- 1Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy
- 2Department of Clinical and Experimental Medicine, University of Foggia, Foggia, Italy
- 3Department of Nervous System and Behavior Sciences, University of Pavia, Pavia, Italy
- 4Stella Maris, Scientific Institute of Child Neurology and Psychiatry, Pisa, Italy
- 5Child Neuropsychiatry, Genoa and Department of Neuroscience (DINOGMI), IRCCS G. Gaslini Institute, University of Genoa, Genoa, Italy
- 6Department of Neuroscience, University of Genoa, Genoa, Italy
- 7Department of Biomedical Sciences, University of Cagliari, Cagliari, Italy
- 8Department of Life Sciences and Publich Health, Catholic University and Bambino Gesù, Rome, Italy
- 9Children's Hospital, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Rome, Italy
Background: The current conceptualization of schizophrenia as neurodevelopmental disorder should lead to innovative public health policies in terms of a reorganization of the mental health care systems, particularly in the transition from adolescence to adulthood, to reduce personal, familiar, and social costs and burdens. The purpose of the project was to perform a survey among a panel of Italian schizophrenia experts, to share evidence-based information on adolescent schizophrenia and explore the degree of consensus among professionals in the following four macro-areas: early diagnosis; pharmacological treatment; health care system organization and transition process from adolescent to adulthood; and psychosocial interventions.
Methods: The consensus process consisted of a two-step web-based Delphi method, which took place between June and November 2021. The survey was developed by a panel of four psychiatrists and four child neuropsychiatrists, identified as key opinion leaders (KOLs). The KOLs identified 21 statements involving a total of 70 items with a major need of clarification on early-onset schizophrenia (EOS). The survey was distributed to 86 specialists in psychiatry and child neuropsychiatry.
Results: The results revealed a large agreement among the expert group on all the investigated areas of adolescent schizophrenia patterns of care and management. Consensus was ultimately reached for 67 items of the Delphi survey (95.7%), while negative consensus was reached for 2 items and no consensus was reached for 1 item.
Conclusions: Overall, results showed a significant gap between the acquired scientific knowledge and clinical practice. In this scenario, it should be necessary to plan specific initiatives at a multiple level, to edit recommendations on clinical decision-making, as well as to prompt changes at the political and organizational levels, also involving scientific societies, patients, and family associations, to overcome the barriers that delay the implementation process.
Introduction
Schizophrenia is a highly prevalent, severe mental illness, representing one of the main causes of years lost due to disability (YLD) in adults in Europe (1). Schizophrenia onset usually occurs in late adolescence or early adulthood, but it is frequently anticipated by a prodromal phase, in which cognitive impairment, negative symptoms and poor social functioning occur several years before the first episode of psychosis (2). Within the broader psychosis spectrum, childhood and adolescence schizophrenia are peculiar disorders (3). Particularly, in adolescent it is more often a severe and debilitating psychotic disorder with considerable impairments in psychosocial, educational, and occupational functioning with a heavy burden on health care services. Despite the relatively high (up to 5%) prevalence of psychotic symptoms in otherwise healthy children, childhood-onset schizophrenia (COS) is rare, so epidemiologic incidence data with diagnoses based on standardized clinical assessments are lacking. Since clinical, cognitive, genetic, and neuroimaging characteristics of early-onset schizophrenia (EOS) patients are, in part, outlined, current findings point toward continuity between the early and adult-onset schizophrenia, with the former possibly being a more severe variant of the latter (4), suggesting the needs to implement mental health systems to improve possible interventions, especially in the transition from youth to adult facilities. The purpose of the present paper is to provide an exhaustive evaluation of adolescent schizophrenia, covering epidemiologic, neurobiological, and clinical features, in order to identify feasible treatments plans, both pharmacological and psychosocial, reducing personal, familiar, and society burdens, and improving prognosis, psychosocial functioning, and quality of life (QoL). Moreover, the paper covers initial programs aimed to rethink mental health system in the transition from adolescence to adulthood. Specifically, a Delphi approach was used to share evidence-based information on adolescent schizophrenia and assess the degree of consensus among professionals in the following investigation areas: (i) early diagnosis; (ii) pharmacological treatment; (iii) health care system organization and transition process from adolescent to adulthood; and (iv) psychosocial interventions.
In the following section, we report a summary of the evidence provided by the scientific board, that lead to some brief and explicit statements on adolescent schizophrenia.
A General Overview: Adolescence as a Major Risk Phase for Psychopathology
Schizophrenia is currently described as a neurodevelopmental disorder due to the interaction of different genetic and environmental factors that act long before the beginning of pathophysiological processes (5). Although psychotic onset is generally in early adulthood, less common in adolescence and quite rare in childhood, about 11–18% of patients present with their first episode of psychosis before the age of 18 (6, 7). Hence if schizophrenia peak onset is generally between 15 and 25 years of age (8), incidence rates increase around 14 years of age (9), with ~39% of male and 23% of female patients developing schizophrenia before 19 years of age (10). Schizophrenia before the age of 18 years is usually divided into two categories. Early onset schizophrenia (EOS) presents between the ages of 13 and 17 years, whereas very-early-onset schizophrenia (VEOS) presents at or before the age of 12 years. An early identification after the onset of psychotic symptoms is aimed at reducing possible adverse factors that determine poor psychosocial functioning and QoL in young patients (11–15). Among these factors, the duration of untreated psychosis (DUP), that is the time from the onset of psychotic symptoms to the commencement of adequate treatment, is one of the main issues (16). In this context, the early detection and treatment of help-seeking individuals and of those already in the earliest phases of a psychotic disorder is currently considered as the most promising strategy to improve treatment outcomes and long-term prognosis, and thus to reduce worst consequences of a full-blown psychotic disorder in youth populations (17).
Adolescent Schizophrenia: Nosographic Background and Clinical Dimensions
If among children, schizophrenia is definitively a rare neuropsychiatric disorder with incidence rates at around 0.04% based on the observations from the National Institutes of Mental Health (NIMH) cohort (18, 19), adolescent schizophrenia is a devastating disorder, probably underdiagnosed and undertreated, characterized by greater clinical severity and worse outcomes compared to the adult-onset disorder (20, 21). In this scenario, although several definitions are currently applied to describe children and adolescent patients with early onset schizophrenia with no apparent consensus (22), some definitions should be highlighted. Based on age at onset, VEOS emerges before 12 years, while EOS starts before 17 years (23). VEOS was found to have a prevalence rate of 1/10,000, while EOS at around 1–2/100 (18). Since these operational definitions might be overlapping, two more strictly classifications are provided: COS is defined with an age of onset at 12 years or younger, while adolescent-onset schizophrenia is defined as beginning between 13 and 17 years (24). According to the scientific literature and for better understanding of the text, we will consider the terms EOS as adolescent schizophrenia and VEOS as COS (3). Despite these attempts in identifying the different forms of early-onset psychosis, at a nosological level patients with adolescent schizophrenia (EOS) or with COS (VEOS) are diagnosed using the same criteria as for adult-onset schizophrenia (AOS), following the Diagnostic and Statistical Manual [DSM-5; (25)] or the International Classification of Diseases, 10th Revision (26). This categorical approach could lead to not recognizing the juvenile variants of schizophrenia, with serious consequences for young subjects. From this point of view, a dimensional approach, rather than a categorical one, could favor early recognition and intervention of adolescent schizophrenia and COS (20, 27). At a developmental level, adolescent schizophrenia has been associated with poor premorbid functioning and developmental delays in reaching crucial milestones (28). At a clinical level, adolescent schizophrenia, compared to adult-onset schizophrenia is more commonly characterized by an insidious onset (21, 24), with prevalent negative symptoms (20, 29). Summing up these data, a systematic review, involving 1.506 patients with child or adolescent psychosis, showed peculiar clinical features in these samples: auditory hallucinations (81.9%), delusions (77.5%; mainly persecutory), thought disorders (65.5%), bizarre or disorganized behavior (52.8%), and negative symptoms (flat or blunted affect) (52.3%). Moreover, high comorbid rates such as posttraumatic stress disorder (PTSD) (34.3%), attention-deficit/hyperactivity disorder (ADHD), disruptive behavior disorders (33.5%), and substance abuse/dependence (32.0%) were also reported (30). In addition, cognitive impairment is a common feature of adolescent schizophrenia (31, 32), which occurs at the time of illness onset and once established, appears to be stable over time, without continued deterioration (33, 34). Regarding illness progression and outcomes, adolescent schizophrenia shows worse prognosis, with a severe and chronic course, so that only a minority of patients is able to get symptomatic remission and functional recovery (21, 35, 36). Taking these observations together, a recent systematic review confirmed that predictors of worse clinical, cognitive, and functional outcomes in adolescent schizophrenia are represented by premorbid difficulties, symptom severity at baseline (especially of negative symptoms) and longer DUP (37). Among these factors, current literature highlighted the association between greater clinical severity, worse outcomes, and longer DUP (38), that for adolescent schizophrenia is 3 to 5 times longer than the DUP in AOS (30).
Adolescent Schizophrenia: Early Diagnosis
With these notions in mind, worldwide mental health policies are claimed to give priority to early intervention services for children and adolescents. Adolescent schizophrenia is grossly diagnosed with the same criteria of International Classification of Diseases (26) and Diagnostic and Statistical Manual [DSM-5; (25)], as used for adult patients. Thus, a good quality assessment should include a detailed history from all possible sources as well as a physical and mental state examination. In particular, psychotic symptoms dimensions, comorbid psychiatric and medical conditions such as developmental disorders (including speech and language difficulties), comorbid substance abuse, risk of harms/suicidality as well as psychosocial functioning, and socio-cultural milieu of the patient and family should be evaluated (17, 27, 39). Moreover, medical work-up is always needed with basic pediatric assessment (e.g., routine laboratory testing), neurological and cognitive examination, neuroimaging, and tests for specific medical syndromes (e.g., genetic, infectious, autoimmune, rheumatologic, metabolic, and toxicology screens) (39). However, clinicians should keep in mind that a definitive diagnosis of early-onset/adolescent schizophrenia requires time and repeated assessments since clinical presentations tend to change especially during the first few years of the psychotic disorder. Therefore, adolescent schizophrenia diagnosis should be made with caution and sensitivity as it is associated with significant negative psychosocial consequences, both for the patients and their caregivers (27, 39).
Adolescent Schizophrenia: Treatment Options and Patterns of Care
As in AOS, treatment decisions in the adolescent schizophrenia population should be drawn by consulting all figures involved in the care of these patients, particularly, their caregivers, taking into account familiar perspectives and dynamics (17, 21). Clinicians should provide an integrated approach, including pharmacological, psychological, psychosocial, rehabilitative, and family-oriented interventions to address all the needs of the patients and their families (24, 27, 39). Admission at acute inpatient facility is recommended when the adolescent exhibits suicidal projects or attempts, self-injurious behaviors, aggression, severe agitation, poor general psychical conditions or when the familiar milieu is unsupportive or even hostile (39).
Pharmacological Interventions
At pharmacological level, antipsychotic agents are considered as the first line of treatment in the youth population. The main goals of pharmacotherapy interventions are to menage acute psychotic states and prevent relapse, always minimizing possible adverse events (24). Particularly, second-generation agents (SGAs) are typically offered as the first choice in early-onset/adolescent schizophrenia (27, 40, 41). Drugs like risperidone, aripiprazole, quetiapine, paliperidone, and olanzapine have actually received Food and Drug Administration (FDA) approval for treating schizophrenia in adolescents 13 years and older (42) since reductions of psychotic symptoms severity were observed compared to placebo (40). To date, in Europe only three SGAs - oral aripiprazole, oral paliperidone and lurasidone - have received approval from the European Medicine Agency (EMA) for treating adolescents with schizophrenia. Specifically, oral aripiprazole and oral paliperidone are recommended for adolescents aged 15 year and older. Since its positive efficacy and safety in adolescents - aged 13–17 years - with acute schizophrenia, lurasidone has been recently approved by EMA for adolescent schizophrenia starting from 13 years of age. Lurasidone favorable efficacy and safety profile in adolescent schizophrenia patients aged 13–17 years has also been demonstrated in the long-term period, through a 2-year extension study of the former (43). A recent network meta-analysis, including 28 randomized controlled trials (RCTs) with 3.003 participants, confirmed these findings, showing that olanzapine, risperidone, lurasidone, aripiprazole, quetiapine, paliperidone, and asenapine were significantly better than placebo, while haloperidol, trifluperazine, loxapine, and ziprasidone were not (44). Moreover, clozapine was found to be significantly more effective than all other included antipsychotics (44). However, clozapine should be proposed as a second-line agent in child and adolescent samples especially in treating refractory conditions: this is due to potential adverse events of clozapine, including risk of agranulocytosis, seizures, and metabolic disturbances (19, 45). Clinicians should keep in mind a higher risk of extrapyramidal symptoms (EPS), akathisia, prolactin elevation, sedation, cardiovascular effects (QTc prolongation, orthostatic hypotension, tachycardia, and pericarditis) and metabolic effects such as weight gain, dyslipidemia, glucose intolerance were reported in adolescent population rather than in adults, with polypharmacotherapy contributing to an increased risk (41, 46, 47). Although existing data indicate similar efficacy between first generation antipsychotics (FGAs) and SGAs (48), SGAs were also found to improve QoL and social functioning in adolescent schizophrenia samples (44). In particular, quetiapine and lurasidone were significantly more efficacious than placebo at improving QoL (43), while no significant effects were observed for asenapine and aripiprazole (44). On the other hand, risperidone, aripiprazole and lurasidone showed significantly better improvements in social functioning compared to placebo (44). However, despite the established efficacy, antipsychotic discontinuation is a common phenomenon also in adolescent schizophrenia patients. A national survey found that approximately 75% of the sample discontinued SGAs within 18 months of initiating treatment (49) and the Treatment of Early Onset Schizophrenia Spectrum Disorders Study (TEOSS) found that only 12% of subjects completed the 12-months period of taking their medications (50). Several reasons should explain this issue, mostly including presenting adverse events due to prescribed drugs (47). Thus, to limit this problem, clinician should keep in mind that FGAs are not recommended over SGAs in adolescent patients with schizophrenia due to increased risks of EPS and akathisia (27). On the other hand, a recent open-label study highlighted that, in the long-term, lurasidone in adolescents (13–17 years) with schizophrenia was associated with minimal effects on body weight, lipids, glycemic, and prolactin indices (43), while metanalytic evidence confirmed a reduced discontinuation rates for lurasidone over other antipsychotic agents (51). Guidelines recommend to carefully consider tolerability profile in the selection of an antipsychotic with a specific patient (51), taking into account several factors including tolerability drugs profile, patient and family preference, drug cost and availability (41, 47, 52).
Psychosocial Interventions
Since pharmacological treatments showed limited efficacy on negative and cognitive symptoms, and functional recovery in these populations (21), there is a growing interest in non-pharmacological approaches such as psychosocial interventions, although few data is available to date in adolescent schizophrenia patients. Adjunctive psychosocial interventions should be provided in combination with medications to reduce morbidity burden and promote treatment adherence and alliance (21). Preliminary evidence is provided for cognitive remediation (CR) efficacy in the first episode or in early schizophrenia, despite more research is needed to confirm the efficacy and the effectiveness of CR in the early course of schizophrenia (53). Concerning psychotherapy, although cognitive behavioral therapy (CBT) is an established treatment in AOS sample, only one report is currently available targeting early-onset patients (54). Only preliminary evidence was obtained with psychoeducation interventions (24), showing lower rates of rehospitalization in a small sample of adolescents with early onset psychosis (55). More recently, a RCT assessed the efficacy of a comprehensive psychoeducation problem solving intervention group in 55 adolescents with early onset schizophrenia and their parents (56). In this perspective, family-oriented interventions are particularly relevant during the early phases of the disorder (57), and current meta-analytic evidence confirmed the efficacy of family support interventions to reduce relapse and rehospitalization rates in this population (58). In this way, family support interventions resulted in improved caregivers' psychological health and general wellbeing and in reduced burdens of care (58).
Health Care System Organization and Transition Process From Adolescent to Adulthood
In order to reduce personal, familiar, social costs and burdens, innovative public health policies are needed in terms of a practicable reorganization of the mental health care systems. A structural problem is that in most European countries, mental health care for children and adolescents with psychiatric problems is independent and operationally separated from that for adults (59). This type of organization, also reflecting differences in specific training programs for resident doctors, could lead to difficulties in the transition from adolescence to adulthood between mental health services, bringing the patients to receive less support in adult facilities and troubled changes in diagnosis and treatments (29). Thus, two alternative models of transition between child/adolescent and adult' services may be considered. The first model is based on the identification of a transitional team operating independently from youth and adult services: this model has been implemented in prevention and early intervention in psychosis programs, although the main weakness of this model is the introduction of additional splits within the system (29). Otherwise, the interlocking model requires the use of multidisciplinary care protocols interlocking child/adolescent and adults' services in which transition from these facilities is guaranteed by sharing all information and recommendations about several aspects of psychiatric pathways performed up to now (29). In Italy, the interlocking model was advised by the National Action Plan for Mental Health manifesto (60) providing recommendations in order to develop experimental projects aimed at prevention and early intervention. In particular, it was mostly recommended the creation of integrated and multidisciplinary teams, including both youth and adult mental health services, also involving families, educational facilities and environmental context. On the other hand, the ITAlian Partnership for Psychosis Prevention (ITAPP) project included five Clinical High Risk for Psychosis (CHR-P) academic centers across Italy, representing a promising template for transitional mental health services, aimed at early detection and intervention. In fact, serving both adolescents and young adults with multidisciplinary and integrated interventions, ITAPP project is aimed at developing specialized facilities that bridge the gap in the transitioning phase from youth to adulthood, thus ameliorating presenting symptoms, delaying, and preventing psychosis onset while reducing DUP (61).
Objective
The purpose of this study was to perform a Delphi survey among a panel of Italian schizophrenia experts, in order to obtain a qualified consensus in managing patients with adolescent schizophrenia. In particular, the aims were to identify the characteristics of adolescent patients with schizophrenia, to define the best pathways for the management of schizophrenia in adolescent patients, especially in the transition phase, to understand the available psychopharmacological and psychosocial treatments and their impact on the patients' QoL, to identify patients' and caregivers' needs, and to find actions to address stigma.
The Delphi approach was used to share evidence-based information on adolescent schizophrenia and assess the degree of consensus among professionals in the following four macro-areas: (i) early diagnosis; (ii) pharmacological treatment; (iii) health care system organization and transition process from adolescent to adulthood; and (iv) psychosocial interventions.
Materials and Methods
The Delphi method is a structured technique aimed at obtaining by repeated rounds of questionnaires a consensus opinion from a panel of experts in areas wherein evidence is scarce and opinion is important (62, 63). In the present manuscript, the consensus process consisted of a two-step web-based Delphi method, which took place between June and November 2021. The survey was developed by a panel of eight physicians (four psychiatrists, four child neuropsychiatrists) identified as key opinion leaders (KOLs) in their respective fields in Italy. The KOLs met to fully analyse the published literature and discuss the unmet needs about early-onset and adolescent schizophrenia. The first step of question sourcing served to collect an initial pool of feedback on areas that the KOLs considered most critical based on their clinical practice. Comments were then analyzed and coded into themes, grouping subsets of related items of enquiry. The organization of themes and items into a coherent and meaningful set of statements for the Delphi questionnaire was further informed by a literature review on the management of EOS. The first draft of the Delphi questionnaire was submitted to the KOLs for critical appraisal and improvement of the draft to ensure that items were relevant to the research question, were clearly worded and did not overlap with previous items. The KOLs identified 21 statements involving a total of 66 items with a major need of clarification, focused on the following topics: (i) early diagnosis; (ii) pharmacological treatment; (iii) health care system organization and transition process from adolescent to adulthood; and (iv) psychosocial interventions. Once developed, the survey was distributed to 86 specialists in psychiatry and child neuropsychiatry via an online survey platform with anonymized results. Panelists were psychiatrists and child neuropsychiatrists selected by the scientific board, working in academic and non-academic settings with solid experience in the field of schizophrenia (at least 5 years of clinical experience). The size of the expert panel was determined by involving specialists from 15 Italian regions, in order to have a representative sample of the national territory and a homogeneous distribution. Panelists were invited to rate their level of agreement or disagreement on each statement using a 5-point Likert scale, scored from 1 to 5 (1, extremely disagree; 2, disagree; 3, agree; 4, mostly agree; and 5, extremely agree). Results were expressed as a percentage of respondents who scored each item as 1 or 2 (disagreement) or as 3, 4, or 5 (agreement). A cutoff of 66% of agreement/disagreement was chosen a priori to represent positive or negative consensus, respectively. No consensus was reached when <66% of the answers fell in the same category (62, 63). In the first round of the Delphi survey, there were 70 respondents among the 86 invited panelists. For the statements and items on which consensus had not been achieved, panelists were asked to rate again in a second round their agreement/disagreement. The second round was completed by all the 70 panelists who responded to the first round. Table 1, in results section, shows demographic characteristics of responders. Descriptive statistics were performed to summarize the results.
Results
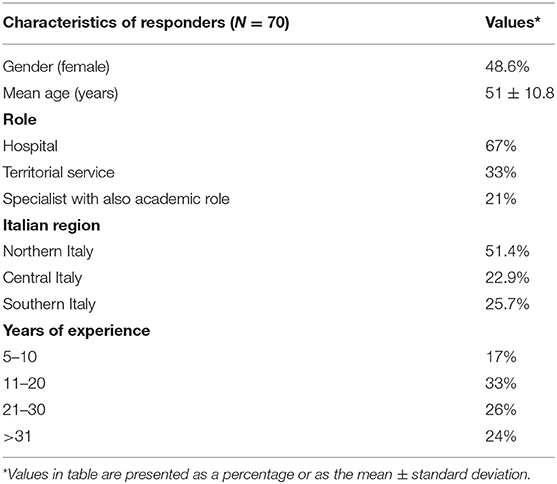
The first round of the Delphi survey had a response rate of 81.4%, whereas 100% of panelists who responded to round 1 completed also round 2. The average age of the respondents was 51 years, 34 (48.6%) were females, 34 (48.6%) were specialists in psychiatry and 36 (51.4%) in child neuropsychiatry. Table 1 summarizes the characteristics of responders in the Delphi survey, also including their role, years of clinical experience, and geographical distribution.
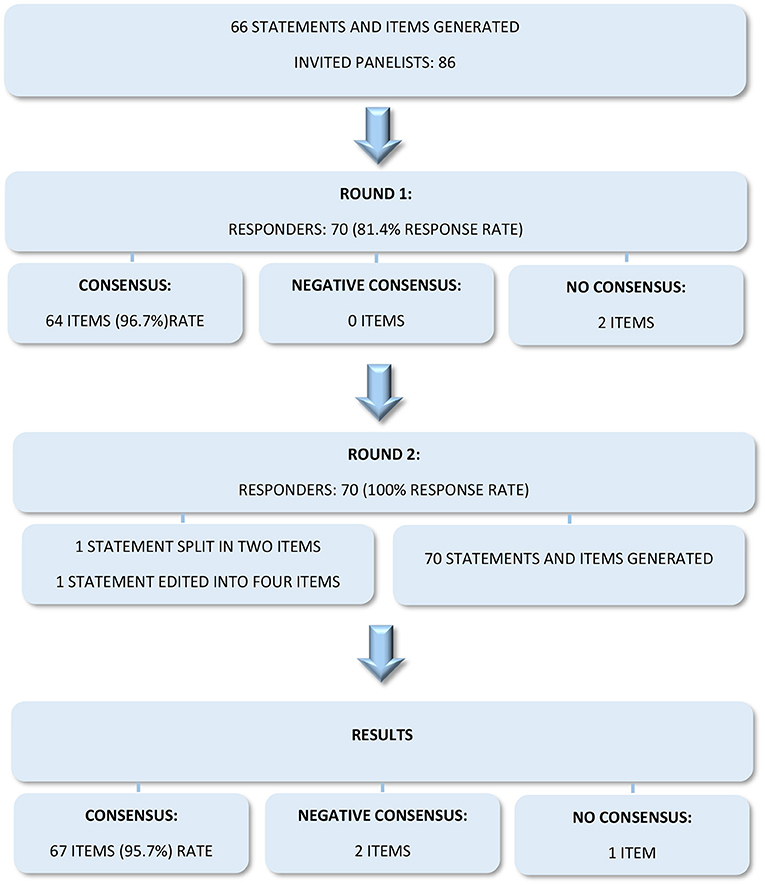
In round 1, consensus was reached for 64 of the 66 statements and items (96.7%), while no consensus was reached for two statements. The second round was performed on the two statements for which consensus had not been reached, after revising and clarifying the items. Specifically, one statement was split into two items, while the second one was edited into four clearer items, getting a final number of statements and items of 70. Overall, consensus was ultimately reached for 67 items of the Delphi survey (95.7%), while negative consensus was reached for 2 items and no consensus was reached for 1 item (Figure 1).
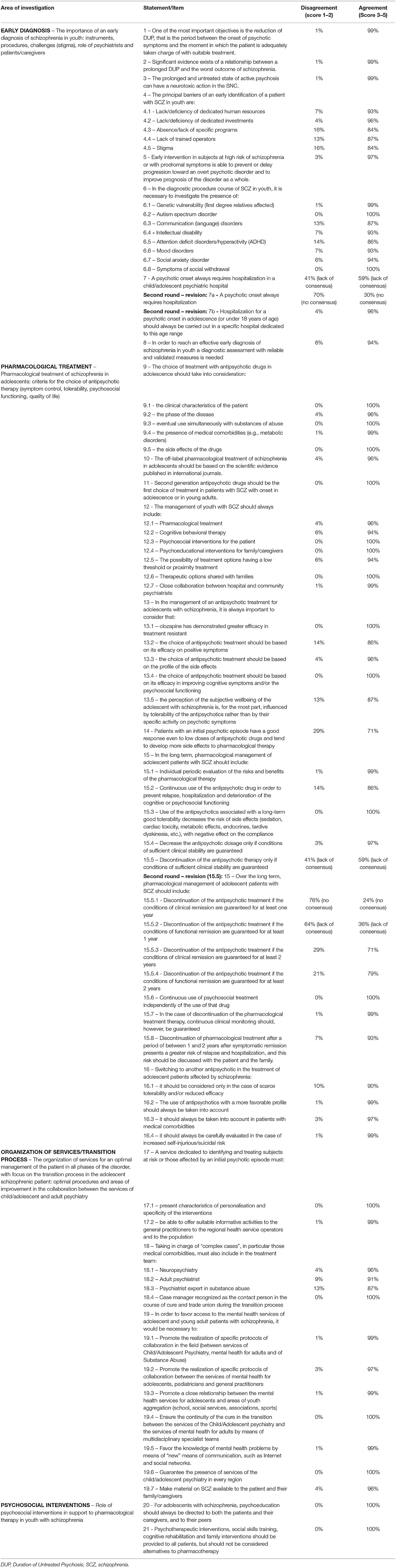
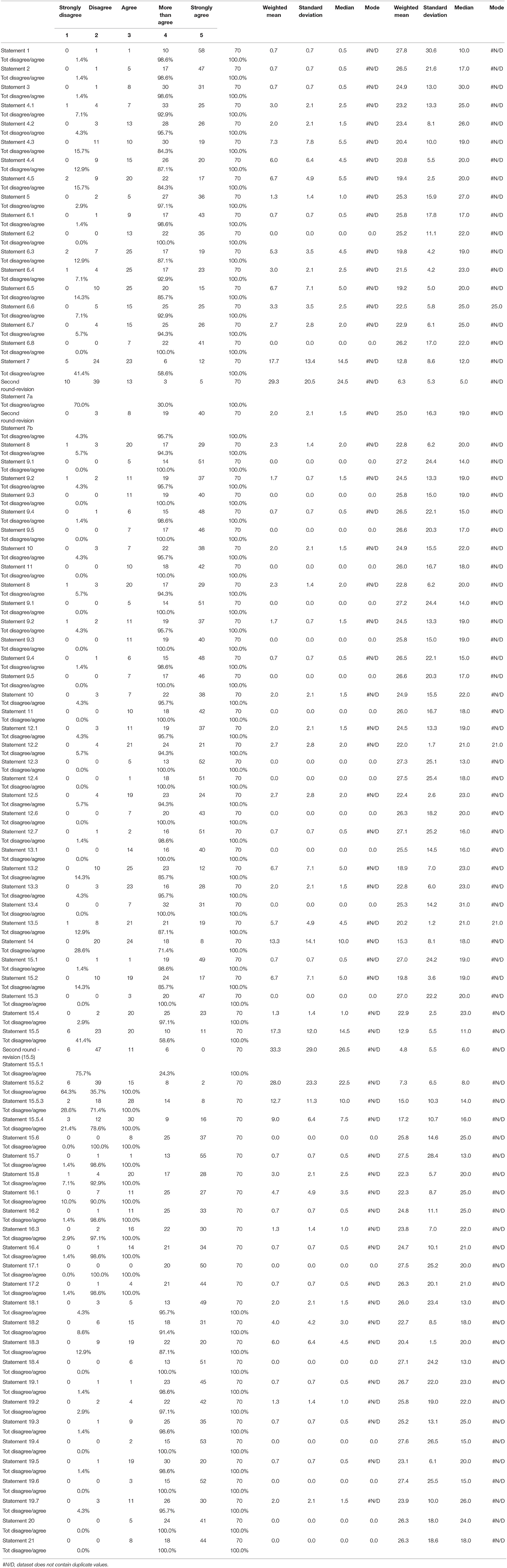
Tables 2.1, 2.2 summarize all the statements and items of the consensus, indicating the percentages of agreement and disagreement, mean, median, mode and standard deviation for each of them.
Major statements, grouped in the four macro-areas, are reported below.
Early Diagnosis
This area includes eight statements and 19 items, concerning: the DUP, the importance of an early diagnosis and an early intervention, the diagnostic process, the use of assessment tools, and the challenges and the barriers for an early recognition. In the second round of the survey, one statement of this investigating area (statement - 7) was split in two items. More in detail, a high consensus was reached in the following items: reducing DUP, recognizing adolescents at risk of developing psychosis and in prodromal phase, investigating the presence of other neurodevelopment disorders and other comorbidity using standardized and validated assessment tools, and hospitalization (if necessary) only in structures specifically dedicated for this development stage. Furthermore, a broad consensus was obtained regarding the barriers and obstacles in recognition and in early identification of subjects with adolescent schizophrenia, such as the lack of human resources and trained operators, the scarcity of investments and specific dedicated programs and the adverse role of stigma. On the other hand, a negative consensus was expressed regarding the need of hospitalization in any patients with first-episode psychosis.
Pharmacological Treatment
This area includes eight statements and 32 items, concerning: the choice of antipsychotic treatment, FGAs and SGAs, the use of off-label drugs, the efficacy on positive, negative and cognitive symptoms, side effects, safety, the duration of treatment, the presence of comorbidities, a concomitant substance abuse, when considering a switch, clinical and functional outcome, patient wellbeing, and family involvement. In the second round of the survey, one statement of this investigating area (statement – 15; item 15.5) was edited into four items. In particular, a broad consensus was achieved in the following items: the importance of the choice of antipsychotic treatments on the basis of the clinical characteristics, such as the stage of the illness, the presence of medical comorbidities and eventual concomitant substance abuse, also taking into account side effects, safety, and the characteristics of the drug, such as the preference for SGAs, and the efficacy on positive, negative, and cognitive symptoms. Furthermore, a large consensus was also obtained regarding the need of a continuous pharmacological treatment, shared with the patient and the family, better if integrated with psychosocial interventions, considering not only the symptomatic, but also the functional remission and the subjective wellbeing. A broad agreement was additionally expressed concerning the off-label drugs utilization, the utility of clozapine in resistant patients, and when considering a switch to other antipsychotics. Concerning this last point, a high consensus was achieved regarding the need of a switch in cases of reduced clinical efficacy and poor tolerability, including metabolic side effects, the presence of medical comorbidities and a high suicidal risk. Instead, the experts displayed a lack of or a negative consensus about the opportunity to stop an antipsychotic therapy. More specifically, they seem to advise against a suspension of antipsychotics after 1 year of treatment, even if there is a clinical and/or functional remission, while they show some agreement on the possibility to stop antipsychotics after at least 2 years of treatment, only if there is a clinical and/or functional remission.
Health Care System Organization and Transition Process From Adolescent to Adulthood
This area includes three statements and 13 items, concerning: the characteristics of a mental health service for adolescents, the multidisciplinary team-working, the role of the case manager, how to facilitate access to mental health services, how to promote transition between child neuropsychiatry and adult psychiatry, and how to ensure continuity of care in the early phases of schizophrenia. The experts considered the need to implement a service dedicated to the early identification and early intervention, which would operate in close collaboration with the local services, including general practitioners and population. Furthermore, the management of complex patients should include a joint and integrated work between the services of child neuropsychiatry and adult psychiatry, also including the services for addiction and identifying a case manager. Finally, a broad consensus was also reached with respect to the characteristics required to facilitate the access to the mental health services for adolescents and young adults. More specifically, it would be necessary to implement some collaboration protocols between child neuropsychiatry services, adult mental health services, addiction services, pediatricians, and general practitioners, in order to ensure a continuity of care in the early phases of schizophrenia and to promote the process of transition between child neuropsychiatry and adult psychiatry. This process could be facilitated implementing specialized multidisciplinary cross teams to the different services. Full consensus was also demonstrated regards the need to ensure the presence of child neuropsychiatry services in every territory at a national level. Lastly, it emerged how important it is to give a particular attention to the correct dissemination of information to patients and family members, also through the new social media, as well as promoting a close relationship with the areas of youth aggregation.
Psychosocial Interventions
This area includes two statements, concerning: psychoeducational interventions for the patient and for the family, evidence-based rehabilitation interventions, and integrated treatments. This area of investigation also obtained a full consensus. In particular among rehabilitation interventions, those evidence-based, such as psychoeducation, social skills training, and cognitive rehabilitation, should be taken into account.
Discussion
A two-step Delphi approach was used to share evidence-based information on early-onset/adolescent schizophrenia management, assessing the degree of consensus among specialists in psychiatry and child neuropsychiatry on the following key issues: (i) early diagnosis; (ii) pharmacological treatment; (iii) health care system organization as well as transition process from adolescent to adulthood; and (iv) psychosocial interventions. The results of the survey revealed a large consensus among the experts on all the investigated areas of adolescent schizophrenia patterns of care and management.
A high consensus was reached in the first area of investigation about early diagnosis and intervention and, particularly, the importance of the following variables: reducing DUP, recognizing adolescents at risk of developing psychosis and in prodromal phase, investigating the presence of other neurodevelopment disorders and other comorbidity using standardized and validated assessment tools, and hospitalization (if necessary) only in structures specifically dedicated for this development stage. Furthermore, a broad consensus was obtained regarding the barriers and obstacles in recognition and in early identification of subjects with adolescent schizophrenia, such as the lack of human resources and trained operators, the scarcity of investments and specific dedicated programs and the adverse role of stigma. These results show how psychiatrists and child neuropsychiatrists, in accordance with the scientific literature, and ministerial and regional recommendations, are completely aware of the importance of early recognition and intervention, even in subjects at risk of psychosis and in the prodromal phases (16, 17, 60). However, this approach is not always applied and is not feasible throughout the national territory, due to some barriers identified by the survey.
On the other hand, a negative consensus was expressed regarding the need of hospitalization in any patients with first-episode psychosis. This interesting result, in agreement with national and international literature (64, 65), could mean the necessity and the awareness of the experts to implement a community intervention, not based only on hospitalization.
The survey demonstrated a broad consensus in the second area of investigation that is the pharmacological treatment. In particular, it was outlined the importance of the choice of antipsychotic treatments on the basis of the clinical characteristics of the patient, such as the stage of the illness, the presence of medical comorbidities and eventual concomitant substance abuse. Side effects and the characteristics of the drug, such as the preference for SGAs, the efficacy on positive, negative and cognitive symptoms and the safety must be also considered. Furthermore, a large consensus was also obtained regarding the need of a continuous pharmacological treatment, shared with the patient and the family, better if integrated with psychosocial interventions, considering not only the symptomatic, but also the functional remission and the subjective wellbeing. A broad agreement was additionally expressed concerning the off-label drugs utilization (an option which could be considered, for example, for adolescent patients with demonstrated non-adherence to approved antipsychotics or in those with reduced clinical response or occurrence of adverse effects associated with approved antipsychotics), the utility of clozapine in resistant patients, and when considering a switch to other antipsychotics. In particular, for this last point, a high consensus was achieved regarding the need of a switch in cases of reduced clinical efficacy and poor tolerability, including metabolic side effects, the presence of medical comorbidities and a high suicidal risk. Regarding this area of investigation, results show that the choice of an antipsychotic therapy requires a careful and comprehensive patient assessment, giving attention not only to the symptomatic remission, but also to the functional remission and subjective wellbeing (35). In this regard, it is relevant to remind that the aim of schizophrenia treatment is not the remission of specific psychotic symptoms, but the improvement of functional outcomes and quality of life, always keeping in mind patient goals (66). Moreover, the risk/benefit ratio between effectiveness and side effects should be weighted for each patient (i.e., the long-term risk of metabolic side effects) (67). It should be emphasized how these results are in line with the international literature (15, 68–70). Instead, the experts displayed a lack of or a negative consensus about the opportunity to stop an antipsychotic therapy. More specifically, they seem to advise against a suspension of antipsychotics after 1 year of treatment, even if there is a clinical and/or functional remission, while they show some agreement on the possibility to stop antipsychotics after at least 2 years of treatment, only if there is a clinical and/or functional remission. It is interesting to note that this result is in any case consistent with the non-definitive and controversial international scientific literature on this still debated topic (71–74). The duration of maintenance treatment following a first-episode of schizophrenia is one of the most debated issue in the treatment of youth with schizophrenia, that has been addressed in a well-conducted systematic review performed by Keating et al. (72). In this regard, although good quality guidelines to assist in pharmacological treatment optimization exist, authors pointed out the inconsistencies between guidelines after the first-episode, underlining that the evidence base required to answer key health questions relevant to the pharmacological treatment of first-episode schizophrenia is still limited.
The third investigated area on the health care system organization and transition process from adolescent to adulthood reached high rates of consensus. In particular, the experts considered the need to implement a service, with specific characteristics, dedicated to the early identification and early intervention, which would operate in close collaboration with the local services, including general practitioners and population. Furthermore, the management of complex patients should include a joint and integrated work between the services of child neuropsychiatry and adult psychiatry, also including the services for addiction and identifying a case manager. Finally, a broad consensus was also reached with respect to the characteristics required to facilitate the access to the mental health services for adolescents and young adults. More specifically, it would be necessary to implement some collaboration protocols between child neuropsychiatry services, adult mental health services, addiction services, pediatricians, and general practitioners, in order to ensure a continuity of care in the early phases of schizophrenia and to promote the process of transition between child neuropsychiatry and adult psychiatry. This process could be facilitated implementing specialized multidisciplinary cross teams to the different services. Full consensus was also demonstrated regards the need to ensure the presence of child neuropsychiatry services in every territory at a national level. Lastly, it emerged how important it is to give a particular attention to the correct dissemination of information to patients and family members, also through the new social media, as well as promoting a close relationship with the areas of youth aggregation. Overall, in line with the existing scientific literature (75), this area of investigation about the organization of mental health services and on the transition process from adolescent to adulthood obtained a broad consensus among experts. Despite this agreement, the mental health services reality is not always the same expressed in the survey results and the dedicated services for early recognition and intervention, especially in the acute phases, are not uniformly spread throughout the national territory. Furthermore, these services, when existing, are not always well-integrated with each other, and do not work in multidisciplinary teams, therefore without promoting a stable patient health care path and a suitable transition between neuropsychiatry and adult psychiatry.
The fourth area of investigation obtained a full consensus on the use of integrated psychotherapeutic and psychosocial interventions. Among rehabilitation interventions, those evidence-based should be taken into account, in particular psychoeducation aimed at both patients and family members, social skills training, and cognitive rehabilitation. Again, the experts' panel was absolutely in agreement with the scientific literature (76–78). As in previous research fields taken into account in the present survey, such as the implementation of early recognition and identification services, evidence-based rehabilitation interventions and integrated treatments showed a significant gap between the acquired scientific knowledge and clinical practice. This means that, despite the growing scientific literature on these topics, a major concern is that evidence-based rehabilitation interventions and integrated treatments are not largely available in the real-world setting of mental health services (79).
Lastly, cost-effectiveness is an issue common to all the four investigated areas. In fact, both for early diagnosis, pharmacological and psychosocial treatments, as well as health care system organization, it is relevant to consider resources. In the real-world setting of adolescents and adults Mental Health Services, adequate resources for implementing the best clinical-therapeutic practices are not always available. In this scenario, even if psychotherapeutic and psychoeducational approaches may be helpful, but with very low evidence in youth (80), pharmacotherapy should always be the first option, even when other interventions are unavailable. However, it should also be highlighted that many psychosocial interventions, such as psychoeducation (81) and other integrated interventions (82), may be both clinically beneficial and cost-effectiveness in the early stages of the schizophrenia spectrum disorders.
Limitations
In this project some limitations are to be addressed. First, adherence to drug therapy and in particular the use of long-acting injectable (LAI) antipsychotics was not directly investigated. Second, the results may not be representative of the entire national territory and may not be generalizable to other Countries. Third, the survey involved only specialists in child neuropsychiatry and in adult psychiatry, but not pediatricians, general practitioners, other mental health workers, and patients and family association members, so it does not cover the views of all the stakeholders involved in this complex field.
Conclusion
To our knowledge, this is the first Delphi-based consensus survey on patterns of care in adolescent schizophrenia, involving experts and specialists in child neuropsychiatry and in adult psychiatry. The results of this consensus Delphi approach revealed a large agreement among the expert group of Italian specialists in child neuropsychiatry and in adult psychiatry on all the investigated areas of adolescent schizophrenia patterns of care and management. In particular, the level of agreement was maximum in the following crucial issues: early diagnosis; pharmacological treatment; health care system organization as well as transition process from adolescent to adulthood; and psychosocial interventions. Overall, results showed a significant gap between the acquired scientific knowledge and clinical practice. This means that, despite the growing scientific literature on early-onset/adolescent schizophrenia management, a major concern is that knowledge is not largely available in the real-world setting of mental health services. Of particular interest is that this science-to-service gap seems to be well-recognized by Italian specialists, who identify the lack of human resources and trained operators and the paucity of investments and specific dedicated programs as the main barriers that do not allow to fill the gap.
In this scenario, it should be necessary to program specific training events on adolescent/early onset schizophrenia and on the transition process, to draft and spread agreement protocols between child neuropsychiatry and adult psychiatry and to set up multidisciplinary teams transversal to services. Moreover, appear crucial to edit recommendations on clinical decision-making as well as to prompt changes at the political and organizational levels, also involving scientific societies, patients and family associations and all the stakeholders involved, in order to overcome the barriers that delay the implementation process.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The study was based on a survey that does not involve the participation of human subjects nor patient data management. Consequently, this study did not require ethical approval. All experts involved in the Delphi survey were informed of the study's objectives and the possibility of publishing the results in a peer-reviewed article. The participation was voluntary.
Author Contributions
All authors contributed to the writing and editing of the manuscript. All authors approved the final version of the manuscript.
Funding
GM was supported by funds of the Italian Ministry of Health: Ricerca Corrente (Project 2.10, PI Gabriele Masi). The authors declare that this study received funding from Angelina Pharma. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Ethos srl for logistic support in conducting the Delphi study.
External Validators
Paolo Cacciani, Brescia
Pietro De Rossi, Roma
Giacomo Deste, Brescia
Giovanni Valeri, Roma
Delphi Expert Panel Group:
Veronica Aiello, Genova
Mario Altamura, Bari
Anna Rita Atti, Bologna
Gianfranca Auricchio, Napoli
Roberto Averna, Roma
Elena Barletta, Genova
Luigi Basso, Bolzano
Stefano Berloffa, Pisa
Paola Bona, Savona
Albacenzina Borelli, Foggia
Stefania Borghetti, Milano
Carmela Bravaccio, Napoli
Pietro Calcagno, Genova
Angela Carofiglio, Bari
Alessandro Carozzi, Milano
Manuela Carpaneto, Alessandria
Alessandra Carta, Sassari
Sara Carucci, Cagliari
Chiara Caucci, Teramo
Nicolò Cipriani, Genova
Giulio Corrivetti, Salerno
Giulia D'Acunto, Pisa
Andrea De Giacomo, Bari
Elisa De Grandis, Genova
Gianluigi Di Cesare, Roma
Diana Di Pietro, Roma
Andrea Escelsior, Genova
Mauro Ferrara, Roma
Giuliana Gai, Genova
Roberto Gaggero, Genova
Gabriele Giacomini, Genova
Giuseppe Imperadore, Verona
Dario Lamonaca, Verona
Silvestro La Pia, Napoli
Riccardo Loparrino, Firenze
Liliana Lorettu, Sassari
Luciano Luccherino, Arezzo
Francesco Margari, Foggia
Chiara Margarita, Roma
Stefania Millepiedi, Viareggio
Maria Giulia Nanni, Ferrara
Silvia Paba, Cagliari
Sara Pacella, Genova
Giulia Piccinini, Genova
Sara Pignatelli, Genova
Maurizio Pincherle, Macerata
Tiziana Pisano, Firenze
Anna Polito, Foggia
Nicola Poloni, Varese
Matteo Porcellana, Milano
Andrea Presta, Genova
Pier Paolo Rizzo, Genova
Matteo Rocchetti, Pavia
Vincenzo Santospirito, Matera
Valeria Scandurra, Siena
Renato Scifo, Catania
Irene Serio, Savona
Michele Severini, Ancona
Laura Siri, Genova
Bruno Spinetoli, Roma
Luca Tarantola, Vercelli
Sarah Tosato, Verona
Marco Toscano, Milano
Sabrina Trudu, Cagliari
Fabiana Vercellino, Alessandria
Caterina Viganò, Milano
Benedetto Vitiello, Torino
Carmelo Zaffora, Messina
Elisabetta Zanotto, Genova
Spyridon Zotos, Ferrara
References
1. Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. (2011) 21:655–79. doi: 10.1016/j.euroneuro.2011.07.018
2. Lieberman JA, Perkins D, Belger A, Chakos M, Jarskog F, Boteva K, Gilmore J. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, therapeutic approaches. Biol Psychiatry. (2001) 50:884–97. doi: 10.1016/S0006-3223(01)01303-8
3. Clemmensen L, Vernal DL, Steinhausen HC. A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry. (2012) 12:150. doi: 10.1186/1471-244X-12-150
4. Kyriakopoulos M, Frangou S. Pathophysiology of early onset schizophrenia. Int Rev. Psychiatry. (2007) 19:315–24. doi: 10.1080/09540260701486258
5. Seidman LJ, Mirsky AF. Evolving notions of schizophrenia as a developmental neurocognitive disorder. J Int Neuropsychol Soc. (2017) 23:881–92. doi: 10.1017/S1355617717001114
6. Schimmelmann BG, Conus P, Cotton S, McGorry PD, Lambert M. Pre-treatment, baseline, and outcome differences between early-onset and adult-onset psychosis in an epidemiological cohort of 636 first-episode patients. Schizophr Res. (2007) 95:1–8. doi: 10.1016/j.schres.2007.06.004
7. Amminger GP, Henry LP, Harrigan SM, Harris MG, Alvarez-Jimenez M, Herrman H, et al. Outcome in early-onset schizophrenia revisited: findings from the early psychosis prevention and intervention centre long-term follow-up study. Schizophr Res. (2011) 131:112–9. doi: 10.1016/j.schres.2011.06.009
8. Sham PC, MacLean CJ, Kendler KS. A typological model of schizophrenia based on age at onset, sex and familial morbidity. Acta Psychiatr Scand. (1994) 89:135–41. doi: 10.1111/j.1600-0447.1994.tb01501.x
9. Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry. (2020) 77:155–64. doi: 10.1001/jamapsychiatry.2019.3523
10. Loranger AW. Sex difference in age at onset of schizophrenia. Arch Gen Psychiatry. (1984) 41:157–61. doi: 10.1001/archpsyc.1984.01790130053007
11. Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. (2008) 65:28–37. doi: 10.1001/archgenpsychiatry.2007.3
12. Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. (2012) 69:220–9. doi: 10.1001/archgenpsychiatry.2011.1472
13. Pontillo M, Tata MC, Averna R, Gargiullo P, Guerrera S, Vicari S. Clinical profile, conversion rate, and suicidal thinking and behaviour in children and adolescents at ultra-high risk for psychosis: a theoretical perspective. Res Psychother. (2020) 23:455. doi: 10.4081/ripppo.2020.455
14. Pontillo M, Averna R, Tata MC, Chieppa F, Pucciarini ML, Vicari S. Neurodevelopmental trajectories and clinical profiles in a sample of children and adolescents with early- and very-early-onset schizophrenia. Front Psychiatry. (2021) 12:662093. doi: 10.3389/fpsyt.2021.662093
15. Maj M, van Os J, De Hert M, Gaebel W, Galderisi S, Green MF, et al. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry. (2021) 20:4–33. doi: 10.1002/wps.20809
16. Penttil ä M, Jääskeläinen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. (2014) 205:88–94. doi: 10.1192/bjp.bp.113.127753
17. National Institute for Health Clinical Excellence (NICE): Guidance. Psychosis and Schizophrenia in Children and Young People: Recognition and Management. National Collaborating Centre for Mental Health (UK). Leicester: British Psychological Society (2013). Available online at: https://www.nice.org.uk/guidance/cg155 (accessed March 8, 2022).
18. Driver DI, Gogtay N, Rapoport JL. Childhood onset schizophrenia and early onset schizophrenia spectrum disorders. Child Adolesc Psychiatr Clin N Am. (2013) 22:539–55. doi: 10.1016/j.chc.2013.04.001
19. Driver DI, Thomas S, Gogtay N, Rapoport JL. Childhood-onset schizophrenia and early-onset schizophrenia spectrum disorders: an update. Child Adolesc Psychiatr Clin N Am. (2020) 29:71–90. doi: 10.1016/j.chc.2019.08.017
20. Hollis C. Adolescent schizophrenia. Adv Psychiatr Treat. (2000) 6:83–92. doi: 10.1192/apt.6.2.83
21. Hollis, C, Birchwood, M, Garralda, E, James, A, McDougall, T, Morrison, A,. Psychosis and Schizophrenia in Children and Young People: Evidence Update March 2015: A Summary of Selected New Evidence Relevant to NICE Clinical Guideline 155 ‘Psychosis and Schizophrenia in Children and Young People: Recognition and Management'. London: National Institute for Health and Care Excellence. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK552055/ (accessed March 8, 2022).
22. Newton R, Rouleau A, Nylander AG, Loze JY, Resemann HK, Steeves S, et al. Diverse definitions of the early course of schizophrenia-a targeted literature review. NPJ Schizophr. (2018) 4:21. doi: 10.1038/s41537-018-0063-7
23. Werry JS. Child and adolescent (early onset) schizophrenia: a review in light of DSM-III-R. J Autism Dev Disord. (1992) 22:601–24. doi: 10.1007/BF01046330
24. Remschmidt H, Theisen F. Early-onset schizophrenia1. Neuropsychobiology. (2012) 66:63–9. doi: 10.1159/000338548
25. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5h edition. DSM-5. Washington, DC: American Psychiatric Association (2013).
26. WHO. The ICD-10 Classification of Mental and Behavioural Disorders. Genève: World Health Organization (1993).
27. McClellan J, Stock S. Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. J Am Acad Child Adolesc Psychiatry. (2013) 52:976–90. doi: 10.1016/j.jaac.2013.02.008
28. Hollis C. Child and adolescent (juvenile onset) schizophrenia. A case control study of premorbid developmental impairments. Br J Psychiatry. (1995) 166:489–95. doi: 10.1192/bjp.166.4.489
29. De Berardis D, De Filippis S, Masi G, Vicari S, Zuddas A. A neurodevelopment approach for a transitional model of early onset schizophrenia. Brain Sci. (2021) 11:275. doi: 10.3390/brainsci11020275
30. Stentebjerg-Olesen M, Pagsberg AK, Fink-Jensen A, Correll CU, Jeppesen P. Clinical characteristics and predictors of outcome of schizophrenia-spectrum psychosis in children and adolescents: a systematic review. J Child Adolesc Psychopharmacol. (2016) 26:410–27. doi: 10.1089/cap.2015.0097
31. Frangou S. Cognitive function in early onset schizophrenia: a selective review. Front Hum Neurosci. (2010) 3:79. doi: 10.3389/neuro.09.079.2009
32. Harvey PD, Isner EC. Cognition, social cognition, and functional capacity in early-onset schizophrenia. Child Adolesc Psychiatr Clin N Am. (2020) 29:171–82. doi: 10.1016/j.chc.2019.08.008
33. Kravariti E, Morris RG, Rabe-Hesketh S, Murray RM, Frangou S. The Maudsley early-onset schizophrenia study: cognitive function in adolescent-onset schizophrenia. Schizophr Res. (2003) 65:95–103. doi: 10.1016/S0920-9964(03)00067-7
34. Vita A, Barlati S, De Peri L, Deste G, Sacchetti E. Schizophrenia. Lancet. (2016) 388:1280. doi: 10.1016/S0140-6736(16)31674-9
35. Vita A, Barlati S. Recovery from schizophrenia: is it possible? Curr Opin Psychiatry. (2018) 31:246–55. doi: 10.1097/YCO.0000000000000407
36. Vyas NS, Patel NH, Puri BK. Neurobiology and phenotypic expression in early onset schizophrenia. Early Interv Psychiatry. (2011) 5:3–14. doi: 10.1111/j.1751-7893.2010.00253.x
37. Díaz-Caneja CM, Pina-Camacho L, Rodríguez-Quiroga A, Fraguas D, Parellada M, Arango C. Predictors of outcome in early-onset psychosis: a systematic review. NPJ Schizophr. (2015) 1:14005. doi: 10.1038/npjschz.2014.5
38. Coulon N, Godin O, Bulzacka E, Dubertret C, Mallet J, Fond G, et al. Early and very early-onset schizophrenia compared with adult-onset schizophrenia: French FACE-SZ database. Brain Behav. (2020) 10:e01495. doi: 10.1002/brb3.1495
39. Grover S, Avasthi A. Clinical practice guidelines for the management of schizophrenia in children and adolescents. Indian Psychiatry J. (2019) 61:277–93. doi: 10.4103/psychiatry.IndianJPsychiatry_556_18
40. Kumra S, Oberstar JV, Sikich L, Findling RL, McClellan JM, Vinogradov S, et al. Efficacy and tolerability of second-generation antipsychotics in children and adolescents with schizophrenia. Schizophr Bull. (2008) 34:60–71. doi: 10.1093/schbul/sbm109
41. Lee ES, Kronsberg H, Findling RL. Psychopharmacologic treatment of schizophrenia in adolescents and children. Child Adolesc Psychiatr Clin N Am. (2020) 29:183–210. doi: 10.1016/j.chc.2019.08.009
42. Christian R, Saavedra, L, Gaynes, BN, Sheitman, B, Wines, RCM, Jonas, DE,. Future Research Needs for First- Second-Generation Antipsychotics for Children Young Adults Rockville, MD: Agency for Healthcare Research Quality (US) (Future Research Needs Papers, No. 13) (2012). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK84660/ (accessed March 8, 2022).
43. Correll CU, Findling RL, Tocco M, Pikalov A, Deng L, Goldman R. Safety and effectiveness of lurasidone in adolescents with schizophrenia: results of a 2-year, open-label extension study. CNS Spectr. (2022) 1:118–28. doi: 10.1017/S1092852920001893
44. Krause M, Zhu Y, Huhn M, Schneider-Thoma J, Bighelli I, Chaimani A, et al. Efficacy, acceptability, and tolerability of antipsychotics in children and adolescents with schizophrenia: a network meta-analysis. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol. (2018) 28:659–74. doi: 10.1016/j.euroneuro.2018.03.008
45. Gogtay N, Rapoport J. Clozapine use in children and adolescents. Expert Opin Pharmacother. (2008) 9:459–65. doi: 10.1517/14656566.9.3.459
46. Correll CU, Penzner JB, Parikh UH, Mughal T, Javed T, Carbon M, et al. Recognizing and monitoring adverse events of second-generation antipsychotics in children and adolescents. Child Adolesc Psychiatr Clin N Am. (2006) 15:177–206. doi: 10.1016/j.chc.2005.08.007
47. Solmi M, Fornaro M, Ostinelli EG, Zangani C, Croatto G, Monaco F, et al. Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects. World Psychiatry. (2020) 19:214–32. doi: 10.1002/wps.20765
48. Pagsberg AK, Tarp S, Glintborg D, Stenstrøm AD, Fink-Jensen A, Correll CU, et al. Acute antipsychotic treatment of children and adolescents with schizophrenia-spectrum disorders: a systematic review and network meta-analysis. J Am Acad Child Adolesc Psychiatry. (2017) 56:191–202. doi: 10.1016/j.jaac.2016.12.013
49. Olfson M, Gerhard T, Huang C, Lieberman JA, Bobo WV, Crystal S. Comparative effectiveness of second-generation antipsychotic medications in early-onset schizophrenia. Schizophr Bull. (2012) 38:845–53. doi: 10.1093/schbul/sbq172
50. Sikich L, Frazier JA, McClellan J, Findling RL, Vitiello B, Ritz L, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. (2008) 165:1420–31. doi: 10.1176/appi.ajp.2008.08050756
51. Arango C, Ng-Mak D, Finn E, Byrne A, Loebel A. Lurasidone compared to other atypical antipsychotic monotherapies for adolescent schizophrenia: a systematic literature review and network meta-analysis. Eur Child Adolesc Psychiatry. (2020) 29:1195–205. doi: 10.1007/s00787-019-01425-2
52. Kendall T, Hollis C, Stafford M, Taylor C. Guideline Development Group. Recognition and management of psychosis and schizophrenia in children and young people: summary of NICE guidance. BMJ. (2013) 23:346:f150. doi: 10.1136/bmj.f150
53. Barlati S, De Peri L, Deste G, Fusar-Poli P, Vita A. Cognitive remediation in the early course of schizophrenia: a critical review. Curr Pharm Des. (2012) 18:534–41. doi: 10.2174/138161212799316091
54. Müller H, Kommescher M, Güttgemanns J, Wessels H, Walger P, Lehmkuhl G, et al. Cognitive behavioral therapy in adolescents with early-onset psychosis: a randomized controlled pilot study. Eur Child Adolesc Psychiatry. (2020) 29:1011–22. doi: 10.1007/s00787-019-01415-4
55. Rund BR, Moe L, Sollien T, Fjell A, Borchgrevink T, Hallert M, et al. The psychosis project: outcome and cost-effectiveness of a psychoeducational treatment programme for schizophrenic adolescents. Acta Psychiatr Scand. (1994) 89:211–8. doi: 10.1111/j.1600-0447.1994.tb08094.x
56. Calvo A, Moreno M, Ruiz-Sancho A, Rapado-Castro M, Moreno C, Sánchez-Gutiérrez T, et al. Intervention for adolescents with early-onset psychosis and their families: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2014) 53:688–96. doi: 10.1016/j.jaac.2014.04.004
57. Addington J, Coldham EL, Jones B, Ko T, Addington D. The first episode of psychosis: the experience of relatives. Acta Psychiatr Scand. (2003) 108:285–9. doi: 10.1034/j.1600-0447.2003.00153.x
58. Claxton M, Onwumere J, Fornells-Ambrojo M. Do family interventions improve outcomes in early psychosis? A systematic review and meta-analysis. Front Psychol. (2017) 8:371. doi: 10.3389/fpsyg.2017.00371
59. Signorini G, Singh SP, Marsanic VB, Dieleman G, Dodig-Curkovi ć K, et al. The interface between child/adolescent and adult mental health services: results from a European 28-country survey. Eur Child A dolesc Psychiatry. (2018) 27:501–11. doi: 10.1007/s00787-018-1112-5
60. National Action Plan for Mental Health Manifesto. (2013). Available online at: https://www.salute.gov.it (accessed March 8, 2022).
61. Fusar-Poli P, Minichino A, Brambilla P, Raballo A, Bertolino A, Borgatti R, et al. ITAlian partnership for psychosis prevention (ITAPP): improving the mental health of young people. Eur Psychiatry. (2021) 64:e62. doi: 10.1192/j.eurpsy.2021.2232
62. Giannarou L, Zervas E. Using Delphi technique to build consensus in practice. Int J Bus Sci Appl Manage. (2014) 9:65–82.
63. Jorm AF. Using the Delphi expert consensus method in mental health research. Aust N Z J Psychiatry. (2015) 49:887–97. doi: 10.1177/0004867415600891
64. Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. (2016) 173:362–72. doi: 10.1176/appi.ajp.2015.15050632
65. Parabiaghi A, Confalonieri L, Magnani N, Lora A, Butteri E, Prato K, et al. Integrated programs for early recognition of severe mental disorders: recommendations from an italian multicenter project. Front Psychiatry. (2019) 10:844. doi: 10.3389/fpsyt.2019.00844
66. Mohr P, Galderisi S, Boyer P, Wasserman D, Arteel P, Ieven A, et al. Value of schizophrenia treatment I: the patient journey. Eur Psychiatry. (2018) 53:107–15. doi: 10.1016/j.eurpsy.2018.06.007
67. Tandon R, Lenderking WR, Weiss C, Shalhoub H, Barbosa CD, Chen J, et al. The impact on functioning of second-generation antipsychotic medication side effects for patients with schizophrenia: a worldwide, cross-sectional, web-based survey. Ann Gen Psychiatry. (2020) 19:42. doi: 10.1186/s12991-020-00292-5
68. Bernardo M, Vieta E, Saiz Ruiz J, Rico-Villademoros F, Alamo C, Bobes J, et al. Recommendations for switching antipsychotics. A position statement of the Spanish Society of Psychiatry and the Spanish Society of Biological Psychiatry. Rev Psiquiatr Salud Ment. (2011) 4:150–168. doi: 10.1016/j.rpsm.2011.07.003
69. Thomas SP, Nandhra HS, Singh SP. Pharmacologic treatment of first-episode schizophrenia: a review of the literature. Prim Care Comp CNS Disord. (2012) 14:PCC.11r01198. doi: 10.4088/PCC.11r01198
70. National Institute for Health and Clinical Excellence (NICE). Psychosis and Schizophrenia in Children and Young People: Recognition and Management. London: National Institute for Health and Care Excellence (2016).
71. Crespo-Facorro B, Pelayo-Teran JM, Mayoral-van Son J. Current data on and clinical insights into the treatment of first episode nonaffective psychosis: a comprehensive review. Neurol Ther. (2016) 5:105–30. doi: 10.1007/s40120-016-0050-8
72. Keating D, McWilliams S, Schneider I, Hynes C, Cousins G, Strawbridge J, et al. Pharmacological guidelines for schizophrenia: a systematic review and comparison of recommendations for the first episode. BMJ Open. (2017) 7:e013881. doi: 10.1136/bmjopen-2016-013881
73. Kishi T, Ikuta T, Matsui Y, Inada K, Matsuda Y, Mishima K, et al. Effect of discontinuation v. maintenance of antipsychotic medication on relapse rates in patients with remitted/stable first-episode psychosis: a meta-analysis. Psychol Med. (2019) 49:772–779. doi: 10.1017/S0033291718001393
74. Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, et al. Should psychiatrists be more cautious about the long-term prophylactic use of antipsychotics? Br J Psychiatry. (2016) 209:361–5. doi: 10.1192/bjp.bp.116.182683
75. Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. (2018) 75:555–65. doi: 10.1001/jamapsychiatry.2018.0623
76. Bighelli I, Rodolico A, García-Mieres H, Pitschel-Walz G, Hansen WP, Schneider-Thoma J, et al. Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis. Lancet Psychiatry. (2021) 8:969–80. doi: 10.1016/S2215-0366(21)00243-1
77. Nibbio G, Barlati S, Cacciani P, Corsini P, Mosca A, Ceraso A, et al. Evidence-based integrated intervention in patients with schizophrenia: a pilot study of feasibility and effectiveness in a real-world rehabilitation setting. Int J Environ Res Public Health. (2020) 17:3352. doi: 10.3390/ijerph17103352
78. Vita A, Barlati S, Ceraso A, Nibbio G, Ariu C, Deste G, et al. Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. (2021) 78:848–58. doi: 10.1001/jamapsychiatry.2021.0620
79. Vita A, Barlati S. The implementation of evidence-based psychiatric rehabilitation: challenges and opportunities for mental health services. Front Psychiatry. (2019) 10:147. doi: 10.3389/fpsyt.2019.00147
80. Daruvala R, Kumar A, Datta SS. Do psychological interventions work for psychosis in adolescents? Schizophr Bull. (2021) 47:692–94. doi: 10.1093/schbul/sbaa132
81. Breitborde NJ, Woods SW, Srihari VH. Multifamily psychoeducation for first-episode psychosis: a cost-effectiveness analysis. Psychiatr Serv. (2009) 60:1477–83. doi: 10.1176/ps.2009.60.11.1477
Keywords: adolescent schizophrenia, Delphi method, early diagnosis, expert consensus, pattern of care, treatment gaps
Citation: Vita A, Barlati S, Bellomo A, Poli PF, Masi G, Nobili L, Serafini G, Zuddas A and Vicari S (2022) Patterns of Care for Adolescent With Schizophrenia: A Delphi-Based Consensus Study. Front. Psychiatry 13:844098. doi: 10.3389/fpsyt.2022.844098
Received: 27 December 2021; Accepted: 08 March 2022;
Published: 30 March 2022.
Edited by:
Veit Roessner, University Hospital Carl Gustav Carus, Dresden, GermanyReviewed by:
Paola Rocca, University of Turin, ItalyFilip Rybakowski, Poznan University of Medical Sciences, Poland
Copyright © 2022 Vita, Barlati, Bellomo, Poli, Masi, Nobili, Serafini, Zuddas and Vicari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stefano Barlati, c3RlZmFuby5iYXJsYXRpQHVuaWJzLml0
 Antonio Vita
Antonio Vita Stefano Barlati
Stefano Barlati Antonello Bellomo2
Antonello Bellomo2 Paolo Fusar Poli
Paolo Fusar Poli Gabriele Masi
Gabriele Masi Lino Nobili
Lino Nobili Gianluca Serafini
Gianluca Serafini