
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 18 March 2022
Sec. Sleep Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.841097
This article is part of the Research Topic Assessing and Evaluating the Impact Of The Covid 19 Pandemic on Anxiety And Stress: A Global Perspective View all 16 articles
Background: Women’s ability to get sleep can be affected by pregnancy-related hormonal changes or other external stressful situations like the coronavirus disease 2019 (COVID-19).
Objective: The objective of this study was to assess the proportion of poor sleep quality during the COVID-19 pandemic and its determinants among pregnant women attending antenatal care (ANC) services.
Methods: An institutional-based cross-sectional study was conducted among 423 women attending ANC services at the health facilities in Debre Berhan Town, Ethiopia, from May to June 2020. A systematic random sampling technique was used to select the required samples. The tool consisted of questions that assessed (1) socio-demographic characteristics, obstetric and health care service-related characteristics; and media exposure to get information regarding COVID-19 infection; (2) To assess sleep quality; the Pittsburgh Sleep Quality Index (PSQI) was applied. And a global score of >5 indicates poor sleep quality, and a global score of ≤5 indicates good sleep quality.
Result: The overall prevalence of poor sleep quality was 62.8%, and was associated with pregnant women aged ≥46 years (AOR = 4.27), being in the third trimester (AOR = 2.51), being multigravida (AOR = 2.72), and having co-morbidity (AOR = 3.57).
Conclusion: The prevalence of poor sleep quality among pregnant women during the pandemic was found to be high. Advanced maternal age, third trimester pregnancy, being multigravida, and having comorbidity were determinants of poor sleep quality among pregnant women during the COVID-19 pandemic.
Pregnancy is a process accompanied by dramatic hormonal changes (1–3) that create significant anatomical, physiological, and biochemical changes in a woman’s life. These hormonal changes can also have profound effects on women’s ability to sleep and may result in poor sleep quality (4–7). Sleep is a physiological process and a basic requirement for the physical and mental well-being of pregnant women and their fetuses (2, 8). Furthermore, sleep disturbances and short sleep duration are common during pregnancy (9, 10), which can have an impact on health-related quality of life. Although a sleep problem may start soon after conception, it worsens in frequency and duration as the pregnancy advances more (11).
Sleep has a critical role in promoting the health of both the mother and the fetus (12). Worldwide, approximately one-third of all pregnant women reported that they had disturbed sleep during pregnancy (13). Disturbed sleep during pregnancy is linked to several complications, including preeclampsia, pre-mature birth, gestational diabetes, postpartum depression, and intrauterine growth retardation (9, 13). Studies in different areas of the world reported that the prevalence of poor sleep quality among pregnant women was 17% in Peru (14), 41.2% in Vietnam (15), 43.1% in the Asian population (4), 45.7% in Canada (16), 51.8–87% in China (10, 11), 53.3% in Pakistan (17), 59.5% in Indonesia (18), 73% in the United States (1). Some studies showed the prevalence of poor sleep quality among pregnant women before the pandemic in Ethiopia at Jimma medical center 30.8% (8) and Wadila primary hospital 68.4% (2).
The determinants of poor sleep quality among pregnant women significantly varied with the trimester of the pregnancy. Overall, poor sleep quality had a direct correlation with advanced age, maternal education level, being unmarried, anxiety, depression, stress, gestational age, multiparous, multigravida, and watching television in the bedroom (2, 8, 10, 11, 15, 18). In addition, there are also many external stressful situations, like the coronavirus disease 2019 (COVID-19), which can result in disturbed sleep during pregnancy.
Studies reported that COVID-19 harmed sleep quality in the general populations (19–21). This problem may become worsen in pregnant women. The global pandemic COVID-19 infection has been shown to have an important impact on pregnant women and their fetuses. Pregnant women may experience fear of contracting COVID-19 (22) and its consequences, which can result in anxiety, depression, stress, and insomnia (23, 24). Additionally, pregnant women encountered partial immune suppression and became more susceptible to COVID-19 infection during the pandemic (25). All of this can lead to the development of negative emotions and cause pregnant women to be more concerned about the COVID-19 infection, resulting in sleep disruption (12) and poor sleep quality (26).
COVID-19 related morbidity and mortality are shockingly increasing in Ethiopia. This phenomenon may create stressful situations, especially for those at high risk, like pregnant women. Consequently, this COVID-19-related negative emotion among pregnant women could result in difficulty in getting sleep. However, there are limited studies done regarding sleep quality among pregnant women during the COVID-19 pandemic in Ethiopia. So, this study aimed to assess the prevalence of poor sleep quality and its determinant factors among pregnant women attending antenatal care (ANC) services during the era of the COVID-19 pandemic at Debre Berhan Town, Ethiopia in 2020.
An institutional-based cross-sectional study was conducted from May 1 to June 1, 2020, in Debre Berhan Town public health institutions. The source populations for the study were all pregnant women who are attending antenatal care services in Debre Berhan town. All pregnant women who are attending antenatal care services in the Town during the study period and fulfill the inclusion criteria were included as the study population. The sample size was determined by using the single population proportion formula with the assumption of 50% poor sleep quality, a 95% confidence interval, and a 5% marginal error. After adding a 10% non-response rate, the final sample size was 423. In this study, pregnant women who visited the public health institutions in Debre Berhan Town for ANC services were included in the study. And pregnant women who were unable to communicate effectively due to serious illness were excluded from the study. To select our study participants, all public health facilities in Debre Berhan town were considered, and then based on the number of pregnant women that visited the public health facilities during the preceding month before data collection, proportional allocation of the total sample size was carried out to get the required sample from each public health facility. Finally, the determined samples were selected with a mean age of 28 years (SD ± 4.86) by a systematic random sampling technique.
Pretested and interviewer-administered questionnaires were used for the whole survey. The tool consisted of 33 items categorized in to two sections, (1) socio-demographic characteristics, obstetric and health care service-related characteristics; and media exposure to get information regarding COVID-19 infection with a total of 14 items; (2) items to assess sleep quality by the Pittsburgh Sleep Quality Index (PSQI). The Pittsburgh Sleep Quality Index contains 19 Likert-type and open-ended questions. Respondents were asked about their overall sleep quality and how frequently they had experienced certain sleep difficulties in the previous month. The 19 items were combined to form seven component scores, each of which had a range of 0–3, with a higher score indicating more acute sleep disturbances. Then, the seven component scores were added to yield a single global score ranging from 0 to 21, with the higher score indicating severe sleep difficulties in all areas. PSQI developers have suggested a cutoff score of 5 for the global scale as it was 88.5% valid to correctly identify the problem (27–29). The Cronbach alpha of PSQI in the current study was 0.72. Furthermore, the data was collected by trained BSc midwives, and the consistency and completeness of the data were checked daily by supervisors.
Is defined based on the PSQI score; hence, a global score of >5 indicates poor sleep quality, and a global score of ≤5 indicates good sleep quality (27).
Women who had access to either television, radio, or read newspapers at least once a week was considered exposed to the media.
Is defined as the co-existence of diagnosed chronic medical conditions like asthma, diabetes mellitus, heart disease, hypertension, depression, cancer, and chronic kidney disease among pregnant women (30).
The data was first entered into EPI INFO™ 7 and then exported to STATA version 14, statistical software for analysis. Frequencies and cross-tabulations were applied to summarize descriptive statistics of the data, and tables were used for data presentation. A binary logistic regression model was used to identify factors associated with poor sleep quality. Those variables with a p-value less than or equal to 0.2 from the bi-variable analysis were candidates for multivariable analysis. Variables with a p-value of less than 0.05 in multivariable analysis were declared as statistically significant factors for poor sleep quality. Moreover, the association was measured using odds ratios with a 95% confidence interval. Model fitness was also checked by the Hosmer-Lemeshow goodness of fit test (P-value = 0.491).
This study was approved by the Institutional Review Board (IRB) of Debre Berhan University and an official permission letter was gained from the concerned body. Written informed consent was obtained from each participant before conducting the actual data collection process. Additionally, confidentiality was maintained by avoiding registration of personal identifiers and no raw data was given to anyone other than the investigator.
Of the 423 pregnant women, almost all (99.8%) participated in the analysis. Of these, 175 (41.47%) were found under the category of age 25 years or less, with a mean age of 28 years (SD ± 4.86). The majority (86.73%) of the participants were married, and 164 (38.86%) of the women had primary education levels. Of all the participants included in the analysis, 241 (57.11%) were housewives. About one-third (34.36%) of the participants’ husbands were at the primary education level, and 216 (51.18%) of their husbands were merchants. One hundred ninety-four (46%) pregnant women lived 2–5 km away from the health facility. Similarly, more than half (54.5%) of the participants were in the third trimester and 250 (59.24%) were multi-gravida. On the other hand, the majority of the women (89.8%) had no known co-morbid diseases. Around 81.5 and 57.4% of the women watched television and heard the radio to get information, including COVID-19, respectively. But, the majority of the women (90.52%) didn’t have the habit of reading newspapers during the era of the pandemic (Table 1).
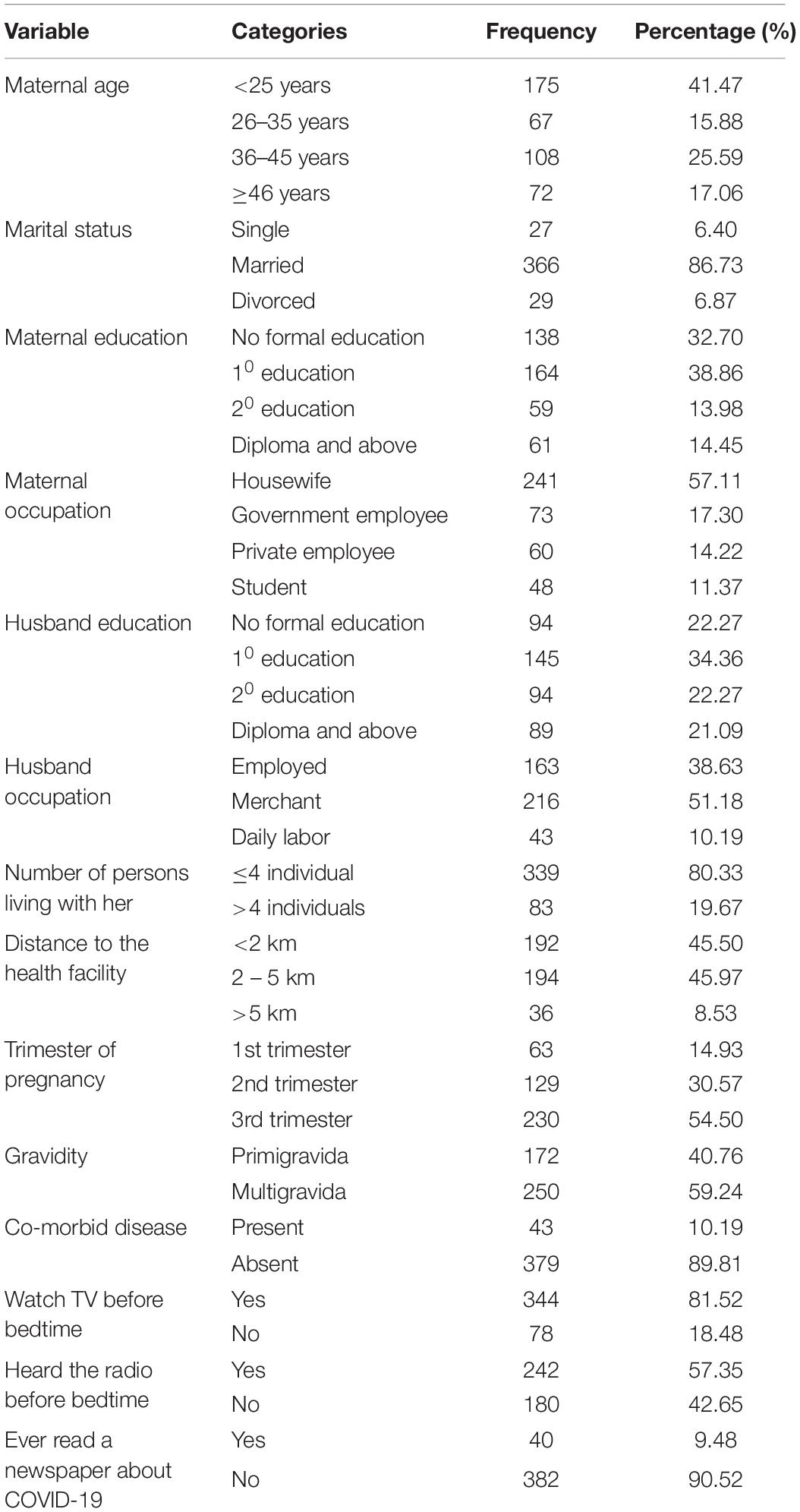
Table 1. The socio-demographic and obstetric-related characteristics of pregnant women attending antenatal care (ANC) services in Debre Berhan (n = 422).
The overall prevalence of poor sleep quality among pregnant women attending ANC service at health facilities in Debre Berhan town was 62.8% (95% CI: 58.1–67.3). The prevalence of poor sleep quality among pregnant women increases with gestational age, showing the highest proportion in the third trimester (Figure 1).
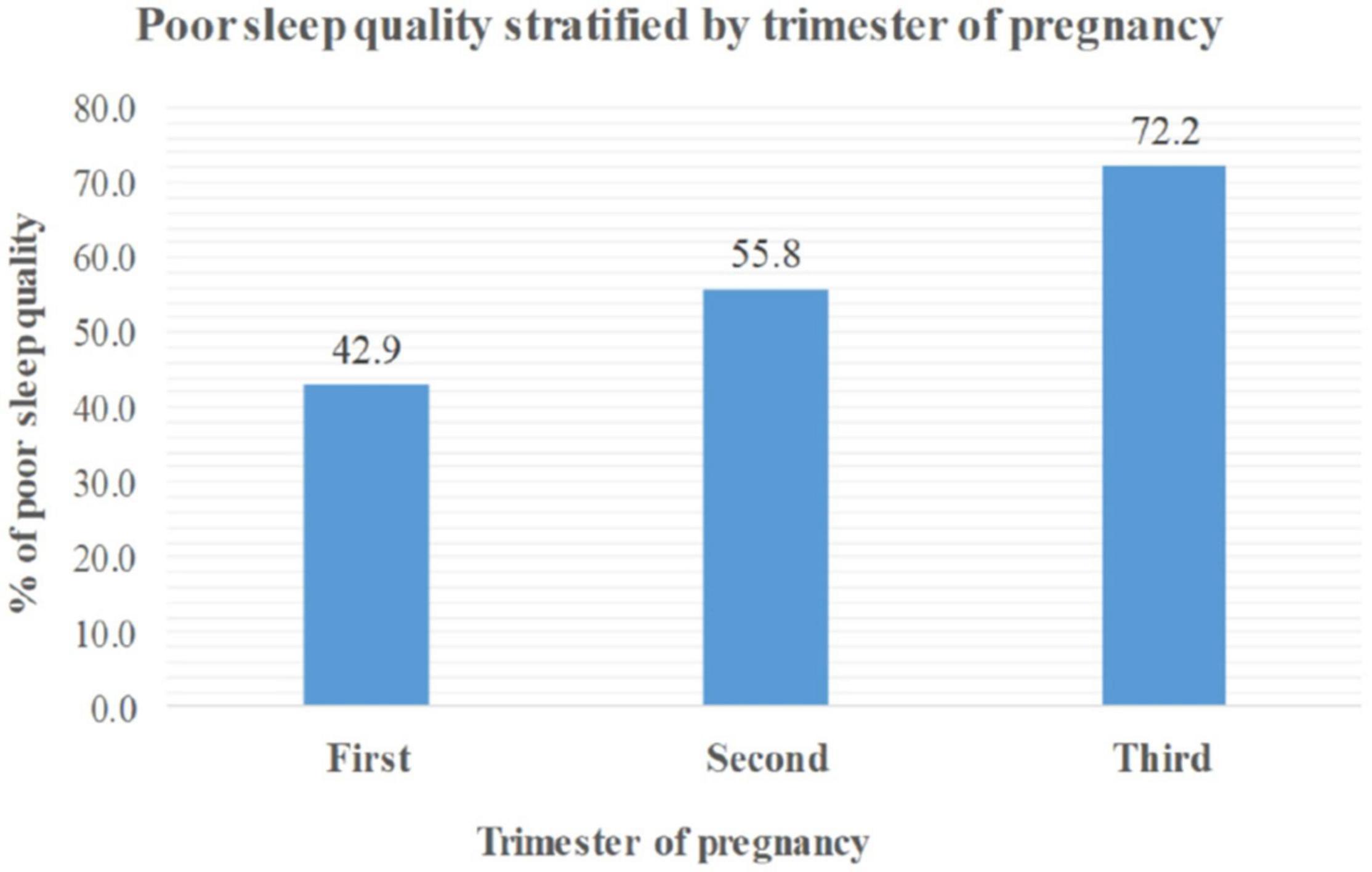
Figure 1. Poor sleep quality among pregnant women stratified by trimester at Debre Berhan town, Ethiopia, 2020.
After applying multivariable binary logistic regression, four variables, namely maternal age, trimester of pregnancy, gravidity, and presence of co-morbidity, were significantly associated with poor sleep quality among pregnant women. Thus, the odds of having poor sleep quality among pregnant women aged ≥46 years was 4.27 times that of women aged less than 25 years [AOR = 4.27; 95% CI: 1.43–12.79]. Similarly, the likelihood of experiencing poor sleep quality was 2.51 times higher in the third trimester compared to the first trimester [AOR = 2.51; 95% CI: 1.175–42]. Likewise, multigravida women were 2.72 times more likely than primigravida women to have poor sleep quality [AOR = 2.72; 95% CI: 1.34–5.50]. Pregnant women with the co-morbid disease were 3.57 times more likely to have poor sleep quality than pregnant women without comorbidity [AOR = 3.57; 95% CI: 1.45–8.78] (Table 2).
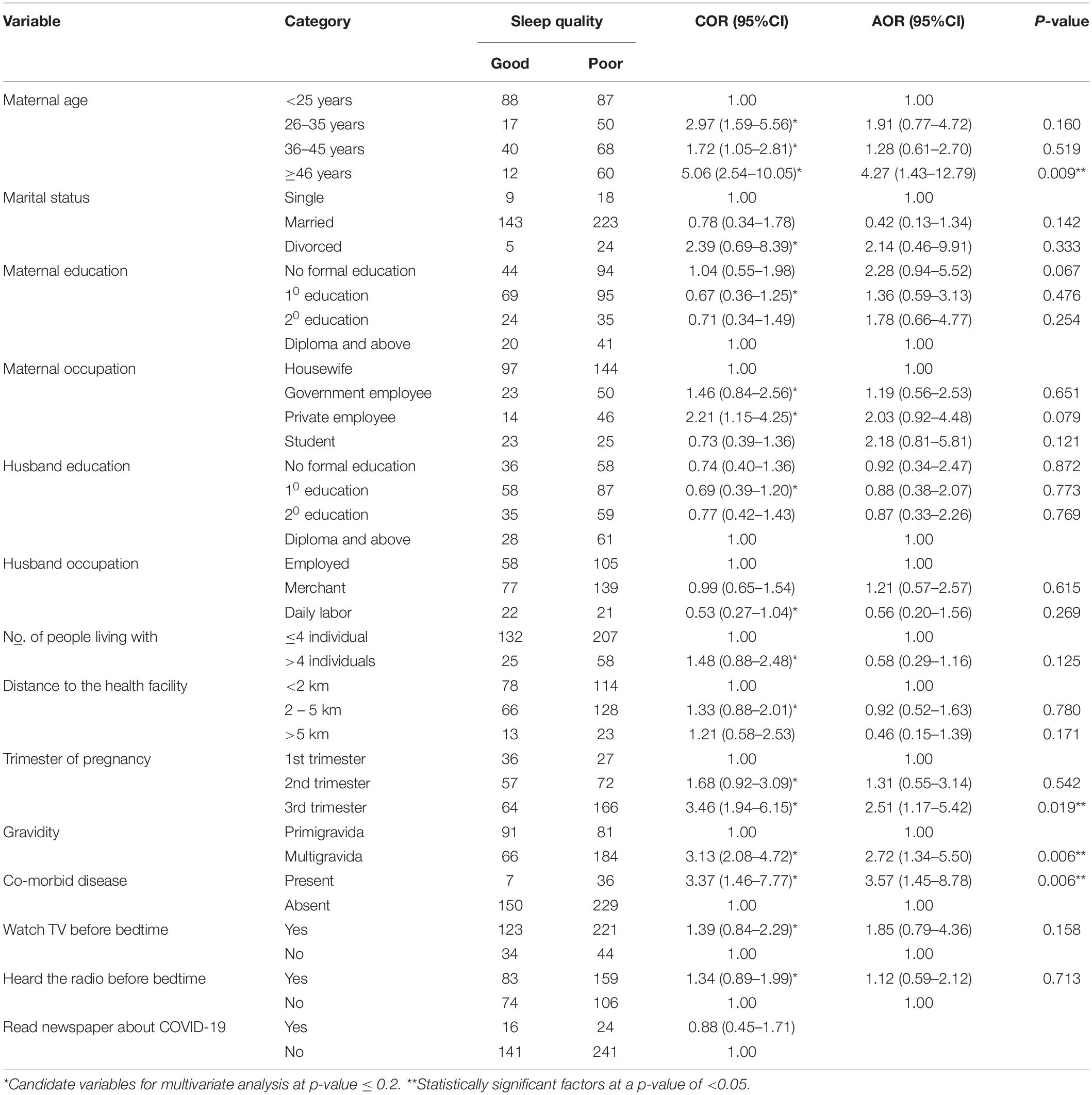
Table 2. Bivariate and multivariate sleep quality analysis among pregnant women in Debre Berhan (n = 422).
In this study, the overall magnitude of poor sleep quality among pregnant women during the era of COVID-19 was 62.8% (95% CI: 58.1–67.3). This is in line with studies conducted in Indonesia (59.5%) (18) and Northern Ethiopia (68.4%) (2). But, the magnitude of poor sleep quality in the current study was lower than in studies conducted in Turkey (88%) (26), China (87%) (11), and the United States (73%) (1). The discrepancy might be due to differences in socio-demographic characteristics and in the time when the study was conducted. On the other hand, poor sleep quality in the current study was higher than in studies from Peru, China, Pakistan, Vietnam, the Asian population, and Canada, ranging from 17 to 53.3% (4, 10, 14–17, 31, 32). The majority of these previous studies were conducted before the outbreak of the global COVID-19 pandemic, so the women couldn’t worry about the infection compared to the women in the current study. Furthermore, being quarantined and apart from loved ones during the COVID-19 pandemic might increase the proportion of depressive symptoms, stress, and anxiety. These psychological situations in turn affect the sleep quality of pregnant women (18, 33).
The odds of having poor sleep quality were 4.27 times higher in pregnant women aged 46 years and older than in women aged less than 25 years. This is supported by studies from China (11), and Ethiopia (2, 8). As maternal age increases, the likelihood of women being affected by physiological and psychological factors will also increase (34). This might in turn result in poor sleep quality (35).
Similarly, a significant association between gestational age and sleep quality was detected, showing that sleep quality declines as pregnancy advances. Hence, the risk of developing poor sleep quality among pregnant women in the third trimester was 2.51 times greater than that of pregnant women in the first trimester. This is consistent with studies from China (10, 11), Turkey (36), and Ethiopia (2). As gestational age increases, the tendency for frequent urination, even at night, increases and results in disturbed sleep (37). Additionally, when the woman approaches her end date of delivery, she might worry about childbirth, finance, labor, and delivery, or the baby’s health, which all could be risk factors for disturbed sleep (37, 38). Weight gain, along with hormonal and physiological changes, induces pregnant women to have sleep-disordered breathing like snoring and obstructive sleep apnea, which in turn disturbs the normal sleep pattern (38).
A significant association between gravidity and sleep quality was discovered, showing that sleep quality declines as the number of pregnancies increases. When compared to primigravida, the likelihood of having poor sleep quality was 2.72 times among women with multigravida. This is consistent with research on pregnant women in Jimma, Ethiopia (8), and South Korea (39). This may be explained by the fact that maternal sleep quality is disturbed as a result of being overstressed about bearing extra roles after childbirth and the way they integrate the new role into their pre-existing responsibilities. Excessive worry caused by rehearsing physical pain during labor and delivery may also contribute to poor sleep quality in multigravida women (39).
Lastly, the presence of co-morbid disease among pregnant women was found to be significantly associated with poor sleep quality. Hence, pregnant women with co-morbid disease were 3.57 times more likely to develop poor sleep quality compared to pregnant women without comorbidity. This is supported by studies from Indonesia and the United States which declared that depression and gestational diabetes mellitus were directly associated with poor sleep quality (1, 18), respectively. This could be a reason for extra worry among pregnant women with medical comorbidity, which might induce a disturbed sleep pattern. Additionally, fear of a bad outcome for her baby and her as a result of existing comorbidity may contribute to the occurrence of poor sleep quality.
Nearly two-thirds of pregnant women in this study had poor sleep quality. Women with advanced age, being in the third trimester, multigravida, and comorbidity were associated with poor sleep quality among pregnant women. Giving special attention to women of advanced age, third trimester pregnancy, multigravida, and counseling of the women with comorbidity in their consecutive antenatal care visits is crucial to reduce the risk of developing poor sleep quality and its consequences.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Debre Berhan University College of Health Science research committee. The patients/participants provided their written informed consent to participate in this study.
NA conceived the idea, designed the work, and collected the data. BC collected the data and participated in the manuscript writing. AA analyzed the data, interpreted the results, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to acknowledge the pregnant women and healthcare workers for their collaboration during the data collection. Also, the authors’ heartfelt thank go to the Debre Berhan University for providing ethical clearance to conduct the study.
1. Chirwa S, Nwabuisi CR, Ladson GM, Korley L, Whitty JE, Atkinson R, et al. Poor sleep quality is associated with higher hemoglobin A1c in pregnant women: a pilot observational study. Int J Environ Res Public Health. (2018) 15:2287. doi: 10.3390/ijerph15102287
2. Jemere T, Getahun B, Tadele F, Kefale B, Walle G. Poor sleep quality and its associated factors among pregnant women in Northern Ethiopia, 2020: a cross sectional study. PLoS One. (2021) 16:e0250985. doi: 10.1371/journal.pone.0250985
3. Hung H-M, Tsai P-S, Ko S-H, Chen C-H. Patterns and predictors of sleep quality in Taiwanese pregnant women. MCN Am J Mater Child Nurs. (2013) 38:95–101. doi: 10.1097/NMC.0b013e3182659345
4. Cai S, Tan S, Gluckman PD, Godfrey KM, Saw S-M, Teoh OH, et al. Sleep quality and nocturnal sleep duration in pregnancy and risk of gestational diabetes mellitus. Sleep. (2017) 40:zsw058. doi: 10.1093/sleep/zsw058
5. Reshadat S, Zakiei A, Karami J, Ahmadi E. A study of the psychological and family factors associated with sleep quality among pregnant women. Sleep Hypnosis. (2018) 20:17–24.
6. Peters B. How Sleep Changes During Pregnancy. Hormones, Problems, and the Best Positions. (2020). Available online at: https://www.verywellhealth.com/sleep-in-pregnancy-3015077 (accessed October 29, 2021).
8. Anbesaw T, Abebe H, Kassaw C, Bete T, Molla A. Sleep quality and associated factors among pregnant women attending antenatal care at Jimma medical center, Jimma, Southwest Ethiopia, 2020: cross-sectional study. BMC Psychiatry. (2021) 21:469. doi: 10.1186/s12888-021-03483-w
9. Kay-Stacey M, Attarian HP. Managing sleep disorders during pregnancy. Gender Genome. (2017) 1:34–45. doi: 10.1089/gg.2016.0006
10. Zhang H, Li P, Fan D, Wu S, Rao J, Lin D, et al. Prevalence of and risk factors for poor sleep during different trimesters of pregnancy among women in China: a cross-sectional study. Nat Sci Sleep. (2021) 13:811. doi: 10.2147/NSS.S303763
11. Yang Y, Mao J, Ye Z, Zeng X, Zhao H, Liu Y, et al. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J Mater Fetal Neonatal Med. (2018) 31:2980–5. doi: 10.1080/14767058.2017.1359831
12. Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Ann Rev Psychol. (2015) 66:143–72. doi: 10.1146/annurev-psych-010213-115205
13. Van Ravesteyn LM, Tulen JH, Kamperman AM, Raats ME, Schneider A, Birnie E, et al. Perceived sleep quality is worse than objective parameters of sleep in pregnant women with a mental disorder. J Clin Sleep Med. (2014) 10:1137–41. doi: 10.5664/jcsm.4118
14. Gelaye B, Addae G, Neway B, Larrabure-Torrealva GT, Qiu C, Stoner L, et al. Poor sleep quality, antepartum depression and suicidal ideation among pregnant women. J Affect Disord. (2017) 209:195–200. doi: 10.1016/j.jad.2016.11.020
16. Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. (2018) 38:168–76. doi: 10.1016/j.smrv.2017.06.005
17. Ahmed N, Khan A, Waseem A, Khan T, Shabbir H, Waqas A. Prevalence of sleep disturbances during pregnancy–a pilot study. BAOJ Gynaec. (2019) 2:1–8. doi: 10.1016/0002-9378(72)90091-9
18. Argo T, Kurniawan A, Liem J, Sugianto J, Michael R, Agatha L, et al. Association between depression, anxiety, and stress with sleep quality in Indonesian people during the COVID-19 pandemic. Public Health Indones. (2021) 7:58–66.
19. Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M, Pérez CA. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: a longitudinal study. Appetite. (2021) 158:105019. doi: 10.1016/j.appet.2020.105019
20. Pérez-Carbonell L, Meurling IJ, Wassermann D, Gnoni V, Leschziner G, Weighall A, et al. Impact of the novel coronavirus (COVID-19) pandemic on sleep. J Thorac Dis. (2020) 12(Suppl. 2):S163–75.
21. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. (2020) 29:e13074. doi: 10.1111/jsr.13074
22. Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. (2020) 62:370.
23. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
24. Mortensen CR, Becker DV, Ackerman JM, Neuberg SL, Kenrick DT. Infection breeds reticence: the effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychol Sci. (2010) 21:440–7. doi: 10.1177/0956797610361706
25. Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. (2020) 99:439–42. doi: 10.1111/aogs.13836
26. Alan S, Vurgec BA, Cevik A, Gozuyesil E, Surucu SG. The effects of COVID-19 pandemic on pregnant women: perceived stress, social support and sleep quality. Yonago Acta Med. (2020) 3:360–7. doi: 10.33160/yam.2020.11.016
27. Shahid A, Wilkinson K, Marcu S, Shapiro CM. Pittsburgh sleep quality index (PSQI). In: A Shahid, K Wilkinson, S Marcu, C Shapiro editors. STOP, That and One Hundred Other Sleep Scales. New York, NY: Springer (2011). p. 279–83.
28. Zhong Q-Y, Gelaye B, Sánchez SE, Williams MA. Psychometric properties of the Pittsburgh sleep quality index (PSQI) in a cohort of Peruvian pregnant women. J Clin Sleep Med. (2015) 11:869–77. doi: 10.5664/jcsm.4936
29. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
30. Schlichting LE, Insaf TZ, Zaidi AN, Lui GK, Van Zutphen AR. Maternal comorbidities and complications of delivery in pregnant women with congenital heart disease. J Am Coll Cardiol. (2019) 73:2181–91. doi: 10.1016/j.jacc.2019.01.069
31. Xu K, Zhang Y, Zhang Y, Xu Q, Lv L, Zhang J. Mental health among pregnant women under public health interventions during COVID-19 outbreak in Wuhan, China. Psychiatry Res. (2021) 301:113977. doi: 10.1016/j.psychres.2021.113977
32. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. (2020) 11:617001. doi: 10.3389/fpsyg.2020.617001
33. Lin W, Wu B, Chen B, Lai G, Huang S, Li S, et al. Sleep conditions associate with anxiety and depression symptoms among pregnant women during the epidemic of COVID-19 in Shenzhen. J Affect Disord. (2021) 281:567–73. doi: 10.1016/j.jad.2020.11.114
34. Qin C, Mi C, Xia A, Chen WT, Chen C, Li Y, et al. A first look at the effects of long inter-pregnancy interval and advanced maternal age on perinatal outcomes: a retrospective cohort study. Birth. (2017) 44:230–7. doi: 10.1111/birt.12289
35. Cao H. Influence of peer education on sleep quality of elderly parturient women. Modern Clin Nurs. (2014) 13:36–9.
36. Çolak S, Gürlek B, Önal Ö, Yılmaz B, Hocaoglu C. The level of depression, anxiety, and sleep quality in pregnancy during coronavirus disease 2019 pandemic. J Obstet Gynaecol Res. (2021) 47:2666–76. doi: 10.1111/jog.14872
37. Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. (2015) 16:483–8.
38. Shoen S. Sleep Tips for Pregnant Women. (2021). Available online at: https://www.sleepfoundation.org/pregnancy/tips-for-better-sleep (accessed June 15, 2021).
Keywords: COVID-19, sleep quality, women, Ethiopia, pregnancy
Citation: Amare NS, Chekol B and Aemro A (2022) Determinants of Poor Sleep Quality During the COVID-19 Pandemic Among Women Attending Antenatal Care Services at the Health Facilities of Debre Berhan Town, Ethiopia: An Institutional-Based Cross-Sectional Study. Front. Psychiatry 13:841097. doi: 10.3389/fpsyt.2022.841097
Received: 21 December 2021; Accepted: 15 February 2022;
Published: 18 March 2022.
Edited by:
Mehmet Y. Agargün, Yuzuncu Yil University, TurkeyReviewed by:
Nigussie Tadesse Sharew, University of Groningen, NetherlandsCopyright © 2022 Amare, Chekol and Aemro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nakachew Sewnet Amare, anVzdG5ha2FjaGV3QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.