- 1School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Aman, Ethiopia
- 2Department of Psychiatry, School of Medicine, College of Medicine and Health Sciences, Mizan Tepi University, Mizan Aman, Ethiopia
- 3Department of Nursing, College of Medicine and Health Sciences, Mizan Tepi University, Mizan Aman, Ethiopia
- 4Department of Public Health and Epidemiology, Faculty of Medicine, University of Debrecen, Debrecen, Hungary
Background: Adequate sleep is vital for physical and mental wellbeing. Sleep-related problems including poor quality of sleep have been increasing throughout the world among reproductive-aged women. Poor sleep quality has been related with number of diseases and health problems However, evidences are scarce regarding poor sleep quality and its associated factors among women of the reproductive age group in Ethiopia.
Objective: To assess sleep quality and associated factors among women of reproductive age group in Mizan Aman town, Southwest Ethiopia.
Method: Community-based cross-sectional study was conducted among 606 reproductive-aged women from 06 November to 20 December 2020, in Mizan Aman town. Data were collected using structured interview administered questionnaires. Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality. Multivariable logistic regression was applied using an adjusted odds ratio with a corresponding 95% confidence interval to evaluate the statistical significance of associated factors.
Result: The overall prevalence of poor sleep quality was 71.3%. The late age group of 42–49 (AOR, 95% CI; 1.21 (1.08–5.76), palpable/visible thyroid gland (AOR, 95% CI; 2. 12 (1.08–3.82), current substance use (AOR, 95% CI; 1.76 (1.11–6.10) and having premenstrual syndrome (AOR, 95% CI; 1.86 (1.38–3.12) were significantly associated with poor sleep quality among reproductive age group women.
Conclusion: Significant majority of reproductive age group women faced poor sleep quality. Therefore, screening of sleep patterns among this particular age group is warranted. Moreover, education about sleep hygiene needs to be given considering the identified factors to improve sleep quality.
Background
Sleep is a natural physiological process that is necessary for an individual's normal physical, emotional, and mental wellbeing (1). Good quality sleep which is characterized by adequate duration, appropriate timing, regularity, and the absence of sleep disturbances or disorders is essential for one's quality of life (2). Sleep quality may reflect different aspects of sleep measures including Total Sleep Time (TST), Sleep Onset Latency (SOL), sleep maintenance, Total Wake Time (TWT), Sleep Efficiency (SE), and sometimes sleep disruptive events such as spontaneous arousal or apnea (3).
Women are increasingly facing sleep-related problems throughout their life cycle. Shreds of evidence showed women are reporting more sleep-related problems when compared to men (3, 4). Hormonal, behavioral, and mood-related issues could worsen the risk among women throughout their life cycle (5, 6). Sleep fragmentation, sleep continuity disturbance, short or long sleep duration, circadian dysrhythmia, and/or hypoxia could all be relevant domains in terms of sleep disturbance among females (7, 8). Reproductive age group women face difficulties related to sleep in premenstrual, menstrual, pregnancy, and during the postpartum period (9). Poor sleep quality is also associated with early pregnancy loss, failed embryo implantation, anovulation and amenorrhea, and even infertility (10, 11).
The magnitude of sleep quality varies across the countries among reproductive-aged group women. A study conducted among young adult women reported that nearly half (45%) of women had poor sleep quality (12). Similarly, 22% of young Korean women experienced poor sleep quality (13). Moreover, the prevalence of poor sleep quality was 28.2% in Nepal (14), 43.7% in the USA (15), and 57% in Canada (16) among reproductive age group women. Multiple factors were identified as predictors of poor sleep quality in this particular age group including socioeconomic and demographic factors, having a history of chronic medical illness, social support, substance use, and history of mental illness (17–22).
Poor quality sleep has been associated with physical, social, economic, and psychological problems (23). Nearly 70% of mental health illnesses such as depression, suicidal ideations, and postpartum psychosis, are caused by sleep pattern abnormalities (24). Moreover, sleep disturbances are also contributed to daytime weakness, tiredness, sluggishness, languid driving, stress, poor impulse control, and pain (25, 26). Poor sleep quality can also be a cause for non-communicable diseases including obesity, hypertension and type 2 diabetes, and could be a primary driver of other health problems (27, 28). Furthermore, Hundreds of billions of dollars a year are spent on direct medical costs associated with health care expenditure and loss of productivity in the work places (29).
Given the deleterious impact of poor sleep quality on health outcomes and wellbeing of reproductive-aged women, this population group should be screened for poor sleep quality regularly (30). Nevertheless, little study pays attention to the quality of sleep among this age group (31). Despite the growing evidences regarding sleep-related problems in a developed country among reproductive-aged women, the pieces of evidence on developing countries including Ethiopia are limited (32). Besides, most of the available evidences are limited to college students, the general population, pregnant and post-partum mothers (32–35). Furthermore, to the best knowledge of the authors, there is no prior study, which examined the sleep quality of reproductive age group women in the study area. Therefore, this study aimed to assess sleep quality and its associated factors among reproductive age group women in Mizan Aman town, southwest Ethiopia.
Methods and Materials
Study Design, Setting and Period
A community-based cross-sectional study was conducted among reproductive-age women who live in Mizan Aman town, which is located 586 km southwest of Addis Ababa. Mizan Aman is an administrative capital of Bench Sheko Zone and has five kebeles (lower administrative unit of Ethiopian administration). The town has an estimated population of 52, 210, of which 11,554 are women of reproductive age group (15–49 years). There are one teaching hospital, one health center, five health posts, one university, and one college found in the city. The town has five kebeles and the study was conducted in two selectedkebeles from 06 November-20 December, 2020.
Study Population
The source population for this study was all reproductive-aged group women in Mizan Aman town. Reproductive age group women from selected household were the study population and selected reproductive age grouped women from the selected household were the study unit. The study participant was randomly selected from the selected households. Women with serious illness or unable to communicate during the interview were excluded from the study.
Sample Size Determination and Sampling Technique
The minimum required sample size for this study was calculated using a single population proportion formula. Since there was no previous study regarding sleep quality among reproductive-aged group women in Ethiopia, we assumed a 50% proportion of poor sleep quality, precision level of 5%, 95% confidence interval, and 10% for non-response. Accordingly, the estimated sample size was 422. Hence multistage sampling was employed 1.5 design effect was used and the final sample size was 634.
Two selectedkebeles were included in the study. Census was done in the selected kebeles to identify household with reproductive age group women before the data collection. Then, the total sample size (n = 634) was allocated proportionally to each selected kebeles based on the number of eligible women. Then systematic random sampling method was employed to select households from those selected kebeles. The first house was selected randomly and then every 16th house was enrolled. The sampling interval of the households in each Kebele was determined by dividing the total number of households in the specific kebele by the allocated sample size (10,329/634 = 16). In the case of more than one eligible woman was encountered in the selected household, a lottery method was used to determine which woman would be interviewed.
Study Variables, Data Collection Tools, and Measurement
The dependent variable of the study was sleep quality (Good or poor). Independent variables were socio-demographic factors such as age, religion, marital status, ethnicity, educational status, income level, employment, and residence, pregnancy, clinical factors such as depression, palpable (visible) thyroid gland, known history of mental illness, and medical illness, and substance use such as alcohol use, khat use, and smoking cigarettes.
To measure poor sleep quality (PSQ) a validated standardized test, the Pittsburgh Sleep Quality Index (PSQI) was used. The PSQI is a 19-item self-report measure designed to measure sleep quality over the past month. It has seven subscales and these subscales are added to determine a global sleep quality score (GSQ). The GSQ score ranges from 0 to 21, the score >5 was labeled as having poor sleep quality and those with PSQI score ≤5 were labeled as having good sleep quality (33). The reliability (Cronbach's alpha) in this study was 0.89.
Depression was assessed by using Patient Health Questionnaire-9 (PHQ-9) and the study participants were considered to have depression if their PHQ-9 score was ≥10 (36).
Current substance use: consuming any substance (Alcohol, Khat and cigarettes smoking) within the last 1 month/30 days (37).
Premenstrual syndrome (PMS): A 10-item tool validated for the assessment of PMS. It has subscales, namely affect, water retention and pain. The total scores were calculated and a score >27 was considered as PMS (38, 39).
Medical illness: Reproductive aged women with chronic medical illness and their diagnosis confirmed in any health institution and assessed by “Yes” or “No” questions.
Palpable (visible): The goiter examination was done and graded according to WHO classification. Grade 0: no goiter (neither visible nor palpable); grade 1: thyroid palpable but not visible; grade 2: thyroid visible with the neck in normal position. Palpable (visible) thyroid gland was considered a grade 1 and 2 thyroid (29).
Data Quality Control
The data were collected using a standard structured interview administered questionnaire. The English version questionnaires were translated to the local language Amharic. Data were collected by trained three data collectors and two supervisors qualified with a Bachelor of Science degree in psychiatry nursing. The collected data were evaluated for completeness, clarity, and consistency by the supervisor and investigators daily.
Data Processing and Analysis
The collected data were coded and entered into Epi Data manager version 4.0.2, then, exported to SPSS version 25 statistical software for data analysis. Descriptive statistics like proportion (for categorical variables), mean and SD (for normally distribute continuous variables) were done for different variables. Normality plots (Q-Q plots and/or histograms) were used to check for normality assumptions. Hence, for non-normally distributed variables we used median and interquartile range (IQR) for summary statistics. Bivariable logistic regression was used to identify the associations between the dependent and independent variables. Those variables with a p-value of < 0.25 on bivariable logistic regression analysis were transferred to multivariable logistic regression. Interactions and confounders were tested using beta change at cutoff point 20%. Multicollinearity was checked explanatory variables and the variance inflation factor (VIF) was found to be <4. The final model fitness status was checked by Hosmer and Lemeshow's goodness of fit chi-square test (value = 0.79). Adjusted odds ratio (AOR) with a corresponding 95% CI was considered to declare a level of significance for PSQ in multivariable logistic regression analysis.
Results
Socio-Demographic Characteristics of the Study Participants
Six hundred six reproductive age group women were enrolled in this study, which makes a 95.6% response rate. The study participants median (IQR) age was 25 (22–36) years and nearly half (45.7%) were in the age group of 24–33 years. Three hundred sixty (59.4%) of the participant were completed secondary or above education and the majority of the participants were located in the monthly income level of ≤1,500 ETB (Table 1).
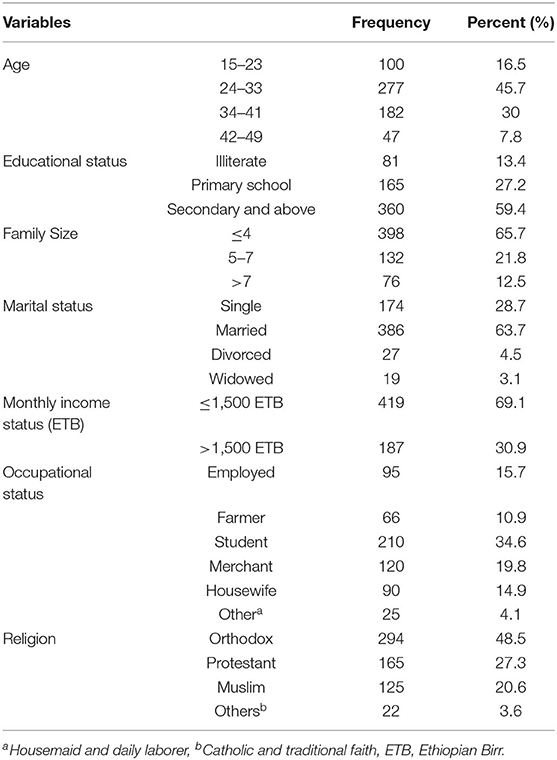
Table 1. Sociodemographic characteristics of a study participant in Mizan Aman town, Southwestern Ethiopia, 2020 (n = 606).
Substance Use and Medical Illness
Two hundred forty-one (39.8%) of the participant used substances (Khat, alcohol, or cigarette) at least once in the past 1 month and sixty-four reproductive age group women had a history of mental illness. More than half (51.1%) of the participants had depression (Table 2).
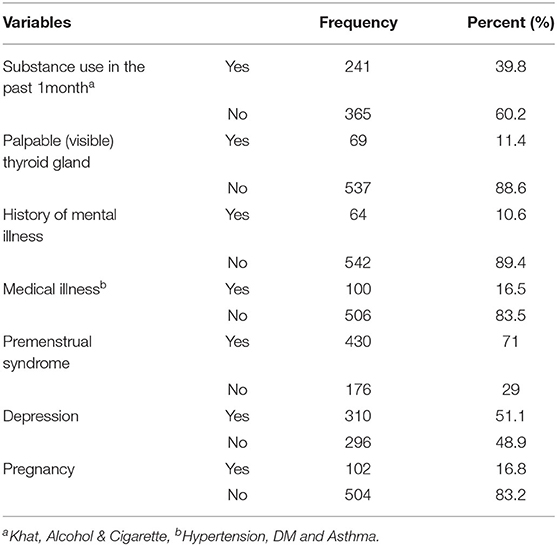
Table 2. Substance use and medical conditions among reproductive age group women in Mizan Aman Town, Southwestern Ethiopia, 2020 (n = 606).
Prevalence of Sleep Quality and Its Component Scores
The overall prevalence of PSQ was 71.3% (95% CI 64–75%). The seven components of sleep quality were assessed using the PSQI and accordingly 153 (25.2%) participants rated their subjective sleep quality very bad and 202 (33.4%) of reproductive women had >7 h of sleep per night. Again, eight participants reported the use of sleep medication during the last month (a month before data collection). Moreover, the habitual sleep efficiency was ≥85% in 20% and <65% in 16.3% of the study participants (Table 3).
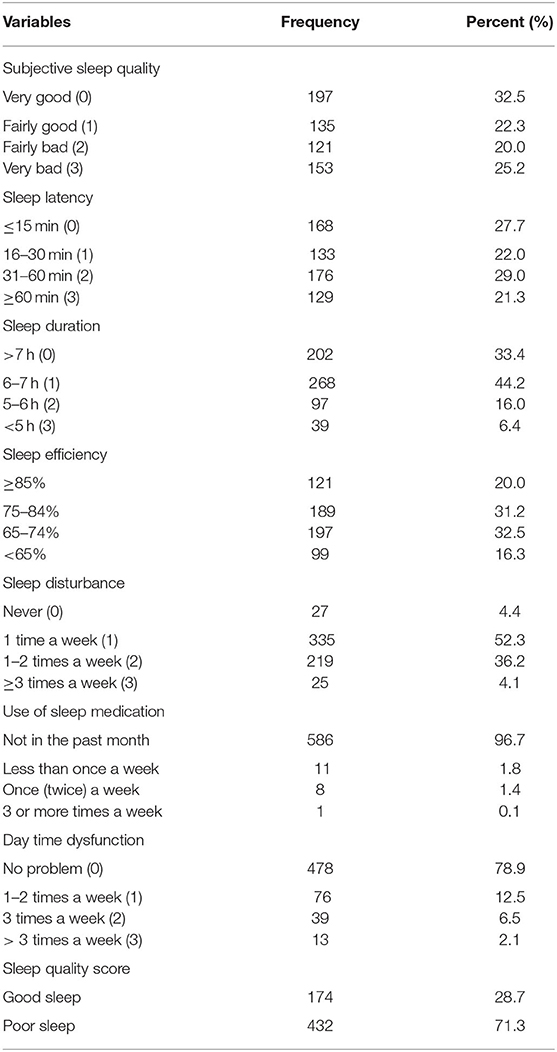
Table 3. Sleep quality and its component scores among reproductive age group women in Mizan Aman Town, Southwestern Ethiopia, 2020 (n = 606).
Factors Associated With Poor Sleep Quality
Multivariable logistic regression analysis was conducted with those variables with p < 0.25 in bivariable logistic regression analysis. Accordingly, the age of the participant, palpable (visible) thyroid gland, current substance use, and the premenstrual syndrome were independent predictors of PSQ among the study participants (Table 4).
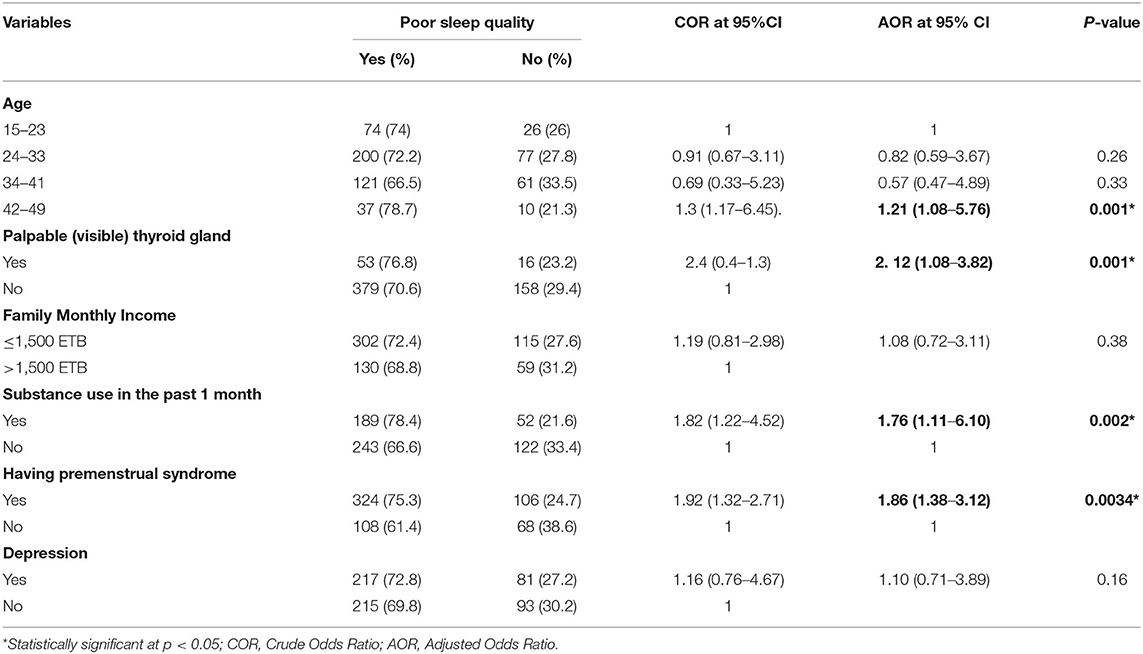
Table 4. Bivariable and multivariable logistic regression analysis for factors associated with poor sleep quality among reproductive age group women in Mizan Aman Town, Southwest Ethiopia, 2020 (N = 606).
Women in the age group of 42–49 [AOR, 95%CI; 1.21 (1.08-5.76)] years were more likely to experience poor sleep quality in comparison to young women in the age group of 15–23 years. The odds of poor sleep quality were 2.12 times higher in women with palpable (visible) thyroid glands than in women with no palpable (visible) thyroid gland. Furthermore, current substance users and women with premenstrual syndrome were 1.86 and 1.76 times more likely to be affected by poor sleep quality, respectively (Table 4).
Discussion
This study was aimed to determine the prevalence of sleep quality and its associated factors among reproductive age group women. Accordingly, the prevalence of sleep quality is 71.3% (95% CI 64–75). The prevalence observed in this study is comparable with the study conducted in Brazil (66%) (40). However, the prevalence in the current study is higher than studies conducted in Canada (52.8%) (16) and Southeast Texas (43.7%) (15). The possible explanation for this variation could be the socio-economic and socio-cultural differences. This study was conducted during the time the first wave of Covid-19 hit Ethiopia, so there are anxiety and fear of the pandemic, which in turn increase the magnitude of poor sleep quality. Furthermore, being locked down and inability to engage with friends and relatives due to Covid-19 restrictions could also rise the prevalence (41–44). In this study, more than half (51%) of the participants had depression, which is a known risk factor for poor sleep quality and could be another explanation for the observed high prevalence of poor sleep quality (45, 46). Moreover, the study area is around gold mining site where production and problematic substance use are relatively high. Even in our study, 40% of reproductive age group uses substances (Khat, alcohol and cigarette). Substance use especially khat which is an amphetamine type stimulant plant leave produced and consumed locally has been strongly associated with insomnia and could increase the magnitude of poor sleep quality (47, 48).
Women age showed a statistically significant association with poor sleep quality. It indicated that women of premenopausal age are more likely to suffer poor sleep quality. This finding is corroborated by a study conducted in Taiwan were older mothers were three times more likely to have poor sleep quality than younger mothers (49). Premenopausal age has marked with menstrual irregularity due to hormonal alteration and mood changes. The vasomotor symptoms (hot flashes and night sweats) and lower urinary tract symptoms are also common during this period. These changes during premenopausal period further complicates and leads to decline in sleep quality (30, 50).
The current study also showed palpable/visible thyroid gland as a significant factor for poor sleep quality. Women with palpable/visible thyroid glands were at increased odds of having poor sleep quality. Both hyperthyroidism and hypothyroidism has been linked with sleep problems. Hyperthyroidism (overactive) can cause difficulty sleeping due to arousals from nervousness or irritability (51, 52). An overactive thyroid may also lead to night sweats and frequent urges to urinate, both of which can disrupt sleep (52, 53). Similarly, studies showed hypothyroidism also linked with longer onset and shorter duration of sleep caused by difficulty of tolerating cold at night and joint or muscle pain (51, 52). Therefore, these implied the need to screen sleep problems among individuals with palpable (visible) thyroid.
In addition, poor sleep quality is more common among substance users when compared with non-substance users. Substance use including Alcohol, cigarette smoking, and Khat chewing has been identified as a predictor of frequent sleep problems. This finding is consistent with studies done on Norwegian (47) and US adolescents (48) where substance use and sleep problems have a bi-directional effect. Growing evidence shows substance use has a link to mental and physical health problems including sleep disturbance. Sleep-related outcomes of substance use range from extended sleep onset latency (SOL), reduced total sleep time (TST), more nighttime awakenings, and decreased slow-wave sleep (SWS) to rapid eye movement (REM) sleep (54). Educating the effect of substance use on sleep quality needs to be considered in this particular age group.
Moreover, our study showed women with premenstrual syndrome are at increased odds to have poor sleep quality. This is in agreement with studies in South Africa (9), Turkey (55), and Taiwan (56). In support of this finding, menstrual-related hormonal fluctuations may be responsible for this sleep disturbance, which is a common problem during menstruation. Some severe forms of premenstrual syndrome are associated with sleep onset insomnia, frequent night time awakenings, and non-restoration of sleep (57). This calls for the need to give due attention to sleep problems during menstrual period.
The community-based nature of the study and using a validated tool to measure sleep quality among study participants are the strength of this study. However, this study could suffer from social desirability and recall biases.
Conclusion
This study showed high prevalence of poor sleep quality among reproductive age group women. Age, substance use, premenstrual syndrome, and palpable/visible thyroid gland are identified as factors associated with poor sleep quality. Therefore, due attention needs to be given for this age group women. Moreover, designing effective health education and promotion considering the identified predictors of poor sleep quality could be helpful to decrease the burden of poor quality sleep among reproductive age group women.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical clearance and a supportive letter were obtained from Mizan Tepi University College of Medicine and Health Sciences Ethics Committee (Reference number: 0142/2020) for the commencement of data collection. Written informed consent was obtained from study subjects. For illiterate participant who could not read consent form, the document was orally presented to them or their legally authorized representative as approved by the ethics committee. Again, for minors (age less than 16 years) written informed consent was obtained from parents and/or legal guardian. The participants were informed to decline and stop the interview when they want to do it without any preconditions. Personal identifiers were omitted to maintain the confidentiality of the information. Moreover, the collected data was kept safe throughout the whole data collection and analysis. Those participants diagnosed with depression and goiter were linked to the hospital. This study was conducted following a Helsinki declaration for research ethics.
Author Contributions
AW designed the study, supervised data, and reviewed the manuscript. BB participated in the design of the study, carried out the statistical analysis, drafted the manuscript, and critically reviewed the manuscript. NM, BBB, and GM participated in statistical analysis and reviewing of the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank data collectors and supervisors for their cooperation. We also extend our appreciation to study participants for their kind support during data collection time.
References
1. Benjamins JS, Migliorati F, Dekker K, Wassing R, Moens S, Blanken TF, et al. Insomnia heterogeneity: characteristics to consider for data-driven multivariate subtyping. Sleep Med Rev. (2017) 36:71–81. doi: 10.1016/j.smrv.2016.10.005
2. Recommended Amount of Sleep for a Healthy Adult: a joint consensus statement of the american academy of sleep medicine and sleep research society. Sleep. 2015 38:843–4. doi: 10.5665/sleep.4716
3. Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. (2008) 9:S10–7. doi: 10.1016/S1389-9457(08)70011-X
4. Tang J, Liao Y, Kelly BC, Xie L, Xiang YT, Qi C, et al. Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan Province of China. Sci Rep. (2017) 7:43690. doi: 10.1038/srep43690
5. Amaral O, Pereira C, Veiga N, Coutinho E, Chaves C. Gender and age differences in the sleep habits : a cross-sectional study in adolescents. Atención Primaria. (2016) 48:178–82.
6. Morssinkhof MWL, van Wylick DW, Priester-Vink S, van der Werf YD, den Heijer M, van den Heuvel OA, et al. Associations between sex hormones, sleep problems and depression: a systematic review. Neurosci Biobehav Rev. (2020) 118:669–80. doi: 10.1016/j.neubiorev.2020.08.006
7. Labyak S, Lava S, Turek F, Zee P. Effects of shiftwork on sleep and menstrual function in nurses. Health Care Women Int. (2002) 23:703–14. doi: 10.1080/07399330290107449
8. Mahoney MM. Shift work, jet lag, and female reproduction. Int J Endocrinol. (2010) 2010:813764. doi: 10.1155/2010/813764
9. Nowakowski S, Meers J, Heimbach E. Sleep and women's health. Sleep Med Res. (2013) 4:1–22. doi: 10.17241/smr.2013.4.1.1
10. Kloss JD, Perlis ML, Zamzow JA, Culnan EJ, Gracia CR. Sleep, sleep disturbance, and fertility in women. Sleep Med Rev. (2015) 22:78–87. doi: 10.1016/j.smrv.2014.10.005
11. Lateef OM, Akintubosun MO. Sleep and Reproductive Health. J Circadian Rhythms. (2020) 18:1. doi: 10.5334/jcr.190
12. Young DR, Sidell MA, Grandner MA, Koebnick C, Troxel W. Dietary behaviors and poor sleep quality among young adult women: watch that sugary caffeine! Sleep Heal. (2020) 6:214–9. doi: 10.1016/j.sleh.2019.12.006
13. Kim K, Lee H, Hong JP, Cho MJ, Fava M, Mischoulon D, et al. Poor sleep quality and suicide attempt among adults with internet addiction: a nationwide community sample of Korea. PLoS ONE. (2017) 12:e0174619. doi: 10.1371/journal.pone.0174619
14. Khadka R, Hong SA, Chang YS. Prevalence and determinants of poor sleep quality and depression among postpartum women: a community-based study in Ramechhap district, Nepal. Int Health. (2020) 12:125–31. doi: 10.1093/inthealth/ihz032
15. Kachikis AB, Breitkopf CR. Predictors of sleep characteristics among women in Southeast Texas. Women's Heal Issues. (2012) 22:e99–109. doi: 10.1016/j.whi.2011.07.004
16. Vézina-Im LA, Lebel A, Gagnon P, Nicklas TA, Baranowski T. Association between sleep and overweight/obesity among women of childbearing age in Canada. Can J Public Health. (2018) 109:516–26. doi: 10.17269/s41997-018-0071-4
17. Sezgin AU, Punamäki RL. Impacts of early marriage and adolescent pregnancy on mental and somatic health: the role of partner violence. Arch Womens Ment Health. (2020) 23:155–66. doi: 10.1007/s00737-019-00960-w
18. Yang Y, Li W, Ma TJ, Zhang L, Hall BJ, Ungvari GS, et al. Prevalence of poor sleep quality in perinatal and postnatal women: a comprehensive meta-analysis of observational studies. Front Psychiatry. (2020) 11:161. doi: 10.3389/fpsyt.2020.00161
19. Yu Y, Zhu X, Xu H, Hu Z, Zhou W, Zheng B, et al. Prevalence of depression symptoms and its influencing factors among pregnant women in late pregnancy in urban areas of Hengyang City, Hunan Province, China: a cross-sectional study. BMJ Open. (2020) 10:e038511. doi: 10.1136/bmjopen-2020-038511
20. Christian LM, Carroll JE, Porter K, Hall MH. Sleep quality across pregnancy and postpartum: effects of parity and race. Sleep Heal. (2019) 5:327–34. doi: 10.1016/j.sleh.2019.03.005
21. Iranpour S, Kheirabadi GR, Esmaillzadeh A, Heidari-Beni M, Maracy MR. Association between sleep quality and postpartum depression. J Res Med Sci. (2016) 21:110. doi: 10.4103/1735-1995.193500
22. Salarinia F, Bani S, Jafarabadi MA, Hasanpoor S, Abasalizadeh S, Ansari K. Women on the between other side of war and poverty : its effect and relationship sleep quality and overweight on the health of reproduction obesity in women of reproductive age referred to health centers in Yazd. Aras Part Med Int Press. (2017) 5:231–6. doi: 10.15296/ijwhr.2017.41
23. Cattane N, Räikkönen K, Anniverno R, Mencacci C, Riva MA, Pariante CM, et al. Depression, obesity and their comorbidity during pregnancy: effects on the offspring's mental and physical health. Mol Psychiatry. (2021) 26:462–81. doi: 10.1038/s41380-020-0813-6
24. Moradi S, Zobeiri M, Feizi A, Clark CCT, Entezari MH. The effects of spirulina (Arthrospira platensis) supplementation on anthropometric indices, blood pressure, sleep quality, mental health, fatigue status and quality of life in patients with ulcerative colitis: A randomised, double-blinded, placebo-control. Int J Clin Pract. (2021) 75:e14472. doi: 10.1111/ijcp.14472
25. Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthc (Basel, Switzerland). (2018) 7:1. doi: 10.3390/healthcare7010001
26. Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. (2017) 9:151–61. doi: 10.2147/NSS.S134864
27. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
28. Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. (2021) 18:1082. doi: 10.3390/ijerph18031082
29. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 4, Functional and Economic Impact of Sleep Loss and Sleep-Related Disorders. Available online at: https://www.ncbi.nlm.nih.gov/books/NB (accessed May 26, 2022).
30. Yang Y, Mao J, Ye Z, Zeng X, Zhao H, Liu Y, et al. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J Matern Neonatal Med. (2018) 31:2980–5. doi: 10.1080/14767058.2017.1359831
31. Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest. (2018) 154:196–206. doi: 10.1016/j.chest.2018.04.005
32. Manzar MD, Bekele BB, Noohu MM, Salahuddin M, Albougami A, Spence DW, et al. Prevalence of poor sleep quality in the Ethiopian population: a systematic review and meta-analysis. Sleep Breath. (2020) 24:709–16. doi: 10.1007/s11325-019-01871-x
33. Jemere T, Getahun B, Tadele F, Kefale B, Walle G. Poor sleep quality and its associated factors among pregnant women in Northern Ethiopia, 2020: a cross sectional study. PLoS ONE. (2021) 16:e0250985. doi: 10.1371/journal.pone.0250985
34. Wondie T, Molla A, Mulat H, Damene W, Bekele M, Madoro D, et al. Magnitude and correlates of sleep quality among undergraduate medical students in Ethiopia: cross –sectional study. Sleep Sci Pract. (2021) 5:7. doi: 10.1186/s41606-021-00058-2
35. Belete H, Misgan E. Determinants of Insomnia among Mothers during Postpartum Period in Northwest Ethiopia. Sleep Disord. (2019) 2019:3157637. doi: 10.1155/2019/3157637
36. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210:653–61. doi: 10.1016/j.psychres.2013.07.015
37. Yosef T, Getachew D, Bogale B, Wondimu W, Shifera N, Negesse Y, et al. Psychoactive substance use and its associated factors among truck drivers in Ethiopia. Biomed Res Int. (2021) 2021:1604245. doi: 10.1155/2021/1604245
38. Lee MH, Kim JW, Lee JH, Kim DM. The standardization of the shortened premenstrual assessment form and applicability on the internet. J Korean Neuropsychiatr Assoc. (2002) 41:159–67.
39. Bhuvaneswari K, Rabindran P, Bharadwaj B. Prevalence of premenstrual syndrome and its impact on quality of life among selected college students in Puducherry. Natl Med J India. (2019) 32:17–9. doi: 10.4103/0970-258X.272109
40. Hachul H, Bisse AR, Sanchez ZM, Araujo F, Guazzelli CAF, Tufik S, et al. Sleep quality in women who use different contraceptive methods. Sleep Sci. (2020) 13:131–7. doi: 10.5935/1984-0063.20190142
41. Pérez-Carbonell L, Meurling IJ, Wassermann D, Gnoni V, Leschziner G, Weighall A, et al. Impact of the novel coronavirus (COVID-19) pandemic on sleep. J Thorac Dis. (2020) 12:S163–75. doi: 10.21037/jtd-cus-2020-015
42. Guo J, Yang L, Xu Y, Zhang C, Luo X, Liu S, et al. Prevalence and risk factors associated with insomnia symptoms among the chinese general public after the coronavirus disease 2019 epidemic was initially controlled. Nat Sci Sleep. (2021) 13:703–12. doi: 10.2147/NSS.S307996
43. Phelan N, Behan LA, Owens L. The impact of the COVID-19 pandemic on women's reproductive health. Front Endocrinol (Lausanne). (2021) 12:642755. doi: 10.3389/fendo.2021.642755
44. Amare NS, Chekol B, Aemro A. Determinants of poor sleep quality during the COVID-19 pandemic among women attending antenatal care services at the health facilities of Debre Berhan Town, Ethiopia: an institutional-based cross-sectional study. Frontiers in Psychiatry. (2022) 13:841097. doi: 10.3389/fpsyt.2022.841097
45. Oh CM, Kim HY, Na HK, Cho KH, Chu MK. The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: a population-based study. Front Neurol. (2019) 10:849. doi: 10.3389/fneur.2019.00849
46. Gupta R, Dahiya S, Bhatia MS. Effect of depression on sleep: qualitative or quantitative? Indian J Psychiatry. (2009) 51:117–21. doi: 10.4103/0019-5545.49451
47. Sivertsen B, Skogen JC, Jakobsen R, Hysing M. Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug Alcohol Depend. (2015) 149:180–6. doi: 10.1016/j.drugalcdep.2015.01.045
48. Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcohol Clin Exp Res. (2015) 39:355–62. doi: 10.1111/acer.12618
49. Tai SY, Wang WF, Yang YH. Current status of sleep quality in Taiwan: a nationwide walk-in survey. Ann Gen Psychiatry. (2015) 14:36. doi: 10.1186/s12991-015-0078-7
50. Jones HJ, Zak R, Lee KA. Sleep disturbances in midlife women at the cusp of the menopausal transition. J Clin Sleep Med. (2018) 14:1127–33. doi: 10.5664/jcsm.7208
51. Song L, Lei J, Jiang K, Lei Y, Tang Y, Zhu J, et al. The association between subclinical hypothyroidism and sleep quality: a population-based study. Risk Manag Healthc Policy. (2019) 12:369–74. doi: 10.2147/RMHP.S234552
52. Kim W, Lee J, Ha J, Jo K, Lim DJ, Lee JM, et al. Association between sleep duration and subclinical thyroid dysfunction based on nationally representative data. J Clin Med. (2019) 8:2010. doi: 10.3390/jcm8112010
53. Green ME, Bernet V, Cheung J. Thyroid dysfunction and sleep disorders. Front Endocrinol (Lausanne). (2021) 12:725829. doi: 10.3389/fendo.2021.725829
54. Hasler BP, Smith LJ, Cousins JC, Bootzin RR. Circadian rhythms, sleep, and substance abuse. Sleep Med Rev. (2012) 16:67–81. doi: 10.1016/j.smrv.2011.03.004
55. Aşci Ö, Gökdemir F, Kahyaoglu Süt H, Payam F. The relationship of premenstrual syndrome symptoms with menstrual attitude and sleep quality in turkish nursing student. J Caring Sci. (2015) 4:179–87. doi: 10.15171/jcs.2015.018
56. Lin PC, Ko CH, Lin YJ, Yen JY. Insomnia, inattention and fatigue symptoms of women with premenstrual dysphoric disorder. Inte J Environ Res Public Health. (2021) 18:6192. doi: 10.3390/ijerph18126192
Keywords: poor sleep quality, reproductive age group women, Mizan Aman, Ethiopia, factors
Citation: Bogale B, Wolde A, Mohammed N, Midaksa G and Bekele BB (2022) Poor Sleep Quality and Factors Among Reproductive-Age Women in Southwest Ethiopia. Front. Psychiatry 13:913821. doi: 10.3389/fpsyt.2022.913821
Received: 06 April 2022; Accepted: 17 June 2022;
Published: 13 July 2022.
Edited by:
Fortunato Battaglia, Hackensack Meridian School of Medicine, United StatesReviewed by:
Firanbon Teshome, Jimma University, EthiopiaTadeg Jemere, Debre Tabor University, Ethiopia
Elias Amaje, Bule Hora University, Ethiopia
Carmen Concerto, University of Catania, Italy
Tamirat Melis, Wolkite University, Ethiopia
Tamrat Anbesaw, Wollo University, Ethiopia
Copyright © 2022 Bogale, Wolde, Mohammed, Midaksa and Bekele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biruk Bogale, YnVyYWJvZ2FsZUBnbWFpbC5jb20=; YmlydWtAbXR1LmVkdS5ldA==
 Biruk Bogale
Biruk Bogale Asrat Wolde2
Asrat Wolde2 Nuredin Mohammed
Nuredin Mohammed Gachana Midaksa
Gachana Midaksa Bayu Begashaw Bekele
Bayu Begashaw Bekele