app: a randomized controlled trial. Mindfulness. (2018) 9:1584–93. doi: 10.1007/s12671-018-0905-4
34. Howells A, Ivtzan I, Eiroa-Orosa FJ. Putting the ‘apptin happiness: a randomised controlled trial of a smartphone-based Mindfulness intervention to enhance wellbeing. J Happ Stud. (2016) 17:163–85. doi: 10.1007/s10902-014-9589-1
35. Friis-Healy EA, Nagy GA, Kollins SH. It is time to REACT: opportunities for digital mental health apps to reduce mental health disparities in racially and ethnically minoritized groups. JMIR Ment Health. (2021) 8:e25456. doi: 10.2196/25456
37. Hariri FZ, Moghaddam-Banaem L, Siah Bazi S, Saki Malehi A, Montazeri A. The Iranian version of the premenstrual symptoms screening tool (PSST): a validation study. Arch Womens Ment Health. (2013) 16:531–7. doi: 10.1007/s00737-013-0375-6
38. Patricio B, Sergio B. Normal Menstrual Cycle. In: Menstrual Cycle. IntechOpen. (2019). doi: 10.5772/intechopen.79876
39. Nazifi M, Mokarami H, Akbaritabar A, Faraji Kujerdi M, Tabrizi R, Rahi A. Reliability, validity and factor structure of the persian translation of general health questionnire (GHQ-28) in Hospitals of Kerman University of Medical Sciences. J Adv Biomed Sci. (2014) 3:336–42. doi: 10.17795/jhealthscope-15547
40. Chaskalson M. Mindfulness in Eight Weeks: The Revolutionary Eight Week Plan to Clear Your Mind and Calm Your Life. London: HarperThorsens (2014).
41. Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. (1979) 9:139–45. doi: 10.1017/S0033291700021644
42. Sterling M. General health questionnaire - 28 (GHQ-28). J Physiother. (2011) 57:259. doi: 10.1016/S1836-9553(11)70060-1
43. Steiner M, Macdougall M, Brown E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch Womens Ment Health. (2003) 6:203–9. doi: 10.1007/s00737-003-0018-4
44. Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
45. Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item Short Form Health Survey (SF-12): factor structure, internal consistency and construct validity. BMC Public Health. (2009) 9:1–10. doi: 10.1186/1471-2458-9-341
46. Askari S, Behroozy N, Abbaspoor Z. The effect of mindfulness-based cognitive-behavioral therapy on premenstrual syndrome. Iran Red Crescent Med J. (2018) 20. doi: 10.5812/ircmj.57538
47. Bagheri S, Sajjadian I. Effectiveness of mindfulness-based stress reduction treatment on the severity of sympoms and pain catastrophizing in students with premenstrual dysphoric disorder. J Anesthesiol Pain. (2018) 9:52–65.
48. Lustyk MKB, Gerrish WG, Douglas H, Bowen S, Marlatt GA. Relationships among premenstrual symptom reports, menstrual attitudes, and mindfulness. Mindfulness. (2011) 2:37–48. doi: 10.1007/s12671-011-0041-x
49. Farrokh-Eslamlou H, Oshnouei S, Heshmatian B, Akbari E. Premenstrual syndrome and quality of life in Iranian medical students. Sex Reprod Healthc. (2015) 6:23–7. doi: 10.1016/j.srhc.2014.06.009
50. Rezaei Shojaei S, Farokhzad P, Ghaemi F, Farrokhi N. A comparison of effectiveness of Mindfulness training and pilates on reducing symptoms of premenstrual syndrome in girl. J Psychol Sci. (2019) 17:957–62.
51. Deihimi M, Noori M. Effectiveness of group therapy of mindfulness -based stress reduction on rumination and loneliness of women with premenstrual syndrome. J Psychol Stud. (2019) 15:39–54.
52. Enayat F, Ataee Far R, Abaspoor Azar Z. The effectiveness of training mindfulness skills on depression, anxiety and stress of female with premenstrual syndrome. AUMJ. (2021) 10:427–38.
53. Validi Pak A, Khodai A, Sheykhaleh S. Effectiveness of cognitive-based mindfulness training of depression reduction on patient suffering from cancer. J Clin Psychol Pers. (2020) 14:49–57.
54. van Emmerik AAP, Berings F, Lancee J. Efficacy of a mindfulness-based mobile application: a randomized waiting-list controlled trial. Mindfulness. (2018) 9:187–98. doi: 10.1007/s12671-017-0761-7
55. Nyklíček I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med. (2008) 35:331–40. doi: 10.1007/s12160-008-9030-2
56. Godfrin KA, van Heeringen C. The effects of Mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behav Res Ther. (2010) 48:738–46. doi: 10.1016/j.brat.2010.04.006
57. Smith B, Metzker K, Waite R, Gerrity P. Short-form Mindfulness-based stress reduction reduces anxiety and improves health-related quality of life in an inner-city population. Holist Nurs Pract. (2015) 29:70–7. doi: 10.1097/HNP.0000000000000075
Keywords: Mindfulness, premenstrual syndrome, quality of life, Mindfulness-app, mobile health (MHealth)
Citation: Mazaheri Asadi D, Zahedi Tajrishi K and Gharaei B (2022) Mindfulness Training Intervention With the Persian Version of the Mindfulness Training Mobile App for Premenstrual Syndrome: A Randomized Controlled Trial. Front. Psychiatry 13:922360. doi: 10.3389/fpsyt.2022.922360
Received: 17 April 2022; Accepted: 23 May 2022;
Published: 17 June 2022.
Edited by:
Barna Konkoly-Thege, Waypoint Centre for Mental Health Care, CanadaReviewed by:
Ali Asgharzadeh, Tabriz University of Medical Sciences, IranCopyright © 2022 Mazaheri Asadi, Zahedi Tajrishi and Gharaei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Komeil Zahedi Tajrishi, emFoZWRpLmtAaXVtcy5hYy5pcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.