- Department of Psychiatry, Dr. Carol Davila University Emergency Central Military Hospital, Bucharest, Romania
Substance use disorders (SUDs) are an extremely challenging category of disorders because of the high rate of relapse, lower life expectancy, important rate of psychiatric and somatic co-morbidity, lack of patients' insight during most of the disease duration, healthcare costs, etc. One of the reasons to consider these disorders very difficult for physicians and the healthcare system is the lack of adequate pharmacological agents with long-term proven efficacy. So far, there are no Food and Drug Administration (FDA) or European Medicines Agency (EMA)-approved treatments for most of the SUDs, except for alcohol use disorder, nicotine use disorder, and opioid use disorder. Immunotherapy has been considered a possible solution to SUDs because it may selectively target a certain drug of abuse, it may have a long-lasting effect (several weeks or months), and it ensures an adequate therapeutic adherence. The objective of this paper was to establish the current stage of research in the field of SUDs vaccines, based on a brief literature review. Vaccines for cocaine and nicotine dependence have reached phase III trials, while other researchers are focusing on passive immunization therapy for methamphetamine use disorder. New generations of vaccines are currently explored, and they are based on superior technologies compared to the first generation of immune therapy (e.g., viral transfer genes, more immunogenic adjuvants, or higher specificity haptens). Therefore, finding immune therapies for substance use disorders SUDs remains a matter of interest, and this approach may be useful for the management of an extremely dangerous and versatile psychiatric pathology.
Introduction
Substance use disorders (SUDs) represent a complex and polymorphic pathology with severe psychological, social, and biological negative consequences (1). SUDs are responsible for significant rates of worldwide morbidity, mortality, quality of life impairments, financial and social burden, thus representing a major challenge for patients, their physicians, and caregivers, but also for the society and health care systems (2, 3). Despite SUDs' importance, there are currently only a few U.S. Food and Drug Administration (FDA) or European Medicines Agency (EMA)-approved medications, and for only a limited number of addictions, i.e., alcohol, nicotine, and opioid dependence (2, 3).
In the context of the COVID-19 pandemic, the problem of SUDs received increased attention, since recreational drug use may be perceived as a harmless way to cope with lockdown or isolation stress, and not as a gateway to addiction (4). Psychosocial stressors are well-known risk factors for SUDs, therefore search for new methods to cope with the challenge of substance abuse received a new impulse in the pandemic context (4, 5).
SUDs are frequently associated with psychiatric disorders or somatic diseases comorbidity, a phenomenon that lower life expectancy, alters patients' adherence to other, prescribed psychotropic or somatic treatments, increases healthcare costs, and decreases the probability of a complete functional recovery (6–8). Because there is a limited choice of drugs available for the treatment of SUDs, and these options are often criticized for the high rates of relapse, new strategies are acutely needed for these patients (9). The need to re-configure SUDs therapeutic management using a long-term approach, and not treatments focused only on the acute episodes of substance abuse, is supported by evidence like patients' lack of insight, high rate of treatment discontinuation, high risk of complications, and personality factors that are maintaining the addictive patterns (9–11). Therefore, a change of paradigm from orally-administered medicines to long-acting injectable treatments may be beneficial for patients, and the use of intramuscular injectable extended-release naltrexone is the first step in this direction (10, 12). Unlike oral naltrexone, the injectable formula does not imply first-pass metabolism in the liver, which allows for lower doses administration and lower peak plasma concentrations (10, 12).
Immunotherapy is another way to conceive a long-term treatment for SUDs with a focus on increased adherence and reduced risk for relapse. Another advantage of immunotherapy is targeting selective drugs of abuse, e.g., heroin, which is different from the non-selectivity of currently available, orally administered μ-opioid receptor (MOR) antagonists, for example (13). Unlike orally administered MOR antagonists, SUDs vaccines do not imply the need for prior detoxification, nor do they require daily supervision of treatment adherence.
The development of a vaccine, based on a hapten structurally similar to the target drug, which is conjugated to an immunogenic carrier protein, is considered able to elicit serum IgG antibodies and was associated with positive results in preclinical models of addiction (e.g., decreased drug self-administration, and attenuated the reward effects) (14). These antibodies are expected to sequester the target drug in order to prevent its entry into the brain, acting as an antagonist for the circulating drugs of abuse (14).
Several challenges are difficult to overcome, although significant progress has been made in this domain: lack of protection against a structurally dissimilar drug with the same pharmacodynamic properties as the drug of choice, lack of a significant effect over craving, which is responsible for relapse, and significant variability in antibody formation and their duration of life within blood circulation (15). The nature of haptens and adjuvants is very important in order to obtain a sustained and efficient response after the vaccine administration, in patients with SUDs. Despite the failure of first-generation conjugate vaccines against cocaine and nicotine in clinical trials, second-generation vaccines have shown superior results in preclinical models (14).
Regarding the general benefits of vaccines for SUDs, it is important to mention that this approach can offer the possibility of much closer treatment adherence monitoring (because the injectable treatment is administered only by a health care specialist, and it is not self-administered as the oral treatment), there are virtually no pharmacokinetic interactions, and these vaccines may significantly decrease the risk of overdose. The limitations are related to the variable titer of anti-bodies produced after vaccines administration, different selectivity and affinity of these products, and to the need to accept an injectable treatment by patients with low motivation for any type of therapy.
Combining multiple types of immune therapy, like an association of anti-drug antibodies with synthetic enzymes -that are able to stimulate abused substances metabolism- has also been investigated in preclinical models of SUDs (16). The purpose of this strategy was to explore the possible complementary action of anti-cocaine antibodies when added to cocaine hydroxylase (CoH) to decrease the drug uptake in the brain and to block the centrally-evoked locomotor stimulation (16). Synergistic actions of these types of interventions warrant further exploration in the treatment of selected SUDs (16). These methods involve viral gene transfer for a specific enzyme, e.g., CoH derived from human butyrylcholinesterase with the help of an adeno-associated viral vector, but these interventions are not yet approved for human trials (17).
Objective
The primary objective of this review was to establish the stage of the current research in the field of SUD vaccines. The analysis of efficacy and tolerability of the investigational products targeting SUDs was based on a brief review of the clinical trials.
Methodology
The search for investigational immunization products targeting SUDs included main clinical trials repositories run by the United States National Library of Medicine and the National Institutes of Health (clinicaltrials.gov) and the European Union (EU Clinical Trial Register). All phases of clinical investigation (I to IV) were considered for this review if trials were focused on specific SUDs and enrolled adult population.
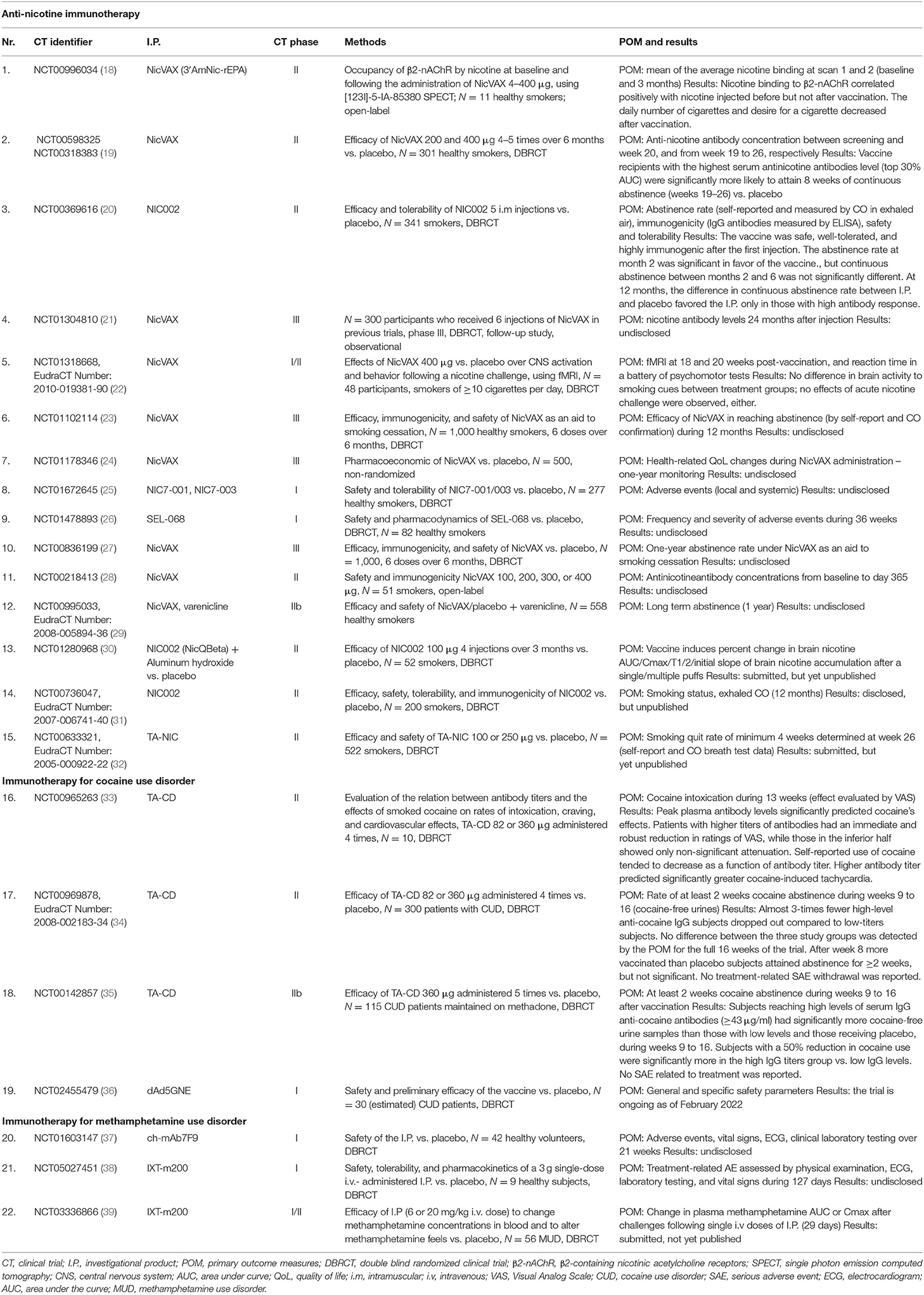
In the second stage of this review, identifiers of the first stage-collected trials were included as keywords in the main electronic databases (PubMed, MEDLINE, Cochrane, Web of Science (Core Collection), PsychINFO, Scopus, and EMBASE in order to find associated, relevant articles containing study results. All in-extenso papers found in this stage were reviewed, and data about clinical trials methodology and results were synthesized in Table 1. If no published, relevant data were found in the second stage for specific trials, only methodological aspects were mentioned in Table 1. Data referring to animal studies were not included in the review.
Results
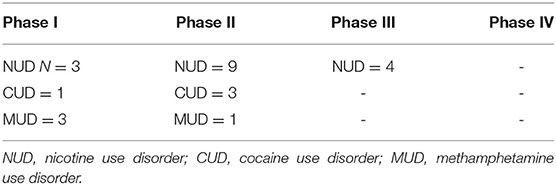
A number of 22 phase I to III clinical trials referring to nicotine use disorder, cocaine use disorder, and methamphetamine use disorder, including both active and passive immunization products, were found after the primary search. Out of these 22 trials, only 7 have been identified as having published results in the secondary search. The vast majority of identified trials were phase II, targeting nicotine use disorder, using active immunization (NicVAX, NIC002, TA-NIC, NIC7-001/003, and SEL-068), and presented mixed results (18–20). The tolerability of these vaccines was good, but continuous abstinence was significant only in subjects with the highest serum antinicotine levels (19), or it was significant only in short term (20). No published results of phase III trials evaluating vaccines for nicotine use disorder were found (21–24).
Immunization for patients with cocaine use disorder (TA-CD, dAd5GNE) was explored in phase I and II clinical trials (33–36). Self-reported use of cocaine tended to decrease as a function of antibody titer in one trial (33), while in another trial subjects reaching high levels of serum IgG anti-cocaine antibodies (≥43 μg/ml) had significantly more cocaine-free urine samples than those with low levels and those receiving placebo, during week 9–16 (35). Although yet another trial with TA-CD did not reach its primary outcome after week 8 more vaccinated than placebo subjects attained abstinence for ≥2 weeks, without reaching the significance level (34).
Immunotherapy for methamphetamine use disorder is still in its early phase, and passive immunization is the only clinically explored option (37–39). This therapy is based on human-murine chimeric monoclonal antibodies, which are considered able to bind methamphetamine with presumed high specificity and affinity (37–39). Unfortunately, no results of clinical trials are yet available to support this claim.
The evolution of the research in the field of immunotherapy for SUD is reflected by the development of second-generation investigational products. This progress was fueled by the need to find newer haptens and better carriers, able to induce more specific and intense immune responses, which translate to better efficacy. Also, adjuvants are important for triggering a persistent immune response, and new substances from this category are needed, besides aluminum.
In the case of anti-nicotine vaccines, the first generation of products used 3'-aminomethyl nicotine conjugated with Pseudomonas aeruginosa r-exoprotein in case of NicVAX, a non-infectious pseudo-viral particle (VLP) in case of NIC-002, or recombinant cholera toxin B (rCTB) subunit as transporter molecule for TA-NIC (18, 20). In the case of second-generation products, the transporter is represented by cross-reacting material (CRM) for NIC7-001, and a nanoparticle technology (targeted synthetic particles) for SEL-068 (25, 26). In the case of cocaine use disorder, the first-generation vaccine, TA-CD, used rCTB, while the newest investigational product, dAd5GNE, used the proteins of a modified adenovirus conjugated with a cocaine analog (33–36).
An overview of the trials presented in Table 1 shows the need to find better defined primary outcome measures and to extend the duration of monitoring over 12 months. Also, trials with active comparators should be designed, and quantification of the patients' tolerability and quality of life during the study could also be useful.
Conclusions
The limited number of phase III clinical trials detected by this review (N = 4) indicates the need to re-evaluate the conceptual design of immune therapy in SUDs (Table 2). Despite the mixed, and mostly negative evidence of efficacy for the first-generation conjugate vaccines against cocaine and nicotine in clinical trials, second-generation vaccines are developing, thus renewing the potential clinical utility of active immunization in the treatment of substance use disorder (14). Even the first generation trials contained several positive results, but only in specific sub-populations, i.e., patients able to develop high levels of antibodies targeting the specific drug of abuse (19, 35). No significant tolerability and safety aspects were reported in trials with published results, which monitored the adverse events rate.
As limitations of the review, it is important to mention that no data about the current status of each investigational product were collected, as no such information has been found in the searched databases. Note releases from the manufacturers' sites regarding these products were not included in this review. Preclinical studies may be important to review, but this article was focused only on human trials.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Daley DC. Family and social aspects of substance use disorders and treatment. J Food Drug Anal. (2013) 21:S73–S76. doi: 10.1016/j.jfda.2013.09.038
2. Volkow NA. Personalizing the treatment of substance use disorders. Am J Psychiatry. (2020) 177:113–6. doi: 10.1176/appi.ajp.2019.19121284
3. Connery HS, McHugh RK, Reilly M, Shin S, Greenfield SF. Substance use disorders in global mental health delivery: epidemiology, treatment gap, and implementation of evidence-based treatments. Harv Rev Psychiatry. (2020) 28:316–27. doi: 10.1097/HRP.0000000000000271
4. Vasiliu O, Vasile D, Vasiliu DG, Ciobanu OM. Quality of life impairments and stress coping strategies during the Covid-19 pandemic isolation and quarantine- A web-based survey. Rom J Mil Med. (2021) 124:10–21. doi: 10.55453/rjmm.2021.124.1.2
5. López-Pelayo H, Aubin HJ, Drummond C, Dom G, Pascual F, Rehm J, et al. “The post-COVID era”: challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med. (2020) 18:241. doi: 10.1186/s12916-020-01693-9
6. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. (2006) 101:76–88. doi: 10.1111/j.1360-0443.2006.01592.x
7. Langås AM, Malt UF, Opjordsmoen S. Comorbid mental disorders in substance users from a single catchment area- a clinical study. BMC Psychiatry. (2011) 11:25. doi: 10.1186/1471-244X-11-25
8. Onyeka IN, Høegh MC, Eien EMN, Nwaru BI, Melle I. Comorbidity of physical disorders among patients with severe mental illness with and without substance use disorders: a systematic review and meta-analysis. J Dual Diagn. (2019) 15:192–206. doi: 10.1080/15504263.2019.1619007
9. McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. J Am Med Assoc. (2000) 284:1689–95. doi: 10.1001/jama.284.13.1689
10. Vasiliu O. Maintenance pharmacologic therapies for opioid use disorders: beyond opioid agonists. Rom J Mil Med. (2019) CXXII:52–70.
11. Vasiliu O. Current status of evidence for a new diagnosis: food addiction- A literature review. Front Psychiatry. (2022) 12:824936. doi: 10.3389/fpsyt.2021.824936
12. Jarvis BP, Holtyn AF, Subramaniam S, Tompkins DA, Oga EA, Bigelow GE, et al. Extended-release injectable naltrexone for opioid use disorder: a systematic review. Addiction. (2018) 113:1188–209. doi: 10.1111/add.14180
13. Niciu MJ, Arias AJ. Targeted opioid receptor antagonists in the treatment of alcohol use disorders. CNS Drugs. (2013) 27:777–87. doi: 10.1007/s40263-013-0096-4
14. Bremer PT, Janda KD. Conjugate vaccine immunotherapy for substance use disorder. Pharmacol Rev. (2017) 69:298–315. doi: 10.1124/pr.117.013904
15. Kantak KM. Vaccines against drugs of abuse: a viable treatment option? Drugs. (2003) 63:341–52. doi: 10.2165/00003495-200363040-00001
16. Brimijoin S, Orson F, Kosten T, Kinsey B, Shen XY, White SJ, et al. Anti-cocaine antibody and butyrylcholinesterase-derived cocaine hydrolase exert cooperative effects on cocaine pharmacokinetics and cocaine-induced locomotor activity in mice. Chem Biol Interact. (2013) 203:212–16. doi: 10.1016/j.cbi.2012.08.015
17. Gao Y, Geng L, Orson F, Kinsey B, Kosten TR, Shen X, et al. Effects of anti-cocaine vaccine and viral gene transfer of cocaine hydrolase in mice on cocaine toxicity including motor strength and liver damage. Chem Biol Interact. (2013) 203:208–11. doi: 10.1016/j.cbi.2012.08.006
18. Esterlis I, Hannestad JO, Perkins E, Bois F, D'Souza DC, Tyndale RF, et al. Effect of a nicotine vaccine on nicotine binding to β2*-nicotinic acetylcholine receptors in vivo in human tobacco smokers. Am J Psychiatry. (2013) 170:399–407. doi: 10.1176/appi.ajp.2012.12060793
19. Hatsukami DK, Jorenby DE, Gonzales D, Rigotti NA, Glover ED, Oncken CA, et al. Immunogenicity and smoking-cessation outcomes for a novel nicotine immunotherapeutic. Clin Pharmacol Ther. (2011) 89:392–9. doi: 10.1038/clpt.2010.317
20. Cornuz J, Zwahlen S, Jungi WF, Osterwalder J, Klinger K, van Melle G, et al. A vaccine against nicotine for smoking cessation: a randomized controlled trial. PLoS ONE. (2008) 3:e2547. doi: 10.1371/journal.pone.0002547
21. Nabi Pharmaceuticals. A follow-up study to assess long-term immunogenicity and safety of NicVAX/Placebo as an aid to smoking cessation. Available online at: https://www.clinicaltrials.gov/ct2/show/NCT01304810 (accessed: February 10, 2022).
22. Havermans A, Vuurman EF, van der Hurk, Hoogsteder P, van Schayck OCP. Treatment with a nicotine vaccine does not lead to changes in brain activity during smoking cue exposure or a working memory task. Addiction. (2014) 109:1260–7. doi: 10.1111/add.12577
23. Nabi, Pharmaceuticals. A Second Study of NicVAX/Placebo as an Aid for Smoking Cessation. Available online at: https://clinicaltrials.gov/ct2/show/NCT01102114 (accessed: February 12, 2022).
24. Nabi, Pharmaceuticals. Pharmacoeconomic Assessment in Nabi-4514 and Nabi-4515 Phase 3 Studies. Available online at: https://clinicaltrials.gov/ct2/show/NCT01178346 (accessed: February 12, 2022).
25. Pfizer. A Study to Assess the Safety and Tolerability of Different Doses of PF-05402536 and PF-06413367 in Healthy Adult Smokers. Available online at: https://clinicaltrials.gov/ct2/show/NCT01672645 (accessed: February 20, 2022).
26. Selecta, Biosciences, Inc. Safety and Pharmacodynamics of SEL_068 Vaccine in Smokers and Non-Smokers. Available online at: https://clinicaltrials.gov/ct2/show/NCT01478893 (accessed: February 20, 2022).
27. Nabi, Pharmaceuticals. NicVAX/placebo as an Aid for Smoking Cessation. Available online at: https://clinicaltrials.gov/ct2/show/NCT00836199. (accessed: February 12, 2022).
28. Nabi, Pharmaceuticals. Safety and Effectiveness of NicVAX In Treating Nicotine-Dependent Individuals. Available online at: https://clinicaltrials.gov/ct2/show/NCT00218413 (accessed: February 12, 2022).
29. Maastricht University Medical Center. Efficacy and Safety of NicVAX co-Administered With Varenicline (Champix). Available online at https://clinicaltrials.gov/ct2/show/NCT00995033. (accessed: February 16, 2022).
30. Alexey, Mukhin. Improving the Efficacy of Anti-Nicotine Immunotherapy (PETNic002). Available online at: https://clinicaltrials.gov/ct2/show/NCT01280968 (accessed: February 16, 2022).
31. Novartis. Study to Evaluate the Efficacy, Safety, Tolerability and Immunogenicity of 100 μg NIC002 Vaccine in Cigarette Smokers Who Are Motivated to Quit Smoking. Available online at: https://clinicaltrials.gov/ct2/show/NCT00736047 (accessed: February 16, 2022).
32. Celtic, Pharma Development Sevices. Study of TA-NIC to Assess the Efficacy and Safety of the Vaccine as an Aid to Smoking Cessation. Available online at: https://clinicaltrials.gov/ct2/show/results/NCT0063332 (accessed: February 20, 2022).
33. Haney M, Gunderson EW, Jiang H, Collins ED, Foltin RW. Cocaine-specific antibodies blunt the subjective effects of smoked cocaine in humans. Biol Psychiatry. (2010) 67:59–65. doi: 10.1016/j.biopsych.2009.08.031
34. Kosten TR, Domingo CB, Shorter D, Orson F, Green C, Somoza E, et al. Vaccine for cocaine dependence: a randomized double-blind placebo-controlled efficacy trial. Drug Alcohol Depend. (2014) 140:42–7. doi: 10.1016/j.drugalcdep.2014.04.003
35. Martell BA, Orson FM, Poling J, Mitchell E, Rossen RD, Gardner T, et al. Cocaine vaccine for the treatment of cocaine dependence in methadone-maintained patients: a randomized, double-blind, placebo-controlled efficacy trial. Arch Gen Psychiatry. (2009) 66:1116–23. doi: 10.1001/archgenpsychiatry.2009.128
36. Weill Medical College of Cornell University. Safety study of a disrupted adenovirus (Ad) serotype cocaine vaccine for cocaine-dependent individuals. Available online at: https://clinicaltrials.gov/ct2/show/NCT02455479 (accessed: February 20, 2022).
37. InterveXion, Therapeutics. Safety Study of Ch-mAb7F9 for Methamphetamine Abuse. Available online at: https://clinicaltrials.gov/ct2/show/NCT01603147 (accessed: February 20, 2022).
38. InterVexion, Therapeutics. Safety, Tolerability, and Pharmacokinetics of IXT-m200. Available online at: https://clinicaltrials.gov/ct2/show/NCT05027451 (accessed: February 20, 2022).
39. InterveXion, Therapeutics. Study of Antibody for Methamphetamine Outpatient Therapy (STAMPOUT). Available online at: https://clinicaltrials.gov/ct2/show/NCT03336866 (accessed: February 20, 2022).
Keywords: substance use disorders, vaccines, immune therapy, cocaine use disorder, nicotine use disorder
Citation: Vasiliu O (2022) Current Trends and Perspectives in the Immune Therapy for Substance Use Disorders. Front. Psychiatry 13:882491. doi: 10.3389/fpsyt.2022.882491
Received: 23 February 2022; Accepted: 11 April 2022;
Published: 28 April 2022.
Edited by:
Kenneth Michael Dürsteler, University Psychiatric Clinic Basel, SwitzerlandReviewed by:
Leandro Franco Vendruscolo, National Institute on Drug Abuse (NIH), United StatesCopyright © 2022 Vasiliu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Octavian Vasiliu, b2N0YXZ2YXNpbGl1QHlhaG9vLmNvbQ==
 Octavian Vasiliu
Octavian Vasiliu