- 1Psychiatric Department, Research Center for Addiction and Risky Behaviors, Iran University of Medical Sciences, Tehran, Iran
- 2Department for Mental Health and Substance Abuse, Ministry of Health and Medical Education, Tehran, Iran
- 3University Counselling Center, Shahed University, Tehran, Iran
- 4Non-communicable Diseases Research Center, Endocrinology and Metabolism Research Institute, Tehran University of Medical Sciences, Tehran, Iran
- 5Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Introduction: The COVID-19 pandemic has caused increasing levels of mental health problems such as anxiety and depression among doctors, nurses and other healthcare workers in hospitals or health centers. The main objective of this study was to assess the mental health, job stressors, and burnout among healthcare workers in Iran.
Materials and Methods: A cross-sectional study was performed in the primary healthcare centers and hospitals affiliated with six of the medical universities in Iran. The selection of participants was done using multi-center convenient sampling. The Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, and Copenhagen Burnout Inventory were used for gathering data through an online platform. Data related to job stressors were obtained using a validated checklist. Data analysis was performed using Chi-square and multiple regression tests and the phi coefficient.
Results: The results of our study showed that 53% of the healthcare workers of the hospitals and primary healthcare centers enrolled in our study either had generalized anxiety disorder or major depressive disorder or both disorders. Moderate and high levels of burnout were seen among 48.9% of the study participants. The prevalence of mental disorders and burnout were significantly higher among the female healthcare workers compared to the male (p = 0.0001) and a higher rate of mental disorder and burnout was also seen among healthcare workers of hospitals compared to those working in primary healthcare centers (p = 0.024). “Worry about children and old members of family,” “family worries for my health condition” and “lack of specific effective treatment for COVID-19” were found to be predictive of mental disorder and burnout. The most prevalent job stressor among the total sample was “low payment or income during the COVID-19 period”.
Conclusion: The results of our study revealed high psychological distress and burnout among healthcare workers of the hospitals during the fourth peak of the COVID-19 pandemic in Iran. This study highlights the need for health officials to pay attention to the job stressors of healthcare workers and obliges them to perform effective interventions to address their needs and concerns.
Introduction
The World Health Organization (WHO) declared the SARS-Cov-2 outbreak as a pandemic on March 11th 2020 (1). Until March 2022, which is the time of inscribing this article, the COVID-19 cases worldwide have surpassed 445 million and there have been more than 6 million COVID-19 reported deaths confirmed globally (2). The uncontrollable nature of COVID-19 has posed remarkable challenges to the health care systems in most of the nations affected (3). Some countries have reported temporary shortage of health care providers and/or health equipment and supply in the midst of the peaks of the pandemic (4). Other than that, the current pandemic has caused increasing levels of mental health problems such as anxiety and depression among doctors, nurses and other healthcare workers in hospitals or health centers (5). As reported, many health personnel have lost their lives due to COVID-19 and many of them have been infected with the virus or transferred the illness to their family members (6).
Pandemics such as the COVID-19 provoke fear and anxiety, which is common among healthcare workers who are directly involved in the management of ill patients. The healthcare workers' exposure to patients' suffering and deaths (7) also increases their fear and anxiety. Unattended anxiety negatively impacts work performance and job satisfaction of health personnel, leading to frequent absenteeism and eventual turnover (8). Available data suggest that the prevalence of anxiety and depression among health care workers during the COVID-19 pandemic ranged from 22.6% (9) to 47% (10) and 22.8% (7) to 50.4% (11) respectively. The prevalence of burnout among healthcare workers in the COVID-19 has also been frequently studied in different regions and countries and high-level burnout rates of 49.3% (12) and 50% (13), to more than 60% (14) and even 67% (15) have been reported among healthcare workers in the COVID-19 pandemic. Studies have also shown high rates of anxiety and depression among Iranian healthcare workers in the COVID-19 pandemic (16–18), especially among the female (19). Iranian studies have shown negative psychological experiences caused by COVID-19 in healthcare workers, such as fatigue, discomfort, and helplessness due to high-intensity work, anxiety, and worry about family members (20). An Iranian study performed by Jalili et al. (21) have reported high levels of burnout among 53% of the healthcare workers in the COVID-19 pandemic.
Studies have defined variable psychosocial stressors that the COVID-19 pandemic has brought about and led to exceeding levels of psychological distress (22), mental health problems such as anxiety and depression (23), and burnout (5, 24–26) among healthcare personnel worldwide.
Throughout the COVID-19 pandemic, frontline healthcare workers have been facing the fear of infection of themselves or their families and dealt with considerable initial uncertainty about disease standard treatment regimens (27). They have also been faced with complex ethical issues in practice, and frustrated by moral conflicts (28). Excessive workloads, long working hours, lack of enough time for recovery, insufficient personal protective equipment at the beginning of the pandemic, not being able to tell their manager if they are not coping (29), and inadequate hospital facilities for the patients are all important factors that have put them under persistent pressure and sometimes affected the quality of patient care (10).
Several psychosocial and demographic variables like gender, age, profession, place of work, family income (30), and risk factors such as poor social support, low senses of self-efficacy, and experiencing stigma (22) are associated with increased stress, anxiety and depressive symptoms and burnout (31) among healthcare workers during the COVID-19 pandemic (32). For instance, some studies convey that being a woman (33), having a younger age, being the parents of dependent children (34), and working in high-risk areas may have more negative psychological health outcomes (11). This reality is even more negative in the case of nurses due to the high emotional burden of continued contact with patients' suffering and pain (35).
The main objective of this study was to assess the prevalence of depression, anxiety and burnout among Iranian healthcare workers of the PHC system and hospitals in the COVID-19 pandemic. This is the first large-scale multi-provincial study performed for assessing burnout and adverse mental health effects of the COVID-19 pandemic on a heterogeneous group of healthcare workers in Iran.
Materials and Methods
Study Design and Settings
A cross-sectional study was performed in the primary healthcare centers and hospitals affiliated with six medical universities located in the provinces of Tehran, Tabriz, Gilan, Ahvaz, Ghom, and Kurdistan of Iran. The medical universities were selected based on their geographical diversity and the capacity of their primary healthcare centers for providing services. In each university, one hospital and five primary healthcare centers were chosen for performing the study.
Study Participants
The target population in this study included physicians, nurses, dentists, mental health workers, environmental and occupational health workers, community health workers, medical technicians, and staff members working in hospitals and primary healthcare centers. The samples size was calculated to be 1,055. We considered a sample size which was 10% larger to cover possible drop-out of participants and ultimately came up with an approximate number of 1,170 participant. According to probability-proportional-to-size sampling (36), 120 individuals were selected from each hospital, making a total of 720 participants from the hospital setting and 15 individuals were selected for each PHC center, making a total of 450 participants from primary healthcare centers to cover different job categories. The selection of participants was done using multi-center convenient sampling. Any healthcare worker working at hospitals or PHC centers at the time of the study, working at least between 44 and 50 h a week was recognized eligible to receive the questionnaire link and was asked to respond to all of the questions in the time period announced, and therefore was initially enrolled in the study. Only one reminder was performed 2 weeks after the initial call for participation. At the end of the data gathering process, 37 participants who had missing demographic data or had not filled out one or more of the questionnaires were excluded from the study and 1,133 participants remained.
Study Instruments
Demographic data were obtained in the beginning of the questionnaire. Data related to job stressors were obtained using a checklist which was developed after thorough literature and desk review and finalized after performing individual deep interviews with experts and focus group discussions (FGD) with members of each of the target groups. We initially came up with a job stress checklist of 80 items. Content validity of all items was measured with the consultation of 10 experts and items with a CVR of lower than 0.75 (37) and an I-CVI of lower than 0.78 (38) were excluded from the checklist, and so the final checklist was consisted of 65 items. For identifying the top ten stressor as selected by the participants, all of the 65 stressors were presented to the participants in the online questionnaire and participants were asked to score the importance of each stressor on a 5-point Likert scale.
Data related to the study variables, burnout, and mental health status were obtained using online validated questionnaires, as follows:
Patient Health Questionnaire-9
The PHQ-9 (39) is a nine-item instrument designed for detecting major depressive disorder (MDD) based on the fourth version of the Diagnostic and Statistical Manual of Mental disorders (DSM-IV) (40). The internal reliability of the PHQ-9 was excellent, with a Cronbach's α of 0.89 in the PHQ Primary Care Study (39). Scores are calculated based on how frequently a person experiences the mentioned feelings. In scoring, each “not at all” response is scored as 0; each “several days” response is 1; each “more than half the days” response is 2; and each “nearly every day” response is 3 (39). Therefore, scores range from 0 to 27 with higher scores indicating more severe MDD symptoms. The PHQ-9 has been validated for use among the Iranian population with a Cronbach's α of 0.856 (41) and a cut-off score of 13 which provided an optimal balance between sensitivity and specificity (42).
Generalized Anxiety Disorder-7
The GAD-7 (43) is a seven-item self-report scale developed for the diagnosis of generalized anxiety disorder (GAD) according to the DSM-IV. The GAD-7 score is calculated by assigning scores of 0, 1, 2, and 3, to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day”. Scores range from 0 to 21 with higher scores indicating more severe GAD symptoms (43). The GAD-7 has been validated to use among the Iranian population with an α Cronbach value of 0.88 and a cut-off point of 10 for diagnosing GAD (44).
Copenhagen Burnout Inventory
The CBI (45) was used to measure the fatigue and exhaustion as core constructs of burnout among participants. This 19-item questionnaire measures three burnout sub-dimensions: personal burnout (6 items), work-related burnout (7 items), and client-related burnout (6 items). Each item is scored by the participant on a 5-point Likert scale. Scores fall into the four categories of “no burnout” (0–25), “mild burnout” (25.1–50), “moderate burnout” (50.1–75), “high burnout” (75.1–99). Separate scores can be reported for each sub-dimension and the total score of the test is the mean score of all three sub-dimensions (46). The original version of the instrument had presented a good internal consistency for all three subscales: personal burnout (α = 0.87), work related burnout (α = 0.87), and client-related burnout (α = 0.85). The internal consistency of the Persian version ranged from a Cronbach's α of 0.82 to 0.90 and the test-retest reliability was excellent with the ICC ranging from 0.85 to 0.95 (47).
Procedure
In each university, the director of the mental health department was the coordinator of the project. Project managers were appointed for each of the hospitals for coordination and monitoring of the process of data collection. The project coordinators and managers were trained through a 1-day training session and were instructed on the sampling method, research design and assessment tools. A detailed guideline on the aim of the study and the methodology including number of participants needed for each job category were also sent to them via electronic mail. Participants were chosen by the project coordinator and project managers by convenient sampling. The PORS-LINE platform was used for gathering data. The link of the questionnaire was sent to each participant and they were asked to fill out the questionnaire from June 23rd 2021 to July 18th 2021. It is worth mentioning that this study was performed in the fourth peak of COVID-19 in Iran which was simultaneous with the peaks in India and Brazil (48).
Data Analysis
Data entry and analysis was performed with the SPSS V.23 software. We used descriptive analysis using one and two-variable frequency tables for displaying numbers, percentages and frequencies. Chi-square tests were used for qualitative variables, and the phi coefficient was used for two-state variables and multiple regression tests were used for continuous quantitative variables.
Results
Demographic Data
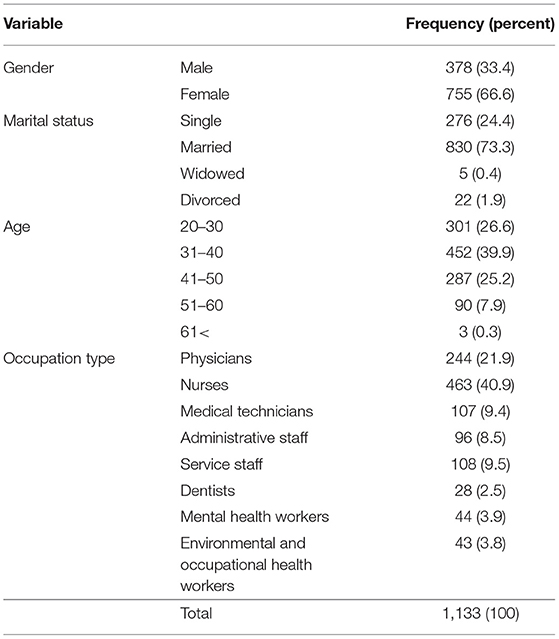
At the end of the deadline of data gathering, 37 questionnaires were excluded from the study because the participant had not filled out some of the questionnaires, and we ultimately had 1,133 completed questionnaires from 1,133 participants. Among these, 755 (66.6%) were female. The majority (66.5%) of the participants were aged 20 to 40 and were married (73.3%). Participants were consisted of physicians, nurses and other workers and staff members from which 715 (63.1%) of them worked at hospitals. The largest group regarding occupation were the nurses with 41 percent of the participants (see Table 1).
Job Stressors
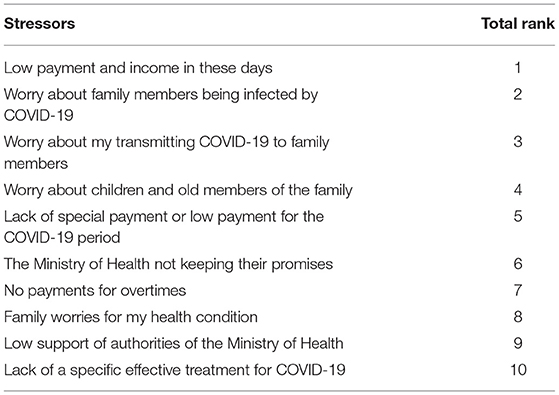
The most prevalent job stressor among the total sample was “low payment or income during the COVID-19 period,” and “worry about family members being infected by COVID-19,” “worry about my transmitting COVID-19 to family members,” and “worry about children and old members of the family” came afterwards (see Table 2).
Mental Disorder
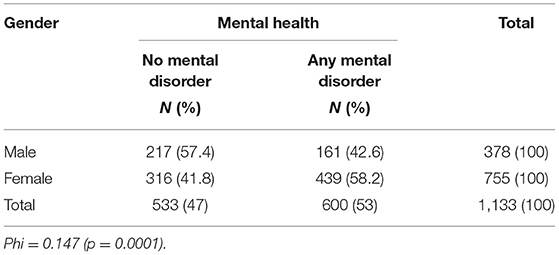
The presence of generalized anxiety disorder (GAD) and major depressive disorder (MDD) among study participants was assessed with the PHQ-9 and GAD-7 tools respectively. According to the results, among the male participants, 35.7 and 30.2% and among the female participants, 53.1 and 38.9% had GAD and MDD respectively. Considering both genders, among the 1,133 participants, a total of 536 (47.3%) participants had GAD and 408 (36%) had MDD, and a total of 600 (53%) of the participants had either GAD or MDD or both of the disorders, which is referred to as “any mental disorder.” Among those with any mental disorder, 344 (30.36%) had both MDD and GAD, 192 (16.9%) had only GAD and 64 (5.6%) had only MDD. Study results showed that 58.2% of the female and 42.6% of the male participants had any mental disorder. A higher rate of mental disorder among the female compared to the male participants was statistically significant (p = 0.0001) (see Table 3).
Regarding workplace, a total of 397 participants (55.5%) of those working in hospitals and 203 (48.6%) of those working in PHC centers had any mental disorder. The higher rate of mental disorders of the healthcare workers in the hospitals was statistically significant (p = 0.024).
Burnout
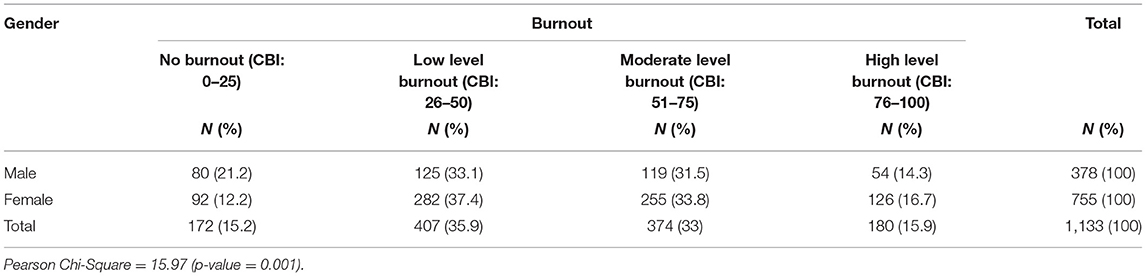
According to the results, among the 1,133 participants, a total of 554 (48.9%) participants had moderate and high level burnout (36%). Also, study results showed that 381 (50.5%) of the female and 173 (45.8%) of the male participants had moderate and high level burnout. A higher rate of burnout among the female compared to the male participants was statistically significant (p = 0.001) (see Table 4). The mean score of burnout among individuals was 61.1 in the participants with any mental disorder and 37.7 in the participants without any mental disorder. This means that there is a significant relationship between the presence of anxiety and depression with burnout (p < 0.0001, t = 21.054).
Regarding workplace, a total of 375 participants (52.4%) of those working in hospitals and 179 (42.8%) of those working in PHC centers had moderate to high levels of burnout. The higher rate of burnout of the healthcare workers in the hospitals in comparison to the PHC centers was statistically significant (p = 0.011). Our findings showed a significant correlation between burnout and MDD (R = 0.64, p = 0.0001) and also between burnout and GAD (R = 0.58, p = 0.0001).
Predictors of Mental Disorder and Burnout
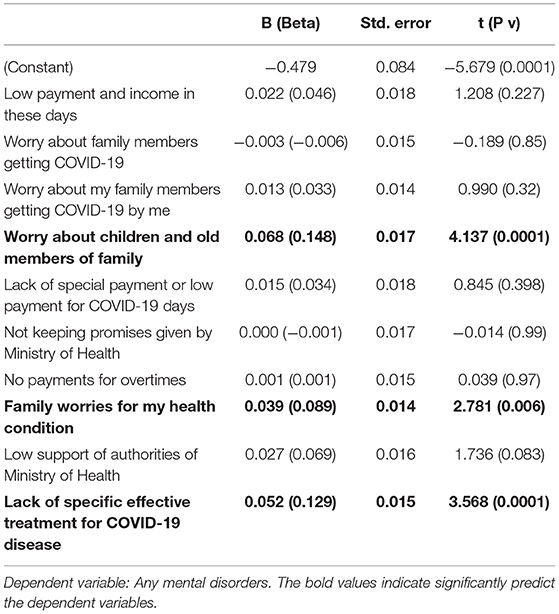
The regression performed for predicting any mental disorder based on the ten top-ranking stressors showed that the regression coefficient is equal to 0.374 and the determination coefficient (R2) is equal to 0.14. In other words, the ten stressors predicted 14 percent of any mental disorder. The F is equal to 18.27 and confirms the significance of the regression model with a 0.01 error (see Table 5).
The regression model shows that “worry about children and old members of family,” “family worries for my health condition,” “lack of specific effective treatment for COVID-19” could significantly predict the outcome of any mental disorder.
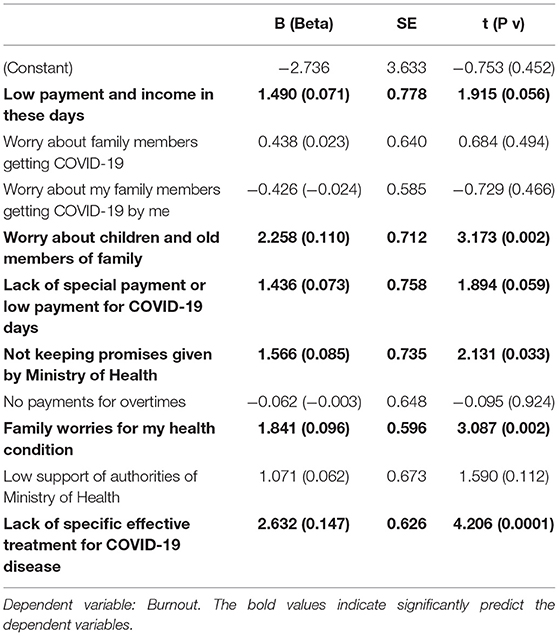
The regression performed for predicting burnout based on the ten top-rank stressors showed that the regression coefficient (R) was 0.437 and the determination coefficient was (R2) 0.19. Therefore, the top ten stressors were able to predict 19 percent of the outcome of burnout. The F value is equal to 26.55 and it confirms the significance of the regression model with an error of 0.01 (see Table 6).
The regression model shows that among the ten top-ranking stressors, “low payment and income,” “worry about children and old members of the family,” “lack of special payment or low payment for COVID-19 days,” “the MOH not keeping their promises,” “family worries for the individuals' health condition,” and “the lack of specific effective treatment for COVID-19” could predict burnout significantly.
For summarizing the results of the multiple regression models performed for assessing the relationship between the top ten stressors with the outcomes of any mental disorder and burnout, Table 7 is presented. In this table, the job stressors which could significantly predict the outcomes are bolded. As is seen, “worry about children and old members of family,” “family worries for my health condition” and “lack of specific effective treatment for COVID-19” are the three job stressors that could significantly predict both of the two outcomes of mental disorder and burnout (see Table 7).
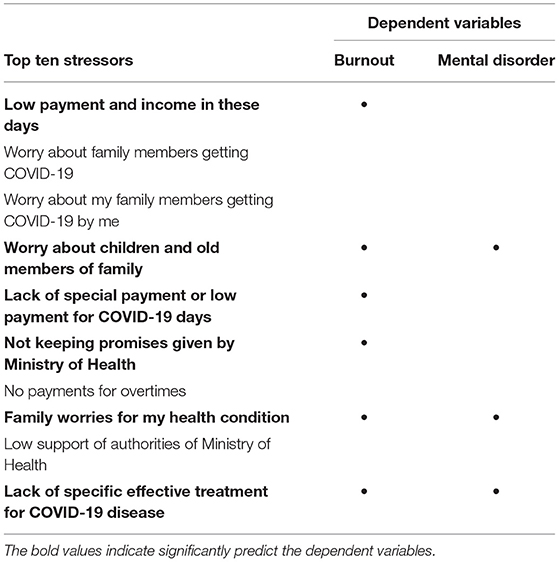
Table 7. Summary of multiple regression analysis for top ten stressors predicting dependent variables.
Discussion
Our study shows a higher than 50% prevalence of mental disorders among healthcare workers of hospitals and PHC centers in the midst of one of the deadliest COVID-19 pandemic peaks in Iran. This reported prevalence is higher than that of the general population which has been reported to be 29.7% in the same time period (49). This finding is similar to a number of international (7, 9–11) and national (16–20) studies conducted at the time of the COVID-19 pandemic for assessing psychological distress and mental health problems among healthcare workers which have reported a high prevalence of anxiety and depression. One similar study performed a year earlier among healthcare workers from twelve different cities in India revealed that 52.9% of the participants had the risk of psychological distress that needed further evaluation (50). The higher prevalence of mental disorders among female healthcare workers found in our study has also been replicated in many studies (51–55). Results also showed a raised prevalence ratio of female/male regarding GAD and a decreased prevalence ratio of female/male regarding MDD among the healthcare workers compared to previous population studies (56).
Moderate to severe levels of burnout have been seen among nearly half of our study participants, mostly reported in healthcare workers of hospitals. Our findings are similar to findings of other studies assessing burnout levels among health care workers in the COVID-19 pandemic (12–14), one study even showing a burnout prevalence of 67% (15). Alrawashdeh et al. (33) showed in their study which was performed among physicians that several significant factors were positively associated with burnout, including female gender, working at highly loaded hospitals, working for long hours, doing night shifts, and lack of sufficient access to personal protective equipment. Regarding the fact that the further mentioned risk factors for burnout are usually mostly relevant to hospitals and not outpatient centers, we can perhaps conclude that the higher prevalence of burnout in hospitals found in our study can be rationalized. Results of one study showed a significant association of depression, anxiety and stress with cumulative psychological burnout, consistent with our study results (57).
The most prevalent job stressor reported by the participants of our study was low payment and income in the COVID-19 days. Concerning the role of the sufficiency of the income for family needs, Tarcan et al. (58) suggest that higher income tended to be related with better health status and with lower burnout levels, both for general physicians and nurses. Several authors have identified a relationship between better payment or income earned and higher job satisfaction, which in turn decreases burnout level (59–61). Despite this general view, one study (62) did not find such relation between payment and burnout syndrome and Linzer et al. (63) even concluded that the relevant factor for physicians was rather the relationship with patients than the monetary compensation.
Our study findings have shown that the three factors of “worry about children and old members of the family,” “family worries for my health condition,” and “lack of a specific effective treatment for COVID-19” can significantly predict the severity of the two outcomes of mental disorder and burnout. Concerns about personal and family health (64) and fear for personal and family safety had (65) also been reported among healthcare workers throughout different epidemics such as the SARS and MERS. Worry about children among the healthcare workers in the COVID-19 pandemic has been stated in other studies, especially among nurses who have been distanced from their children for a while (66). One study in the United States also showed that it was most stressful for healthcare workers to think they could transmit the disease to their family and friends (67). This finding has also been replicated in many other studies (8, 10, 23). Results of other studies have also revealed more psychological stress among married healthcare workers and those having children (68, 69), possibly resembling the concern these individuals have about the health of their family members.
Conducting this study during the ongoing outbreak of COVID-19 and in the midst of one of the worst pandemic peaks in Iran imposed methodological limitations for our study. The main one was that an online platform was selected for gathering data from the participants in order to minimize human encountering. This prevented the researchers to select a specific time, place and circumstance for meeting the participants and filling out the questionnaires, which could have enhanced the quality of the data gathering. Convenient sampling also limits the generalizability of our results due to possible under-representation of the study sample as a whole.
One of the main strength points of this study is that the researchers managed to reach out to a great number of healthcare workers in six provinces in different geographical zones in the country. Another strength point was that a holistic approach was adopted and different types of healthcare workers and health staff who worked in hospitals and PHC centers were selected for enrollment in the study. Standard tools have been used for assessing mental disorders and burnout among the participants in this study which enables comparison with the results of other studies of this kind.
Conclusion
The results of our study revealed high psychological distress and burnout among healthcare workers of the hospitals during the fourth peak of the COVID-19 pandemic in Iran. Higher levels of distress among female healthcare workers and those working in hospitals as seen in many other studies should be an area of special consideration and special interventions should be conducted in this regard. Burnout among healthcare workers may lead to lower quality of care for the patients and increase the probability of medical mismanagement, which is a critical issue regarding the fact that the health system is faced with shortage of human resources and high workload due to the COVID-19 pandemic. This study highlights the need for health officials to pay attention to the stressing effect of low payment and also the fear and concerns of healthcare workers about personal and family safety in the COVID-19 pandemic and obliges them to perform effective interventions to address their needs and concerns.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of Iran University of Medical Sciences. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AhH and FT have contributed in conducting the research. MZ has performed the data analysis. AhH, MA, FT, AmH, and MZ have contributed to inscribing the main body of the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. (2020). Available online at: https://www.who.int/dg/speeches/detail (accessed June 03, 2022).
2. Worldometer. Coronavirus Cases. (2021). Available online at: www.worldometers.info/coronavirus (accessed June 03, 2022).
3. Silva SJRD, Pena L. Collapse of the public health system and the emergence of new variants during the second wave of the COVID-19 pandemic in Brazil. One Health. (2021) 13:100287. doi: 10.1016/j.onehlt.2021.100287
4. Bong CL, Brasher C, Chikumba E, McDougall R, Mellin-Olsen J, Enright A. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. (2020) 131:86–92. doi: 10.1213/ANE.0000000000004846
5. Hall H. The effect of the COVID-19 pandemic on healthcare workers' mental health. JAAPA. (2020) 33:45–8. doi: 10.1097/01.JAA.0000669772.78848.8c
6. World Health Organization. The Impact of COVID-19 on Health and Care Workers: A Closer Look at Deaths. Health Workforce Department -Working Paper 1. Geneva: World Health Organization (WHO/HWF/WorkingPaper/2021.1) (2021). Available online at: https://apps.who.int/iris/handle/10665/345300 (accessed August 02, 2022).
7. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
8. Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J Nurs Manag. (2020) 28:1653–61. doi: 10.1111/jonm.13121
9. Sanghera J, Pattani N, Hashmi Y, Varley KF, Cheruvu MS, Bradley A, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. (2020) 62:e12175. doi: 10.1002/1348-9585.12175
10. Greene T, Harju-Seppänen J, Adeniji M, Steel C, Grey N, Brewin CR, et al. Predictors and rates of PTSD, depression and anxiety in UK frontline health and social care workers during COVID-19. Eur J Psychotraumatol. (2021) 12:1882781. doi: 10.1080/20008198.2021.1882781
11. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
12. Chor WP, Ng WM, Cheng L, Situ W, Chong JW, Ng LY, et al. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: a multi-center study. Am J Emerg Med. (2021) 46:700–2. doi: 10.1016/j.ajem.2020.10.040
13. Nishimura Y, Miyoshi T, Hagiya H, Kosaki Y, Otsuka F. Burnout of healthcare workers amid the COVID-19 pandemic: a Japanese cross-sectional survey. Int J Environ Res Public Health. (2021) 18:2434. doi: 10.3390/ijerph18052434
14. Maunder RG, Heeney ND, Strudwick G, Danielle Shin H, O'Neill B, Young N. Burnout in hospital-based healthcare workers during COVID-19. Sci Briefs Ontario COVID-19 Sci Advis Table. (2021) 2:46. doi: 10.47326/ocsat.2021.02.46.1.0
15. Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. (2021). Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS ONE 16:e0238666. doi: 10.1371/journal.pone.0238666
16. Zakeri MA, Dehghan M, Ghaedi-Heidari F, Zakeri M, Bazmandegan G. Chronic patients' activation and its association with stress, anxiety, depression, and quality of life: a survey in southeast Iran. Front Neurosci. (2021) 15:6614566. doi: 10.1155/2021/6614566
17. Zakeri MA, Rahiminezhad E, Salehi F, Ganjeh H, Dehghan M. Burnout, anxiety, stress, and depression among Iranian nurses: before and during the first wave of the COVID-19 pandemic. Front Psychol. (2021) 12:789737. doi: 10.3389/fpsyg.2021.789737
18. Rouhbakhsh A, Arbabi M, Nejatisafa A, Sharafi S, Etesam F, Shahmansouri N, et al. Mental health of health care workers at Imam Khomeini Hospital in Tehran during COVID-19 pandemic. J Iran Med Council. (2021) 4:209–20. doi: 10.18502/jimc.v4i4.8468
19. Mohamadzadeh Tabrizi Z, Mohammadzadeh F, Davarinia Motlagh Quchan A, et al. COVID-19 anxiety and quality of life among Iranian nurses. BMC Nurs. (2022) 21:27. doi: 10.1186/s12912-021-00800-2
20. Bahrami Moghadam H, Khedri R, Forouzan A, Maniati M, Amini P, Delirrooyfard A, et al. The deadly nature of the virus depression: iranian medical staff battling COVID-19. EBHPME. (2021) 5:234–43. doi: 10.18502/jebhpme.v5i4.8158
21. Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. (2021) 94:1345–52. doi: 10.1007/s00420-021-01695-x
22. Huo L, Zhou Y, Li S, Ning Y, Zeng L, Liu Z, et al. Burnout and its relationship with depressive symptoms in medical staff during the COVID-19 epidemic in China. Front Psychol. (2021) 12:616369. doi: 10.3389/fpsyg.2021.616369
23. Labrague LJ, de Los Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. (2021) 29:395–403. doi: 10.1111/jonm.13168
24. Manzano García G, Ayala Calvo JC. The threat of COVID-19 and its influence on nursing staff burnout. J Adv Nurs. (2021) 77:832–44. doi: 10.1111/jan.14642
25. Murat M, Köse S, Savaşer S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30:533–43. doi: 10.1111/inm.12818
26. Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, et al. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J Am Med Dir Assoc. (2020) 21:1751–1758.e5. doi: 10.1016/j.jamda.2020.09.035
27. Suñer-Soler R, Grau-Martín A, Flichtentrei D, Prats M, Braga F, Font-Mayolas S, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burnout Res. (2014) 1:82–89. doi: 10.1016/j.burn.2014.07.004
28. Nyashanu M, Pfende F, Ekpenyong M. Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region, UK. J Interprof Care. (2020) 34:655–61. doi: 10.1080/13561820.2020.1792425
29. Turale S, Meechamnan C, Kunaviktikul W. Challenging times: ethics, nursing and the COVID-19 pandemic. Int Nurs Rev. (2020) 67:164–7. doi: 10.1111/inr.12598
30. Lee H, Cummings GG. Factors influencing job satisfaction of front-line nurse managers: a systematic review. J NursManag. (2008) 16:768–83. doi: 10.1111/j.1365-2834.2008.00879.x
31. Sirois FM, Owens J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: a rapid systematic review of the evidence. Front Psychiatry. (2021) 11:589545. doi: 10.3389/fpsyt.2020.589545
32. Spoorthy MS, Pratapa SK, Mahant SJA. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatry. (2020) 51:102119. doi: 10.1016/j.ajp.2020.102119
33. Alrawashdeh HM, Al-Tammemi AA, Alzawahreh MK, Al-Tamimi A, Elkholy M, Al Sarireh F, et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: a convergent parallel mixed-method study. BMC Public Health. (2021) 21:811. doi: 10.1186/s12889-021-10897-4
34. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. (2020) 369:m1642. doi: 10.1136/bmj.m1642
35. Molina-Praena J, Ramirez-Baena L, Gómez-Urquiza JL, Cañadas GR, De la Fuente EI, Cañadas-De la Fuente GA. Levels of burnout and risk factors in medical area nurses: a meta-analytic study. Int J Environ Res Public Health. (2018) 15:2800. doi: 10.3390/ijerph15122800
36. Skinner CJ. Probability proportional to size (PPS) sampling. Wiley StatsRef: Statistics Reference Online. (2014) 14:1–5. doi: 10.1002/9781118445112.stat03346
37. Lawshe CH. A quantitative approach to content validity. Pers Psychol. (1975) 28:563–75. doi: 10.1111/j.1744-6570.1975.tb01393.x
38. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? appraisal and recommendations. Res Nurs Health. (2007) 30:459–67. doi: 10.1002/nur.20199
39. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
40. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. Washington, DC: American Psychiatric Association (1994).
41. Farrahi H, Gharraee B, Oghabian MA, Zare R, Pirmoradi MR, Najibi SM et al. Psychometric properties of the Persian version of patient health questionnaire-9. IJPCP. (2021) (2):248–63. doi: 10.32598/ijpcp.27.2.3375.1
42. Khamseh ME, Baradaran HR, Javanbakht A, Mirghorbani M, Yadollahi Z, Malek MJB. Comparison of the CES-D and PHQ-9 depression scales in people with type 2 diabetes in Tehran, Iran. BMC Psychiatry. (2011) 11:1–6. doi: 10.1186/1471-244X-11-61
43. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
44. Omani-Samani R, Maroufizadeh S, Ghaheri A, Navid BJ. Generalized anxiety Disorder-7 (GAD-7) in people with infertility: a reliability and validity study. Middle East Fertility Soc J. (2018) 23:446–9. doi: 10.1016/j.mefs.2018.01.013
45. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. (2005) 19:192–207. doi: 10.1080/02678370500297720
46. Creedy DK, Sidebotham M, Gamble J, Pallant J, Fenwick J. Prevalence of burnout, depression, anxiety and stress in Australian midwives: a cross-sectional survey. BMC Preg Childbirth. (2017) 17:13. doi: 10.1186/s12884-016-1212-5
47. Javanshir E, Dianat I, Asghari-Jafarabadi M. Psychometric properties of the Iranian version of the Copenhagen Burnout Inventory. Health Promot Perspect. (2019) 9:137. doi: 10.15171/hpp.2019.19
48. Worldometer. Coronavirus Cases. Available online at: www.worldometers.info/coronavirus/country/iran/ (accessed Jun 3, 2022).
49. Noorbala AA, Maleki A, Bagheri Yazdi SA, Faghihzadeh E, Hoseinzade Z, Hajibabaei M, et al. The survey on mental health status in iranian population aged 15 and above one year after the outbreak of COVID-19: A population-based study. Arch Iran Med. (In Press).
50. Menon GR, Yadav J, Aggarwal S, Singh R, Kaur S, Chakma T, et al. (2022). Psychological distress and burnout among healthcare worker during COVID-19 pandemic in India—a cross-sectional study. PLoS ONE. 17:e0264956. doi: 10.1371/journal.pone.0264956
51. Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. (2020) 277:347–57. doi: 10.1016/j.jad.2020.08.034
52. Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1–12. doi: 10.1007/s40200-020-00643-9
53. Couarraze S, Delamarre L, Marhar F, Quach B, Jiao J, Avilés Dorlhiac R, et al. The major worldwide stress of healthcare professionals during the first wave of the COVID-19 pandemic—the international COVISTRESS survey. PLoS ONE. (2021) 16:e0257840. doi: 10.1371/journal.pone.0257840
54. Saeed BA, Shabila NP, Aziz AJ. Stress and anxiety among physicians during the COVID-19 outbreak in the Iraqi Kurdistan region: an online survey. PLoS ONE. (2021) 16:e0253903. doi: 10.1371/journal.pone.0253903
55. Jang Y, You M, Lee H, Lee M, Lee Y, Han JO, et al. Burnout and peritraumatic distress of healthcare workers in the COVID-19 pandemic. BMC Public Health. (2021) 21:2075. doi: 10.1186/s12889-021-11978-0
56. Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iranian Med. (2015) 18:74–5.
57. Ashraf F, Ahmad H, Shakeel M, Aftab S, Masood A. Mental health problems and psychological burnout in Medical Health Practitioners: A study of associations and triadic comorbidity. Pak J Med Sci. (2019) 35:1558–64. doi: 10.12669/pjms.35.6.444
58. Tarcan GY, Tarcan TM, Top M. An analysis of relationship between burnout and job satisfaction among emergency health professionals. Total QualManag Bus Excell. (2017) 28:1339–56. doi: 10.1080/14783363.2016.1141659
59. Kisa S, Kisa A, Younis MZ. A discussion of job dissatisfaction and burnout among public hospital physicians. Int J Health PromotEduc. (2009) 47:104–11. doi: 10.1080/14635240.2009.10708168
60. Maslach C, Leiter MP. The Truth About Burnout: How Organizations Cause Personal Stress and What to Do About It. San Francisco: Jossey-Bass, Wiley Brand (1997).
61. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff. (2011) 30:202–10. doi: 10.1377/hlthaff.2010.0100
62. Picquendar G, Guedon A, Moulinet F, Schuers M. Influence of medical shortage on GP burnout: a cross-sectional study. FamPract. (2019) 36:291–6. doi: 10.1093/fampra/cmy080
63. Linzer M, Manwell LB, Williams ES. MEMO: (Minimizing Error. Maximizing Outcome) Investigators Working conditions in primary care: physician reactions and care quality. Ann Intern Med. (2009) 151:28–36. doi: 10.7326/0003-4819-151-1-200907070-00006
64. De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS ONE. (2020) 15:e0244052. doi: 10.1371/journal.pone.0244052
65. Daneshvar E, Otterbach S, Alameddine M, Safikhani H, Sousa-Poza A. Sources of anxiety among health care workers in Tehran during the COVID-19 pandemic. Health Policy Plan. (2022) 37:310–21. doi: 10.1093/heapol/czab136
66. Coşkun Simşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. (2021) 68:219–27. doi: 10.1111/inr.12651
67. Rose S, Hartnett J, Pillai S. Healthcare worker's emotions, perceived stressors and coping mechanisms during the COVID-19 pandemic. PLoS ONE. (2021) 16:e0254252. doi: 10.1371/journal.pone.0254252
68. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMed. (2020) 24:100424. doi: 10.1016/j.eclinm.2020.100424
Keywords: mental health, burnout, job stressors, COVID-19, healthcare workers, Iran
Citation: Hajebi A, Abbasinejad M, Zafar M, Hajebi A and Taremian F (2022) Mental Health, Burnout, and Job Stressors Among Healthcare Workers During the COVID-19 Pandemic in Iran: A Cross-Sectional Survey. Front. Psychiatry 13:891430. doi: 10.3389/fpsyt.2022.891430
Received: 07 March 2022; Accepted: 19 April 2022;
Published: 12 May 2022.
Edited by:
Renato de Filippis, Magna Græcia University, ItalyReviewed by:
Mahsa Nahidi, Mashhad University of Medical Sciences, IranMahlagha Dehghan, Kerman University of Medical Sciences, Iran
Copyright © 2022 Hajebi, Abbasinejad, Zafar, Hajebi and Taremian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farhad Taremian, ZmEudGFyZW1pYW4mI3gwMDA0MDt1c3dyLmFjLmly
 Ahmad Hajebi
Ahmad Hajebi Maryam Abbasinejad
Maryam Abbasinejad Masoud Zafar
Masoud Zafar Amirali Hajebi
Amirali Hajebi Farhad Taremian
Farhad Taremian