
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 17 May 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.880331
This article is part of the Research Topic Mental-Health-Related Stigma and Discrimination: Prevention, Role, and Management Strategies View all 16 articles
 Majid Zare-Bidaki1
Majid Zare-Bidaki1 Alireza Ehteshampour1
Alireza Ehteshampour1 Masoud Reisaliakbarighomi2
Masoud Reisaliakbarighomi2 Robabeh Mazinani3
Robabeh Mazinani3 Mohammad Reza Khodaie Ardakani3
Mohammad Reza Khodaie Ardakani3 Arash Mirabzadeh2,3
Arash Mirabzadeh2,3 Rosa Alikhani3
Rosa Alikhani3 Mehdi Noroozi3
Mehdi Noroozi3 Fereshteh Momeni3
Fereshteh Momeni3 Amir Dehghani Samani1
Amir Dehghani Samani1 Mohammad Mahdi Mehrabi Tavana4
Mohammad Mahdi Mehrabi Tavana4 Aliakbar Esmaeili5,6
Aliakbar Esmaeili5,6 S. Bentolhoda Mousavi2,3*
S. Bentolhoda Mousavi2,3*Objectives: Applying technologies such as virtual reality (VR) in education has gained popularity especially in comprehending abstract and subjective phenomena. Previous studies have shown that applying a virtual reality simulation of psychosis (VRSP) is useful in increasing knowledge and empathy toward patients. Here, the efficacy of using VRSP in altering stigma, empathy and knowledge as well as side effects have been assessed in medical students in comparison with the routine education (visiting the patients).
Method: After attending one session of lecture about positive psychotic symptoms, medical students were allocated to two groups: experiencing one session of VRSP or visiting patients under supervision as routine practice in the ward. Before and after the first session and after the second one, questionnaires of knowledge, empathy and stigma were filled by students. Finally, the results were compared in two groups.
Results: Both interventions were effective in reducing stigma as well as increasing knowledge and empathy toward patients with psychotic experiences. VRSP could significantly reduce stigma and increase knowledge and empathy compared with the traditional visiting patients under supervision. The side effects were minimal and ameliorated right after the experience.
Conclusion: VRSP is an effective tool in decreasing stigma and increasing empathy and knowledge of the students and can be incorporated in psychiatric education with minimal side effects.
Psychiatric disorders are associated with an overwhelming stigma, not only among general population, but also within healthcare providers and students especially the novitiates (1–3). Stigma directly affects help-seeking behaviors (4–6). In case of mental health problems, holding negative attitudes toward psychiatric disorders and perceived negative social consequences related to them, leads to denial, which subsequently results in postponing the necessary treatment (4). Even the attitudes, manners, and speech of mental health professionals can nourish stigma, which is called the “Iatrogenic stigma” (7, 8).
Anti-stigma movements have proposed different interventions to overcome the stigma toward patients, among which social interaction in combination with education is the most effective one (2, 9). Different curricula applied in psychiatric education have been shown to decrease stigma toward patients with mental illness through education as well as direct contact with patients (10, 11).
Recent literature suggests that simulations of first-hand experiences in virtual environments can decrease implicit stereotypes and reduce stigma (9, 12). Utilizing compound contact-based interventions such as watching film and live contact can considerably improve outcomes of attitude and knowledge toward mental illness (2, 13). There are, however, concerns over a mere simulation of psychotic disorders without any education as such interventions may prove counterproductive (12). This is an important criticism that efforts of reducing stigma through focusing on first-hand experience simulation, might lead to an excessive focus on symptom experience without appreciation for the “whole person” that one might obtain from a contact experience.
Educational methods have improved dramatically in recent years and incorporating innovative technologies such as virtual reality (VR) into traditional pedagogic methods has gained popularity. Literature suggests that utilizing VR, as an immersive environment, can increase motivation, engagement, and the time spent for learning in students. Using VR in education promotes students’ ability in cognitive tasks and indorses affective and psychomotor skills (14, 15). VR can also improve students’ knowledge, empathy, and reduce stigma toward patients with mental health disorders (16, 17). The graphical quality and the sense of presence (immersion) have been proposed to be important factors affecting learning outcomes (14, 18).
Virtual environments have several applications in psychiatric education. Simulating a complex or nontangible condition for students to get involved in -as a first-person experience- is one of these applications (16, 17). Positive psychotic symptoms such as hallucinations and delusions are subjective and complicated experiences that are difficult to understand. Hallucinations are perceptions without any external source and delusions are misbeliefs without any factual evidence to support them (17, 19, 20). These symptoms present not only in psychiatric disorders but also in other medical conditions such as hearing loss or neurological conditions (20, 21). Despite the prevalence, students often complain of the difficulty of understanding the symptoms. On the other hand, holding negative attitudes towards patients experiencing psychotic symptoms (stigma) is common among students and health care providers (7, 17, 22, 23).
Limited studies have assessed the outcomes of incorporating VR in routine education in reducing stigma toward patients. Previous studies suggest that simulating first-person experiences in VR can effectively increase knowledge of the symptoms and empathy toward patients with minor side effects such as mild cybersickness (17, 24). For instance, Formosa et al. simulated positive psychosis symptoms in a VR setting; their study suggests that one session of experiencing it could increase students’ knowledge, attitude, and improve empathy toward patients with psychosis (16). In their study, however, questionnaires only were applied before and after applying VR; where VR stands in comparison with the current methods of education is still under question.
In another study, Yellowlees et al. developed a VR psychosis simulation on an internet platform and showed the user-friendliness and feasibility of applying it as a practical method (24). In their study, participants filled a questionnaire only after experiencing the simulation so there was no comparison whether before or after or with other methods, and the study population was only limited to a certain group of internet users.
In this study, after simulating auditory hallucinations with persecutory content and reference delusion in a VR setting, we compared one session of virtual reality simulation of psychosis (VRSP) to the routine educational program- that is visiting patients under supervision as its counterpart in altering stigma, empathy, and knowledge about psychosis in medical students as well as evaluating potential side effects.
In this project, we assessed the effects of experiencing one session of virtual reality simulation of psychosis (VRSP) on stigma, empathy, and knowledge in medical students in comparison with the traditional learning style; that is, visiting patients at the psychiatric ward. In the first phase of the study, we have developed a simulation of psychotic experience in a VR setting with a scenario based on the real experiences of the patients and the consensus of a psychiatrist team. After providing consent, 10 patients with schizophrenia in remission were interviewed by two different psychiatrists for their experiments during their last psychotic episode. The documents were assessed by a panel of four psychiatrists for extracting the most prevalent themes. Among those, the ones that could be reproduced in a simulated environment (such as auditory hallucinations and some form of delusions) were chosen to be the content of the experiment. The VR environment provided a three-dimensional, 360-degree video that was displayed by a VR headset mounted on the user’s head (Figure 1). The basic graphical environment (patient’s home) was designed by the objects needed for the scenario (modeled by 3D Max, Maya, and After Effect software). For the production of special effects (for example: displaying the other homeowner, broadcasting meteorological reports on television, etc.), we utilized 4K resolution filming technology. The sounds were recorded using the Qubis software; to maximize the clarity and orientation of the sounds, each one tailored to different positions to the user. After rendering, the final VR file was easily accessible through any mobile operating system (Android or iOS) and could be displayed by a VR headset for 4 and a half minutes.
In this scenario, the experiencer assumes herself/himself in a position of a person who hears voices with persecutory content and experiences the TV news host sending her/him messages (delusion of reference) which were the most prevalent experience based on our interviews and are some of the prevalent forms of delusions and hallucinations (20, 21, 25). At first, the person assumes that she/he is sitting on a couch in a living room of an apartment which has been designed with some elements of Iranian culture, such as red carpet, calligraphy on the wall, and some famous Persian books on the table and in the shelf that cause the experiencer feeling familiar with the environment. The atmosphere is as much as possible neutral (with no dark color that causes feelings of horror), so it can be similar to real life. There is an actor, sitting in the living room, talking and leading the experiencer through several occasions, such as turning on/off the TV or asking her/him to do some favors, such as moving into the kitchen where some hallucinations happen.
Auditory hallucinations (three-dimensional sounds) start with the voice of knocking on the door several times and some voices (both adult male and female with real-life tone), asking the participant not to open the door as there might be some neighbors trying to hurt her/him. Voices also talk about the actor and tell the participants that he might have some intentions to hurt her/him (persecutory content). When the actor turns on the TV to watch some news, the host of the news keeps addressing the participant and trying to undervalue her/him with her words (simulating the process of delusions of reference). After the scenario leads the participant to the kitchen, the voices comment on her/his actions in the kitchen as the third person (running commentary).
Medical students in Iran train psychiatry during their clerkship by attending to the visits by an attending psychiatrist (a Faculty) or psychiatry residents as passive observers. That is, the attending or the psychiatry resident visits the patients and the trainees observe the process of interviewing and examining mental status. After several sessions of observation, they can interview one or more patients to gain psychiatry history for their final project. The first stage (passive observation) has been compared to VRSP in the current study.
The study population was all the 2nd and 3rd year medical students in the Birjand University of Medical Sciences, who haven’t passed any psychiatry course or training before. The inclusion criteria were: having no previous history of severe psychiatric disorders themselves or in their first degree families. No previous history of chronic types of headaches, vertigo or seizures. The exclusion criteria were developing any side effects during the experience. This study was approved by the Research Ethics boards of Birjand University of Medical Sciences (IR.BUMS.REC.1397.174).
Using Cohen standardized effect sizes, sample size was calculated 64 in each group and considering 10% attrition rate, the total of 72 students participated in each group [alpha = 0.05, power = 0.80, and Cohen’s d = 0.5 (a medium effect)]. After providing written informed consent, all participants who enrolled in the study with the convenient method of sampling took part in one session of a lecture on theoretical concepts targeting positive psychotic symptoms. The students were cluster-randomized and allocated to two groups: experiencing one session of VR Simulated Psychosis (VRSP) or visiting patients under supervision as the routine practice in the ward. Before and after the first session and after the second one, questionnaires of knowledge, stigma, empathy, and side effects were filled by students. Finally, the results were compared in two groups. We also conducted a telephone follow up after 1 week and 1 month to record the participants’ experience of any long-lasting side effects, as stressors can be related to the psychiatric symptoms if there is a reasonable temporal relationship to it, which according to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is considered 1 month (26).
As knowledge of basic psychological facts can be measured quantitatively (16, 24), participants completed a pen and paper educational achievement test, designed to assess knowledge of definitions and examples of delusions and hallucinations based on DSM-5 criteria. Two independent research assistants scored students’ answers by using a scoring guide to reduce the potential of subjective interpretation. In case of any discrepancy, the third rater would score the items independently. Inter-rater reliability analysis was done, and the average amount was counted for each student as the score of knowledge. The Persian version of the “Mental illness stigma by world psychiatric association” was used to assess positive and negative attitudes towards patients with psychotic symptoms. Its validity and reliability in Farsi have been documented by Nojomi et al. (27, 28). Also, the Persian version of the Jefferson Scale of Physician Empathy- students (S-version) was applied, which was validated by Shariat et al. (29, 30). For side effects, seven items were assessed by a 7-point Likert scale anchored between “1” indicating “none” and “7” signifying “extremely high”. Blurry vision, headaches, nausea, and dizziness were assessed as general side effects (Cybersickness) and difficulty in accepting reality, paranoia, and any change in auditory perception as psychological side effects. Researchers were trained to monitor participants in the VR group for distress and participants were told that they can discontinue anytime they felt distressed. The telephone follow-up was conducted according to the same checklist 1 week and 1 month after the study; if any of the participants reported any symptoms that has bothered them, could get a free visit by a psychiatrist or neurologist for further evaluations.
Analyses were performed by Statistical Package for Social Sciences (SPSS version 21.0). The independent t-test was performed to compare means in each stage. To consider the role of potential confounders, a univariate analysis of covariates was performed to compare means at the final assessment and the effect size was calculated. The descriptive statistics were also reported as means and standard deviations. In all analyses P-value < 0.05 was considered statistically significant.
Table 1 shows the demographic characteristics of participants in each group. The mean age of the two groups that visited patients and experienced VRSP were 20.38 ± 1.04 and 19.90 ± 1.47 respectively and had no significant difference (p = 0.843). 65 males and 79 females participated in the study and the analysis of the distribution between groups showed no significant difference between groups (P = 0.402) (Table 1). The mean scores and standard deviations of knowledge, empathy, and stigma in different stages of assessment have been shown in Table 2. There were 3 levels of assessment and for convenience, we showed them as level 1 indicating pretest, level 2 indicating assessment after one session of theory education, and level 3 as post interventions test. There was no significant difference between the scores of the two groups at baseline in variables of knowledge (p = 0.506), empathy (p = 0.161), and stigma (p = 0.450) based on the t-test analysis. The univariate analysis of covariates (ANCOVA) showed that VRSP could significantly increase knowledge (p < 0.000), decrease stigma (p < 0.000), and improve empathy (p < 0.000) toward patients in comparison with one session of visiting patients under supervision (Table 3). Table 4 shows the side effects of one session of experiencing VRSP. Most of the participants experienced no side effects and the minor side effects were reported by a few participants, which subsided quickly. No signs of distress were reported by research assistants and none of the participants withdrew from the study due to personal distress. In the follow-up study, neither after 1 week nor after 1 month, none of the participants in the VRSP group reported any problem asked according to the checklist, so there was no need for an in-person visit by specialists.
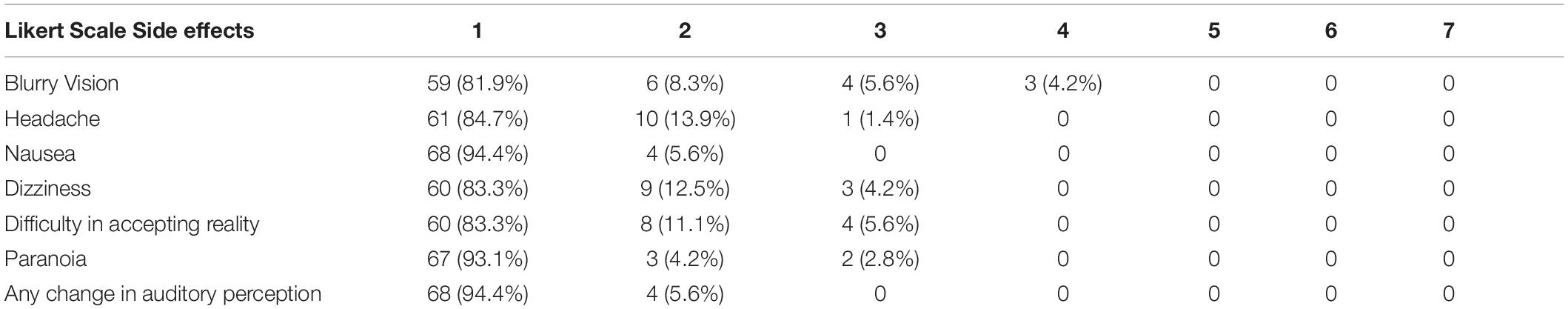
Table 4. Assessing side effects of one session of experiencing Virtual Reality Simulation of Psychosis.
The aim of this study was to assess the effects of experiencing one session of virtual reality simulation of psychosis (VRSP) on the stigma, empathy, and knowledge of medical students towards patients with psychosis in comparison with the routine training - that is visiting the patients in wards under supervision- as well as assessing any side effects. Highlighting the prominence of this study, to the best of our research, this is among the few head-to-head studies, examining the efficacy of incorporating virtual simulation in training, compared with routine educational program. There is minimal research regarding head-to-head studies comparing the two modalities (21).
In line with previous studies, the findings of the current study suggest that applying one session of VRSP can increase knowledge about psychosis (16, 17, 24), and this increase is significantly more than one session of visiting patients under supervision. Students, in this study, had no previous knowledge of the psychotic symptoms and this could reduce the potential bias in assessing the knowledge. VR has usages such as learning and training based on the constructivism theory of learning. VR can increase users’ knowledge about some concepts that are complicated and difficult to understand. In mental health disorders, subjective symptoms such as delusions and hallucinations are tough to perceive (16, 31). The constructivist perspective that VR fundament on, emphasizes building the knowledge based on the real-life experiences and VR can provide a semi-real-life environment for students to experience symptoms first hand.
To further explain the findings on knowledge, simulation in VR was consistent, that is all students experienced all the simulated symptoms in one session. Visiting patients under the supervision, on the other hand, has some limitations such as patients might have different mental status in each visit, leading to presentation of different symptomatology in each session (32). Moreover, patients might not be willing to or feel safe enough to reveal their inner experiences in a crowded setting, resulting in non-cooperativeness. Patients experience variety of symptoms and students have to observe and/or visit a number of patients in order to get familiar with a complete picture of the disorder manifestation. Immersive experiences in VR, can add to the benefits of the visits by providing the facility to experience more symptoms and removing distractions (14, 18, 33). The key point here is that VRSP cannot and should not assumed to replace visiting patients, but can be seen as an effective pedagogical tool that is used alongside visiting patients to address the limitations that students might face in wards.
In this study, both groups showed a reduction in stigma score after one session of visiting patients and after VRSP. In VRSP, however, the stigma scores decreased significantly compared with visiting patients. Whether and to what extent the direct contact with the patients affects stigma reduction is still controversial. On one hand, some literature suggest that direct contact with patients- whether it is a real in-person contact or a virtual one-can decrease stigma (2); anti-stigma movements propose different forms of interventions, among which social interaction in combination with education is the most effective one (2, 9). Also, curriculums applied in psychiatric education have decreased stigma toward patients with mental illness through education as well as direct contact with patients (10, 11). On the other hand, some literature suggest that mental health care givers that work in inpatient settings, are prone to have more stigmatizing attitudes toward patients due to several reasons such as burnout and associative stigma (3). Clinicians who work in inpatient settings often tend to work with patients with long-term conditions and worse prognosis which enhances the phenomena of “the clinician’s illusion.” (34), which might explain the mentioned stigma to some extent (3). In this study, the sample consisted of medical students without any history of psychiatric conditions themselves or in their first degree family members, therefore the mentioned mechanism of familiarity that might lead to increase stigma, was eliminated in this study.
There are lack of evidence to explain the mechanism of associative stigma- that is the phenomena of increased stigma in the first degree families of patients with severe psychiatric conditions and care givers. the proposed mechanisms consist of the burden of these disorders to families as well as burnout in care givers (3). The mediating role of empathy in theses process has not been explored yet. In this study the empathy scores increased in both interventions and whether the increase in empathy can be a mediating factor for decreasing stigma should be explored in future studies.
Some qualitative studies has extracted important themes mirroring associative stigma among mental health care providers: devaluating the occupation, media representation, and assumptions/expectations about the job. Publicly, psychiatry practice is frequently perceived as unproductive or even destructive (3). Moreover, medical students might see psychiatry as low status and non-priority (35). Applying technologies, such as VR, has shown to increase the motivation of students. However, assessing whether incorporating such technologies in psychiatric education would modify such attitudes needs more in depth studies.
Recent literature suggest that simulations of first hand experiences in virtual environments can decrease implicit stereotypes and reduce stigma (9, 12). Utilizing compound contact-based interventions such as watching film and live contact can considerably improve outcomes of attitude and knowledge toward mental illness (2, 13). This is consistent with our findings, confirming our hypothesis that using simulations incorporated into routine medical education can improve knowledge and attitudes towards stigmatizing others. There are, however, concerns over mere simulation of psychotic disorders without any education (12); in a study on the effects of a virtual reality simulator on perceptions of schizophrenia, Kalyanaraman et al., argued that using simulations of hallucination, without any education to participants might increase negative attitudes toward patients with schizophrenia (12). Efforts of reducing stigma through focusing on merely simulating the symptoms, might lead to an excessive focus on symptom experience without appreciation for the “whole person” that one might obtain from a contact based-experience. Therefore, we believe that education must be an important component in such interventions.
It is argued that simulations that portrays psychosis as a terrifying experience with dramatic environmental features in a dark or horrifying setting- in contrast with using neutral environmental cues-, might have negative effects on participants attitude towards patients (12). These are important ethical concerns; increasing literature suggest that interventions that seek to enhance empathy are required to represent the symptoms in an unbiased way and according to the real experiences of the subjects with whom empathy is to be enhanced. Using more realistic environmental features is more similar to the real experiences of people with psychotic disorders. In a study of simulating symptoms in an augmented reality (AR) environment, where the hallucinations are experienced in the actual environment (9), in line with our findings, simulation showed to be a promising approach in reducing stigma.
In recent years, VR studies have focused on promoting some concepts that are essential in human relationship such as empathy. The ability to empathize is a crucial skill for all mental health professionals and affects all aspects of psychiatric and psychological interventions (36, 37). In this study, both groups showed increase in empathic abilities-assessed by the Jefferson Scale of Physician Empathy- students (S-version). The VRSP group had significantly more empathy toward patients than students who visited patients under supervision. This confirms previous findings that suggests application of simulation of psychosis can increase empathy among students (16, 17) and general population (24).
Empathy has been defined as having non-judgmental attitude and understanding patients’ viewpoints and emotions. It is a dynamic interpersonal process, depending on the relationship. It is also a multidimensional construct containing cognitive and affective components (38, 39). When arguing about training empathic abilities, it is essential to make a vivid discrimination between potential and actual skills. Empathy must be cultivated in a proper environment with required elements and support (31, 40). Studies suggest that the empathy increases with the years of experience. That is the more you have the firsthand experience with patients, the more you have the opportunity to develop empathy (41).
VR is a proper method for empathy training (42). VR technology can help student feel patient mental situation as if it’s their own and provide a judgmental free environment to learn through exploring one experience as many times as it is needed to be learned. As it is retrieved from constructivist theory, VR has elements that the person can reshape his inner world according the new and unique experience he passed in VR. Experiences of embodiment in an immersive VR environment (EVR) allow users to literally step into the shoes of others and see the world from their perspective. Research on EVR has explored how manipulations of the senses can be used to modulate empathic responses. Experiences of stepping into the shoes of outgroup members have shown significant plasticity of empathic abilities (43).
For training empathy there are some abilities that need to be developed such as (perspective taking between group empathy, compassion, self-regulation) and some that need to be evaded such as subjective distress (31). While the aforementioned skills can improve empathy toward patients, personal distress might even cause stigma through increasing avoidant responses. Developing a sense of familiarity with others experiences can increase the feeling of affiliation to that group which make it easier to empathize with that group (31).
Empathic responses are crucial for a productive doctor-patient relationship. However, unhealthy empathic reactions might induce personal distress that cause burnout and stigmatizing attitudes that cause avoidant responses (39, 44, 45). Reasonable amount of distress, however, is needed for feeling empathy toward others (31, 46). Therefore, it is crucial to assess whether experiencing a simulation of psychosis has any side effects such as personal distress or other psychiatric conditions. In this study none of the participants in the VRSP was withdrawn from the study due to personal distress and no personal distress was reported by observers.
Consistent with previous studies, the participants only reported mild general side effects (Cybersickness) which ameliorated quickly after several minutes (16, 47). None of the participants reported any psychosis-like symptoms, neither right after the experience, nor after 1 week and 1 month of follow-up. This is one of the first studies addressing psychiatric side effects and despite the rigorous inclusion criteria, the results are promising.
There are some limitations in this study that should be addressed in future studies. First of all, the VRSP in this study was only a passive experience and the participants couldn’t actively explore all the components of the environment. It was done because we wanted to compare the experience with the passive observation during the clerkship and the future studies can make the comparison with more interaction between the participants and the virtual environment. With regard to the definition of stigma, in this study only attitudes and knowledge of students were measured. The behavioral component of stigma such as intended social distance or micro-aggressions needs to be addressed in future studies. Also, these results were only obtained in a population with no previous knowledge or contact with patients with severe mental health problems. The replicability in other populations is under question and whether such relationship would show different result must be explored.
In conclusion, applying simulation of psychosis can be an effective tool in reducing stigma, increase knowledge, and empathy in medical students and it seems to be a good choice to be incorporated in routine educational practice.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Research Ethics boards of Birjand University of Medical Sciences (IR.BUMS.REC.1397.174). The patients/participants provided their written informed consent to participate in this study.
SM has provided the main idea of the study. MZ-B and SM have contributed significantly in designing and conducting the project as well as writing and reviewing the manuscript. AE, MR, RM, RA, MM, and FM has contributed in conducting the study, gathering the data, and drafting the manuscript. AM, MK, and AE has contributed in conducting the study and reviewing the manuscript critically. MN and AS has contributed significantly in statistical analyzing and drafting. All authors contributed to the article and approved the submitted version.
This project was funded by the National Agency for Strategic Research in Medical Education, Tehran, Iran, Grant No. 970457.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the Research and Technology Deputy and the Psychosis Research Center of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. We are also grateful to the Education Deputy and the Center for E-learning and Developing Virtual Education and all the students of the Birjand University of Medical Sciences, Birjand, Iran who took part and helped in producing the VRSP.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.880331/full#supplementary-material
1. Oliveira AM, Machado D, Fonseca JB, Palha F, Silva Moreira P, Sousa N, et al. Stigmatizing attitudes toward patients with psychiatric disorders among medical students and professionals. Front Psychiatry. (2020) 11:326. doi: 10.3389/fpsyt.2020.00326
2. Lien Y-Y, Lin H-S, Lien Y-J, Tsai C-H, Wu T-T, Li H, et al. Challenging mental illness stigma in healthcare professionals and students: a systematic review and network meta-analysis. Psychol Health. (2020) 36:669–84. doi: 10.1080/08870446.2020
3. Corrigan PW, Nieweglowski K. How does familiarity impact the stigma of mental illness? Clin Psychol Rev. (2019) 70:40–50.
4. Wrigley S, Jackson H, Judd F, Komiti A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust N Z J Psychiatry. (2005) 39:514–21.
5. Saeed F, Mihan R, Mousavi SZ, Reniers RL, Bateni FS, Alikhani R, et al. A narrative review of stigma related to infectious disease outbreaks: what can be learned in the face of the Covid-19 pandemic? Front Psychiatry. (2020) 11:565919. doi: 10.3389/fpsyt.2020.565919
6. Mousavi SB. Coronavirus disease 2019 pandemic: do not forget patients with severe mental illness. Int J Soc Psychiatry. (2020) 67:830–2. doi: 10.1177/0020764020939982
7. Sartorius N. Iatrogenic stigma of mental illness. Begins with behaviour and attitudes of medical professionals, especially psychiatrists. BMJ (2002) 324:1470–1. doi: 10.1136/bmj.324.7352.1470
8. Mousavi SB, Lecic-Tosevski D, Khalili H, Mousavi SZ. To be able, or disable, that is the question: a critical discussion on how language affects the stigma and self-determination in people with parability. Int J Soc Psychiatry. (2020) 66:424–30.
9. Silva RDC, Albuquerque SGC, Muniz AV, Filho PPR, Ribeiro S, Pinheiro PR, et al. Reducing the schizophrenia stigma: a new approach based on augmented reality. Comput Intell Neurosci. (2017) 2017:2721846. doi: 10.1155/2017/2721846
10. Lyons Z, Janca A. Impact of a psychiatry clerkship on stigma, attitudes towards psychiatry, and psychiatry as a career choice. BMC Med Educ. (2015) 15:34. doi: 10.1186/s12909-015-0307-4
11. Wang P-W, Ko C-H, Chen C-S, Yang Y-HC, Lin H-C, Cheng C-C, et al. Changes of explicit and implicit stigma in medical students during psychiatric clerkship. Acad Psychiatry. (2016) 40:224–8.
12. Kalyanaraman SS, Penn DL, Ivory JD, Judge A. The virtual doppelganger: effects of a virtual reality simulator on perceptions of schizophrenia. J Nerv Ment Dis. (2010) 198:437–43.
13. Knaak S, Modgill G, Patten SB. Key ingredients of anti-stigma programs for health care providers: a data synthesis of evaluative studies. Can J Psychiatry. (2014) 59(10 Suppl. 1):S19–26.
14. Jensen L, Konradsen F. A review of the use of virtual reality head-mounted displays in education and training. Educ Inf Technol. (2018) 23:1515–29.
15. Radianti J, Majchrzak TA, Fromm J, Wohlgenannt I. A systematic review of immersive virtual reality applications for higher education: design elements, lessons learned, and research agenda. Comput Educ. (2020) 147:103778.
16. Formosa NJ, Morrison BW, Hill G, Stone D. Testing the efficacy of a virtual reality-based simulation in enhancing users’ knowledge, attitudes, and empathy relating to psychosis. Aust J Psychol. (2018) 70:57–65. doi: 10.1111/ajpy.12167
17. Tichon J, Banks J. The application of virtual reality to the understanding and treatment of schizophrenia. In: V Palade, RJ Howlett, L Jain editors. Knowledge-Based Intelligent Information and Engineering Systems. Berlin: Springer (2003). p. 1064–8.
18. Chavez B, Bayona S. Virtual reality in the learning process. In: Á Rocha, H Adeli, L Reis, S Costanzo editors. Trends and Advances in Information Systems and Technologies. WorldCIST’18 2018. Advances in Intelligent Systems and Computing. Cham: Springer (2018). p. 1345–56. doi: 10.1007/978-3-319-77712-2_129
19. Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. (2013) 150:3–10.
22. Horsfall J, Cleary M, Hunt GE. Stigma in mental health: clients and professionals. Issues Ment Health Nurs. (2010) 31:450–5.
23. Brown SA. Implementing a brief hallucination simulation as a mental illness stigma reduction strategy. Community Ment Health J. (2010) 46:500–4. doi: 10.1007/s10597-009-9229-0
24. Yellowlees PM, Cook JN. Education about hallucinations using an internet virtual reality system: a qualitative survey. Acad Psychiatry. (2006) 30:534–9.
25. Glasner-Edwards S, Mooney LJ. Methamphetamine psychosis: epidemiology and management. CNS Drugs. (2014) 28:1115–26.
26. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5§). Washington, D.C: American Psychiatric Publishing (2013).
27. Nojomi M, Malakouti S, Ghanean H, Joghataei M, Jacobson L. Mental illness stigma in city of Tehran, 2009. Razi J Med Sci. (2010) 17:45–52.
28. Stuart H, Arboleda-Flórez J. Community attitudes toward people with schizophrenia. Can J Psychiatry Rev Can Psychiatr. (2001) 46:245–52. doi: 10.1177/070674370104600304
29. Shariat SV, Habibi M. Empathy in Iranian medical students: measurement model of the Jefferson scale of empathy. Med Teach. (2013) 35:e913–8. doi: 10.3109/0142159X.2012.714881
30. Ward J, Schaal M, Sullivan J, Bowen ME, Erdmann JB, Hojat M. Reliability and validity of the Jefferson scale of empathy in undergraduate nursing students. J Nurs Meas. (2009) 17:73. doi: 10.1891/1061-3749.17.1.73
31. Bertrand P, Guegan J, Robieux L, McCall CA, Zenasni F. Learning empathy through virtual reality: multiple strategies for training empathy-related abilities using body ownership illusions in embodied virtual reality. Front Robot AI. (2018) 5:26. doi: 10.3389/frobt.2018.00026
32. Luttrull MD, Boulter DJ, Kirsch CFE, Aulino JM, Broder JS, Chakraborty S, et al. ACR appropriateness criteria® acute mental status change, delirium, and new onset psychosis. J Am Coll Radiol. (2019) 16:S26–37. doi: 10.1016/j.jacr.2019.02.024
33. Hamilton D, McKechnie J, Edgerton E, Wilson C. Immersive virtual reality as a pedagogical tool in education: a systematic literature review of quantitative learning outcomes and experimental design. J Comput Educ. (2021) 8:1–32. doi: 10.1007/s40692-020-00169-2
35. Sartorius N, Gaebel W, Cleveland H-R, Stuart H, Akiyama T, Arboleda-Flórez J, et al. WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry (2010) 9:131–44.
36. Esagian G, Esagian-Pouftsis S, Kaprinis S. Empathy in psychiatry and psychotherapy. Psychiatriki. (2019) 30:156–64.
37. Fox V. Empathy: the wonder quality of mental health treatment. Psychiatr Rehabil J. (2000) 23:292. doi: 10.1037/h0095154
38. Håkansson Eklund J, Summer Meranius M. Toward a consensus on the nature of empathy: a review of reviews. Patient Educ Couns. (2021) 104:300–7.
39. Cuff BM, Brown SJ, Taylor L, Howat DJ. Empathy: a review of the concept. Emot Rev. (2016) 8:144–53.
41. Khajavi F, Hekmat HA. Comparative study of empathy: the effects of psychiatric training. Arch Gen Psychiatry. (1971) 25:490–3. doi: 10.1001/archpsyc.1971.01750180010002
42. Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc. (2018) 106:498–500. doi: 10.5195/jmla.2018.518
43. Peck TC, Seinfeld S, Aglioti SM, Slater M. Putting yourself in the skin of a black avatar reduces implicit racial bias. Conscious Cogn. (2013) 22:779–87. doi: 10.1016/j.concog.2013.04.016
44. Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. (2009) 84:1182–91. doi: 10.1097/ACM.0b013e3181b17e55
45. de Vignemont F, Singer T. The empathic brain: how, when and why? Trends Cogn Sci. (2006) 10:435–41. doi: 10.1016/j.tics.2006.08.008
46. Decety J. The neurodevelopment of empathy in humans. Dev Neurosci. (2010) 32:257–67. doi: 10.1159/000317771
Keywords: psychosis, stigma, empathy, virtual reality, simulation, medical education, E-learning
Citation: Zare-Bidaki M, Ehteshampour A, Reisaliakbarighomi M, Mazinani R, Khodaie Ardakani MR, Mirabzadeh A, Alikhani R, Noroozi M, Momeni F, Samani AD, Mehrabi Tavana MM, Esmaeili A and Mousavi SB (2022) Evaluating the Effects of Experiencing Virtual Reality Simulation of Psychosis on Mental Illness Stigma, Empathy, and Knowledge in Medical Students. Front. Psychiatry 13:880331. doi: 10.3389/fpsyt.2022.880331
Received: 21 February 2022; Accepted: 23 March 2022;
Published: 17 May 2022.
Edited by:
Renato de Filippis, Magna Græcia University, ItalyReviewed by:
Philip Theodore Yanos, John Jay College of Criminal Justice, United StatesCopyright © 2022 Zare-Bidaki, Ehteshampour, Reisaliakbarighomi, Mazinani, Khodaie Ardakani, Mirabzadeh, Alikhani, Noroozi, Momeni, Samani, Mehrabi Tavana, Esmaeili and Mousavi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: S. Bentolhoda Mousavi, YmUubW91c2F2aUB1c3dyLmFjLmly
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.