- 1Doxy.me Research, Doxy.me Inc., Rochester, NY, United States
- 2Department of Psychiatry and Behavioral Neurosciences, University of South Florida, Tampa, FL, United States
- 3Biomedical Informatics Center, Medical University of South Carolina, Charleston, SC, United States
The COVID-19 pandemic accelerated adoption of telemental health (TMH). Providers with limited TMH experience faced challenges during the rapid switch to remote patient care. We investigated TMH providers’ perceptions about remote care one year into the pandemic according to when providers adopted telemedicine (i.e., before vs. after March 2020) and how much of their caseloads were served remotely (i.e., < 50% vs. ≥ 50%). Between February–March 2021, 472 TMH providers completed a cross-sectional, web-based survey that measured perceived benefits and satisfaction with telemedicine, therapeutic alliance, patient-centered communication, eHealth literacy, multicultural counseling self-efficacy, and facilitating factors of using telemedicine. Providers who began using telemedicine before the pandemic reported having better training, task-related therapeutic alliance with patients, and ability to conduct multicultural interventions, assessments, and session management. Providers who served ≥ 50% of their caseload remotely reported greater satisfaction with their practice, stronger beliefs about the benefits of telemedicine, and greater perceived effects of telemedicine on alleviating the impact of COVID-19. There were no differences in reports of patient-centered communication nor eHealth literacy. In conclusion, providers who adopted TMH more recently may require additional training and support to successfully establish a working alliance with their patients, especially with multicultural aspects of care.
Introduction
Coronavirus Disease 2019 (COVID-19) ignited a shift in mental health care from in-person to remote delivery. In response to the pandemic, studies estimate over 97% of mental health providers have adopted telemental health (TMH) to supplement or replace in-person care (1, 2). Some mental health providers’ caseloads increased by 25–50% during the pandemic with patient surges as high as 6,558% (1, 3). Telemedicine revolutionized the delivery of evidence-based mental health care (4), and proved to be a dependable solution that 90% of providers surveyed intend to use beyond the resolution of COVID-19 (5). It is imperative to understand how mental health providers deliver remote services to inform and sustain post-pandemic TMH care models.
Mental health providers were highly satisfied with telemedicine before the pandemic, despite its slow uptake (2, 6). High satisfaction and benefits of TMH have been attributed to its convenience, the ability to reach more patients, and the opportunity for a better work-life balance (7). The COVID-19 pandemic led to an abrupt transition from in-person care to TMH for most providers, making TMH less of a choice and more of a requirement to continue practicing (8). In a study conducted during the initial months of the pandemic, mental health providers practicing in the state of Florida believed they were still delivering high-quality care and communicating effectively with their patients despite the transition to TMH care (2). We are now years into the pandemic and it is unknown whether TMH providers remain satisfied with their capacity to conduct high-quality care. The purpose of this study is therefore to further explore perceptions of delivering high-quality healthcare remotely among a nationally representative United States sample of TMH providers.
High-quality healthcare is effective, safe, and equitable and delivered by a provider who clearly communicates and involves patients in health decisions (9). Therapeutic alliance–the relationship and tasks to achieve mutually established health goals–is reliably among the strongest predictors of mental health treatment success, making strategies and tactics for building a strong patient-provider relationship paramount to high-quality care (10–14). Consistent with high-quality care, therapeutic alliance thrives in patient-centered environments where providers elicit the “true” wishes of patients to recognize and respond to their needs and values (15). For in-person healthcare settings, patient-centered communication is commonly described as asking and welcoming questions to understand patients’ beliefs and needs to ensure that healthcare is concordant with their values (16). The capacity to practice patient-centered communication requires providers to practice cultural competencies, or multicultural counseling self-efficacy (17). Patient-centeredness is integral to the capacity of providers to recognize and become responsive to the diverse backgrounds of patients and integrate their values into clinical decision-making (18). In TMH settings, patient-centered communication occurs when providers help patients navigate the telemedicine platform, which includes facilitating an environment where they can access, evaluate, and discuss online resources as partners in care (i.e., eHealth literacy) (19). Therapeutic alliance, eHealth literacy, and multicultural competence in a patient-centered environment are vital for success in mental health care, but it is unclear how these indicators of high-quality care have fared throughout the pandemic.
Delivering high-quality TMH care is also attributed to organizational factors that facilitate or support providers in using telemedicine. A recent study found that having strong organizational capabilities, such as sufficient information technology infrastructure, is integral to successful telemedicine adoption in healthcare systems (20). However, healthcare providers must also feel supported in using telemedicine to practice their specialty with fidelity and to effectively provide care to their patients (21). This includes feeling confident that the overarching healthcare system is supportive of telemedicine utilization (e.g., timely reimbursement processes), as well as having enough training or resources available to help them most effectively practice their specialty remotely. Harst et al. (22) found that perceptions of organizational factors which impact telemedicine use has most often been explored among patients rather than providers. This is a significant gap in the literature that our study aims to address.
Telemental health providers’ perceptions about the quality of care they provide to patients remotely may vary according to when they adopted telemedicine and how frequently they use it. For example, Zhu et al. (1) found that TMH providers were more comfortable with telemedicine during the pandemic than before it began. Other than this finding, little empirical attention has been paid to examining how the temporal aspects of TMH uptake affect perceptions of TMH care delivery. The decision whether to use telemedicine largely depends on the healthcare provider, making them gatekeepers of telemedicine (23, 24). Therefore, it is imperative to understand how perceptions of TMH care vary according to when it was adopted and the frequency of its use.
The purpose of this study was to investigate TMH providers’ perceptions about TMH care delivery during the pandemic. Participants were surveyed about their perceptions of TMH satisfaction, benefits, therapeutic alliance, patient-centered communication, eHealth literacy, cultural competence, and organizational factors that facilitate TMH use. A secondary purpose of the study was to examine how perceptions of TMH care vary depending on when telemedicine was adopted (before or after the onset of COVID-19) and the proportion of caseload served remotely (<50% or ≥50%). Our investigation occurred in Spring 2021, approximately one year after global leaders announced the COVID-19 pandemic.
Materials and Methods
Sample and Procedures
Telemental health providers (N = 472) completed a cross-sectional, web-based survey between February and March 2021. Emails were sent to TMH providers who used the Doxy.me telemedicine platform, sampling from which has shown to be consistent with mental health industry demographics (1, 2, 7, 25, 26). After providing electronic informed consent, providers completed a series of screening questions. English-speaking adults (i.e., ≥ 18 years) who identified as practicing mental and/or behavioral health providers were eligible to participate. Providers were compensated with a free 1-month Doxy.me professional membership. Study procedures were approved by the Institutional Review Board of the University of South Florida (IRB#002053).
Survey and Measures
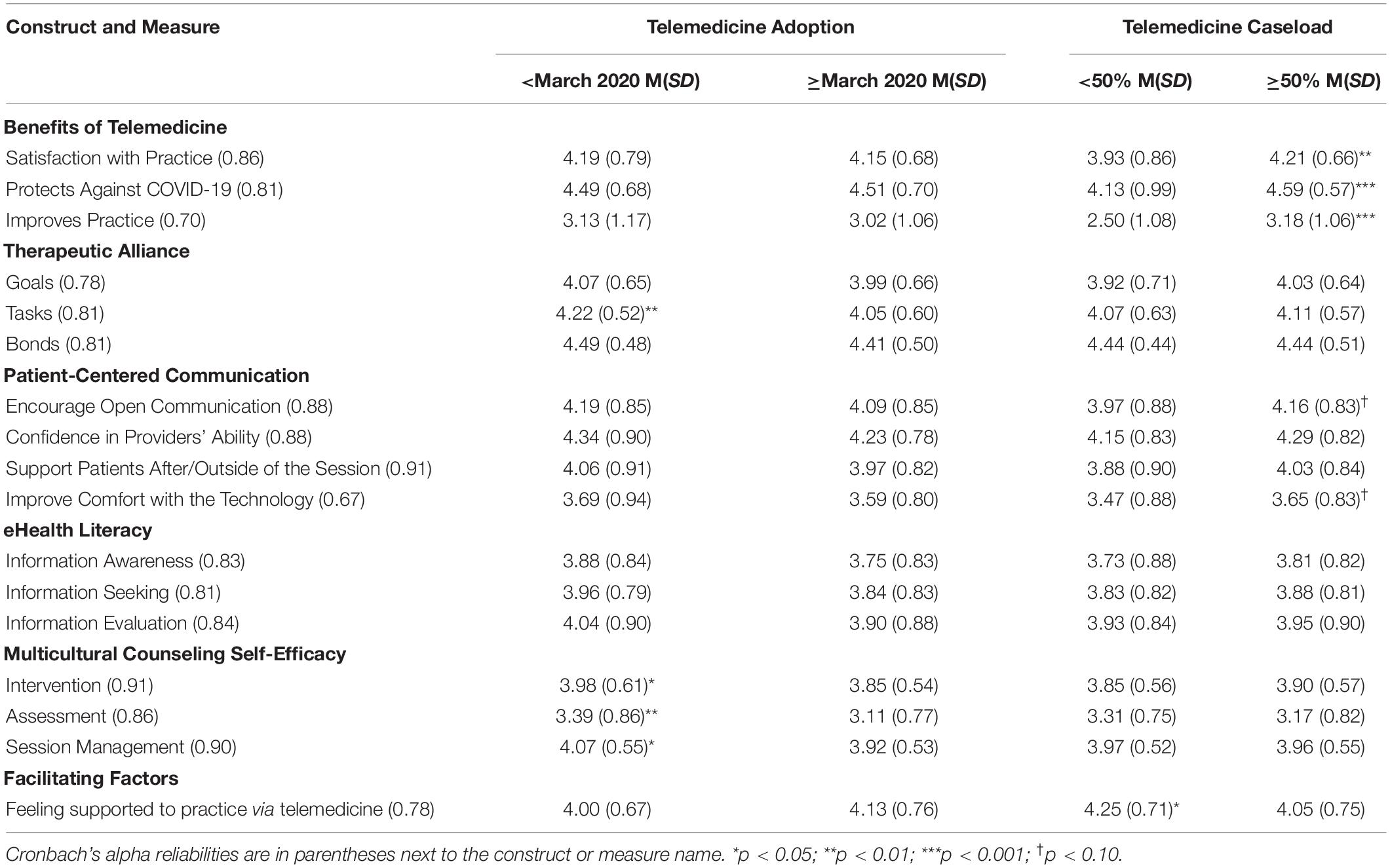
The survey was iteratively developed and refined based on prior studies exploring TMH practice (1, 2, 7). The survey included a variety of items selected from validated scales, questions adapted from validated scales, and novel questions related to TMH practice during COVID-19. See Table 1 for Cronbach’s alpha reliabilities for each measure.
Personal and Professional Characteristics of Telemental Health Providers
We collected demographic (e.g., age, gender, race, ethnicity, rurality) and professional characteristics (e.g., professional title, theoretical orientation, disorders treated, age group primarily treated, change in overhead costs).
Beliefs About the Satisfaction and Benefits of Telemedicine Experience
Perception of providers’ satisfaction with telemedicine experience was measured using several items reported in Slone et al. (2). These items were linearly rescaled to create a unidimensional satisfaction measure. Each item was anchored on a 5-point Likert scale from Extremely Dissatisfied to Extremely Satisfied. Benefits of telemedicine (general) was measured using 3 items anchored on a scale from 1 = Not at all to 5 = Extremely. Benefits of telemedicine specific to COVID-19 was similarly measured using 3 items anchored on a scale from 1 = Not at all to 5 = Extremely.
Therapeutic Alliance
Therapeutic alliance with patients via telemedicine was captured using the Working Alliance Inventory - Short Revised – Therapist version (WAI-SR-T) (27). This measure consists of three subscales: goals, tasks, and bonds. Responses ranged from 1 = Seldom to 5 = Always.
Patient-Centered Communication
Patient-centered communication via telemedicine was measured with an 11-item instrument. Based on best practices in patient-centered communication (28, 29), we identified four subscales: encourage expression, increase confidence in ability, support patients outside the session, and help patients overcome technology issues. Responses ranged from 1 = Very difficult to 5 = Very easy.
Electronic Health Literacy
Electronic health (eHealth) literacy was measured based off items from the eHealth Literacy Scale (eHEALS) (30) adapted to fit the therapist perspective. For example, “I know what health resources are available on the internet” was rephrased as “I know what health resources are available on the Internet for my clients.” We identified three subscales adapted from a prior eHEALS 3-factor model study (31): information awareness, information seeking, and information evaluation. Responses were anchored on a 5-point Likert scale from 1 = Strongly disagree to 5 = Strongly agree.
Multicultural Counseling Self-Efficacy
Multicultural counseling competence was measured with the Multicultural Counseling Self-Efficacy Scale – Racial Diversity Form (MCSE-RD) (17). The measure focuses on MH providers’ confidence in multicultural counseling skills with racially diverse clients, a central aspect of multicultural competence. We measured three subscales: multicultural intervention, multicultural assessment, and multicultural counseling session management. The 60 items in the MCSE-RD were reduced to 22 by consulting two clinical content experts. Criteria for inclusion included eliminating redundancies in scale items and item relevance to TMH practice. Each subscale displayed adequate internal reliability. Responses were anchored on a 5-point Likert scale from 1 = No confidence at all to 5 = Complete confidence.
Facilitating Factors
Finally, we measured the degree that providers receive organizational support to use telemedicine (e.g., training, resources) using a 4-item measure with response ranging from 1 = Strongly disagree to 5 = Strongly agree.
Data Analysis
SPSS v28 (IBM Corp.) was used for all analyses. Descriptive and frequency statistics were computed to describe the sample and responses to survey items. A series of χ2 tests were conducted to examine how demographic factors varied according to our two independent variables (IVs), which included when providers began using telemedicine (0 = before March 2020; 1 = March 2020 or later) and how much of their caseload was served remotely (0 ≤ 50%; 1 ≥ 50%). A series of independent samples t-tests were also conducted to examine how perceptions of care quality varied by both IVs. Statistical significance was set at p < 0.05.
Results
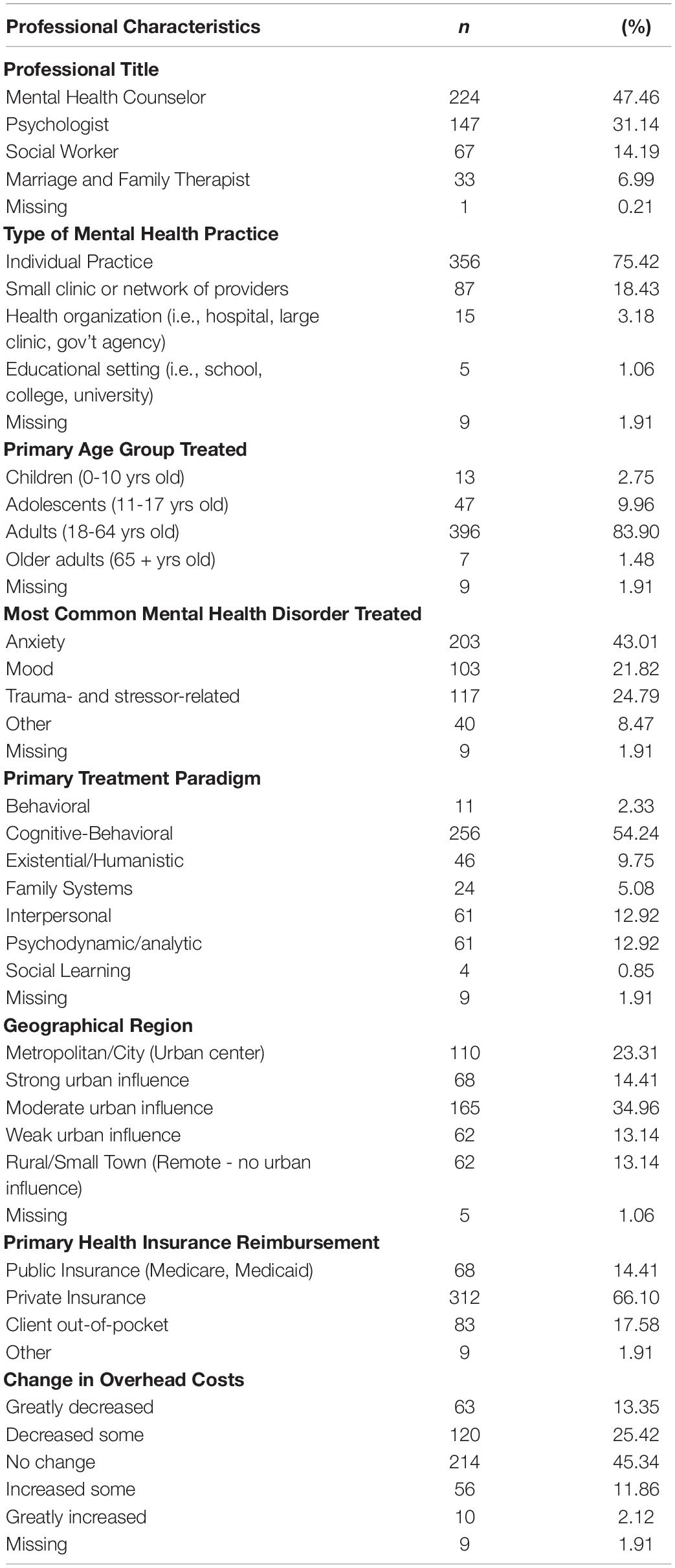
Table 2 shows that TMH providers in this study were, on average, 53.19 years old (SD = 13.16) and predominantly female (81.36%), white (80.51%), and non-Hispanic (91.10%). Most (72.68%) providers lived in a Metropolitan area, with either a moderate or strong urban influence.
Table 3 shows the professional characteristics of the providers. Most identified as mental health counselors (47.46%), psychologists (31.14%), and social workers (14.19%). Nearly three-quarters of providers (75.42%) reported working in an individual practice and 18.43% in a network of providers or a small clinic. Over half of providers primarily treated anxiety and mood related disorders (i.e., anxiety, 43.01%; mood, 21.82%; trauma- and stressor-related disorders, 24.79%), followed the cognitive-behavioral treatment paradigm (54.24%), and served adults (18-64 years old; 83.90%). Private health insurance was the most common form of reimbursement for telemedicine services. About half (45.34%) of providers said their overhead costs (including rent, supplies) had not changed because of providing telehealth services. Over half (67.58%) of providers (n = 319) started using telemedicine March 2020 or later, and 79.66% (n = 376) reported seeing at least 50% of their patients via telemedicine. There was no statistically significant association between percent of caseload served via telemedicine and whether telemedicine was adopted before or during the pandemic (p = 0.20).
Personal and Professional Characteristics of Telemental Health Providers
Most providers who used telemedicine, regardless of onset, were women; however, the proportion of women who used telemedicine was significantly greater during the COVID-19 pandemic (85.48%) than before it (77.46%), χ2 (1, N = 459) = 4.48, p < 0.05. No other statistically significant relations existed for personal demographics.
Providers who used telemedicine to treat the majority (50% or more) of their caseload were more likely to treat adults (18 + years old) rather than children and adolescents (0-17 years old), χ2 (1, N = 463) = 11.10, p < 0.05. There were no statistically significant differences in changes to overhead costs because of adopting telemedicine technology. However, providers who served less than 50% of their caseload reported that overhead costs “haven’t changed” (M = 2.91; SD = 0.60) whereas providers who served more than 50% of their caseload via telehealth reported that overhead costs have “decreased some” (M = 2.57; SD = 0.99), t (461) = 3.07, p < 0.01. This difference should be noted as having a moderate effect (Cohen’s d = 0.42). No other statistically significant relationships existed for professional characteristics and telemedicine use.
Beliefs About the Satisfaction and Benefits of Telemental Health Care
Table 1 includes the responses to general satisfaction of using telemedicine and the benefits (i.e., general to telemedicine and specific to protecting against COVID-19 transmission). Providers reported feeling somewhat satisfied with their TMH practice (M = 4.16; SD = 0.71). They believed that telemedicine services moderately benefitted their practice (M = 3.05; SD = 1.09) but that it had been very-to-extremely beneficial in protecting against the spread of COVID-19 while supporting continuity of care (M = 4.50; SD = 0.69). The timing of telemedicine adoption (before or after March 2020) was not associated with providers’ satisfaction using telemedicine or its perceived benefits. However, compared with their counterparts who served fewer patients remotely, providers who served 50% or more of their caseload remotely reported greater satisfaction with their telemedicine practice (M = 4.22 SD = 0.66 vs. M = 3.93 SD = 0.86), t (371) = −3.14; 95% CI = −0.47, −0.11; p < 0.01. Providers who served most of their caseload remotely also reported stronger beliefs about the benefits of telemedicine to support their practice (M = 3.18 SD = 1.06 vs. M = 2.50 SD = 1.08), t (421) = −5.50; 95% CI = −0.94, −0.42; p < 0.001). They were also more likely to report that telemedicine helped to alleviate the impacts of COVID-19 (M = 4.59 SD = 0.57 vs. M = 4.13 SD = 0.99), t (421) = −5.13; 95% CI = −0.62, −0.20; p < 0.001.
Therapeutic Alliance
Table 1 shows that providers reported very often agreeing with their patients on the therapeutic goals (M = 4.01; SD = 0.65) and tasks to achieve those goals (M = 4.10; SD = 0.58) via telemedicine. Providers also felt they very often-to-always established a meaningful bond with the patients they served remotely (M = 4.44; SD = 0.50). Compared with providers who started using telemedicine during the pandemic, providers who used telemedicine before the pandemic reported having a greater task-related alliance with their patients (M = 4.22 SD = 0.52 vs. M = 4.05 SD = 0.60), t (357) = 2.62; 95% CI = 0.04, 0.31; p < 0.01. There were no other statistically significant differences in therapeutic alliance sub-scores based on when providers began using telemedicine or the proportion of caseload served remotely.
Patient-Centered Communication
Table 1 also shows that providers generally felt that it was somewhat easy to encourage patients to openly communicate via telemedicine (M = 4.12; SD = 0.85), to increase patients’ confidence in their ability as a healthcare professional (M = 4.26; SD = 0.82), and to stay engaged with them outside the telemedicine session (M = 4.00; SD = 0.85). They reported it was “neither easy nor difficult” to help patients feel more comfortable using telemedicine (M = 3.62; SD = 0.84). There were no statistically significant differences in patient-centered communication based on when providers began using telemedicine or how much of their caseload is served remotely. However, two subscales approached statistical significance based on the percent of patients seen via telemedicine; providers who served more than 50% of their caseload remotely felt it was easier to encourage their patients to openly communicate (p = 0.06) and help them feel more comfortable to use telemedicine (p = 0.07).
eHealth Literacy
In Table 1, providers somewhat agreed that they were knowledgeable about where to find health information on the Internet to benefit their patients (M = 3.79; SD = 0.83), how to help their patients find health information on the Internet (M = 3.87; SD = 0.81), and how to help their patients evaluate the quality of health information they find on the Internet (M = 3.94; SD = 0.89). There were no statistically significant differences in online health information awareness, seeking, and evaluation skills according to when providers began using telemedicine and the percentage of caseload they served remotely.
Multicultural Counseling Self-Efficacy
Table 1 includes the responses to providers’ multicultural counseling self-efficacy. Providers reported some confidence in their ability to conduct multicultural assessment (M = 3.19; SD = 0.81) and some-to-a lot of confidence in their ability to conduct multicultural interventions (M = 3.89; SD = 0.56) and multicultural counseling session management (M = 3.96; SD = 0.54). Compared to providers who began using telemedicine March 2020 or later, providers who used telemedicine before the COVID-19 pandemic reported a statistically significant higher ability to conduct: (a) multicultural interventions (M = 3.98 SD = 0.61 vs. M = 3.85 SD = 0.54), t (344) = 2.00; 95% CI = 0.00, 0.26; p < 0.05, (b) multicultural assessments (M = 3.39 SD = 0.86 vs. M = 3.11 SD = 0.77), t (344) = 3.07; 95% CI = 0.10, 0.47; p < 0.01, and (c) multicultural counseling session management (M = 4.07 SD = 0.55 vs. M = 3.92 SD = 0.53), t (344) = 2.35; 95% CI = 0.02, 0.27; p < 0.05. There was no statistically significant difference in multicultural counseling self-efficacy based on the percentage of their caseload served remotely.
Facilitating Factors
Table 1 shows that providers somewhat agreed they were adequately trained and supported to provide services via telemedicine (M = 4.11; SD = 0.74). This perception was stronger among providers who began using telemedicine before rather than during the COVID-19 pandemic (M = 4.25 SD = 0.71 vs. M = 4.05 SD = 0.75), t (409) = 2.54; 95% CI = 0.05, 0.36; p < 0.05. Perceptions about facilitating factors did not vary according to percentage of patients served remotely.
Discussion
The current study aimed to investigate TMH providers’ perceptions about remote healthcare delivery one year into the pandemic. A secondary aim was to examine the variability in these perceptions according to when TMH providers adopted telemedicine (i.e., before or during the pandemic) and how much of their caseload was served remotely (i.e., less than 50%; 50% or more). Approximately 80% of providers in this study, regardless of whether they adopted telemedicine before or during the pandemic, reported treating at least half of their patient caseload via telemedicine. Findings demonstrate heterogeneity in TMH providers’ perceptions of delivering care via telemedicine.
Principal Results
Telemental health providers generally reported being satisfied with using telemedicine to deliver care one year into the COVID-19 pandemic. Providers believed that telemedicine was beneficial to their practice and to the safety of themselves and their patients during the COVID-19 pandemic. Positive beliefs were consistent among providers who adopted telemedicine before or during pandemic. However, they were strongest among providers who used telemedicine to treat 50% or more of their caseload. In previous research, TMH providers have cited telemedicine as a convenient and considerably low-cost approach to reach patients who otherwise would not have access to care (7). Although TMH providers were generally satisfied with their telemedicine experience, positive beliefs about using telemedicine to deliver care were cultivated when the technology was regularly integrated into their practice.
TMH providers generally felt confident in their ability to establish a therapeutic alliance with their patients. This is a positive finding, as a therapeutic alliance is an integral component of effective mental health care (14). TMH providers reported establishing treatment goals with their patients, despite the challenges of cultivating task-related alliances. Specifically, TMH providers who began using telemedicine during the pandemic reported the weakest task-oriented alliances with their patients. There are several barriers that may impede the ability of providers to achieve mutual understanding and agreement on exercises to help their patients achieve treatment goals. Some examples include poor internet connection, challenges using devices and software, limited knowledge about how to engage patients remotely, and believing that patients are unreceptive to telemedicine (32). In a study conducted prior to the pandemic (26), TMH providers commonly assigned patients exercises that involved coping and emotional regulation, problem solving, mindfulness, interpersonal skills, and modifying and addressing core beliefs. Future research is needed to examine if and how these exercises are conducted by mental health providers who began using telemedicine during the pandemic. Such inquiry would be useful to inform instructional efforts to help providers new to telemedicine to succeed in cultivating therapeutic alliances.
The strongest therapeutic alliances are cultivated within patient-centered environments, meaning that care is discussed and coordinated with the patients’ needs, preferences, and values in mind (18). Telemedicine can challenge the patient-centeredness and therapeutic alliances of healthcare appointments, as self-expression and relational connections among other considerations may manifest differently than in-person appointments (33, 34). As a result, telemedicine has a reputation for being provider-centered, as observational analyses of clinical encounters have found that providers exhibit verbal and information dominance (35, 36). And although there is enthusiasm for telemedicine as a patient-centered healthcare delivery solution (37), a study conducted in the early phases of the pandemic found that disparities in patient-centered communication exist via telemedicine (e.g., limited opportunities for open-ended communication and poorly expressed empathy) (38). Future research is needed to capture both patient and provider assessments of therapeutic alliance following telehealth appointments.
There are two important findings related to patient-centered care and communication in this study. First, TMH providers believed it was somewhat easy to encourage their patients to openly communicate about their feelings, values, and needs via telemedicine. This positive perception about facilitating open communication was consistent regardless of when providers began using telemedicine and how frequently it is used to serve their caseload. Second, providers also felt it was somewhat easy to help patients feel confident in their abilities as a remote healthcare professional. Patients are more likely to ask for providers to repeat information via telemedicine than in-person consultations (35). As a result, providers may perceive patients’ expressions of perceptual difficulty as engagement, giving them greater opportunity to exhibit their knowledge about subject matter. Future research examining remote patient-centered communication and investigating its effect on how care is delivered by providers and received by patients is a fruitful area.
Another aspect of patient-centered communication is helping patients feel comfortable receiving and navigating health care. In this study, TMH providers in this study felt it was neither easy nor difficult to help their patients feel comfortable receiving care via telemedicine. Further, they felt somewhat knowledgeable about where to find online health information and how to help their patients evaluate its quality to support their health-related goals. Nearly 60% of healthcare providers have shared and recommended online health information to their patients (39), and this proportion is expected to be higher now that the internet has penetrated the daily lives of most people worldwide. Future research is needed to explore what online health information is discussed during telemedicine appointments. Understanding what content is introduced during these appointments and exploring the process by which the information is shared and navigated will inform future interventions to support providers in this endeavor.
To appropriately establish patient-centered care and cultivate therapeutic alliance among racially/ethnically diverse patients, TMH providers must be capable of providing culturally sensitive treatments. TMH providers reported some confidence in their ability to apply multicultural competencies in mental health assessment, intervention, and session management. Multicultural counseling self-efficacy was strongest among providers who reported using telemedicine before the pandemic. This difference may be due to differences in the amount of experience using telemedicine to deliver culturally sensitive care, or perhaps the availability of cultural competence training. Despite a great deal of heterogeneity in workforce cultural competence trainings, common strategies include increasing providers’ knowledge and skills to facilitate culturally competent care (40). Future research might focus on patients demographics and include observational studies of multicultural counseling competencies in practice via telemedicine. Overall, findings of this study echo the need for training to support TMH providers in serving culturally diverse patient caseloads, especially those residing in medically underserved communities who are disproportionately at-risk for mental health concerns (31).
Although not specific to cultural competence, TMH providers reported being trained and feeling supported by their professional organization in using telemedicine to practice their specialty. Providers who felt supported in using telemedicine were more likely to have started using telemedicine before the pandemic rather than during it. Weaker perceptions of support among novice telemedicine users may be due to the abrupt, and sometimes mandated shifts from in-person to remote care in March 2020. Harst et al. (22) report that positive attitudes toward telemedicine and its acceptability (e.g., perceived usefulness and ease-of-use) are some of the most important predictors for its personal decision to adopt the technology. However, social policies and organizational infrastructure are also important predictors of telemedicine acceptance, and they are also crucial in considering the long-term adoption and sustainability of telemedicine. In this study, we operationalized facilitating factors as providers’ beliefs about whether they are supported to use telemedicine and adequately trained and provided resources to practice their specialty remotely. Future research is needed to explore the interpersonal, organizational, and policy-oriented factors that facilitate mental health providers’ telemedicine use. Several social and organizational factors have been found to affect providers’ adoption of mobile health solutions in their practice (e.g., workflow, patient, policy/regulation, social influence, monetary factors, evidence-base, awareness, and user engagement) (41). Similar research conducted among TMH providers will begin to inform policy and future procedural practices of telemedicine.
Limitations
This study was cross-sectional, and it is limited to a single time-point during the COVID-19 pandemic. Surveillance efforts are needed to monitor TMH providers’ perceptions about their delivery of care throughout the remainder of the pandemic and after its resolution. Participant recruitment was limited to users of the Doxy.me telemedicine platform, which may not be representative of all TMH providers or practices. However, participant demographics collected in this study are consistent with those reported in mental health industry statistics (1, 2, 7, 24, 25). Meta-analyses and systematic reviews will be vital to aggregate findings across participant samples and studies. Lastly, these survey data are the product of self-report. Studies in the direct observation of TMH sessions and multicultural care practices will be necessary to understand how providers are adapting to remote care.
Conclusion
Telemental health providers have positive beliefs about telemedicine one year after the pandemic. They felt satisfied and adequately supported in using telemedicine to provide high-quality care to patients. Providers also reported being capable of supporting a remote, patient-centered environment conducive to openly discussing and evaluating online health resources, cultivating therapeutic alliances, and conducting multicultural competent counseling. However, heterogeneity exists in TMH providers’ perceptions of healthcare delivery according to when they adopted telemedicine in relation to COVID-19 and how much of their patient caseload is served remotely. Telemedicine is used now more than ever, and providers who hold positive beliefs about the technology are using it with most of their caseload. However, novice TMH providers may require additional training and support to successfully establish a working alliance with their patients, especially those who are multicultural.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of South Florida. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed equally to conceptualization, research, and manuscript preparation.
Funding
BB was funded by the National Institute of Mental Health (Grant Nos. K23MH118482 and R41MH126734) and BW was funded by the National Cancer Institute (Grant No. K07CA211786).
Conflict of Interest
BW is a shareholder, and all other authors are employees of Doxy.me Inc., a commercial telemedicine company.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, Coronavirus Disease 2019; eHEALS, eHealth Literacy Scale; IRB, Institutional Review Board; MCSE-RD, Multicultural Counseling Self-Efficacy Scale – Racial Diversity; MH, Mental Health; TMH, Telemental Health; US, United States; WAI-SR-T, Working Alliance Inventory - Short Revised – Therapist.
References
1. Zhu D, Paige SR, Slone H, Gutierrez A, Lutzky C, Hedriana H, et al. Exploring telemental health practice before, during, and after the COVID-19 pandemic. J Telemed Telecare. (2021). [Online ahead of print]. doi: 10.1177/1357633X211025943
2. Slone H, Gutierrez A, Lutzky C, Zhu D, Hedriana H, Barrera JF, et al. Assessing the impact of COVID-19 on mental health providers in the southeastern United States. Psychiatry Res. (2021) 302:114055. doi: 10.1016/j.psychres.2021.114055
3. Humer E, Pieh C, Kuska M, Barke A, Doering BK, Gossmann K, et al. Provision of psychotherapy during the COVID-19 pandemic among Czech, German and Slovak psychotherapists. Int J Environ Res Public Health. (2020) 17:4811. doi: 10.3390/ijerph17134811
4. Doran JM, Lawson JL. The impact of COVID-19 on provider perceptions of telemental health. Psychiatr Q. (2021) 92:1241–58. doi: 10.1007/s11126-021-09899-7
5. Sammons MT, VandenBos GR, Martin JN, Elchert DM. Psychological practice at six months of COVID-19: a follow-up to the first national survey of psychologists during the pandemic. J Health Serv Psychol. (2020). [Online ahead of print]. doi: 10.1007/s42843-020-00024-z
6. Douglas MD, Xu J, Heggs A, Wrenn G, Mack DH, Rust G. Assessing telemedicine utilization by using medicaid claims data. Psychiatr Serv. (2017) 68:173–8. doi: 10.1176/appi.ps.201500518
7. Bunnell BE, Barrera JF, Paige SR, Turner D, Welch BM. Acceptability of telemedicine features to promote its uptake in practice: a survey of community telemental health providers. Int J Environ Res Public Health. (2020) 17:8525. doi: 10.3390/ijerph17228525
8. Payne L, Flannery H, Kambakara Gedara C, Daniilidi X, Hitchcock M, Lambert D, et al. Business as usual? Psychological support at a distance. Clin Child Psychol Psychiatry. (2020) 25:672–86. doi: 10.1177/1359104520937378
9. Six Domains of Health Care Quality.Six Domains of Health Care Quality. (2018) Available online at: https://www.ahrq.gov/talkingquality/measures/six-domains.html (Accessed December 15, 2021)
10. Cameron SK, Rodgers J, Dagnan D. The relationship between the therapeutic alliance and clinical outcomes in cognitive behaviour therapy for adults with depression: a meta-analytic review. Clin Psychol Psychother. (2018) 25:446–56. doi: 10.1002/cpp.2180
11. Lopez A, Schwenk S, Schneck CD, Griffin RJ, Mishkind MC. Technology-Based Mental Health Treatment and the Impact on the Therapeutic Alliance. Curr Psychiatry Rep. (2019) 21:76. doi: 10.1007/s11920-019-1055-7
12. Kaiser J, Hanschmidt F, Kersting A. The association between therapeutic alliance and outcome in internet-based psychological interventions: a meta-analysis. Comput Human Behav. (2021) 114:106512. doi: 10.1016/j.chb.2020.106512
13. Glass VQ, Bickler A. Cultivating the therapeutic alliance in a telemental health setting. Contemp Fam Ther. (2021) 43:189–98. doi: 10.1007/s10591-021-09570-0
14. Bolsinger J, Jaeger M, Hoff P, Theodoridou A. Challenges and opportunities in building and maintaining a good therapeutic relationship in acute psychiatric settings: a narrative review. Front Psychiatry. (2019) 10:965. doi: 10.3389/fpsyt.2019.00965
15. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. (2011) 9:100–3. doi: 10.1370/afm.1239
16. Levinson W. Patient-centred communication: a sophisticated procedure. BMJ Qual Saf. (2011) 20:823–5. doi: 10.1136/bmjqs-2011-000323
17. Sheu H-B, Lent RW. Development and initial validation of the Multicultural Counseling Self-Efficacy Scale–Racial Diversity Form. Psychotherapy. (2007) 44:30–45. doi: 10.1037/0033-3204.44.1.30
18. Stubbe DE. Practicing cultural competence and cultural humility in the care of diverse patients. Focus. (2020) 18:49–51. doi: 10.1176/appi.focus.20190041
19. Norman CD, Skinner HA. eHealth Literacy: essential Skills for Consumer Health in a Networked World. J Med Internet Res. (2006) 8:e9. doi: 10.2196/jmir.8.2.e9
20. Chen C-H, Lan Y-L, Yang W-P, Hsu F-M, Lin C-L, Chen H-C. Exploring the impact of a telehealth care system on organizational capabilities and organizational performance from a resource-based perspective. Int J Environ Res Public Health. (2019) 16:3988. doi: 10.3390/ijerph16203988
21. Kichloo A, Albosta M, Dettloff K, Wani F, El-Amir Z, Singh J, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. (2020) 8:e000530. doi: 10.1136/fmch-2020-000530
22. Harst L, Lantzsch H, Scheibe M. Theories predicting end-user acceptance of telemedicine use: systematic review. J Med Internet Res. (2019) 21:e13117. doi: 10.2196/13117
23. Cowan KE, McKean AJ, Gentry MT, Hilty DM. Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. (2019) 94:2510–23. doi: 10.1016/j.mayocp.2019.04.018
24. Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clin Psychol. (2020) 27:e12311. doi: 10.1111/cpsp.12311
25. American Psychological Association [APA]. Demographics of the U.S. Psychology Workforce: Findings from the 2007-16 American Community Survey. Washington, DC: American Psychological Association (2018).
26. Bunnell BE, Kazantzis N, Paige SR, Barrera J, Thakkar RN, Turner D, et al. Provision of care by “Real World” telemental health providers. Front Psychol. (2021) 12:653652. doi: 10.3389/fpsyg.2021.653652
27. Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychother Res. (2006) 16:12–25. doi: 10.1080/10503300500352500
28. Bylund CL, Banerjee SC, Bialer PA, Manna R, Levin TT, Parker PA, et al. A rigorous evaluation of an institutionally-based communication skills program for post-graduate oncology trainees. Patient Educ Couns. (2018) 101:1924–33. doi: 10.1016/j.pec.2018.05.026
30. Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e27. doi: 10.2196/jmir.8.4.e27
31. Paige SR, Miller MD, Krieger JL, Stellefson M, Cheong J. Electronic health literacy across the lifespan: measurement invariance study. J Med Internet Res. (2018) 20:e10434. doi: 10.2196/10434
32. Substance Abuse and Mental Health Services Administration.Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration. (2021).
33. Tremain H, McEnery C, Fletcher K, Murray G. The therapeutic alliance in digital mental health interventions for serious mental illnesses: narrative review. JMIR Ment Health. (2020) 7:e17204. doi: 10.2196/17204
34. Simpson S, Richardson L, Pietrabissa G, Castelnuovo G, Reid C. Videotherapy and therapeutic alliance in the age of COVID-19. Clin Psychol Psychother. (2021) 28:409–21. doi: 10.1002/cpp.2521
35. Agha Z, Roter DL, Schapira RM. An evaluation of patient-physician communication style during telemedicine consultations. J Med Internet Res. (2009) 11:e36. doi: 10.2196/jmir.1193
36. Street RL, Wheeler EJ, McCaughan WT. Specialist–primary care provider–patient communication in telemedical consultations. Telemed J. (2000) 6:45–54. doi: 10.1089/107830200311842
37. Alkureishi MA, Lenti G, Choo Z-Y, Castaneda J, Weyer G, Oyler J, et al. Teaching telemedicine: the next frontier for medical educators. JMIR Med Educ. (2021) 7:e29099. doi: 10.2196/29099
38. Paige SR, Bunnell BE, Bylund CL. Disparities in patient-centered communication via telemedicine. Telemed J E Health. (2021) 28:212–8. doi: 10.1089/tmj.2021.0001
39. Podichetty VK, Booher J, Whitfield M, Biscup RS. Assessment of internet use and effects among healthcare professionals: a cross sectional survey. Postgrad Med J. (2006) 82:274–9. doi: 10.1136/pgmj.2005.040675
40. Jongen C, McCalman J, Bainbridge R. Health workforce cultural competency interventions: a systematic scoping review. BMC Health Serv Res. (2018) 18:232. doi: 10.1186/s12913-018-3001-5
Keywords: telemedicine, telemental health, mental health, quality of care, COVID-19
Citation: Wilczewski H, Paige SR, Ong T, Barrera JF, Soni H, Welch BM and Bunnell BE (2022) Perceptions of Telemental Health Care Delivery During COVID-19: A Cross-Sectional Study With Providers, February-March 2021. Front. Psychiatry 13:855138. doi: 10.3389/fpsyt.2022.855138
Received: 14 January 2022; Accepted: 09 March 2022;
Published: 04 April 2022.
Edited by:
Xenia Gonda, Semmelweis University, HungaryReviewed by:
Carly McCord, Texas A&M University, United StatesCharles Doarn, University of Cincinnati, United States
Copyright © 2022 Wilczewski, Paige, Ong, Barrera, Soni, Welch and Bunnell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hattie Wilczewski, aGF0dGllLndpbGN6ZXdza2lAZG94eS5tZQ==
 Hattie Wilczewski
Hattie Wilczewski Samantha R. Paige1
Samantha R. Paige1 Triton Ong
Triton Ong Janelle F. Barrera
Janelle F. Barrera Hiral Soni
Hiral Soni Brian E. Bunnell
Brian E. Bunnell