
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 28 April 2022
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.839630
This article is part of the Research Topic Trauma, Psychosis, and Posttraumatic Stress Disorder, Volume II View all 8 articles
 Jie Zhao1
Jie Zhao1 Xiao-Hua Lu2
Xiao-Hua Lu2 Yuan Liu3
Yuan Liu3 Nan Wang4
Nan Wang4 Dong-Yang Chen1
Dong-Yang Chen1 Iun-An Lin1
Iun-An Lin1 Xiao-Hong Li1*
Xiao-Hong Li1* Fu-Chun Zhou1*
Fu-Chun Zhou1* Chuan-Yue Wang1*
Chuan-Yue Wang1*Objectives: Both bullying and psychosis-like experiences (PLEs) have gained much attention in recent years, but their interactions are not fully unraveled. The aim of the current study was to validate the Chinese version of Bullying Scale for Adults (C-BSA), and to investigate whether past bullying experiences independently predict the presence of PLEs in university students.
Methods: The validity and reliability of the C-BSA were determined in two independent samples. A battery of psychological inventories was also administered to assess the presence of PLEs, maltreatment history in the family, and current depression and anxiety, including the 15-item positive subscale of the community assessment of psychic experiences (CAPE-p15), the Chinese version of the Childhood Trauma Questionnaire (CTQ), Self-Rating Depression Scale (SDS), and Self-Rating Anxiety Scale (SAS).
Results: In the construction sample (N = 629), a Cronbach's α of 0.921 indicated a good internal consistency of C-BSA. The exploratory factor analysis (EFA) yielded a four-factor model and a three-factor model, and both were verified by using the confirmatory factorial analysis (CFA) in the validation sample (N = 629). The total scores of C-BSA were significantly correlated with that of CTQ, CAPE-p15, SDS, and SAS. Multivariate logistic regression revealed that bullying was associated with 2.0 or 3.7 times of risk for the presence of PLEs (numbers of bullying types < = 3 or > 3, respectively) after controlling for CTQ, SDS, and SAS scores.
Conclusions: C-BSA has shown good psychometric properties in college students. The contribution of past bullying experiences to the present PLEs seems to be independent of other childhood trauma, current depression, and anxiety.
It had been believed that psychosis was a categorical concept and a clear boundary existed between psychotic and Non-psychotic status. However, the conception of continua of human behaviors has received much attention in past years. The crucial role of both functional and dysfunctional behaviors on the continua has been discussed both in clinical contexts and in neuroscientific and neuroevolutionary contexts (1, 2). Recent years have seen an increasing trend to consider psychosis as a continua (3), ranging from psychosis-like experiences (PLE) (or psychotic-like experiences), clinical high risk for psychosis (CHR), to full-blown psychosis.
The term PLEs is widely used to describe transitory hallucinatory and (or) delusional experiences that are below the threshold of clinical psychosis. According to a systematic review by Lee et al. (4), PLEs have been defined by three different approaches, including (i) preset criteria, (ii) assessment tools with predetermined threshold (e.g., Comprehensive assessment of at-risk mental states, CAARMS), and (iii) assessment tools quantitatively without predefined criteria (e.g., Community Assessment of Psychic Experiences, CAPE) (4). PLEs are frequently reported in the community with a prevalence rate of 5–8%. PLEs have also been linked to an increased risk of developing psychotic disorders as well as suicidal behavior in the future (5–7).
For the past few years, the role of trauma on the psychosis continuum has gained increasing attention. Meta-analyses have revealed that childhood adversities are related to an increased risk for developing psychosis and persistence of psychotic-like experiences (8, 9). Dose-responses between trauma and psychotic symptoms or Non-clinical psychotic-like experiences were found in different research, and this makes the role of trauma hard to be ignored (10–15). Psychotic patients with childhood adversities tend to have declined psychosocial functioning, more severe clinical symptoms, longer hospital stays, lower self-rated life quality scores, as well as slower symptomatic remission rates over time (16–20).
In consideration of the variety of trauma types, various measurements are taken to capture the different dimensions of trauma. Many investigators use either some modules from structured interviews (e.g., The Composite International Diagnostic Interview, CIDI) or single scale (e.g., The Short version of the Childhood Trauma Questionnaire, CTQ) to assess trauma, however, only specific aspects of trauma (21, 22) are covered. For instance, most of the five dimensions of CTQ only inquire about the abuses and neglects which happen within the family context. However, school and workplace bullying events are also traumatic and this needs to be assessed independently.
Bullying is defined as a kind of aggressive behavior characterized by intentional harm or causing discomfort and is also accompanied by imbalanced power between the two parties (23). Bullying can manifest in different ways, such as direct assaulting, calling names, or indirect isolation from a group (24). A large cross-sectional investigation conducted in over forty countries illustrated that nearly 11% of teenager students bullied others, 13% were bullied, and 3.6% were in both roles (25). In 2019, a Chinese school-based survey of 2,579 students (aged from 10 to 17) revealed that 12.4% of them experienced bullying, of which the most common types were verbal and cyber bullying (26). Bebbington et al. reported that in people with “definite or probable” psychotic disorders, there was a clear plenitude of victimization experiences, many of which occurred in childhood (27). Furthermore, Campbell et al. found that being bullied at middle school was prominently associated with hallucinations, dissociation, and paranoia (28), and Lataster et al. reported similar findings that, after controlling for age and sex, “being bullied” was strongly related to a 3 times higher risk for having Non-clinical psychotic experiences (29).
As mentioned above, both bullying and childhood abuse and (or) neglect are traumatic experiences that contribute to the development of psychotic experiences. However, data from the Avon Longitudinal Study of Parents and Children in the UK (ALSPAC) and the Great Smoky Mountains Study in the USA (GSMS) suggested that bullying had a unique effect on mental health. Children who were only bullied by peers were more likely than children who were only maltreated (abused or neglected in family) to have depression, anxiety, and suicidal behaviors in both cohorts (30). However, it remains unclear whether bullying independently predicts PLEs, when other traumatic experiences such as abuse and (or) neglect, as well as current depression and anxiety, are controlled.
Bullying events are usually assessed by questionnaires or scales that primarily focus on the present situations (29, 31). Only two retrospective measurement tools that specifically look at past bullying events (32, 33). The Bullying Scale for Adult (BSA) is a brief self-rating questionnaire derived from the traditional bullying scale. The variety of types of bullying experiences covered in BSA allow us to investigate the dose-response effect of bullying measured by the number of endorsed items about being bullied. So far, no retrospective bullying scales for adults are available in China. Therefore, the present study aimed (1) to validate the Chinese version of Bullying Scale for Adults (C-BSA) and to retrospectively investigate the prevalence rate of bullying in Chinese university students, and (2) to determine if bullying has a unique role contributing to PLEs when other childhood trauma (abuse and neglect in family), as well as other psychopathology (depression and anxiety), are all controlled.
Participants in the construction sample and the validation sample were all recruited in several elective courses about psychological health at a comprehensive university in North China. After teachers introduced the whole program, the voluntary students scanned a Quick Response (QR) code by WeChat (The most popular messaging app in China) and then completed a series of questionnaires. To ensure the responses validity, we embedded two quality control items (1. Please choose “not a bit”; 2. My real name is Trump) in the online questionnaires to filter out the irresponsible answers. Data with more than 5 “don't know” answers on C-BSA were also excluded.
This study was part of the project “Detection of subclinical psychotic population with traumatic symptoms and EMDR intervention”, which had been approved by the Ethics Committee of Beijing Anding Hospital, Capital Medical University. As personal identity data were not collected in this part of the project, informed consent for the current study was waived.
The English version of BSA was independently translated into Chinese by two authors (JZ & DYC). The translated scripts were reviewed and revised by a senior consultant psychiatrist (FCZ) and an associate professor in psychology (XHL) by taking into consideration of the semantic, idiomatic, and cultural equivalence of each item. All the four authors are native in Chinese and proficient in English. Then, this final version was back translated into English by a bilingual health professional (YL). The back-translated version was sent to the original author of BSA (Theresa Katharina Haidl) to ensure the equivalence. The C-BSA was administered in the construction sample to determine the items to retain, so as to generate the definitive the questionnaire (Study 1). Then the definitive questionnaire was tested in the validation sample (Study 2). Besides C-BSA, a battery of questionnaires covering traumatic experiences and emotional distress were also administered.
The BSA was developed to evaluate adults' past bullying experiences, which was a modified version from the Bully Survey (33–35). The entire scale is divided into three parts: part A is about subjective experiences of being bullied, consisting of 13 items representing 13 types of bullying behaviors. For each item, a five-point Likert rating is used (0 = never to 4 = always) with an additional option of “don't know”. If a score other than “0” is endorsed, more detailed items about the perpetrator, time, and duration need to be answered. Part B is the personal consequences of bullying, including six items measured by a five-point Likert scale (“0—Never a problem” to “4—Always a problem”). Part C includes two items inquiring about the experience of acting as a bully perpetrator. As mentioned above, the English version of BSA was translated into Chinese to generate C-BSA.
In order to create a shorter scale with good internal consistency for self-rating psychosis-like experience, Capra and colleagues developed CAPE-p15 (36). In 2020, Meng Sun and colleagues validated the psychometric properties of the Chinese version of CAPE-p15 in college students in China (37). The frequency and distress level related to PLEs are measured in each item. Options from 1 (never) to 4 (nearly always) are used to assess the frequency while options from 1 (not distressed) to 4 (very distressed) are for measuring distress level. Three factors were confirmed from previous studies: persecutory ideation (PI), bizarre experiences (BEs), and perceptual abnormalities (PAs) (37, 38). The Chinese version of CAPE-p15 exhibited good validity and satisfactory internal consistency (Cronbach's alpha = 0.88).
The CTQ is a 28-item self-reported questionnaire developed by Bernstein for assessing childhood trauma that occurred before age 16. It consists of five subscales: emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN) and physical neglect (PN) (39). Responses on a five-point Likert scale are rated from 0-never to 4-very often. The Chinese version of the CTQ showed good psychometric properties (40, 41).
The Chinese version of self-rating depression scale (SDS) (42) and self-rating anxiety scale (SAS) (43) were also administered to evaluate depressive and anxiety symptoms in the past week. Both scales are rated based on a 4-point Likert scale and both have presented with good psychometric profiles in college students (44–46).
Data were analyzed by using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) and Mplus version 8.3. Continuous variables such as age, years of schooling, scores of CTQ, C-BSA, CAPE_FT, CAPE_PT, SDS, and SAS were summarized as Mean ± SD, whereas categorical variables (sex) were summarized as N (%). The comparisons between the construction sample and the validation sample in terms of sociodemographic, traumatic experiences, and emotional distress were carried out by using the Chi-squared test (categorical variables), t-test (normally distributed continuous variables) or Non-parametric test (skewed continuous variables).
Cronbach's α was calculated to determine the internal consistency. A Cronbach's α higher than 0.7 is considered acceptable, while higher than 0.9 indicates excellent (47). Exploratory factor analysis (EFA) was conducted in the construction sample to determine the reliable factor structure and which items to delete. Principal axis factoring was used to extract factors with eigenvalues >1. Promax rotation with kappa = 4 was performed (33, 48, 49). Kaiser-Meyer-Olkin (KMO) and Bartlett's test was carried out to evaluate the adequacy of factor analysis. KMO higher than 0.9 indicated perfect for factor analysis, while KMO higher 0.7 suggested acceptable (50). Items with a single factor loading no <0.4 were considered sufficient. Parallel analysis has been considered a valid method for determining the number of factors to retain (51, 52). By comparing the eigenvalues generated from the actual data with the those from a Monte-Carlo simulated matrix of the same size, the ideal number of final factors is determined. In this study, both the parallel analysis and the Kaiser's eigenvalue-greater-than-one rule were carried out.
Data of the validation sample was used for confirmatory factor analysis (CFA) to test the construct validity of C-BSA. Weighted Least Squares with Means and Variance Adjusted estimation (WLSMV) method was used as data were category variables. Fit indices including root mean square error of approximation (RMSEA), comparative fit index (CFI), Tucker-Lewis index (TLI), standardized root mean square residual (SRMR) were utilized to evaluate the model fit. RMSEA <0.08, CFI > 0.90, TLI > 0.90, SRMR <0.06 and a normed chi-square (x 2/ df) <5 were acceptable (50, 51, 53).
Spearman's correlation analysis was applied to check for associations between the scores of C-BSA and that of CTQ, CAPE-p15, SAS and SDS to assess the concurrent validity or correlations. According to the study of Sun et al. (37), the frequency score of 1.57 was the best to detect the “genuine PLEs” of the last month (54). We divided the entire sample into two groups: PLEs (frequency score ≤ 1.57 on CAPE-p15) and non-PLEs (frequency score <1.57 on CAPE-p15). To explore the independent role of bullying in predicting PLEs status (0 = no PLEs, 1 = PLEs) and to explore the dose-response effect of multiple bullying types, two logistic regression analyses with the forward LR method were conducted. In model 1, the total score of C-BSA, CTQ, SAS and SDS were entered as independent variables; in model 2, multiple experiences of being bullied (dummy coded as: 0 = no bullying, 1 = number of bullying types < = 3, 2 = number of bullying types > 3), CTQ, SAS, and SDS and sociodemographic variables were entered as independent variables.
A P value <0.05 was set to be significant level, and all tests were two tailed.
Six hundred and forty-nine students agreed to participate in Study 1. After excluding Non-conscientious data, 629 students formed the construction sample (Table 1).
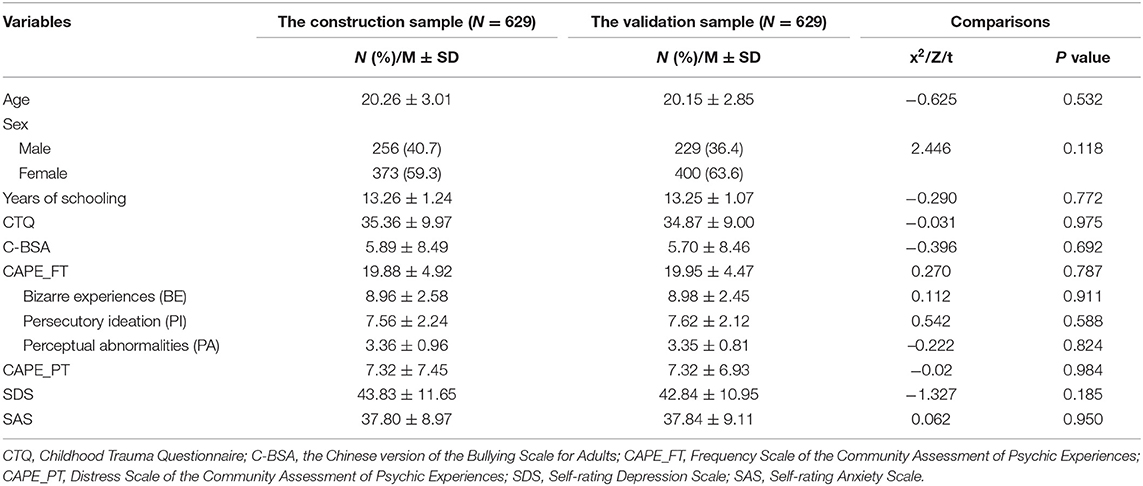
Table 1. Demographic and clinical characteristics of the construction sample and the validation sample.
A Cronbach's α of 0.921 indicated excellent consistency (Table 2). One item had an item-scale correlation below 0.3 (0.211 for item 10) (Supplementary Table 1). One hundred and twenty-three students completed the 1-week retest and the test-retest reliability coefficient was 0.824 (P < 0.01). These results indicated that the C-BSA was of high reliability.
EFA was performed in the construction sample. A Kaiser–Meyer–Olkin (KMO) of 0.907 and the Bartlett's test of sphericity (P < 0.001) supported the adequacy of factor analysis.
(1) Four factors with eigenvalues of more than 1 were extracted which explained the 55.65% of the cumulative variance (four-factor model). Factor names, items, communalities, and loadings were showed in Table 2. Factor 1 “Emotional abuse” composed of items 1, 2, 4, 5, 6, 11, 12, 13 which explained 40.55% of the variance; factor 2 “Interpersonal difficulties” composed of items 14 to 19 which accounted for 6.88% of the variance; factor 3 “Physical abuse” including item 3, 7, 8 which explained 4.84% of the variance; and factor 4 “Sexual harassment” including item 9 and 10 which accounted for 3.39% of the variance (Table 2).
(2) In parallel analysis, only eigenvalues higher than the upper limit of 95% confidence intervals (CIs) of the simulated datasets were retained, resulting in a three-factor model. The three factors' eigenvalues were 8.130, 1.737, and 1.363, respectively. The latent variables explained 40.382, 6.293, and 4.741 percent of the variance, accounting for 51.415 percent of the total variance. The factor distribution differed slightly from that of the four-factor model, with two same factors and the third factor being the combination of factors 3 and 4 of the four-factor model (Table 2).
Six hundred and sixty-seven students agreed to participate in Study 2. After excluding Non-conscientious data, 629 students formed the validation sample (Table 1). In comparison of the demographic and clinical characteristics between the two samples, no significant differences were found.
Confirmatory Factorial Analysis (CFA) in the validation sample was carried out to verify the four-factor model and the three-factor model revealed in EFA. The four-factor model showed good fit for the data. The fit indices of the model were χ2 = 406.637, p < 0.001, RMSEA = 0.053, SRMR = 0.049, CFI = 0.980, and TLI = 0.977. The model was considered good, since CFI and TLI exceeded 0.95, and RMSEA was <0.08. These results suggested that the four-factor model gives a close fit to our sample data. As for the three-factor model, all the model fits seemed adequate (RMSEA = 0.057, 95% CI = 0.051 / 0.063; TLI = 0.974, CFI = 0.978, χ2/df = 3.009, SRMR = 0.06).
In combining the construction and the validation samples (the whole sample), 699 (55.56%) reported bully related experiences, including 504 (40.06%) as victims only, 25 (1.99%) as perpetrator only, and 170 (13.51%) as both victims and perpetrators. Regarding experiences of being bullied, the most endorsed item was item 4 “Played jokes on me”, while the least endorsed item was item 10 “Sexually assaulted me”. The frequency distribution of endorsed items about being bullied are shown in Supplementary Table 2.
There was a significantly higher proportion of individuals as bully victims (50.7 vs. 37.8%) and as both victim and perpetrator (28.8 vs. 10.3%) in PLEs than that in non-PLEs (Supplementary Table 3). Data from the two samples showed a significant correlation between the total scores of C-BSA and CTQ, CAPE-p15, SDS, and SAS (Supplementary Table 4). The correlation coefficient between BSA and CTQ was 0.31 indicating moderate correlation.
Regarding the multivariate logistic analyses, both model 1 and model 2 revealed that bullying significantly and independently predicted PLEs status. In model 1, the total score of C-BSA (OR = 1.070, P < 0.001, 95% CI: 1.049–1.092), CTQ (OR = 1.022, P = 0.023, 95% CI: 1.003–1.041), and SAS (OR = 1.091, P < 0.001, 95% CI: 1.067–1.115) were significant predictors of PLEs. In model 2, PLEs were significantly predicted by multiple experiences of being bullied (dummy #1: OR = 2.012, P = 0.003, 95% CI: 1.271–3.184; dummy #2: OR = 3.712, P < 0.001, 95% CI: 2.472–5.573), the total score of CTQ (OR = 1.032, P < 0.001, 95% CI: 1.014–1.050) and SAS (OR = 1.097, P < 0.001, 95% CI: 1.074–1.121) (Table 3).
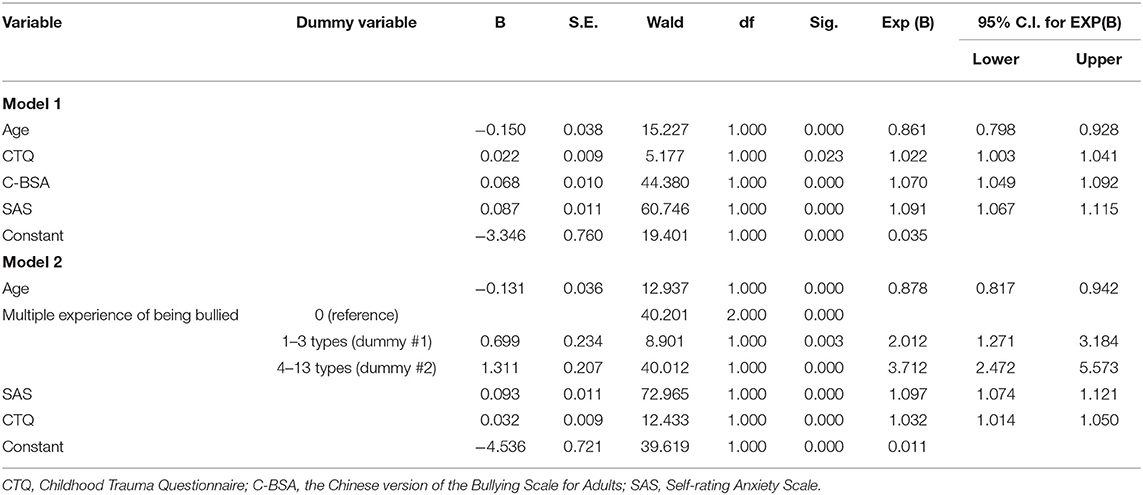
Table 3. Multivariate logistic regression analyses for predicting psychosis-like experiences (PLEs) (N = 1,258).
Figure 1 shows the ROC curves for the predicted probabilities from the two final models. The area under the curve (AUC) was estimated to be 0.808 (95% CI: 0.775 to 0.841) for the first model with a sensitivity of 73.1% and a specificity of 74.1% (Figure 1A); and was 0.807 (95% CI: 0.774 to 0.840) for the second model with a sensitivity of 68.0% and a specificity of 79.3% (Figure 1B).
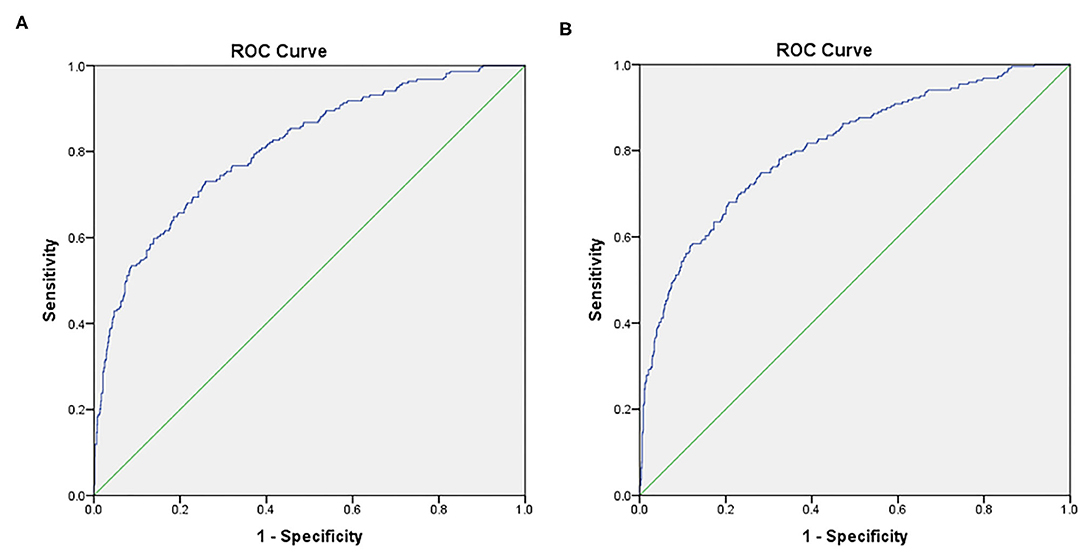
Figure 1. Receiver operating characteristic (ROC) curves for the two models of multivariate logistic regression analyses in predicting the presence of PLEs. The area under the curve (AUC) was estimated to be 0.808 (95% CI: 0.775 to 0.841) for the first model with a sensitivity of 73.1% and a specificity of 74.1% (A); and was 0.807 (95% CI: 0.774 to 0.840) for the second model with a sensitivity of 68.0% and a specificity of 79.3% (B).
To the best of our knowledge, this is the first study that has ever investigated whether past bullying experiences independently contribute to the presence of PLEs. In this study, more than half of the participant students reported at least one past bullying experience based on the endorsed items on C-BSA. Our findings have confirmed the hypothesis that bullying has a unique contribution to the presence of PLEs, which was associated with 2.0 or 3.7 times the risk for the presence of PLEs (numbers of bullying types < = 3 or > 3, respectively) even after the total scores of CTQ, SDS, and SAS were all controlled.
The overall prevalence rate of bullying related behaviors in our sample is 55.56%. Specifically, 1.99% students bullied others, 13.51% reported as both a victim and a perpetrator, and 40.06% reported being bullied. Similar findings can be found in another report which investigated 95,873 students from 85 vocational schools in Southeast China (55). However, the self-reported prevalence of bullying victimization varied dramatically across different studies, ranging from 2 to 66% in Mainland China, possibly due to discrepancies in sampling methods, measurements of bullying, and study designs (56).
Overall, the C-BSA showed good preliminary validity and reliability in the present sample. Regarding internal consistency, item 10 “Sexually assaulted me” had an item-scale correlation below 0.3. This may be explained by the fact that this was the least endorsed item about being bullied. Only 34 (2.70%) students endorsed item 10. The result was interesting when compared with Haidl et al. (33)'s stud. In their study, item 10 showed an item scale correlation of <0.3 in Italy and Finland. This item has not been removed from the C-BSA in the current study because every student who endorsed this item had a frequency score ≤ 1.57 on CAPE-p15, suggesting clinical relevance of the item with PLEs. However, these findings need to be re-examined in larger samples in the future.
The correlation coefficient between BSA and CTQ was 0.31 indicating moderate correlation. This correlation coefficient is well below that in Haidl et al. (33)'s study, in which the coefficient ranged from 0.458 in Finnish sample to 0.680 in German sample. This discrepancy could be due to the difference in sample composition in terms of their clinical settings. In the present study, we only recruited Non-clinical college students while the sample of Haidl et al.'s study consisted of a majority of clinical patients. Moreover, these findings also suggest that bullying may have a unique role in the context of traumatic experiences in Chinese culture, which is relatively independent of family abuse and (or) neglect (indicated by CTQ).
Several lines of evidence have shown that both maltreatment in family and bully victimization in schools would increase the expression of psychosis phenotype (57–59). Individuals at ultra-high risk for psychosis often reported various types of childhood trauma and bullying experiences, as well as anxiety and depression (60–62). In line with these reports, score of CAPE-p15 was also positively correlated with that of SDS, SAS, C-BSA, and CTQ in the present study. Exposure to childhood adversities could disrupt the function of hypothalamic-pituitary-adrenal (HPA) and activate dopaminergic circuits, leading to a vulnerability to psychosis (63). Within the framework of stress-vulnerability model, various trauma are all transdiagnostic risk factors, leading to subsequent mental disorders through common biological pathways (63). In this regard, the risk of psychosis would increase with the accumulation of early life adversities (64), regardless of the type of trauma.
However, the multivariate logistic regression revealed that bullying was associated with 2.0 or 3.7 times the of risk for the presence of PLEs (numbers of bullying types < = 3 or > 3, respectively) even after controlling for CTQ, SDS, and SAS scores, suggesting the contribution of bullying to PLEs is independent of the effect of maltreatment in the family (measured by CTQ). Children being bullied usually have an excessive appraisal of the victimization (65), and an increase of the psychotic-like or paranoid reactivity to stress (66, 67). Beyond the field of psychosis, the unique role of bullying has already been implicated in two cohorts studies (ALSPAC and GSMS), in which children bullied by peers were more likely to have depression, anxiety, and suicidal behaviors than children who were only maltreated in family (30). The dose-response relationship between the numbers of bullying types and the presence of PLEs was a new finding, although the association between the severity of bullying and PLEs has already been established (31). It has also been demonstrated that the PLEs would deteriorate (68) and the transition to psychosis are likely to happen with the increase of bullying severity (31).
Multivariate logistic regression revealed that maltreatment in family (indicated by scores of CTQ) and anxiety (indicated by scores of SAS) also independently correlated with PLEs, which was consistent with previous reports (69–71). However, depression was no longer an independent risk factor for PLEs when traumatic experiences and anxiety were all controlled. Fisher et al. (72) discovered in a student sample that anxiety played a mediating role between emotional abuse and paranoia. Yamasaki et al. (73) demonstrated that depression did not exhibit significant mediation effects between peer victimization and hallucinations. However, inconsistent findings were also reported in previous literatures (74, 75). Further studies are warranted to fully unravel the association of depression and PLEs.
The results should be interpreted with caution due to potential methodological limitations. First, we did not conduct a structured interview for the college students to verify their PLEs in the present study. Subjective reports of PLEs have been linked to a higher false positive rate in the community population (76, 77). Second, all the participants were Non-help seeking college students, which limits the generalizability of the findings to clinical populations. Third, although C-BSA reflects past bullying experiences, the cross-sectional design could not explore dynamic interaction between PLEs, various traumatic experiences, and other psychopathology.
In conclusion, the key findings of this study include (1) C-BSA has showed good psychometric properties in university students in China; (2) The contribution of past bullying experiences to the presence of PLEs seems to be independent of other childhood trauma, current depression, and anxiety; and (3) There is a dose-response relationship between the numbers of bullying types and the presence of PLEs.
The study shed light on the differential contributions between bullying and maltreatment in family to the increased risk of psychosis. By addressing the unique effects of past bullying experiences, the findings of the study would lend support to the future development of individualized therapeutic strategies for individuals with PLEs.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The studies involving human participants were reviewed and approved by the Ethics Committee of Beijing Anding Hospital, Capital Medical University. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
JZ: conceptualization, methodology, formal analysis, and writing—original draft. X-HLu: methodology, formal analysis, and data curation. YL: resources and writing—review and editing. NW: formal analysis and writing—review and editing. D-YC: investigation, software, and data curation. I-AL: investigation, software, and validation. X-HLi: supervision, methodology, and writing—review and editing. F-CZ: conceptualization, project administration, methodology, formal analysis, and writing—review and editing. C-YW: conceptualization, supervision, funding acquisition, and writing—review and editing. All authors contributed to the article and approved the submitted version.
This work was funded by the National Science and Technology Major Project for IND (investigational new drug) (Grant No. 2018ZX09201-014) and the Beijing Municipal Administration of Hospitals Clinical Medicine Development of special funding (ZYLX201815).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to express their gratitude to Dr. Theresa Katharina Haidl from the University of Cologne, Professor Liang Zhou and Dr. Meng Sun from Guangzhou Medical University for their kind support to the study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.839630/full#supplementary-material
1. Di Plinio S, Ebisch SJH. Combining local and global evolutionary trajectories of brain-behaviour relationships through game theory. Eur J Neurosci. (2020) 52:4198–213. doi: 10.1111/ejn.14883
2. Ross CA, Margolis RL. Research domain criteria: cutting edge neuroscience or galen's humors revisited? Mol Neuropsychiatry. (2018) 4:158–63. doi: 10.1159/000493685
3. Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res. (2002) 54:59–65. doi: 10.1016/S0920-9964(01)00352-8
4. Lee KW, Chan KW, Chang WC, Lee EH, Hui CL, Chen EY. A systematic review on definitions and assessments of psychotic-like experiences. Early Interv Psychiatry. (2016) 10:3–16. doi: 10.1111/eip.12228
5. Werbeloff N, Drukker M, Dohrenwend BP, Levav I, Yoffe R, van Os J, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. (2012) 69:467–75. doi: 10.1001/archgenpsychiatry.2011.1580
6. Murray GK, Jones PB. Psychotic symptoms in young people without psychotic illness: mechanisms and meaning. Br J Psychiatry. (2012) 201:4–6. doi: 10.1192/bjp.bp.111.107789
7. Yates K, Lång U, Cederlöf M, Boland F, Taylor P, Cannon M, et al. Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA Psychiatry. (2019) 76:180–9. doi: 10.1001/jamapsychiatry.2018.3514
8. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. (2012) 38:661–71. doi: 10.1093/schbul/sbs050
9. Trotta A, Murray RM, Fisher HL. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol Med. (2015) 45:2481–98. doi: 10.1017/S0033291715000574
10. Heins M, Simons C, Lataster T, Pfeifer S, Versmissen D, Lardinois M, et al. Myin-Germeys: childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. (2011) 168:1286–94. doi: 10.1176/appi.ajp.2011.10101531
11. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children's emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. (2011) 168:65–72. doi: 10.1176/appi.ajp.2010.10040567
12. Shevlin M, Murphy J, Read J, Mallett J, Adamson G, Houston JE. Childhood adversity and hallucinations: a community-based study using the national comorbidity survey replication. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:1203–10. doi: 10.1007/s00127-010-0296-x
13. Spauwen J. Impact of psychological trauma on the development of psychotic symptoms: relationship with psychosis proneness. Br J Psychiatry. (2006) 188:527–33. doi: 10.1192/bjp.bp.105.011346
14. Shevlin M, Dorahy MJ, Adamson G. Trauma and psychosis: an analysis of the national comorbidity survey. Am J Psychiatry. (2007) 164:166–9. doi: 10.1176/ajp.2007.164.1.166
15. Shevlin M, Houston JE, Dorahy MJ, Adamson G. Cumulative traumas and psychosis: an analysis of the national comorbidity survey and the British psychiatric morbidity survey. Schizophr Bull. (2008) 34:193–9. doi: 10.1093/schbul/sbm069
16. Davidson G, Shannon C, Mulholland C, Campbell J. A longitudinal study of the effects of childhood trauma on symptoms and functioning of people with severe mental health problems. J Trauma Dissociation. (2009) 10:57–68. doi: 10.1080/15299730802485169
17. Kilian S, Asmal L, Phahladira L, Plessis SD, Luckhoff H, Scheffler F, et al. The association between childhood trauma and treatment outcomes in schizophrenia spectrum disorders. Psychiatry Res. (2020) 289:113004. doi: 10.1016/j.psychres.2020.113004
18. Ajnakina O, Trotta A, Forti MD, Stilo SA, Kolliakou A, Gardner-Sood P, et al. Different types of childhood adversity and 5-year outcomes in a longitudinal cohort of first-episode psychosis patients. Psychiatry Res. (2018) 269:199–206. doi: 10.1016/j.psychres.2018.08.054
19. Aas M, Andreassen OA, Aminoff SR, Færden A, Romm KL, Nesvåg R, et al. A history of childhood trauma is associated with slower improvement rates: findings from a one-year follow-up study of patients with a first-episode psychosis. BMC Psychiatry. (2016) 16:126. doi: 10.1186/s12888-016-0827-4
20. Pruessner M, King S, Vracotas N, Abadi S, Iyer S, Malla AK, et al. Gender differences in childhood trauma in first episode psychosis: association with symptom severity over two years. Schizophr Res. (2019) 205:30–7. doi: 10.1016/j.schres.2018.06.043
21. Murphy J, Houston JE, Shevlin M, Adamson G. Childhood sexual trauma, cannabis use and psychosis: statistically controlling for pre-trauma psychosis and psychopathology. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:853–61. doi: 10.1007/s00127-012-0592-8
22. Wigman JT, van Winkel R, Jacobs N, Wichers M, Derom C, Thiery E, et al. A twin study of genetic and environmental determinants of abnormal persistence of psychotic experiences in young adulthood. Am J Med Genet B Neuropsychiatr Genet. (2011) 156B:546–52. doi: 10.1002/ajmg.b.31193
23. Olweus D. Bullying at school: knowledge base and an effective intervention program. Ann N Y Acad Sci. (2006) 794:265–76. doi: 10.1111/j.1749-6632.1996.tb32527.x
24. Wolke D, Woods S, Bloomfield L, Karstadt L. The association between direct and relational bullying and behaviour problems among primary school children. J Child Psychol Psychiatry. (2000) 41:989–1002. doi: 10.1111/1469-7610.00687
25. Craig W, Harel-Fisch Y, Fogel-Grinvald H, Dostaler S, Hetland J, Simons-Morton B, et al. A cross-national profile of bullying and victimization among adolescents in 40 countries. Int J Public Health. (2009) 54 (Suppl 2):216–24. doi: 10.1007/s00038-009-5413-9
26. Xiao Y, Jiang L, Yang R, Ran H, Wang T, He X, et al. Childhood maltreatment with school bullying behaviors in Chinese adolescents: a cross-sectional study. J Affect Disord. (2021) 281:941–8. doi: 10.1016/j.jad.2020.11.022
27. Bebbington PE, Bhugra D, Brugha T, Singleton N, Farrell M, Jenkins R, et al. Psychosis, victimisation and childhood disadvantage: evidence from the second British national survey of psychiatric morbidity. Br J Psychiatry. (2004) 185:220–6. doi: 10.1192/bjp.185.3.220
28. Campbell MLC, Morrison AP. The relationship between bullying, psychotic-like experiences and appraisals in 14-16-year olds. Behav Res Ther. (2007) 45:1579–91. doi: 10.1016/j.brat.2006.11.009
29. Lataster T, van Os J, Drukker M, Henquet C, Feron F, Gunther N, et al. Childhood victimisation and developmental expression of non-clinical delusional ideation and hallucinatory experiences: victimisation and non-clinical Psychotic experiences. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:423–8. doi: 10.1007/s00127-006-0060-4
30. Lereya ST, Copeland WE, Costello EJ, Wolke D. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. (2015) 2:524–31. doi: 10.1016/S2215-0366(15)00165-0
31. van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C, de Haan L. Childhood bullying and the association with psychosis in non-clinical and clinical samples: a review and meta-analysis. Psychol Med. (2012) 42:2463–74. doi: 10.1017/S0033291712000360
32. Schäfer M, Korn S, Smith PK, Hunter SC, Mora-Merchán JA, Singer MM, et al. Lonely in the crowd: recollections of bullying. Br J Dev Psychol. (2004) 22:379–94. doi: 10.1348/0261510041552756
33. Haidl TK, Schneider N, Dickmann K, Ruhrmann S, Kaiser N, Rosen M, et al. Validation of the bullying scale for adults - results of the PRONIA-study. J Psychiatr Res. (2020) 129:88–97. doi: 10.1016/j.jpsychires.2020.04.004
34. Swearer SM, Turner RK, Givens JE, Pollack WS. “You're So Gay!”: do different forms of bullying matter for adolescent males? School Psych Rev. (2008) 37:160–73. doi: 10.1080/02796015.2008.12087891
35. Swearer SM, Cary PT. Perceptions and attitudes toward bullying in middle school youth. J Appl Sch Psychol. (2003) 19:63–79. doi: 10.1300/J008v19n02_05
36. Capra C, Kavanagh DJ, Hides L, Scott J. Brief screening for psychosis-like experiences. Schizophr Res. (2013) 149:104–7. doi: 10.1016/j.schres.2013.05.020
37. Sun M, Wang D, Jing L, Xi C, Dai L, Zhou L. Psychometric properties of the 15-item positive subscale of the community assessment of psychic experiences. Schizophr Res. (2020) 222:160–66. doi: 10.1016/j.schres.2020.06.003
38. Bukenaite A, Stochl J, Mossaheb N, Schäfer MR, Klier CM, Becker J, et al. Usefulness of the CAPE-P15 for detecting people at ultra-high risk for psychosis: psychometric properties and cut-off values. Schizophr Res. (2017) 189:69–74. doi: 10.1016/j.schres.2017.02.017
39. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
40. Jiang W-J, Zhong B-L, Liu L-Z, Zhou Y-J, Hu X-H, Li Y. Reliability and validity of the Chinese version of the childhood trauma questionnaire-short form for inpatients with schizophrenia. PLoS One. (2018) 13:e0208779. doi: 10.1371/journal.pone.0208779
41. Fu WX, Yao SQ, Yu HH, Zhao XF, Li R, Li Y, et al. Initial reliability and validity of childhood trauma questionnaire (CTQ-SF) applied in Chinese college students. Chin J Clin Psychol. (2005) 13:40–2. doi: 10.16128/j.cnki.1005-3611.2005.01.012
42. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
43. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
44. Liu X, Tang M, Chen K. A comparative study of SDS and CES-D in the measurement of depression among college students. Chin J Ment Health. (1995) 19:211995.
45. Peng H, Zhang Y, Ying GI, Tang W, Qiang LI, Yan X, et al. Analysis of reliability and validity of Chinese version SDS Scale in women of rural area. Shanghai Med Pharm J. (2013). doi: 10.3969/j.issn.1006-1533.2013.14.011
46. Liu X, Tang M, Chen K. Factor Analysis of Self-Rating Anxiety Scale. Acta Academiae Medicinae Shandong (1995).
47. Taber KS. The use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. (2017) 48:1–24. doi: 10.1007/s11165-016-9602-2
48. Henson RK, Roberts JK. Use of explanatory factor analysis in published research: common errors and some comment on improved practice. Organ Res Methods. (2006) 7:191–205. doi: 10.1177/0013164405282485
49. Matsunaga M. How to factor-analyze your data right: do's, don'ts, and how-to's. Int J Psychol Res. (2011) 3:97–110. doi: 10.21500/20112084.854
51. Patil VH, McPherson MQ, Friesner D. The use of exploratory factor analysis in public health: a note on parallel analysis as a factor retention criterion. Am J Health Promot. (2010) 24:178–81. doi: 10.4278/ajhp.08033131
52. Ledesma RD, Valero-Mora P. Determining the number of factors to retain in EFA: an easy-to- use computer program for carrying out parallel analysis. Pract Assess Res Eval. (2007) 12:2. doi: 10.7275/wjnc-nm63
53. Mueller RM, Lambert MJ, Burlingame GM. Construct validity of the outcome questionnaire: a confirmatory factor analysis. J Pers Assess. (1998) 70:248–62. doi: 10.1207/s15327752jpa7002_5
54. Sun M, Wang D, Jing L, Yang N, Zhou LJEIiP. Comparisons between self-reported and interview-verified psychotic-like experiences in adolescents. Early Interv Psychiatry. (2021) 16:69–77. doi: 10.1111/eip.13132
55. Xu S, Ren J, Li F, Wang L, Wang S. School bullying among vocational school students in china: prevalence and associations with personal, relational, and school factors. J Interpers Violence. (2020) 37:088626052090736. doi: 10.1177/0886260520907360
56. Chan HCO, Wong DS. Traditional school bullying and cyberbullying in Chinese societies: prevalence and a review of the whole-school intervention approach. Aggress Violent Behav. (2015) 23:98–108. doi: 10.1016/j.avb.2015.05.010
57. Schreier A, Wolke D, Thomas K, Horwood J, Hollis C, Gunnell D, et al. Prospective study of peer victimization in childhood and psychotic symptoms in a nonclinical population at age 12 years. Arch Gen Psychiatry. (2009) 66:527–36. doi: 10.1001/archgenpsychiatry.2009.23
58. Fisher HL, Schreier A, Zammit S, Maughan B, Munafò MR, Lewis G, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. (2013) 39:1045–55. doi: 10.1093/schbul/sbs088
59. Gibson LE, Alloy LB, Ellman LM. Trauma and the psychosis spectrum: a review of symptom specificity and explanatory mechanisms. Clin Psychol Rev. (2016) 49:92–105. doi: 10.1016/j.cpr.2016.08.003
60. Addington J, Stowkowy J, Cadenhead KS, Cornblatt BA, McGlashan TH, Perkins DO, et al. Early traumatic experiences in those at clinical high risk for psychosis. Early Interv Psychiatry. (2013) 7:300–5. doi: 10.1111/eip.12020
61. Catone G, Pisano S, Broome M, Lindau JF, Pascotto A, Gritti A. Continuity between stressful experiences and delusion content in adolescents with psychotic disorders-a pilot study. Scand J Child Adolesc Psychiatry Psychol. (2016) 4:14–22. doi: 10.21307/sjcapp-2016-004
62. Falukozi E, Addington J. Impact of trauma on attenuated psychotic symptoms. Psychosis. (2012) 4:203–12. doi: 10.1080/17522439.2011.626867
63. Aiello G, Horowitz M, Hepgul N, Pariante CM, Mondelli V. Stress abnormalities in individuals at risk for psychosis: a review of studies in subjects with familial risk or with “at risk” mental state. Psychoneuroendocrinology. (2012) 37:1600–13. doi: 10.1016/j.psyneuen.2012.05.003
64. Zwicker A, Denovan-Wright EM, Uher R. Gene-environment interplay in the etiology of psychosis. Psychol Med. (2018) 48:1925–36. doi: 10.1017/S003329171700383X
65. Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: 'much ado about nothing'? Psychol Med. (2010) 40:717–29. doi: 10.1017/S0033291709991383
66. Cristóbal-Narváez P, Sheinbaum T, Ballespí S, Mitjavila M, Myin-Germeys I, Kwapil TR, et al. Impact of adverse childhood experiences on psychotic-like symptoms and stress reactivity in daily life in nonclinical young adults. PLoS One. (2016) 11:e0153557. doi: 10.1371/journal.pone.0153557
67. Vaillancourt T, Duku E, Decatanzaro D, Macmillan H, Muir C, Schmidt LA. Variation in hypothalamic-pituitary-adrenal axis activity among bullied and non-bullied children. Aggress Behav. (2008) 34:294–305. doi: 10.1002/ab.20240
68. Mackie C, O'Leary-Barrett M, Al-Khudhairy N, Castellanos-Ryan N, Struve M, Topper L, et al. Adolescent bullying, cannabis use and emerging psychotic experiences: a longitudinal general population study. Psychol Med. (2013) 43:1033–44. doi: 10.1017/S003329171200205X
69. Bell CJ, Foulds JA, Horwood LJ, Mulder RT, Boden JM. Childhood abuse and psychotic experiences in adulthood: findings from a 35-year longitudinal study. Br J Psychiatry. (2019) 214:153–8. doi: 10.1192/bjp.2018.264
70. Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, et al. Childhood abuse as a risk factor for psychotic experiences. Schizophr Res. (2003) 60(1, Supplement):40. doi: 10.1016/S0920-9964(03)80117-2
71. Nishida A, Xu KM, Croudace T, Jones PB, Barnett J, Richards M. Adolescent self-control predicts midlife hallucinatory experiences: 40-year follow-up of a national birth cohort. Schizophr Bull. (2014) 40:1543–51. doi: 10.1093/schbul/sbu050
72. Fisher HL, Appiah-Kusi E, Grant C. Anxiety and negative self-schemas mediate the association between childhood maltreatment and paranoia. Psychiatry Res. (2012) 196:323–4. doi: 10.1016/j.psychres.2011.12.004
73. Yamasaki S, Ando S, Koike S, Usami S, Endo K, French P, et al. Dissociation mediates the relationship between peer victimization and hallucinatory experiences among early adolescents. Schizophr Res Cogn. (2016) 4:18–23. doi: 10.1016/j.scog.2016.04.001
74. Bebbington P, Jonas S, Kuipers E, King M, Cooper C, Brugha T, et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. (2011) 199:29–37. doi: 10.1192/bjp.bp.110.083642
75. Marwaha S, Bebbington P. Mood as a mediator of the link between child sexual abuse and psychosis. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:661–3. doi: 10.1007/s00127-014-0966-1
76. Kim SW, Chung YC, Kang YS, Kim JK, Jang JE, Jhon M, et al. Validation of the Korean version of the 16-item prodromal questionnaire in a non-help-seeking college population. Psychiatry Investig. (2018) 15:111–7. doi: 10.30773/pi.2017.04.24
Keywords: bullying, childhood trauma and adversity, college students, psychosis-like experiences, psychometric properties
Citation: Zhao J, Lu X-H, Liu Y, Wang N, Chen D-Y, Lin I-A, Li X-H, Zhou F-C and Wang C-Y (2022) The Unique Contribution of Past Bullying Experiences to the Presence of Psychosis-Like Experiences in University Students. Front. Psychiatry 13:839630. doi: 10.3389/fpsyt.2022.839630
Received: 20 December 2021; Accepted: 23 February 2022;
Published: 28 April 2022.
Edited by:
Kim T. Mueser, Boston University, United StatesReviewed by:
Simone Di Plinio, University of Studies G. d'Annunzio Chieti and Pescara, ItalyCopyright © 2022 Zhao, Lu, Liu, Wang, Chen, Lin, Li, Zhou and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-Hong Li, bHhoc2h5MjAwMkAxNjMuY29t; Fu-Chun Zhou, ZnJhbmtjaG93QGNjbXUuZWR1LmNu; Chuan-Yue Wang, d2FuZy5jeUAxNjMubmV0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.