
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 04 April 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.867233
This article is part of the Research TopicBurnout in the Health, Social Care and Beyond: Integrating Individuals and SystemsView all 14 articles
 Fayeza Alameri1
Fayeza Alameri1 Noura Aldaheri1
Noura Aldaheri1 Sarah Almesmari1
Sarah Almesmari1 Manea Basaloum1
Manea Basaloum1 Nouf Albdulrahman Albeshr1
Nouf Albdulrahman Albeshr1 Mecit Can Emre Simsekler2
Mecit Can Emre Simsekler2 Nnamdi Valbosco Ugwuoke3
Nnamdi Valbosco Ugwuoke3 Murat Dalkilinc1
Murat Dalkilinc1 Mai Al Qubaisi1
Mai Al Qubaisi1 Luciana Aparecida Campos4,5
Luciana Aparecida Campos4,5 Wael Almahmeed6
Wael Almahmeed6 Eman Alefishat3,7,8
Eman Alefishat3,7,8 Hashel Al Tunaiji1,9*†
Hashel Al Tunaiji1,9*† Ovidiu Constantin Baltatu3,4,5*†
Ovidiu Constantin Baltatu3,4,5*†
Introduction: The objective of this study was to investigate the psychosocial and cardiovascular markers in healthcare professionals during the COVID-19 pandemic.
Methods: This was a STROBE compliant, blended exploratory study. Residents, staff physicians, nurses, and auxiliary healthcare professionals from both inpatient and outpatient medicine services were recruited using a planned random probability sample. The Maslach Burnout Inventory (MBI), Fuster-BEWAT score (FBS), and socio-demographic factors, as well as sleep quality, were studied. The correlations between burnout severity and cardiovascular risk were examined using multivariable linear regression models adjusted for confounding variables, such as sociodemographic and anthropometric characteristics.
Results: The regression analysis with FBS as the outcome showed a negative association between cardiovascular health and emotional exhaustion [Coef.(95%CI): −0.029 (−0.048, −0.01), p = 0.002]. The higher the emotional exhaustion the lower the cardiovascular health. Further, the model showed a positive association between personal accomplishment and cardiovascular health [Coef.(95%CI): 0.045 (0.007, 0.082), p = 0.02]. Emotional exhaustion was significantly positive correlated with REM sleep and light average (Spearman’s rank correlation: 0.37 and 0.35, respectively, with P < 0.05).
Conclusion: The data from this study show that healthcare practitioners who are with burnout and emotional exhaustion have an elevated cardiovascular risk, however, causality cannot be determined. As an adaptive response to stressful situations, REM sleep increases. The findings of this study may be relevant in creating preventive strategies for burnout and cardiovascular risk reduction or prevention.
Clinical Trial Registration: [www.ClinicalTrials.gov], identifier [NCT04422418].
The coronavirus disease 2019 (COVID-19) pandemic has presented healthcare systems with new and unanticipated obstacles. This quickly changing scenario has a significant impact on healthcare professionals (1). During the epidemic, all healthcare modalities encountered similar obstacles, such as limited expert staff availability and the possibility of peri-procedural transmission of SARS-CoV-2 between patients and staff (2). Managing the unforeseeable scenario of the COVID-19 pandemic posed an unprecedented challenge to healthcare leadership, who had to act quickly to restructure and deliver the key resources and information staff required to manage throughout this health crisis (3).
The COVID-19 pandemic resulted in high incidence of anxiety, depression and burnout syndrome, and mental health disorders among nurses and physicians (4–7). The severe COVID-19 outbreak has had a significant impact on the mental health of medical and nursing professionals (8). A recent study in the Middle East Region found that healthcare professionals experienced psychological distress during the outbreak (9). These factors contribute to physician burnout, which is already a significant problem in the healthcare industry (10, 11).
Long-term job stress can cause burnout, persistent weariness, anxiety symptoms, and health problems (12, 13). According to Maslach and Leiter (14), “Burnout is a psychological syndrome emerging as a prolonged response to chronic interpersonal stressors on the job” (14). According to Karasek and Theorell Job Demands Control Support Model (15), there is a relationship between cardiovascular risk factors and burnout, which is mediated by life and job stressors (16). Occupational stress and burnout can cause persistent fatigue symptoms, as well as an increased risk of cardiovascular disease (17). Furthermore, total occupational burden has been linked to cardiovascular risk in physicians (18). Stress and unfavorable psychosocial working conditions may exacerbate cardiovascular disease in the physician occupational group (19). Overwork-related mortality can be linked to cerebrovascular illnesses (17), whereas induced Takotsubo cardiomyopathy has been linked to work-related stress (20, 21).
The goal of this project was to investigate the relationship between burnout and cardiovascular disease in healthcare professionals using multivariable linear regression models that were adjusted for relevant confounding variables such as socio-demographics and anthropometrics, as well as traditional CVD risk factors.
Ethical approval was obtained from the Abu Dhabi COVID19 Research IRB Committee of the Department of Health-Abu Dhabi (DOH/NCVDC/2020/1052) and Emirates IRB for COVID Research Committee (DOH/CVDC/2020/1246). Informed consent was obtained before accepting to complete the online questionnaires (22, 23).
This was an exploratory observational cross-sectional study that covered Hospitals in Abu Dhabi capital of the United Arab Emirates. The study was carried out from July to November 2020, during the second wave of the COVID-19 pandemic, when medical countermeasures were being implemented (24, 25). The STROBE–The EQUATOR Network guidelines were followed to design the protocol of this study (26).
The online survey was distributed to a cohort of healthcare professionals from Abu Dhabi hospitals and healthcare institutions via institutional mass email addressed by either a campus office or the researcher (27, 28). Inclusion criteria were all residents, staff physicians, nurses and auxiliary healthcare professionals from both inpatient and outpatient medical services who agreed to be a part of the study. Exclusion criteria is not willing to complete a written consent form. Potential participants in the study were recruited through institutional mass email, which is sent by either a campus office or the researcher (27). The study uses random probability sampling with each population member having a non-zero chance of being selected. Since our study was sponsored by academic and governmental agencies, we expected to have good response rates for mass email recruitment (29). Electronic surveys are widely used for collecting data in an efficient and timely manner (30) and therefore were used for Maslach Burnout Inventory (MBI), Fuster-BEWAT score (FBS) and socio-demographic characteristics.
Primary outcomes were (I) Burnout through MBI emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA) subscale scores; (II) Cardio-vascular risk through FBS (31, 32). The MBI is the most commonly used standard for assessing burnout in healthcare professionals. This validated instrument contains 22 elements that include an overall measure of burnout as well as three distinct burnout domains: personal accomplishment, emotional exhaustion, and depersonalization (33). The FBS is a cardiovascular health metric consisting of 5 modifiable risk factors: blood pressure, exercise, weight, alimentation, tobacco. Notably, the Fuster-BEWAT and the AHA cardiovascular risk scores predicted the presence and extent of subclinical atherosclerosis (32) and left ventricular hypertrophy classification (34) with similar accuracy. The FBS is a simplified method that does not require laboratory tests and therefore can be applied in primary care settings or communities. Secondary outcomes were (III) sleep quality through wearable monitoring technology (Polar Ignite) (35).
The collection and management of data consisted of 3 distinct steps, as described in the published protocol (28): (a) data collection, (b) data handling and linkage and (c) data visualization. All participant information, and data generated during this study was kept confidential in accordance with the HIPAA (Health Insurance Portability and Accountability Act of 1996) (36) on subject privacy and will not be used for any purpose other than conducting the study. Participant data was coded and matched to random numbers to ensure protection of data.
Descriptive statistics, including the observed frequency counts and percentages for healthcare professionals’ socio-demographic characteristics and cardiovascular risk factors included in the FBS [e.g., blood pressure (B), exercise (E), weight (W), alimentation (A), and tobacco (T)], were performed. Further, the Chi-square statistical test (at a significance level of 0.05) was applied to compare the distribution of responses to the gender. Following this, descriptive statistics (including means, standard deviations and ranges) were calculated for FBS and three MBI scales, namely emotional exhaustion (EE), personal accomplishment (PA) and depersonalization (DP). Further, a correlation analysis was carried out between FBS and all possible predictors, including MBI scales and socio-demographic information, to examine the statistical properties and test each coefficient’s significance using p-values.
Following the descriptive statistics, linear regression analysis was conducted to investigate the association between the outcome variable (FBS) and MBI scales adjusted with the socio-demographic factors. As socio-demographic information may be potential confounders of FBS, no variable selection approach (e.g., stepwise regression analysis) was applied. Considering potential effect of correlation among predictors, different models were created. To select the best fitting regression model, Akaike information criterion (AIC) was used as an estimator to compare the relative quality of statistical models. The variance inflation factor (VIF) diagnostic was also calculated in each model to prevent unreliable estimates of coefficients with possible high correlations among predictors. In the regression model, results are reported as coefficients with 95% confidence intervals (CIs) and p < 0.05 indicating statistical significance. Analyses were performed with STATA 16.1 (Stata Corp., LLC, United States).
By completing the online surveys, 537 healthcare professionals were recruited in the cohort. After cleaning up the data from incomplete or invalid questionnaires, the recruited cohort included 396 (73.7%) participants who completed socio-demographic characteristics, 396 (73.7%) who completed the MBIs’ subscale scores depersonalization (MBI-DP), 392 (73.0%) who completed personal accomplishment (MBI-PA), 389 (72.4%) who completed emotional exhaustion (MBI-EE), and 388 (72.2%) who completed the FBS. Of the 110 participants who used wearable sleep monitoring, 47 (42.73%) who had sleep reports that could be associated with the burnout and cardiovascular health scores were included in the study.
The socio-demographic characteristics of the participants are summarized and compared regarding the gender. As shown in Table 1A, it was noted that there is a difference in the distribution of responses to the gender among some comparison groups, such as age (p = 0.003), marital status (p = 0.002), specialty (p < 0.001), education (p < 0.001), and working hours (p = 0.025).
Table 1B shows there is statistically significant difference in the distribution of responses to the gender among some FBS components, such as blood pressure (p < 0.001), exercise (p < 0.001), and tobacco (p < 0.001).
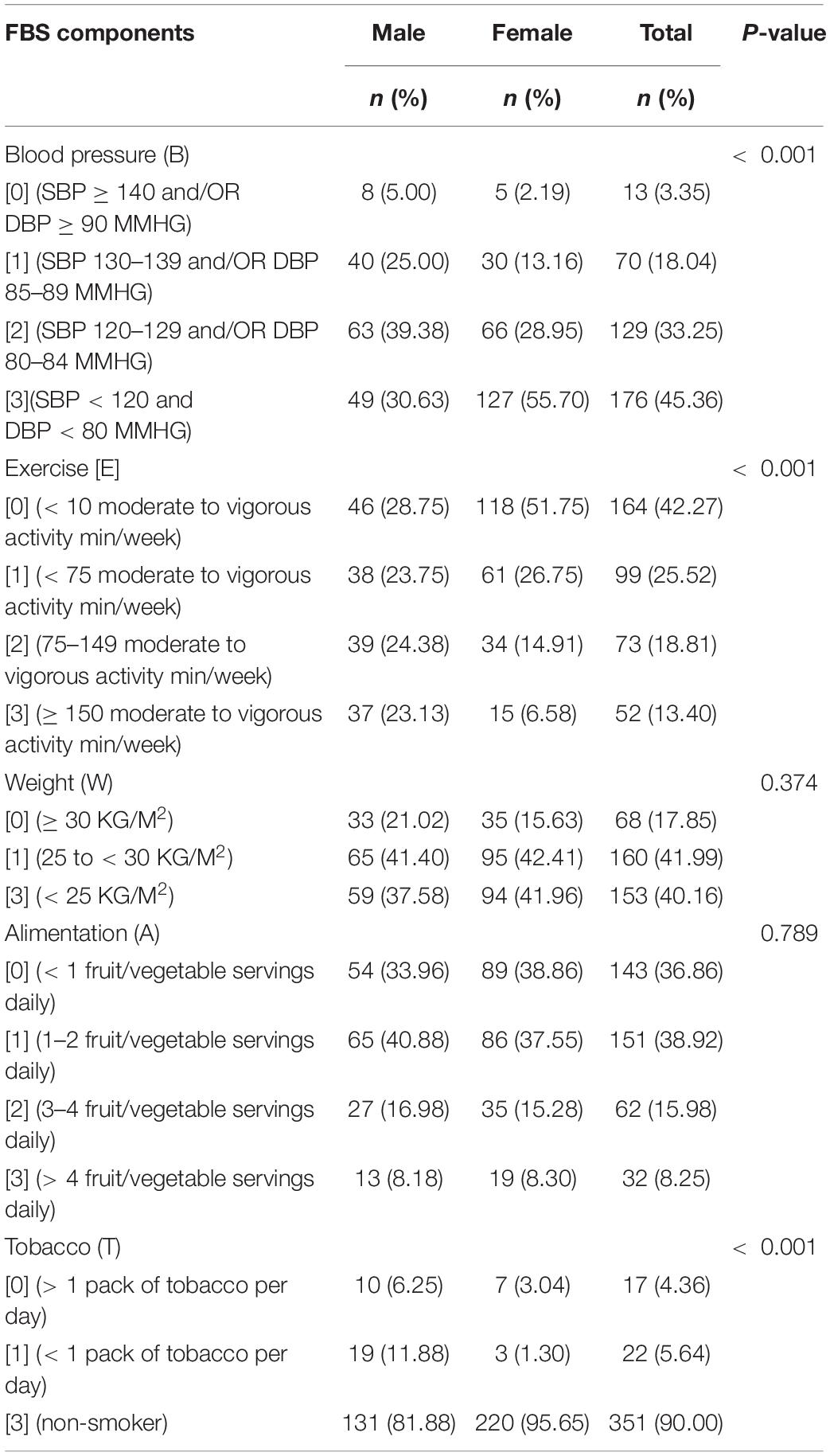
Table 1B. Fuster-BEWAT score (FBS): participant characteristics and descriptive statistics by gender (N = 388).
Table 2 provides the descriptive results, while Table 3 shows the Spearman’s rank correlation coefficients for FBS, MBI scales and socio-demographic information.
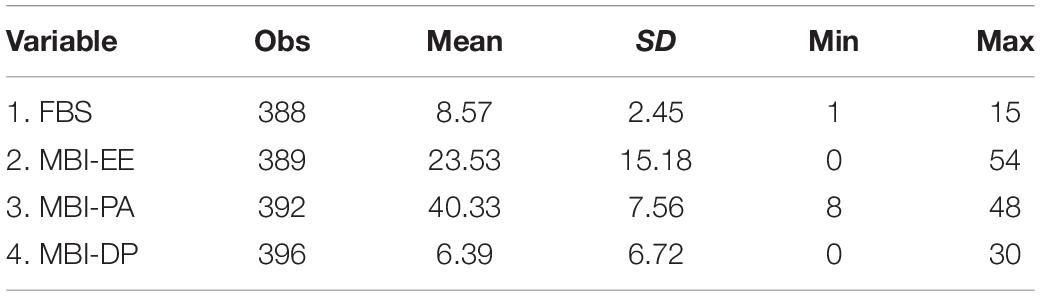
Table 2. Descriptive statistics for fuster-bewat score (FBS), Maslach Burnout Inventory (MBI) emotional exhaustion (MBI-EE), depersonalization (MBI-DP), and personal accomplishment (MBI-PA) subscale scores.
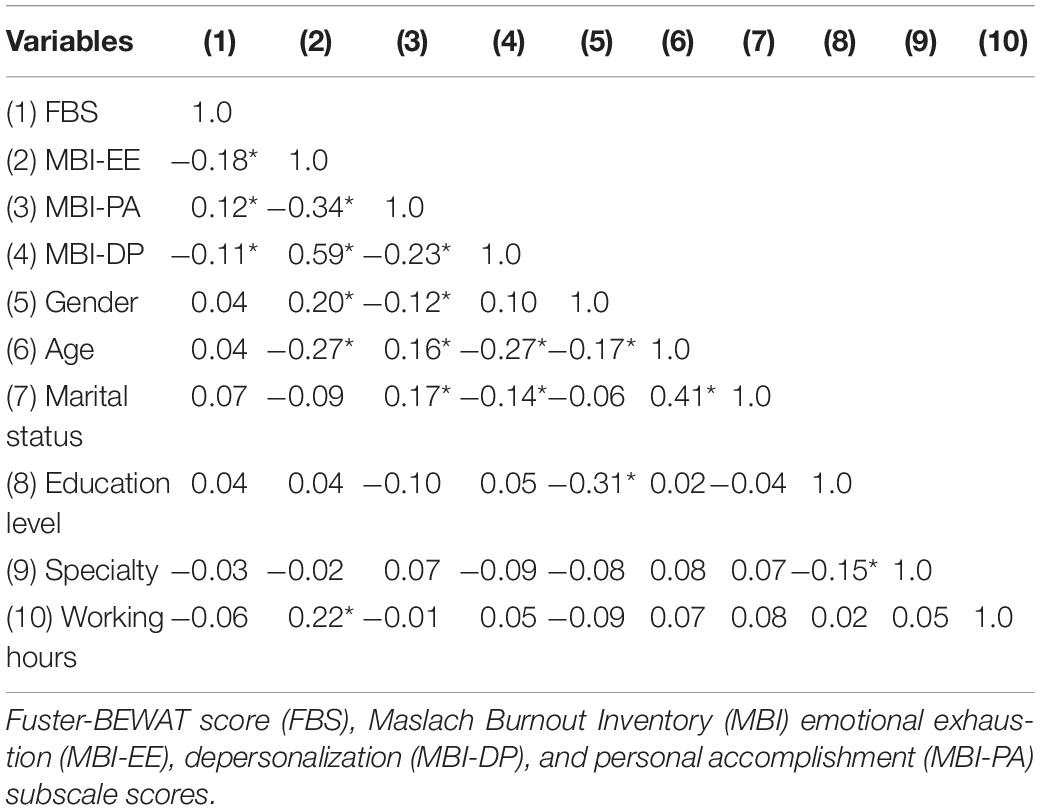
Table 3. Spearman’s rank correlation coefficients for FBS, MBI dimensions and socio-demographic information (*p < 0.05).
Statistically significant correlation has been observed among FBS, MBI components and some socio-demographic variables. In particular, high correlation among MBI components, such as between MBI-EE and MBI-DP (coef: 0.59, p < 0.05, Table 3).
Table 4 presents the results of the regression analysis with FBS as the outcome. Considering high correlations, different regression models were created to investigate the role of MBI components individually (model 1–3) and in combination with each other (model 4–7) adjusted with the socio-demographic factors. Seven models were built and AIC was employed to select the best fitting regression model.
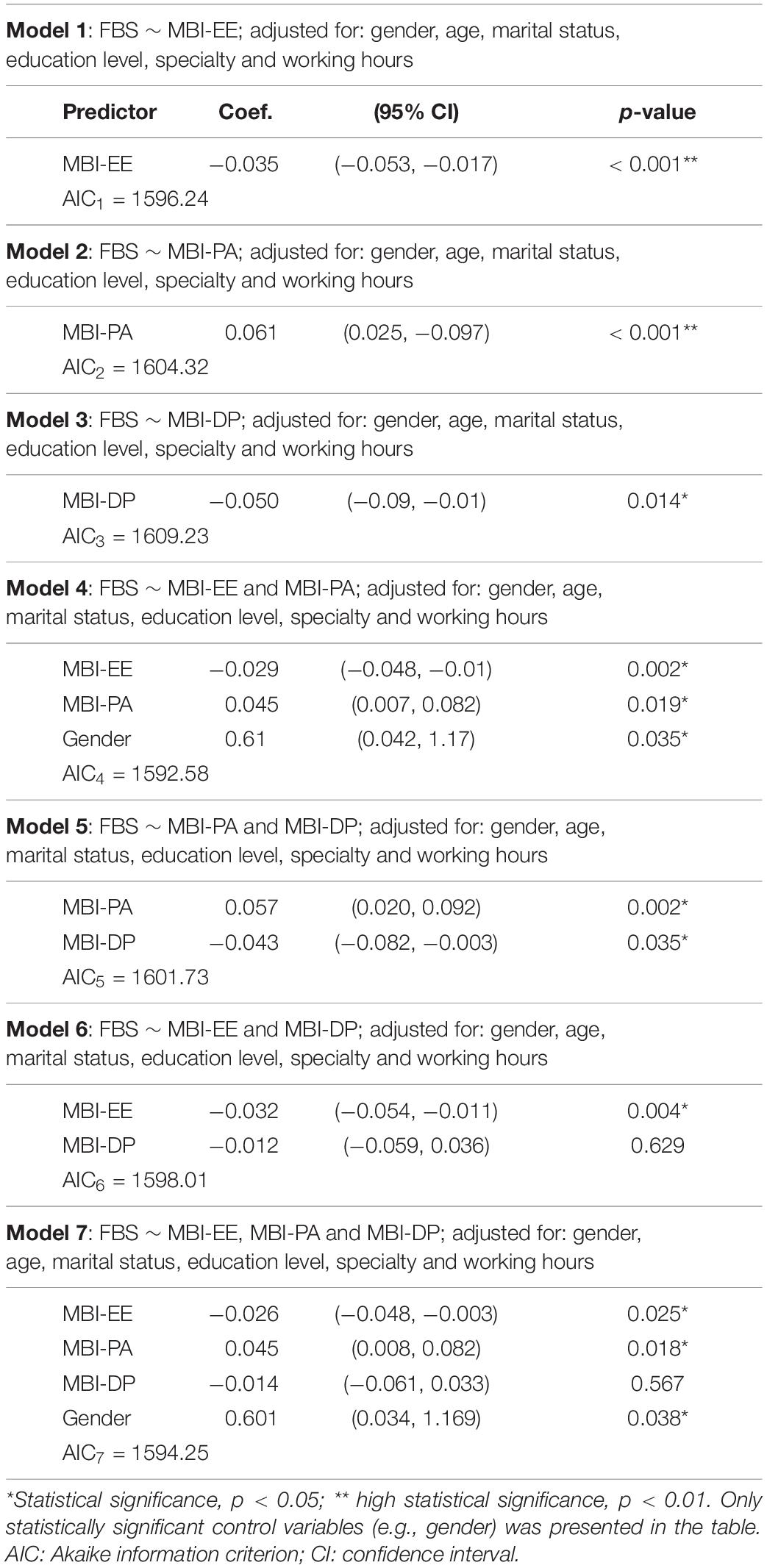
Table 4. The regression models for Fuster-BEWAT score (FBS) with Maslach Burnout Inventory (MBI) emotional exhaustion (MBI-EE), depersonalization (MBI-DP), and personal accomplishment (MBI-PA) subscale scores (N = 388).
Based on the AIC, the results suggested that Model 4 is the best fitting model (AIC4 = 1592.58). It showed a negative association between cardiovascular health and emotional exhaustion (p < 0.05). The higher the emotional exhaustion the lower the cardiovascular health. Further, the model showed a positive association between personal accomplishment and cardiovascular health (p < 0.05). It should be noted that Model 4 does not include depersonalization as a predictor. While Model 3 and 5 showed a statistically significant negative association between cardiovascular health and depersonalization (p < 0.01), Model 6 and 7 did not support this. However, such discrepancy for depersonalization effect may be explained by its monotonic relationship with emotional exhaustion (rho: 0.59, p < 0.05).
Emotional exhaustion was significantly positive correlated with REM and light sleep average (Spearman’s rank correlation: 0.35 and 0.37, respectively, with P < 0.05) (Table 5).
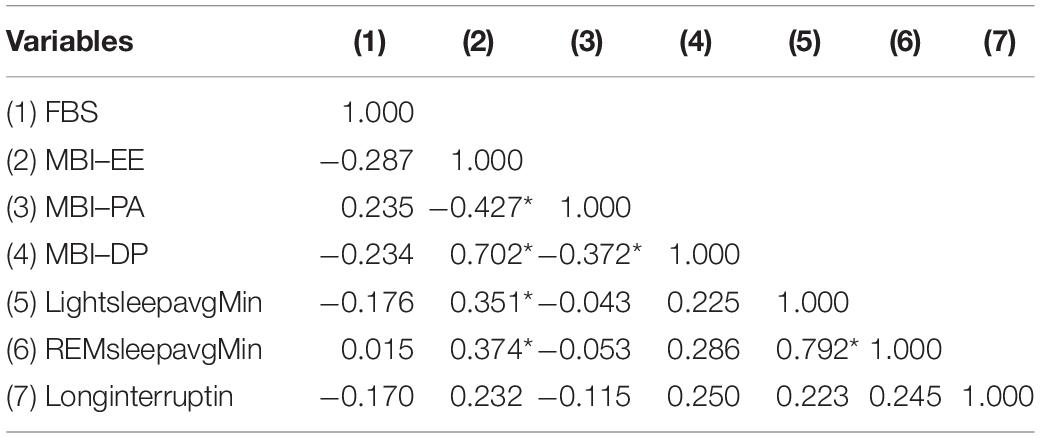
Table 5. Spearman’s rank correlation coefficients between Maslach Burnout Inventory, Fuster-BEWAT score (FBS), and sleep scores (light sleep average, REM sleep average, and long interruptions) (N = 47, *p < 0.05).
As the study’s main finding, healthcare practitioners with a low composite cardiovascular health score are more emotionally exhausted. This is, to the best of our knowledge, the first prospective study in the Middle East that examines the relationship between burnout and cardiovascular health. Although this study cannot conclusively establish a causal relationship between burnout and cardiovascular risk, the data indicate that healthcare practitioners with burnout have an associated cardiovascular risk. Furthermore, preliminary data from this study highlights the relationship between emotional exhaustion and sleep alterations detected through heart rate variability monitoring, implying that sleep and heart rate variability measures could be a promising starting point for explaining the mechanisms underlying burnout symptoms and cardiovascular disease. The findings of this study may be relevant in creating preventive strategies for burnout and cardiovascular risk reduction or prevention.
In this study, some comparison groups have different distributions of responses to gender, such as age (more women in the preponderant age group of 30–39), marital status (higher rate of single women than men, married men than women), specialty (more women than men nurses), working hours (more women than men in the category with 30–40 h per week, and more men than women in the category of more than 40 h per week) and education (more women than men in the preponderant group with bachelor degree). Professional specialty was found to be significantly related to high levels of emotional exhaustion and depersonalization among hospital healthcare workers during the COVID-19 pandemic (37, 38). The groups with a higher response rate in this study may indicate that they are more receptive to psychological support programs. These findings corroborate and complement a study that examined the impact of the COVID-19 outbreak on health professionals in Northern Italy and identified female gender, nurse status, hospital work, and contact with COVID-19 patients as predictors of both emotional exhaustion and depersonalization (39). The disparities in response distribution in our study, on the other hand, could point to a general distribution per category that is independent of the pandemic. For example, the fact that more men reported high blood pressure and smoking while more women reported low physical activity may reflect the well-known high prevalence of hypertension and smoking in men while women are more sedentary (40, 41).
A high correlation between the dimensions of burnout-Emotional Exhaustion (EE), Depersonalization (DP) has been observed in this study. Fear of COVID-19 infection was linked to extreme emotional exhaustion and depersonalization (37). This study is consistent with a study of Bulgarian healthcare professionals, which found that emotional exhaustion and depersonalization are associated with low levels of sense of coherence (SOC) as a salutogenic construct in three dimensions: meaningfulness (Me), the desire of an individual to be motivated to cope; comprehensibility (C), the belief that the challenge is understood; and manageability (Ma), the belief that coping resources are available (42).
A negative association between cardiovascular health and emotional exhaustion has been observed in this study. The higher the emotional exhaustion the lower the cardiovascular health. Further, the model showed a positive association between personal accomplishment and cardiovascular health. Recent research indicates that a variety of psychosocial risk factors, such as work stress (43), vital exhaustion (44), or social isolation (45), raise the risk of recurrent cardiac events as well as cardiac and all-cause mortality. Screening for such psychosocial risk factors in populations with cardiovascular risk factors has the potential to improve understanding of their role in the occurrence and outcome of cardiovascular disease (46).
This study establishes a link between emotional exhaustion and REM sleep periods in healthcare professionals during the COVID-19 pandemic. Sleep, and particularly REMS, have recently been shown to play an important role in the emotional and mental recovery from difficult circumstances (47). A positive relationship between exhaustion and insomnia has been already observed in healthcare professionals already in March and April 2020 during the COVID-19 pandemic (48). Sleep quality can be influenced by high psychological distress, high emotional exhaustion, low depersonalization, and low personal accomplishment (49). Furthermore, sleep disturbances have been linked to psychological distress in healthcare workers during the COVID-19 pandemic (50). Sleep disturbances are increasingly being linked to the development of cardiovascular diseases. The Sleep Heart Health Study, which monitored 3,810 participants for 11 years, revealed that inefficient sleep was related with an increased risk of incident cardiovascular disease events (51). Sleep disturbances have been linked to an increased risk of cardiovascular disease. Heart rate variability, a measure of autonomic nervous system dysfunction seen in sleep disorders, appears to be an essential marker of this risk (52–54). On the mechanisms that may be responsible for these sleep changes, the heart rate variability that is at the heart of the algorithm used to describe these sleep stages is also considered to be a reflection of the autonomic nervous system tone (55, 56). In this line of evidence, a recent study demonstrated that vagal dysfunction is both predictive and specific for burnout symptoms, suggesting that heart rate variability may be a promising starting point for explaining the mechanisms underlying burnout symptoms and cardiovascular diseases (57). Wearable sleep monitoring is gaining popularity, indicating the possibility of expanding burnout research through the use of wearable technology (58). On the other hand, the wide range of accuracy among commercial sleep technologies highlights the critical need for ongoing evaluations of newly developed sleep technologies (59, 60).
The study’s shortcomings must be acknowledged. The main weakness of this cross-sectional study was its inability to assess incidence and draw causal conclusions due to its design. There is no evidence of a temporal link between exposure and result. Although this study was originally intended to be a longitudinal one, it was converted to a cross-sectional one due to pandemic restrictions that made onsite visits difficult (28). As a result, the number of participants using wearable technology was significantly lower when compared to data gathered from online surveys. Another reason for avoiding the use of wearable technology was apprehension about being tracked by a GPS device. Another important factor that contributed to a decrease in interest for both recruiters and participants in participating in onsite visits was the longer-than-expected duration of social restrictions caused by pandemics.
In conclusion, this study provides evidence for a link between burnout and cardiovascular risk. Sleep disturbances caused by an altered autonomic nervous system may represent a mechanistic link between burnout and cardiovascular disease. These findings may lend support for policymakers and organizations campaigning for better occupational health. The development of occupational health surveillance and workplace health promotion initiatives by policymakers to prevent and treat burnout as well as other mental health disorders in the workplace during and after the COVID 19 pandemic is a potential future direction (61).
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval was obtained from the Abu Dhabi COVID19 Research IRB Committee of the Department of Health-Abu Dhabi (DOH/NCVDC/2020/1052) and Emirates IRB for COVID Research Committee (DOH/CVDC/2020/1246). The patients/participants provided their written informed consent to participate in this study.
HA, OB, MA, MD, WA, and LC: study conception and design. FA, NA, SA, MB, NA, MA, and MD: investigation. MS, NU, EA, LC, HA, and OB: data curation and analysis. FA, NA, SA, MB, NA, MS, NU, MD, MA, LC, WA, EA, HA, and OB: interpretation of the data, writing of the manuscript, and critical revision of the manuscript regarding the important intellectual content. All authors contributed to the article and approved the submitted version.
This research was supported by Khalifa University of Science and Technology under Award No. CPRA-2020-034 to OB and Award No. FSU-2020-23 to EA.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We like to express their gratitude to the Abu Dhabi Department of Health for its significant assistance during the course of the study. We thank the healthcare professionals for their time and willingness to participate in the study.
1. Elkind MSV, Harrington RA, Benjamin IJ. The role of the American heart association in the global COVID-19 pandemic. Circulation. (2020) 141:e743–5. doi: 10.1161/CIRCULATIONAHA.120.046749
2. Skulstad H, Cosyns B, Popescu BA, Galderisi M, Salvo GD, Donal E, et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. (2020) 21:592–8. doi: 10.1093/ehjci/jeaa072
3. Barba R, Rosado C, Pardo-Moreno J, Rey-Biel J. Managing People, Roles, and Resources During Covid-19 Surge. NEJM Catalyst | Innovations in Care Delivery. (2020). Available online at: https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0152 (accessed February 23, 2022).
4. Perlis RH. Exercising heart and head in managing coronavirus disease 2019 in Wuhan. JAMA Netw Open. (2020) 3:e204006. doi: 10.1001/jamanetworkopen.2020.4006
5. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. (2020) 173:317–20. doi: 10.7326/M20-1083
6. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7. Chirico F, Ferrari G, Nucera G, Szarpak L. Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: a rapid umbrella review of systematic reviews. J Health Soc Sci. (2021) 6:209–20.
8. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
9. Kader N, Elhusein B, Al Abdulla S, Hamza AH, Al Maslamani M, Chandra P, et al. Risk perception and psychological impact of COVID-19 pandemic among healthcare workers in primary and secondary healthcare settings in Qatar: a National study. J Prim Care Community Health. (2021) 12:21501327211039710. doi: 10.1177/21501327211039714
12. Prochalska C, Gressier F, Corruble E. Chronic fatigue syndrome: an update for psychiatrists. Open J Psychiatr. (2012) 02:40–8. doi: 10.4236/ojpsych.2012.21007
13. Cleland JGF, Chattopadhyay S, Khand A, Houghton T, Kaye GC. Prevalence and incidence of arrhythmias and sudden death in heart failure. Heart Fail Rev. (2002) 7:229–42. doi: 10.1023/a:1020024122726
14. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (2016) 15:103–11. doi: 10.1002/wps.20311
15. Karasek R, Theorell T. Healthy work: Stress, Productivity and the Reconstruction of Working Life. New York, NY: Basic Books (1990).
16. Sacker A, Bartley MJ, Frith D, Fitzpatrick RM, Marmot MG. The relationship between job strain and coronary heart disease: evidence from an english sample of the working male population. Psychol Med. (2001) 31:279–90. doi: 10.1017/s0033291701003270
17. Lo E-WV, Wei Y-H, Hwang B-F. Association between occupational burnout and heart rate variability: a pilot study in a high-tech company in Taiwan. Medicine. (2020) 99:e18630. doi: 10.1097/MD.0000000000018630
18. Belkić K, Nedić O. Night work, total occupational burden and cancer/cardiovascular risk factors in physicians. Med Pregl. (2012) 65:461–9. doi: 10.2298/MPNS1212461B
19. Juárez-Pérez CA, Aguilar-Madrid G, Haro-García LC, Gopar-Nieto R, Cabello-López A, Jiménez-Ramírez C, et al. Increased cardiovascular risk using atherogenic index measurement among healthcare workers. Arch Med Res. (2015) 46:233–9. doi: 10.1016/j.arcmed.2015.03.002
20. O’Sullivan G, O’Sullivan K, Gallagher J. Work-related stress induced takotsubo cardiomyopathy. Ir Med J. (2020) 113:27.
21. Mielczarek A, Kasprzak JD, Marcinkiewicz A, Kurpesa M, Uznańska-Loch B, Wierzbowska-Drabik K. Broken heart as work-related accident: occupational stress as a cause of takotsubo cardiomyopathy in 55-year-old female teacher – Role of automated function imaging in diagnostic workflow. Int J Occup Med Environ Health. (2015) 28:1031–4. doi: 10.13075/ijomeh.1896.00564
22. Lunt H, Connor S, Skinner H, Brogden G. Electronic informed consent: the need to redesign the consent process for the digital age. Intern Med J. (2019) 49:923–9. doi: 10.1111/imj.14339
23. Chen C, Turner SP, Sholle ET, Brown SW, Blau VLI, Brouwer JP, et al. Evaluation of a REDCap-based workflow for supporting federal guidance for electronic informed consent. AMIA Jt Summits Transl Sci Proc. (2019) 2019:163–72.
24. World Health Organization. United Arab Emirates: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data | WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. (2020). Available online at: https://covid19.who.int/region/emro/country/ae (accessed October 21, 2021).
25. World Health Organization. Overview of the COVID-19 Pandemic. (2021). Available online at: https://www.who.int/news-room/events/detail/2021/03/03/default-calendar/overview-of-the-covid-19-pandemic-a-high-level-overview-of-emerging-issues-in-each-phase-of-the-pandemic (accessed October 21, 2021).
26. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
27. Hammersley ML, Okely AD, Batterham MJ, Jones RA. An internet-based childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res. (2019) 21:e11964. doi: 10.2196/11964
28. Al Tunaiji H, Al Qubaisi M, Dalkilinc M, Campos LA, Ugwuoke NV, Alefishat E, et al. Impact of COVID-19 pandemic burnout on cardiovascular risk in healthcare professionals study protocol: a multicenter exploratory longitudinal study. Front Med (Lausanne). (2020) 7:571057. doi: 10.3389/fmed.2020.571057
29. Manfreda KL, Bosnjak M, Berzelak J, Haas I, Vehovar V. Web surveys versus other survey modes: a meta-analysis comparing response rates. Int J Market Res. (2008) 50:79–104. doi: 10.1177/147078530805000107
30. Sutherland MA, Amar AF, Laughon K. Who sends the email? Using electronic surveys in violence research. West J Emerg Med. (2013) 14:363–9. doi: 10.5811/westjem.2013.2.15676
31. Gómez-Pardo E, Fernández-Alvira JM, Vilanova M, Haro D, Martínez R, Carvajal I, et al. A comprehensive lifestyle peer group-based intervention on cardiovascular risk factors: the randomized controlled fifty-fifty program. J Am Coll Cardiol. (2016) 67:476–85. doi: 10.1016/j.jacc.2015.10.033
32. Fernández-Alvira JM, Fuster V, Pocock S, Sanz J, Fernández-Friera L, Laclaustra M, et al. Predicting subclinical atherosclerosis in low-risk individuals: ideal cardiovascular health score and fuster-BEWAT Score. J Am Coll Cardiol. (2017) 70:2463–73. doi: 10.1016/j.jacc.2017.09.032
33. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
34. Wang H, Sun G, Li Z, Guo X, Sun Y. Ideal cardiovascular health score and fuster-BEWAT score as predictors of left ventricular hypertrophy classification. J Am Coll Cardiol. (2018) 72:581–2. doi: 10.1016/j.jacc.2018.05.037
35. Oldenburg M, Jensen H-J. Stress and strain among seafarers related to the occupational groups. Int J Environ Res Public Health. (2019) 16:1153. doi: 10.3390/ijerph16071153
36. Edemekong PF, Annamaraju P, Haydel MJ. Health Insurance Portability and Accountability Act StatPearls. Treasure Island, FL: StatPearls Publishing. (2022).
37. Elhadi M, Msherghi A, Elgzairi M, Alhashimi A, Bouhuwaish A, Biala M, et al. Burnout syndrome among hospital healthcare workers during the COVID-19 pandemic and civil war: a cross-sectional study. Front Psychiatry. (2020) 11:579563. doi: 10.3389/fpsyt.2020.579563
38. Li D, Wang Y, Yu H, Duan Z, Peng K, Wang N, et al. Occupational burnout among frontline health professionals in a high-risk area during the COVID-19 outbreak: a structural equation model. Front Psychiatry. (2021) 12:575005. doi: 10.3389/fpsyt.2021.575005
39. Giusti EM, Pedroli E, D’Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
40. Shehab A, Bhagavathula AS, AlHajri N. Sex differences in the antihypertensive treatment and risk of uncontrolled hypertension in 5308 hypertensive patients in the United Arab Emirates. Blood Press Monit. (2021) 26:333–40. doi: 10.1097/MBP.0000000000000539
41. Mohammadian Khonsari N, Shahrestanaki E, Ejtahed H-S, Djalalinia S, Sheidaei A, Hakak-Zargar B, et al. Long-term trends in hypertension prevalence, awareness, treatment, and control rate in the middle east and North Africa: a systematic review and meta-analysis of 178 population-based studies. Curr Hypertens Rep. (2021) 23:41. doi: 10.1007/s11906-021-01159-0
42. Stoyanova K, Stoyanov DS. Sense of coherence and burnout in healthcare professionals in the COVID-19 era. Front Psychiatry. (2021) 12:709587. doi: 10.3389/fpsyt.2021.709587
43. Sara JD, Prasad M, Eleid MF, Zhang M, Widmer RJ, Lerman A. Association between work-related stress and coronary heart disease: a review of prospective studies through the job strain, effort-reward balance, and organizational justice models. J Am Heart Assoc. (2018) 7:e008073. doi: 10.1161/JAHA.117.008073
44. Frestad D, Prescott E. Vital exhaustion and coronary heart disease risk: a systematic review and meta-analysis. Psychosom Med. (2017) 79:260–72. doi: 10.1097/PSY.0000000000000423
45. Hakulinen C, Pulkki-Råback L, Virtanen M, Jokela M, Kivimäki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK biobank cohort study of 479 054 men and women. Heart. (2018) 104:1536–42. doi: 10.1136/heartjnl-2017-312663
46. Mesa-Vieira C, Grolimund J, von Känel R, Franco OH, Saner H. Psychosocial risk factors in cardiac rehabilitation: time to screen beyond anxiety and depression. Glob Heart. (2021) 16:16. doi: 10.5334/gh.896
47. Suchecki D, Tiba PA, Machado RBREM. Sleep rebound as an adaptive response to stressful situations. Front Neurol. (2012) 3:41. doi: 10.3389/fneur.2012.00041
48. Secosan I, Virga D, Crainiceanu ZP, Bratu LM, Bratu T. Infodemia: another enemy for romanian frontline healthcare workers to fight during the COVID-19 outbreak. Medicina (Kaunas). (2020) 56:679. doi: 10.3390/medicina56120679
49. Wang B, Lu Q, Sun F, Zhang R. The relationship between sleep quality and psychological distress and job burnout among Chinese psychiatric nurses. Ind Health. (2021) 59:427–35. doi: 10.2486/indhealth.2020-0249
50. Pappa S, Sakkas N, Sakka E. A year in review: sleep dysfunction and psychological distress in healthcare workers during the COVID-19 pandemic. Sleep Med. (2021) S1389–S9457:391–9. doi: 10.1016/j.sleep.2021.07.009
51. Yan B, Yang J, Zhao B, Fan Y, Wang W, Ma X. Objective sleep efficiency predicts cardiovascular disease in a community population: the sleep heart health study. J Am Heart Assoc. (2021) 10:e016201. doi: 10.1161/JAHA.120.016201
52. Greenlund IM, Carter JR. Sympathetic neural responses to sleep disorders and insufficiencies. Am J Physiol Heart Circ Physiol. (2022) 322:H337–49. doi: 10.1152/ajpheart.00590.2021
53. Riganello F, Prada V, Soddu A, di Perri C, Sannita WG. Circadian rhythms and measures of cns/autonomic interaction. Int J Environ Res Public Health. (2019) 16:2336. doi: 10.3390/ijerph16132336
54. Milagro J, Deviaene M, Gil E, Lázaro J, Buyse B, Testelmans D, et al. Autonomic dysfunction increases cardiovascular risk in the presence of sleep apnea. Front Physiol. (2019) 10:620. doi: 10.3389/fphys.2019.00620
55. Campos LA, Bueno C, Barcelos IP, Halpern B, Brito LC, Amaral FG, et al. Melatonin therapy improves cardiac autonomic modulation in pinealectomized patients. Front Endocrinol (Lausanne). (2020) 11:239. doi: 10.3389/fendo.2020.00239
56. da Silva ELP, Pereira R, Reis LN, Pereira VL, Campos LA, Wessel N, et al. Heart rate detrended fluctuation indexes as estimate of obstructive sleep apnea severity. Medicine. (2015) 94:e516. doi: 10.1097/MD.0000000000000516
57. Wekenborg MK, Hill LK, Thayer JF, Penz M, Wittling RA, Kirschbaum C. The longitudinal association of reduced vagal tone with burnout. Psychosom Med. (2019) 81:791–8. doi: 10.1097/PSY.0000000000000750
58. Nelson EC, de Keijzer R, Vollenbroek-Hutten MMR, Verhagen T, Noordzij ML. The relationship between diagnosed burnout and sleep measured by activity trackers: four longitudinal case studies. In: Mucchi L, Hämäläinen M, Jayousi S, Morosi S editors. Body Area Networks: Smart IoT and Big Data for Intelligent Health Management. BODYNETS 2019. Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering. (Vol. 297), Cham: Springer (2019). doi: 10.1007/978-3-030-34833-5_24
59. Stone JD, Rentz LE, Forsey J, Ramadan J, Markwald RR, Finomore VS, et al. Evaluations of commercial sleep technologies for objective monitoring during routine sleeping conditions. Nat Sci Sleep. (2020) 12:821–42. doi: 10.2147/NSS.S270705
60. Rentz LE, Ulman HK, Galster SM. Deconstructing commercial wearable technology: contributions toward accurate and free-living monitoring of sleep. Sensors (Basel). (2021) 21:5071. doi: 10.3390/s21155071
Keywords: cardiovascular risk (CV risk), emotional exhaustion (EE), depersonalization (DP), work stress, REM sleep, sleep alterations
Citation: Alameri F, Aldaheri N, Almesmari S, Basaloum M, Albeshr NA, Simsekler MCE, Ugwuoke NV, Dalkilinc M, Al Qubaisi M, Campos LA, Almahmeed W, Alefishat E, Al Tunaiji H and Baltatu OC (2022) Burnout and Cardiovascular Risk in Healthcare Professionals During the COVID-19 Pandemic. Front. Psychiatry 13:867233. doi: 10.3389/fpsyt.2022.867233
Received: 31 January 2022; Accepted: 25 February 2022;
Published: 04 April 2022.
Edited by:
Eka D. Chkonia, Tbilisi State Medical University, GeorgiaReviewed by:
Francesco Chirico, Catholic University of the Sacred Heart, ItalyCopyright © 2022 Alameri, Aldaheri, Almesmari, Basaloum, Albeshr, Simsekler, Ugwuoke, Dalkilinc, Al Qubaisi, Campos, Almahmeed, Alefishat, Al Tunaiji and Baltatu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hashel Al Tunaiji, ZHIuaGFzaGVsQGdtYWlsLmNvbQ==; Ovidiu Constantin Baltatu, b2NiYWx0YXR1QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.