- 1Centre for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2NHC Key Lab of Health Economics and Policy Research, Shandong University, Jinan, China
- 3Department of Health Administration, Graduate School, Yonsei University, Wonju, South Korea
- 4Yonsei Global Health Center, Yonsei University, Wonju, South Korea
Depression among university students and international university students is an increasing problem globally. This study aimed to clarify the differences on the conditions and determinants of the knowledge, preventive practices and depression of the Chinese international students and local Korean students in South Korea during the COVID-19 pandemic. An online cross-sectional questionnaire including general demographic characteristics, COVID-19-related knowledge, preventive practice, and the Patient Health Questionnaire (PHQ-9) was applied from March 23 to April 22, 2020. A total of 533 university students (171 Chinese international students and 362 local South Korean students) were included in the study. The majority of both Chinese international students and local South Korean students had a good comprehension of COVID-19. Chinese international students in South Korea showed better preventive practice than local Korean students, while the proportion of moderate to severe depression of Chinese international students was relatively higher (28.07%) than that of local Korean students (22.38%). Determinants of depression of Chinese international students in South Korea were information satisfaction, likelihood of survival after infection, symptoms of a cough and feelings of discrimination, while for local Korean students were gender, educational level, family, suspected symptoms, self-assessed physical health status, COVID-19 detection, population contact history and online sources of information. These results could be used as a reference for decreasing the depressive symptoms among the university students.
Introduction
The coronavirus disease (COVID-19) first appeared in Wuhan, China, spreading nationwide between December 2019 and early 2020, and then quickly to various countries (1). On January 30, 2020, the World Health Organization (WHO) declared the SARS-CoV-2 outbreak as a public health emergency of international concern, and on March 11, in Geneva, Switzerland, WHO Director-General Desmond Tan attended a press conference wherein he stated that the outbreak should be considered a pandemic (2). Starting in February 2020, South Korea experienced a sharp increase in confirmed cases (3). As of November 8, 2021, there were 126,713 and 5,696 cumulative confirmed cases and deaths, respectively, in China and 381,694 and 2,980 cumulative confirmed cases and deaths in South Korea, and the pandemic is reoccurring and circulating at multiple points. Knowledge and preventive practice are important to restrict the spread and avoid the related mental health problems during COVID-19 (4).
The main routes of transmission are air, droplets, aerosols, and, to a lesser extent, urine and feces (5). The study of knowledge, attitudes, and perceptions of COVID-19 in sub-Saharan Africa noted that, although most participants had adequate knowledge, attitudes were not always positive (6). The effect of control measures on COVID-19 transmission in South Korea confirms the importance of maintaining social distance and emphasizing personal hygiene, such as wearing masks, washing hands, and avoiding gatherings (7). Numerous studies showed that this pandemic leads to additional mental health problems, including anxiety, depression, insomnia, suicide, and self-injury (8–10).
Higher education levels were associated with possible depression and a higher frequency of mask wearing (11). Following preventive health behaviors may be safer for people and their health, It is also associated with lower depression, anxiety, and stress (12). Higher levels of psychological distress were associated with higher levels of fear. Moreover, if higher levels of psychological problems were demonstrated by those who identified as patients and individuals in isolation, then resilience played a key role in overcoming the psychological impact (13). A Malaysian study noted that introducing adequate, easy-to-follow precautions and standard operating procedures by university healthcare workers was associated with a reduction in their depression, anxiety, and stress (14). The use of online psychotherapy and the promotion of online social platforms to maintain social communication and relationships were significantly associated with increased physical, psychological, and social quality of life (QoL) and decreased depressive and anxiety symptoms as well as depression with anxiety symptoms during the COVID-19 (15).
During COVID-19 pandemic, a significant increase in psychological distress, fear, allostatic load, fatigue, loneliness, and worry was observed across different populations (16–18). During an outbreak, children are restricted to their homes without outdoor activities or interaction with friends. Hence, the negative impact on mental health can be more severe (19). COVID-19 led to significantly higher unemployment and suicide rates, and insecurity and uncertainty about the future deteriorated the psychological condition of migrant workers (20). There is a higher prevalence of anxiety, burnout, depression, and psychological distress among healthcare workers (21). COVID-19 infection negatively affects the psychological state of soccer players, with higher scores for depression, stress, and psychological distress among soccer players with higher income loss (22).
Although some studies explored the psychological adverse effects of COVID-19, the investigation of depression symptoms during the COVID-19 pandemic among the Chinese and Korean students had received little attention. According to the Korea Education Development Agency, among the total number of international students in South Korea, 67,030 were Chinese in 2020, accounting for 43.6% (23). The university students in South Korea, who are socially vulnerable, are more prone to depression during the COVID-19 pandemic (24). Although there is no nationwide lockdown in South Korea, strict control measures are implemented in public places, educational institutions, churches, and university campuses, where isolation and disconnection from society are a greater burden for young college students (25).
Concerning the international students in South Korea, a study of psychological problems in Korea showed that the prevalence of anxiety and depression among them was 39.6 and 49%, respectively (9). The dire situation during COVID-19 exacerbated the difficult situation for Chinese international students studying in South Korea. They faced isolation and discrimination because China was the first country to experience a pandemic. They were unable to return home and faced many problems such as online classes, difficulty in buying masks, and psychological issues on foreign campuses (26). Higher severity of depression may lower university students' QoL (27). This aggravates their depressive condition.
Although living in the same country, the international students and local students may face different situations and confront different mental health problems during the pandemic (28). However, to date, no study has examined the difference between the Chinese international students' and local Korean students' knowledge, preventive practice, and depression in South Korea during the pandemic. Thus, this study aimed to investigate the differences between knowledge, preventive practice, and depression among Chinese international students and local Korean students in South Korea, and identify the determinants of depression among them to provide policy references on preventive measures.
Materials and Methods
Data and Sample
Sampling Method
An online cross-sectional survey was used to collect data through an anonymous questionnaire in South Korea (during the COVID-19 pandemic). A total of 570 questionnaires were collected by snowball sampling, including many universities in South Korea. From March 23 to April 8, 2020, 180 responses from Chinese students and from March 23 to April 22, 2020, 390 responses from South Korean students were collected. Since the subjects were university students, 37 students who positively answered the employment question were excluded, leaving 533 students (171 Chinese international students and 362 South Korean students in South Korea). All respondents expressed their willingness to participate and claimed to understand the research background and purpose.
Data Collection Procedure
First, the English version of the COVID-19 questionnaire used by Wang et al. (29) and colleagues was adopted. Second, the required sample size was calculated using the G*Power 3.19 program. Based on the parameters of a two-sided test and χ2 test, a residual variance of 0.83, α probability = 0.05, and power = 0.95 for F tests and linear multiple regression analysis, the minimum total sample size was estimated to be 356.
With limited access to respondents due to social distancing policies in South Korea during the COVID-19 pandemic, an online cross-sectional survey was conducted. Before conducting the survey, the content of the questionnaire was verified through an online pre-survey of 15–30 students, to ensure that the questions were understandable, and the statements were appropriate. Researchers examined the questionnaires' reliability and the simplicity of the responses. Potential respondents were sent a specific link to participate. In total, with the help of collaborators and native Korean speakers, the questionnaire was placed on the Naver Form Tool survey platform in South Korea.
Measurements
The questionnaire included two sections: (1) a questionnaire on COVID-19 and (2) the Patient Health Questionnaire-9 (PHQ-9). The first section comprised questions that covered (1) demographics and physical health data, (2) knowledge of COVID-19, and (3) preventive practices in the past 14 days.
Description of the Variables
General Demographics
In this study, to reflect on the participants' demographic characteristics, the basic survey asked respondents about their gender, age, education level, marital status, family size, health insurance, chronic diseases, traveling status in the past 14 days, isolation, COVID-19 symptoms, and their self-assessed physical condition. The choices for education level were undergraduate and graduate and for marital status were single and married. Family size was divided into one person, two people, three to five people, and six or more people. Questions about medical insurance, chronic disease, traveling, self-quarantine, and symptoms were answered with yes or no. Regarding self-assessed physical condition, respondents were asked to choose from four levels: poor, fair, good, or very good.
Knowledge of COVID-19
Assessed knowledge of COVID-19 included transmission route, attention to updated information, information sources, concern for COVID-19, satisfaction with the information, confidence in diagnosis, infection probability, probability of survival after infection, concern for family members, feelings of being discriminated against, purchase face masks, and additional information about COVID-19.
Preventive Practices of COVID-19
The questionnaire included nine basic preventive practices. The responses to these questions corresponded to the degree to which a measure was practiced daily (1 = never do this and 5 = do this every day). The total score indicates the extent to which preventive practices were performed. The reliability (Cronbach's α) of the preventive practices of the COVID-19 scale in this study was 0.71 and the validity was 0.76.
Patient Health Questionnaire-9
Depressive symptoms were diagnosed according to the nine criteria for depression in the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association (30). The options for each question in the PHQ-9 were (corresponding to the relative scores): not at all (0 points), occasionally (1 point), frequently (2 points), and almost every day (3 points). Respondents were divided into five groups according to their total score (31) (0–4, 5–9, 10–14, 15–19, and 20–27), corresponding to no depression, mild, moderate, moderately severe, and severe depression (32). The higher the score, the more severe the depression (33). The reliability of the PHQ-9 was 0.89, and its validity was 0.90 (34).
Statistical Analysis
In this study, SPSS 24.0 (IBM Corp., Armonk, NY, US) was used to conduct the statistical analysis, and p-values < 0.05 were regarded as statistically significant. First, descriptive statistics, t-test, and chi-squared test were performed to compare each variable between the Chinese international and local students in South Korea. Second, stepwise linear regression was used to explore the determinants of depression among two student groups.
Results
General Characteristics
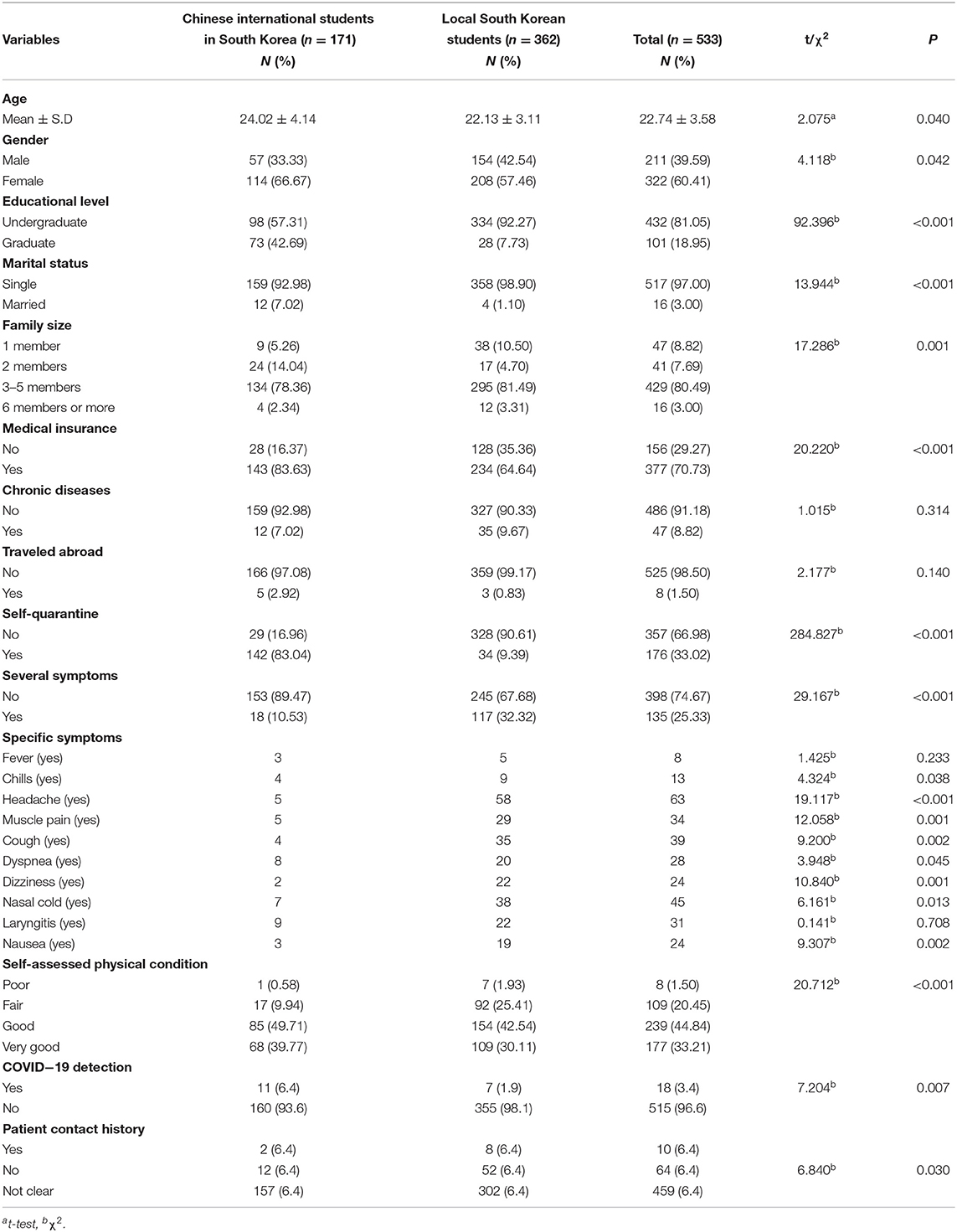
As shown in Table 1, there were significant differences between the two groups, regarding gender, age, educational level, marital status, family size, health insurance, self-quarantine, symptoms, and self-assessed physical condition. Among them, the female respondents were far higher than the male respondents, specifically, among the Chinese international students. The average age of Chinese international students was 24.02 ± 4.14 years, while that of local South Korean students was 22.13 ± 3.11 years. Moreover, the proportion of graduate students, married respondents, families with two people, and medical insurance of Chinese international students was higher. In contrast, most Chinese international students in South Korea (83.04%) have experienced self-isolation, while more than 90% of local respondents stated that they have not. Chinese international students showed better physical condition and fewer suspected symptoms (10.53%) than local students (32.32%).
Knowledge of COVID-19
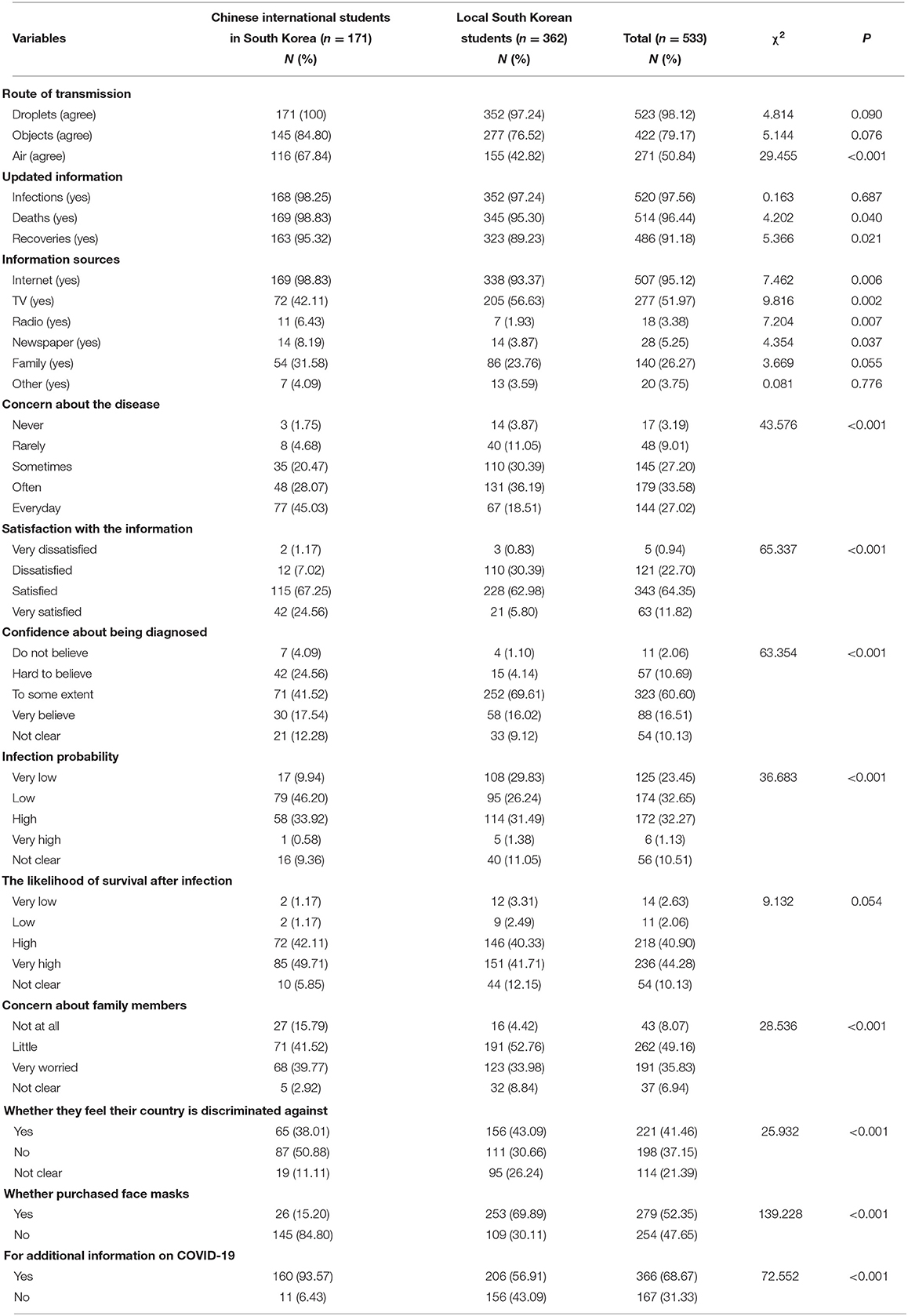
Table 2 shows the participants' knowledge of COVID-19, with about 98.12% knowing that the virus can be transmitted by droplets, 79.17% agreeing that transmission is possible through objects touched by the infected person, and only half (50.84%) agreeing that it can be transmitted through the air. Most students in both groups (more than 90%) were interested in the latest information on infections, cures, and deaths. Their main sources of information are the Internet, TV, and family, and they rarely get information from other channels.
Chinese international students showed high levels of concern about COVID-19, with 45% worrying about it daily. Among the local South Korean students, 30% were dissatisfied with the information currently provided, compared to <10% of Chinese international students. Some showed a degree of confidence about getting infected (41.52% for Chinese international and 69.61% for local students) and 30% of respondents in each group said they were very likely to be infected, but most also thought they had a good chance of survival. Some from the two groups were significantly worried about their families (39.77% for Chinese international and 33.98% for local students). Nearly half of the Chinese international students surveyed felt there was no discrimination regarding their country, compared to 30% of local South Korean students. As many as 85% of Chinese international students stated that they could not buy masks for reasons such as the lack of South Korea's national health insurance and the shortage. A small number of local students (30.11%) were unable to buy masks due to long queues and lack of availability.
Differences in the Type of Information They Want to Obtain
Figure 1 shows the types of information that Chinese international students and local students wanted to obtain. The former were eager to access more information. More than half of the Chinese international students wanted to know specific details of symptoms, advice on prevention, up-to-date information, the number of people and places diagnosed, and the school's prevention code. The top five types of information in demand among local Korean students were up-to-date information, specific details of symptoms, availability, and effectiveness of vaccines/drugs, number of people and places infected, and prevention advice.
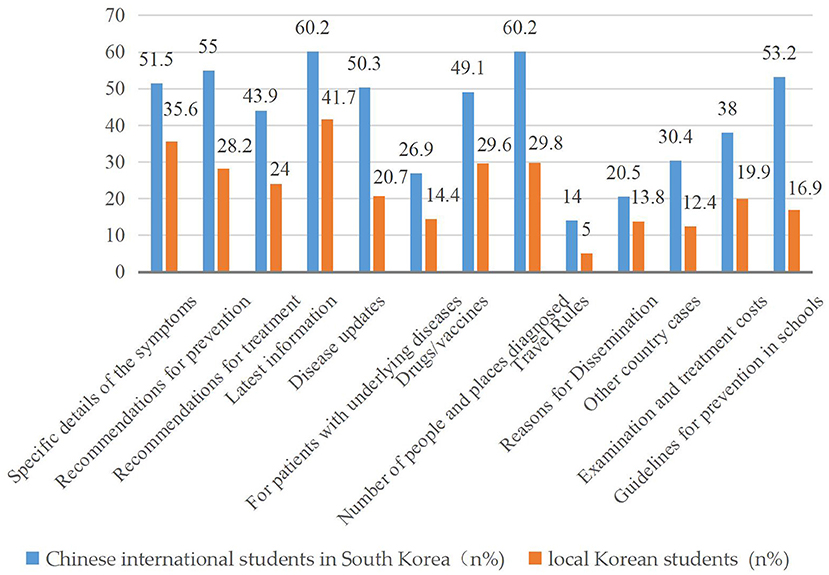
Figure 1. Type of information expected between Chinese international students and local Korean students in South Korea.
Differences in Preventive Practices Between the Two Groups
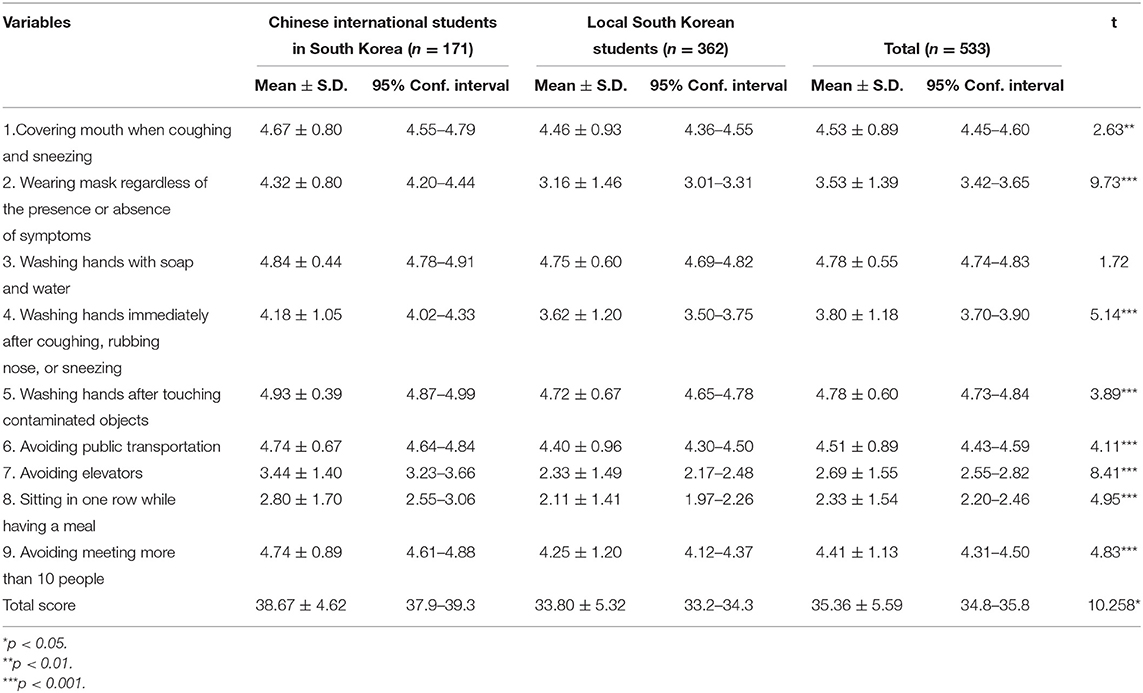
Table 3 shows the preventive practices of Chinese international students and local Korean students in South Korea. The average total score of the Chinese international students (38.67%) was slightly higher than that of local Korean students (33.80%). There were statistically significant differences regarding the eight preventive behaviors between the two groups. This included when coughing and sneezing, wearing masks regardless of the presence or absence of symptoms, washing hands immediately after coughing, rubbing the nose, sneezing, washing hands after touching contaminated objects, avoiding public transportation, avoiding elevators, sitting in one row while having a meal, and avoiding meeting more than 10 people.
Results and Analysis of Depressive Conditions
A chi-square test was used to determine the difference in the level of depressive symptoms between Chinese international students and local Korean students (Table 4). In this study, depressive symptoms were classified as 0–4 (no depression), 5–9 (mild depression), 10–14 (moderate depression), 15–19 (moderate to severe depression), and 20–27 (severe depression). As shown in Table 4, the differences between the two groups were statistically significant (χ2= 11.224, p < 0.05), and Chinese international students were slightly more depressed.
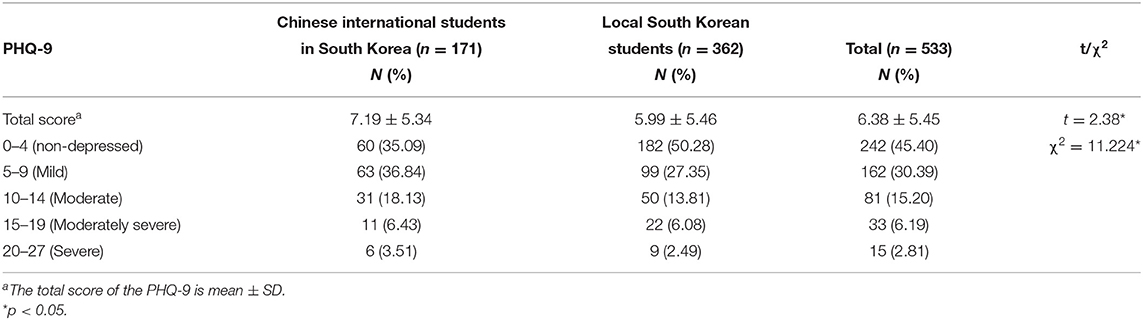
Table 4. Difference in depressive symptoms between the Chinese international students and local Korean students.
Linear stepwise regression was used to explore the factors affecting the depressive status of the Chinese international students (Table 5) and the local South Korean students (Table 6), separately. P-values < 0.05 were regarded as statistically significant. All variables that were statistically significant in Tables 1–3 were all included in Tables 5, 6. These included age, gender, education, marital status, family size, health insurance, self-isolation, general symptoms and specific symptoms, self-assessed physical health status, means of transmission, updated information, information sources (Internet, TV, radio, newspapers, family), level of satisfaction with information, COVID-19 testing, patient contact history, confidence in confirmed diagnosis, probability of infection and surviving infection, level of concern about family members, discrimination, mask purchase, additional information, and eight preventive measures. The results in Table 5 showed that among Chinese international students, perceived discrimination in their country, probability of survival after infection, cough symptoms, and satisfaction with information were statistically significantly related to respondents' depression. Regarding the local South Korean students, the results in Table 6 illustrated that gender, education level, family size, self-assessed physical health status, symptoms of nausea and dyspnea, nucleic acid testing, history of patient exposure, and receipt of outbreak-related information from family members and the Internet were statistically significantly related to respondents' depression.
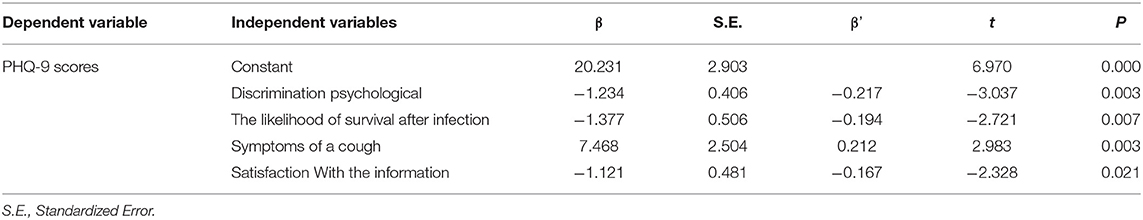
Table 5. Stepwise regression analysis of the factors of depression due to COVID-19 among Chinese international students in South Korea.
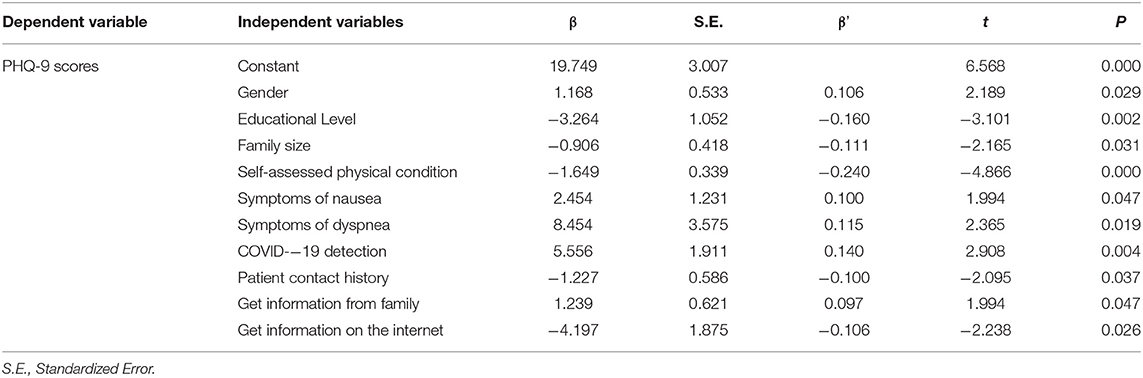
Table 6. Stepwise regression analysis of the factors of depression due to COVID-19 among local South Korean students.
Discussion
Principal Findings and Comparison With Other Studies
This study used univariate and multiple linear regression analyses to clarify the relationship between knowledge, preventive practices, and depression among Chinese international students and local Korean students in South Korea. The results revealed that the determinants of depression affecting the two groups were different. Targeted measures should be taken to reduce depression.
Demographic Characteristics of Chinese International Students and Local South Korean Students
Most international students in the sample reported having insurance, However, it was international student insurance rather than South Korean national health insurance. This resulted in Chinese international students in South Korea being unable to buy masks at the beginning of the outbreak due to the restrictions of the national health insurance (35). Most of them in the sample were self-isolated, while the vast majority of local South Korean students did not experience self-isolation. This is because South Korea is a narrow and densely populated country, and the government did not take measures (36) for widespread self-isolation of the population in the early stages of the COVID-19 pandemic but only isolated and treated confirmed patients. The self-assessed physical health of the local South Korean students in the sample was less favorable overall, consistent with the findings of Sun Jung Kim's study (37), which found that Chinese students in South Korea had a high level of self-assessed health and cultural adaptation.
Knowledge and Preventive Practice of Chinese International Students and Local South Korean Students
In this study, both student groups were concerned about COVID-19 and showed a good level of knowledge, which is consistent with the results of other studies (38, 39). The Internet is the main information source, and they are satisfied with the information currently provided. This is because the central and local public health authorities in South Korea provide daily updates of all laboratory-confirmed COVID-19 cases on their web pages including information on the number of national and local cases, age, sex, symptoms, date of onset of symptoms, source, date of exposure, and location of the infection (within or outside Korea) (40). Chinese international students generally perceive themselves as having a low probability of being infected, which is also linked to the widespread self-isolation of international students (4). The local students believe that the higher probability of infection is related to the surge in the number of infections in Korea at the beginning of the pandemic (41). Chinese students have significantly better preventive practice behaviors, specifically, Chinese international students are particularly better at wearing masks and washing their hands, which also suggests that they were more afraid of being infected and more vulnerable to the effects of the pandemic (42).
Differences in Depression Between Chinese International Students and Local South Korean Students
Depression rates were fairly high for both student groups, since the Chinese international students in South Korea have a higher rate (18.13%) of moderate depression than local students (13.81%), and a slightly higher rate (3.51%) of severe depression than local students (2.49%). This result is consistent with many local South Korean studies. Jimhee's survey showed that the prevalence of depression among the general population of Korea at the beginning of the pandemic was 19%(43), Lee's study on adolescents in Daegu, South Korea, during the COVID-19 pandemic showed that 19.8% and 12.3% of students experienced depression and anxiety, respectively (44), Hoo's study of adults aged 20 to 49 in Chungnam Province, South Korea, during the COVID-19 pandemic found that 18.8% of participants had symptoms of depression (45). In Kim's study of 180 nurses during the pandemic, 30.6% had moderate or higher levels of depression (46). Kim and Lee's study found that depression's prevalence diagnosed in South Korea in 2016 was 3%, with a slightly higher prevalence among males (3.1%) than females (2.9%) among those aged 18–29 years (47), indicating the pandemic may increase the prevalence of the depression.
Satisfaction with information was associated with depression among Chinese international students in South Korea in this sample. Specifically, students who showed higher satisfaction were less likely to be depressed. This also confirmed the importance of the provision of accurate and truthful information by the government during a pandemic. Kim's research during the Korean pandemic indicated that useful information related to COVID-19 could help prevent infection as well as promote anxiety and fear, leading to negative behavior (47). Another factor that influenced depression among the Chinese international students in the sample was the likelihood of survival after infection. This is clear proof that international students are significantly worried about the pandemic (38). The feeling of being discriminated against was a predictor of depression among Chinese international students. This was consistent with the findings of a study by Li on Chinese and American students, who noted that the former live in fear of discrimination in the US, which significantly affected their emotions and self-esteem (48). Therefore, greater attention should be paid to international students' mental health to help them build self-esteem and self-confidence.
For the local South Korean students in the sample, gender and education level were predictors of depression. This was consistent with the findings of Won, who found higher rates of depression among women in a South Korean community survey (49). Self-assessed physical health status was associated with depression among local South Korean students. The result was similar to the findings of an online survey on 400 South Korean people conducted by Hye during the pandemic from March to June 2020, which found a statistically significant association between mental and physical health (25). Another noteworthy factor affecting depression among local South Korean students was the information source, mainly the Internet. South Korea had done a good job of disclosing all information about COVID-19 to the public openly and transparently, holding detailed press conferences twice a day since the first COVID-19 case was diagnosed, and full disclosure promotes public trust and support for the government (50). Alwin noted that the South Korean government's transparency in sharing information about the main features of the outbreak and the standard procedures to be followed helped to combat the spread of rumors related to the outbreak (51). Information from families and family size could influence depression among local South Korean students, indicating the importance in their minds (52). Finally, nucleic acid testing and patient exposure history were correlated with depression among local South Korean students, which showed the importance of correct disclosure of information about COVID-19 (53).
Finally, there are two factors to be concerned about. First, the result showed that symptoms affected the depression among local South Korean and Chinese international students in South Korea. Symptoms of COVID-19 vary across patients, but the most common clinical symptoms include fever, malaise, cough, sputum, and shortness of breath at all stages of the disease, along with less common symptoms such as sore throat, headache, confusion, hemoptysis, shortness of breath and chest tightness. Moreover, minor symptoms include nausea, vomiting, diarrhea, and gastrointestinal complications. Therefore, it is difficult to identify the suspected COVID-19 symptoms because they are diverse, and for university students, the presence of a symptom adds to their psychological burden (54). Second, this study could not directly prove that personal precautions (wearing masks, washing hands regularly, and so on) would affect depression in both student groups. Christoph's findings also indicated that there is little evidence that public health measures were associated with direct mental health impairment (55). Wendy's research at American University also found that students' perceptions of wearing masks varied (56). While one study in Hong Kong concluded that the insecurity associated with wearing and reusing masks could increase the participants' psychological burden (57). A study conducted in mainland China among children and adolescents revealed that the frequency of wearing a mask and the duration of exercise were associated with mental health (58).
Implications
The South Korean government is supposed to continue its efforts and support student development during the outbreak. For the international students in South Korea, first, as a large group, the government should remove the restriction on buying masks from national insurance. Second, transparent, open, and truthful information should be provided to international students. Third, attention should be paid to international students' mental health, providing them warmth and care in a timely manner so that they can build their self-esteem and self-confidence. Fourth, psychiatrists could use telemedicine for psychotherapy and the continuation of interpersonal therapy (59). Regarding local South Korean students, first, the government should pay attention to the mental health status of university students of different genders and educational levels. Second, measures to lower the history of outside contact should be undertaken. Third, attention should be paid to physical health and improving university students' physical fitness in South Korea. Fourth, the family's role in preventing infection and caring for patients should not be overlooked. Fifth, the Internet should be used as a positive guide to deliver accurate information. Finally, the testing speed of COVID-19 should be accelerated. Clinicians should use the sequential model which integrates psychotherapy and pharmacotherapy to prevent the recurrence of depression (60).
Limitations and Future Research
This study had several limitations. First, it was conducted online, which may cause issues such as the uncertainty of the respondents' attitude and seriousness when completing it. Moreover, the self-assessed physical health status may not be the same as the one judged by professionals. Second, this study used snowball sampling and the sample size is not huge. Hence, the sample may not be representative of the general population. Third, the study would be more accurate if the comparison was between similar populations, with the only difference being nationality. It would be more informative to include the questionnaire used to assess the general demographics, knowledge of COVID-19, and preventive practices. Fourth, anxiety was not measured and anxiety level should be considered as a potential confounding variable in future studies. Besides, this study did not assess the factors that are associated with depression among university students such as the frustration due to loss of daily life and study interruptions, pre-existing depression, anxiety, and social support (61). Despite these limitations, this study provides useful information on the knowledge, prevention practices, and depression status of Chinese international and local Korean students in South Korea who experienced the most severe moments of the COVID-19 outbreak. It could serve as an evidence-based reference for providing psychological help to local and international students during the pandemic of infectious diseases.
Conclusions
This study investigated the conditions and determinants of knowledge, preventive behaviors, and depression among Chinese international and local students living in South Korea during the early stage of COVID-19 pandemic. The results revealed that both student groups had good knowledge of COVID-19. Chinese international students had better preventive practice and showed higher levels of depression. Information satisfaction, the likelihood of survival after infection, symptoms of a cough, and feelings of discrimination were the determinants of depression among Chinese international students. Gender, educational level, family, suspected symptoms, self-assessed physical health status, COVID-19 detection, population contact history, and online sources of information were the determinants of the local students. The data may serve as a preliminary study on lowering the negative impact of COVID-19 on the mental health of the international and native students in a country and can be used as a guide for further studies in different regions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Chair, Yonsei University Mirae Institutional Review Board. Affiliation: College of Health Sciences/Health Administration. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conceptualization: EN and BZ. Methodology, software, and data curation: BZ. Validation: FK, EN, and BZ. Formal analysis and writing—original draft preparation: XJ. Investigation and resources: FK and BZ. Writing—review and editing and supervision: FK and EN. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported and funded by the National Natural Science Foundation of China (No. 71804094), China Postdoctoral Science Foundation (No. 2016M592161).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank all respondents for their participation in this research and the researchers from the Yonsei Global Health Center for their cooperation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.920887/full#supplementary-material
References
1. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
2. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
3. Jeong SJ, Chung WS, Sohn Y, Hyun JH, Baek YJ, Cho Y, et al. Clinical characteristics and online mental health care of asymptomatic or mildly symptomatic patients with coronavirus disease 2019. PLoS ONE. (2020) 15:e0242130. doi: 10.1371/journal.pone.0242130
4. Zhao B, Kong F, Aung MN, Yuasa M, Nam EW. Novel coronavirus (COVID-19) knowledge, precaution practice, and associated depression symptoms among University Students in Korea, China, and Japan. Int J Environ Res Public Health. (2020) 17:6671. doi: 10.3390/ijerph17186671
5. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. (2021) 19:141–54. doi: 10.1038/s41579-020-00459-7
6. Nwagbara UI, Osual EC, Chireshe R, Bolarinwa OA, Saeed BQ, Khuzwayo N, et al. Knowledge, attitude, perception, and preventative practices towards COVID-19 in sub-Saharan Africa: a scoping review. PLoS ONE. (2021) 16:e0249853. doi: 10.1371/journal.pone.0249853
7. Lee T, Kwon HD, Lee J. The effect of control measures on COVID-19 transmission in South Korea. PLoS One. (2021) 16:e0249262. doi: 10.1371/journal.pone.0249262
8. Kim SW, Park IH, Kim M, Park AL, Jhon M, Kim JW, et al. Risk and protective factors of depression in the general population during the COVID-19 epidemic in Korea. BMC Psychiatry. (2021) 21:445. doi: 10.1186/s12888-021-03449-y
9. Kim IH, Jeong YW, Park HK, Kim IH, Jeong YW, Park HK. Korean University students' problematic alcohol use, depression, and non-suicidal self-injury during COVID-19 lockdown. Chronic Stress. (2021) 5:24705470211053042. doi: 10.1177/24705470211053042
10. Jung SJ, Jeon YJ, Yang JS, Park M, Kim K, Chibnik LB, et al. Impact of COVID-19 on mental health according to prior depression status: A mental health survey of community prospective cohort data. J Psychosom Res. (2021) 148:110552. doi: 10.1016/j.jpsychores.2021.110552
11. Wang Q, Mo PKH, Song B, Di JL, Zhou FR, Zhao J, et al. Mental health and preventive behavior of pregnant women in China during the early phase of the COVID-19 period. Infect Dis Poverty. (2020) 10:37. doi: 10.1186/s40249-021-00825-4
12. Aydin F, Kaya F. Does compliance with the preventive health behaviours against COVID-19 mitigate the effects of depression, anxiety and stress? (Cumplir con los comportamientos preventivos de salud contra el COVID-19 reduce los efectos de la depresion, la ansiedad y el estres?). Stud Psychol. (2021) 42:652–76. doi: 10.1080/02109395.2021.1950462
13. Bahar Moni AS, Abdullah S, Bin Abdullah MFIL, Kabir MS, Alif SM, Sultana F, et al. Psychological distress, fear and coping among Malaysians during the COVID-19 pandemic. PLoS One. (2021) 16:e0257304. doi: 10.1371/journal.pone.0257304
14. Woon LS, Sidi H, Nik Jaafar NR, Leong Bin Abdullah MFI. Mental Health Status of University healthcare workers during the COVID-19 pandemic: a post-movement lockdown assessment. Int J Environ Res Public Health. (2020) 17:9155. doi: 10.3390/ijerph17249155
15. Leong Bin Abdullah MFI, Ahmad Yusof H, Mohd Shariff N, Hami R, Nisman NF, Law KS. Depression and anxiety in the Malaysian urban population and their association with demographic characteristics, quality of life, and the emergence of the COVID-19 pandemic. Curr Psychol. (2021) 40:6259–70. doi: 10.1007/s12144-021-01492-2
16. Brailovskaia J, Margraf J, Schneider S. Social media as source of information, stress symptoms, and burden caused by coronavirus (COVID-19) a cross-national investigation of predictors. European Psychologist. (2021) 26:373–86. doi: 10.1027/1016-9040/a000452
17. Mansueto G, Lopes FL, Grassi L, Cosci F. Impact of COVID-19 outbreak on Italian healthcare workers versus general population: results from an online survey. Clin Psychol Psychother. (2021) 28:1334–45. doi: 10.1002/cpp.2644
18. Zhang XR, Huang QM, Wang XM, Cheng X, Li ZH, Wang ZH, et al. Prevalence of anxiety and depression symptoms, and association with epidemic-related factors during the epidemic period of COVID-19 among 123,768 workers in China: a large cross-sectional study. J Affect Disord. (2020) 277:495–502. doi: 10.1016/j.jad.2020.08.041
19. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. (2020) 395:945–7. doi: 10.1016/S0140-6736(20)30547-X
20. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. (2020) 7:389–90. doi: 10.1016/S2215-0366(20)30141-3
21. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
22. Lima Y, Denerel N, Öz ND, Senisik S. The psychological impact of COVID-19 infection on athletes: example of professional male football players. Sci Med Footb. (2021) 5:53–61. doi: 10.1080/24733938.2021.1933156
23. Ryu S, Ali ST, Lim JS, Chun BC. Estimation of the excess COVID-19 cases in Seoul, South Korea by the students arriving from China. Int J Environ Res Public Health. (2020) 17:3113. doi: 10.3390/ijerph17093113
24. Lin J, Guo T, Becker B, Yu Q, Chen ST, Brendon S, et al. Depression is associated with moderate-intensity physical activity among college students during the COVID-19 pandemic: differs by activity level, gender and gender role. Psychol Res Behav Manag. (2020) 13:1123–34. doi: 10.2147/PRBM.S277435
25. Lee HS, Dean D, Baxter T, Griffith T, Park S. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. (2021) 295:113570. doi: 10.1016/j.psychres.2020.113570
26. Chen Y, Liu Y, Zhang Y, Li Z, Zhou T. The effect of fear of the COVID-19 on depression among Chinese outbound students studying online in China amid the COVID-19 pandemic period: the role of resilience and social support. Front Psychol. (2021) 12:750011. doi: 10.3389/fpsyg.2021.750011
27. Leong Bin Abdullah M, Mansor NS, Mohamad MA, Teoh SH. Quality of life and associated factors among university students during the COVID-19 pandemic: a cross-sectional study. BMJ Open. (2021) 11:e048446. doi: 10.1136/bmjopen-2020-048446
28. Alam MD, Lu J, Ni L, Hu S, Xu Y. Psychological outcomes and associated factors among the international students living in China during the COVID-19 pandemic. Front Psychiatry. (2021) 12:707342. doi: 10.3389/fpsyt.2021.707342
29. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial Stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
30. Stafford L, Berk M, Jackson HJ. Validity of the hospital anxiety and depression scale and patient health questionnaire-9 to screen for depression in patients with coronary artery disease. Gen Hosp Psychiatry. (2007) 29:417–24. doi: 10.1016/j.genhosppsych.2007.06.005
31. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
32. Maroufizadeh S, Omani-Samani R, Almasi-Hashiani A, Amini P, Sepidarkish M. The reliability and validity of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with infertility. Reprod Health. (2019) 16:137. doi: 10.1186/s12978-019-0802-x
33. Sun Y, Fu Z, Bo Q, Mao Z, Ma X, Wang C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. (2020) 20:474. doi: 10.1186/s12888-020-02885-6
34. Kim K, Yang J, Jeon YJ, Lee YJ, Lee Y, Kim HC, et al. The effect of information-seeking behaviours on prevention behaviour implementation during the COVID-19 pandemic: mediating effects of anxiety and fear. Epidemiol Health. (2021) 43:e2021085. doi: 10.4178/epih.e2021085
35. Yu S, Kim S, Kang J. Face mask policies in South Korea in response to COVID-19. Asia Pac J Public health. (2020) 32:497–9. doi: 10.1177/1010539520951397
36. Chang MC, Baek JH, Park D. Lessons from South Korea regarding the early stage of the COVID-19 outbreak. Healthcare. (2020) 8:229. doi: 10.3390/healthcare8030229
37. Kim SJ, Yoo IY. Health promotion behavior of Chinese international students in Korea including acculturation factors: a structural equation model. Asian Nurs Res. (2016) 10:25–31. doi: 10.1016/j.anr.2015.10.008
38. Lee YH, Ha J, Park H. Volunteering and social engagement of medical students in South Korea during the COVID-19 pandemic. Korean J Med Educ. (2021) 33:441–4. doi: 10.3946/kjme.2021.212
39. Hong J, Jung I, Park M, Kim K, Yeo S, Lee J, et al. Attitude of medical students about their role and social accountability in the COVID-19 pandemic. Front Psychiatry. (2021) 12:645340. doi: 10.3389/fpsyt.2021.645340
40. Ryu S, Ali ST, Noh E, Kim D, Lau E, Cowling BJ. Transmission dynamics and control of two epidemic waves of SARS-CoV-2 in South Korea. BMC Infect Dis. (2021) 21:485. doi: 10.1186/s12879-021-06204-6
41. Kim YJ, Cho JH, Kim ES. Differences in sense of belonging, pride, and mental health in the daegu metropolitan region due to COVID-19: comparison between the presence and absence of national disaster relief fund. Int J Environ Res Public Health. (2020) 17:4910. doi: 10.3390/ijerph17134910
42. Fujii R, Suzuki K, Niimi J. Public perceptions, individual characteristics, and preventive behaviors for COVID-19 in six countries: a cross-sectional study. Environ Health Prev Med. (2021) 26:29. doi: 10.1186/s12199-021-00952-2
43. Kim YE, Lee B. The psychometric properties of the patient health questionnaire-9 in a sample of Korean University students. Psychiatry Investig. (2019) 16:904–10. doi: 10.30773/pi.2019.0226
44. Hyun J, Kim S, Kim H, Choi YJ, Choi YK, Lee YR, et al. COVID-19 and risk factors of anxiety and depression in South Korea. Psychiatry Investig. (2021) 18:801–8. doi: 10.30773/pi.2021.0125
45. Lee H, Noh Y, Seo JY, Park SH, Kim MH, Won S. Impact of the COVID-19 pandemic on the mental health of adolescent students in Daegu, Korea. J Korean Med Sci. (2021) 36:e321. doi: 10.3346/jkms.2021.36.e321
46. Lee HY, Choi D, Lee JJ. Depression, anxiety, and stress in South Korea general population during the COVID-19 pandemic. Epidemiol Health. (2022) 44:e2022018. doi: 10.4178/epih.e2022018
47. Kim MY, Yang YY. Mental health status and its influencing factors: the case of nurses working in COVID-19 hospitals in South Korea. Int J Environ Res Public Health. (2021) 18:6531. doi: 10.3390/ijerph18126531
48. Li M, Sun W, Wang Y, Qi C. Prevalence and differences of depression, anxiety, and substance use between chinese college-age students studying in China and America during the coronavirus disease 2019 pandemic. Front Psychiatry. (2022) 13:805120. doi: 10.3389/fpsyt.2022.805120
49. Cha WT, Joo HJ, Park YS, Park EC, Kim SY. Depression before and during-COVID-19 by gender in the Korean Population. Int J Environ Res Public Health. (2022) 19:3477. doi: 10.3390/ijerph19063477
50. Lee D, Heo K, Seo Y. COVID-19 in South Korea: Lessons for developing countries. World Dev. (2020) 135:105057. doi: 10.1016/j.worlddev.2020.105057
51. Issac A, Stephen S, Jacob J, Vr V, Radhakrishnan RV, Krishnan N, et al. The pandemic league of COVID-19: Korea versus the United States, with lessons for the entire world. J Prev Med Public Health. (2020) 53:228–32. doi: 10.3961/jpmph.20.166
52. Park JY, Pardosi JF, Seale H. Examining the inclusion of patients and their family members in infection prevention and control policies and guidelines across Bangladesh, Indonesia, and South Korea. Am J Infect Control. (2020) 48:599–608. doi: 10.1016/j.ajic.2019.10.001
53. Hong KH, Lee SW, Kim TS, Huh HJ, Lee J, Kim SY, et al. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med. (2020) 40:351–60. doi: 10.3343/alm.2020.40.5.351
54. Majumder J, Minko T. Recent developments on therapeutic and diagnostic approaches for COVID-19. AAPS J. (2021) 23:14. doi: 10.1208/s12248-020-00532-2
55. Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
56. Birmingham WC, Wadsworth LL, Lassetter JH, Graff TC, Lauren E, Hung M. COVID-19 lockdown: Impact on college students' lives. J Am Coll Health. (2021) 1–15. doi: 10.1080/07448481.2021.1909041
57. Bressington DT, Cheung T, Lam SC, Suen L, Fong T, Ho H, et al. Association between depression, health beliefs, and face mask use during the COVID-19 pandemic. Front Psychiatry. (2020) 11:571179. doi: 10.3389/fpsyt.2020.571179
58. Qin Z, Shi L, Xue Y, Lin H, Zhang J, Liang P, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. (2021) 4:e2035487. doi: 10.1001/jamanetworkopen.2020.35487
59. Cosci F, Mansueto G, Fava GA. Relapse prevention in recurrent major depressive disorder. A comparison of different treatment options based on clinical experience and a critical review of the literature. Int J Psychiatry Clin Pract. (2020) 24:341–8. doi: 10.1080/13651501.2020.1779308
60. Cosci F, Guidi J, Mansueto G, Fava GA. Psychotherapy in recurrent depression: efficacy, pitfalls, and recommendations. Expert Rev Neurother. (2020) 20:1169–75. doi: 10.1080/14737175.2020.1804870
61. Woon LS, Leong Bin Abdullah MFI, Sidi H, Mansor NS, Nik Jaafar NR. Depression, anxiety, and the COVID-19 pandemic: Severity of symptoms and associated factors among university students after the end of the movement lockdown. PLoS ONE. (2021) 16:e0252481.0252481. doi: 10.1371/journal.pone.0252481
Keywords: depression, preventive practices, PHQ-9, Chinese international students, South Korea, COVID-19
Citation: Jiang X, Zhao B, Nam EW and Kong F (2022) Assessing Knowledge, Preventive Practices, and Depression Among Chinese International Students and Local Korean Students in South Korea During the COVID-19 Pandemic: An Online Cross-Sectional Study. Front. Psychiatry 13:920887. doi: 10.3389/fpsyt.2022.920887
Received: 15 April 2022; Accepted: 31 May 2022;
Published: 21 June 2022.
Edited by:
Haibo Yang, Tianjin Normal University, ChinaReviewed by:
Giovanni Mansueto, University of Florence, ItalyJuan Moisés De La Serna, Universidad Internacional de la Rioja, Spain
Mohammad Farris Iman Leong Bin Abdullah, Universiti Sains Malaysia (USM), Malaysia
Copyright © 2022 Jiang, Zhao, Nam and Kong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eun Woo Nam, ZXduYW0mI3gwMDA0MDt5b25zZWkuYWMua3I=; Fanlei Kong, a29uZ2ZhbmxlaSYjeDAwMDQwO3NkdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Xiaoxu Jiang
Xiaoxu Jiang Bo Zhao
Bo Zhao Eun Woo Nam
Eun Woo Nam Fanlei Kong
Fanlei Kong