
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 29 April 2022
Sec. Child and Adolescent Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.878173
This article is part of the Research Topic Catatonia across the Lifespan View all 8 articles
 James Luccarelli1,2,3*
James Luccarelli1,2,3* Mark Kalinich3
Mark Kalinich3 Carlos Fernandez-Robles1,3
Carlos Fernandez-Robles1,3 Gregory Fricchione1,3
Gregory Fricchione1,3 Scott R. Beach1,3
Scott R. Beach1,3Objective: Catatonia is a neuropsychiatric condition occurring across the age spectrum and associated with great morbidity and mortality. While prospective cohorts have investigated catatonia incidence among psychiatric patients, no studies have comprehensively explored the incidence of catatonia in general hospitals. We examine the incidence of catatonia diagnosis, demographics of catatonia patients, comorbidities, and inpatient procedures utilized among pediatric patients hospitalized with catatonia in the United States.
Methods: The Kids' Inpatient Database, a national all-payors sample of pediatric hospitalizations in general hospitals, was examined for the year 2019. Hospitalizations with a discharge diagnosis of catatonia were included in the analysis. Hospitalizations with catatonia as the primary discharge diagnosis were compared to hospitalizations with catatonia as a secondary discharge diagnosis.
Results: A total of 900 (95% CI: 850–949) pediatric discharges (291 with catatonia as a primary diagnosis, 609 with catatonia as a secondary diagnosis) occurred during the study year. Mean age was 15.6 ± 2.6 years, and 9.9% were under age 13. Comorbidities were common among patients with catatonia, with psychotic disorders (165; 18.3%), major depressive disorder (69; 7.7%), bipolar disorder (39; 4.3%) and substance-related disorders (20; 2.2%) as the most common primary diagnoses. There was significant comorbidity with neurologic illness, developmental disorders, autism spectrum disorder, and inflammatory conditions. In total 390 catatonia discharges (43.3%) included at least one procedure during admission.
Conclusions: catatonia is rarely diagnosed in pediatric patients in general hospitals but is associated with significant and severe psychiatric and medical comorbidities. Further research is needed into the optimal diagnosis, workup, and treatment of catatonia in pediatric patients.
Catatonia is a disorder characterized by a range of motor and behavioral disturbances which can be diagnosed in both pediatric and adult patients (1). Diagnosis is based on clinical exam (2), noting a series of motor, speech, and activity traits that may be observed or elicited (3). Pediatric catatonia and its manifestations are associated with strikingly high morbidity and mortality, with a 6,000% increased mortality relative to age-matched controls over a 4 year follow-up period (4). Benzodiazepines are the gold-standard treatment of catatonia (5), with electroconvulsive therapy for refractory cases and only weak evidence for alternative medications (6, 7). Catatonia has been diagnosed across the age spectrum, with a reported prevalence of catatonia of 5.5% among new intakes at a child and adolescent psychiatry outpatient clinic (8), and a rate of 17.8% among outpatients with disorders linked to catatonia (including autism, psychosis, and intellectual disability) (9).
While catatonia has been studied for over a century, and large-scale studies have investigated clinical factors associated with catatonia diagnosis in adults (10), there is relatively little research in the pediatric population. The largest existing cohort of pediatric catatonia patients is a multi-decade single-center study of 89 children and adolescents diagnosed with catatonia in France (11), and there is a paucity of multi-center studies. As a result, little is known about the demographics of pediatric patients diagnosed with catatonia nor of their treatment or comorbidities. This study explores the demographics of patients hospitalized for catatonia in general hospitals, as well as comorbid conditions and treatments using a national all-payors database of pediatric hospitalizations in the United States.
Analysis used the 2019 version of the Kids' Inpatient Database (KID) from the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The KID samples 80% of non-newborn discharges (and 10% of normal newborn births) from 3,998 general hospitals in 49 states in the United States, regardless of payor. The sample is then weighted to provide national estimates. In total the 2019 KID contains a weighted 5,902,538 hospitalizations, including normal newborn births. As this is a de-identified, publicly-available database this study was determined to be Not Human Subjects Research by the MassGeneral Brigham Institutional Review Board.
Individual hospitalizations in the KID can include up to 40 discharge diagnoses. Catatonia hospitalizations were those whose discharge diagnoses included the International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes F06.1 (catatonic disorder due to a known physiological condition) or F20.2 (catatonic schizophrenia). These limited nosologic categories prevent any fine-grained analysis of catatonic syndrome subtypes so our goal in this paper is to present data on what clinicians diagnosed as catatonia using these 2 ICD-10-CM categories and the associated diagnoses and comorbidities that were noted in this dataset. Hospitalizations were classified as primary catatonia if the primary discharge diagnosis was catatonia, while those with catatonia as a secondary diagnosis were classified as secondary catatonia. Comorbidities were identified from the discharge diagnoses, and classified according to the Pediatric Clinical Classification System (PECCS) (12), which groups the 72,446 ICD-10-CM diagnosis codes into 834 clinically distinctive categories for pediatric medical conditions.
The design of the KID incorporates survey design, with hospitals clustered within strata and then non-newborn discharges sampled 80% without replacement. Because of this survey design, all statistics from the sample have a corresponding variance. This variance is presented for the total number of patients in the sample, with other values presented as weighted point estimates. Baseline demographics of the primary catatonia and secondary catatonia groups were compared using the χ2 test for categorical variables. Age, hospital length of stay, and total cost were compared using the Mann-Whitney U-test. All tests were 2-sided, with P-values < 0.05 considered statistically significant, with no correction for multiple hypothesis testing. All analyses were conducted on data weighted according to the appropriate KID discharge weight to obtain national estimates. Analyses were conducted using SPSS (version 28; IBM Software, Inc, Armonk, NY). Results are reported in accordance with the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement (13).
From the 2019 KID, 900 pediatric hospitalizations (95% CI: 850–949) included a discharge diagnosis of catatonia (Table 1). Of these 291 (95% CI: 276–306; 32.3%), had catatonia as the primary discharge diagnosis, while 609 (95% CI: 573–644; 67.7%) had catatonia as a secondary discharge diagnosis. Males (512) made up 56.9% of the sample. Mean age was 15.6 ± 2.6 years. The age distribution of patients was skewed toward older adolescents, but 25 patients (2.8%) were under 10 years old, and 89 (9.9%) were under age 13 (Figure 1). The racial breakdown of the sample was 308 (34.2%) White patients, 252 (28.0%) Black patients, 169 (18.8%) Hispanic patients, 56 (6.2%) Asian or Pacific Islander patients, and 70 (7.8%) other. Racial information was missing for 46 individuals (5.1%). Most hospitalizations occurred in urban regions, with 628 patients (69.8%) coming from counties with populations of >1 million individuals, and only 67 (7.4%) from counties with populations of <50,000. Medicaid was the primary payor for 466 patients (51.8%), with commercial insurance used for 390 (43.3%). Hospitalizations were non-elective for 786 (87.3%) patients, and 306 (34.0%) involved a transfer from another healthcare facility. At the end of hospitalization 674 (74.9%) were discharged home, while the remainder were transferred to another acute care hospital (54; 6.0%) or another healthcare facility (180; 20.0%). Median hospital length of stay was 9.0 days (IQR 5.0–21.0), with median healthcare charges of $48,457 (IQR $24,401–102,412).
Hospitalizations for primary catatonia involved male patients more often than did hospitalizations with secondary catatonia (66.7 vs. 52.2%; χ2 = 16.76, df = 1, P < 0.0001), and were less likely to involve elective admission (8.2 vs. 14.4%; χ2 = 6.780, df = 1, P = 0.009). Primary catatonia hospitalizations had overall lower hospital charges (median of $43,129 vs. $52,029; Mann-Whitney U, U = 42,901, P = 0.009). Primary and secondary catatonia discharges did not differ on other demographic or hospital factors including age, race, region, income, primary payor, or hospital length of stay (Table 1).
Primary discharge diagnoses for hospitalizations involving catatonia are listed in Table 2. Other than catatonia itself, psychiatric diagnoses include psychotic disorders (165; 19.3%), major depressive disorder (69; 7.7%), bipolar disorder (39; 4.3%) and substance-related disorders (20; 2.2%). Notably, developmental, neurologic, and autoimmune illnesses were also common. In total, encephalitis, autism spectrum disorders, other neurologic disorders (of which 13 of 18 are encephalopathy), and systemic lupus erythematosus were the principal diagnoses for 106 discharges (11.8%).
As hospitalizations could include up to 40 overall diagnoses, individual hospitalizations could include diagnoses in multiple medical and psychiatric categories. Analyzing all diagnoses (up to 40 primary and secondary discharge diagnoses) for all 900 catatonia hospitalizations, the 12 most common diagnoses (excluding catatonia itself), each occurring in >10% of patients, include six psychiatric comorbidities: unspecified anxiety disorder (216; 24.0%), major depressive disorder single episode (137; 15.2%), suicidal ideation (124; 13.8%), unspecified psychosis (123; 13.7%), unspecified insomnia (115; 12.8%), and unspecified attention-deficit hyperactivity disorder (113; 12.6%). The most common individual medical diagnoses were unspecified constipation (125; 13.9%), dehydration (112; 12.4%), and unspecified tachycardia (91; 10.1%). Autism spectrum disorder was diagnosed in 142 (15.8%). A full table of codes diagnosed in ≥11 discharges is given in Supplementary Table 1.
Grouping individual billing codes into relevant pediatric categories using the PECCS demonstrates diverse comorbidities among patients diagnosed with catatonia. Table 3 lists the PECCS categories diagnosed >100 times and includes the top three individual billing codes contributing to the category. Consistent with the individual discharge diagnoses, PECCS categories are dominated by psychiatric comorbidities including psychotic disorders, anxiety disorders, substance use disorders, and mood disorders. Neurologic disorders are also common (251 diagnoses), as are autism spectrum disorders (142 diagnoses) and other developmental disorders (160 diagnoses). A full list of PECCS categories is given in Supplementary Table 2. While the KID cannot distinguish between complications of a diagnosis that occurred in-hospital vs. were present on admission, many of the discharge diagnoses are potential complications of catatonia. These include constipation (125), tachycardia (91), dehydration (112), the use of physical restraints (86), urinary incontinence (52), restlessness and agitation (50), hypokalemia (40), malnutrition (37), acute renal failure (35), and rhabdomyolysis (27).
In total 390 catatonia hospitalizations (43.3%) had at least one procedure performed during admission (Table 4). The most frequent procedure was a lumbar puncture, performed in 189 (21.0%) of hospitalizations. Electroconvulsive therapy was utilized in 48 admissions (5.3%). Supportive care procedures included central line insertion (39; 4.3%), enteral feeding (34; 3.8%), gastrostomy tube placement (22; 2.4%), and mechanical ventilation (19; 2.1%). Immunomodulatory therapy by intravenous globulin infusion (21; 2.3%) and plasmapheresis (19; 2.1%) were also performed.
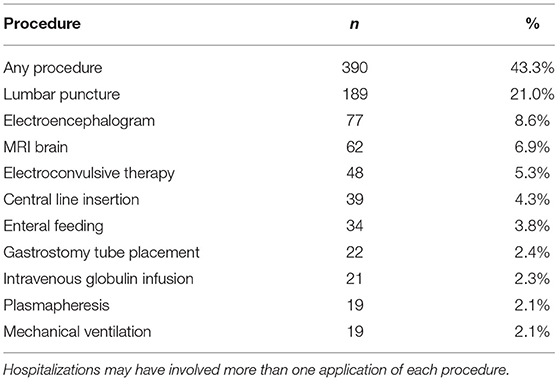
Table 4. Top 10 procedures performed during hospitalization based on number of hospitalizations including the indicated procedure.
In 2019, a total of 900 discharges (95% CI: 850–949) of pediatric patients from general medical hospitals included a diagnosis of catatonia. These results add to understanding of the demographics and comorbidities of catatonia in pediatric patients.
Demographically, the incidence of pediatric catatonia increases with age, perhaps reflecting the increased diagnosis of serious mental illness in older teenagers (14). It is notable, however, that catatonia is diagnosed in younger children as well, and 9.9% of the hospitalizations in this sample are for pre-teens in whom the diagnosis may be less frequently considered. Given the ready treatment of catatonia with medications or electroconvulsive therapy (15), and the fact that longer length of catatonia correlates with greater treatment-resistance (16), a failure to diagnose the condition in younger patients subjects them to significant morbidity. As a result, it is important to consider the diagnosis in patients across the age spectrum. Males were diagnosed with catatonia more frequently than females, but our study did not find the 2:1 ratio of male to female patients demonstrated in one prior sample (17). Notably, females were overrepresented in cases of secondary catatonia, which may relate to higher rates of certain underlying illnesses, including paraneoplastic limbic encephalitidies, lupus, and other autoimmune disorders (18, 19).
Catatonia discharges occurred at similar rates across the year, and included patients of all income strata, although income data is based on ZIP code of residence and not on individual patient data. Racially, patients diagnosed with catatonia do not match the demographics of children and adolescents in the United States as a whole, with non-Hispanic White individuals representing 34.2% of catatonia diagnoses vs. 50% of the children under age 18, and Black individuals representing 28.0% of catatonia patients vs. 14% of the pediatric population (population figures from the 2019 American Community Survey 1-year estimates) (20). This may reflect racial bias, neighborhood factors, cumulative trauma, and perinatal complications that cumulatively have led to Black patients being more readily diagnosed with psychotic disorders compared to mood disorders (21, 22). Differences in diagnosis by race were not significantly different for primary vs. secondary catatonia, however, so other factors may be responsible for the increased diagnosis of catatonia in children from racial minorities. Catatonia hospitalizations were overall costly, with a median hospital charge of $48,457 (IQR $24,401–102,412). This makes catatonia among the most costly pediatric mental health disorders on a per-case basis, with a 2009 analysis of the KID finding the most expensive pediatric mental health condition to be eating disorders, with a mean charge of $46,130 per hospitalization (23). In contrast hospitalizations for depression averaged $13,200 per case and psychosis $19,676, although these charges likely increased in the intervening decade.
Diagnostically, pediatric catatonia patients were more likely to have a primary psychiatric diagnosis of psychotic disorders (18.3%) than major depressive disorder (7.7%) or bipolar disorders (4.3%). Neurologic, developmental, and inflammatory illnesses were also common (11.8%). This diagnostic distribution has similarities with descriptions from prior pediatric catatonia literature. For instance, in a retrospective study of 52 child and adolescent psychiatric inpatients diagnosed with catatonia (mean age 16.8 years), psychotic disorders were diagnosed in 78.8%, affective disorders in 9.6%, and general medical illnesses (including epilepsy and systemic lupus erythematosus) in 15.4% (24). Similarly, a prospective series of 58 child and adolescent psychiatric inpatients diagnosed with catatonia (mean age 15.0) found schizophrenia as the main diagnosis in 55.2%, major depression in 31.0%, and mania in 10.3% of patients (17). Additionally, post-traumatic stress disorder was diagnosed in 58 patients in this sample (6.4%). Acute trauma has been linked to the development of catatonia (25), with one theory positing catatonia as an exaggerated form of fear response (1, 26), but the nature and time course of trauma in these patients is not systematically captured by the KID. This sample likewise demonstrated a high proportion of medical illnesses, with 22.4% diagnosed with conditions including anti-NMDA receptor encephalitis, systemic lupus erythematosus, and epilepsy.
Notably, this distribution of primary psychiatric diagnoses is different from the spectrum of comorbidity seen in adult patients, in which higher proportions of mood disorders (particularly bipolar disorder) than psychotic disorders have been found in catatonic patients. For instance, in a prospective evaluation of 55 adult inpatients with catatonia, Abrams and Taylor found only 7.3% to have schizophrenia while 62% had mania and 9% had depression (27). A further study of 201 adult psychiatric inpatients found a catatonia prevalence of 10.5% in psychosis vs. 12.8% in bipolar disorder and 7.1% in unipolar depression (28).
Analysis of comorbidities reveals a high rate of comorbid medical and psychiatric illnesses among pediatric patients diagnosed with catatonia. In addition to the psychotic and affective disorders discussed above, there were 327 comorbid anxiety disorders and 257 comorbid substance use disorders. Notably, anxiety disorders are not commonly represented among causes of catatonia for adults, though catatonia is believed by some to be an evolutionary fear response to acute stress (16). Substance use disorder diagnoses were mostly related to cannabis, which is the most commonly abused non-alcohol substance in adolescents (29). Interestingly, while cannabis and particularly synthetic cannabinoids are linked to development or worsening of psychosis (30), cannabis use has not been highly associated with catatonia in adults. Developmental disorders were also very common, with 160 diagnoses of developmental disorders and 142 of autism spectrum disorder. The connection between ASD and catatonia is particularly important for clinicians to recognize, as some estimates suggest that 4–17% of patients with ASD will have an episode of catatonia in adolescence or adulthood (31). Furthermore, the diverse nature of medical diagnoses that may be complications of catatonia highlights the substantial clinical impact of catatonia on multiple organ systems.
Diagnostic and therapeutic procedures were commonly performed during hospitalizations for catatonia, with 390 (43.3%) involving at least one procedure performed during the hospitalization. Diagnostically, lumbar punctures were more common than either electroencephalography or brain imaging. As there is no clear role for lumbar puncture in the diagnosis of catatonia itself, these procedures were likely performed to rule out neurologic or medical causes of catatonia such as autoimmune encephalitis (32), although the recommended workup for this condition generally involves lumbar puncture, EEG, and MRI. Beyond diagnostic procedures, a significant fraction of patients required invasive treatments. This includes electroconvulsive therapy, which is an FDA-approved device for the treatment for catatonia in patients aged 13 or older, for 48 patients (5.3%). This is a lower rate of ECT utilization than in adult patients, with a nationwide inpatient survey finding 8.3% of adult patients diagnosed with catatonia received ECT (33). As the efficacy cognitive side effects of ECT are comparable in adolescents and young adults (34), this may represent an underutilization of this treatment. Pediatric access to ECT is curtailed by law in 21 states (35), and nationwide children make up <1% of ECT recipients (36), but this sample demonstrates that it remains a necessary treatment for some catatonic children. Furthermore, many of the patients in the sample required significant supportive treatments that could only be provided in a general medical hospital including enteral feeding, central lines, and mechanical ventilation.
Strengths of this study derive from utilizing nationwide all-payor database that includes 80% of pediatric discharges from general medical hospitals. This detailed capture of discharges allows for the accurate measure of rare comorbidities and provides unbiased estimates of clinical practice throughout the US. This also allows for a very large sample size—indeed the 900 discharges described here are an order of magnitude larger than the previous largest pediatric catatonia cohort (89 patients admitted to a single center over 20 years) (11). As a result, the demographic information reported here likely provides the most comprehensive demographic accounting of the condition yet reported.
Limitations of the study derive from the retrospective observational nature of the sample. Cases are derived from billing data, and so to be counted as a pediatric catatonia case in this study requires that the treating team accurately diagnosed the condition. While there are no studies on the accuracy of pediatric provider identification of catatonia, among adult physicians in the hospital setting, one retrospective chart review by expert clinicians found that only 59% of likely catatonia cases were diagnosed by the treatment team (37), with neurologists rarely identifying catatonia in the emergency department (38). As a result this study may underestimate the true number of catatonia cases as catatonic patients who were not diagnosed with the condition by the treatment team would erroneously be counted as non-cases. Conversely, it is unlikely catatonia will be listed as a discharge diagnosis unless it was clearly diagnosed, so the hospitalizations identified here likely represent true cases. Moreover, the KID only includes general hospitals and does not survey freestanding psychiatric hospitals or long-term rehabilitation hospitals; the incidence of pediatric catatonia in those settings is unclear. Additionally, the 2019 KID utilizes ICD-10-CM diagnostic codes. There are significant differences in the classification of catatonia among diagnostic schema, and for instance ICD-11 introduces substantial revisions to catatonia diagnosis (39). As the KID only contains ICD-10-CM codes, we are unable to assess if diagnoses might be different using alternative classification schemes. Finally, since the KID weights discharges and not individual patients, some individuals who may have been hospitalized more than once for catatonia (or in more than one general hospital for the same episode) may be counted multiple times.
Publicly available datasets were analyzed in this study. This data can be found here: The dataset analyzed for this study can be obtained from the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality at: https://www.hcup-us.ahrq.gov/db/nation/kid/kiddbdocumentation.jsp.
JL, MK, CF-R, GF, and SB contributed to conception and design of the study. JL and MK performed the statistical analysis. JL wrote the first draft of the manuscript. MK, CF-R, GF, and SB wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version. All authors agree to be accountable for the content of the work.
This work was supported by the National Institute of Mental Health (R25MH094612), JL and the Avery D. Weisman Fund of the Massachusetts General Hospital Department of Psychiatry.
MK is currently employed by and has equity in Watershed Informatics, whose work is unrelated to pediatric catatonia.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.878173/full#supplementary-material
1. Shorter E, Fink M. The Madness of Fear: A History of Catatonia. 1st ed. Oxford: Oxford University Press (2018). 224 p.
2. Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. (1996) 93:129–36. doi: 10.1111/j.1600-0447.1996.tb09814.x
3. Luccarelli J, Fricchione G, Newton AW, Wozniak J. The diagnosis and treatment of catatonia via telemedicine: a case report and proposed diagnostic criteria. Schizophr Res. (2022) 241:66–7. doi: 10.1016/j.schres.2022.01.038
4. Cornic F, Consoli A, Tanguy M-L, Bonnot O, Périsse D, Tordjman S, et al. Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res. (2009) 113:233–40. doi: 10.1016/j.schres.2009.04.021
5. Fricchione GL, Cassem NH, Hooberman D, Hobson D. Intravenous lorazepam in neuroleptic-indueed catatonia. J Clin Psychopharmacol. (1983) 3:338–42. doi: 10.1097/00004714-198312000-00002
6. Beach SR, Gomez-Bernal F, Huffman JC, Fricchione GL. Alternative treatment strategies for catatonia: a systematic review. Gen Hosp Psychiatry. (2017) 48:1–19. doi: 10.1016/j.genhosppsych.2017.06.011
7. Sorg EM, Chaney-Catchpole M, Hazen EP. Pediatric catatonia: a case series-based review of presentation, evaluation, and management. Psychosomatics. (2018) 59:531–8. doi: 10.1016/j.psym.2018.05.012
8. Thakur A, Jagadheesan K, Dutta S, Sinha VK. Incidence of catatonia in children and adolescents in a paediatric psychiatric clinic. Aust N Z J Psychiatry. (2003) 37:200–3. doi: 10.1046/j.1440-1614.2003.01125.x
9. Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. (2012) 125:33–8. doi: 10.1111/j.1600-0447.2011.01778.x
10. Solmi M, Pigato GG, Roiter B, Guaglianone A, Martini L, Fornaro M, et al. Prevalence of catatonia and its moderators in clinical samples: results from a meta-analysis and meta-regression analysis. Schizophr Bull. (2018) 44:1133–50. doi: 10.1093/schbul/sbx157
11. Raffin M, Consoli A, Giannitelli M, Philippe A, Keren B, Bodeau N, et al. Catatonia in children and adolescents: a high rate of genetic conditions. J Am Acad Child Adolesc Psychiatry. (2018) 57:518. doi: 10.1016/j.jaac.2018.03.020
12. Gill PJ, Anwar MR, Thavam T, Hall M, Rodean J, Mahant S. Pediatric clinical classification system for use in inpatient settings. JAMA Pediatr. (2021) 175:525–7. doi: 10.1001/jamapediatrics.2020.6007
13. Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. (2015) 12:e1001885. doi: 10.1371/journal.pmed.1001885
14. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2022) 27:281–295. doi: 10.1038/s41380-021-01161-7
15. Raffin M, Zugaj-Bensaou L, Bodeau N, Milhiet V, Laurent C, Cohen D, et al. Treatment use in a prospective naturalistic cohort of children and adolescents with catatonia. Eur Child Adolesc Psychiatry. (2015) 24:441–9. doi: 10.1007/s00787-014-0595-y
16. Fink M, Taylor MA. Catatonia: A Clinician's Guide to Diagnosis and Treatment. Cambridge: Cambridge University Press (2006). 276 p.
17. Consoli A, Raffin M, Laurent C, Bodeau N, Campion D, Amoura Z, et al. Medical and developmental risk factors of catatonia in children and adolescents: a prospective case–control study. Schizophr Res. (2012) 137:151–8. doi: 10.1016/j.schres.2012.02.012
18. Altintas A, Dargvainiene J, Schneider-Gold C, Asgari N, Ayzenberg I, Ciplea AI, et al. Gender issues of antibody-mediated diseases in neurology: (NMOSD/autoimmune encephalitis/MG). Ther Adv Neurol Disord. (2020) 13:1756286420949808. doi: 10.1177/1756286420949808
19. Angum F, Khan T, Kaler J, Siddiqui L, Hussain A. The prevalence of autoimmune disorders in women: a narrative review. Cureus. (2020) 12:e8094. doi: 10.7759/cureus.8094
20. US, Census Bureau. American Community Survey 1-Year Estimates. Available online at: https://data.census.gov/ (accessed January 10, 2022).
21. Minsky S, Vega W, Miskimen T, Gara M, Escobar J. Diagnostic patterns in Latino, African American, and European American psychiatric patients. Arch Gen Psychiatry. (2003) 60:637–44. doi: 10.1001/archpsyc.60.6.637
22. Anglin DM, Ereshefsky S, Klaunig MJ, Bridgwater MA, Niendam TA, Ellman LM, et al. From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am J Psychiatry. (2021) 178:599–610. doi: 10.1176/appi.ajp.2020.20071091
23. Bardach NS, Coker TR, Zima BT, Murphy JM, Knapp P, Richardson LP, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. (2014) 133:602–9. doi: 10.1542/peds.2013-3165
24. Grover S, Chauhan N, Sharma A, Chakrabarti S, Avasthi A. Symptom profile of catatonia in children and adolescents admitted to psychiatry inpatient unit. Asian J Psychiatry. (2017) 29:91–5. doi: 10.1016/j.ajp.2017.04.016
25. Ahmed GK, Elbeh K, Karim AA, Khedr EM. Case report: catatonia associated with post-traumatic stress disorder. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.740436
26. Fink M, Shorter E. Does persisting fear sustain catatonia? Acta Psychiatr Scand. (2017) 136:441–4. doi: 10.1111/acps.12796
27. Abrams R, Taylor MA. Catatonia. A prospective clinical study. Arch Gen Psychiatry. (1976) 33:579–81. doi: 10.1001/archpsyc.1976.01770050043006
28. Grover S, Chakrabarti S, Ghormode D, Agarwal M, Sharma A, Avasthi A. Catatonia in inpatients with psychiatric disorders: a comparison of schizophrenia and mood disorders. Psychiatry Res. (2015) 229:919–25. doi: 10.1016/j.psychres.2015.07.020
29. Kulak JA, Griswold KS. Adolescent substance use and misuse: recognition and management. Am Fam Physician. (2019) 99:689–96.
30. Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. (2016) 73:292–7. doi: 10.1001/jamapsychiatry.2015.3278
31. Dhossche DM. Decalogue of catatonia in autism spectrum disorders. Front Psychiatry. (2014) 5:157. doi: 10.3389/fpsyt.2014.00157
32. Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. (2016) 15:391–404. doi: 10.1016/S1474-4422(15)00401-9
33. Trivedi C, Manikkara G, Zhang M, Mansuri Z, Jain S. ECT utilization in the treatment of catatonic patients in the United States: a Nationwide in-patient sample analysis. J ECT. (2021) 37:107–11. doi: 10.1097/YCT.0000000000000753
34. Luccarelli J, McCoy TH, Uchida M, Green A, Seiner SJ, Henry ME. The efficacy and cognitive effects of acute course electroconvulsive therapy are equal in adolescents, transitional age youth, and young adults. J Child Adolesc Psychopharmacol. (2021) 31:538–44. doi: 10.1089/cap.2021.0064
35. Livingston R, Wu C, Mu K, Coffey MJ. Regulation of electroconvulsive therapy: a systematic review of US State Laws. J ECT. (2018) 34:60. doi: 10.1097/YCT.0000000000000460
36. Luccarelli J, Henry ME, McCoy TH. Demographics of patients receiving electroconvulsive therapy based on state-mandated reporting data. J ECT. (2020) 36:229–33. doi: 10.1097/YCT.0000000000000692
37. Llesuy JR, Medina M, Jacobson KC, Cooper JJ. Catatonia under-diagnosis in the general hospital. J Neuropsychiatry Clin Neurosci. (2018) 30:145–51. doi: 10.1176/appi.neuropsych.17060123
38. Anand S, Paliwal VK, Singh LS, Uniyal R. Why do neurologists miss catatonia in neurology emergency? A case series and brief literature review. Clin Neurol Neurosurg. (2019) 184:105375. doi: 10.1016/j.clineuro.2019.105375
Keywords: catatonia, adolescent psychiatry, cohort studies, mood disorders, psychotic disorder, demography
Citation: Luccarelli J, Kalinich M, Fernandez-Robles C, Fricchione G and Beach SR (2022) The Incidence of Catatonia Diagnosis Among Pediatric Patients Discharged From General Hospitals in the United States: A Kids' Inpatient Database Study. Front. Psychiatry 13:878173. doi: 10.3389/fpsyt.2022.878173
Received: 17 February 2022; Accepted: 04 April 2022;
Published: 29 April 2022.
Edited by:
Walter Jaimes-Albornoz, Donostia University Hospital, SpainReviewed by:
Asma Bouden, Tunis El Manar University, TunisiaCopyright © 2022 Luccarelli, Kalinich, Fernandez-Robles, Fricchione and Beach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: James Luccarelli, amx1Y2NhcmVsbGlAcGFydG5lcnMub3Jn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.