
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry, 08 September 2022
Sec. Child and Adolescent Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.886590
This article is part of the Research TopicWomen in Psychiatry 2022: Child and Adolescent PsychiatryView all 6 articles
Background: Resilience allows a more positive coping and improves parents' wellbeing when they face a difficult situation like having a child with a neurodevelopmental disorder (NDD). We aim to analyze the development of resilience in parents of children with different NDD (ASD, DLD and ADHD) with different levels of structural language and social cognition, as well as the social support available for their families, and compare it to children with typical development (TD).
Method: We analyzed the level of resilience of 156 parents, 73 with children with TD and 73 with three different NDD, taking into account variables such as age, structural language (receptive grammar) and social cognition (emotional understanding) of the children, and also the type of social support available to them.
Results: Children with DLD and ASD showed lower receptive grammar and emotional comprehension skills, although only parents of children with ASD obtained better resilience scores. Moreover, age of children and formal support variables predicted the resilience of the parents according to the type of NDD.
Discussion: The severity of social cognition and structural language difficulties of children with NDD and the fact of having support from professionals and family associations have a significant influence on the development of parental resilience.
Having a child with a disability becomes an adverse situation for parents because it involves many physical and emotional demands, sacrifices to meet their needs, or living with the insecurity of having an uncertain future (1).
In this regard, when raising children with neurodevelopmental disorders (NDD)—such as autistic spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD) or developmental language disorder (DLD)—who face social communication and behavioral difficulties to a greater or lesser extent, parents experience complex everyday situations that often lead to higher levels of stress (2), greater depressive symptoms (3), and sometimes poorer quality of life in comparison to parents with typically developing children (TD) (4).
The literature shows different studies that relate inappropriate behaviors of children with NDD to parental mental health (5, 6), but these studies were mostly conducted with parents of children with ASD (7). Therefore, the impact of behaviors characteristic of disorders such as ADHD or DLD on the mental health of their parents is less known.
Existing empirical evidence comparing the impact on the mental health of parents with children with ASD with other difficulties such as Down Syndrome (DS) or Intellectual Disability (ID), report large differences due to the type of behaviors specific to each disorder. Authors conclude that ASD is the disorder that produces the most parental stress and also that the severity of emotional and behavioral problems of these children are associated with the higher levels of stress of their parents (8, 9).
Given this fact, recent studies have focused on exploring factors that protect parents during the care and upbringing of an autistic child, stressing the importance of resilience skills. Resilience refers to an adaptive response that is activated when a person faces difficult conditions (10) (such as having a child with difficulties), facing the situation in a positive way, and coming out of it strengthened (11). Having resilient skills does not imply not experiencing these situations as adverse, but knowing how to handle, cope with and overcome them (12). The main constructs of resilience theory risk factors (those that predispose people to physical and mental health problems because they affect the way a person adapts to stress), protective factors (those that promote resilience by reducing the effects of risk and the negative reaction to it), and resilience indicators (internal aspects such as self-efficacy, acceptance, sense of coherence or optimism) (13). According to resilience theory, an individual's resilience is determined by the balance between these factors in the face of adversity (14).
Consequently, resilience significantly reduces stress (15, 16) and improves parental mental health (17), including suffering less depression (18), perceiving greater psychological wellbeing (19) and greater life satisfaction (20).
In this sense, literature specifies that risk factors for caregivers of individuals with ASD include severity of symptoms (21–23), poor family relationship (24, 25), and having more than one child with ASD (26). Several studies relate the severity of ASD symptoms (including social communication aspects) to lower parental psychological wellbeing, lower life satisfaction, and a higher prevalence of depression (25, 26). Particularly, it was seen that emotional, communication and behavioral problems of the children increased the mental health problems of their mothers (27).
In parallel, other studies show that social communication is related with development of structural language and social cognition skills not only in children with ASD (28), but also in children with DLD (29) and ADHD (30), who usually differ from children with ASD in the degree of their pragmatic language impairments. In this regard, although structural language (specially grammar) and social cognition abilities (including theory of mind and emotion understanding) are prerequisites of social communication skills, there are few studies that analyse whether they are associated with parental resilience in children with different levels of ASD or with other NDD (31).
Within relatives of children with ASD, protective factors of parental resilience are the age of the child (26), the social support of the family (32, 33), and other aspects such as religious beliefs and spirituality (34). In this sense, behaviors inappropriate to age are related to the perceived stress of parents of children with ASD (28) and to parenting burden (25). Moreover, social support has been shown to alleviate the impact of children's NDD symptom severity on parents' mental health, improving their wellbeing and reducing anxiety and depressive symptoms (35, 36).
However, few studies have compared the level of resilience in parents with different NDD who present social communication problems in a greater or a lesser degree.
In parallel, the paper of social support for the parents of children with NDD has been raised. First, formal support received from a professional is a source of informational and instrumental support, which provides resources for the whole family (such as attending a psychoeducational intervention or occupational therapy center) (20). Second, informal support includes attending family associations or activities with other families provides emotional support and a space for unwind (such as being part of an association of parents of children with a specific disorder, parenting schools or clubs that organize activities for parents) (37). And third, family support can act as a protective factor by having support for the care of children with NDD, as the presence of family members who assist in the care of the child with problems reduces the burden and stress on parents (38).
However, mixed evidences have been found regarding the availability of social support, and some of them point out that this social support is not related to parent's adaptation and resilience (39), which may be due to a failure to account for different types of social support. In this sense, although most existent studies deal with social support in a comprehensive manner, different types of social support can be distinguished (40).
So, as pointed above, since most of the studies that analyze mental health and resilience development of parents of children with NDD are focused on children with ASD, it is considered necessary to make a cross-disorder comparison of these variables including other children with NDD with mild but existent social cognition and language difficulties that could lead to inappropriate social and emotional behaviors, such as children with ADHD and DLD.
Consequently, this comparison will allow us to understand which factors influence the development of parental resilience of a child with NDD, and therefore, to establish guidelines to train parents of children with NDD to develop strategies to modify those behaviors of their children that generate stressful situations. Furthermore, considering the positive influence of resilience on the wellbeing of parents with children with NDD, this comparison will allow us to establish the type of supports required by each group as well. In this sense, it will help us to clarify the weight of social supports in the development of resilience, and will enable us to know better how different types of social support influence the development of resilience in parents with children with different NDD. Finally, knowing both the characteristics of the children and the contextual aspects that influence in the development of resilience will allow us to specify what aspects need to be worked on to foster resilient skills in their parents. This is to provide them of skills to better adapt themselves to the situation of having a child with NDD, what will lead them to improve their wellbeing and mental health.
Therefore, the overall aim of the present study is to examine the development of resilience of parents of children with different NDD, and to find out the influence of age, structural language and social cognition skills of their children, as well as the influence of different types of social support in the family (formal, informal and family support).
Accordingly, the following hypotheses are proposed:
• Parents of children with NDD will present higher scores on all factors that make up resilience (persistence, tenacity and self-efficacy; control under pressure; adaptability and support networks; control and purpose; spirituality) in comparison to parents of children with TD.
• Within children with NDD, parents of children with ASD (and subsequent more social communication problems), will present a higher level of resilience than parents of children with ADHD and DLD.
• Among personal features of children with NDD, factors such as age, structural language and social cognition will predict the resilience of parents of children with any type of NDD. Among contextual factors, formal support is the factor that will most influence the resilience of parents of children with any type of NDD.
A non-probabilistic convenience sampling method was used for the present study. A total of 156 children attending different ordinary schools in Spain together with their 156 parents of children took part of the sample: 73 were parents of 73 children with a diagnosed NDD (clinical group), and 73 were parents of 73 children with TD (control group). Both samples came from the same context and ordinary public schools, so all of the participant families had a similar average socio-economic status.
All the selected children with NDD (57 boys and 16 girls) had an updated diagnosis at the time of the investigation and had been previously diagnosed by school psychologists following the regional protocols and meeting the DSM-5 criteria for the assessment of these disorders with standardized common specific measures. They were all aged between 5 and 12 years (M = 107.81 months; SD = 26.83; range 60–155). This clinical group (NDD) was organized intro three subgroups:
• 36 parents and 36 children with ASD (M = 106.78 months; SD = 25.41; range 60–154).
• 20 parents and 20 children with ADHD (M = 117.05 months; SD = 22.88; range 74–155).
• 17 parents and 17 children with DLD (M = 99.12 months; SD = 31.85; range 60–153).
There were no cases with ADHD or DLD comorbid with other clinical conditions. However, two children of the ASD group showed an ADHD condition in their reports, and a child presented ADHD and DLD.
The control group (TD) consisted of 73 parents and 73 typically developing children. The children were aged 5 to 12 years (M = 110.45 months; SD = 24.42; range 63–146), and they were matched with NDD children by gender and age (within ±3 months). In the clinical group there were 59 mothers and 14 fathers, and in the control group there were 48 mothers and 25 fathers.
Finally, children in both groups were assessed with the Raven Colored Progressive Matrices test (41) or Raven's Progressive Matrices revised version (42), depending on their age. The 73 children with NDD and the 73 children with TD were seen to present scores within 1.5 SD of the mean on these tests (NDD M percentile = 45.58, SD = 30.38; TD M percentile = 56.56, SD = 27.02). Nevertheless, no significant differences were found with Kruskal-Wallis test at the non-verbal reasoning level between the three subgroups of clinical participants when they were compared (ASD: M = 51.4; SD = 31.82; ADHD: M = 39.10; SD = 30.18; DLD: M = 41.23; SD = 26.72): H(3) = 2.161, p = 0.339.
Research group created a form where parents were asked about the following aspects: whether they attended a specific professional center for their child's problems (FS: formal support); whether they attended a family association or group (IS: informal support); whether they had more children (MCh) (other sons or daughters) and whether they had the support of grandparents for the care of their children (FamS: family support-grandparents). All the questions were dichotomous (yes or no).
This is a questionnaire completed by families and was used to assess the resilience skills of parents of children with and without NDD.
The Resilience Scale (43) consists of 25 items with a scale from 0 to 4. The total score ranges from 0 to 100 (Tot R). The construct is composed of five factors: F1: persistence, tenacity and self-efficacy (items 10–12, 16, 17, 23–25; score 0–32); F2: control under pressure (items 6, 7, 14, 15, 18, 19, 20; score 0–24); F3: adaptability and support networks (items 1, 2, 4, 5, 8; score 0–20); F4: control and purpose (items 13, 21, 22; score 0–12); and F5: spirituality (items 3, 9; score 0–8). The authors of the questionnaire obtained good psychometric properties (43). They show that the items were grouped into five dimensions and Cronbach's alpha coefficient was 0.89; test-retest reliability, the mean (sd) CD-RISC scores at time 1 [52.7 (17.9)] and time 2 [52.8 (19.9)] demonstrated a high level of agreement, with an intraclass correlation coefficient of 0.87.
The Comprensión de Estructuras Gramaticales (CEG) (44) is a formal measure of grammatical comprehension for children aged 4–11 years, and it is the Spanish adaptation of the Test for Reception of Grammar (TROG) (45). In the present study, it was used to assess receptive language skills of children with NDD, as measure structural language skills linked to social communication.
The CEG allows to assess children's ability to understand different types of grammatical structures that vary in lengths and degrees of complexity. The child hears a sentence and he must choose which is the one that corresponds to it between four given pictures. It contains 80 items (raw score 0–80).
The test has adequate psychometric properties: The internal consistency used as a measure of reliability (Cronbach's alpha) showed an index of 0.91; Validity of criteria, correlation values: CEG-Peabody Picture Vocabulary Test (r = 0.809, p < 0.001) and CEG-Illinois Test Psycholinguistic Abilities (r = 0.644, p < 0.001) [Peabody Picture Vocabulary Test (47)].
The Test of Emotion Comprehension (TEC) is a formal and standardized measure of emotional understanding for children between 3 and 11 years of age which is considered an appropriate global measure of social cognition as it tests the comprehension of the nature, causes, and regulation of emotion (e.g., emotions based on external causes or in other mental states such as desires or beliefs) (45). So, it was used to obtain a social cognition measure linked with the social communication of children with NDD.
This instrument allows for the evaluation of nine components of emotional understanding: Recognition of emotions (component 1), External causes (component 2), Emotions based on desires (component 3), Emotions based on beliefs (component 4), Emotions based on memories (component 5), Regulation of emotions (component 6), Hiding emotions (component 7), Mixed emotions (component 8) and Moral Emotions (component 9). The TEC raw score ranged from 0 to 9 and it is obtained by adding the sub-scores for the nine components.
The TEC consists of 23 picture stories. A brief story is read by the examiner first, and then the child is asked to choose the correct facial expression (emotion) for the main character from among four given options. The possible emotions to appear across the 23 items are happy, sad, angry, scared and/or well.
The Spanish version of the TEC is currently under validation, so one of the authors provided the research group with the Spanish version of the instructions (translated and adapted by Carlos Hernández Blasi and Francisco Pons).
The test has good test-retest reliability after 3 months of delay [r(18) = 0.84], and good test-retest correlation after 13 months of delay [r(40) = 0.64 and r(32) = 0.54] (48, 49). Moreover, internal consistency used as a measure of reliability (Cronbach's alpha) showed all the values were in the range of 0.61–0.97.
The corresponding permissions were requested from the autonomous government and the school authorities of the regular schools where the children with and without NDD attended.
At each regular school, the educational psychologist assisted the research group in recruiting the clinical sample with the proposed inclusion criteria (see next paragraph) and also age-and gender-matched peers to conform a control TD group. First, the parents of all selected children were informed of the aims of the study, and then they were given a document to sign their informed consent for their own participation and for their children's participation in the study. Finally, they were asked to fill out the informed consent form and return it to their child's teacher.
The inclusion criteria for the clinical sample were (NDD group): (1) to have a current diagnosis of ASD, ADHD or DLD according to regional county diagnostic protocols and meeting DSM-5 criteria for assessment of these disorders with specific common standardized measures; and (2) to be between the ages of 5 and 12 years. For the age-matched sample (TD group), the inclusion criteria were to be matched with a child with NDD by gender and age. In addition, children in both groups were seen to score within 1.5 SD on the Raven's Colored Progressive Matrices test (40) or with the revised version of the Raven's Progressive Matrices (41), depending on the child's age.
Each child was individually assessed by the research group during a 40-min session (approximately) in a quiet room provided by the school. The tasks were administered in random order. In parallel, parents were given an envelope containing the contextual data questionnaire on parental social support and the resilience scale for completion. They had one week to fill out the form and the questionnaire, and then give them to their child's teacher. The parent who spent the most time with the child was asked to participate.
The original sample of this study included 162 participants/parents, but 6 questionnaires were not completed by the parents, so the final sample comprised 156 participants/parents.
Statistical analysis was performed using SPSS 27.0. First, the Kolmogorov-Smirnov test was performed. It was found that for the dependent variable (resilience), the data did not have a normal distribution (p < 0.05).
With respect to hypothesis 1, the Mann-Whitney U test was used to perform group contrasts on the level of resilience between parents of children with TD and those with NDD. To obtain the sample effect size, the statistical formula described by Tomczak and Tomczak (50) was used (r = Z/√N, where Z is taken as the absolute value; a value of 0–0.1 is considered a small effect, 0.2–0.4 a medium effect, and 0.5–1 a large effect).
In relation to hypothesis 2, the Kruskal-Wallis test was performed to analyze whether there is a difference in the level of parental resilience according to the type of NDD (ASD, ADHD or DLD). In addition, the Mann-Whitney U test was calculated to find out the difference between the three subgroups according to age, structural language (receptive grammar in this study) and social cognition (emotional comprehension in this study) performance.
Finally, with respect to hypothesis 3, the Mann-Whitney U test was performed to analyze between-group differences in the resilience of the parents of children with NDD according to the social support variables. Moreover, a hierarchical linear regression was also performed in the clinical and the three subgroups (ASD, ADHD, and DLD) to find out which factors of social support, structural language and social cognition predicted of greater development of parental resilience.
Table 1 shows the level of total resilience and the scores obtained in all the factors that make up resilience (F1: persistence, tenacity and self-efficacy; F2: control under pressure; F3: adaptability and support networks; F4: control and purpose; F5: spirituality), as well as the level of social communication (in this study, measured with grammatical and emotional comprehension) of the children in the NDD and TD groups. Between-group differences obtained with Mann-Whitney U test indicated a significant difference with a large size effect in the Total Score of Resilience (r = 0.55), finding a higher level of resilience in parents in the NDD group. Similarly, this pattern was also found in all individual resilience factors with large and medium size effects [F3 (r = 0.69), F1 (r = 0.43), F2 (r = 0.39), F4 (r = 0.28), F5 (r = 0.17)].
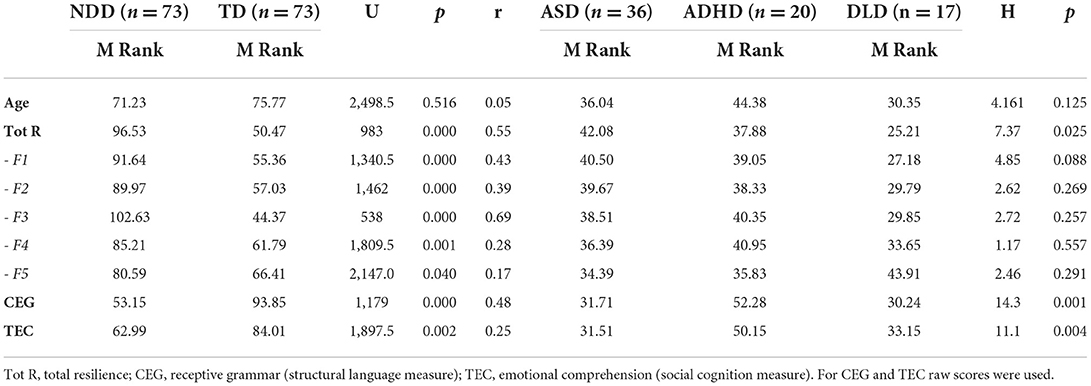
Table 1. Mean ranks and between-group comparisons between children with NDD (n = 73) and children with TD (n = 73) on Resilience Scale (Total and Factors: F1, F2, F3, F4, and F5), structural language and social cognition measures; and comparison of subgroups per separate: ASD, ADHD, and DLD.
Regarding the age of the participants, no significant differences were found between the two groups. Regarding the children's receptive grammar and emotional comprehension, significant differences were observed between the NDD and TD groups with large and medium effect sizes (CEG, r = 0.48; TEC r = 0.25).
Table 1 also shows the data of the clinical group, comparing the results obtained in each subgroup (ASD, ADHD, and DLD). In this sense, the values of the Krustal-Wallis test showed that the level of total resilience was significantly different in the three subgroups. The parents of children with ASD are the ones who obtained a higher level of resilience, followed by the ADHD subgroup, with the DLD subgroup presenting a lower level of resilience.
Between-group comparisons carried out with Mann-Whitney U test show that there were no differences in the level of resilience between parents of children with ASD and ADHD (U = 320, p = 0.49, r = 0.09); nor between parents of children with ADHD and DLD (U = 113, p = 0.082, r = 0.28); but a significant difference was found between the level of resilience of parents of children with ASD and DLD with a large effect size (U = 162.5, p = 0.006, r = 0.37).
With respect to the age of participants, no significant differences were observed between the three clinical subgroups.
Regarding the level of structural language and social cognition of the participants, the Kruskal-Wallis test showed significant differences in both the receptive grammar and emotional comprehension skills among the three subgroups. First, regarding receptive grammar performance, DLD subgroup underperformed ASD and ADHD groups. Between-group comparisons with Mann-Whitney U test showed that there were significant differences between the ASD and ADHD groups (U = 156, p < 0.001, r = 0.46), and also the ADHD and DLD group (U = 68, p = 0.002, r = 0.53), but not between the ASD and DLD groups (U = 292.5, p = 0.797, r = 0.05). Second, with respect to the emotional comprehension, ASD subgroup scored lower than the other two subgroups. In this case, Mann-Whitney U test showed that there were significant differences between the ASD and ADHD groups (U = 174, p = 0.001, r = 0.43), and ADHD and DLD groups (U = 92, p = 0.010, r = 0.40), but not between ASD and DLD groups (U = 294, p = 0.816, r = 0.03).
Table 2 presents data on the effect of different types of supports (formal, informal, and family) and having more children on the level of resilience of parents. Mann-Whitney U showed that there were significant differences in the level of parental resilience between those with and without formal and informal supports in the ASD group (with a medium effect size) and in the ADHD group (with a large effect size), but not in the DLD group. Related variables to family support such as having help from grandparents or having more children, did not significantly impact parental resilience in either group.
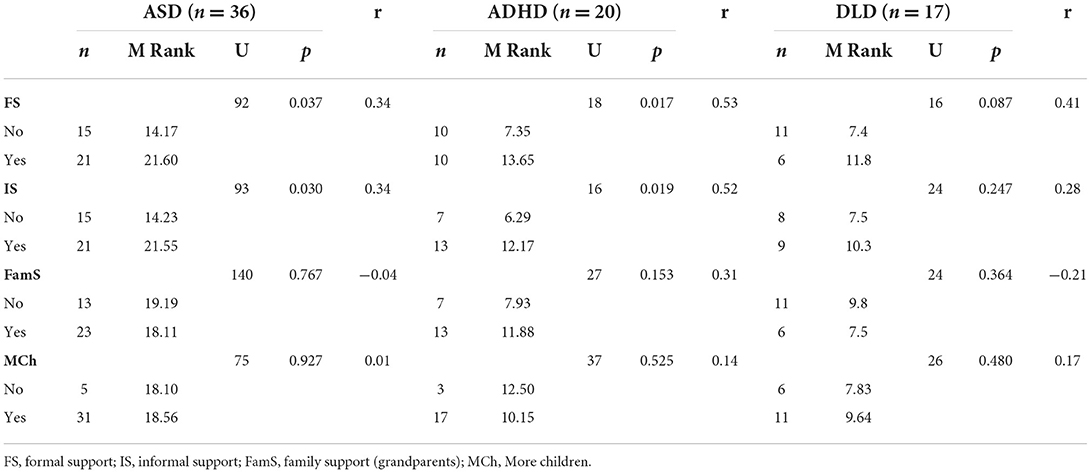
Table 2. Relationship between the different types of social supports and the level of resilience of parents in the different clinical groups.
Finally, a hierarchical linear regression was carried out to predict parental resilience in the group of children with NDD. This analysis was performed on the total score of the Resilience Scale. To this end, five variables were used: age of children, formal support, informal support, level of receptive grammar (structural language) and level of emotional understanding (social cognition) of the children.
Table 3 shows the regression analyses of the general model obtained. A total 31.9% of the variance was explained: F(4, 68) = 7.953, R2 = 0.319, p < 0.001. Specifically, Step 5 pointed out the importance of the variable age of children (β = 0.036) and having formal support (β = 0.003) as aspects that can predict resilience of parents with children with NDD. Nevertheless, the effect of the variables informal support, structural language and social cognition (grammar and emotional comprehension levels) were not seen significant.
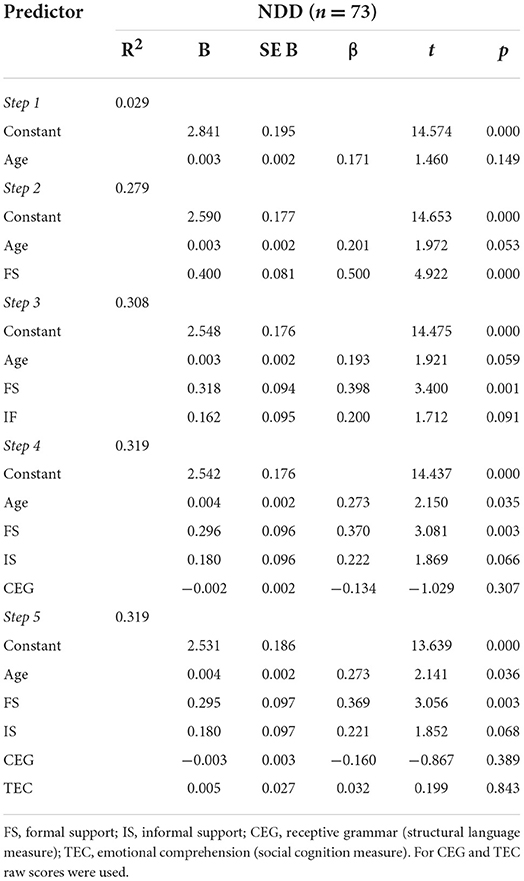
Table 3. Summary of the regression coefficients of Resilience Scale total scores within the NDD group.
Similarly, three hierarchical linear regressions were carried out to predict parental resilience in each subgroup of children with NDD (ASD, DLD and ADHD separately). Again, these analyses were performed on the total score of the Resilience Scale, and the same five variables were used.
Table 4 shows the regression analyses of the general model performed for the three groups. Regarding the group of children with ASD, 27.8 % of the variance was explained: F(5, 30) = 2.305, R2 = 0.278, p = 0.069, formal support being significant in step 2 (β = 0.42). Similarly, in the group of children with ADHD, 44 % of the variance was explained: F(5, 14) = 2.255, R2 = 0.446, p = 0.162, with Age being significant at step 1 (β = 0.45) and formal support being significant at step 2 (β = 0.44). And finally, in the group of children with DLD, 51% of the variance was explained: F(5, 11) = 2.268, R2 = 0.508, p = 0.120, and the significance of formal support stands out in step 2 (β = 0.60).

Table 4. Summary of the regression coefficients of Resilience Scale total scores within the ASD, the ADHD and the DLD group.
The present study aimed to examine the resilience of parents of children with different NDD (in this study, ASD, ADHD, and DLD), and also to examine which individual factors of the child and which contextual factors of the family support that parental resilience. So, the role of structural language, social cognition and social support of the family was explored.
With respect to Hypothesis 1, it was expected that parents of children with NDD would show higher parental resilience scores compared to parents of children with TD on all factors that make up resilience. In this sense, results of the present study verified this hypothesis and between-group comparisons pointed out that having a child with a disorder usually leads to the development of greater resilience skills, probably because these skills allow them to cope with the difficult situation and the barriers they have to face in their daily lives (41). Moreover, when analyzing the level of resilience among the different types of NDD (ASD, ADHD, and DLD per separate), between-group comparisons showed that the level of general resilience is significantly different in the different groups (p = 0.025). Thus, the fact of having a child with a disorder does not always mean developing greater resilience skills per se (42), but the differences on parental resilience found between the clinical subgroups [ASD-ADHD (U = 320, p = 0.49, r = −0.09); ADHD-DLD (U = 113, p = 0.082, r = −0.28); ASD-DLD (U = 162.5, p = 0.006, r = −0.37)] indicate that it depends on the type of disorder (42).
These results represent an important contribution to existent literature, since most of the studies assessing resilience in parents of children with NDD focus on parents with children with ASD (5–9), but a cross-disorder comparison comparing the level of resilience in parents with children with other NDD who also show social and communication difficulties were limited (51).
In this sense, it was considered necessary to analyse the difference in the level of parental resilience according to the type of disorder in order to find out the possible relationship between the type of NDD (ASD, DLD, and ADHD), the age of the children, and severity of their symptoms (taking into account their level of structural language and social cognition, as prerequisites of social communication) and the level of parental resilience. As expected in Hypothesis 2, the data from our study show that the level of resilience is greater in parents of children with ASD, followed by the group of parents of children with ADHD and the group of parents of children with DLD, the latter having the lowest level of resilience. In this sense, both ASD and DLD groups performed similarly on receptive grammar and emotional comprehension tests, but they showed significant lower scores when compared to those with ADHD. Nevertheless, total resilience scores of parents were only significantly different between these two subgroups (DLD and ASD). Thus, it seems that the lower level of receptive grammar and emotional comprehension showed by children with ASD and the level of resilience of their parents (see Table 1) is in line with previous studies, as they showed that emotional, communication and behavioral problems in children increased the mental health problems of mothers with ASD children (27).
Specifically, for children with ASD, the data of the present study shows that the lower the children's level of receptive grammar and emotional comprehension are, the higher parental resilience is. Nevertheless, this affirmation does not apply to those children with DLD and their parents. This finding may indicate that resilient skills start to develop when parents perceive their children's problems as an “adverse situation” (e.g., when a confirmed diagnose of ASD is received, in contrast to a diagnose of DLD, perhaps because it is a disorder whose prognosis and course is seen less severe. Additionally, parents of children with ASD experience a parenting dealing with greater social communication problems of their children that are present in their everyday situations (with a greater number of behavioral and emotional issues), and more severe than in children with DLD or ADHD. It seems that, during these developmental stages (school period), communicating effectively with their children, getting their children to respect social and family norms, or connect emotionally with them, can be more challenging for parents of children with ASD than for children with DLD or ADHD. Consequently, all these issues may contribute to experience the situation as more “adverse” or complex, which is a key aspect for the development of resilience (21).
Therefore, data from the present study support the results of previous studies (7, 21, 23) that associate ASD and ADHD symptoms with a higher degree of stress and mental health problems in parents, but also provide information concerning parents of children with DLD.
Finally, as stated in the first part of Hypothesis 3, it was expected to find that among personal features of children with NDD, the age and their difficulties in receptive grammar and emotional comprehension (as they are prerequisites of social communication) will predict the resilience of their parents in any type of NDD; and among contextual factors, it was expected that formal support would be the factor more associated with the resilience of parents of children with any type of NDD.
In this respect, our data partially verifies this third hypothesis. Regarding personal features of children, the age of the children did influence the resilience of the parents of children with NDD in general, although this predictive power was only observed for those children with ADHD (but not for those with ASD or DLD). Moreover, variables related to structural language and social cognition (receptive grammar and emotional understanding), were not powerful enough to predict total resilience scores of parents of children with NDD (both in general and within the three subgroups).
Furthermore, according to the second part of the Hypothesis 3, formal support was expected to be the factor that would explained more the resilience of parents of children with any type of NDD. Between-group comparisons according to the different types of social supports and the level of resilience of parents in the different clinical groups allows us to verify this assumption, pointing out the importance of having formal and informal support for the development of parents' resilience. Specially, this is important for the groups of children with ASD and ADHD whose parents showed less parental resilience (and therefore, for maybe less perceived wellbeing). Formal and informal support may provide a source of informational support (information about the characteristics of the disorder itself, as well as its evolution), instrumental support (they offer guidelines for day-to-day intervention) and emotional support (they are a source of relief and comfort) (37, 42, 46). In contrast, our data suggest that other variables like the presence of grandparents or having other children in the family (sons/daughters) do not influence the level of parental resilience. Possibly, although having support in the upbringing of children with a disorder is considered a protective factor because it relieves parents (52), sometimes the lack of understanding of some behaviors by a family member can generate more stress for parents (15). Also, several studies suggest that siblings without problems perceive their siblings with a disorder as a burden (53).
The importance of formal support was confirmed in the regression analysis, and it was found to be a significant predictor of parental residence both within the NDD group and in the clinical subgroups per separate. So, these results provide a key contribution to previous research because although many studies establish social support as a protective factor that facilitates individual resilience and reduces parental stress (54–56), most of these studies were conducted with only parents with ASD children and furthermore do not differentiate between different types of social support. Thus, formal support is also important for those parents of children with ADHD and DLD.
For example, for children with NDD and their families, one of the most effective formal support is the one offered by psycho-pedagogical counselors, as they provide the parents with guidelines adapted to the development level and real skills of the child, taking into account previously acquired knowledge and skills. In addition, they also focus on personal aspects of the child that are hindering their participation in social and academic contexts (such as reducing inappropriate behaviors); social and communication nuclear and related aspects (such as improving their structural language or social cognition skills); and academic aspects if necessary (such as improving curricular adaptations to facilitate or enable the learning process) (57).
Limitations of this study include the sample size of the three clinical groups and the unequal number of participants of the three different diagnoses (ASD, DLD, and ADHD). In this respect, future cross-disorder studies must check resilience models with similar and greater sample sizes, as the predictors of parental resilience related to structural language and social cognition may reach significance. Moreover, regarding the social cognition measure, the limited number of elements of each component and the fact that it covers partial aspects of social cognition must be noted. Maybe other features of social communication deficits are more related with resilience (e.g., pragmatics skills related to intention comprehension or dealing with complex mental states as errors or mistakes) have not been assessed with our social cognition measure (the TEC). Thus, another limitation of the present study is that no direct assessments of social communication taken in real communication settings were included. Finally, the present study focuses also on contextual aspects of parenting. So, as formal support has been seen a key factor to promote parents' resilience, another limitation of the study is that the time they have been receiving this formal support was not collected. Moreover, future studies should also focus on personal aspects of parents (such as age of parents or educational level, for example).
It must be noted that the main results of the present study have important implications for clinical and educational professionals who attend families of children with NDD. These professionals are the ones who provide formal support for parents, as mentioned above. So, when a child is diagnosed with any type of NDD, it is very important that parents are informed of the benefits of receiving this type of support.
Considering how the development of structural language and social cognition is associated with social communication skills, and how these variables are related to emotional stress (28), formal support could include counseling and training for parents in three different domains:
• in the behavioral domain, providing parents with strategies to intervene or redirect inappropriate social and emotional behaviors of their children to decrease parental stress (58);
• in the psychoeducational domain, providing parents with strategies to cope with the academic activities that children have to perform at home, and also with the socialization problems of their children (e.g., teaching them to promote social interaction of their children with their peers, where they can act as mediators; how to expand their structural language and social cognition skills with indirect strategies), which would increase parents' self-efficacy (56, 58);
• in resilience domain (that is, the development of individual skills, knowing protective factors, and knowing how to act with risk factors) (59). In this respect, the development of resilience should be worked not only with parents to reduce individual stress (60), but with the maximum family members (family resilience) to try to reduce the stress generated within the family functioning (61).
Likewise, there are other types of methods such as mindfulness-based interventions that have been shown to have a positive effect on the psychological wellbeing and stress reduction of parents with NDD (62, 63).
Another implication of the present study, addressed to autonomic governments, is the importance of reinforcing public educational centers where children with NDD attend with a greater number of educational psychologists, who could help more families to receive the formal support described. Sometimes, the professionals who attend these children do not have time to attend to all the cases they have in the school and their families, and therefore they establish a priority based on the severity of the children's symptoms.
Finally, the results also encourage families to create and/or participate in associations of relatives of children with a given disorder. These centers provide informal support to families, since they are a communication space to share experiences, a leisure space where playful activities can be carried out as a family, and also a space where training and intervention programs can be organized by professionals for families on aspects related to the child's education and from where the resilience of the family members, including the child with NDD, can be developed. With this type of support, it is intended to improve the mental health of families and therefore an improvement in their quality of life.
The datasets generated for this study are available from the corresponding author upon reasonable request.
The studies involving human participants were reviewed and approved by CD/17/2022. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
RF-B and CA-R have contributed to the conceptualization of the study, design and development of the research, and co-directors of the research projects that funded this study. In addition, all authors have contributed to the data analysis, discussed the results, and collaborated jointly in writing the current draft and revising the final manuscript before submission.
This study was funded by Ministry of Science and Innovation (Spain) (PID2020-115167GA-I00) and the Universitat Jaume I of Castellón (UJI-B2020-29).
The researchers would like to thank the children and families who took part in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Walker R, Belperio I, Gordon S, Hutchinson C, Rillotta F. Caring for a family member with intellectual disability into old age: applying the sociocultural stress and coping model to Italian and Greek migrants in Australia. J Appl Res Intellect Disabil. (2020) 33:887–97. doi: 10.1111/jar.12710
2. Baker-Ericzén, Mary J, Brookman-Frazee L, Stahmer A. Stress levels and adaptability in parents of toddlers with and without autism spectrum disorders. Res Pract Persons Severe Disabl. (2005) 30:194–204. doi: 10.2511/rpsd.30.4.194
3. Bailey D, Golden R, Roberts J, Ford A. Maternal depression and developmental disability: research critique. Ment Retard Dev Disabil Res Rev. (2007) 13:321–9. doi: 10.1002/mrdd.20172
4. Mugno D, Ruta L, D'Arrigo VG, Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health Qual Life Outcomes. (2007) 5:22. doi: 10.1186/1477-7525-5-22
5. Rooke MI, Pereira-Silva NL. Indicators of family resilience in families of children with Down's syndrome. Estudios de psicología. (2016) 33:117–126. doi: 10.1590/1982-027520160001000012
6. Whitehead K, Dorstyn D, Ward L. Psychological adjustment in families affected by autism spectrum disorder. J Dev Phys Disabil. (2015) 27:703–17. doi: 10.1007/s10882-015-9446-0
7. Pastor-Cerezuela G, Fernández-Andrés MI, Tárraga-Mínguez R, Navarro-Peña JM. Parental stress and ASD: relationship with autism symptom severity, IQ, and resilience. Focus Autism Other Dev Disabil. (2016) 31:300–11. doi: 10.1177/1088357615583471
8. Craig F, Operto FF, De Giacomo A, Margari L, Frolli A, Conson M, et al. Parenting stress among parents of children with neurodevelopmental disorders. Psychiatry Res. (2016) 242:121–9. doi: 10.1016/j.psychres.2016.05.016
9. Valicenti-McDermott M, Lawson K, Hottinger K, Seijo R, Schechtman M, Shulman L, et al. Parental stress in families of children with autism and other developmental disabilities. J Child Neurol. (2015) 30:1728–35. doi: 10.1177/0883073815579705
10. Piña JA. Un análisis crítico del concepto de resiliencia en psicología. Anales de Psicología. (2015) 31:751–8. doi: 10.6018/analesps.31.3.185631
11. Rajan AM, Romate J. Resilience and impact of childreńs intellectual disability on Indian parents. J Intellect Disabil. (2017) 21:315–24. doi: 10.1177/1744629516654588
12. Brooks R, Goldstein S. The Mindset of Teachers Capable of Fostering Resilience in Students. Can J Sch Psychol. (2008) 23:114–26. doi: 10.1177/0829573508316597
13. Bekhet AK, Johnson N, Zauszniewski J. Effects on resilience of caregivers of persons with autism spectrum disorder: the role of positive cognitions. J Am Psychiatr Nurses Assoc. (2012) 18:337–44. doi: 10.1177/1078390312467056
14. Luthar S, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. (2000) 71:543–62. doi: 10.1111/1467-8624.00164
15. Suzuki K, Hiratani M, Mizukoshi N, Hayashi T, Inagaki M. Family resilience elements alleviate the relationship between maternal psychological distress and the severity of children's developmental disorders. Res Dev Disabil. (2018) 83:91–8. doi: 10.1016/j.ridd.2018.08.006
16. Gardiner E, Mâsse LC, Iarocci G. A psychometric study of the family resilience assessment scale among families of children with autism spectrum disorder. Health Qual Life Outcomes. (2019) 17:45. doi: 10.1186/s12955-019-1117-x
17. Van-Breda AD. Resilience Theory: A Literature Review. South African Military Psychological Institute (2001). Available online at: http://vanbreda.org/adrian/resilience/resilience_theory_review.pdf (accessed January 27, 2022).
18. Kaniel S, Siman-Tov A. Comparison between mothers and fathers in coping with autistic children: a multivariate model. Eur J Spec Needs Educ. (2011) 26:479–93. doi: 10.1080/08856257.2011.597186
19. Kuhn JC, Carter AS. Maternal self-efficacy and associated parenting cognitions among mothers of children with autism. Am J Orthopsychiatry. (2006) 76:564–75. doi: 10.1037/0002-9432.76.4.564
20. Oñate L, Calvete E. A qualitative approach to the resilience factors in families of people with intellectual disabilities in Spain. Psychol Intervent. (2017) 26:93–101. doi: 10.1016/j.psi.2016.11.002
21. Halstead E, Ekas N, Hastings R, Griffith G. Associations between resilience and the well-being of mothers of children with autism spectrum disorder and other developmental disabilities. J Autism Dev Disord. (2018) 48:1108–21. doi: 10.1007/s10803-017-3447-z
22. Hill-Chapman CR, Herzog TK, Maduro RS. Aligning over the child: parenting alliance mediates the association of autism spectrum disorder atypicality with parenting stress. Dev Disabil Res Rev. (2013) 34:1498–504. doi: 10.1016/j.ridd.2013.01.004
23. Theule J, Wiener J, Tannock R, Jenkins JM. Parenting stress in families of children with ADHD: a meta-analysis. J Emot Behav Disord. (2013) 21:3–17. doi: 10.1177/1063426610387433
24. Brobst J, Clopton J, Hendrick S. Parenting children with autism spectrum disorders: the couple's relationship. Focus Autism Other Dev Disabil. (2009) 24:38–49. doi: 10.1177/1088357608323699
25. Hartley SL, Barker ET, Seltzer MM, Greenberg JS, Floyd FJ. Marital satisfaction and parenting experi-ences of mothers and fathers of adolescents and adults withautism. AAIDD. (2011) 116:81–95. doi: 10.1352/1944-7558-116.1.81
26. Ekas NV, Whitman TL. Autism symptom topography and maternal socioemotional functioning. Am J Intellect Dev Disabil. (2010) 115:234–49. doi: 10.1352/1944-7558-115.3.234
27. Laister D, Vivanti G, Marschik PB, Fellinger J, Holzinger D. Enhancement of social communication behaviours in young children with autism affects maternal stress. Front Psychiatry. (2021) 12:797148. doi: 10.3389/fpsyt.2021.797148
28. Andrés-Roqueta C, Katsos N. The contribution of grammar, vocabulary and theory of mind in pragmatic language competence in children with autistic spectrum disorders. Front. Psychol. (2017) 8:996. doi: 10.3389/fpsyg.2017.00996
29. Andrés-Roqueta C, Katsos N. A distinction between linguistic social pragmatics helps the precise characterization of pragmatic challenges in children with autism spectrum disorders developmental language disorder. J Speech Lang Hear Res. (2020) 63:1494–508. doi: 10.1044/2020_JSLHR-19-00263
30. Carruthers S, Taylor L, Sadiq H, Tripp G. The profile of pragmatic language impairments in children with ADHD: a systematic review. Dev. Psychopathol. (2021) 1–23. doi: 10.1017/S0954579421000328
31. Garrido D, Carballo G, Franco V, García-Retamero R. Dificultades de comprensión del lenguaje en niños no verbales con trastornos del espectro autista y sus implicaciones en la calidad de vida familiar. Rev Neurol. (2015) 60:207–14. doi: 10.33588/rn.6005.2014226
32. Ekas NV, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. J Autism Dev Disord. (2010) 40:1274–84. doi: 10.1007/s10803-010-0986-y
33. Hall HR, Graff JC. The relationships among adaptive behaviours of children with autism, family support, parenting stress, and coping. Issues Compr Pediatr Nurs. (2011) 34:4–25. doi: 10.3109/01460862.2011.555270
34. Ekas NV, Whitman TL, Shivers C. Religiosity, spirituality, and socioemotional functioning in mothers of children with autism spectrum disorder. J Autism Dev Disord. (2009) 39:706–19. doi: 10.1007/s10803-008-0673-4
35. Lovell B, Moss M, Wetherell M. The psychosocial, endocrine and immune consequences of caring for a child with autism or ADHD. Psychoneuroendocrinology. (2012) 37:534–42. doi: 10.1016/j.psyneuen.2011.08.003
36. Suzuki K, Kobayashi T, Moriyama K, Kaga M, Hiratani M, Watanabe K, et al. Development and evaluation of a parenting resilience elements questionnaire (PREQ) measuring resiliency in rearing children with developmental disorders. PLoS ONE. (2015) 10:e0143946. doi: 10.1371/journal.pone.0143946
37. Cattik M. The relationship between social support and self-efficacy levels of parents of children with developmental disabilities and life satisfaction levels. M.Sc. Turkey: Institute of Educational Sciences, Special Education (2015).
38. Karaman E, Efilti E. Investigation of social support perception and self-esteem as predictors of psychological resilience of parents who have children with special educational needs. Asian J Educ Training. (2019) 5:112–20. doi: 10.20448/journal.522.2019.51.112.120
39. Elfiti K. Investigating the psychological resilience of fathers with mentally handicapped children. Int Electron J Elementary Educ. (2019) 11:353–60. doi: 10.26822/iejee.2019450793
40. Greeff AP, Nolting C. Resilience in families of children with developmental disabilities. Fam Syst Health. (2013) 31:396–405. doi: 10.1037/a0035059
41. Raven JC. Manual for the Coloured Progressive Matrices (Revised). Windsor, UK: NFER-Nelson (1984).
42. Raven JC, Court JH, Raven J. Manual for the Raven's Progressive Matrices and Vocabulary Scales. Oxford: Oxford Psychologist Press (1990).
43. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
44. Mendoza E, Carballo G, Muñoz J, Fresneda MD. CEG: Test de Comprensión de Estructuras Gramaticales [Grammatical Structures Comprehension Test]. Madrid: TEA Ediciones (2005).
45. Bishop DVM. Test for Reception of Grammar. Medical Research Council. Manchester: Chapel Press (1983).
46. Dunn LM, Dunn LM, Arribas D. PPVT-III Peabody, Test de Vocabulario en Imágenes. Madrid: TEA Ediciones (2006).
47. Pons F, Harris PL. Test of Emotion Comprehension (TEC). Spanish versión. Oxford: Oxford University (2000).
48. Pons F, Harris PL. Longitudinal change and longitudinal stability of individual differences in children's emotion understanding. Cognit Emot. (2005) 19:1158–74. doi: 10.1080/02699930500282108
49. Pons F, Harris PL, Doudin PA. Teaching emotion understanding. Eur J Psychol Educ. (2002) 17:293–304, doi: 10.1007/BF03173538
50. Tomczak M, Tomczak E. The need to report effect size estimates revisited. Trends Sport Sci. (2014) 1:19–25. Available online at: http://tss.awf.poznan.pl/files/3_Trends_Vol21_2014__no1_20.pdf (accessed February 4, 2022).
51. Greenberg JS, Seltzer MM, Krauss MW, Chou RJA, Hong J. The effect of quality of the relationship between mothers and adult children with schizophrenia, autism, or Down syndrome on maternal well-being: the mediating role of optimism. Am J Orthopsychiatry. (2004) 74:14–25. doi: 10.1037/0002-9432.74.1.14
52. Cornejo N. Comparison of the levels of mental load and resilience possessed by families with children with functional diversity compared to families with children without functional diversity. R. Psicol. Educ. (2022) 17:79–96. doi: 10.23923/rpye2022.01.218
53. Bågenholm A, Gillberg C. Psychosocial effects on siblings of children with autism and mental retardation: a population-based study. J Ment Defic Res. (1991) 35:291–307. doi: 10.1111/j.1365-2788.1991.tb00403.x
54. Lindsey R, Barry T. Protective factors against distress for caregivers of a child with autism spectrum disorder. J Autism Dev Disord. (2018) 48:1092–107. doi: 10.1007/s10803-017-3372-1
55. Lu MH, Wang GH, Lei H, Shi ML, Zhu R, Jiang F. Social support as mediator and moderator of the relationship between parenting stress and life satisfaction among the Chinese parents of children with ASD. J Autism Dev Disord. (2018) 48:1181–8. doi: 10.1007/s10803-017-3448-y
56. Pozo P, Sarriá E, Brioso A. Family quality of life and psychological well-being in parents of children with autism spectrum disorders: a double ABCX model. J Intellect Disabil Res. (2014) 58:442–58. doi: 10.1111/jir.12042
57. Luong J, Yoder MK, Canham D. Southeast Asian parents raising a child with autism: a qualitative investigation of coping styles. J Sch Nurs. (2009) 25:222–9. doi: 10.1177/1059840509334365
58. Iadarola S, Levato L, Harrison B, Smith T, Lecavalier L, Johnson C, et al. Teaching parents behavioral strategies for autism spectrum disorder (ASD): effects on stress, strain, and competence. J Autism Dev Disord. (2018) 48:1031–40. doi: 10.1007/s10803-017-3339-2
59. Karst JS, Van Hecke AV, Carson AM, Stevens S, Schohl K, Dolan B. Parent and family outcomes of PEERS: a social skills intervention for adolescents with autism spectrum disorder. J Autism Dev Disord. (2015) 45:752–65. doi: 10.1007/s10803-014-2231-6
60. Fang X, Vincent W, Calabrese SK, Heckman TG, Sikkema KJ, Humphries DL, et al. Resilience, stress, and life quality in older adults living with HIV/AIDS. Aging Ment Health. (2015) 19:1015–21. doi: 10.1080/13607863.2014.1003287
61. Deist M, Greeff AP. Living with a parent with dementia: a family resilience study. Dementia. (2017) 16:126–41. doi: 10.1177/1471301215621853
62. Jones L, Hastings RP, Totsika V, Keane L, Rhule N. Child behavior problems and parental well-being in families of children with autism: the mediating role of mindfulness and acceptance. Am J Intellect Dev Disabil. (2014) 119:171–85. doi: 10.1352/1944-7558-119.2.171
Keywords: parental resilience, neurodevelopmental disorders (NDD), autistic spectrum disorders (ASD), attention-deficit/hyperactivity disorder (ADHD), developmental language disorder (DLD), social cognition, structural language, social support
Citation: Flores-Buils R and Andrés-Roqueta C (2022) Factors influencing resilience of parents with children with neurodevelopmental disorders: The role of structural language, social cognition, and social support. Front. Psychiatry 13:886590. doi: 10.3389/fpsyt.2022.886590
Received: 28 February 2022; Accepted: 22 August 2022;
Published: 08 September 2022.
Edited by:
Daniel Holzinger, Hospitaller Brothers of Saint John of God Linz, AustriaReviewed by:
Cynthia Y. Y. Lai, Hong Kong Polytechnic University, Hong Kong SAR, ChinaCopyright © 2022 Flores-Buils and Andrés-Roqueta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raquel Flores-Buils, ZmxvcmVzQHVqaS5lcw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.