
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 21 September 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.855016
This article is part of the Research TopicNoncommunicable Diseases and Mental Health Experiences Before and After the COVID-19 PandemicView all 14 articles
Background: The COVID-19 outbreak became a continuing global health agenda. It has a significant impact on individuals’ quality of life (QOL). Patients with preexisting medical conditions may have severely reduced QOL. The aim of this study was to assess QOL and its associated factors among patients with chronic non-communicable diseases (NCDs) during COVID-19 pandemic at Sidama Regional State, southern Ethiopia.
Methods: We conducted a multicenter, cross-sectional study from 1 June to 1 September 2021. A total of 633 participants took part in the study, using an interviewer-administered structured questionnaire. The QOL was measured using the World Health Organization Quality of Life (WHOQOL-BREF) Scale, which has 12 items. To describe different variables, descriptive statistics were employed. To find independent factors associated with QOL, we used multivariable linear regression analysis. P-value of < 0.05 was declared statistically significant at 95% confidence interval (CI).
Results: The majority (56.4%) of participants were male and about half (53.1%) had a diagnosis of diabetes mellitus. The multivariable linear regression model showed statistically significant negative association between different independent variables such as age (β = −0.188, 95% CI = −0.238 to −0.139), being female (β = −1.942, 95% CI = −3.237 to −0.647), duration of illness ≤ 5 years (β = −4.222, 95% CI = −6.358 to −2.087), alcohol use in the past 3 months (β = −4.574, 95% CI = −6.905 to −2.243), common mental disorder (CMD) (β = −1.512, 95% CI = −2.924 to −0.100), insomnia (β = −0.274, 95% CI = −0.380 to −0.168), and QOL. Also, there is a statistically significant positive association between QOL and being illiterate (β = 3.919, 95% CI = 1.998–5.841) and living in the rural area (β = 2.616, 95% CI = 1.242–3.990).
Conclusion: In general, the findings confirmed that the COVID-19 pandemic had a negative impact on patients with chronic NCDs QOL. The QOL was significantly influenced by age, gender, educational status, residence area, duration of illness, alcohol use, CMD, and insomnia during COVID-19 pandemic. Thus, this study suggests that addressing insomnia, co-morbidities of mental disorders, and alcohol use has the potential effect to improve the QOL of patients with chronic medical illnesses.
The coronavirus disease (COVID-19) pandemic, which began in China in December 2019, is still posing a global health risk (1). Over 304 million confirmed cases and 5.4 million deaths had been reported globally in the 2 years since its emergence, as of the first week of January 2022 (2). As of 2 January 2022, there were over 400 thousand COVID-19 confirmed cases in Ethiopia, and the virus was responsible for about 7,000 fatalities. Risk communication and awareness campaigns are being used to address worries about the alarming rise in COVID-19 cases and the widespread dissemination of flu-like symptoms among Ethiopians. Additionally, the COVID-19 vaccine has been given in doses totaling close to 11 million up to January 2022 (3).
The severity and mortality of COVID-19 infections are thought to be increased in patients with preexisting medical conditions like diabetes mellitus (DM), hypertension, and malignancies (4). The case-fatality ratio was higher in patients with cardiovascular diseases (10.5%), diabetes (7.3%), and hypertension (6%) compared to the general population (2.3%) (5). Aside from physical health, COVID-19 has had a negative impact on mental health, causing significant anxiety and depression in people (6), and interfering with daily lives, jobs, and relationships. People are afraid of infection, dying, and losing family members during the COVID-19 outbreak. At the same time, many people have lost or are in danger of losing their jobs, have become socially isolated and separated from loved ones, and have seen stay-at-home orders implemented in some countries in drastic ways (7).
As a result, whether infected or not, COVID-19 has had a significant impact on people’s quality of life (QOL) (8, 9). The COVID-19 outbreak is regarded as an unforeseen traumatic life event that has harmed individuals’ QOL in general and particularly their health-related quality of life (HRQOL). HRQOL is a multidimensional concept that describes how an individual assesses his or her mental, physical, emotional, and social wellbeing (10). Many studies have been conducted to investigate the QOL of recovered COVID-19 cases in the general population, hospitalized patients, and chronic illness patients (9, 11–13).
The COVID-19 pandemic has a significant negative impact on QOL, especially in terms of physical, mental, social, and spiritual wellbeing (9, 14–17). A recent study in Bangladesh found a link between chronic diseases such as hypertension (HTN), diabetes mellitus (DM), heart disease, asthma, kidney diseases, and cancer and significantly lower QOL in all domains (18). According to a recent Egyptian study, 64% and 62% of diabetic patients reported poor physical and mental QOL, respectively. (19). In a similar study conducted in the Netherlands, 43% of patients with chronic kidney disease reported that the COVID19 pandemic had reduced their QOL (20).
People with non-communicable chronic diseases (NCDs) found it challenging to see a doctor and have their prescriptions filled (21) during the COVID-19 pandemic. During the peak of the COVID-19 pandemic, movement restrictions and social isolation became the new normal, contributing to a substantial reduction in people’ activities, which is associated with a significant decline in overall QOL (22). As a result, it is essential to look into how the COVID-19 pandemic affected the QOL of individuals living with chronic NCDs.
The unbearable impact of the COVID-19 pandemic may have had a significant impact on the QOL of patients with chronic medical conditions. To the best of our knowledge, data on QOL assessment among chronic disease patients in response to the COVID-19 pandemic are scarce, particularly in low-income countries like Ethiopia. Furthermore, there is a scarcity of data on the relationship between COVID-19-related psychological complications (such as depression, anxiety, and stress) and QOL among chronic disease patients during the COVID-19 pandemic. Therefore, this study fills a research gap by (1) describing QOL among patients with chronic medical conditions and (2) identifying the association between various socio-demographic, clinical, and psychological factors and QOL to identify significant predictors of QOL among patients with chronic medical conditions during the era of COVID-19 pandemic.
We conducted a cross-sectional study between 1 June and 1 September 2021 at four selected hospitals [Hawassa University Comprehensive Specialized Hospital (HUCSH), Adare General Hospital (AGH), Yirgalem General Hospital (YGH), and Leku Primary Hospital (LPH)] in Sidama National Regional State, southern Ethiopia.
This study was conducted among patients with chronic non-communicable diseases such as diabetes mellitus, hypertension, chronic cardiovascular diseases, and respiratory diseases (e.g., asthma) that have regular follow-up visits. Patients receiving follow-up care in the outpatient departments of the four hospitals were consecutively requested to participate in the study, if they met the following criteria: (I) age ≥18 years with chronic NCDs confirmed by physicians; (II) clinically stable and able to understand the purpose of the study; and (III) patients without any known psychiatric and neurocognitive disorders. However, patients with chronic NCDs who were admitted to the emergency/inpatient department for any reason were excluded from the study. We were planning to include 650 patients with chronic NCDs from the four hospitals based on the monthly patient flow (250 from HUCSH, 150 from AGH, 125 from YGH, and 125 from LPH). We used a consecutive sampling technique, and patients with chronic NCDs who visited hospitals during the study period and met the inclusion criteria were included in the study until the final study sample size was reached.
A structured self-administered questionnaire was used to gather data. The questionnaire is divided into various sections, such as the socio-demographic and clinical characteristics of the patient, the Oslo Social Support Scale (OSSS), the Self-Reporting Questionnaire-20 (SRQ-20) to evaluate common mental disorders (CMD), the Insomnia Severity Index (ISI) to evaluate insomnia, and the World Health Organization Quality of Life Instruments (WHOQOL-BREF) to evaluate QOL. The questionnaire was prepared in English and translated to the local language Amharic. The Amharic version of the questionnaire was used to collect the data.
The level of social support among patients with chronic NCDs was assessed using the 3-item Oslo Social Support Scale (OSSS), and the scores range from 3 to 14. It is categorized as poor [3–8], moderate [9–11], and strong [12–14] social support (23).
A 20-item (SRQ-20) WHO screening tool was used to assess CMDs (24). Only binary (yes/no) questions are included, with “1” indicating the presence of a symptom and “0” indicating the absence of a symptom. The SRQ-20 item questions cover depression, anxiety, and psychosomatic complaints, which are all classified as CMD (25). The SRQ-20′s validity, reliability, and cutoff score vary by population (culture, language, setting, and gender) in different settings (25–28). With a sensitivity of 78.6% and specificity of 81.5%, the SRQ-20 had good internal reliability (α = 0.78) and an optimal cutoff score of 5/6 (29). The SRQ-20 measure demonstrated good internal consistency (Cronbach’s α = 0.89) in our study.
The ISI is a 7-item self-assessment questionnaire that assesses the nature, severity, and impact of insomnia (30). The dimensions evaluated are severity of sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties in the last month. Each item is rated on a 5-point Likert scale (e.g., 0 = no problem; 4 = very severe problem), yielding a total score ranging from 0 to 28. The total score is divided into four categories, namely, no insomnia [0–7], sub-threshold insomnia [8–14], moderate insomnia [15–21], and severe insomnia [22–28]. A higher score indicates a severe insomnia (30–32). The ISI measure demonstrated very good internal consistency (Cronbach’s α = 0.96) in our study.
We used the adapted version of 12 items (9), from the WHOQOL-BREF Scale to assess the impact of the COVID-19 pandemic on QOL (33, 34). The adapted WHOQOL-BREF Scale had 12 items, each with a five-point rating from 1 = very low to 5 = very high; thus, the lowest possible score was 12, and the highest possible score was 60 for the total scale. Low scores indicate a lower QOL as a result of the COVID-19 pandemic’s negative effects. The QOL measure demonstrated good internal consistency in the previous study (Cronbach’s α = 0.81) (9). The WHOQOL-BRIEF 12 items (Supplementary File 1) used in our study demonstrated good internal consistency (Cronbach’s α = 0.82).
Collected data were entered to Epi-data version 3.1 and exported to SPSS (Statistical Package for Social Sciences) version 24 for analysis. Descriptive statistics such as frequency, percentage, mean, standard deviation, and median were used to describe different variables. Assumptions such as normality, lack of multi-collinearity among explanatory variables, presence of linearity relationship, independence, and homoscedasticity of the errors were checked. Simple and multivariable linear regressions were performed to identify independent predictors of QOL. P-values of < 0.05 were declared statistically significant at 95% confidence interval (CI).
This study included 633 participants. The majority of study participants (56.4%) were male, and 64.8% were married. About half (55.6%) were Protestant religious followers, followed by Orthodox Christians (25.9%), and about one-fourth (27.6%) were illiterate. More than one-fifth (22.7%) worked as a farmer, while 55.8% lived in urban. The mean age of the respondents was 46.49 ± 17.71 years as described in Table 1.
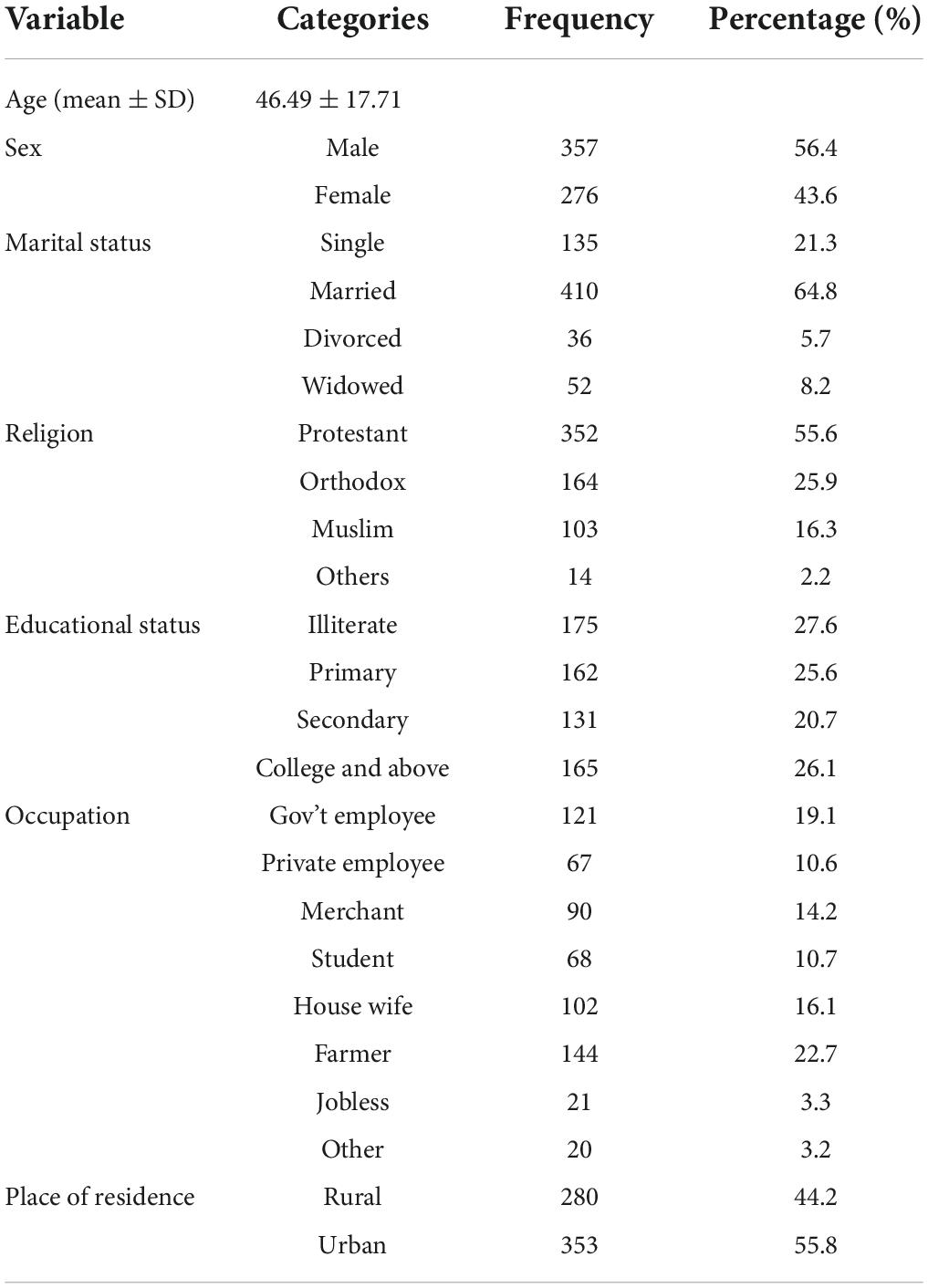
Table 1. Socio-demographic characteristics of study participants at Sidama National Regional State, southern Ethiopia, 2021 (n = 633).
About half of the participants (53.1%) had diabetes mellitus, followed by hypertension (17.5%), and nearly one-third (31.6%) had a comorbid diagnosis. The majority of participants (57.5%) had been sick for 5 years, and 9.6% and 7.7% had used alcohol and khat in the previous 3 months, respectively. More than one-third (35.4%) of all participants had poor social support, while about half (52.4%) had moderate social support. The mean SRQ-20 and ISI scores were 6.06 ± 5.09 and 6.62 ± 6.89, respectively (Table 2).
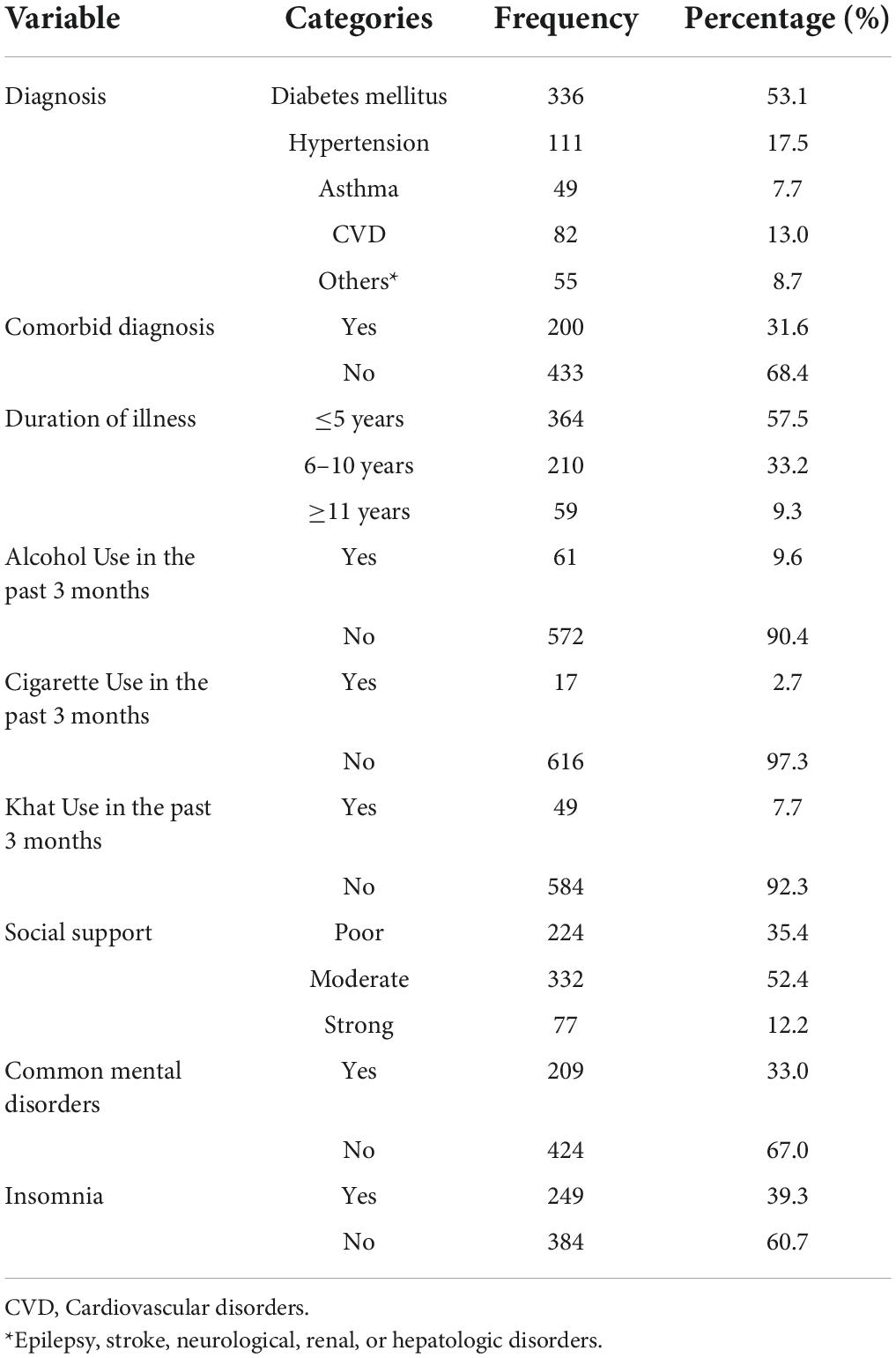
Table 2. Clinical characteristics of study participants at Sidama National Regional State, southern Ethiopia, 2021 (n = 633).
According to the WHOQOL-Brief (12-items) scale score, the mean QOL score of the participants was 33.07 ± 8.90 with a minimum score of 12 and a maximum score of 53.
Estimates of the multivariable linear regression model showed a statistically significant and negative association between different independent variables such as age (β = −0.188, 95% CI = −0.238 to −0.139), CMD (SRQ-20 scale) (β = −1.512, 95% CI = −2.924 to −0.100), insomnia (ISI scale) (β = −0.274, 95% CI = −0.380 to −0.168), being female (β = −1.942, 95% CI = −3.237 to −0.647), duration of illness ≤5 years (β = −4.222, 95% CI = −6.358 to −2.087), alcohol use in the past 3 months (β = −4.574, 95% CI = −6.905 to −2.243), and the outcome variable QOL during COVID-19 pandemic. On the contrary, there is a statistically significant and positive association between QOL and being illiterate (β = 3.919, 95% CI = 1.998–5.841) and living in the rural area (β = 2.616, 95% CI = 1.242–3.990) (see Table 3).
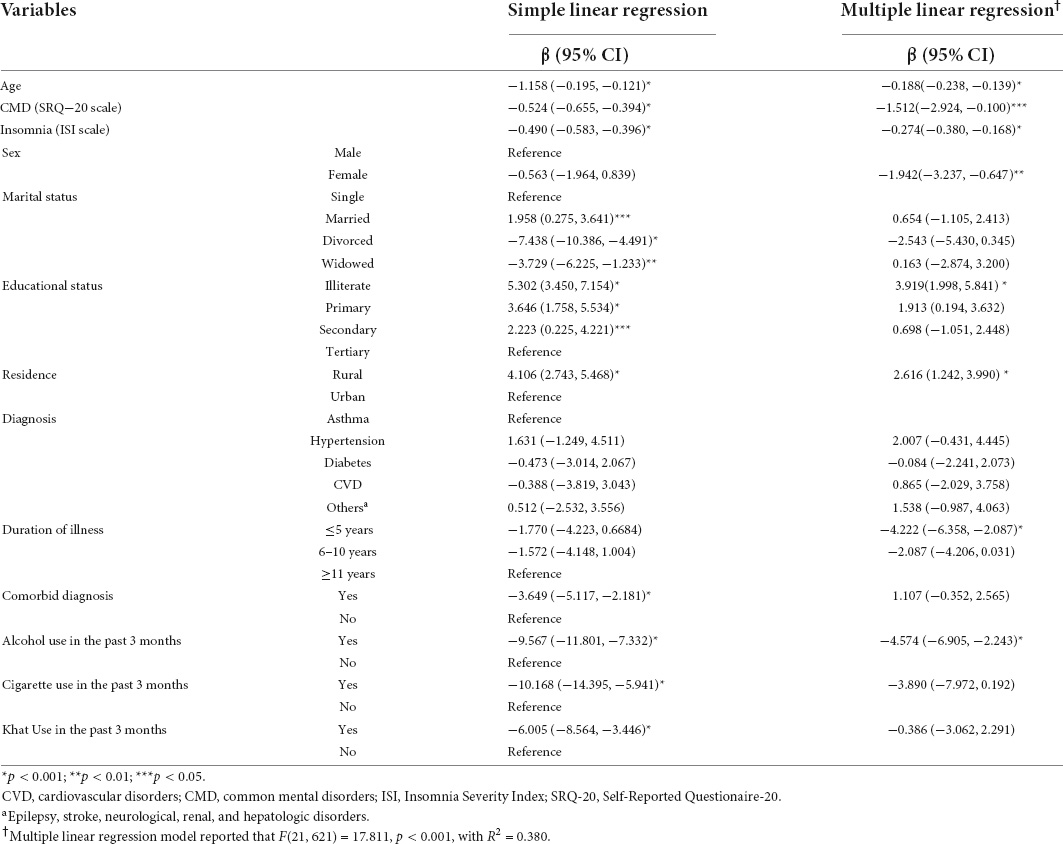
Table 3. Simple and multiple linear regression for quality of life among patients with chronic medical illness during COVID-19 pandemic at southern Ethiopia, 2021 (n = 633).
The global COVID-19 outbreak has wreaked havoc. Millions of lives were lost, and billions of people suffered psychologically and economically as a result. This study was used to assess the QOL of people who had chronic medical illnesses, as well as factors that were found to be significantly associated with QOL during the COVID-19 pandemic.
When the total WHOQOL-BRIEF score was compared to the sample socio-demographic characteristics, age was found to be a significant predictor, with QOL decreasing as age increased. This result was consistent with recent follow-up studies that found out older age was a risk factor for poor QOL (11, 35). This association can be explained by the fact that older age is associated with lower levels of overall health and physical function (12). QOL is projected to decline as people age, as they are more likely to suffer from many health problems (36). Another explanation could be that when people become older, the risk of COVID-19 infection increases severely (37). This suggests that during the COVID-19 pandemic, aging had a detrimental impact on QOL scores among chronic medical ill individuals.
In our study, the QOL scores of female patients were significantly lower than that of male patients, indicating that their QOL was significantly worse. Similar associations have been discovered in earlier studies, which supports our conclusion (12, 35). During the COVID-19 outbreak, women were shown to be more vulnerable to a variety of psychological problems (such as anxiety and depression) as compared to men (38, 39). Moreover, it is a known fact that females are more likely to have a lower income, more hurdles to healthcare access, and more domestic task obligations. All of these reasons may have contributed to the poor QOL in females.
We found out that educational status is significantly associated with QOL, i.e., lower educational attainment has better QOL scores. This is supported by a recent study, which found that QOL scores were shown to be lower in patients with a higher degree of education (8), due to a higher level of awareness and concern about COVID-19 and its negative effect on QOL. In addition, according to Nguyen et al. those with a high level of education had a higher prevalence of depression during the pandemic, resulting in a stress burden that adversely affects their health-related QOL (40). On the contrary, previous studies also found that, with higher levels of education, there was a general increment in QOL scores (18, 41). Higher educational attainment is often associated with greater career prospects and higher earnings, hence improving an individual’s QOL (41). However, uneducated participants claimed that their QOL was barely adequate in terms of thinking capacity, perceived physical safety and security, and vitality (41). Another rationale is that highly educated people may have a lot of wants and requirements in their daily lives, which may be jeopardized by the COVID-19 pandemic.
In our study, rural resident participants had higher QOL scores as compared to their counterparts. This is in line with previous study conducted by Hawlader et al. in Bangladesh (18). In urban areas, high population density and pollution levels may also have a negative impact on subjective QOL (42).
Duration of illness is another significant predictor of QOL in our study. Those patients with ≤5 years duration of illness have lower QOL score as compared to those with ≥11 years. This may be because of the fact that QOL can improve over time as patients adjust to chronic illness, symptoms stabilize, and more effective treatment alternatives become available over the course of long-term illness (43–45).
Our study showed that the QOL score was found to be lower among alcohol users when compared to non-alcohol users. Similar findings were reported in previous studies such that alcoholism is related to a reduced QOL (46, 47). Alcohol use has been shown to rise during stressful times such as pandemics (48). Alcohol consumption has a variety of intangible negative consequences, such as suffering, loss of healthy living, and deterioration of social and familial bonding, all of which contribute to a decrease in the individual’s QOL (49). In addition, alcohol is related to an increased risk of weakening the immune system, making people more susceptible to infectious disorders such as COVID-19 (50). Individuals use alcohol to cope with COVID-19′s stressful adaptive challenges (51). Some studies have revealed that those who drink have a much lower QOL, particularly in terms of their mental health and social functioning (52, 53).
Our study also showed that participants who had CMD had a higher probability of having lower QOL scores. The findings were consistent with a prior study, which found lower QOL scores in those who reported higher levels of anxiety, depression, and stress (9). Depression and anxiety have been linked to cognitive dysfunction (54), physical distress (55), and poor social functioning (56), all of which have been associated with a reduction in patients’ QOL. Previous studies well established that there is an inverse association between QOL and mental health problems such as depression and anxiety (57). As a result, it is not surprising that having more perceived CMDs lowers the QOL of patients with chronic medical illness, as found by this study.
This study found a statistically significant negative association between the insomnia severity index scale and the QOL scale. Similarly, recent studies indicated that impaired QOL was found to be independently associated with lower sleep quality and insomnia (58, 59). Insomnia’s impact on QOL could be due to physical or mental health comorbidities, medications, and/or a variety of psychosocial issues, or it could be a symptom of a primary disease. Furthermore, insomnia causes significant impairments in occupational and social functioning, as evidenced by decreased productivity of work, recurrent absenteeism, decreased cognition and mood, and increased physical and psychological morbidity (60). These directly or indirectly affects QOL of individuals.
This study has some limitations. First, we recognize that a cross-sectional study could not detect the continuing impact of the COVID-19 pandemic on different dimensions of QOL; thus, future research could be done using data based on a longitudinal design. Second, we did not use preferred tools to assess QOL such as SF-6D that was primarily designed to measure QOL in clinical populations. Third, because only participants from south Ethiopia were included in the study, the results cannot be applied to all Ethiopians who have chronic NCDs. These results need to be verified by additional research using a larger sample size and perhaps even a qualitative assessment. Additionally, the use of the non-probability consecutive sampling method could be viewed as a limitation. Fourth, there is a potential for social desirability bias. For instance, when data were collected using an interviewer-administered method, participants may have over- or underreported their responses for a variety of reasons.
In general, increase in age, higher SRQ-20 score (having CMD), increased ISI score (insomnia), being female, shorter duration of illness (<5 years), and alcohol use have a significant negative association with high QOL in patients with chronic medical condition during COVID-19 pandemic, whereas being illiterate and living in rural residence have a positive association with high QOL. Overall, the findings confirmed that the COVID-19 pandemic had a negative impact on an individual’s QOL in a variety of ways. Thus, this study suggests that addressing insomnia, co-morbidities of mental disorders, and alcohol use has the potential effect to improve the QOL of patients with chronic medical illnesses.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Hawassa University, College of Medicine and Health Sciences, Institutional Review Board (IRB) with reference number: IRB/076/13. The participants provided their written informed consent to participate in this study.
MA, BD, AG, and SH participated in the conception, designed the study, and were involved in the data collection. MA, BD, and SD performed the analysis of the study. MA and SD prepared the manuscript for publication. BD, AG, SH, and SD critically reviewed the manuscript. All authors read and approved the final manuscript.
Hawassa University was funding this research to be conducted.
We would like to thank Hawassa University for providing fund to conduct this study. Our heartfelt gratitude also to the data collectors and participants for their valuable contributions to the study process.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.855016/full#supplementary-material
1. Wang C. A novel coronavirus outbreak of global health concern. Lancet. (2020) 2020:470–3. doi: 10.1016/S0140-6736(20)30185-9
2. World Health Organization [WHO]. COVID-19 Weekly Epidemiological Update: Edition 74. Geneva: World Health Organization (2022). p. 1–23.
3. Ethiopian Public Health Institute [EPHI]. COVID-19 Pandemic Preparedness and Response in Ethiopia Weekly Bulletin. Addis Ababa: Ethiopian Public Health Institute (2022). p. 1–17.
4. Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. (2020) 323:1406–7. doi: 10.1001/jama.2020.2565
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
6. Arora T, Grey I, Östlundh L, Lam KBH, Omar OM, Arnone D. The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. J Health Psychol. (2020) 27:805–24. doi: 10.1177/1359105320966639
7. United Nations. Policy Brief: COVID-19 and the Need for Action on Mental Health. New York, NY: United Nations (2020).
8. Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect. (2020) 11:296–302. doi: 10.24171/j.phrp.2020.11.5.05
9. Algahtani FD, Hassan S, Alsaif B. Assessment of the quality of life during COVID-19 pandemic: a cross-sectional survey from the kingdom of Saudi Arabia. Int J Environ Res Public Health. (2021) 2021:847. doi: 10.3390/ijerph18030847
10. Hays RD. Measurement and modelling of health-related quality of life. In: Killewo J, Heggenhougen HK, Quah S editors. Epidemiology and Demography in Public Health. San Diego, CA: Academic Press (2008). p. 195–205.
11. Chen KY, Li T, Gong FH, Zhang JS, Li XK. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psychiatry. (2020) 11:668. doi: 10.3389/fpsyt.2020.00668
12. Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C, et al. Health-related quality of life of COVID-19 patients after discharge: a multicenter follow-up study. J Clin Nurs. (2021) 30:1742–50. doi: 10.1111/jocn.15733
13. Wu C, Cheng J, Zou J, Duan L, Campbell JE. Health-related quality of life of hospitalized COVID-19 survivors: an initial exploration in Nanning city, China. Soc Sci Med. (2021) 274:113748. doi: 10.1016/j.socscimed.2021.113748
14. Hay JW, Gong CL, Jiao X, Zawadzki NK, Zawadzki RS, Pickard AS, et al. A US population health survey on the impact of COVID-19 using the EQ-5D-5L. J Gen Intern Med. (2021) 36:1292–301. doi: 10.1007/s11606-021-06674-z
15. Epifanio MS, Andrei F, Mancini G, Agostini F, Piombo MA, Spicuzza V, et al. The impact of COVID-19 pandemic and lockdown measures on quality of life among Italian general population. J Clin Med. (2021) 10:289. doi: 10.3390/jcm10020289
16. Qi M, Li P, Moyle W, Weeks B, Jones C. Physical activity, health-related quality of life, and stress among the Chinese adult population during the COVID-19 pandemic. Int J Env Res Public Health. (2020) 17:6494. doi: 10.3390/ijerph17186494
17. Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning province, China: a cross-sectional study. Int J Env Res Public Health. (2020) 17:2381. doi: 10.3390/ijerph17072381
18. Hawlader MDH, Rashid MU, Khan MAS, Ara T, Nabi MH, Haque MMA, et al. Quality of life of COVID-19 recovered patients in Bangladesh. PLoS One. (2021) 16:e0257421. doi: 10.1371/journal.pone.0257421
19. Abdelghani M, Hamed MG, Said A, Fouad E. Evaluation of perceived fears of COVID – 19 virus infection and its relationship to health – related quality of life among patients with diabetes mellitus in Egypt during pandemic: a developing country single – center study. Diabetol Int. (2021) 13:108–16. doi: 10.1007/s13340-021-00511-8
20. O’Dwyer MC, Meixner K, Albiac LC, El Khoury C, Capizzano JN, Ramakrishnan M, et al. Health-related quality of life for people with acute and chronic illnesses during the COVID-19 pandemic. J Am Board Fam Med. (2021) 34:509–21. doi: 10.3122/jabfm.2021.03.200593
21. Rose KJ, Scibilia R. The COVID19 pandemic—perspectives from people living with diabetes. Diabetes Res Clin Pract. (2021) 173:108343. doi: 10.1016/j.diabres.2020.108343
22. Szczepańska A, Pietrzyka K. The COVID-19 epidemic in Poland and its influence on the quality of life of university students (young adults) in the context of restricted access to public spaces. Z Gesundh Wiss. (2021). Online ahead of print. doi: 10.1007/s10389-020-01456-z
23. Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC Geriatr. (2012) 12:27. doi: 10.1186/1471-2318-12-27
24. Sartorius N, Janca A. Psychiatric assessment instruments developed by the world health organization. Soc Psychiatry Psychiatr Epidemiol. (1996) 31:55–69. doi: 10.1007/BF00801901
25. Beusenbrg M, Orley J. A user’s Guide to the Self-Reporting Questionnaire (SRQ). Geneva: World Health Organization (1994).
26. Khan AM, Flora MS. Maternal common mental disorders and associated factors: a cross-sectional study in an urban slum area of Dhaka, Bangladesh. Int J Ment Health Syst. (2017) 11:23. doi: 10.1186/s13033-017-0129-3
27. Cherian VI, Peltzer K, Cherian L. The factor structure of the self-reporting questionnaire (SRQ-20) in South Africa. East Afr Med J. (1998) 75:654–6.
28. Giang KB, Allebeck P, Kullgren G, Tuan NV. The Vietnamese version of the self-reporting questionnaire 20 (SRQ 20) in detecting mental disorders in rural Vietnam: a validation study. Int J Soc Psychiatry. (2006) 52:175–84. doi: 10.1177/0020764006061251
29. Netsereab TB, Kifle MM, Tesfagiorgis RB, Habteab SG, Weldeabzgi YK, Tesfamariam OZ. Validation of the WHO self - reporting questionnaire - 20 (SRQ - 20) item in primary health care settings in Eritrea. Int J Ment Health Syst. (2018) 16:1–9. doi: 10.1186/s13033-018-0242-y
30. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
31. Yu DS. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. (2010) 66:2350–9. doi: 10.1111/j.1365-2648.2010.05394.x
32. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
33. Ohaeri JU, Awadalla AW. The reliability and validity of the short version of the WHO quality of life instrument in an Arab general population. Ann Saudi Med. (2009) 29:98–104. doi: 10.4103/0256-4947.51790
34. World Health Organization [WHO]. WHOQOL-BREF; Introduction, Administration, Scoring and Generic Version of the Assessment. Geneva: World Health Organization (1996). p. 1–18.
35. Algamdi MM. Assessment of post-COVID-19 quality of life using the quality of life index. Patient Prefer Adherence. (2021) 15:2587–96. doi: 10.2147/PPA.S340868
36. Khaje-bishak Y, Payahoo L, Pourghasem B, Jafarabadi MA. Assessing the quality of life in elderly people and related factors in Tabriz, Iran. J Caring Sci. (2014) 3:257–63.
37. Starke KR, Petereit-haack G, Schubert M, Kämpf D, Schliebner A, Hegewald J, et al. The age-related risk of severe outcomes due to COVID-19 infection: a rapid review, meta-analysis, and meta-regression. Int J Environ Res Public Health. (2020) 17:1–22. doi: 10.3390/ijerph17165974
38. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio- demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID- 19. Eur Child Adolesc Psychiatry. (2020) 29:749–58.
39. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1–25. doi: 10.3390/ijerph17051729
40. Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health related quality of life: the potential benefit of health literacy. J Clin Med. (2020) 9:965. doi: 10.3390/jcm9040965
41. Skevington SM. Qualities of life, educational level and human development: an international investigation of health. Soc Psychiat Epidemiol. (2010) 45:999–1009.
42. Darçin M. How air pollution affects subjective well-being. In: Mollaoglu M editor. Well-Being And Quality Of Life - Medical Perspective. London: IntechOpen (2017). doi: 10.5772/67742
43. Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. (2011) 52:199–209. doi: 10.1016/j.psym.2011.01.036
44. Livneh H. Psychosocial adaptation to chronic illness and disability: a conceptual framework. Rehabil Couns Bull. (2001) 44:151–60. doi: 10.1177/003435520104400305
45. Fischer M, Scharloo M, Abbink J, van ‘t Hul A, van Ranst D, Rudolphus A, et al. The dynamics of illness perceptions: testing assumptions of Leventhal’s common-sense model in a pulmonary rehabilitation setting. Br J Health Psychol. (2010) 15:887–903. doi: 10.1348/135910710X492693
46. Colpaert K, De Maeyer J, Broekaert E, Vanderplasschen W. Impact of addiction severity and psychiatric comorbidity on the quality of life of in residential treatment. Eur Addict Res. (2013) 19:173–83. doi: 10.1159/000343098
47. Olickal JJ, Saya GK, Selvaraj R, Chinnakali P. Association of alcohol use with quality of life (QoL): a community based study from Puducherry, India. Clin Epidemiol Glob Health. (2021) 10:100697. doi: 10.1016/j.cegh.2021.100697
48. Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Env Med. (2018) 60:248–57. doi: 10.1097/JOM.0000000000001235
49. Møller L, Matic S. Best Practice in Estimating the Costs of Alcohol: Recommendations for Future Studies. Copenhagen: World Health Organization Regional Office for Europe (2010).
50. Testino G. Are patients with alcohol use disorders at increased risk for covid-19 infection? Alcohol Alcohol. (2020) 55:344–6. doi: 10.1093/alcalc/agaa037
51. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20.
52. Kirchner JE, Zubritsky C, Cody M, Coakley E, Chen H, Ware JH, et al. Alcohol consumption among older adults in primary care. J Gen Intern Med. (2007) 22:92–7.
53. Goel A, Jat SL, Sasi A, Paliwal VK, Aggarwal R. Prevalence, severity, and impact on quality of life of restless leg syndrome in patients with liver cirrhosis in India. Indian J Gastroenterol. (2016) 35:216–21. doi: 10.1007/s12664-016-0668-6
54. Li W, Zhao N, Yan X, Zou S, Wang H, Li Y, et al. The prevalence of depressive and anxiety symptoms and their associations with quality of life among clinically stable older patients with psychiatric disorders during the COVID-19 pandemic. Transl Psychiatry. (2021) 11:75. doi: 10.1038/s41398-021-01196-y
55. Holvast F, van Hattem BA, Sinnige J, Schellevis F, Taxis K, Burger H, et al. Late-life depression and the association with multimorbidity and polypharmacy: a cross-sectional study. Fam Pr. (2017) 34:539–45.
56. Prina A, Ferri C, Guerra M, Brayne C, Prince M. Co-occurrence of anxiety and depression amongst older adults in low-and middle-income countries: findings from the 10/66 study. Psychol Med. (2011) 41:2047. doi: 10.1017/S0033291711000444
57. Farris M, Leong I, Abdullah B, Yusof HA, Shariff NM, Hami R, et al. Depression and anxiety in the Malaysian urban population and their association with demographic characteristics, quality of life, and the emergence of the COVID-19 pandemic. Curr Psychol. (2021) 40:6259–70. doi: 10.1007/s12144-021-01492-2
58. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. (2020) 368:1211.
59. El Sayed S, Gomaa S, Shokry D, Kabil A, Eissa A. Sleep in post – COVID – 19 recovery period and its impact on different domains of quality of life. Egypt J Neurol Psychiatry Neurosurg. (2021) 57:1–10. doi: 10.1186/s41983-021-00429-7
Keywords: COVID-19, quality of life, QOL, predictors, Ethiopia
Citation: Ayalew M, Deribe B, Hussen S, Defar S and Gedefaw A (2022) Quality of life among patients with chronic non-communicable diseases during COVID-19 pandemic in Southern Ethiopia: A cross-sectional analytical study. Front. Psychiatry 13:855016. doi: 10.3389/fpsyt.2022.855016
Received: 14 January 2022; Accepted: 29 August 2022;
Published: 21 September 2022.
Edited by:
Jerome T. Galea, University of South Florida, United StatesReviewed by:
Ehsan Sarbazi, Tabriz University of Medical Sciences, IranCopyright © 2022 Ayalew, Deribe, Hussen, Defar and Gedefaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Ayalew, bWFtZWF5YWxlQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.