- 1Department of Psychiatry, Faculty of Medicine, Cipto Mangunkusumo National Referral Hospital, Universitas Indonesia, Jakarta, Indonesia
- 2Neuroscience and Brain Development Research Cluster, Faculty of Medicine, Indonesia Medical Education and Research Institute, Universitas Indonesia, Jakarta, Indonesia
Introduction: This study aims to identify the psychosocial determinants and examine the mediation mechanisms of the compliance with COVID-19 health protocols among people undergoing isolation in health facilities that specifically treat COVID-19 cases in Jakarta, Indonesia.
Methods: This is a cross-sectional study which used socio-cognitive approach, known as the Health Action Process Approach (HAPA), to understand the complexity of issues related to compliance with health protocols. A total of 1,584 subjects participated in this study, including 865 men and 719 women over the age of 18 years old during the data collection period (October 19–26, 2020). The data were collected using questionnaire that was developed by a team of experts from the Faculty of Medicine, Universitas Indonesia—Dr. Cipto Mangunkusumo General Hospital, and survivors. The data that has been collected were then analyzed using Structural Equation Modeling, a multivariate data analysis technique.
Results: The final research model in this study fulfills the criteria for a good model fit. This study found that individuals who have strong self-efficacy regarding their ability to implement behaviors and overcome obstacles will have stronger intent to comply in the future. The study also found that stronger intent will lead to stronger planning, and planning was found mediating intention and compliance with health protocols.
Conclusion: This research model is comprehensive and useful in understanding compliance with health protocols among people undergoing isolation in health facilities for COVID-19 (Wisma Atlet and RSCM Kiara Ultimate). Having intent (related to the risk perception, outcome expectancies, and self-efficacy) and having a plan can positively influence the behavior of people undergoing isolation, resulting in better compliance to health protocols. The understanding gained from this study can be used to improve strategies related to compliance with health protocols against COVID-19 in the communities.
Introduction
The COVID-19 pandemic that has occurred over the last 2 years around the world presented great challenges not only to health workers, but also to the economy, government, education, and many other sectors in society (1, 2). Based on the latest data from WHO as of the time of writing (April 13, 2022), there have been 499,119,316 confirmed cases of COVID-19, with a total of 6,185,242 deaths. Indonesia has recorded 6,036,909 confirmed cases of COVID-19 and 155,746 deaths (3). The high transmission rate of COVID-19 continues to be a concern, especially the Delta and Omicron variant which was found to have a much higher transmission rate than the first strain encountered at the beginning of the pandemic. Due to its high transmission rate, various interventions to prevent the transmission of COVID-19 are also continuously being developed. These include physical distancing, self-isolation, quarantine, and health protocols. Vaccination program has also been implemented and is one of the main strategies currently used to control the COVID-19 pandemic. Although the vaccination program will run continuously until the transmission rate in the community decreases, prevention strategies in the form of health protocols, such as regularly washing hands, wearing masks, maintaining distance, avoiding crowds, as well as limiting mobility and interaction, still need to be carried out regularly. The CDC also recommends that vaccinated people should continue to comply with health protocols to prevent transmission (4, 5). Dewi and Probandari (6) also found a significant association between compliant behavior to health protocols, such as wearing masks and physical distancing outside the home and at the workplace, and the COVID-19 rapid test results.
Due to the importance of health behavior in the prevention of disease, various forms of health promotion continue to be conducted to achieve behavior change in terms of compliance with health protocols at the community level. However, community compliance level to the health protocols remains low in Indonesia. Based on a survey on community compliance with health protocols conducted by AC Nielsen with UNICEF, in six major cities in Indonesia, there were only 31.5% of respondents who performed all health protocol behaviors (including wearing masks, maintaining distance, and washing hands) in a disciplined manner. Others performed two of the three health protocol behaviors (36%), one of the three health protocol behaviors (23.2%), or did not comply with the health protocols at all (9.3%) (7). Fuady et al. (8), who conducted a study in Indonesian youths, also found that despite having good knowledge and attitude, in practice the results were significantly different. Fuady et al. (8) found that in Indonesian youth, the non-compliance rate to the health protocols was high, suggesting that knowledge and attitude alone are not enough to make a person perform health behaviors, particularly related to preventive strategies against COVID-19.
To achieve effective behavioral changes, it is necessary to identify the behavioral determinants that can be potentially modified and used as targets for intervention. Common obstacles that often keeps people from doing behavioral changes, let alone doing it consistently, are whether or not there is an intention to do the behavior and the gap between having intent and doing the behavior. A socio-cognitive approach, known as Health Action Process Approach (HAPA), can be used to understand the mechanism for someone to have intents and understand the gap between intent and behavior. HAPA helps to bridge and look for more specific determinant factors on how intent emerges into sustained behavioral change. HAPA distinguishes the two processes leading to health behavioral change, namely the pre-intentional motivation process and the post-intentional volitional process. In the motivational phase of HAPA, three socio-cognitive components influence the emergence of intent to change behaviors. The three components consist of expectations of the desired outcome, self-efficacy to make behavioral changes, and perception of personal risk. Expectations of the desired outcome may be in the form of social, physical, or emotional outcome expectancies. Self-efficacy is a person's belief in his capacity to perform the desired behavior. Risk perception is the identification and interpretation of a person's health risks, whether as specific diseases or non-specific conditions. In the volitional phase, two main components implicate the change after the intent emerges, which include planning and self-efficacy (both for maintaining behavior and recovery). Planning consists of two things: planning for actions, such as when, where, and how to act, and planning for coping that will be performed if there are obstacles encountered. Self-efficacy in the volitional phase includes a person's belief in one's capacity to maintain new behaviors through various coping mechanisms in dealing with the obstacles, as well as to reconduct the expected behavioral change if one fails. Moreover, there is action control that may also influence the behavioral changes, which is a self-regulatory strategy done when the behavior has already taken place and been continuously evaluated (9–15).
This study used HAPA to understand the complexity of compliance issues to health protocols. Previously, HAPA has also been used in several studies on health behaviors related to COVID-19, such as study conducted by Lao et al. (16) that found both motivation and volitional factors included in HAPA might improve compliance with several health protocols related to COVID-19, i.e., wearing facemask and handwash. Hamilton et al. (17) also used HAPA to assess social distancing behavior during the pandemic, and found that both processes from HAPA can be used to understand the behavior. Beeckman et al. (14) who also used HAPA as the framework for the study found the same results. Another study by Duan et al. (15) also identified some social-cognition determinants by integrating the theory of planned behavior, health knowledge, and HAPA on three health behaviors related to COVID-19. The study found that intents might be predicted by motivational self-efficacy, attitude and subjective norms, while behaviors might be predicted by health knowledge and action control, and also mediated by planning from volitional self-efficacy (15).
Although several studies have been found examining HAPA on health behaviors related to COVID-19, until this writing was made, no studies were found examining HAPA in the specific population, namely people who are undergoing isolation in health facilities, especially in Indonesia. In Indonesia, the government has provided some isolation facilities where people might undergo isolation and were guaranteed that they will receive masks, available handrub, be supervised continuously, and share appropriate rooms with some distance with other people. With the condition that all the supplies needed were available, this study tried to learn about the mechanism related to the compliance behavior in that specific population. Therefore, this study was conducted, aiming to identify the psychosocial determinants and examine the mediation mechanisms of the compliance with COVID-19 health protocols among people undergoing isolation in health facilities that specifically treat COVID-19 cases in Jakarta, Indonesia. The understanding are important to be known and may be used in developing future programs that targeted the compliance with health protocols of COVID-19 more specifically.
In this study, it was hypothesized that in people undergoing isolation in health facilities related to COVID-19 where the facilities needed where provided, there can be found direct association between self-efficacy in taking actions, outcome expectancies, and risk perception with intents. Moreover, this study also hypothesized that having intents has direct association with planning, planning has direct association with compliance to health protocols, and self-efficacy in maintaining behavior has a direct association with compliance and planning. Moreover, this study also hypothesized that planning mediate intention and compliance to health protocol.
Materials and Methods
Study Design
This is a cross-sectional study, that used HAPA to understand the process leading to behavior change, i.e., compliance with health protocols. There were eight hypotheses tested in this study, as listed in Figure 1 below, including H1: Self-efficacy in taking actions has a direct association with intents; H2: outcome expectancies have a direct association with intents; H3: risk perception has a direct association with intents; H4: intents have a direct association with planning; H5: planning has a direct association with compliance; H6: Self-efficacy in maintaining behavior has a direct relationship with planning; H7: Self-efficacy in maintaining behavior has a direct association with compliance. Furthermore, this study also hypothesized that planning will mediate intention and compliance to health protocol, filling the intention-behavior gap in this community (H8).
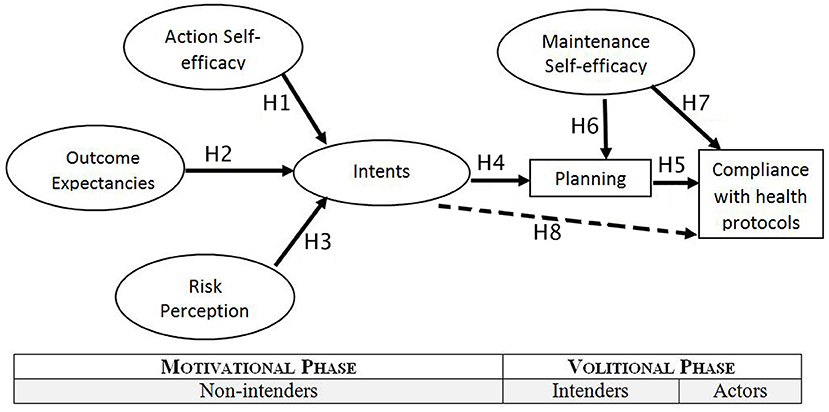
Figure 1. Hypothesis model in this study, adapted from Schwarzer (18), with permission.
Participants
This study included individuals who had been confirmed of having COVID-19, and were undergoing isolation at the health facilities for COVID-19 in Jakarta, Indonesia (Wisma Atlet Kemayoran and Kiara Ultimate RSCM Jakarta) during the data collection period (October 19–26 2020). The inclusion criteria for this study was all people who were undergoing isolation at the health facilities for being confirmed of having COVID-19. The exclusion criteria was the subjects who were in a bad condition that affecting their understanding about the study and having difficulties filling out the distributed questionnaire. The a-priori sample size was determined based on the calculation formula for Structural Equation Modeling (SEM), with anticipated effect size 0.1, desired statistical power level 0.8, number of latent variables 7, number of observed variables 5, and probability level 0.05. Based on the calculation formula (19), the minimum sample size required to detect the effect is 1,808 samples, with a minimum of 805 samples for the model structure. In this study, subjects who met the inclusion and exclusion criteria were included until the time limit was over (the data collection period for this study was limited to 8 days). As many as 1,584 subjects completed the study, including 865 men and 719 women over the age of 18 years old.
Procedures
The medical staffs worked in Wisma Atlet Kemayoran and Kiara Ultimate RSCM Jakarta were included to explain about the study to the respondents during the data collection period. The respondents who were selected based on the inclusion and exclusion criteria listed above were being informed about the aim of the study, steps to fill the questionnaire distributed, and the confidentiality issues. All of the participants who agree to join in this study have given the permission by signing in the online form of the informed consent form. The questionnaire in this study was distributed using an electronic form, following the regulations of the health facility where the study was conducted, to avoid COVID-19 transmission. When completing the questionnaire, respondents were accompanied by the research team.
Research Instrument
To test the hypotheses, a survey questionnaire adapted from the questionnaire made by Schwarzer (11) was used in this study. The questionnaire was developed by a team of experts from the Faculty of Medicine, Universitas Indonesia—Dr. Cipto Mangunkusumo General Hospital, and survivors. The development was conducted by first creating, distributing, and collecting data using a pre-test questionnaire, followed by modifications to develop a formal questionnaire which was then distributed for study data collection. The developed questionnaire contains several questions on how often respondents follow quarantine guidelines and is scored using a 5-point Likert scale. Score is calculated based on the respondents' answers, with a score of 1 given if the respondent answered 'never' up to a score of 5 if the respondent answered 'always' on the statement item for the behavior. The distributed questionnaire consists of three parts, covering the characteristics of the interviewees (gender, age, and level of education), measurements of risk perception, outcome expectancies, self-efficacy, intent, planning, and compliance, as well as scores given by respondents (Appendix A). The questionnaire distributed may need ~15–20 min to be fulfilled.
Statistical Analysis
This study used the SEM multivariate data analysis technique. There are two types of variables in structural equation modeling: latent and measured variables. Latent variables are variables that cannot be observed or measured directly. In this study, the latent variables that were assessed included risk perception, outcome expectancies, self-efficacy, intent, planning, and compliance. Measured variables, also known as indicators, are variables that can be observed or measured directly (20, 21).
The structural equation modeling consists of measurement/outer model and structural/inner model. The measurement model is used to explain the association between measured variables and latent variables, while the structural model describes the association between latent variables. In the structural/inner model, there are exogenous latent variables that can predict other variables and endogenous latent variables that are predicted by other variables and show their effects. An approach that can be used for SEM is Partial Least Squares (PLS) which is a path modeling approach without any assumptions about the data distribution. PLS-SEM has several advantages such as being suitable when the sample size is limited, when the data distribution is skewed/asymmetrical, as well as when the prediction accuracy is desired. The PLS-SEM approach can be performed using the SmartPLS application software (20–23). This study also assessed the relationship between demographic factors of the participants (education and sex variables) as control variables and the compliance behaviors.
Measurement/Outer Model
The analysis of the outer model is important because the validity and reliability of the association in the inner model are also determined by the outer model. The outer model analysis assesses internal consistency reliability, indicator/measured variable reliability, convergent validity, average variance extracted (AVE), and discriminant validity. Internal consistency reliability analysis based on the association between the variables observed in this study was performed using Cronbach's alpha and composite reliability measurements. A value closer to one indicates better reliability. In this study, Cronbach's alpha and composite reliability values of >0.7 are acceptable. Indicators with outer loading values >0.7 were accepted, while those <0.4 were omitted (24, 25).
Loading factor indicator, composite reliability, and AVE were observed to assess convergent validity. An AVE value >0.5 is considered adequate for convergent validity, and can also be used to assess discriminant validity. Assessment of discriminant validity was performed to ensure that the latent constructs used in this study are truly unrelated and do not measure the similar construct as other variables (24–26). In this study, discriminant validity was calculated using the Fornell and Larcker criterion and the Heterotrait-monotrait (HTMT) criterion from Henseler (26, 27). According to the Fornell-Larcker criterion, the latent variables should be better at explaining the variance of their indicator variable than other latent variables and are indicated by a larger square root of the AVE value. According to the HTMT criterion, a value closer to 1 indicates a lack of discriminant validity (25, 26).
Structural/Inner Model
Analysis of the inner model quality includes an assessment of the coefficient of determination (R2), path coefficient, and effect size (f2). R-square (R2) or the coefficient of determination is used to assess the predictive power of the model proposed in the hypothesis and see the combined effect of the exogenous variables on endogenous variables. The R2 values range from 0 to 1, with a value closer to one indicating a better model (24).
Analysis of the path coefficient can describe the association between variables in the hypothesis. The path coefficient values range from −1 to +1, with a coefficient closer to 1 indicating a stronger association, whether the association is positive or negative. The significance can then be obtained through standard error using bootstrapping technique. P-Value of <0.05 indicates a significant prediction between independent and dependent variables. The effect size (Cohen's f2) was determined by assessing the change in the coefficient of determination when a specific variable in the model was omitted, as well as by estimating two PLS path models (the complete model that fits the hypothesis and model with some exogenous variables that have been omitted). The effect size of each association was determined as follows: 0.02 (small effect), 0.15 (medium effect), and 0.35 (large effect) (24).
Goodness of Fit
The Goodness of Fit of the models can be measured by using SmartPLS (23). The measurements include Standardized Root Mean Square Residual (SRMR), Normal Fit Index (NFI), and Root Mean Square Theta (RMS_theta). SRMR shows how big the difference of root mean square between observed and expected correlations is. The recommended SRMR value is <0.10 or 0.08 in the conservative version. In this study, the SRMR value limit used was 0.08. The RMS_theta values (root mean square residual covariance) were also assessed with a value <0.12 indicating a well-fitting model, and a higher value indicating a lack of fit in the model. The expected NFI value is ≤ 1, with a value closer to 1 indicating a very good fit, and a value <0.9 usually representing an acceptable fit (28, 29).
Mediation Analysis
Mediation analysis was made to know the process or “how” the relation between the two variables, to better understand the mechanism the effect happens. In this study, mediation analysis were made with smartPLS with the variables: intention, compliance and planning (23, 30). The total effect, direct and indirect effect will be presented in the table with the coefficient and significance value.
Ethical Approval Statement
This study has obtained ethical clearance from the Faculty of Medicine, Universitas Indonesia on April 27, 2020, with reference number KET-444/UN2.F1/ETIK/PPM.00.02/2020.
Results
Demographic Characteristics of Participants
Table 1 shows the demographic characteristics of the participants in this study. The participants consisted of 55% males and 45% females with the majority (61%) having completed secondary high school. Most of the participants were in the range of 18–35 years old (65.49%). The marital status of the participants were 53% married, 42% unmarried, and 5% divorced. For control variables, there were no significant relationship found to the compliance behaviors (P = 0.365 for education; P = 0.263 for sex variables).
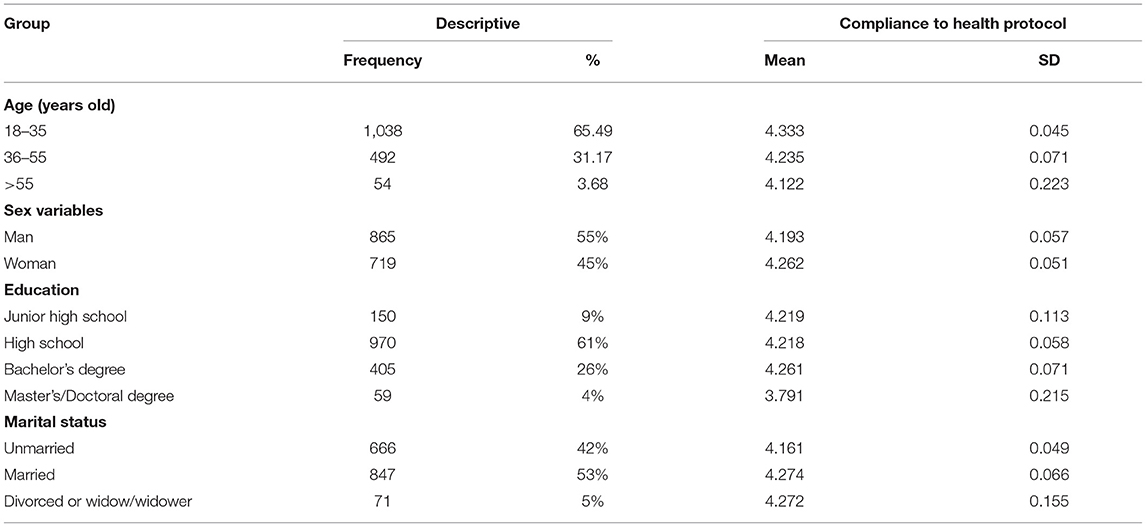
Table 1. Demographic characteristics and difference in perceived compliance to health protocol among subjects (n = 1,584).
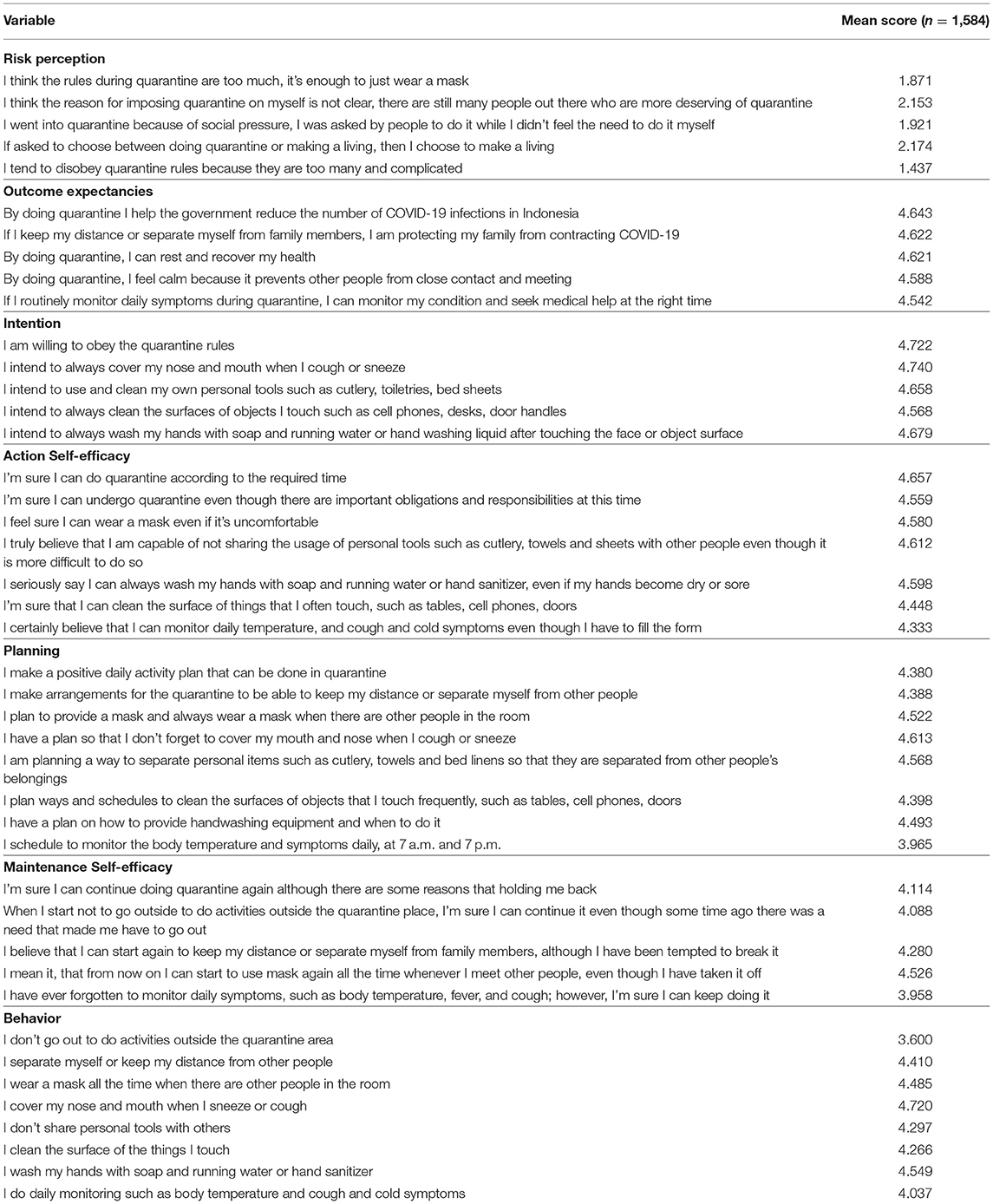
Research Variables
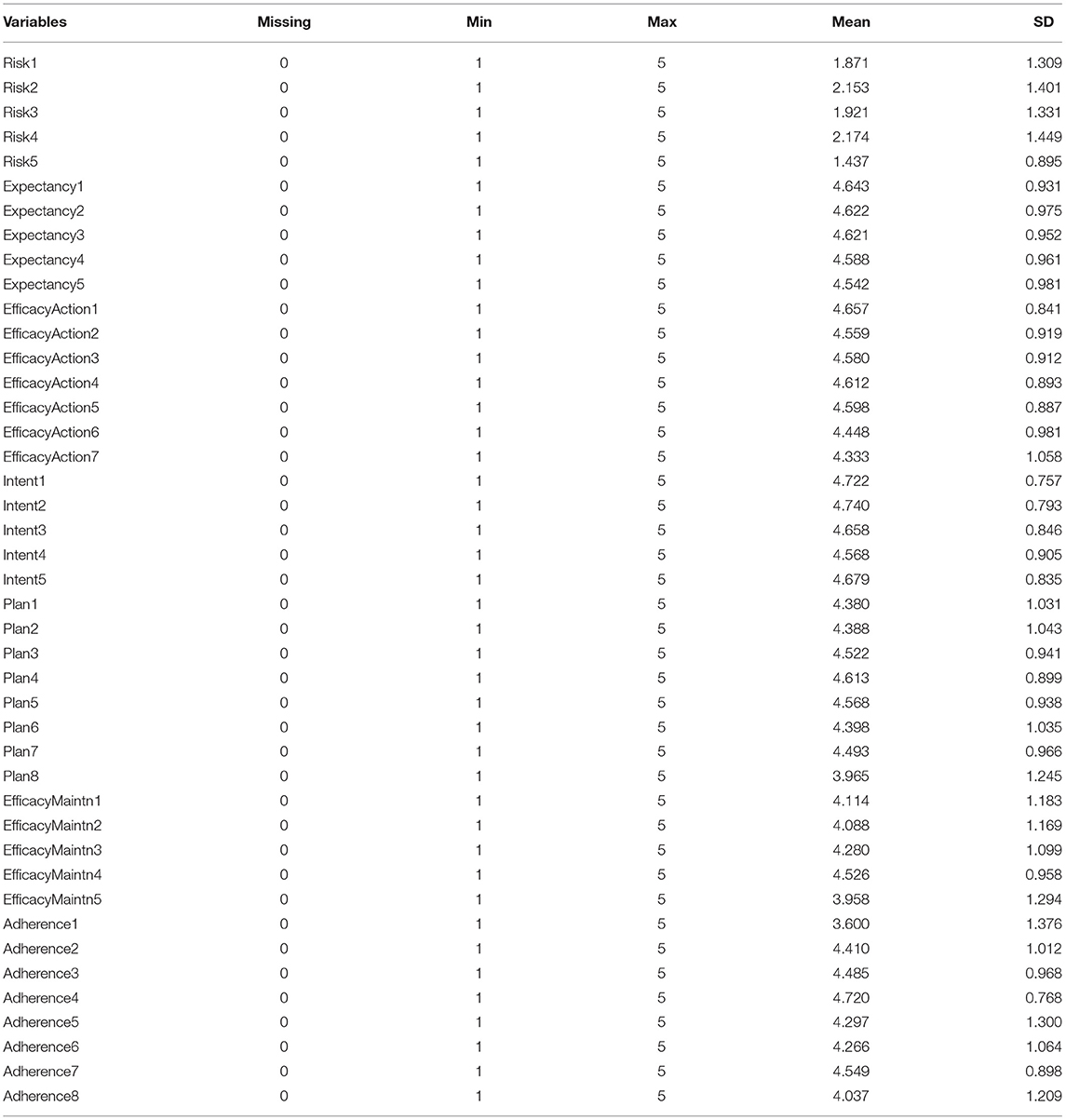
Table 2 describes the variables and the measurement indicators used in this study. There was no missing data during the data collection phase, with each variable having a minimum value of 1 and a maximum value of 5.
Measurement Model
Internal Consistency Reliability
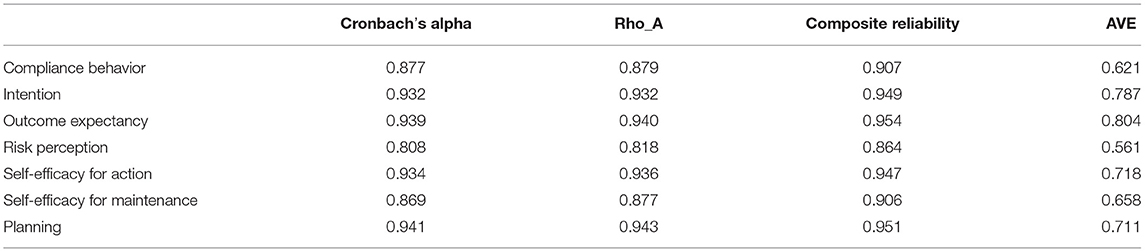
Table 3 below shows the Cronbach's alpha and composite reliability value of the variables. For compliance, intent, outcome expectancies, planning, perception of risk, and self-efficacy in action and maintaining behaviors, all of the Cronbach's alpha and composite reliability values are above the expected value (0.7), indicating good internal consistency.
Reliability Indicator
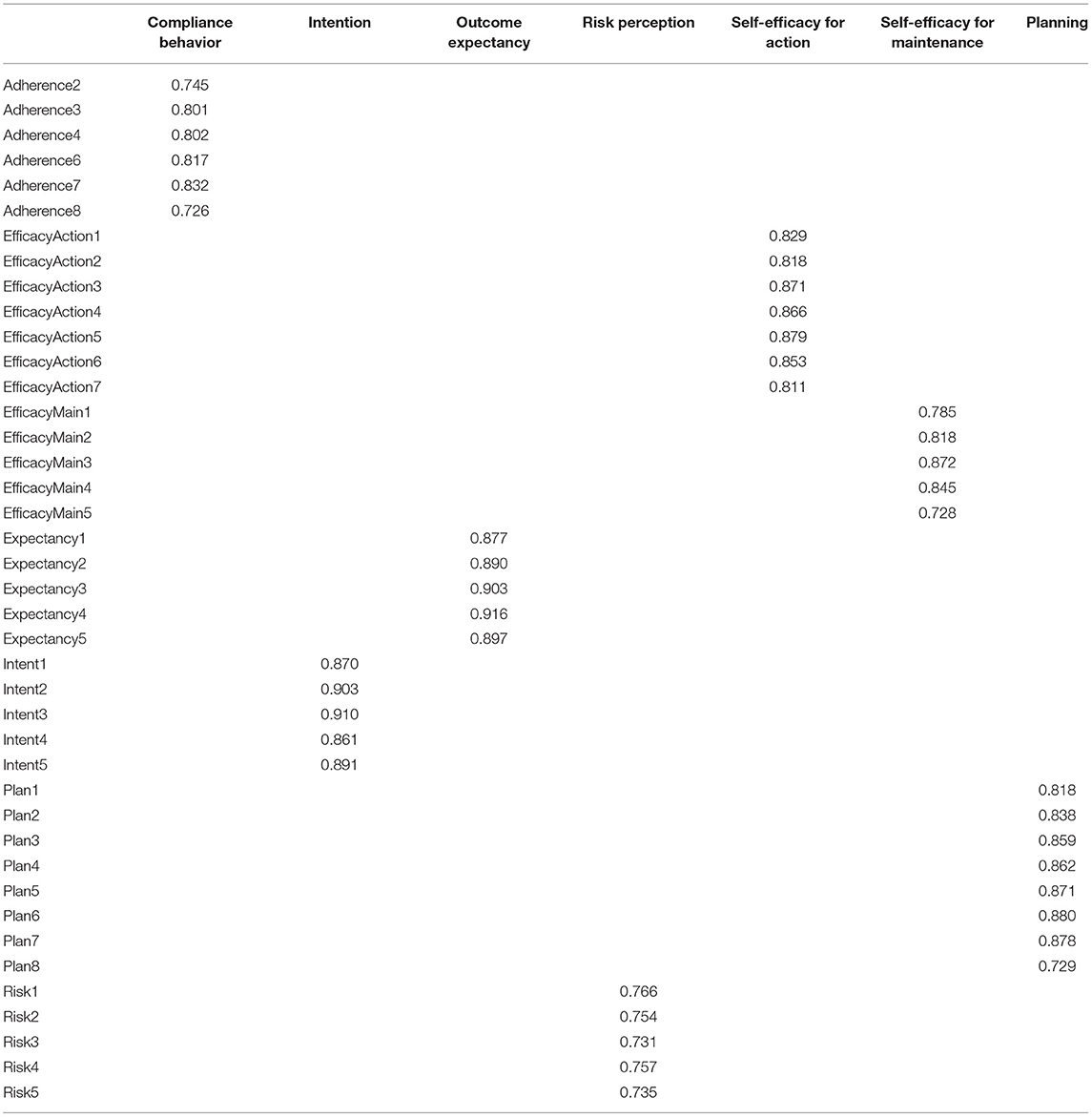
Table 4 shows the results of the indicator reliability of the measurement model as a whole with outer loading values of more than 0.7. Initial analysis found outer loading values that were below 0.7, thus did not fulfill the expected limits, and some variables were removed from the construction model. The variables removed include “adherence1” and “adherence5.”
AVE and Convergent Validity
The AVE value was between 0.621 and 0.804, which is above the expected value (0.5). The composite reliability and AVE values show sufficient convergent validity in the measurement model created.
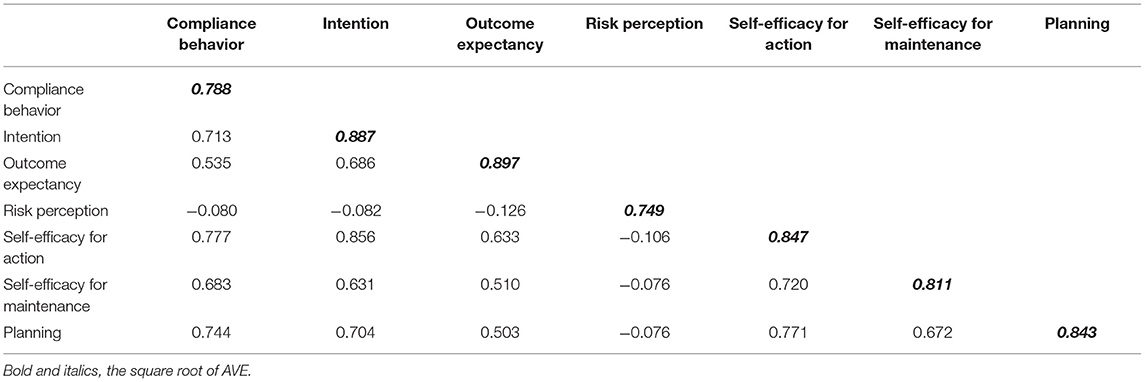
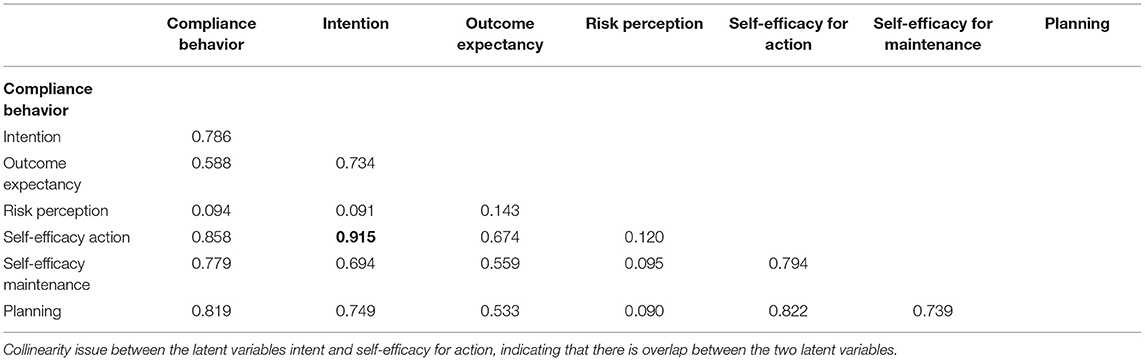
Discriminant Validity
Table 5 below describes the correlation between latent variables by comparing the square root of each AVE with the correlation coefficient of other latent variables. The square root of each variable's AVE in this study was larger than the correlation with other latent variables, thus the discriminant validity is accepted, based on the Fornell Larcker Criterion. The HTMT criterion was also used to calculate discriminant validity. In Table 6 revealed an issue with collinearity between the latent variables intent, and self-efficacy for action, indicating that there is overlap between the two latent variables. There was no overlap between other items.
Structural Model
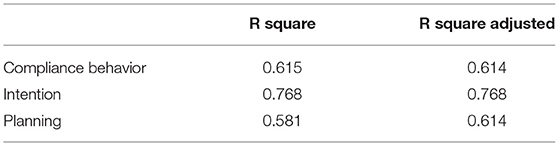
Determination Coefficient
Table 7 shows the determination coefficient or strength of the predictive model created for behavior, intent, outcome expectancies, planning, and risk perception. The model could explain the variations in 61.5% of compliance, 76.8% of intent, and 58.1% of planning.
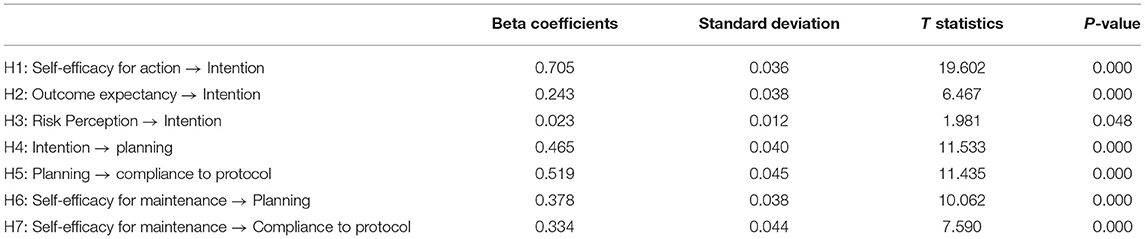
Path Coefficient
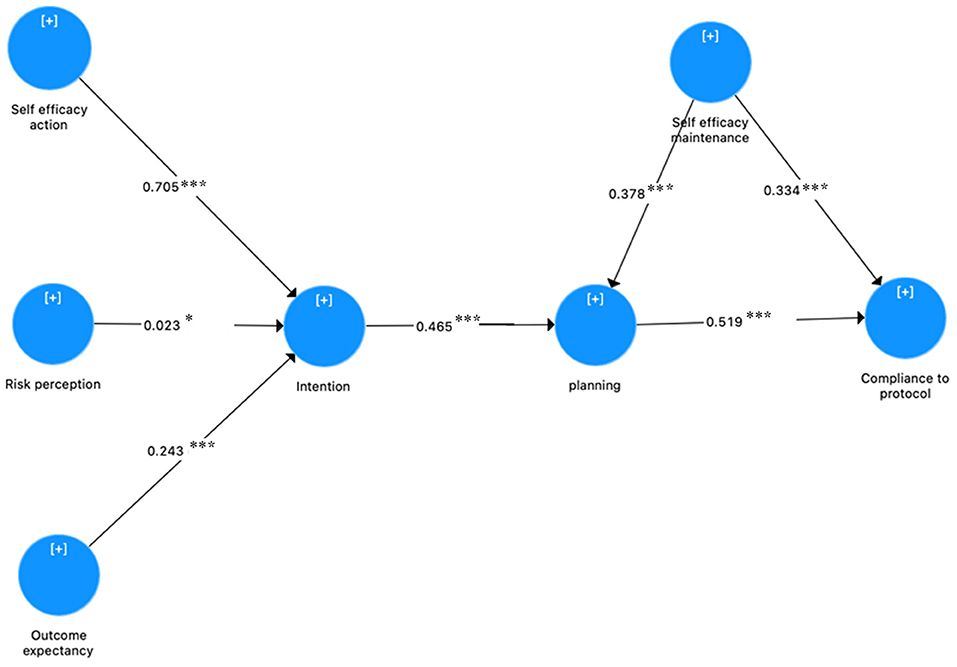
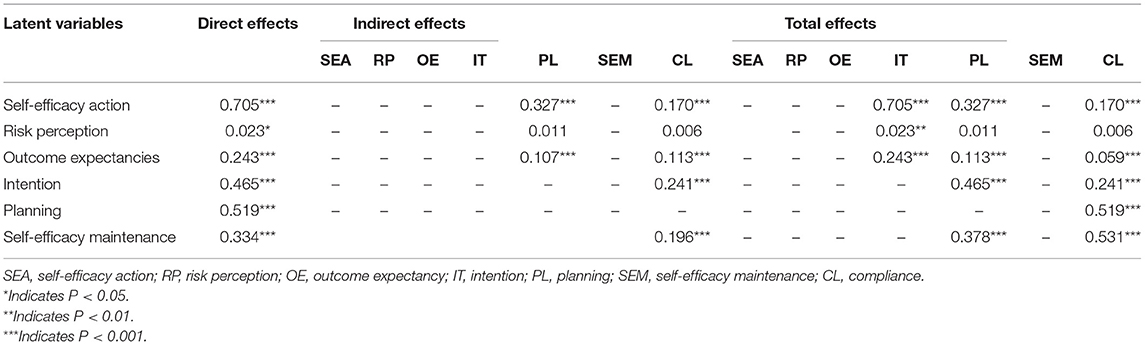
Table 8 shows the path coefficient for all paths proposed in the study model. All seven path coefficients proposed in this study were significant. The results in Table 8 show that and self-efficacy for action, outcome expectancies, and risk perception is related to intent, supporting H1 (β = 0.705; P = 0.000; T-value = 19.602), H2 (β = 0.243; P = 0.000; T-value = 6.467), and H3 (β = 0.023; P = 0.048; T-value = 1.981). Furthermore, intent has a significant effect on planning, and planning has a significant effect on compliance to with health protocols, supporting H4 (β = 0.465; P = 0.000; T-value = 11.533) and H5 (β = 0.519; P = 0.000; T-value = 11.435). Additionally, self-efficacy in maintaining behaviors was also found to have a positive effect on planning and compliance to health protocols which supports H6 (β = 0.378; P = 0.000; T-value = 10.062) and H7 (β = 0.334; P = 0.000; T-value = 7.590). Compared to results by Hamilton et al. (17), this study found the same results in how self-efficacy may predict intention and having intents predicted behavior [in Hamilton et al., (17) the results were β = 0.314, P < 0.001 and β = 0.261, P = 0.026, respectively]. However, Hamilton et al. (17) did not found that risk perception may predict intention significantly (β = 0.150, P = 0.077) (17).
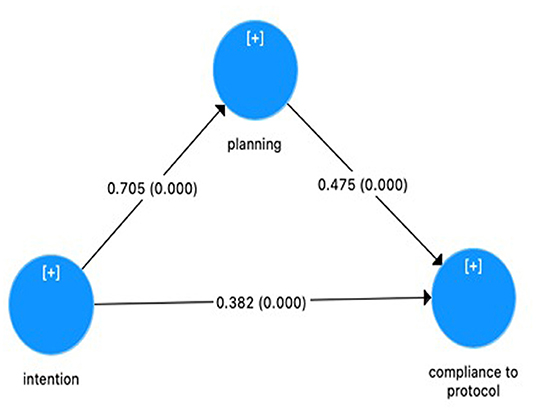
The final path coefficient from compliant behaviors to health protocols is described in Figure 2. The figure was obtained from SmartPLS software (23). Table 9 describes the direct, indirect and total effects of the variables in the HAPA model. The total effect of a latent variable on the HAPA model is the combination of direct and indirect effects. The results showed that self-efficacy action had the greatest direct effect on intention (βtotal = 0.705, P < 0.000) and self-efficacy maintenance had the greatest total effect on compliance (βtotal = 0.531, P < 0.000). Higher level of intention and self-efficacy maintenance gave rise to the higher level of planning, and planning also had a high effect on compliance (βtotal = 0.519, P < 0.000). Self-efficacy action and intention had a moderate total effect on compliance (βtotal = 0.170, P < 0.000 and βtotal = 0.241, P < 0.000). Outcome expectancy had a small total effect on compliance (βtotal = 0.059, P < 0.000).
Effect Size
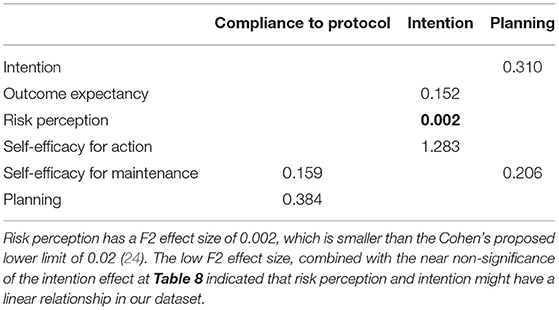
Table 10 shows the effect sizes of H1-H7. A medium effect size was found for H2 (outcome expectancies to intents), H4 (intents to planning), H6 (self-efficacy in maintaining behavior to planning), and H7 (self-efficacy in maintaining behavior to compliance). A large effect size was found for H1 (from self-efficacy for action to intent) and H5 (planning to compliance).
Goodness of Fit
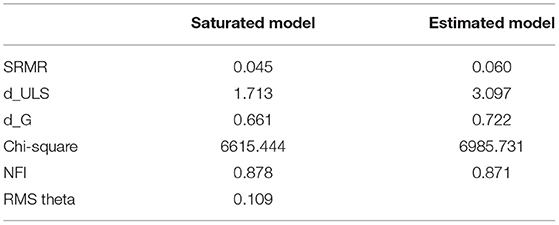
Table 11 shows the results of the model fit measurement, including the saturated model and estimated model. In this study, the SRMR value was 0.045 which is below the expected value of 0.08. Therefore, it can be concluded that the model fulfills the criteria for a good model fit. The RMS_theta value also had a value below 0.109, indicating a well-fitting model. The NFI value was also close to 1, which indicates an accepted fit (28).
Mediation Analysis
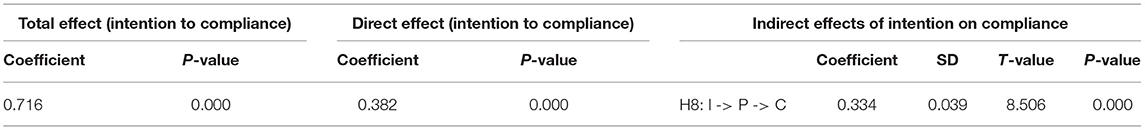
The total effect which is the effect of having intents on compliance without the involvement of planning was significant (β = 0.716; P = 0.000). Moreover, further analysis also found that having intents also have a significant impact on compliance in the presence of planning as the mediator (β = 0.382; P = 0.000) and significant impact of having intents on compliance through planning (β = 0.334; P = 0.000). These results can be seen in Table 12. Figure 3 shows that planning partially mediates an effect from intent to be compliant toward health protocols significantly.
Discussion
This study was conducted to fill the gap by trying to look more specifically about the behavioral change, i.e., compliance to health protocols, in people who are undergoing isolation in the health facilities for COVID-19 in Indonesia. The participants in this study include confirmed COVID-19 cases. Indrayathi et al. (31) found that COVID-19 test histories, either with PCR or rapid antibody test, and also knowing someone who had been confirmed positive or died from COVID-19 were related significantly with adherence to prevention measures. In people undergoing isolation which mean that they have been confirmed of having COVID-19, it may be suspected that they will be more comply to the health protocols. They will see their surroundings who are using full health protocols in the health facilities, in which human behavior will be influenced by the culture, including how they perceive other people will think about them, and also how they see people around them behaving (32). So, this condition in the health facilities may influence them to be more motivated and planning to comply to the behaviors. However, it was still unclear because they may also feel as they have experienced COVID-19, they will be more free and feel careless to comply. On the other hand, the health facilities where the isolation takes place were also providing the facilities needed, such as continuous observation, handrub, and they will be more exposed to information/education related to COVID-19. The behaviors assessed in the study including not going out to do activities outside the quarantine area, and it is a must in healthcare facilities. They will also separate themself or keep some distance from other people as the bed were organized to be in some safe distance. They will also have to wear a mask all the time when there are other people in the room, and the behaviors will be confirmed and reminded when the medical staffs visit them in the daily round. In the health facilities, they will not also share personal tools with others as they may usually do in their daily life outside the isolation place and they will also be assessed daily for the body temperature and symptoms. This study was conducted to look more closely on the behavior changes in these conditions, aiming to provide information about the mediating mechanisms and determinants of compliance with health protocols in people who have been provided by the facilities needed.
This study found that the model proposed is a good fit, and may explain the determinants for behavioral changes among people undergoing isolation in COVID-19 healthcare facilities (Wisma Atlet and RSCM Kiara Ultimate), starting from one's risk perception to COVID-19 transmission, their expectation of the outcome, and their confidence of their own capability to comply, thus allowing them to form intent, plan, and start acting to comply to health protocols and to continuously maintain such compliance. Luszcynska et al. (33) who also used HAPA as the framework to assess compliance to handwashing behavior, found that risk perception and outcome expectancies were linked but only indirectly to the expected behavior. That study found that self-efficacy and self-monitoring or action control are more consistent in predicting expected health behavior (33). Unfortunately, in this study, the action control were not assessed. However, the results for the risk perception and outcome expectancies were also found to be the same in this study, and the self-efficacy's result is also consistent. Based on the results of this study, both forms of self-efficacy (to perform and maintain behaviors) have a permanent effect on health behaviors and play an important role. In those with strong self-efficacy regarding their ability to perform the behavioral change, they also tend to have bigger intent toward compliance. This study also found that stronger intent will trigger stronger planning.
This result is also in-line with the statement from Bandura (34) regarding cognitive social theory in the effort to promote health and prevent diseases. Bandura (34) stated that among all determinants, confidence in self-efficacy plays an important role in personal change because it is needed to overcome obstacles faced in changing behaviors and becomes the foundation for self-motivation and action. This study is also in-line with a study of Isa et al. (35) that found inverse relation between self-efficacy scores to intent-behavior gap. They found in children with intention-behavior gap, they tend to have lower self-efficacy (35). Beeckman et al. (14) also found that self-efficacy were related to adherence to physical distancing as the behavior measured in the study, along with outcome expectancies, having intents and planning. However, in this study, the relation between outcome expectancies to compliance were not found to be large enough. Luc PT (36) which found no direct relation between outcome expectancies to intention in social entrepreneurial, suggested that outcome expectancies are flexible, related to others' support and recognition of the opportunities.
At the intender phase, an individual is already planning to change behaviors. Differ to study by Lao et al. (16) and Hamilton et al. (17) which found that planning did not mediate having intents to behavior change, this study found that planning mediate the two processes and may be used to understand the intention-behavior gap that often found when someone want to do behavior changes. After the behavior has been started, maintaining the behavior is almost as challenging as beginning to do the behavior (37, 38). It is unclear whether the changes in behavior can be maintained in the long term. However, self-efficacy in maintaining behavior are related to the compliance and is related to various factors, including personal factors such as age and level of education, as well as environmental factors such as obstacles and social support. To maintain self-efficacy for the long term, modifiable factors such as continuous social support are needed (39–41).
From the behavioral model proposed in this study, potential improvements can be identified in several points that have high benefits for change, thus the community can become more compliant toward health protocols to prevent COVID-19 transmission. With this knowledge, interventions can be implemented through various strategies targeted at increasing self-efficacy. Individuals who are doubtful toward self-efficacy can be given support and input through consultation. Those with low self-efficacy can be given a structured program to develop a strong sense of confidence in implementing or maintaining behaviors. Additionally, other strategies such as education, reflection on previous experiences, provision of behavior models, or interventions through mental imagery can also be performed. Programs to improve self-management abilities may also be beneficial, such as creating target behaviors that need to be achieved, assessing the situation when the behavior has been performed, and obtaining feedback or appreciation for each behavior that is following the target. The intervention strategies can vary between individuals, depending on each individual's preparedness toward change (10, 34, 42).
Limitations
This study has some limitations. First, this study was limited to subjects undergoing isolation in healthcare facilities. Second, the instrument used in this study was self-reported, and it may affect the results because of the social desirability bias. The participants may also report their condition during their isolation (after being exposed to COVID-19) or report about their behavior usually before being exposed to COVID-19 and underwent the isolation in the facilities where the study was taken place. Third, the cross-sectional data used in this study also reduce the power of the study in forming a conclusion, as it may not give temporal relationship between the factors being hypothesized. With the cross-sectional study design, some recall bias may also be considered as limitation. Fourth, this study also did not portray the subject's past lifestyle or previous exposure to COVID-19 infection and/or other infectious diseases. Therefore, future studies may gather data longitudinally to investigate the effect of change and reciprocals between the construct models, comparing between individuals undergoing isolation in healthcare facilities and at home, and perform experimental studies that target changes in the HAPA construct individually. Future studies may also include more psychosocial determinants, such as psychosocial wellbeing, lifestyle, or social support, that were found related to difficulties in adherence behavior in a study conducted by Beeckman et al. (14). Moreover, although action control, which can be found in the original HAPA model suggested by Schwarzer et al. (12), was something crucial, but it was not included in the hypothesis or the path model in this study. This study also simplified the coping and action planning as “planning,” which includes both action and coping planning (13, 18). More specific HAPA construct which include action control and specify planning into action and coping planning may also be done in the future research.
Conclusion
This study was conducted to fill the gap by trying to look more specifically about the behavioral change in the population who were undergoing isolation in health facilities related to COVID-19, especially in Indonesia. It can be concluded that intent, which related to the perception of risk, expected outcome, and self-efficacy has a positive influence on people undergoing isolation in healthcare facilities regarding their compliance with health protocols. Planning was also found mediates intention and compliance with health protocols. The understanding gained from this study can be used to improve strategies related to compliance with health protocols against COVID-19 in the communities, such as providing education, support, and consultation when needed.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study obtained ethical clearance from the Faculty of Medicine, Universitas Indonesia on 27th April 2020 under ethical clearance number KET-444/UN2.F1/ETIK/PPM.00.02/2020. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KM, NA, AK, and PL conceptualized and designed. KM supervised the study and analyzed the data. KM, RK, LM, and LD collected the data. KM and AL wrote the manuscript and review. All authors have read and approved of the publication manuscript.
Funding
This study was funded by Covid-19 research and innovation consortium from National Research and Innovation Agency Ministry of Research and Technology, Republic of Indonesia, with grant numbers 110/FI/PKS-KCOVID-19.F/VI/2020.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to express their gratitude to directors, staff and study participants at Emergency Hospital for COVID-19 Wisma Atlit Kemayoran and RSCM Kiara Ultimate Jakarta for their support in this study.
References
1. Silva Junior FJGD, Sales JCES, Monteiro CFDS, Costa APC, Campos LRB, Miranda PIG, et al. Impact of COVID-19 pandemic on mental health of young people and adults: a systematic review protocol of observational studies. BMJ Open. (2020) 10:e039426. doi: 10.1136/bmjopen-2020-039426
3. World Health Organization(WHO). WHO Coronavirus (COVID-19) Dashboard. (2022). Available online at: https://covid19.who.int/ (accessed April 14, 2022).
4. Regmi K, Lwin CM. Impact of non-pharmaceutical interventions for reducing transmission of COVID-19: a systematic review and meta-analysis protocol. BMJ Open. (2020) 10:e041383. doi: 10.1136/bmjopen-2020-041383
5. Christie A, Brooks JT, Hicks LA, Sauber-Schatz EK, Yoder JS, Honein MA. Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. Morb Mortal Wkly Rep. (2021) 70:1044–7. doi: 10.15585/mmwr.mm7030e2
6. Dewi YK, Probandari A. Covid-19 risk factors and health protocol compliance among mall employees and officers in Yogyakarta. BKM J Community Med Public Heal. (2021) 37:21–6. doi: 10.22146/bkm.59065
7. Tim Komunikasi Komite Penanganan COVID-19 dan Pemulihan Ekonomi Nasional. Memahami Perilaku dan Informasi Tepat untuk Mencegah Penularan COVID-19. (2020). Available online at: https://covid19.go.id/berita/memahami-perilaku-dan-informasi-tepat-untuk-mencegah-penularan-covid-19 [accessed November 16, 2021].
8. Fuady A, Khoe LC, Azzahra TB, Lestari HM, Sutanto RL, Yo EC, et al. Good knowledge but poor practice toward COVID-19 among Indonesian youth. Asia-Pacific J Public Heal. (2021) 33:605–7. doi: 10.1177/10105395211015048
9. Schwarzer R, Luszczynska A. How to overcome health-compromising behaviors: the health action process approach. Eur Psychol. (2008) 13:141–51. doi: 10.1027/1016-9040.13.2.141
10. Zhang CQ, Zhang R, Schwarzer R, Hagger MS. A meta-analysis of the health action process approach. Heal Psychol. (2019) 38:623–37. doi: 10.1037/hea0000728
11. Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
12. Schwarzer R, Hamilton K. Changing behavior using the health action process approach. In: Hagger MS, Cameron LD, Hamilton K, Hankonen N, Lintunen T, editors, The Handbook of Behavior Change (Cambridge Handbooks in Psychology). Cambridge: Cambridge University Press (2020). p. 89–103. doi: 10.1017/9781108677318.007
13. Schwarzer R. Health Action Process Approach (HAPA) as a Theoretical Framework to Understand Behavior Change. Actual en Psicol. (2016) 30:119–30. Available online at: https://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S2215-35352016000200119 (accessed February 10, 2022).
14. Beeckman M, De Paepe A, Van Alboom M, Maes S, Wauters A, Baert F, et al. Adherence to the physical distancing measures during the COVID-19 pandemic: a HAPA-based perspective. Appl Psychol Heal Well-Being. (2020) 12:1224–43. doi: 10.1111/aphw.12242
15. Duan Y, Shang B, Liang W, Lin Z, Hu C, Baker JS, et al. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the covid-19 pandemic: an integrated social cognition model. BMC Geriatr. (2022) 22:1–16. doi: 10.1186/s12877-022-02785-2
16. Lao CK, Li X, Zhao N, Gou M, Zhou G. Using the health action process approach to predict facemask use and hand washing in the early stages of the COVID-19 pandemic in China. Curr Psychol. (2021) 21:1985. doi: 10.1007/s12144-021-01985-0
17. Hamilton K, Smith SR, Keech JJ, Moyers SA, Hagger MS. Application of the health action process approach to social distancing behavior during COVID-19. Appl Psychol Heal Well-Being. (2020) 12:1244–69. doi: 10.1111/aphw.12231
18. Schwarzer R. The Health Action Process Approach. (2014). Available online at: http://userpage.fu-berlin.de/~health/hapa.htm (accessed February 10, 2022).
19. Free Statistics Calculators. A-priori Sample Size Calculator for Structural Equation Models. Available online at: https://www.danielsoper.com/statcalc/calculator.aspx?id=89 (accessed November 30, 2020).
20. Morrison TG, Morrison MA, McCutcheon JM. Best practice recommendations for using structural equation modelling in psychological research. Psychology. (2017) 8:1326–41. doi: 10.4236/psych.2017.89086
21. Wong KK-K. Partial least squares structural equation modeling (PLS-SEM) techniques using SmartPLS. Mark Bull. (2013) 24:1–32.
22. Wong KK-K. Handling small survey sample sizes and skewed data sets with partial least square path modelling. Vue Mag Mark Res Intell Assoc. (2010) 2010:20–3.
23. Ringle CM, Wende S, Becker J-M. “SmartPLS 3.” Boenningstedt: SmartPLS (2015). Available online at: www.smartpls.com
24. Hair JF, Sarstedt M, Hopkins L, Kuppelwieser VG. Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev. (2014) 26:106–21. doi: 10.1108/EBR-10-2013-0128
25. Ab Hamid MR, Sami W, Mohmad Sidek MH. Discriminant validity assessment: use of Fornell & Larcker criterion versus HTMT criterion. J Phys Conf Ser. (2017) 890:12163. doi: 10.1088/1742-6596/890/1/012163
26. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. (1981) 18:39–50. doi: 10.1177/002224378101800104
27. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. (2015) 43:115–35. doi: 10.1007/s11747-014-0403-8
28. Ringle CM, Wende S, Becker J-M. Model Fit. Boenningstedt: SmartPLS (2015). Available online at: https://www.smartpls.com/documentation/algorithms-and-techniques/model-fit [accessed November 17, 2021].
29. Henseler J, Dijkstra TK, Sarstedt M, Ringle CM, Diamantopoulos A, Straub DW, et al. Common beliefs and reality about PLS: comments on Rönkkö and Evermann (2013). Organ Res Methods. (2014) 17:182–209. doi: 10.1177/1094428114526928
30. Hayes AF. The simple mediation model. In: Little TD, editor. Introduction to Mediation, Moderation, and Conditional Process Analysis: a Regression-Based Approach. New York, NY: The Guilford Press (2022). p. 79–117.
31. Indrayathi PA, Januraga PP, Pradnyani PE, Gesesew HA, Ward PR. Perceived social norms as determinants of adherence to public health measures related to COVID-19 in Bali, Indonesia. Front Public Heal. (2021) 9:646764. doi: 10.3389/fpubh.2021.646764
32. Yanti B, Wahyudi E, Wahiduddin W, Novika RGH, Arina YMD, Martani NS, et al. Community knowledge, attitudes, and behavior towards social distancing policy as prevention transmission of Covid-19 in Indonesia. J Adm Kesehat Indones. (2020) 8:4. doi: 10.20473/jaki.v8i2.2020.4-14
33. Luszczynska A, Szczuka Z, Abraham C, Baban A, Brooks S, Cipolletta S, et al. The interplay between strictness of policies and individuals' self-regulatory efforts: associations with handwashing during the COVID-19 pandemic. Ann Behav Med. (2021) 2021:kaab102. doi: 10.1093/abm/kaab102
34. Bandura A. Health promotion by social cognitive means. Heal Educ Behav. (2004) 31:143–64. doi: 10.1177/1090198104263660
35. Isa T, Ueda Y, Nakamura R, Misu S, Ono R. Relationship between the intention–behavior gap and self-efficacy for physical activity during childhood. J Child Heal Care. (2019) 23:79–86. doi: 10.1177/1367493518777297
36. Luc PT. Outcome expectations and social entrepreneurial intention: integration of planned behavior and social cognitive career theory. J Asian Financ Econ Bus. (2020) 7:399–407. doi: 10.13106/jafeb.2020.vol7.no6.399
37. Lippke S, Plotnikoff RC. Testing two principles of the health action process approach in individuals with type 2 diabetes. Heal Psychol. (2014) 33:77–84. doi: 10.1037/a0030182
38. Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the health action process approach (HAPA). Rehabil Psychol. (2011) 56:161–70. doi: 10.1037/a0024509
39. Yang L, Li K, Liang Y, Zhao Q, Cui D, Zhu X. Mediating role diet self-efficacy plays in the relationship between social support and diet self-management for patients with type 2 diabetes. Arch Public Heal. (2021) 79:14. doi: 10.1186/s13690-021-00533-3
40. Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Heal Psychol. (2006) 25:282–91. doi: 10.1037/0278-6133.25.3.282
41. Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change. A systematic review. Am J Prev Med. (2007) 32:419–34. doi: 10.1016/j.amepre.2007.01.004
42. Conroy D, Hagger MS. Imagery interventions in health behavior: a meta-analysis. Heal Psychol. (2018) 37:668–79. doi: 10.1037/hea0000625
Appendix
Keywords: Health Action Process Approach, COVID-19, compliance with health protocols, isolation in health facility, Indonesia
Citation: Malik K, Amir N, Kusumawardhani AAAA, Lukman PR, Karnovinanda R, Melisa L, Dewi LP and Lasmono A (2022) Health Action Process Approach (HAPA) as a Framework to Understand Compliance Issues With Health Protocols Among People Undergoing Isolation at Emergency Hospital for COVID-19 Wisma Atlet Kemayoran and RSCM Kiara Ultimate Jakarta Indonesia. Front. Psychiatry 13:871448. doi: 10.3389/fpsyt.2022.871448
Received: 08 February 2022; Accepted: 02 May 2022;
Published: 26 May 2022.
Edited by:
Daria Smirnova, Samara State Medical University, RussiaReviewed by:
Kun-Shan Wu, Tamkang University, TaiwanWei Liang, Hong Kong Baptist University, Hong Kong SAR, China
Copyright © 2022 Malik, Amir, Kusumawardhani, Lukman, Karnovinanda, Melisa, Dewi and Lasmono. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khamelia Malik, a2hhbWVsaWFwc2lAZ21haWwuY29t; Agnes Lasmono, YWduZXMubGFzbW9ub0Bob3RtYWlsLmNvbQ==
 Khamelia Malik
Khamelia Malik Nurmiati Amir
Nurmiati Amir A. A. A. A. Kusumawardhani
A. A. A. A. Kusumawardhani Petrin Redayani Lukman
Petrin Redayani Lukman Rhapsody Karnovinanda
Rhapsody Karnovinanda Leslie Melisa
Leslie Melisa Lidya Purnama Dewi
Lidya Purnama Dewi Agnes Lasmono
Agnes Lasmono