
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 29 March 2022
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.836350
This article is part of the Research Topic Violent Relationships: Acute and Long-term Implications View all 8 articles
The cross-sectional study INVITE (INtimate partner VIolence care and Treatment prEferences in postpartum women) aims to examine treatment and counseling preferences and barriers in relation to the experience of intimate partner violence (IPV), depression and anxiety, and (childbirth-related) posttraumatic stress disorder (PTSD) among postpartum women in Dresden, Germany. Currently, the INVITE study consists of an interim sample of N = 1,787 participants with n = 891 completed interviews. Recruitment is ongoing, targeting a community sample of at least N = 4,000 women who complete various quantitative questionnaires via telephone interviews at 3–4 months postpartum. The differences in rates of IPV, postpartum depression and anxiety, and/or (childbirth-related) PTSD as well as treatment and counseling preferences and barriers between affected and non-affected women will be assessed. Further, predisposing variables, past and present stress exposure, enabling resources, as well as past and present health will be examined as predictors of service preferences and barriers. In this study protocol, the theoretical background, methods, as well as preliminary results regarding sociodemographic characteristics and birth-related factors of the interim sample are presented and discussed in terms of their socio-political relevance. Simultaneously assessing IPV, postpartum depression and anxiety, and (childbirth-related) PTSD will facilitate exploring comorbidities and concomitant special needs of affected women. Results of the INVITE study will therefore set the ground for well-aimed development and improvement of treatment and counseling services for the respective target groups by informing health care professionals and policy makers about specific preferences and barriers to treatment. This will yield the possibility to tailor services to the needs of postpartum women.
Intimate partner violence (IPV), depressive and anxiety disorders, as well as posttraumatic stress disorder (PTSD) are three global health care burdens affecting women of reproductive age, with detrimental consequences for both the individual and society (1–5). Women have been shown to be especially vulnerable to the experience of IPV, depression and anxiety, and PTSD during pregnancy and the postpartum period (6). Although equal access to health care is a central goal in all European health-care systems, international studies show that this aim has not been accomplished yet (7, 8). Rather, previous studies revealed inter-individual differences in access to health care and actual health care utilization due to socioeconomic, cultural, and ethnic characteristics (9–11).
The first global health care burden, IPV against women, refers to any behavior within a present or former intimate relationship that causes physical, psychological, or sexual harm. These behaviors include any acts of physical violence (e.g., slapping, kicking, and beating), sexual violence (e.g., forced sexual intercourse and other forms of sexual coercion), psychological abuse (e.g., insults, constant humiliation, intimidation, and threats), and any controlling behaviors (e.g., isolating a person from family and friends, monitoring their movements, and restricting access to financial resources, employment, education, or medical care) (12).
Violence by an intimate partner has lasting adverse effects on women and children’s health, wellbeing, and relationships (13, 14). In affected women, IPV is associated with compromised mental health and increased suicidality (8, 15, 16). Depression, anxiety, PTSD, panic disorders, and substance abuse disorders have been documented as the most common psychological consequences of IPV for mothers during the perinatal period (17, 18). It is estimated, that nearly one in three women worldwide experiences IPV during her lifetime (19, 20). In Germany, it is estimated that 22% of women experience at least one form of physical and/or sexual intimate partner violence in their lifetime, and 3% experienced it during the past year. Psychological abuse by a current or former partner was experienced by 50% of women in Germany (21). Regarding the perinatal period, on average, one-quarter of pregnant women is exposed globally (22) and the prevalence for IPV during the first year postpartum ranges from 2% in Sweden to 58% in Iran (23).
Regarding the second health care burden, women suffering from postpartum depression and anxiety represent a high-risk population for many types of morbidity. The worldwide pooled prevalence for postpartum depression is 17.7% (24), while the prevalence of postpartum anxiety disorders ranges from 15 to 20% (25, 26). Thus, especially in the vulnerable postpartum period, these women may struggle having their physical and psychological health needs met (27, 28). Postpartum depression and anxiety disorders furthermore increase the mother’s risk of poor physical health, lower self-esteem, higher perceived stress, lower social functioning, relationship difficulties, and poorer overall psychological health (29, 30). The most common cause of death for women in the first year after giving birth is suicide, which in turn is strongly related to symptoms of postpartum depression (31, 32).
Maternal postpartum depression and anxiety are also associated with negative effects on the child. Increased risk of becoming a victim of child abuse and poorer child health practices are observed in children of mothers suffering from postpartum depression (33–35). Further, children of mothers with postpartum depression and anxiety disorders are more likely to show difficult early temperament and impaired development (36–39). Partners of affected women also experience greater levels of stress, depression, and anxiety (4, 40). Therefore, identification and support of women affected by mental health issues during the postpartum period is not only important to prevent negative consequences for the whole family. It can also help to reduce the potential costs for society pertaining to increased health care costs (41).
Another health care burden affecting postpartum women is PTSD due to traumatic childbirth, which is referred to as childbirth-related PTSD. There are varying estimates of the prevalence of childbirth-related PTSD, with studies reporting rates from 3.1 to 4.0% in community samples to 15.7–18.5% in high-risk groups [e.g., women experiencing severe complications during pregnancy and labor or experiencing fetal or infant loss; (42, 43)]. Childbirth-related PTSD or higher levels of posttraumatic stress symptoms related to childbirth have been suggested to be associated with a decreased likelihood of having further children or delaying a subsequent pregnancy (44, 45). It has also been proposed that a new pregnancy has the potential to reactivate the posttraumatic symptoms (46). Although this research field is still to be explored, previous studies have demonstrated its great adverse potential for the mother, her children, the relationship with her baby and the relationship with her partner (47–50). Prior studies found a prospective impact of childbirth-related PTSD symptoms on children’s social-emotional development, not initiating breastfeeding, less favorable child sleep, and low couple relationship satisfaction (3, 51–53).
Intimate partner violence, postpartum depression and anxiety, and (childbirth-related) PTSD seem to be linked to each other. Firstly, IPV victimization is associated with PTSD (54, 55). Is has been argued that violence inflicted by an intimate partner has the potential to be even more psychologically damaging than violence inflicted by a stranger because it cannot be seen as a random attack. Instead, the perpetrator is someone the victim used to trust, so that the violence has to be interpreted as the purposeful intent to harm (56). Experiencing abuse can affect the victim on a cognitive, affective, and behavioral level and may lead to a higher risk of revictimization (57). In turn, repeatedly experiencing victimization like IPV further increases the risk for PTSD (58).
Secondly, comorbidity between depression, anxiety, and PTSD is high (48, 59–61), especially in the weeks prior to delivery and 6 weeks postpartum (62). According to systematic reviews, this link could partly be due to the fact that women with postpartum depression and anxiety symptoms have a high prevalence and increased odds of having experienced childhood abuse and neglect (63–65) as well as partner violence during their lifetime and the past year (6, 23) and therefore also have a higher risk of suffering from PTSD. Additionally, previous studies have shown that current IPV significantly increased the likelihood of reporting traumatic childbirth experiences (66), which also increase the likelihood of postpartum depression and anxiety (67) and may result in childbirth-related PTSD. However, especially the link between postpartum depression and childbirth-related PTSD still needs further research. While pre-existing depression is a strong risk factor for developing childbirth-related PTSD, pre-existing PTSD increases the risk for postpartum depression (68–70), questioning the temporal relationship of both disorders.
Women who experience postpartum depression, anxiety, or (childbirth-related) PTSD and who are suffering from having an abusive relationship with their partner might be the least likely to seek help. Only 33% of women who are physically or sexually abused by their partner contact the authorities (21). Furthermore, women experiencing IPV often do not seek help because they consider it as not needed or not useful, or they indicate that the violence or situation is not serious enough (71). Therefore, it is crucial to raise awareness regarding the seriousness of violence, whether it is physical, sexual, and/or psychological. Because investment in prevention and intervention services for survivors remains inadequate (72), it is crucial to improve possibilities of disclosure within the health care system (73). This is underlined by the fact that physicians’ motivation and readiness to address IPV contrast with uncertainty and lack of awareness (74).
Additionally, many women affected by postpartum depression, anxiety, or (childbirth-related) PTSD do not recognize the mental state they are in and rather attribute their symptoms to a normal part of motherhood such as fatigue, relationship difficulties after becoming parents, or personal weakness. Their partner, family, and friends may share this opinion and often even discourage women from seeking help (75, 76). Thus, high-quality evidence is now needed on how maternity and mental health services should address these issues in order to improve health outcomes for women and their families in the postpartum period. Although empirical evidence demonstrates that postpartum depression, anxiety, and (childbirth-related) PTSD are treatable (77–82), many women still do not receive any or only non-guideline based treatment. For instance, postpartum anxiety can be concealed by postpartum depression and therefore overlooked (83), also because women affected by postpartum anxiety seek professional help less often than women with postpartum depression (84). In the case of childbirth-related PTSD, women are also often misdiagnosed with postpartum depression (61, 85) and guideline-based treatment for childbirth-related PTSD is not offered to them as a result. Additionally, most postpartum women express confusion about treatment options and often opt out of treatment, partly out of concern over the impact of medication on breast milk or fear of being stigmatized as a “bad mother” (86–88). Knowing that women often are the gatekeepers for health in their families (89, 90), it is particularly important to create a service system that meets their needs.
In order to investigate the associations between IPV, postpartum depression and anxiety, and (childbirth-related) PTSD and women’s individual treatment and counseling preferences and barriers, the current study applies concepts of Andersen’s Behavioral Model of Access to Health Care [BMCHC; (91)] and a model from Liang et al. (92) as the study’s theoretical framework (Figure 1). The BMCHC highlights the importance of predisposing variables (e.g., age, education, socio-economic status, and migration status), which can either be barriers or facilitators to service use. These predisposing variables may be associated with past and present stress exposure, available enabling resources, and past and present health, which in turn may also influence each other. Stress exposure might be due to IPV or other stressful life events during childhood or adulthood. In case of IPV, abuse severity can play an important role for the likelihood of help seeking (92, 93). Enabling resources include family and social network structures that may increase help-seeking behaviors, the subjective assessment of one’s own health needs, as well as prior use of services and interventions, which may have been effective. The past and present health status incorporates the mother’s mental health and the mother’s and child’s physical health. Within the theoretical model, these various factors culminate in women’s treatment and counseling preferences, which can be specific or non-specific to the issue and include service providers from the social, psychosocial, or medical sector.
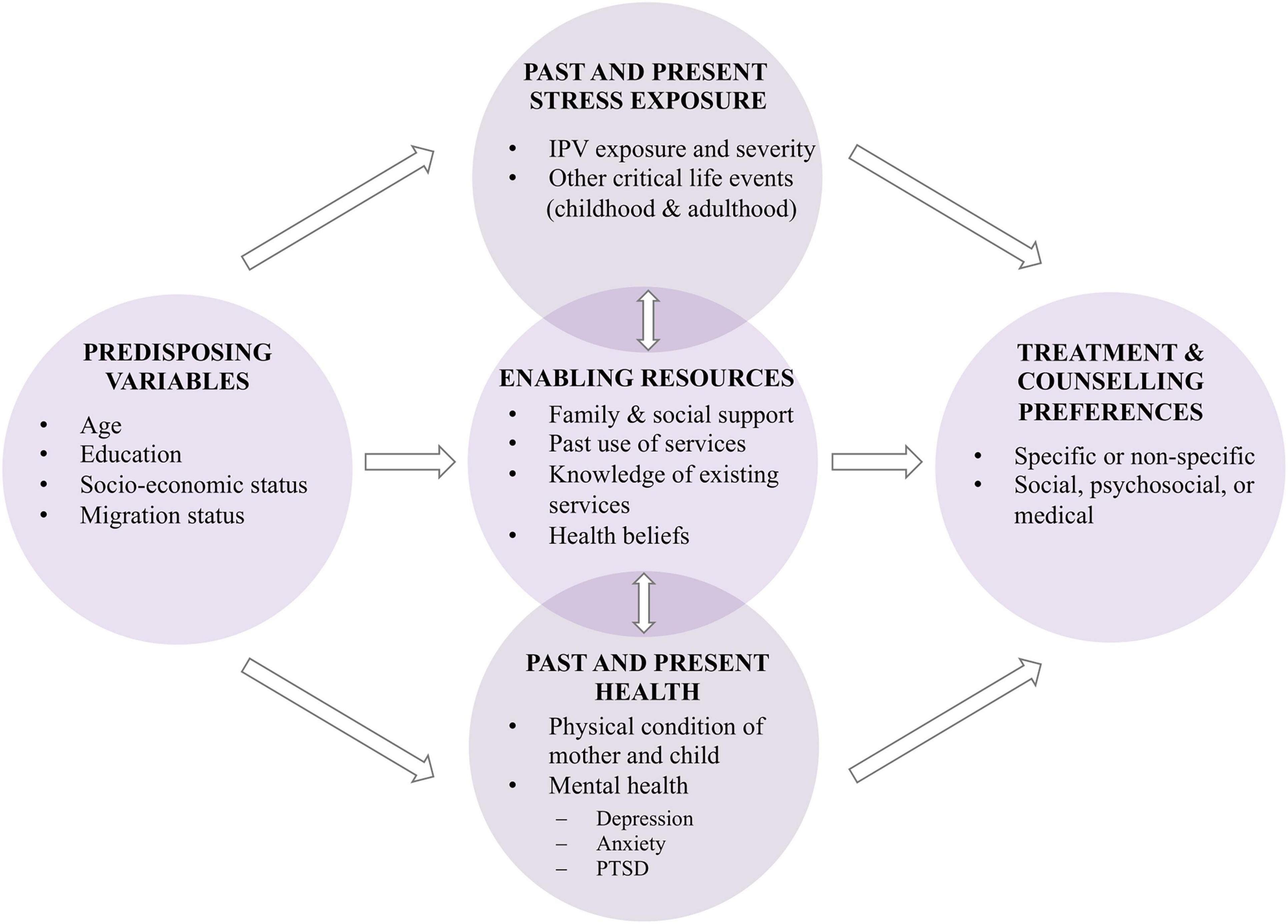
Figure 1. Theoretical framework of the INVITE study. Adapted from Andersen (91) and Liang et al. (92).
The present cross-sectional study called INVITE (INtimate partner VIolence care and Treatment prEferences in postpartum women) intends to examine treatment and counseling preferences and barriers in relation to the experience of IPV, postpartum depression and anxiety, and (childbirth-related) PTSD among women delivering a child in Dresden, Germany at 3–4 months postpartum.
Based on the theoretical model, the main research questions are as follows:
1. Which factors predict higher/lower rates of IPV, depression and anxiety, and/or (childbirth-related) PTSD in postpartum women?
2. Are postpartum women who experience IPV, depression and anxiety, and/or (childbirth-related) PTSD less likely to seek treatment and counseling services compared to postpartum women who do not experience IPV, depression and anxiety, and/or (childbirth-related) PTSD?
3. Which type of treatment and counseling service, professional service provider, and service delivery mode do postpartum women who experience IPV, depression and anxiety, and/or (childbirth-related) PTSD prefer compared to postpartum women who do not experience IPV, depression and anxiety, and/or (childbirth-related) PTSD?
4. Does the severity of IPV, depression and anxiety, and/or (childbirth-related) PTSD in postpartum women predict the likelihood of service utilization?
Secondary research questions are as follows:
1. Do critical life events in the past predict the likelihood of service utilization in postpartum women?
2. Do family and social support predict the likelihood of service utilization in postpartum women?
3. Do knowledge about treatment and counseling services, the number of previous contacts with these services, and positive or negative experiences with them predict the likelihood of service utilization in postpartum women?
4. Do health beliefs about the usefulness of treatment and counseling services predict the likelihood of service utilization in postpartum women?
5. Do the mental or physical health of postpartum women or the physical health of their babies predict the likelihood of service utilization?
By filling the knowledge gap on how to improve postpartum women’s help seeking behavior, this study will improve health care services by informing health care professionals and policy makers about enabling factors as well as specific barriers to treatment. This in turn will yield the possibility to tailor services to the preferences of postpartum women.
The INVITE study is a cross-sectional study targeting a community sample of postpartum women in and around Dresden, Germany. Inclusion criteria are the birth of one or more children within the last 3--4 months and sufficient German or English skills to take part in the study. Women with a stillborn baby or an infant who died after birth are not excluded. Recruitment for the INVITE study started in November 2020. Women are either recruited at the maternity wards of two large hospitals in Dresden, at midwife (antenatal) appointments approximately 6 weeks prior to the planned delivery date, at birth information events of the hospitals, or at freestanding birth centers.1 Student assistants approach all mothers on the wards, at the antenatal clinics, and at the information events. At one hospital and the birth centers, women are approached by midwives instead. Recruitment therefore covers all maternity hospitals and most birth centers in Dresden, which offer different levels of specialization for high and low risk pregnancies, including pre-term deliveries. It ensures that almost all women delivering in Dresden are informed about the INVITE study and facilitates assembling a representative sample of postpartum women.
Recruitment procedures vary between the different hospitals and birth centers to accommodate their respective routines and preferences. Nevertheless, all women receive written information about the study’s aims and procedures as well as a small chocolate as an incentive. Women who agree to participate are asked to provide written informed consent. Unfortunately, the recruitment method had to be altered temporarily due to the COVID-19 pandemic. During lockdowns, all hospital visitation was prohibited and thus student assistants were not allowed to enter the hospitals for recruitment. Instead, nurses on the maternity wards and midwives at the antenatal appointments gave out the study material to interested women. This resulted in student assistants’ in-person recruitment starting December 2020 in one hospital, March 2021 in a second hospital, and July 2021 in the two remaining hospitals.
Ten weeks after the birth of their child or their expected delivery date, women are contacted to schedule an appointment for a standardized telephone interview, which lasts for approximately 1 h. The appointment takes place 3–4 months following birth, thus after completion of the puerperal period and at a time at which women are usually settling into everyday life with their newborn. An interview was chosen as our data collection method over an online or paper-pencil questionnaire for several reasons. Firstly, by calling and asking the women for the actual birth date of their child, we verify that all participants answer the questions 3–4 months after birth, even if they were recruited during pregnancy and we only know the expected delivery date. Secondly, by leading the women through the questions and being able to resolve any ambiguity straight away, the interview is less demanding for the participants than an online or paper-pencil questionnaire and therefore more suitable for postpartum mothers with a newborn that needs their attention, and for women whose mother tongue is not German or English. This assessment method also leads to higher data quality and less missing values, because questions can be explained to women who might not understand them correctly and hesitant women not wanting to answer questions due to privacy concerns can be assured of the pseudonymization strategy and motivated to answer all questions. Thirdly, a telephone interview is more personal than filling out a questionnaire, which makes it easier to transport the importance of the study to participating women and therefore reduces dropout.
After the interview, all women—regardless of whether or not they are affected by IPV, postpartum depression and anxiety, and/or (childbirth-related) PTSD—are offered a list with suitable treatment and counseling services in Dresden. Monetary compensation for study participation pertains to 20€. Women who were approached by student assistants and not the midwives received part of the compensation for participation (i.e., 5€ of 20€) at the time of recruitment.
The INVITE study includes various quantitative questionnaires to assess the constructs of interest. Whenever possible, standardized and validated instruments with good psychometric properties were included and pertain to basic demographic and socioeconomic factors, pregnancy complications, birth-related medical information (e.g., mode of birth and birth complications), birth experience and childbirth-related posttraumatic stress symptoms, questions regarding the women’s and child’s physical health, critical life events, past and current mental health difficulties and treatments, symptoms of depression, anxiety, and non-birth-related PTSD, experience of IPV, social support, and resilience. Additionally, women are asked about their treatment and counseling preferences in case of experience of IPV, postpartum symptoms of depression, anxiety, or (childbirth-related) PTSD, barriers to service utilization, and their knowledge about suitable services. Women who are not affected by any of these symptoms or problems are asked to imagine the respective situation and answer the questions as if they were affected. Comparing affected to non-affected women will allow us to explore why affected women might not seek appropriate treatment.
Treatment and counseling services can range from very specific options tailored to IPV, postpartum depression and anxiety, and/or (childbirth-related) PTSD to more general services for all women such as the family physician. Possible approaches to treatment and counseling can be social, psychosocial, or medical. Figure 2 shows the different dimensions of treatment within the German support system. Regarding treatment and counseling preferences, women are asked to indicate how likely it is that they would pick a specific service if they are or imagine they were affected by IPV, postpartum depression and anxiety, and/or (childbirth-related) PTSD (“not at all,” “rather no,” “rather yes,” and “definitely”).
In the following, we present the instruments utilized to assess the main research questions. A comprehensive list of all assessed constructs can be found in Table 1. As the INVITE study collaborates with the International Survey of Childbirth-Related Trauma (94), a large, international project which examines birth trauma in different cultures around the world, some of our constructs were aligned with the mandatory measures of the INTERSECT study.
The Violence against Women Instrument [VAWI; (124)] is used to assess any experiences of IPV. All questions pertain to violence perpetrated by a current or any former partner. The instrument consists of behavior-specific items related to psychological (four items), physical (six items), and sexual IPV (three items). The physical violence items are further divided into “moderate” (the two first items) and “severe” (the following four items) violence based on the likelihood of physical injury. Respondents are categorized as having been exposed to IPV if they answer any question affirmatively (“yes” coded as 1, or “no” coded as 0), with separate indicators created for each type of IPV (113). For each question, respondents are asked whether they had experienced the specific act during the past year and/or earlier in life. The frequency of experienced IPV is also assessed and coded as 1 (“once”), 2 (“a few times”), and 3 (“many times”). Cronbach’s α coefficient was found to be satisfactory for the subscales in the VAWI conceptual model: 0.79 (psychological scale), 0.80 (physical scale), 0.72 (sexual scale), and 0.88 (total scale) (125). The instrument was translated to German according to the suggestions of the World Health Organization (126) and first checked by researchers involved in the present study who could compare the English version with its translation (expert panel). These researchers then conducted lengthy oral back translation with step-by-step discussion of each question with non-experts fluent in German and English to decide on a final version of the instrument. The research team is planning to conduct a validation study for the translated German version of the instrument.
To assess postpartum depression, we use the Edinburgh Postnatal Depression Scale [EPDS; (106, 107)]. The EPDS was developed as a screening tool for postnatal depression, measuring depressive symptoms during the last week. The scale consists of 10 items rated on a 4-point scale, ranging from 0 to 3, with a maximum score of 30 where higher scores indicate more severe symptoms of depression (127). Cronbach’s α for the German version is high [α = 0.81; (106)].
To measure postpartum anxiety, we use the “anxiety” subscale of the Symptom Checklist-Revised [SCL-90-R; (108)]. It consists of 10 items pertaining to symptoms during the last 7 days. Each item is rated on a 5-point Likert scale, ranging from 0 (“not at all”) to 4 (“extremely”). The total score ranges from 0 to 40 with higher scores indicating more severe levels of anxiety. Cronbach’s α for the subscale “anxiety” is high [α = 0.84; (108)].
The City Birth Trauma Scale [City BiTS; (102, 103)] is used to assess childbirth-related PTSD symptoms and consists of 22 questions, which map onto DSM-5 diagnostic criteria and therefore measure re-experiencing or avoidance of the traumatic event, negative cognitions and mood, and hyperarousal. Symptoms are rated according to frequency over the last week and scored on a scale ranging from 0 (“not at all”) to 3 (“5 or more times”). A higher score indicates more and/or higher frequency of symptoms of childbirth-related PTSD. Diagnostic criterion A items (i.e., perceived threat of serious injuries to mother or child or perceived threat that the mother or child might die) are scored on a yes/no scale. Distress, disability, and potential physical causes are rated as yes/no/maybe. Cronbach’s α for the total German scale is high [α = 0.92; (103)]. In addition to the City BiTS, women were asked to indicate how traumatic they found their recent and potential earlier births on a scale from 0 (not at all traumatic) to 10 (very traumatic).
A short version of the Primary Care PTSD Screen for DSM-5 [PC-PTSD-5; (109, 128)] is used to assess PTSD symptoms due to non-birth-related events. The measure consists of five items and begins with a question designed to assess whether the respondent has had any exposure to traumatic events. If a respondent denies exposure, the PC-PTSD-5 is complete with a score of 0. If a respondent indicates that they have experienced a traumatic event over the course of their life, the respondent is instructed to respond to five additional yes/no questions about how that trauma exposure has affected them over the past month. However, in the INVITE study, the PC-PTSD-5 was adjusted so that women are asked to think of an event that was “so frightening, horrible, or upsetting” that they may have experienced any of the five symptoms during the past month. This way, all women are asked for possible PTSD symptoms. This adjustment was done according to Harrison et al. (129). Additionally, if a woman answers “yes” to any of the items, she is asked how stressful she found this symptom.
All data are collected and managed using Research Electronic Data Capture (REDCap), which is a secure, web-based application for data capture within research studies, hosted at the “Koordinierungszentrum für Klinische Studien” at the Faculty of Medicine of the Technische Universität Dresden, Germany (130, 131).
A flow chart of the INVITE study is depicted in Figure 3. By 29 October 2021, N = 4,944 women were approached and informed about the study. In total, N = 1,787 of the approached women gave written informed consent and were included in the interim sample (recruitment ongoing). This corresponds to a participation rate of 36.1%. Some of these women (n = 766) were not due to be interviewed yet at the time of data extraction because they gave birth less than 3 months ago and others still needed to be contacted to arrange an interview (n = 46). Only n = 84 (4.7%) of the women who gave consent dropped out of the study before the interview took place, because they could not be reached or indicated not having time to complete the interview. In total, N = 891 interviews (49.9% of those who gave consent) were completed by the end of October 2021. To calculate the response rate, we compared the proportion of approached women who had their baby before 7 August 2021 (i.e., more than 3 months before data extraction; N = 3,502) with the proportion of women who participated in the interview. This resulted in a response rate of 25.4%.
The response rate will likely increase over the course of the study because our recruitment method had to be altered temporarily due to the COVID-19 pandemic. As described above, during lockdowns, student assistants were prohibited from entering the hospitals for recruitment and thus, maternity ward nurses and midwives at the antenatal appointments gave out the study material instead. There are several reasons why this procedure resulted in fewer participating women. For instance, nurses and midwives were not able to explain the study in detail, answer questions, or give out the initial incentive of 5€. This might have resulted in women taking the materials home but forgetting about them. This altered procedure does not correspond with our intended recruitment method of proactive outreach, with which an entire population is individually addressed, contacted, and motivated to participate in the study, and may explain why the response rate is lower than anticipated. Since the implementation of proactive outreach in all four hospitals in July 2021, participation rates have increased to 60–80%. When calculating the response rate for the time when student assistants were recruiting in person in two out of four hospitals (i.e., from March 2021), the rate increases to 35.4% (n = 2,084 women were approached of which n = 737 completed the interview).
Table 2 shows where the participating women were recruited. The majority (75.3%) were recruited on the maternity wards of the two largest hospitals with a delivery room in Dresden. These are Level 1 and Level 2 hospitals, which means that they are equipped to handle high-risk pregnancies and pre-term births and have a neonatal intensive care unit. Most of the remaining women were recruited at antenatal appointments of the midwife-led outpatient clinics (23%) of the other two hospitals (both are certified as baby-friendly by the World Health Organization and UNICEF). Additionally, some women were recruited by midwives at two freestanding birth centers or contacted the study team directly to participate (1.7%).
To answer main research questions 1 and 4 as well as all secondary research questions, we will compute simple and multiple linear regression analyses. This will allow us to identify factors predicting higher/lower rates of IPV, depression and anxiety, and/or (childbirth-related) PTSD in postpartum women and to investigate factors predicting likelihood of service utilization. To answer main research question 2 and to examine potential differences between treatment and counseling preferences of postpartum women affected vs. those not affected by IPV, depression and anxiety, and/or (childbirth-related) PTSD, we will utilize one-way ANOVA and post-hoc tests to determine specific differences. To answer main research question 3 and to specify the type of treatment and counseling service, professional service provider, and service delivery mode postpartum women affected vs. not affected by IPV, depression and anxiety, and/or (childbirth-related) PTSD prefer, we will utilize one-way MANOVA and MANCOVA and post-hoc tests to identify specific differences. For the ANOVA, MANOVA, and MANCOVA, participating women will be divided into groups depending on their scores on the VAWI, EPDS, SCL-90-R, City BiTS, and PC-PTSD-5. Group allocation will be performed using the respective questionnaire’s cut-off score. Women scoring below the cut-off will be considered as not affected (i.e., they imagined being affected by any of the issues to answer the questions on treatment and counseling preferences).
An a priori power analysis was computed using G*Power 3.1.9.2 (132) to determine the required sample size. Because the main research questions investigate group differences between women with and without experience of IPV, postpartum depression and anxiety, and/or (childbirth-related) PTSD regarding treatment and counseling preferences, the power analysis was computed for independent samples t-tests. Other research questions will be investigated through multiple linear regression analyses—the interim sample is already large enough to detect small effects with sufficient power (results not shown). Results of the power analysis for independent samples t-tests indicated that a total sample of n = 1,360 women is needed to detect small effects (d = 0.2) with 80% (1-beta) power and alpha at 0.05, with a prevalence of 17.5% for postpartum depression and anxiety (24–26). Moreover, according to a recent meta-analysis, the prevalence of significant levels of childbirth-related posttraumatic stress symptoms is estimated at 13% (133), thus requiring a sample size of n = 1,740 to detect a small-sized effect with 80% power. For IPV, the prevalence for physical and sexual violence during the last 12 months is estimated at 3% in Germany (21), which results in an estimated required sample size of n = 6,678 to detect small-sized effects with a power of 80%. As it might not be feasible to recruit this many women for the study, we may only be able to detect medium (d = 0.5) or large effects (d = 0.8) for physical and sexual IPV, requiring samples of n = 1,072 and n = 424 women, respectively. For psychological violence by a current or former partner on the other hand, the prevalence is estimated at 50% in Germany (21), which corresponds to a required sample size of n = 788 to detect small effects.
Given these analyses, a minimum of n = 1,740 women has to be interviewed for our study to detect small effects for postpartum depression, anxiety, childbirth-related posttraumatic stress symptoms, and psychological IPV and medium effects for physical and sexual IPV with a power of at least 80% and alpha at 0.05. However, according to our current estimation, we will recruit at least n = 4,000 women until the end of the study’s funding period, which provides us with a highly powered study to detect even smaller effects and include potential confounding variables in our analyses as well.
Although recruitment is ongoing, we already have a large enough interim sample to compute multiple linear regression analyses examining risk and protective factors for IPV, postpartum depression and anxiety, and (childbirth-related) PTSD and examining the predictive value of several factors for service utilization.
Below, preliminary results regarding the sample of the INVITE study are presented.
Preliminary sociodemographic characteristics of the sample are presented in Table 3. The mean age of participating mothers was 32.5 years (SD = 4.5; Range = 19--51). The majority (91.0%) was born in Germany and had German nationality (93.7%). Compared to Dresden’s general population,2 our sample had a slightly lower rate of women without German nationality [6.3 vs. 8.6%; (134)]. Among mothers without German nationality, most had a permanent residence status (69.6%). Nearly all participants were currently in a partnership (97.8%). The majority (64.6%) had a subject-related or higher education entrance qualification (A-level) and a university degree (48.1%). Compared to the general German (135) and Dresden population (136), our sample is characterized by a high educational and professional status. Slightly more than half the women were primiparous (51.2%) and on average, the interviews were held 12.1 weeks after birth (SD = 2.6; Range = 4–45).
Table 4 displays birth-related characteristics of the sample. Most mothers gave birth to one child (97.9%) with the rest giving birth to twins. The sex ratio of the children was nearly balanced with 50.2% being female. On average, women gave birth at 39.9 weeks of gestation (SD = 1.5; Range = 30--43) and the pre-term birth rate was 6.1%. The latter is slightly lower than the German average of 8.2%3 (137). Most mothers delivered vaginally (74.2%) and the rate of cesarean sections was 19.2%, which is low compared to the German average of 30.9% (137) and slightly lower than the Dresden average of 21.3% (138).
Examining experiences of IPV, symptoms of depression and anxiety, and (childbirth-related) PTSD in postpartum women, the INVITE study is one of the first studies to assess and compare counseling and treatment preferences as well as barriers to help seeking among mothers affected by IPV and postpartum mental health problems vs. those who are not affected.
In sum, the INVITE study has various major strengths. It is one of the first studies to examine differential risk and protective factors for IPV, depression, anxiety, and (childbirth-related) PTSD in postpartum women, which will enable us to also explore comorbidities and concomitant special needs of affected women. Moreover, our study not only analyzes women’s knowledge on and previous experience with various German service providers, but also their preferences for these services and service delivery modes. Asking about different providers from the social, psychosocial, and medical sector will identify specific services that postpartum women may find especially helpful and should therefore be advertised and recommended to mothers experiencing IPV or showing signs of postpartum depression, anxiety, and/or (childbirth-related) PTSD. Furthermore, the INVITE study considers possible barriers to treatment and counseling services based on the Health Belief Model (120). This will enable us to identify reasons for a potentially low utilization of services among postpartum women and ways to improve existing services. Because several instruments (e.g., birth satisfaction and IPV) were not available in German and thus had to be translated by our team, we plan to conduct several validation studies. This way, we will further contribute to adequately assessing IPV and mental health related issues in postpartum women in German-speaking regions.
Additionally, due to our successful recruitment method, we are able to reach most women giving birth in Dresden. In fact, almost 5,000 women were approached for our study in the first 12 months of recruitment compared to 5,747 live births in Dresden in 2020 (139). By increasing the proportion of proactive outreach through our student assistants (instead of passive recruitment through hospital staff), we were able to steadily increase our participation rate to 60–80%. This is not yet reflected in the presented interim sample because proactive outreach was only implemented in all hospitals in July 2021 due to COVID-19-related restrictions. Despite this delay in recruitment, we would already be able to address several of our research questions.
Another strength of the INVITE study is the ability to capture a genuine image of the experience of IPV, postpartum depression and anxiety, and (childbirth-related) PTSD and respective treatment and counseling services among women with a migrant background in Germany. Previous research has often been limited in generalizability by under-representing migrant populations, especially in the context of IPV and mental health (140–142). Because women with a migrant background may encounter specific challenges regarding treatment and counseling [e.g., language barriers, needing an interpreter, and corresponding costs as well as additional expenditure of time; (143)], it is especially important to assess these women’s preferences and barriers to better tailor services to their needs. Offering the interview in both German and English has resulted in a participation rate of women with a migrant background which is close to the rate in the general population of Dresden.
Finally, the INVITE study collaborates with the INTERSECT study (94), which assesses birth trauma and childbirth-related PTSD across low-, middle-, and high-income countries and therefore offers the opportunity for cross-cultural comparisons on various variables, including prevalence of childbirth-related PTSD, differences in symptom presentation, and etiology. In addition, most participating countries also assess birth satisfaction and postpartum depression, and some investigate IPV, which will facilitate comparing prevalence and characteristics of these issues as well. Next to these data, we will have access to information about the context of maternity care in the respective countries (e.g., private vs. public health care, service providers, service utilization rate, and obstetric intervention rates). This information will enable us to interpret the cross-cultural comparisons of various factors against the background of care provided to postpartum women within these countries. Thus, while the INVITE study is of outmost national importance due to its detailed assessment of postpartum women in Germany, the collaboration with the INTERSECT study expands this importance to an international level.
First results on the interim sample show that women participating in the INVITE study are characterized by a rather high educational and professional level compared to the general German population (135) and the population of Dresden (136). This is in line with previous research on large epidemiological studies (95, 144, 145) and indicates that our results might not be generalizable to less educated samples. However, our sample is comprised of almost equal amounts of primiparous and multiparous women. This is important for differential analyses regarding birth-related characteristics, because parity has been identified as a significant covariate in some studies, for example on birth experience (146, 147). The interim sample further mostly includes mothers who had a vaginal birth as can be expected for Dresden (138), where the rate of cesarean sections is low compared to the national average. Moreover, the rate of pre-term births in our sample was slightly lower than the national average (137). This may be explained by pre-term babies needing extensive and time-consuming care and mothers of these babies therefore not feeling capable of doing a long telephone interview but could also be a normal variation in numbers.
To summarize, the data generated by the present study will set the ground for a set of future publications that in turn will serve for a well-aimed development of treatment and counseling services for the respective target groups. These publications will primarily answer our main and secondary research questions. Further publications in collaboration with the INTERSECT study are also planned in the context of providing cross-cultural comparisons. Moreover, validation studies will be published for the utilized instruments for IPV and birth satisfaction. This will further enhance future research methodology in the present context. Hence, the INVITE study will improve current health care system services by informing health care professionals and policy makers about specific barriers to treatment and will thus yield the possibility to tailor services to the preferences of postpartum women. Beyond that, we will deliver important information on how to prevent IPV, postpartum depression and anxiety, and (childbirth-related) PTSD in the first place. Through the telephone interviews and by offering women a list with suitable treatment and counseling services in Dresden, we create awareness and encourage treatment or preventive steps before women get to the point where those experiences are seriously influencing their quality of life and interaction with their families. Finally, the results of the INVITE study are not only important on a scientific level, but also of socio-political relevance. Informing policy makers and politicians about the results of the study may help generate more political interest in these pressing issues for women and their families. In particular information on specific services, which women find helpful may drive decision makers to rearrange attention and funding to these services as investing in prevention and delivering effective help decreases long-term health-care costs (41).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Faculty of Medicine of the Technische Universität Dresden. The patients/participants provided their written informed consent to participate in this study.
SG-N and JS acquired funding and were responsible for conception and design of the INVITE study as well as the coordination and supervision of the (ongoing) data collection. LS, AM, and FT supported the conduction of the study and data collection. AM and LS prepared the data for statistical analysis and wrote the first draft of the manuscript. LS performed the statistical analysis. All authors contributed to manuscript revision, read, and approved the submitted version.
The INVITE study was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation; GA 2287/7-1 and SCHE 1986/6-1). This paper contributes to the EU COST Action 18211 supported by COST (European Cooperation in Science and Technology).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We want to thank all participating women for supporting our project. We would also like to thank all cooperating hospitals, birthing centers, and midwives for providing access to the potential participants as well as all student assistants for performing the recruitment and telephone interviews. Also, LS, FT, and SG-N are (management committee) members of COST action CA18211: DEVOTION: Perinatal Mental Health and Birth-Related Trauma: Maximizing best practice and optimal outcomes.
1. Ashford MT, Ayers S, Olander EK. Supporting women with postpartum anxiety: exploring views and experiences of specialist community public health nurses in the UK. Health Soc Care Commun. (2017) 25:1257–64. doi: 10.1111/HSC.12428
2. Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Health care utilization and costs associated with physical and nonphysical-only intimate partner violence. Health Serv Res. (2009) 44:1052–67. doi: 10.1111/j.1475-6773.2009.00955.x
3. Garthus-Niegel S, Horsch A, Handtke E, von Soest T, Ayers S, Weidner K, et al. The impact of postpartum posttraumatic stress and depression symptoms on couples’ relationship satisfaction: a population-based prospective study. Front Psychol. (2018) 9:1728. doi: 10.3389/fpsyg.2018.01728
4. Moore Simas TA, Huang MY, Patton C, Reinhart M, Chawla AJ, Clemson C, et al. The humanistic burden of postpartum depression: a systematic literature review. Curr Med Res Opin. (2018) 35:383–93. doi: 10.1080/03007995.2018.1552039
5. Peterson C, Kearns MC, McIntosh WL, Estefan LF, Nicolaidis C, McCollister KE, et al. Lifetime economic burden of intimate partner violence among US adults. Am J Prev Med. (2018) 55:433–44. doi: 10.1016/j.amepre.2018.04.049
6. Howard LM, Oram S, Galley H, Trevillion K, Feder G. Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med. (2013) 10:e1001452. doi: 10.1371/journal.pmed.1001452
7. Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P. WHO European review of social determinants of health and the health divide. Lancet. (2012) 380:1011–29. doi: 10.1016/S0140-6736(12)61228-8
8. World Health Organization [WHO].Global Plan of Action to Strengthen the Role of the Health System within A National Multisectoral Response to Address Interpersonal Violence, in Particular Against Women and Girls, and Against Children. (2016). Geneva: World Health Organization
9. Agerholm J, Bruce D, BurstrÃm B, Ponce Leon A. Socioeconomic differences in healthcare utilization, with and without adjustment for need: an example from Stockholm, Sweden. Scand J Public Health. (2013) 41:318–25. doi: 10.1177/1403494812473205
10. Fish JN, Turpin RE, Williams ND, Boekeloo BO. Sexual identity differences in access to and satisfaction with health care: findings from nationally representative data. Am J Epidemiol. (2021) 190:1281–93. doi: 10.1093/aje/kwab012
11. Richardson LD, Norris M. Access to health and health care: how race and ethnicity matter. Mt Sinai J Med. (2010) 77:166–77. doi: 10.1002/msj.20174
12. World Health Organization [WHO].Understanding and Addressing Violence Against Women: Intimate Partner Violence. (2012). Geneva: World Health Organization.
13. Finnbogadóttir H, Baird K, Thies-Lagergren L. Birth outcomes in a Swedish population of women reporting a history of violence including domestic violence during pregnancy: a longitudinal cohort study. BMC Pregnancy Childbirth (2020) 20:183. doi: 10.1186/S12884-020-02864-5/TABLES/5
14. The European Institute for Gender Equality.Understanding Intimate Partner Violence in the EU: The Role of Data. Vilnius, LT: The European Institute for Gender Equality. (2019). doi: 10.2839/926986
15. Ellsberg M, Jansen HAFM, Heise L, Watts CH, García-Moreno C. IPV and womens physical and mental health in the WHO multi-country study on womens health and domestic violence: an observational study. Lancet. (2008) 371:1165–72. doi: 10.1016/s0140-6736(08)60522-x
16. Ferrari G, Agnew-Davies R, Bailey J, Howard L, Howarth E, Peters TJ, et al. Domestic violence and mental health: a cross-sectional survey of women seeking help from domestic violence support services. Glob Health Action. (2014) 7:25519. doi: 10.3402/gha.v7.25519
17. Devries KM, Kishor S, Johnson H, Stöckl H, Bacchus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. (2010) 18:158–70. doi: 10.1016/S0968-8080(10)36533-5
18. Rose L, Althusen J, Bhandari S, Soeken K, Marcantonio K, Bullock L, et al. Impact of intimate partner violence on pregnant women’s mental health: mental distress and mental strength. Issues Ment Health Nurs. (2010) 31:103–11. doi: 10.3109/01612840903254834
19. Devries KM, Mak JYT, García-Moreno C, Petzold M, Child JC, Falder G, et al. The global prevalence of intimate partner violence against women. Science. (2013) 340:1527–8. doi: 10.1126/science.1240937
20. Heise LL, Kotsadam A. Cross-national and multilevel correlates of partner violence: an analysis of data from population-based surveys. Lancet Glob Health. (2015) 3:e332–40. doi: 10.1016/S2214-109X(15)00013-3
21. European Union Agency for Fundamental Rights.Violence Against Women: An EU-Wide Survey. Vienna: European Union Agency for Fundamental Rights (2014).
22. Román-Gálvez RM, Martín-Peláez S, Fernández-Félix BM, Zamora J, Khan KS, Bueno-Cavanillas A. Worldwide prevalence of intimate partner violence in pregnancy. A systematic review and meta-analysis. Front Public Health. (2021) 9:1278. doi: 10.3389/FPUBH.2021.738459/BIBTEX
23. Mojahed A, Alaidarous N, Kopp M, Pogarell A, Thiel F, Garthus-Niegel S. Prevalence of intimate partner violence among intimate partners during the perinatal period: a narrative literature review. Front Psychiatry. (2021) 12:601236. doi: 10.3389/FPSYT.2021.601236
24. Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front Psychiatry. (2018) 8:248. doi: 10.3389/fpsyt.2017.00248
25. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
26. Fawcett EJ, Fairbrother N, Cox ML, White IR, Fawcett JM. The prevalence of anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry. (2019) 80:18r12527. doi: 10.4088/jcp.18r12527
27. McCarthy M, Houghton C, Matvienko-Sikar K. Women’s experiences and perceptions of anxiety and stress during the perinatal period: a systematic review and qualitative evidence synthesis. BMC Pregnancy Childbirth. (2021) 21:811. doi: 10.1186/s12884-021-04271-w
28. O’Mahony JM, Donnelly T. Immigrant and refugee women’s post-partum depression help-seeking experiences and access to care: a review and analysis of the literature. J Psychiatr Ment Health Nurs. (2010) 17:917–28. doi: 10.1111/j.1365-2850.2010.01625.x
29. Goodman JH, Watson GR, Stubbs B. Anxiety disorders in postpartum women: a systematic review and meta-analysis. J Affect Disord. (2016) 203:292–331. doi: 10.1016/j.jad.2016.05.033
30. Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health. (2019) 15:1745506519844044. doi: 10.1177/1745506519844044
31. Chang J, Berg CJ, Saltzman LE, Herndon J. Homicide: a leading cause of injury deaths among pregnant and postpartum women in the United States, 1991-1999. Am J Public Health. (2005) 95:471–7. doi: 10.2105/AJPH.2003.029868
32. Wisner KL, Chambers C, Sit DKY. Postpartum Depression: a Major Public Health Problem. JAMA. (2006) 296:2216–618. doi: 10.6224/JN.60.6.22
33. Choi KW, Houts R, Arseneault L, Pariante C, Sikkema KJ, Moffitt TE. Maternal depression in the intergenerational transmission of childhood maltreatment and its sequelae: testing postpartum effects in a longitudinal birth cohort. Dev Psychopathol. (2018) 31:143–156. doi: 10.1017/S0954579418000032
34. Earls MF, Siegel BS, Dobbins MI, Garner AS, McGuinn L, Pascoe J, et al. Clinical report - Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. (2010) 126:1032–9. doi: 10.1542/peds.2010-2348
35. Madlala SS, Kassier SM. Antenatal and postpartum depression: effects on infant and young child health and feeding practices. S Afr J Clin Nutr. (2018) 31:1–7. doi: 10.1080/16070658.2017.1333753
36. Junge C, Garthus-Niegel S, Slinning K, Polte C, Simonsen TB, Eberhard-Gran M. The impact of perinatal depression on children’s social-emotional development: a longitudinal study. Matern Child Health J. (2017) 21:607–15. doi: 10.1007/s10995-016-2146-2
37. Martini J, Petzoldt J, Knappe S, Garthus-Niegel S, Asselmann E, Wittchen H-U. Infant, maternal, and familial predictors and correlates of regulatory problems in early infancy: the differential role of infant temperament and maternal anxiety and depression. Early Hum Dev. (2017) 115:23–31. doi: 10.1016/j.earlhumdev.2017.08.005
38. Polte C, Junge C, von Soest T, Seidler A, Eberhard-Gran M, Garthus-Niegel S. Impact of maternal perinatal anxiety on social-emotional development of 2-year-olds, a prospective study of norwegian mothers and their offspring: the impact of perinatal anxiety on child development. Matern Child Health J. (2019) 23:386–96. doi: 10.1007/s10995-018-2684-x
39. Thiel F, Iffland L, Drozd F, Haga SM, Martini J, Weidner K. Specific relations of dimensional anxiety and manifest anxiety disorders during pregnancy with difficult early infant temperament: a longitudinal cohort study. Arch Womens Ment Health. (2020) 23:535–546. doi: 10.1007/s00737-019-01015-w
40. Thiel F, Pittelkow MM, Wittchen HU, Garthus-Niegel S. The relationship between paternal and maternal depression during the perinatal period: a systematic review and meta-analysis. Front Psychiatry. (2020) 11:563287. doi: 10.3389/fpsyt.2020.563287
41. Bauer A, Parsonage M, Knapp M, Iemmi V, Bayo A. The Costs of Perinatal Mental Health Problems. London: Centre for Mental Health. (2014).
42. Dikmen Yildiz P, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord. (2017) 208:634–45. doi: 10.1016/j.jad.2016.10.009
43. Grekin R, O’Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. (2014) 34:389–401. doi: 10.1016/j.cpr.2014.05.003
44. Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol. (2000) 39:35–51. doi: 10.1186/1471-244X-14-200
45. Gottvall K, Waldenström U. Does a traumatic birth experience have an impact on future reproduction? BJOG. (2002) 109:254–60. doi: 10.1111/j.1471-0528.2002.01200.x
46. Slade A. Parental reflective functioning: an introduction. Attach Hum Dev. (2005) 7:269–81. doi: 10.1080/14616730500245906
47. Dekel S, Thiel F, Dishy G, Ashenfarb AL. Is childbirth-induced PTSD associated with low maternal attachment? Arch Womens Ment Health. (2019) 22:119–22. doi: 10.1007/s00737-018-0853-y
48. McKenzie-McHarg K, Ayers S, Ford E, Horsch A, Jomeen J, Sawyer A, et al. Post-traumatic stress disorder following childbirth: an update of current issues and recommendations for future research. J Reprod Infant Psychol. (2015) 33:219–37. doi: 10.1080/02646838.2015.1031646
49. Nicholls K, Ayers S. Childbirth-related post-traumatic stress disorder in couples: a qualitative study. Br J Health Psychol. (2007) 12:491–509. doi: 10.1348/135910706X120627
50. Parfitt YM, Ayers S. The effect of post-natal symptoms of post-traumatic stress and depression on the couple’s relationship and parent-baby bond. J Reprod Infant Psychol. (2009) 27:127–42. doi: 10.1080/02646830802350831
51. Garthus-Niegel S, Ayers S, Martini J, Von Soest T, Eberhard-Gran M. The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychol Med. (2017) 47:161–70. doi: 10.1017/S003329171600235X
52. Garthus-Niegel S, Horsch A, Ayers S, Junge-Hoffmeister J, Weidner K, Eberhard-Gran M. The influence of postpartum PTSD on breastfeeding: a longitudinal population-based study. Birth. (2018) 45:193–201. doi: 10.1111/BIRT.12328
53. Garthus-Niegel S, Horsch A, Bickle Graz M, Martini J, von Soest T, Weidner K, et al. The prospective relationship between postpartum PTSD and child sleep: a 2-year follow-up study. J Affect Disord. (2018) 241:71–9. doi: 10.1016/J.JAD.2018.07.067
54. Lagdon S, Armour C, Stringer M. Adult experience of mental health outcomes as a result of intimate partner violence: a systematic review. Eur J Psychotraumatol. (2014) 5:24794. doi: 10.3402/ejpt.v5.24794
55. Spencer C, Mallory AB, Cafferky BM, Kimmes JG, Beck AR, Stith SM. Mental health factors and intimate partner violence perpetration and victimization: a meta-analysis. Psychol Violence. (2019) 9:1–17. doi: 10.1037/vio0000156
56. Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Trauma Stress. (1992) 5:377–91. doi: 10.1002/JTS.2490050305
57. Davies J, Frawley M. Treating the Adult Survivor of Childhood Sexual Abuse. New York, NY: Basic Books (1994).
58. Griffing S, Lewis CS, Chu M, Sage RE, Madry L, Primm BJ. Exposure to interpersonal violence as a predictor of PTSD symptomatology in domestic violence survivors. J Interpers Violence. (2006) 21:936–54. doi: 10.1177/0886260506288938
59. Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB. Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med. (2012) 75:959–75. doi: 10.1016/j.socscimed.2012.04.025
60. Onoye JM, Goebert D, Morland L, Matsu C, Wright T. PTSD and postpartum mental health in a sample of Caucasian, Asian, and Pacific Islander women. Arch Womens Ment Health. (2009) 12:393–400. doi: 10.1007/s00737-009-0087-0
61. White T, Matthey S, Boyd K, Barnett B. Postnatal depression and post-traumatic stress after childbirth: prevalence, course and co-occurrence. J Reprod Infant Psychol. (2006) 24:107–20. doi: 10.1080/02646830600643874
62. Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD Symptomatology and Mental Health During Pregnancy and Postpartum. Arch Womens Ment Health. (2013) 16:453–63. doi: 10.1007/s00737-013-0365-8.Changes
63. Cohen MM, Schei B, Ansara D, Gallop R, Stuckless N, Stewart DE. A history of personal violence and postpartum depression: is there a link? Arch Womens Ment Health. (2002) 4:83–92. doi: 10.1007/s007370200004
64. Plaza A, Garcia-Esteve L, Torres A, Ascaso C, Gelabert E, Luisa Imaz M, et al. Childhood physical abuse as a common risk factor for depression and thyroid dysfunction in the earlier postpartum. Psychiatry Res. (2012) 200:329–35. doi: 10.1016/j.psychres.2012.06.032
65. Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. J Midwifery Womens Health. (2013) 58:57–68. doi: 10.1111/j.1542-2011.2012.00237.x
66. Oz Y, Sarid O, Peleg R, Sheiner E. Sense of coherence predicts uncomplicated delivery: a prospective observational study. J Psychosom Obstet Gynecol. (2009) 30:29–33. doi: 10.1080/01674820802546196
67. Segal-Engelchin D, Sarid O, Cwikel J. Pregnancy, childbirth and postpartum experiences of israeli women in the negev. J Prenat Perinat Psychol Health. (2009) 24:3. doi: 10.1016/j.midw.2015.02.011
68. Oh W, Muzik M, Waxler, McGinnis E, Hamilton L, Menke RA, et al. Comorbid trajectories of postpartum depression and PTSD among mothers with childhood trauma history: course, predictors, processes and child adjustment. J Affect Disord. (2016) 200:133–41. doi: 10.1016/j.jad.2016.04.037
69. Söderquist J, Wijma B, Thorbert G, Wijma K. Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG. (2009) 116:672–80. doi: 10.1111/j.1471-0528.2008.02083.x
70. van Son MJM, Verkerk G, van der Hart O, Komproe I, Pop V. Prenatal depression, mode of delivery and perinatal dissociation as predictors of postpartum posttraumatic stress: an empirical study. Clin Psychol Psychother. (2005) 12:297–312. doi: 10.1002/cpp.446
71. Fugate M, Landis L, Riordan K, Naureckas S, Engel B. Barriers to domestic violence help seeking: implications for intervention. Violence Against Women. (2005) 11:290–310. doi: 10.1177/1077801204271959
72. Garcia-Moreno C, Watts C. Violence against women: an urgent public health priority. Bull World Health Org. (2011) 89:2. doi: 10.1067/mob.2003.274
73. Graß HL, Gahr B, Ritz-Timme S. Umgang mit Opfern von häuslicher Gewalt in der ärztlichen Praxis: anregungen für den Praxisalltag. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2016) 59:81–7. doi: 10.1007/s00103-015-2269-4
74. Schellong J, Epple F, Lorenz P, Ritschel G, Croy I, Lenk M, et al. Häusliche Gewalt und Partnerschaftsgewalt - eine Herausforderung im Gesundheitssektor. Psychiatr Prax. (2021). [Epub ahead of print]. doi: 10.1055/a-1630-4619
75. Edhborg M, Lundh W, Widström AM, Friberg M. “Struggling with life”: narratives from women with signs of postpartum depression. Scand J Public Health. (2005) 33:261–7. doi: 10.1080/14034940510005725
76. Nicole L, Duffett-Leger L, Stewart M, Hegadoren K, Dennis CL, Rinaldi CM, et al. Canadian mothers’ perceived support needs during postpartum depression. J Obstet Gynecol Neonatal Nurs. (2007) 36:441–9. doi: 10.1111/j.1552-6909.2007.00174.x
77. Cirino NH, Knapp JM. Perinatal posttraumatic stress disorder: a review of risk factors, diagnosis, and treatment. Obstet Gynecol Surv. (2019) 74:369–76. doi: 10.1097/01.pec.0000526609.89886.37
78. Fitelson E, Kim S, Baker AS, Leight K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health. (2011) 3:1–14. doi: 10.2147/IJWH.S6938
79. Green SM, Donegan E, McCabe RE, Streiner DL, Agako A, Frey BN. Cognitive behavioral therapy for perinatal anxiety: a randomized controlled trial. Aust. N Z J Psychiatry. (2020) 54:423–32. doi: 10.1177/0004867419898528
80. Loughnan SA, Wallace M, Joubert AE, Haskelberg H, Andrews G, Newby JM. A systematic review of psychological treatments for clinical anxiety during the perinatal period. Arch Womens Ment Health. (2018) 21:481–90. doi: 10.1007/s00737-018-0812-7
81. Marchesi C, Ossola P, Amerio A, Daniel BD, Tonna M, De Panfilis C. Clinical management of perinatal anxiety disorders: a systematic review. J Affect Disord. (2016) 190:543–50. doi: 10.1016/j.jad.2015.11.004
82. Shulman B, Dueck R, Ryan D, Breau G, Sadowski I, Misri S. Feasibility of a mindfulness-based cognitive therapy group intervention as an adjunctive treatment for postpartum depression and anxiety. J Affect Disord. (2018) 235:61–7. doi: 10.1016/J.JAD.2017.12.065
83. Field T. Postpartum anxiety prevalence, predictors and effects on child development: a review. J Psychiatry Psychiatr Disord. (2017) 1:86–102. doi: 10.26502/jppd.2572-519x0010
84. Woolhouse H, Brown S, Krastev A, Perlen S, Gunn J. Seeking help for anxiety and depression after childbirth: results of the Maternal Health Study. Arch Womens Ment Health. (2009) 12:75–83. doi: 10.1007/s00737-009-0049-6
85. Taubman-Ben-Ari O, Rabinowitz J, Feldman D, Vaturi R. Post-traumatic stress disorder in primary-care settings: prevalence and physicians’ detection. Psychol Med. (2001) 31:555–60. doi: 10.1017/s0033291701003658
86. Einarson A, Davis W. Barriers to the pharmacological treatment of women with psychiatric disorders during pregnancy and breastfeeding: results of a survey. J Obstet Gynaecol Can. (2013) 35:504–5. doi: 10.1016/S1701-2163(15)30905-1
87. McLoughlin J. Stigma associated with postnatal depression: a literature review. Br J Midwifery. (2013) 21:784–91. doi: 10.12968/bjom.2013.21.11.784
88. Moore D, Ayers S, Drey N. A thematic analysis of stigma and disclosure for perinatal depression on an online forum. JMIR Ment Healh. (2016) 3:e18. doi: 10.2196/mental.5611
89. Puhlman DJ, Pasley K. Rethinking maternal gatekeeping. J Fam Theory Rev. (2013) 5:176–93. doi: 10.1111/JFTR.12016
90. Zvara BJ, Schoppe-Sullivan SJ, Dush CK. Fathers’ involvement in child health care: associations with prenatal involvement, parents’ beliefs, and maternal gatekeeping. Fam Relat. (2013) 62:649–61. doi: 10.1111/FARE.12023
91. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
92. Liang B, Goodman LA, Tummala-Narra P, Weintraub S. A theoretical framework for understanding help-seeking processes among survivors of intimate partner violence. Am J Commun Psychol. (2005) 36:71–84. doi: 10.1007/s10464-005-6233-6
93. Haggerty LA, Goodman LA. Stages of change-based nursing interventions for victims of interpersonal violence. J Obstet Gynecol Neonatal Nurs. (2003) 32:68–75. doi: 10.1177/0884217502239802
94. INTERSECT.Study Registration of the International Survey of Childbirth-Related Trauma (INTERSECT). (2021). Available online at: https://www.researchregistry.com/browse-the-registry#home/registrationdetails/5ffc7453702012001b80a58c/ (accessed December 14, 2021).
95. Kress V, Steudte-Schmiedgen S, Kopp M, Förster A, Altus C, Schier C, et al. The impact of parental role distributions, work participation, and stress factors on family health-related outcomes: study protocol of the prospective multi-method cohort “Dresden Study on Parenting, Work, and Mental Health” (DREAM). Front Psychol. (2019) 10:1273. doi: 10.3389/fpsyg.2019.01273
96. German National Cohort Consortium. The German National Cohort: aims, study design and organization. Eur J Epidemiol. (2014) 29:371–82. doi: 10.1007/s10654-014-9890-7
97. TNS Infratest Sozialforschung.SOEP 2016 - Erhebungsinstrumente 2016 (Welle 33) des Sozio-oekonomischen Panels: Personenfragebogen, Stichproben A-L3, SOEP Survey Papers, No. 345. Berlin: Deutsches Institut Für Wirtschaftsforschung (2016).
98. Lampert T, Kroll LE. Die Messung des sozioökonomischen Status in sozialepidemiologischen Studien. In: M Richter, K Hurrelmann editors. Gesundheitliche Ungleichheit: Grundlagen, Probleme, Perspektiven. New York, NY: VS Verlag für Sozialwissenschaften (2009). p. 309–34. doi: 10.1007/978-3-531-91643-9_18
99. Junge C, von Soest T, Weidner K, Seidler A, Eberhard-Gran M, Garthus-Niegel S. Labor pain in women with and without severe fear of childbirth: a population-based, longitudinal study. Birth. (2018) 45:469–77. doi: 10.1111/birt.12349
100. Gemeinsamer Bundesausschuss.Mutterpass Richtlinien über die ärztliche Betreuung während der Schwangerschaft und nach der Entbindung: Mutterschafts-Richtlinien. Berlin: Gemeinsamer Bundesausschuss. (2015).
101. Hollins Martin CJ, Martin CR. Development and psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R). Midwifery. (2014) 30:610–9. doi: 10.1016/j.midw.2013.10.006
102. Ayers S, Wright DB, Thornton A. Development of a measure of postpartum PTSD: the city birth trauma scale. Front Psychiatry. (2018) 9:409. doi: 10.3389/fpsyt.2018.00409
103. Weigl T, Beck-Hiestermann FML, Stenzel NM, Benson S, Schedlowski M, Garthus-Niegel S. Assessment of childbirth-related PTSD: psychometric properties of the German Version of the City Birth Trauma Scale. Front Psychiatry. (2021) 12:731537. doi: 10.3389/fpsyt.2021.731537
104. Gemeinsamer Bundesausschuss.Kinder-Untersuchungsheft. Richtlinien über die Früherkennung von Krankheiten bei Kindern bis zur Vollendung des 6. Lebensjahres: Kinder-Richtlinien. Berlin: Gemeinsamer Bundesausschuss. (2016).
105. Thomson RM, Allely CS, Purves D, Puckering C, McConnachie A, Johnson PCD, et al. Predictors of positive and negative parenting behaviours: evidence from the ALSPAC cohort. BMC Pediatr. (2014) 14:247. doi: 10.1186/1471-2431-14-247
106. Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. Deutschsprachige Fassung und validierung der edinburgh postnatal depression scale. Dtsch Med Wochenschr. (1998) 123:35–40. doi: 10.1055/s-2007-1023895
107. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
108. Franke GH. SCL-90-R: Symptom-Checkliste von L. R. Derogatis; Dt. Version. Göttingen: Beltz Test (2002).
109. Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. (2016) 31:1206–11. doi: 10.1007/s11606-016-3703-5
110. Foa EB, Mclean CP, Zang Y, Zhong J, Rauch S, Porter K, et al. Psychometric properties of the posttraumatic diagnostic scale for DSM–5 (PDS–5). Psychol Assess. (2016) 28:1166–71. doi: 10.1037/pas0000258
111. Schumacher J, Leppert K, Gunzelmann T, Strauß B, Brähler E. Die Resilienzskala - Ein fragebogen zur erfassung der psychischen widerstandsfähigkeit als personmerkmal. Z Klin Psychol Psychiatr Psychother. (2005) 53:16–39.
112. European Commission.Special Eurobarometer 449 - “Gender-based violence” Report. Brussels: European Commission. (2017). doi: 10.2838/009088
113. Ellsberg M, Heise L. Researching Violence Against Women: A Practical Guide for Researchers and Activists. Geneva: World Health Organization (2005).
114. Simhi M, Sarid O, Cwikel J. Preferences for mental health treatment for post-partum depression among new mothers. Isr J Health Policy Res. (2019) 8:84. doi: 10.1186/s13584-019-0354-0
115. Castonguay J, Filer CR, Pitts MJ. Seeking help for depression: applying the health belief model to illness narratives. South Commun J. (2016) 81:289–303. doi: 10.1080/1041794X.2016.1165729
116. Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. (2009) 36:60–9. doi: 10.1111/j.1523-536X.2008.00296.x
117. Henshaw EJ, Freedman-Doan CR. Conceptualizing mental health care utilization using the health belief model. Clin Psychol. (2009) 16:420–39. doi: 10.1111/j.1468-2850.2009.01181.x
118. Langley EL, Wootton BM, Grieve R. The utility of the health belief model variables in predicting help-seeking intention for anxiety disorders. Aust Psychol. (2018) 53:291–301. doi: 10.1111/ap.12334
119. Marques L, LeBlanc NJ, Wegarden HM, Timpano KR, Jenike M, Wilhelm S. Barriers to treatment and service utilization in an internet sample of individuals with obsessive-compulsive symptoms. Depress Anxiety. (2010) 27:470–5. doi: 10.1002/da.20694
120. Rosenstock IM. Historical origins of the health belief model. Health Educ Behav. (1974) 2:328–35. doi: 10.1177/109019817400200403
121. Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. In: RJ DiClemente, JL Peterson editors. Preventing AIDS. AIDS Prevention and Mental Health. Heidelberg: Springer (1994). doi: 10.1007/978-1-4899-1193-3_2
122. Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. J Couns Psychol. (2006) 53:325–37. doi: 10.1037/0022-0167.53.3.325
123. Fydrich T, Sommer G, Tydecks S, Brähler E. Fragebogen zur sozialen Unterstützung (F-SozU) Normierung der Kurzform (K-14). Z Med Psychol. (2009) 18:43–8.
124. World Health Organization [WHO].WHO Multi-Country Study On Women’s Health And Domestic Violence Against Women: Summary Report of Initial Results on Prevalence, Health Outcomes and Women’s Responses. (2005). Geneva: World Health Organization
125. Nybergh L, Taft C, Krantz G. Psychometric properties of the WHO violence against women instrument in a female population-based sample in Sweden: a cross-sectional survey. BMJ Open. (2013) 3:e002053. doi: 10.1136/bmjopen-2012-002053
126. World Health Organization [WHO].Process of Translation and Adaptation of Instruments. Geneva: World Health Organization. (2016).
127. Weigl T, Garthus-Niegel S. Questionnaires for the Assessment of Peripartum Depression, Anxiety and Stress (Part 1 of a series on psychological assessment during the peripartum period). Z Geburtshilfe Neonatol. (2021) 225:300–5. doi: 10.1055/A-1471-7256
128. Krüger-Gottschalk A, Knaevelsrud C, Rau H, Dyer A, Schäfer I, Schellong J, et al. The german version of the posttraumatic stress disorder checklist for DSM-5 (PCL-5): psychometric properties and diagnostic utility. BMC Psychiatry. (2017) 17:379. doi: 10.1186/s12888-017-1541-6
129. Harrison SE, Ayers S, Quigley MA, Stein A, Alderdice F. Prevalence and factors associated with postpartum posttraumatic stress in a population-based maternity survey in England. J Affect Disord. (2021) 279:749–56. doi: 10.1016/j.jad.2020.11.102
130. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
131. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
132. Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/bf03193146
133. Heyne C-S, Kazmierczak M, Souday R, Horesh D, Lambregtse-van den Berg M, Weigl T, et al. Prevalence and Risk Factors of Birth-Related Posttraumatic Stress Among Parents: A Comparative Systematic Review and Meta-Analysis. (n.d.).
134. Landeshauptstadt Dresden.Dresden in Zahlen IV. Quartal 2020. (2020). Available online at: https://www.dresden.de/media/pdf/statistik/Dresden_in_Zahlen_2020_IV_Quartal.pdf (accessed December 14, 2021).
135. Statistisches Bundesamt.Bildungsstand der Bevölkerung. Wiesbaden: Statistisches Bundesamt. (2020).
136. Statistisches Landesamt des Freistaates Sachsen.Mikrozensusergebnisse: Bevölkerung nach Schulabschluss und Berufsabschluss. (2018). Available online at: https://www.dresden.de/media/pdf/statistik/Statistik_1601_Ausbildung_Mikrozensus.pdf (accessed December 14, 2021).
137. Institut für Qualitätssicherung und Transparenz im Gesundheitswesen [IQTIG].Bundesauswertung zum Erfassungsjahr 2019. Geburtshilfe Qualitätsindikatoren. Berlin: Institut für Qualitätssicherung und Transparenz im Gesundheitswesen. (2020).
138. Statistisches Landesamt des Freistaates Sachsen.Krankenhausstatistik 2019, Teil I - Grunddaten. Kamenz: Statistisches Landesamt des Freistaates Sachsen. (2021).
139. Melderegister der LH Dresden.Bevölkerungsbewegung. (2021). Available online at: https://www.dresden.de/de/leben/stadtportrait/statistik/bevoelkerung-gebiet/bevoelkerungsbewegung.php (accessed December 14, 2021).
140. Castaneda AE, Çilenti K, Rask S, Lilja E, Skogberg N, Kuusio H, et al. Migrants are underrepresented in mental health and rehabilitation services—survey and register-based findings of russian, somali, and Kurdish origin adults in Finland. Int J Environ Res Public Health. (2020) 17:6223. doi: 10.3390/ijerph17176223
141. Ghafournia N, Easteal P. Are immigrant women visible in australian domestic violence reports that potentially influence policy? Laws. (2018) 7:32. doi: 10.3390/laws7040032
142. Tabibi J, Baker LL. Exploring the Intersections: Immigrant and Refugee Women Fleeing Violence and Experiencing Homelessness in Canada. London: Centre for Research & Education on Violence Against Women & Children. (2017).
143. Pogarell A, Garthus-Niegel S, Mojahed A, von Verschuer C, Rokyta U, Kummer W, et al. Community case study on trauma-specific treatment and counseling for refugee women exposed to intimate partner violence. Front Psychiatry. (2019) 10:891. doi: 10.3389/fpsyt.2019.00891
144. Keeble C, Baxter PD, Barber S, Law GR. Participation rates in epidemiology studies and surveys : a review 2007 – 2015. Intern J Epidemiol. (2015) 14:1–14. doi: 10.5580/IJE.34897
145. Søgaard AJ, Selmer R, Bjertness E, Thelle D. International journal for equity in health the oslo health study: the impact of self-selection in a large, population-based survey. Int J Equity Health. (2004) 3:3. doi: 10.1186/1475-9276-3-3
146. Seefeld L, Weise V, Kopp M, Knappe S, Garthus-Niegel S. Birth experience mediates the association between fear of childbirth and mother-child-bonding up to 14 months postpartum: findings from the prospective cohort study DREAM. Front Psychiatry. (2022) 12:776922. doi: 10.3389/fpsyt.2021.776922
147. Waldenström U, Hildingsson I, Rubertsson C, Rådestad I. A negative birth experience: prevalence and risk factors in a national sample. Birth. (2004) 31:17–27. doi: 10.1111/j.0730-7659.2004.0270.x
Keywords: intimate partner violence, depression, anxiety, PTSD, childbirth-related PTSD, postpartum women, INVITE study, study protocol
Citation: Seefeld L, Mojahed A, Thiel F, Schellong J and Garthus-Niegel S (2022) Preferences and Barriers to Counseling for and Treatment of Intimate Partner Violence, Depression, Anxiety, and Posttraumatic Stress Disorder Among Postpartum Women: Study Protocol of the Cross-Sectional Study INVITE. Front. Psychiatry 13:836350. doi: 10.3389/fpsyt.2022.836350
Received: 15 December 2021; Accepted: 03 March 2022;
Published: 29 March 2022.
Edited by:
Luca Rollè, University of Turin, ItalyReviewed by:
Elisabete Pereira Silva, Federal University of Pernambuco, BrazilCopyright © 2022 Seefeld, Mojahed, Thiel, Schellong and Garthus-Niegel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lara Seefeld, bGFyYS5zZWVmZWxkQHVuaWtsaW5pa3VtLWRyZXNkZW4uZGU=
†These authors share first authorship
‡These authors share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.