- 1Department of Medicine, King Abdullah Medical City, Makkah, Saudi Arabia
- 2Department of Medicine, King Saud bin Abdulaziz University for Health Sciences, King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
- 3Department of Medicine, McGill University, Montreal, QC, Canada
Background: In early December 2019, a cluster of acute pneumonia of viral etiology had been identified in Wuhan, China. Later on, it has been named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing a worldwide pandemic. This pandemic triggered unprecedented health-related psychiatric sequalae. We aim in this study to evaluate the prevalence of depression and its associated factors among confirmed patients with COVID-19.
Methodology: This is a cross-sectional study, we included adult patients more than 18 years old who have been diagnosed with PCR-confirmed COVID-19 and managed in a hospital, home, or hotel. A self-administered online questionnaire based on Patient Health Questionnaire (PHQ-9) Quick Depression Assessment questionnaire was used.
Results: A total of 143 subjects completed the PHQ-9 questionnaire. The prevalence of moderate to severe depression was 34%. Prevalence of depression was positively associated with the female gender (p-value = 0.013). Location of COVID-19 management and financial status did not affect the prevalence of depression.
Conclusion: The prevalence of depression among patients with COVID-19 is high, which underscores the importance of active screening and management of depression in this population.
HIGHLIGHTS
- The prevalence of depression among patients with COVID-19 is high at 33.6%.
- Prevalence of depression was positively associated with the female gender.
- Location of COVID-19 management and financial status did not affect the prevalence of depression.
Introduction
In early December 2019, a cluster of acute pneumonia of unknown etiology had been identified in Wuhan, China. The pathogen was identified as a new RNA virus, which was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). After the rapid global spread of this virus, the WHO declared COVID-19 a pandemic on 12 March 2020 (1).
This outbreak triggered unprecedented health-related anxiety (2). During the pandemic, the rapid spread of SARS-CoV-2 during the pandemic resulted in a great burden on health and the economy, which prompted countries and health agencies to apply strict measures to decrease viral transmission. These measures included community lockdown, social distancing, and other strict measures which resulted in psychosocial and health-related sequences.
It has been demonstrated in various research that infection outbreaks affect people’s mental and psychosocial health significantly. In the initial phase of COVID-19 spread, people started to have symptoms of anxiety especially younger individuals with chronic diseases. These psychosocial and mental symptoms increased particularly after implementing the community lockdown (3), affecting both general populations and healthcare workers. The effect was more prominent among persons who lack social support and those who have been living with a suspected case of COVID-19 (4). As opposed to an influenza outbreak, where the anxiety was ranging from 10 to 33% in the general population (5). Alsaqri and colleagues found that around 67% of the study population were suffering from a degree of social anxiety during the COVID-19 pandemic (6).
In addition to the COVID-19-related strict precautionary measures that can cause mental health problems, COVID-19 disease itself can trigger mental health disorders like depression. It has been found that the prevalence of depression was 43% in clinically stable patients with COVID-19 (7). In a systematic review that evaluated infected patients with COVID-19, the pooled prevalence of depression was 45% (8).
Different studies have shown that depression can be associated with a depressed immune system, especially cellular immunity, which may have a negative impact on COVID-19 disease progression (9). This underscores the importance of screening patients with COVID-19 for any sign of depression. Symptoms of depression can persist even after the resolution of the disease. In one study that evaluated patients with COVID-19 after one month of their discharge from the hospital, the prevalence of depression was 18% (10). A substantial percentage of patients with COVID-19 have persistent symptoms of depression 3–6 months after COVID-19 symptoms onset (11). Thus, awareness and effective management of mental health-related disorders in patients with COVID-19 is strongly required.
The location of isolation either at home or in hospital settings may also have an impact on mental health. This, however, was not sufficiently evaluated in previous studies. We aim in this study to evaluate the prevalence of depression and its associated factors among COVID-19 confirmed patients and the factors, including isolation location that may influence mental health.
Materials and methods
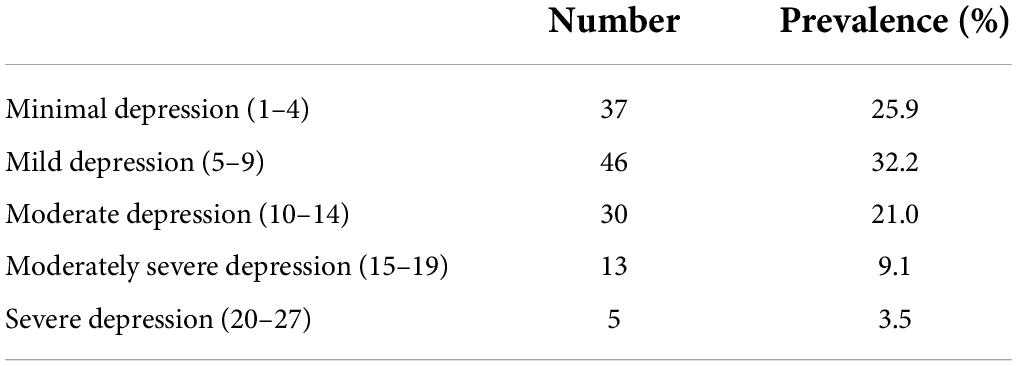
This is a cross-sectional study that included adult patients more than 18 years old who have been diagnosed with SARS-CoV-2 PCR confirmed COVID-19 and managed based on Saudi ministry of health guidelines in hospitals, homes, or hotels were involved. Patients were recruited from the COVID-19 clinic over a period of 3 months (March, April, and May, 2020). Critically ill patients, patients with previous diagnoses of depression, and patients with cognitive impairment such as dementia or delirium were excluded. A self-administered online questionnaire based on Patient Health Questionnaire (PHQ-9) Quick Depression Assessment questionnaire was used. This questionnaire has been validated, and it relies on patient self-report (12, 13). An electronic questionnaire was sent to 300 patients using their e-mails and cell phones. A total of 143 patients out of 300 patients (47.7%) responded and completed the questionnaire. The questionnaire contains questions related to demographic, social, educational, and financial status. We used PHQ-9 which is categorized as the following: A score of 1–4 is minimal depression, a score of 5–9 is mild depression, a score of 10–14 is moderate depression, a score of 15–19 is moderately severe depression, and a score of 20–27 is severe depression.
Statistical analysis
Data were analyzed by using Statistical Package for Social Studies (SPSS 22; IBM Corp., New York, NY, United States). Continuous variables were expressed as mean ± standard deviation and categorical variables were expressed as percentages. The t-test and the one-way ANOVA were used for continuous variables. The chi-square test was used for categorical variables. A p-value of <0.05 was considered statistically significant.
Ethics and confidentiality
Ethical approval, as well as the informed consent form for the study, was taken from the KAMC Institutional Review Board (Approval number: 20-643).
Results
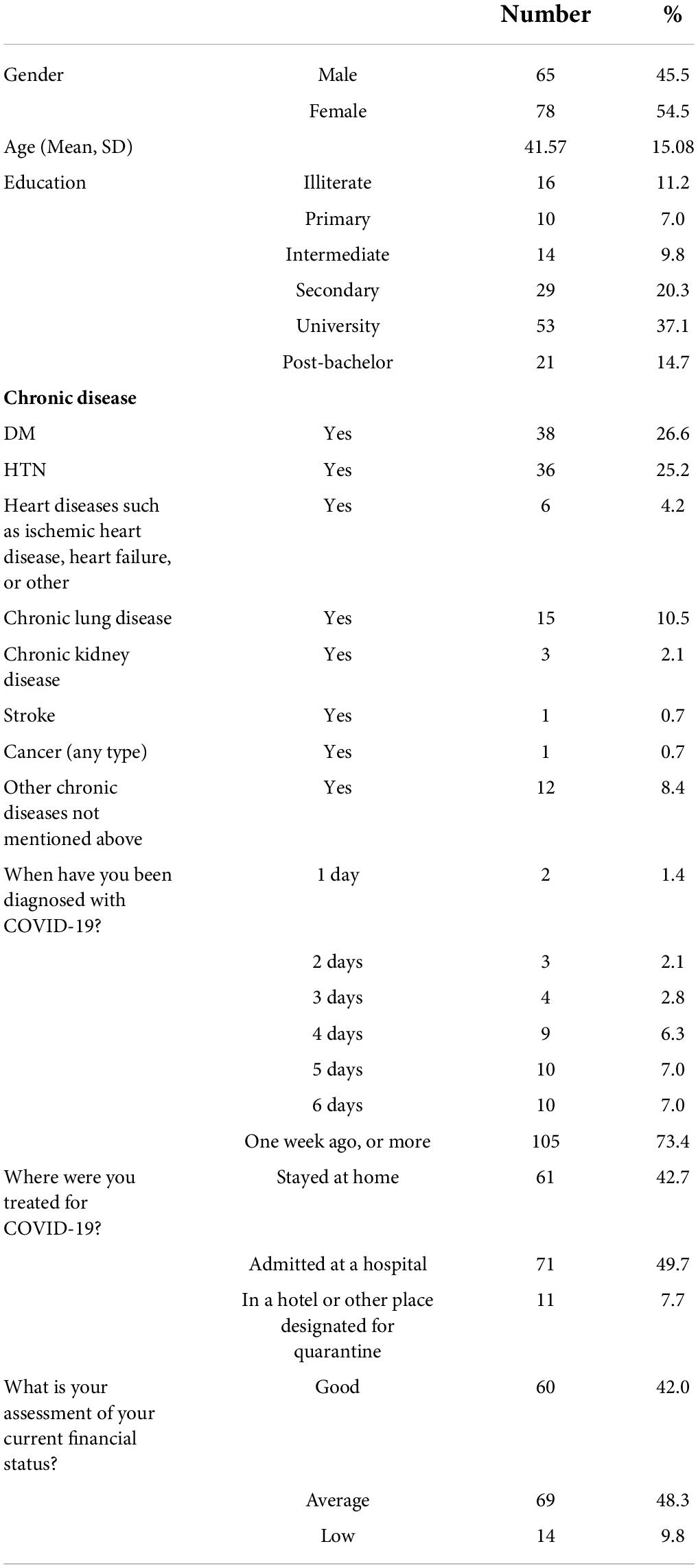
A total of 143 subjects completed the PHQ9 questionnaire and were included. The baseline demographic and disease characteristics are shown in Table 1. The mean age is 41 years, and the majority (78%) of the subjects were women. Most of the subjects (73%) were diagnosed with COVID-19 for more than 1 week and half of them (49.7%) were hospitalized. Subjects with a previous diagnosis of depression represented only 2%.
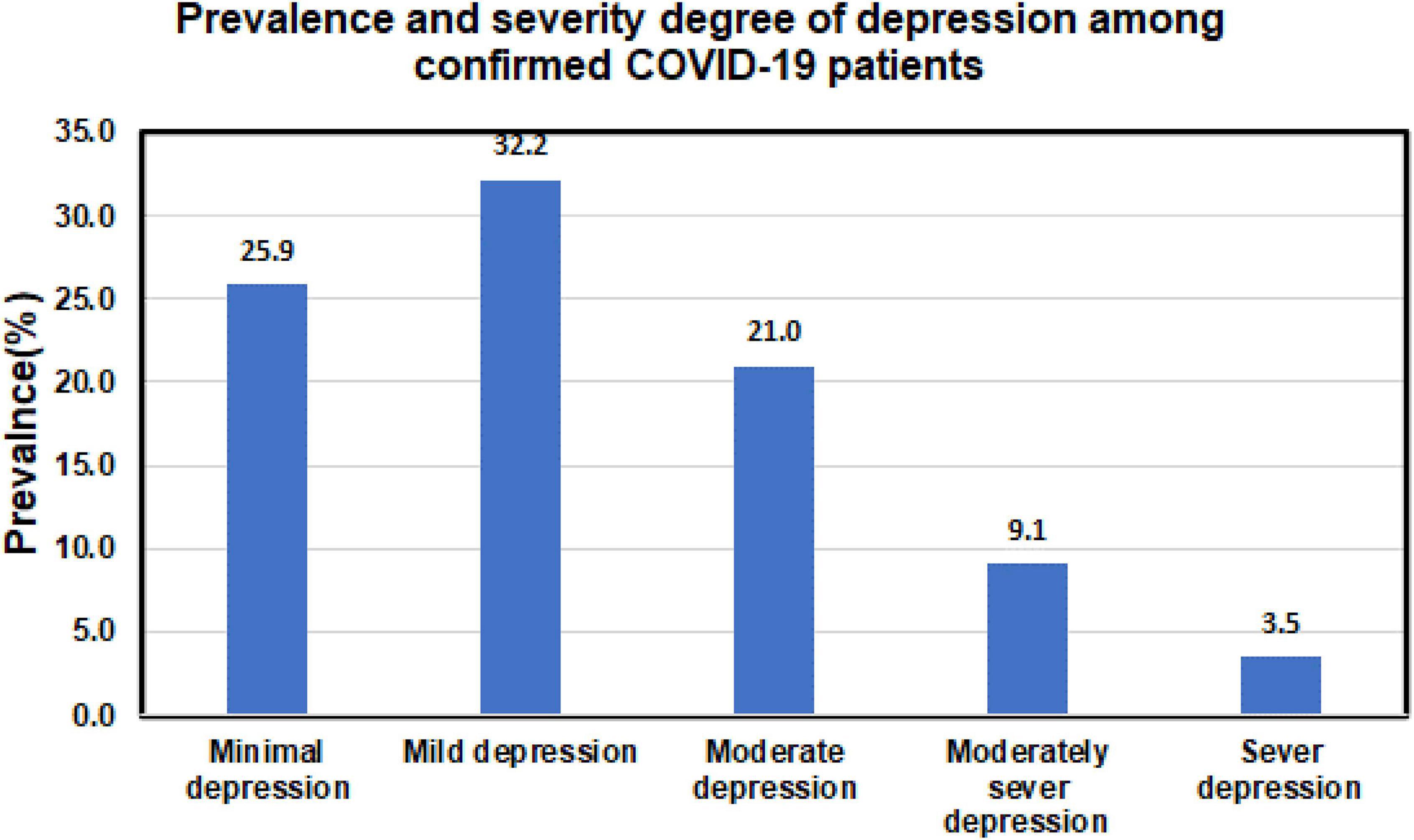
The prevalence of different depression severity categories is shown in Table 2. The prevalence of moderate to severe depression was 34%. The distribution of subjects across different degrees of depression severity is shown in Figure 1.
The severity degree of depression among confirmed patients with COVID-19 by their characteristics is shown in Table 3. The mean score of PHQ-9 for confirmed patients with COVID-19 by their characteristics is shown in Table 4. The prevalence of depression was positively associated with the female gender (p-value = 0.013). Location of COVID-19 management and financial status did not affect the prevalence of depression.

Table 3. The prevalence and severity degree of depression among confirmed patients with COVID-19 by their characteristics.

Table 4. Mean score of PHQ-9 depression questionnaire for confirmed patients with COVID-19 by their characteristics.
Discussion
We found that around one-third (34%) of patients diagnosed with COVID-19 suffered from moderate to severe depression, which was positively associated with the female gender. Location of COVID-19 management (hospital, home, or hotel) and financial status did not affect the prevalence of depression.
Our findings are consistent with what has been found in other studies. Ma and colleagues found that the prevalence of depression among patients with COVID-19 using the PHQ-9 questionnaire was 43.1%. Female gender and family history of severe COVID-19 disease have been found to be strong predictors of depression (7). In another cross-sectional study that was conducted on 1,002 patients with COVID-19 using PHQ-9, the prevalence of moderate to severe depression was as high as 48%. Depression was positively associated with lower family income, sleep disturbance, lack of physical activity, fear of COVID-19 re-infection, and persistent COVID-19 symptoms (14). In our study, female gender was a significant risk factor for depression. Other factors including financial status, comorbidities, duration of having COVID-19, and location of isolation did not affect the prevalence of depression.
Prevalence of depression has been found to be higher in patients with COVID-19 as compared to the general population. Alamri and colleagues found that the prevalence of depression among the general population in Saudi Arabia during the COVID-19 pandemic is 17% (15). It is low as compared to our finding in this study which is 34%. In a systematic review that involved multiple studies in different countries, the overall prevalence of depression in the general population was ranging from 14.6 to 48.3% (16). While in patients with COVID-19, the prevalence was higher as demonstrated in a systematic review and meta-analysis that evaluated infected patients with COVID-19, which found that the pooled prevalence of depression was 45% (8).
During the COVID-19 pandemic prevalence of depression was relatively high compared to the pre-pandemic period. The prevalence of depression symptoms in the United States of America was more than threefold higher during the COVID-19 pandemic compared to the pre-pandemic period (17). In one survey of the general population before the COVID-19 pandemic in Saudi Arabia, the prevalence of depression was 3.8% (18), which increased significantly during the pandemic as indicated in this study is 34%.
Some studies showed a higher prevalence of depression in actively hospitalized patients. Samrah and colleagues did a survey on patients with COVID-19 after 10 days of hospital isolation which showed a very high prevalence of 44% (19). In another study, 97.2% of hospitalized patients with COVID-19 with stable conditions had some degree of depression (20). In our study, the location where the patient received COVID-19 management at home, hotel, or hospital did not affect the prevalence of depression.
Although the high prevalence of depression among patients with COVID-19 could be explained by the quarantine and fear of disease, the inflammatory process of COVID-19 has been found to play a role in the psychiatric sequalae. Baseline systemic immune-inflammation index has positively associated with the prevalence of depression in 402 adults surviving COVID-19 at 1-month follow-up after hospital treatment (21).
It is important to acknowledge the limitations of our study, which include small sample size and an online self-assessment questionnaire rather than a face-to-face meeting and evaluation. Also, the absence of a control group from the general population during the same period is one of the limitations. On the other hand, we used a well-validated questionnaire and assessed different important variables that might affect the mental status.
Our study findings have important clinical implications as they indicate that the prevalence of depression is high in patients with COVID-19 as compared to the general population during the COVID-19 pandemic. This raises the importance of good assessment and evaluation of those patients for health-related psychiatric sequalae. This can be conducted through telemedicine or web-based care. In one study, digitally enabled remote care for people with long COVID-19 syndrome showed promising results; and there are ongoing studies to assess the online cognitive behavioral therapy that will be more accessible with less cost (22–24).
Conclusion
The prevalence of depression among patients with COVID-19 is high (34%), which underscores the importance of active screening and management of depression in this population that can be provided through telemedicine or web-based care. Depression was positively associated with the female gender in our population; however, the location of COVID-19 management and financial status did not influence the prevalence of depression.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The Institutional Review Board (IRB) of King Abdullah Medical City (KAMC) (Approval number: 20-643). The patients/participants provided their written informed consent to participate in this study.
Author contributions
EA and AA designed and supervised the study. EA, AMA, AT, ASA, and RA contributed to protocol development, data collection, interpretation of the analyzed data, and manuscript writing. OA, NG, and HM were involved in data collection and entry as well as manuscript editing. All authors reviewed and approved the final version of the manuscript.
Acknowledgments
We acknowledge the commitment and sacrifice of all healthcare providers during the COVID-19 pandemic.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Coronavirus Disease 2019 (COVID-19) Situation Report –96 2020. (2020). Available online at: https://www.who.int/docs/defaultsource/coronaviruse/situation-reports/20200425-sitrep-96-covid-19.pdf (who.int) (accessed April 25, 2020).
2. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
3. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España. Cadernos De Saude Publica. (2020) 36:e00054020. doi: 10.1590/0102-311X00054020
4. Anindyajati G, Wiguna T, Murtani BJ, Christian H, Wigantara NA, Putra AA, et al. Anxiety and its associated factors during the initial phase of the COVID-19 pandemic in Indonesia. Front Psychiatry. (2021) 12:634585. doi: 10.3389/fpsyt.2021.634585
5. Rubin GJ, Potts HW, Michie S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK. Health Technol Assess. (2010) 14:183–266. doi: 10.3310/hta14340-03
6. Alsaqri SH, Alkwiese MJ, Aldalaykeh MK, Hamzi MI, Mahdi MM, Shafie ZM. Anxiety among the general population during Coronavirus-19 disease in Saudi Arabia: implications for a mental support program. medRxiv [Preprint]. (2020). doi: 10.1101/2020.05.07.20090225
7. Ma YF, Li W, Deng HB, Wang L, Wang Y, Wang PH, et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J Affect Disord. (2020) 275:145–8. doi: 10.1016/j.jad.2020.06.033
8. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
9. Leonard BE. The immune system, depression and the action of antidepressants. Prog Neuro Psychopharmacol Biol Psychiatry. (2001) 25:767–80. doi: 10.1016/s0278-5846(01)00155-5
10. Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J Trauma Stress. (2005) 18:39–42. doi: 10.1002/jts.20004
11. Houben-Wilke S, Goërtz YM, Delbressine JM, Vaes AW, Meys R, Machado FV, et al. The impact of long COVID-19 on mental health: observational 6-month follow-up study. JMIR Mental Health. (2022) 9:e33704. doi: 10.2196/33704
12. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Int Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
13. AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An Arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann Gen Psychiatry. (2017) 16:32. doi: 10.1186/s12991-017-0155-1
14. Islam MS, Ferdous MZ, Islam US, Mosaddek A, Potenza MN, Pardhan S. Treatment, persistent symptoms, and depression in people infected with COVID-19 in Bangladesh. Int J Environ Res Public Health. (2021) 18:1453. doi: 10.3390/ijerph18041453
15. Alamri HS, Algarni A, Shehata SF, Al Bshabshe A, Alshehri NN, ALAsiri AM, et al. Prevalence of depression, anxiety, and stress among the general population in Saudi Arabia during Covid-19 pandemic. Int J Environ Res Public Health. (2020) 17:9183. doi: 10.3390/ijerph17249183
16. Xiong J, Lipsitz O, Nasri F, Lui L, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
17. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
18. Altwaijri YA, Al-Habeeb A, Al-Subaie AS, Bilal L, Al-Desouki M, Shahab MK, et al. Twelve-month prevalence and severity of mental disorders in the Saudi national mental health survey. Int J Methods Psychiatr Res. (2020) 29:e1831. doi: 10.1002/mpr.1831
19. Samrah SM, Al-Mistarehi AH, Aleshawi AJ, Khasawneh AG, Momany SM, Momany BS, et al. Depression and coping among COVID-19-infected individuals after 10 days of mandatory in-hospital quarantine, Irbid, Jordan. Psychol Res Behav Manag. (2020) 13:823–30. doi: 10.2147/PRBM.S267459
20. Zandifar A, Badrfam R, Yazdani S, Arzaghi SM, Rahimi F, Ghasemi S, et al. Prevalence and severity of depression, anxiety, stress and perceived stress in hospitalized patients with COVID-19. J Diabetes Metab Disord. (2020) 19:1431–8. doi: 10.1007/s40200-020-00667-1
21. Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. (2020) 89:594–600. doi: 10.1016/j.bbi.2020.07.037
22. Marano G, Traversi G, Gesualdi A, Biffi A, Gaetani E, Sani G, et al. Mental health and coaching challenges facing the COVID-19 outbreak. Psychiatr Danub. (2021) 33:124–6.
23. Murray E, Goodfellow H, Bindman J, Blandford A, Bradbury K, Chaudhry T, et al. Development, deployment and evaluation of digitally enabled, remote, supported rehabilitation for people with long COVID-19 (Living With COVID-19 Recovery): protocol for a mixed-methods study. BMJ Open. (2022) 12:e057408. doi: 10.1136/bmjopen-2021-057408
24. Reitsma L, Boelen PA, de Keijser J, Lenferink L. Online treatment of persistent complex bereavement disorder, posttraumatic stress disorder, and depression symptoms in people who lost loved ones during the COVID-19 pandemic: study protocol for a randomized controlled trial and a controlled trial. Eur J Psychotraumatol. (2021) 12:1987687. doi: 10.1080/20008198.2021.1987687
Keywords: depression, COVID-19, SARS-CoV-2, PHQ-9, psychiatric sequalae
Citation: Alqurashi E, Aldobyany A, Touman A, Alqahtani A, Alsaggaf R, Alnashiwaaty O, Ghaleb N, Mabar H and Albanna AS (2022) Prevalence of depression and its associated factors among patients with confirmed COVID-19 in Makkah, Saudi Arabia. Front. Psychiatry 13:863215. doi: 10.3389/fpsyt.2022.863215
Received: 26 January 2022; Accepted: 03 August 2022;
Published: 30 August 2022.
Edited by:
Alessandro Colasanti, Brighton and Sussex Medical School, United KingdomReviewed by:
Marianna Mazza, Agostino Gemelli University Polyclinic (IRCCS), ItalySiraj Wali, King Abdulaziz University, Saudi Arabia
Beata Gavurova, Tomas Bata University in Zlín, Czechia
Copyright © 2022 Alqurashi, Aldobyany, Touman, Alqahtani, Alsaggaf, Alnashiwaaty, Ghaleb, Mabar and Albanna. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Aldobyany, YWhtYWQyMTQ1QGhvdG1haWwuY29t
 Eid Alqurashi1
Eid Alqurashi1 Ahmad Aldobyany
Ahmad Aldobyany Abdullah Alqahtani
Abdullah Alqahtani Omar Alnashiwaaty
Omar Alnashiwaaty Amr S. Albanna
Amr S. Albanna