- 1Section of Psychiatry, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Genoa, Italy
- 2Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Ospedale Policlinico San Martino, Genoa, Italy
- 3Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy
- 4Department of Psychiatry, Faculty of Medicine, University of Geneva (UNIGE), Geneva, Switzerland
- 5Faculty of Biomedical Sciences, Università della Svizzera Italiana (USI), Lugano, Switzerland
Introduction: Patients with bipolar disorder (BD) often show comorbidity with substance use disorder (SUD) with a negative impact on clinical course, prognosis, and functioning. The role of polysubstance use disorder (polySUD) is understudied. The aim of the present paper is to evaluate the sociodemographic and clinical characteristics associated with BD and comorbid SUD, focusing on polySUD, in order to phenotype this specific group of patients and implement adequate treatment and prevention strategies.
Methods: A cross-sectional study was conducted involving 556 patients with a primary diagnosis of BD (376 without SUD, 101 with SUD, and 79 with polySUD). A semi-structured interview was administered to collect sociodemographic variables, clinical characteristics, and pharmacological treatment. ANOVA and chi-square tests were used to compare the three groups. Significantly different variables were then inserted in multivariate logistic regression.
Results: Patients affected by BD and polySUD were younger, and more frequently males and single, than patients with SUD or without SUD. Indeed, the prevalence of patients affected by BD and polySUD living in residential facilities was higher than in the other groups. Moreover, earlier age at onset, higher prevalence of psychotic and residual symptoms, involuntary hospitalization, and a family history of psychiatric disorders were associated with polySUD in patients suffering from BD. Lastly, patients with BD and polySUD were more likely to take four or more medications, particularly benzodiazepines and other drugs. At the multinomial regression, younger age, male gender, early age at onset, psychotic and residual symptoms, positive family history of psychiatric disorders, and use of benzodiazepines remained significantly associated with polySUD in patients with BD.
Conclusion: Our findings show a specific profile of patients with BD and polySUD. It is important to conduct research on this topic in order to adopt specific therapeutic strategies, minimize the use of polypharmacy, and aim at full remission and mood stabilization.
Introduction
Bipolar disorder (BD) is a severe, recurrent, and multifactorial psychiatric condition, characterized by the alternation of different phases, specifically hypomanic/manic and major depressive episodes (1). BD affects at least 2–3% of the general population and its onset typically occurs during adolescence or early adulthood (2), influenced often by seasonality and sunlight (3, 4). BD is often associated with several medical conditions, such as cardiovascular and endocrine-metabolic diseases (5–10) and higher inflammatory status (11, 12), leading to a worsening of the quality of life and functioning (13).
Substance use disorder (SUD), which is defined by the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) criteria as “a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems” (1), is a common issue in patients with BD. It has a negative impact on the illness course, including more difficulties to achieve intraepisodic remission and stabilization and maintaining adequate and full adherence to therapeutic strategies (14, 15).
The comorbidity between BD and SUD is frequent, as confirmed by several epidemiological studies. For example, the Epidemiologic Catchment Area (ECA) study found a higher prevalence of substance abuse in subjects diagnosed with BD type I (40.7%) than in the general population (16). In the National Epidemiologic Survey on Alcohol and Related Conditions (NERSAC) studies, patients with BD showed high rates of SUD (17–20), as well as in other epidemiological studies, with a prevalence ranging from 26 to 43% (21–23). In general, patients with BD tend to use illicit substances with a strong statistical association [odds ratio (OR): 4.96] with the following prevalence: alcohol (42%), cannabis (20%), and cocaine and amphetamine (17%) (24). However, the use of novel psychoactive substances has been also associated with young patients with BD more than controls and subjects with other psychiatric disorders (25, 26).
The reasons why patients with BD use illicit substances are different, including seeking relief by self-medication, improving psychic status, relieving tension and boredom, escaping from reality, achieving and/or maintaining elevated mood, and increasing energy (27). Furthermore, common genetic (i.e., polymorphism of the aldehyde hydrogenase and alcohol dehydrogenase, or 5HT2C gene), socioeconomic, and environmental factors (i.e., access and availability of illicit drugs in the community, poverty), stressful events (i.e., trauma, physical, and sexual abuse), temperamental traits (i.e., a sensation of seeking behavior), lifetime suicide attempts, and psychiatric comorbidities (i.e., conduct disorder, cluster B personality disorder, and post-traumatic stress disorder) have been associated with SUD in patients with BD (24, 28, 29).
The comorbidity between BD and SUD is associated with several detrimental clinical characteristics, such as an earlier onset of illness, greater severity of the disorder, more rapid cycling with a higher risk of switching into (hypo)manic or mixed phases and frequent affective relapses, increased risk of suicide attempts or suicide, and accelerated progression of BD with higher prevalence of negative and cognitive symptomatology. Furthermore, patients affected by BD and SUD are characterized by treatment delay due to possible misdiagnosis, reduced response to lithium and other pharmacological treatments with worsening of adherence, presence of medical comorbidities (hepatitis C, acquired immune deficiency syndrome, and others), increased psychosocial problems, and poorer social support (27, 28, 30). Finally, illicit substances, particularly cannabis, are considered risk factors for the onset of BD (31, 32).
Although previous studies have recognized the negative impact of concurrent SUD in patients with BD, to the best of our knowledge, no studies have specifically focused on the factors associated with BD and polysubstance use disorder (polySUD). The present study aimed to evaluate the sociodemographic and clinical characteristics associated with BD and comorbid SUD, focusing specifically on polySUD. In fact, a detailed characterization of the phenotype of patients with BD and polySUD may help the identification and prevention of risk factors for multidrug abuse. This may in turn improve the clinical course and outcomes of BD and may help the building of a meaningful therapeutic relationship and the choice of the most effective treatments (28).
Materials and Methods
Sample and Assessment
A cross-sectional study was conducted involving 556 patients with a primary diagnosis of BD, consecutively admitted to the Section of Psychiatry, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), IRCCS Ospedale Policlinico San Martino, University of Genoa (Italy), during a period of 5 years (January 2017–December 2021).
The inclusion criteria consisted of the following: (a) inpatient status; (b) ongoing major depressive or (hypo)manic episode into a primary diagnosis of BD type I and II, according to the DSM-5 criteria (1); (c) 18 years of age or older; and (d) written informed consent to participate in the study.
The exclusion criteria were as follows: (a) primary diagnosis of schizophrenia and related disorders; (b) pregnancy or recent childbirth; (c) any condition affecting the ability to fill out the assessment, such as major neurocognitive disorders; (d) any severe neurological disorder or positive history of acute neurological injury, including an intellectual disability; and (e) the inability or refusal to provide written informed consent to participate in the study.
A semi-structured interview was administered to collect both sociodemographic and clinical characteristics. Sociodemographic characteristics included age, gender, marital and working status, education level in years, and living status, while the clinical characteristics included family history for psychiatric disorders, age of BD onset, duration of illness, presence of lifetime involuntary hospitalization, psychotic and residual symptoms, suicide attempts and non-suicidal self-injury (NSSI), lifetime SUD, and pharmacological treatment grouped as antidepressants, antipsychotics, mood stabilizers (i.e., lithium, valproate, lamotrigine, and carbamazepine), benzodiazepines, and others (i.e., gabapentin, pregabalin, and oxcarbazepine). Moreover, according to the existing literature, the presence of at least two or four medications was defined as polypharmacy simplex and complex, respectively (33).
Potential participants were provided with an in-depth explanation of the study objectives and procedures and an opportunity to ask questions. The study was designed in agreement with the guidelines from the Declaration of Helsinki (34) and was approved by the Research Ethical Committees.
Statistical Analysis
Continuous and categorical variables were presented as means and standard deviations (SD) or frequency and percentage, respectively.
First, the sample was divided into three subgroups: (a) patients with BD and absence of lifetime SUD; (b) patients with BD and lifetime SUD (use of one illicit drug); and (c) patients with BD and polySUD (at least two concomitant illicit drugs). For the sociodemographic and clinical comparison, ANOVA with Bonferroni’s post hoc correction was used for continuous variables and Pearson’s chi-square test (χ2) for categorical variables. Subsequently, a multinomial regression analysis was used to explore the relationship between patients with BD and polySUD and each of the significant independent variables found in univariate analysis, correcting for age and gender.
The Statistical Package for Social Sciences (SPSS) for Windows 25.0 (IBM Corp., Armonk, NY, United States) was used to carry out all the mentioned statistical analyses, and the value of statistical significance was set at p < 0.05 (two-tailed).
Results
General Characteristics of the Sample
The total sample included 556 patients with a primary diagnosis of BD, of which 43.7% were men (N = 243). The mean (± SD) age was 49.17 (± 14.14) years, and 239 patients (43.0%) were single. Moreover, 198 patients (35.6%) were living alone, and 190 (34.2%) were employed. A total of 277 patients were affected by BD type I, the age of onset was 29.07 (± 13.26) years, while the duration of illness was 19.79 (± 13.10) years. Finally, about half of the patients (N = 225, 40.5%) were taking at least four medications.
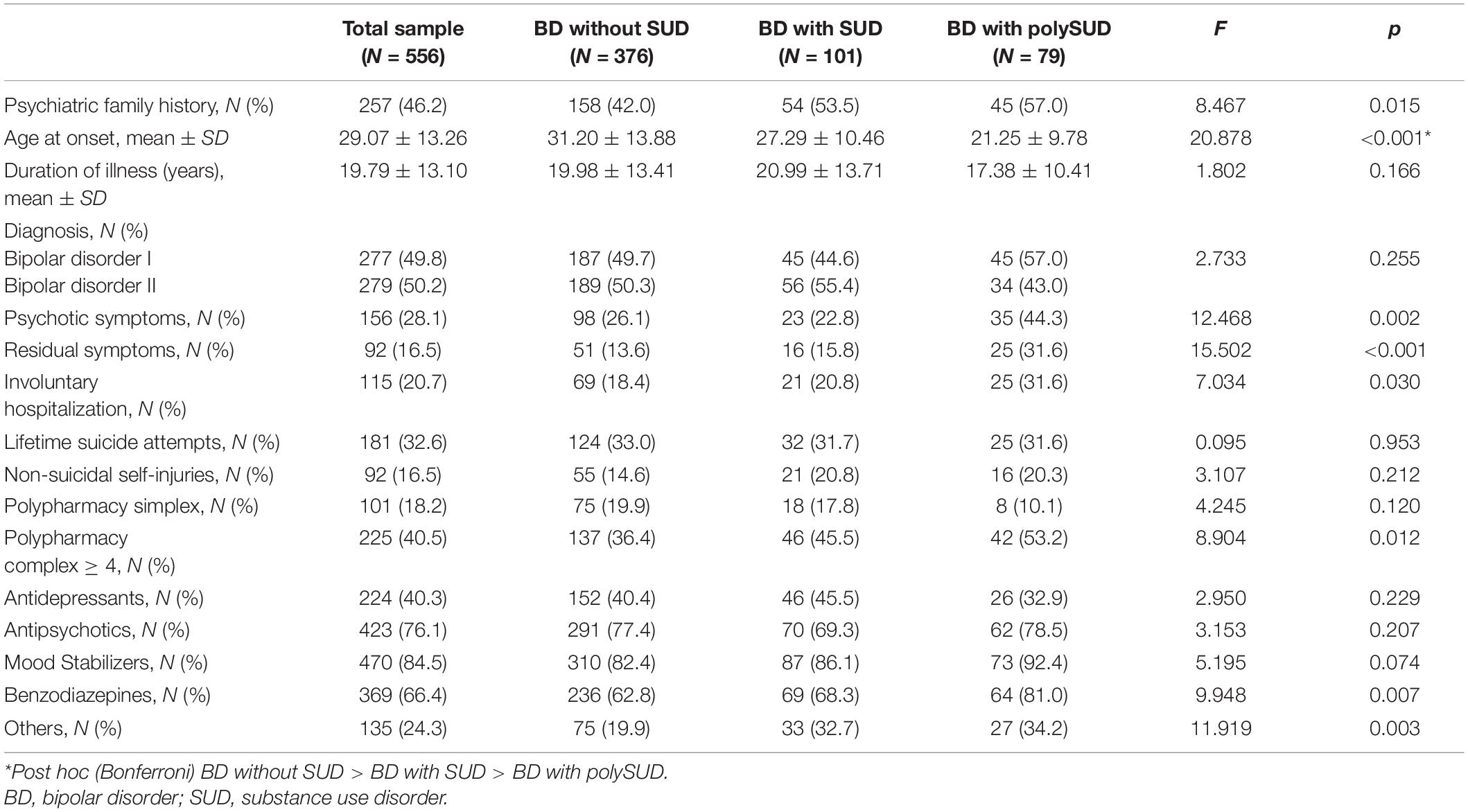
All sociodemographic and clinical characteristics are displayed in Tables 1, 2.

Table 1. Sociodemographic characteristics of the total sample and comparison between the three subgroups.
Comparison of Sociodemographic and Clinical Parameters Between Three Groups of the Sample
Comparing the sociodemographic characteristics, patients with BD and polySUD were more frequently males (65.8% vs. 55.4% vs. 35.9%, p < 0.001), younger (38.90 ± 11.99 vs. 47.98 ± 13.02 vs. 51.64 ± 13.87 years, p < 0.001), single (69.6% vs. 46.5% vs. 36.4%, p < 0.001), and living in a residential facility (11.4% vs. 3.0% vs. 1.3%, p < 0.001) than both participants without SUD or using only one illicit substance.
Regarding the clinical characteristics, patients suffering from BD and polySUD had an earlier age onset (21.25 ± 9.78 vs. 27.29 ± 10.56 vs. 31.20 ± 13.88 years, p < 0.001), a higher prevalence of psychotic (44.3% vs. 22.8% vs. 26.1%, p = 0.002) and residual (31.6% vs. 15.8% vs. 13.6%, p < 0.001) symptoms, and involuntary hospitalization (31.6% vs. 20.8% vs. 18.4%, p < 0.001) than the other subgroups. Finally, a family history for psychiatric disorders was significantly associated with a primary diagnosis of BD and polySUD comorbid (57.0% vs. 53.5% vs. 42.0%, p = 0.015).
Lastly, patients suffering from BD and polySUD showed more polypharmacy complex (53.2% vs. 45.5% vs. 36.4%, p = 0.012) than the other subgroups and the assumption of benzodiazepines (81.0% vs. 68.3% vs. 66.4%, p = 0.007) and other drugs (34.2% vs. 32.7% vs. 19.9%, p = 0.003). All findings are reported in Tables 1, 2.
Multinomial Regression
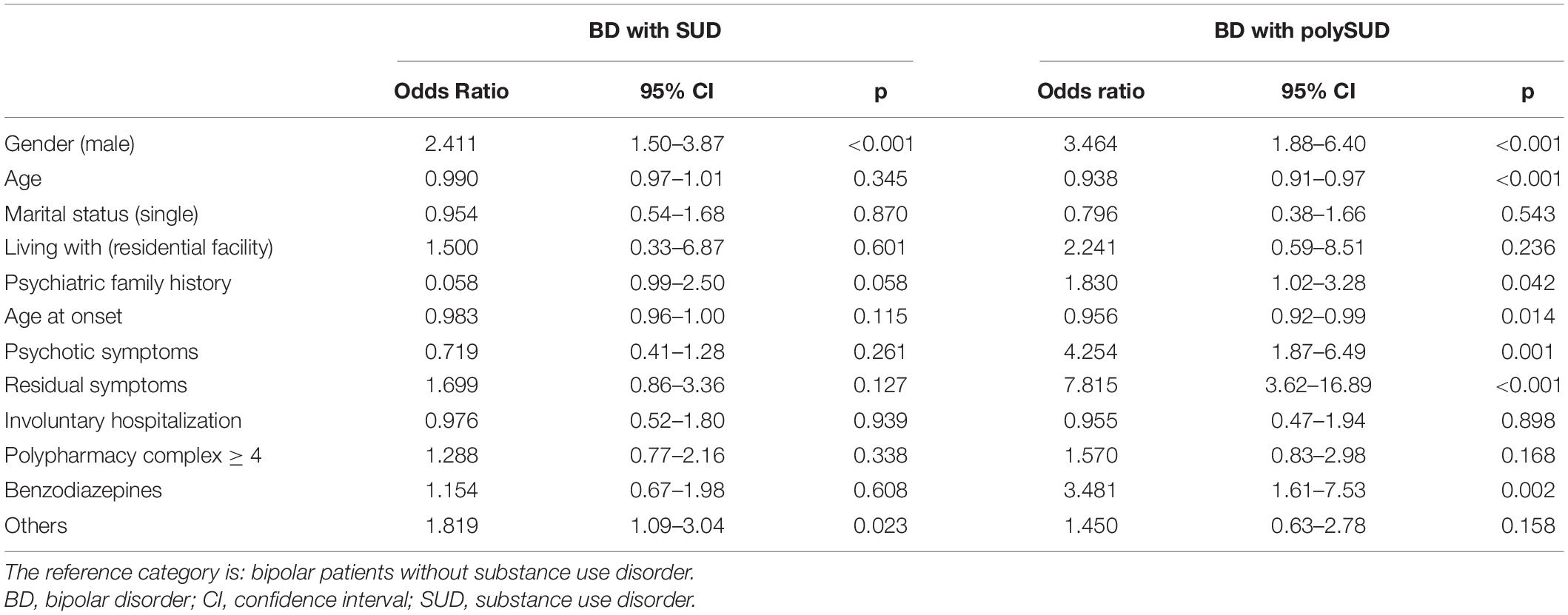
When the multinomial regression was performed with BD without any SUD as the reference category, male gender [OR: 2.411; 95% confidence interval (CI): 1.50–3.87; p < 0.001] and use of other drugs (OR: 1.819; 95% CI: 1.09–3.04; p = 0.023) were associated with SUD in patients affected by BD.
Furthermore, younger age (OR: 0.938; 95% CI: 0.91–0.97; p < 0.001), male gender (OR: 3.464; 95% CI: 1.88–6.40; p < 0.001), earlier age at onset (OR: 0.956; 95% CI: 0.92–0.99; p = 0.014), presence of psychotic (OR: 4.254; 95% CI: 1.87–6.49; p = 0.001), and residual (OR: 7.815; 95% CI: 3.62–16.89; p < 0.001) symptoms, positive family history for psychiatric disorders (OR: 1.830; 95% CI: 1.02–3.28; p = 0.042), and use of benzodiazepines (OR: 3.481; 95% CI: 1.61–7.53; p = 0.002) resulted associated with polySUD in patients with BD, compared to the reference category. All findings are displayed in Table 3.
Discussion
The present paper aimed to evaluate the factors associated with SUD and polySUD in a cohort of patients with BD. Evidence from epidemiological, clinical, and review studies has shown that the comorbidity between patients with a primary diagnosis of BD and SUD is frequent (23, 27, 28, 35). This has also been confirmed in our sample. Moreover, our results showed that while SUD was significantly associated only with the male gender and the category “other drugs,” several sociodemographic and clinical factors were significantly associated with polySUD compared to non-users among patients with BD. Overall, our findings underline that the presence of polySUD should be carefully considered in the pharmacological and non-pharmacological approaches to BD patients for personalized treatment.
According to the existing data literature (26, 36, 37), sociodemographic characteristics such as being male, single, and younger are associated with polySUD. These findings are quite expected, due to the increasing early use of illicit substances in young males in the current society and their well-known negative consequences on neurostructural patterns and functioning, which may impair the building of meaningful social relationships, including marital ones (38–40). However, a difference in marital status emerged only in the univariate but not in the multinomial regression analysis. Furthermore, although our findings showed that patients affected by BD and polySUD lived mainly with family members, the prevalence of patients living in residential facilities was significantly higher than in the other two subgroups. In fact, as indicated by recent guidelines, patients with BD and SUD often need to be addressed toward specific and tailored therapeutic pathways in residential facilities, especially when no familial and social support is present (41). On the one hand, this clinical indication contributes to avoid the use of illicit substances, because patients are placed in a protected context, away from the pathological environment; on the other hand, it allows to follow specific psychological and pharmacological therapeutic strategies, aimed at maintaining the mood stabilization and correcting the unhealthy lifestyles for a better social and familial functioning. Thus, the high rates of comorbidity between severe mental illness and SUD need an integrated approach in psychiatric services with specialized clinicians to encourage early assessment and intervention with active and careful monitoring (42, 43).
Regarding clinical variables, earlier age at onset, the presence of psychotic and residual symptoms, and a family history positive for psychiatric disorders were found to be significantly associated with polySUD in patients with BD. These findings are in line with other studies (35, 37, 44). Illicit substances are considered to be one of the main risk factors and triggers for bipolar illness, as defined by the new diagnostic category named “substance-induced bipolar and related disorder” in the DSM-5 (1). The use of drugs, such as cocaine, amphetamines, or cannabis, is often associated with the first manifestation of an affective episode (31, 32, 45). The earlier age at onset in people with polySUD is not surprising. A timely diagnosis of BD in individuals with SUD may represent a challenge for clinicians, as both the acute and long-term clinical effects of drug abuse and BD symptoms may overlap. Thus, the clinical picture may initially be attributed only to drug use without an accurate assessment for bipolarity, with a consequent misdiagnosis and treatment delay. The actual recognition of an underlying BD may thus be performed only during subsequent hospitalizations.
It is very important to emphasize the association between polySUD and psychotic and residual symptoms. These clinical characteristics were found to be associated with polySUD not only in the univariate but also in the multinomial regression analysis. It is well-known that psychotic and residual symptoms exert a negative impact on the functioning, quality of life, and adherence to treatment in patients with BD (46–49). The relationship between psychotic symptoms and illicit substances in BD could be bidirectional. On the one hand, as mentioned above, illicit substances may induce psychotic symptoms, especially at the onset of BD; moreover, they may determine a switch to a (hypo)manic or mixed episode and the persistence of psychotic symptoms even after the interruption of the pathological use, being potentially related to a gradual and progressive worsening of cognitive functions (50–53). On the other hand, patients suffering from BD may use drugs due to the disinhibition and exaltation typical of manic phases, or to regulate, in the short-term, the negative emotional states typical of major depressive episodes (54). The presence of residual symptoms, intra- or inter- affective episodes, are strongly associated with chronic bipolar illness course, incomplete mood stabilization and frequent affective recurrences, poor sleep quality, as well as social, occupational, and cognitive deterioration with increased subjective stigma and reduced adherence to treatment (46, 55, 56). However, data about the association between residual symptoms and SUD in patients with BD are still controversial and this relationship needs to be explored in depth (44, 57).
Family history of psychiatric disorders has been reported to be a predictor of polySUD in patients with a primary diagnosis of BD, suggesting a vulnerability for this comorbidity (35, 58, 59). Indeed, our results have shown an increase in inpatient involuntary admissions of BD patients with SUD, in line with previous studies (60, 61).
Lastly, our data revealed no difference in SUD between BD type I and II. This is in contrast with previous clinical (26, 35, 62) and epidemiological studies, reporting an increased prevalence of SUD in BD type I (20, 24). No association between polySUD and current or lifetime suicidal behaviors was found in the multinomial regression analysis, although this significant relationship has been reported in a recent meta-analysis (28). Clinicians should always monitor the bipolar illness course in patients with polySUD, focusing mainly on full clinical remission, providing more attention to psychotic symptoms, reducing involuntary admissions, and avoiding the pathological use of illicit substances to decrease suicidality, which should be addressed and evaluated with specific psychometric tools (63, 64).
Finally, with regard to pharmacological treatment, patients with BD and polySUD were more likely to be treated with a complex pharmacological approach, defined as four or more medications (33), compared to the other two subgroups. Even if some level of evidence about the efficacy of polypharmacy exists for BD with comorbid cannabis and cocaine use, unfortunately, a very low grade of evidence is available for heroin, amphetamine, and methamphetamine (41). To our knowledge, this is the first paper that analyzes this particular aspect, and to date, there is no evidence about a possible role of SUD in determining a multiple pharmacological prescriptions in patients affected by BD (33, 65). Our results may underline the necessity to develop more specific guidelines for the treatment of this peculiar subgroup of patients with BD to guide clinicians and avoid the prescription of too many medications with a poor efficacy/side effects balance.
Looking specifically at the pharmacological categories, benzodiazepines and the category of “other drugs” (i.e., gabapentin, pregabalin, oxcarbazepine) were more frequently prescribed among polySUD than the other categories. Several studies showed higher rates of use of benzodiazepines in patients with SUD than in the general population, with a risk of abuse of these drugs (66–68). On the contrary, evidence regarding factors associated with benzodiazepines prescription in patients with BD and comorbid SUD are scarce and inconclusive (69, 70). A recent review explored the use of gabapentin and pregabalin in the treatment of patients with BD, indicating a potential role of these medications in the management of SUD comorbidity (71). Similarly, oxcarbazepine has been proposed as an alternative treatment for SUD during pregnancy (72), but with scarce evidence for the treatment of SUD in comorbidity with BD (73). The increased prevalence of polypharmacy, particularly benzodiazepines and other drugs, in patients suffering from BD and polySUD should be framed as an attempt to reduce abstinence, treat residual symptoms as sleep or anxiety derived from potential subsyndromal psychotic symptoms, or recognize the need for better mood stabilization. However, these hypotheses need to be confirmed by further studies.
Despite the clinical relevance of our findings, several limitations should be discussed. First, our study has a cross-sectional design; therefore, it is not possible to make any inferences on the temporal or causal relationship between the considered variables. Second, several clinical variables (i.e., number of affective episodes, type of bipolar cycle, adherence to treatment, substance switch, and psychiatric comorbidity with personality disorders or anxiety disorders) that could affect the illness course and impact the use of specific drugs were not included in the analyses due to the high number of missing values. Third, no assessment with psychometric tools was made to investigate the potential clinical dimension such as impulsivity, hostility, and aggressiveness. Finally, our data are limited to those derived from a single research center and inpatient unit; therefore, patients with BD in a euthymic phase were not considered.
Conclusion
Our study highlighted that several sociodemograhic and clinical characteristics may be associated with polySUD in patients with a primary diagnosis of BD. Given the significant impact of polySUD on the course and outcome of BD and the need for polypharmacy to guarantee adequate mood stabilization, further research on this topic is needed. Focusing the attention on this specific subtype of patients with BD may help implement personalized pharmacological and psychosocial therapies integrating the different professional roles.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the IRCCS Ospedale Policlinico San Martino. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AAg and AN: statistical analyses and writing the original draft. EB, VP, and EV: data collection and revision of data literature. AAm and AC: supervision of data collection, writing the protocol, review, and editing of the original draft. LF-P: methodology, conceptualization, review, and editing of the original draft. GS, EA, and MA: scientific advisor of the project. All authors approved the final draft of the manuscript before submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018–2022 (Law 232/2016).
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.978089042559
2. Silva Ribeiro J, Pereira D, Salagre E, Coroa M, Santos Oliveira P, Santos V, et al. Risk calculators in bipolar disorder: a systematic review. Brain Sci. (2020) 10:525. doi: 10.3390/brainsci10080525
3. Geoffroy PA, Bellivier F, Scott J, Etain B. Seasonality and bipolar disorder: a systematic review, from admission rates to seasonality of symptoms. J Affect Disord. (2014) 168:210–23. doi: 10.1016/j.jad.2014.07.002
4. Aguglia A, Borsotti A, Maina G. Bipolar disorders: is there an influence of seasonality or photoperiod? Braz J Psychiatry. (2018) 40:6–11. doi: 10.1590/1516-4446-2016-2144
5. Maina G, D’Ambrosio V, Aguglia A, Paschetta E, Salvi V, Bogetto F. Bipolar disorders and metabolic syndrome: a clinical study in 185 patients. Riv Psichiatr. (2010) 45:34–40.
6. Fusar-Poli L, Amerio A, Cimpoesu P, Natale A, Salvi V, Zappa G, et al. Lipid and glycemic profiles in patients with bipolar disorder: cholesterol levels are reduced in mania. Medicina (Kaunas). (2020) 57:28. doi: 10.3390/medicina57010028
7. Salvi V, Aguglia A, Barone-Adesi F, Bianchi D, Donfrancesco C, Dragogna F, et al. Cardiovascular risk in patients with severe mental illness in Italy. Eur Psychiatry. (2020) 63:e96. doi: 10.1192/j.eurpsy.2020.94
8. Aguglia A, Salvi V, Amerio A, Gari M, Dragogna F, Mencacci C, et al. Number of episodes and duration of illness associated with hypertension and 10-year cardiovascular risk in patients with bipolar disorder type I. Psychiatry Res. (2022) 308:114344. doi: 10.1016/j.psychres.2021.114344
9. Foroughi M, Medina Inojosa JR, Lopez-Jimenez F, Saeidifard F, Suarez L, Stokin GB, et al. Association of bipolar disorder with major adverse cardiovascular events: a population-based historical cohort study. Psychosom Med. (2022) 84:97–103. doi: 10.1097/PSY.0000000000001017
10. Liu YK, Ling S, Lui LMW, Ceban F, Vinberg M, Kessing LV, et al. Prevalence of type 2 diabetes mellitus, impaired fasting glucose, general obesity, and abdominal obesity in patients with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. (2022) 300:449–61. doi: 10.1016/j.jad.2021.12.110
11. Fusar-Poli L, Natale A, Amerio A, Cimpoesu P, Grimaldi Filioli P, Aguglia E, et al. Neutrophil-to-lymphocyte, Platelet-to-lymphocyte and monocyte-to-lymphocyte ratio in bipolar disorder. Brain Sci. (2021) 11:58. doi: 10.3390/brainsci11010058
12. Solmi M, Sharma MS, Osimo EF, Fornaro M, Bortolato B, Croatto G, et al. Peripheral levels of C-reactive protein, tumor necrosis factor-α, interleukin-6, and interleukin-1β across the mood spectrum in bipolar disorder: a meta-analysis of mean differences and variability. Brain Behav Immun. (2021) 97:193–203. doi: 10.1016/j.bbi.2021.07.014
13. Khafif TC, Belizario GO, Silva M, Gomes BC, Lafer B. Quality of life and clinical outcomes in bipolar disorder: an 8-year longitudinal study. J Affect Disord. (2021) 278:239–43. doi: 10.1016/j.jad.2020.09.061
14. Kirchner SK, Lauseker M, Adorjan K, Anderson-Schmidt H, Anghelescu IG, Baune BT. Medication adherence in a cross-diagnostic sample of patients from the affective-to-psychotic spectrum: results from the PsyCourse study. Front Psychiatry. (2022) 12:713060. doi: 10.3389/fpsyt.2021.713060
15. Oladunjoye AF, Kaleem SZ, Suresh A, Sahni V, Thoonkuzhy MJ, Anugwom G, et al. Cannabis use and medication nonadherence in bipolar disorder: a nationwide inpatient sample database analysis. J Affect Disord. (2022) 299:174–9. doi: 10.1016/j.jad.2021.11.067
16. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. results from de epidemiologic catchment area (ECA) study. JAMA. (1990) 264:2511–8. doi: 10.1016/0376-8716(93)90010-n
17. Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry. (2015) 72:757–66. doi: 10.1001/jamapsychiatry.2015.0584
18. Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry. (2016) 73:39–47. doi: 10.1001/jamapsychiatry.2015.2132
19. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. (2004) 61:807–16. doi: 10.1001/archpsyc.61.8.807
20. Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Ruan WJ, et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. (2005) 66:1205–15. doi: 10.4088/jcp.v66n1001
21. Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. (2007) 64:543–52. doi: 10.1001/archpsyc.64.5.543
22. Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. (2011) 68:241–51. doi: 10.1001/archgenpsychiatry.2011.12
23. Hunt GE, Malhi GS, Cleary M, Lai HM, Sitharthan T. Comorbidity of bipolar and substance use disorders in national surveys of general populations, 1990-2015: systematic review and meta-analysis. J Affect Disord. (2016) 206:321–30. doi: 10.1016/j.jad.2016.06.051
24. Hunt GE, Malhi GS, Cleary M, Lai HM, Sitharthan T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990-2015: systematic review and meta-analysis. J Affect Disord. (2016) 206:331–49. doi: 10.1016/j.jad.2016.07.011
25. Acciavatti T, Lupi M, Santacroce R, Aguglia A, Attademo L, Bandini L, et al. Novel psychoactive substance consumption is more represented in bipolar disorder than in psychotic disorders: a multicenter-observational study. Hum Psychopharmacol. (2017) 32:e2578. doi: 10.1002/hup.2578
26. Zamora-Rodríguez FJ, Sánchez-Waisen-Hernández MR, Guisado-Macías JA, Vaz-Leal FJ. Substance use and course of bipolar disorder in an inpatient sample. Actas Esp Psiquiatr. (2018) 46:183–91.
27. Preuss UW, Schaefer M, Born C, Grunze H. Bipolar disorder and comorbid use of illicit substances. Medicina (Kaunas). (2021) 57:1256. doi: 10.3390/medicina57111256
28. Messer T, Lammers G, Müller-Siecheneder F, Schmidt RF, Latifi S. Substance abuse in patients with bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. (2017) 253:338–50. doi: 10.1016/j.psychres.2017.02.067
29. Grunze H, Schaefer M, Scherk H, Born C, Preuss UW. Comorbid bipolar and alcohol use disorder-a therapeutic challenge. Front Psychiatry. (2021) 12:660432. doi: 10.3389/fpsyt.2021.660432
30. Tsuboi T, Suzuki T, Azekawa T, Adachi N, Ueda H, Edagawa K, et al. Factors associated with non-remission in bipolar disorder: the multicenter treatment survey for bipolar disorder in psychiatric outpatient clinics (MUSUBI). Neuropsychiatr Dis Treat. (2020) 16:881–90. doi: 10.2147/NDT.S246136
31. Bach SL, Cardoso TA, Moreira FP, Mondin TC, Simjanoski M, Kapczinski FP, et al. Risk factors for new-onset bipolar disorder in a community cohort: a five-year follow up study. Psychiatry Res. (2021) 303:114109. doi: 10.1016/j.psychres.2021.114109
32. Lalli M, Brouillette K, Kapczinski F, de Azevedo Cardoso T. Substance use as a risk factor for bipolar disorder: a systematic review. J Psychiatr Res. (2021) 144:285–95. doi: 10.1016/j.jpsychires.2021.10.012
33. Kim AM, Salstein L, Goldberg JF. A systematic review of complex polypharmacy in bipolar disorder: prevalence, clinical features, adherence, and preliminary recommendations for practitioners. J Clin Psychiatry. (2021) 82:20r13263. doi: 10.4088/JCP.20r13263
34. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4.
35. Menculini G, Steardo L Jr., Verdolini N, Cirimbilli F, Moretti P, Tortorella A. Substance use disorders in bipolar disorders: clinical correlates and treatment response to mood stabilizers. J Affect Disord. (2022) 300:326–33. doi: 10.1016/j.jad.2022.01.001
36. Simhandl C, Radua J, König B, Amann BL. Prevalence and impact of comorbid alcohol use disorder in bipolar disorder: a prospective follow-up study. Aust N Z J Psychiatry. (2016) 50:345–51. doi: 10.1177/0004867415585855
37. Pinto JV, Medeiros LS, Santana da Rosa G, Santana de Oliveira CE, Crippa JAS, Passos IC, et al. The prevalence and clinical correlates of cannabis use and cannabis use disorder among patients with bipolar disorder: a systematic review with meta-analysis and meta-regression. Neurosci Biobehav Rev. (2019) 101:78–84. doi: 10.1016/j.neubiorev.2019.04.004
38. Szmulewicz AG, Valerio MP, Lomastro J, Smith JM, Chiappe V, Martino DJ, et al. Neurocognitive functioning in first-episode bipolar disorder: relationship with functional status. J Affect Disord. (2018) 228:97–100. doi: 10.1016/j.jad.2017.12.015
39. Prisciandaro JJ, Mellick W, Mitaro E, Tolliver BK. An evaluation of the impact of co-occurring anxiety and substance use disorder on bipolar disorder illness outcomes in STEP-BD. J Affect Disord. (2019) 246:794–9. doi: 10.1016/j.jad.2018.12.070
40. Sultan AA, Kennedy KG, Fiksenbaum L, MacIntosh BJ, Goldstein BI. Neurostructural correlates of cannabis use in adolescent bipolar disorder. Int J Neuropsychopharmacol. (2021) 24:181–90. doi: 10.1093/ijnp/pyaa077
41. Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. (2018) 20:97–170. doi: 10.1111/bdi.12609
42. Vieta E, Salagre E, Grande I, Carvalho AF, Fernandes BS, Berk M, et al. Early intervention in bipolar disorder. Am J Psychiatry. (2018) 175:411–26. doi: 10.1176/appi.ajp.2017.17090972
43. Fantuzzi C, Mezzina R. Dual diagnosis: a systematic review of the organization of community health services. Int J Soc Psychiatry. (2020) 66:300–10. doi: 10.1177/0020764019899975
44. Grover S, Chakrabarti S, Sahoo S. Prevalence and clinical correlates of residual symptoms in remitted patients with bipolar disorder: an exploratory study. Indian J Psychiatry. (2020) 62:295–305. doi: 10.4103/psychiatry.IndianJPsychiatry_760_19
45. van Laar M, van Dorsselaer S, Monshouwer K, de Graaf R. Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population? Addiction. (2007) 102:1251–60. doi: 10.1111/j.1360-0443.2007.01875.x
46. Samalin L, de Chazeron I, Vieta E, Bellivier F, Llorca PM. Residual symptoms and specific functional impairments in euthymic patients with bipolar disorder. Bipolar Disord. (2016) 18:164–73. doi: 10.1111/bdi.12376
47. Morton E, Murray G, Michalak EE, Lam RW, Beaulieu S, Sharma V, et al. Quality of life in bipolar disorder: towards a dynamic understanding. Psychol Med. (2018) 48:1111–8. doi: 10.1017/S0033291717002495
48. Bonnín CM, Jiménez E, Solé B, Torrent C, Radua J, Reinares M, et al. Lifetime psychotic symptoms, subthreshold depression and cognitive impairment as barriers to functional recovery in patients with bipolar disorder. J Clin Med. (2019) 8:1046. doi: 10.3390/jcm8071046
49. Consoloni JL, M’Bailara K, Perchec C, Aouizerate B, Aubin V, Azorin JM, et al. Trajectories of medication adherence in patients with bipolar disorder along 2 years-follow-up. J Affect Disord. (2021) 282:812–9. doi: 10.1016/j.jad.2020.12.192
50. Dell’Osso B, Camuri G, Cremaschi L, Dobrea C, Buoli M, Ketter TA, et al. Lifetime presence of psychotic symptoms in bipolar disorder is associated with less favorable socio-demographic and certain clinical features. Compr Psychiatry. (2017) 76:169–76. doi: 10.1016/j.comppsych.2017.04.005
51. Inchausti L, Gorostiza I, Torres G, Oraa R. Diagnostic stability in substance-induced psychosis. Rev Psiquiatr Salud Ment (Engl Ed). (2020): [Epub ahead of print], doi: 10.1016/j.rpsm.2019.10.005
52. Fiorentini A, Cantù F, Crisanti C, Cereda G, Oldani L, Brambilla P. Substance-induced psychoses: an updated literature review. Front Psychiatry. (2021) 12:694863. doi: 10.3389/fpsyt.2021.694863
53. Gogia M, Shah AQ, Kapczinski F, de Azevedo Cardoso T. The impact of substance use disorder comorbidity on cognition of individuals with bipolar disorder: a systematic review. Psychiatr Res. (2022) 311:114525. doi: 10.1016/j.psychres.2022.114525
54. Arias F, Szerman N, Vega P, Mesiìas B, Basurte I, Rentero D. Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones. (2017) 29:186–94. doi: 10.20882/adicciones.782
55. Cretu JB, Culver JL, Goffin KC, Shah S, Ketter TA. Sleep, residual mood symptoms, and time to relapse in recovered patients with bipolar disorder. J Affect Disord. (2016) 190:162–6. doi: 10.1016/j.jad.2015.09.076
56. Samalin L, Boyer L, Murru A, Pacchiarotti I, Reinares M, Bonnin CM, et al. Residual depressive symptoms, sleep disturbance and perceived cognitive impairment as determinants of functioning in patients with bipolar disorder. J Affect Disord. (2017) 210:280–6. doi: 10.1016/j.jad.2016.12.054
57. Serafini G, Vazquez GH, Gonda X, Pompili M, Rihmer Z, Amore M. Depressive residual symptoms are associated with illness course characteristics in a sample of outpatients with bipolar disorder. Eur Arch Psychiatry Clin Neurosci. (2018) 268:757–68. doi: 10.1007/s00406-018-0875-5
58. Duffy A, Horrocks J, Milin R, Doucette S, Persson G, Grof P. Adolescent substance use disorder during the early stages of bipolar disorder: a prospective high- risk study. J Affect Disord. (2012) 142:57–64. doi: 10.1016/j.jad.2012.04.010
59. Hulvershorn LA, King J, Monahan PO, Wilcox HC, Mitchell PB, Fullerton JM, et al. Substance use disorders in adolescent and young adult relatives of probands with bipolar disorder: what drives the increased risk? Compr Psychiatry. (2017) 78:130–9. doi: 10.1016/j.comppsych.2017.07.010
60. Schuepbach D, Goetz I, Boeker H, Hell D. Voluntary vs. involuntary hospital admission in acute mania of bipolar disorder: results from the Swiss sample of the EMBLEM study. J Affect Disord. (2006) 90:57–61. doi: 10.1016/j.jad.2005.09.012
61. Schuepbach D, Novick D, Haro JM, Reed C, Boeker H, Noda S, et al. Determinants of voluntary vs. involuntary admission in bipolar disorder and the impact of adherence. Pharmacopsychiatry. (2008) 41:29–36. doi: 10.1055/s-2007-993213
62. Serafini G, Gonda X, Aguglia A, Amerio A, Santi F, Pompili M, et al. Bipolar subtypes and their clinical correlates in a sample of 391 bipolar individuals. Psychiatry Res. (2019) 281:112528. doi: 10.1016/j.psychres.2019.112528
63. Baertschi M, Costanza A, Canuto A, Weber K. The dimensionality of suicidal ideation and its clinical implications. Int J Methods Psychiatr Res. (2019) 28:e1755. doi: 10.1002/mpr.1755
64. Levola J, Laine R, Pitkanen T. In-patient psychiatric care and non-substance-related psychiatric diagnoses among individuals seeking treatment for alcohol and substance use disorders: associations with all-cause mortality and suicide. Br J Psychiatry. (2022):1–8. doi: 10.1192/bjp.2022.20 [Epub ahead of print].
65. Golden JC, Goethe JW, Woolley SB. Complex psychotropic polypharmacy in bipolar disorder across varying mood polarities: a prospective cohort study of 2712 inpatients. J Affect Disord. (2017) 221:6–10. doi: 10.1016/j.jad.2017.06.005
66. Maust DT, Lin LA, Blow FC. Benzodiazepine use and misuse among adults in the United States. Psychiatr Serv. (2019) 70:97–106. doi: 10.1176/appi.ps.201800321
67. Votaw VR, Geyer R, Rieselbach MM, McHugh RK. The epidemiology of benzodiazepine misuse: a systematic review. Drug Alcohol Depend. (2019) 200:95–114. doi: 10.1016/j.drugalcdep.2019.02.033
68. McHugh RK, Geyer RB, Chase AR, Griffin ML, Bogunovic O, Weiss RD. Sex differences in benzodiazepine misuse among adults with substance use disorders. Addict Behav. (2021) 112:106608. doi: 10.1016/j.addbeh.2020.106608
69. Bobo WV, Reilly-Harrington NA, Ketter TA, Brody BD, Kinrys G, Kemp DE, et al. Complexity of illness and adjunctive benzodiazepine use in outpatients with bipolar I or II disorder: results from the bipolar CHOICE study. J Clin Psychopharmacol. (2015) 35:68–74. doi: 10.1097/JCP.0000000000000257
70. Wingård L, Taipale H, Reutfors J, Westerlund A, Bodén R, Tiihonen J, et al. Initiation and long-term use of benzodiazepines and Z-drugs in bipolar disorder. Bipolar Disord. (2018) 20:634–46. doi: 10.1111/bdi.12626
71. Ng QX, Han MX, Teoh SE, Yaow CYL, Lim YL, Chee KTA. Systematic review of the clinical use of gabapentin and pregabalin in bipolar disorder. Pharmaceuticals (Basel). (2021) 14:834. doi: 10.3390/ph14090834
72. Johnson KD, Miller LN, Pouliot JD, Martin PR. Retrospective analysis of oxcarbazepine in pregnant women with substance use disorders: focus on safety. J Pharm Pract. (2021) 34:28–34. doi: 10.1177/0897190019850700
Keywords: bipolar disorder, substance use disorder, treatment, psychotic symptoms, polypharmacy
Citation: Aguglia A, Natale A, Fusar-Poli L, Amerio A, Bruno E, Placenti V, Vai E, Costanza A, Serafini G, Aguglia E and Amore M (2022) Bipolar Disorder and Polysubstance Use Disorder: Sociodemographic and Clinical Correlates. Front. Psychiatry 13:913965. doi: 10.3389/fpsyt.2022.913965
Received: 06 April 2022; Accepted: 11 May 2022;
Published: 15 June 2022.
Edited by:
Domenico De Berardis, Mental Health Center (CSM) and Psychiatric Service of Diagnosis and Treatment (SPDC), ItalyReviewed by:
Renato de Filippis, Magna Græcia University, ItalyXenia Gonda, Semmelweis University, Hungary
Copyright © 2022 Aguglia, Natale, Fusar-Poli, Amerio, Bruno, Placenti, Vai, Costanza, Serafini, Aguglia and Amore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Aguglia, YW5kcmVhLmFndWdsaWFAdW5pZ2UuaXQ=
 Andrea Aguglia
Andrea Aguglia Antimo Natale
Antimo Natale Laura Fusar-Poli
Laura Fusar-Poli Andrea Amerio
Andrea Amerio Edoardo Bruno1,2
Edoardo Bruno1,2 Alessandra Costanza
Alessandra Costanza Gianluca Serafini
Gianluca Serafini Mario Amore
Mario Amore