- 1Department of Psychiatry, Social Psychiatry and Psychotherapy, Hannover Medical School, Hanover, Germany
- 2Department of Psychiatry Research, The Zucker Hillside Hospital, Glen Oaks, NY, United States
- 3Department of Psychiatry and Molecular Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, United States
- 4Department of Child and Adolescent Psychiatry, Charité – Universitätsmedizin Berlin, Berlin, Germany
Patients with mental disorders have an increased risk to develop cardiovascular disease (CVD), and CVD are frequently comorbid with especially adjustment, anxiety and depressive disorders. Therefore, clinicians need to be aware of effective and safe psychological and pharmacological treatment strategies for patients with comorbid CVD and mental disorders. Cognitive behavioral therapy and third-wave of cognitive-behavioral therapy are effective for patients with CVD and mental disorders. Internet-based psychological treatments may also be considered. In more severe cases, psychopharmacological drugs are frequently used. Although generally well tolerated and efficacious, drug- and dose-dependent side effects require consideration. Among antidepressants, selective serotonin reuptake inhibitors, selective serotonin and noradrenalin reuptake inhibitors, and newer antidepressants, such as mirtazapine, bupropion, agomelatine, and vortioxetine, can be considered, while tricyclic antidepressants should be avoided due to their cardiac side effects. Mood stabilizers have been associated with arrhythmias, and some first- and second-generation antipsychotics can increase QTc and metabolic side effects, although substantial differences exist between drugs. Benzodiazepines are generally safe in patients with CVD when administered short-term, and may mitigate symptoms of acute coronary syndrome. Laboratory and ECG monitoring is always recommended in psychopharmacological drug-treated patients with CVD. Presence of a heart disease should not exclude patients from necessary interventions, but may require careful risk-benefit evaluations. Effectively and safely addressing mental disorders in patients with CVD helps to improve both conditions. Since CVD increase the risk for mental disorders and vice versa, care providers need to screen for these common comorbidities to comprehensively address the patients’ needs.
Introduction
Severe mental disorders, such as major depressive disorder (MDD), pose a higher risk for the development of cardiovascular disease (CVD), and vice versa (1, 2). In particular, adjustment disorder, anxiety disorders and MDD are more frequent in CVD patients compared to the general population (3, 4). The comorbidity of CVD and mental disorders is associated with worse treatment outcomes and decreased quality of life (3, 5–10). The high prevalence of comorbid severe mental diseases and CVD has been attributed to several contributing factors. In this regard, dysregulation of biological systems as well as adverse health behaviors and insufficient economic and social support have been implied (11–15). Overall, severe mental diseases were found to be associated with pathological alterations in stress response systems, with systemic low-grade inflammation, with abnormalities in heart rate variability, and with reduced baroreflex sensitivity (16–18), and of note similar processes were found to profoundly impact metabolic pathways and subsequent development and progression of CVD (19, 20). Additionally, tobacco and alcohol consumption, a sedentary lifestyle, and poor diet, factors known for their contribution to the onset and progression of CVD, are common in patients with severe mental disorders (11, 12). Finally, patients suffering from mental disorders appear less likely to adhere to treatment regimens and were frequently found to have insufficient access to physical health care (21, 22).
Given the significant impact of mental disorders on the outcome of CVD patients, treatment interventions for comorbid patients are clinically important.
According to national and international guidelines, (23, 24) mental disorders within and without the context of an underlying physical illness can be treated using psychological and psychopharmacological interventions. However, iatrogenic effects of psychotropic medications have been described (1, 25). In this regard, the safety and efficacy of psychotropic medications in patients with CVD varies greatly, depending on drug- as well as disease type (26, 27). Consequently, precise knowledge regarding potential adverse effects of frequently used psychotropic medications, i.e., antipsychotics, antidepressants, and mood stabilizers, on parameters of physical health are indispensable in the treatment of comorbid mental disorders and CVD.
Methods
Narrative review of practical clinical considerations when treating patients with cardiovascular and mental disorders pharmacologically and psychologically for their mental disorders.
Results
Psychopharmacological Interventions
Selective Serotonin Reuptake Inhibitors
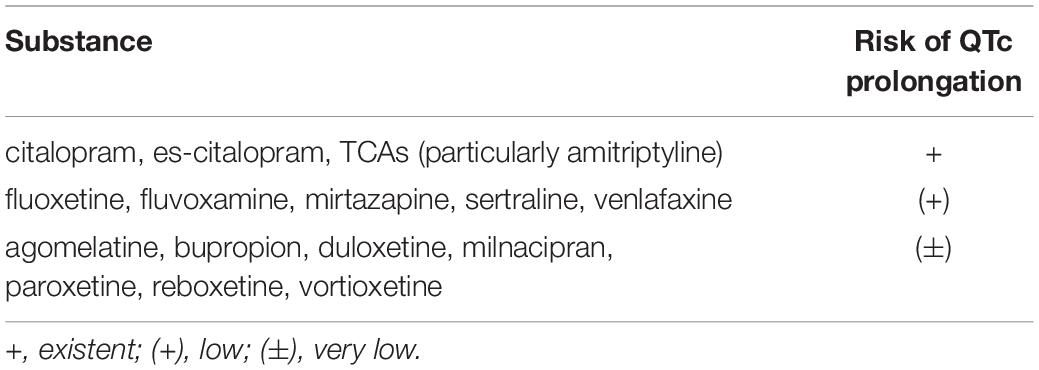
National and international guidelines recommend the use of selective serotonin reuptake inhibitors (SSRIs) for the treatment of MDD and anxiety disorders (23, 24, 28–30). SSRIs are well tolerated in general, and beneficial effects of SSRI treatment in patients with depression following acute coronary syndrome regarding re-hospitalization rates have been shown in a dedicated meta-analysis (31). However, SSRIs pose the risk of cardiovascular side effects in a dose- and substance dependent manner. In principle, all SSRIs can lead to some QTc prolongation. However, especially citalopram (and to a much lesser degree, its enantiomer es-citalopram) pose a relatively higher risk compared to other SSRIs (i.e., fluoxetine, fluvoxamine, paroxetine, sertraline). A meta-analysis revealed that SSRIs as a class increase QTc interval for an average of 6 ms (32). Although on average, this is not clinically relevant, subgroups of patients may experience clinically relevant QTc prolongation. Along with QTc prolongation, the risk for the development of ventricular arrhythmia and Torsades-de-Pointes (TdP) is increased (33–37). Most cases of SSRI-induced QTc interval prolongation and subsequent arrhythmia were observed in older patients above 65 years of age. Further risk factors comprise low potassium levels, female sex, polypharmacy, pre-existing cardiovascular disorders, pre-existing liver and/or kidney disease, and high doses of SSRIs (33, 38, 39). As mentioned above, among the SSRIs, this risk is highest for citalopram and es-citalopram. The United States Food and Drug Administration (FDA) as well as the European Medicines Agency (EMA) accordingly gave a safety warning, recommending doses not higher than 40 mg/day for citalopram and 20 mg/day for es-citalopram (40, 41). The relative risk of QTc prolongation with frequently used antidepressant drugs is summarized in Table 1.
Additionally, among different classes of antidepressants, SSRI treatment was found to be associated with the highest risk for hyponatraemia, brought forward by a drug-induced syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH) (42). While conclusive evidence for differences of individual SSRIs regarding SIADH risk are lacking (43), two larger studies reported lower risks for paroxetine and sertraline compared to other SSRIs including fluoxetine, citalopram, and es-citalopram (44–47). Moreover, elevated SIADH risk under SSRI treatment has been found in the geriatric population and especially in concomitant (thiazide) diuretics (42, 48).
Further side effects of SSRIs with possible cardiovascular relevance are orthostatic hypotension, primarily in elderly patients (49–52), and impaired platelet activation and aggregation, possibly leading to an increased risk for intracerebral hemorrhages (45, 53–56). Therefore, SSRI treatment should be given carefully in patients with underlying hemostatic abnormalities and on anticoagulation treatment; additionally, non-steroidal anti-inflammatory drugs (NSAID) should not be given in SSRI treated patients (32, 57–59).
Serotonin Norepinephrine Reuptake Inhibitors
Serotonin norepinephrine reuptake inhibitors (SNRIs), particularly venlafaxine, can increase heart rate and blood pressure due to their noradrenergic effects (60–65). Among the SNRIs, venlafaxine and duloxetine may be associated with a possible risk of QTc prolongation, particularly in overdose situations (66, 67). Milnacipran, levomilnacipran and reboxetine have sometimes been associated with hypotension, particularly when administered at higher dosages (68–70). Albeit less frequent compared to SSRIs, SNRI treatment can lead to electrolyte disturbances, particularly hyponatremia (25, 42, 44, 71).
Tricyclic Antidepressants
Strong cardiovascular side effects are described with tricyclic antidepressants (TCAs) due to their anticholinergic and chinidine-like properties. In particular, cardiac conduction abnormalities, such as atrioventricular block, QTc prolongation, atrial fibrillation, and ventricular tachycardia, have been described (72–75). Further, the use of TCAs has been associated with acute myocardial infarction and a higher risk of stroke compared to SSRIs (75).
Other Frequently Used Antidepressants
Agomelatine
Agomelatine is a melatonin agonist with antidepressant properties. To date, no evidence of cardiovascular risk has been reported (76). Of note, liver enzymes should be controlled frequently due to its dose-dependent liver toxic properties.
Mirtazapine
Mirtazapine acts as specific serotonergic and noradrenergic antidepressant drug, with a relatively favorable cardiovascular side effect profile (73). However, significant weight gain and sedation have been frequently, and orthostatic hypotension has also sometimes been described (25, 77). A prospective multicenter study including 2,177 patients with myocardial infarction and depression found no significant effect of mirtazapine on cardiac event rate at 18 months (78).
Vortioxetine
Vortioxetine, a multimodal antidepressant and serotonin transporter inhibitor, seems to have a favorable cardiovascular side effect profile (79, 80). Besides antidepressant efficacy, pro-cognitive and anti-inflammatory properties have been described (81).
Bupropion
Bupropion at therapeutic dosages has not been associated with adverse effects on heart rate, blood pressure, and other cardiovascular parameters (82). In patients with CVD, bupropion was found to have a favorable effect on depressive symptoms (83), and was also observed to be safe in the post-myocardial infarction period when given at therapeutic dosages (84). Although hypertension and tachycardia have been described (85), bupropion does not appear to induce severe cardiovascular events, even in overdose.
Recommendations
A substantial body of evidence indicates that the cardiovascular safety profile of newer-generation antidepressants is significantly improved compared to TCAs (76). Nevertheless, regular monitoring concerning blood pressure, heart rate, ECG, body weight, and routine laboratory parameters (such as potassium levels) is generally recommended.
Selective serotonin reuptake inhibitors and SNRIs are generally considered safe in the treatment of patients with comorbid CVD when given within therapeutic limits. Due to the potential to increase the QTc interval (SSRIs and SNRIs) and heart rate/blood pressure (SNRIs), regular ECG and blood pressure monitoring is recommended. A combination of SSRIs with drugs that prolong QTc interval or that are associated with an increased bleeding risk (i.e., NSAIDs) should be avoided.
Newer antidepressant drugs (agomelatine, vortioxetine, mirtazapine, and bupropion) are generally considered safe when given within therapeutic dose limits. Albeit literature appears limited, the risk of QTc prolongation was found to be low for the majority of newer antidepressants (66). Weight monitoring (especially with mirtazapine) and blood pressure monitoring (especially with venlafaxine, duloxetine and bupropion) are recommended. For agomelatine, liver enzyme monitoring is recommended due to its propensity to significantly increase liver enzymes in up to 0.8% of treated patients.
Although substance- and dose-dependent, TCAs should be avoided in patients comorbid with CVD and mental disorders due to their potentially strong cardiovascular side effects.
First-Generation (Typical) and Second-Generation (Atypical) Antipsychotic Drugs
First- and second-generation antipsychotic drugs are used to treat patients with psychotic disorders, particularly schizophrenia (86, 87), and patients with bipolar disorders (88–90). Furthermore, several second-generation antipsychotics are recommended as augmentation strategy in treatment-resistant depression (91).
The increased cardiovascular morbidity and mortality observed in patients that receive antipsychotic drugs has been attributed to several factors, including an increased rate of unhealthy lifestyle (smoking, physical inactivity, and unhealthy eating habits), suboptimal screening and secondary preventive medical measures, and direct and indirect effects of antipsychotic medications (1, 92–94).
First-generation and, especially, second-generation antipsychotics have been associated with QTc prolongation and/or TdP (93, 95–109), as well as sudden cardiac death due to cardiac arrhythmia (95–97, 110, 111). More specifically, QTc prolongation has been reported for some first-generation antipsychotics (i.e., pimozide, IV haloperidol) and some low-potency phenothiazines (especially thioridazine, melperone), which were found to be associated with the greatest risk (112–114). Similarly, some second-generation antipsychotics (i.e., sertindole, iloperidone, amisulpride, ziprasidone) have been associated with OTc interval prolongation. Although a direct risk comparison is complicated by differences in study methodologies (96), especially ziprasidone appears to carry a higher risk for clinically meaningful increases in QTc interval (86, 114, 115). A summary regarding the relative risk of QTc prolongation with frequently used antipsychotic drugs is provided in Table 2. As with QTc prolongation with antidepressant drugs, further risk factors have to be considered, such as female sex, hypopotassemia, hypomagnesemia, higher age, and pre-existent cardiac diseases (116). Polypharmacy and the combination of drugs with the potential to alter cardiac conduction also enhance the risk of QTc prolongation compared to antipsychotic monotherapy (105). Some first- and second-generation antipsychotics are associated with an increased risk for cortical venous thrombosis or pulmonary embolism (117–131). Overall, the risk for hospitalization appears higher for second-generation antipsychotics: quetiapine (hazard ratio 2.68) > risperidone (1.98) > olanzapine (1.87) = clozapine (1.87) > phenothiazines (1.03) or other first-generation agents (0.98) (117).

Table 2. Relative risk of QTc prolongation with frequently used antipsychotic drugs [modified according to Refs. (132, 86)].
Metabolic Syndrome and Type-2 Diabetes Mellitus
Increased blood lipid and glucose levels have been reported with several second-generation and some low-potency first-generation antipsychotics (93, 94, 133–135). Among these, clozapine and olanzapine as well as chlorpromazine and thioridazine have been associated with an increased risk for metabolic disturbances such as glucose disturbance, lipid changes, and in some cases with acute ketoacidosis (93, 94, 133, 136). Further, second-generation antipsychotics have been reported to increase body weight, with clozapine and olanzapine bearing the greatest risk (93). According to a systematic review of randomized, placebo-controlled studies, the risk of weight gain was reported as follows: clozapine and olanzapine > risperidone > quetiapine > aripiprazole > ziprasidone (93).
Increased blood pressure and orthostatic hypotension have been reported in the context of antipsychotic treatment. Concerning blood pressure, around one third of patients with a psychotic disorder presents with elevated blood pressure; however, it is unclear whether this effect is due to antipsychotic medication or to formerly undetected metabolic syndrome and its components (136).
Orthostatic hypotension, most frequently observed in response to treatment with first-generation antipsychotics, such as phenothiazine, chlorpromazine, and thioridazine, is mostly attributed to their antagonistic action on adrenergic receptors (137).
Recommendations
The use of antipsychotic medications is in general safe in patients with comorbid CVD and mental disorder, although caution is necessary concerning direct (ECG alterations) and indirect (cardiometabolic and thromboembolic) side effects of certain drugs. For most psychiatric diseases, second-generation antipsychotics are currently recommended, rather than first-generation antipsychotics. Within the group of second-generation antipsychotics, the risk for cardiometabolic side effects (i.e., weight gain, hyperlipidemia, insulin resistance) differs substantially between drugs and is highest with the use of clozapine and olanzapine. In patients that present with, or display an increased risk for metabolic syndrome, drugs with lower metabolic side effects (i.e., aripiprazole, brexpiprazole, cariprazine, lurasidone, or lumateperone) should be considered.
Patients should be monitored closely for metabolic side effects, particularly in the first year of treatment. ECG monitoring should take place before and during antipsychotic treatment in patients with clinical risk factors for cardiac arrhythmias, i.e., family history of early cardiac death (<55 years old), personal history of structural heart defects, dizziness and, especially, syncope upon exertion, palpitations at rest (138). In CVD patients treated with clozapine, particular attention should be paid to anticholinergic side effects and the risk for myocarditis (139).
According to recommendations detailed in a consensus document by the American Diabetes Association (ADA) and American Psychiatric Association (APA), weight should be monitored monthly for the first three months and then quarterly, fasting blood glucose levels should be assessed at baseline, after 3 months, and then annually. A fasting lipid profile should be obtained at baseline, after 3 months, and then every 5th year (140), although the latter recommendation has been amended since, in that lipid levels ought to be monitored at the same time intervals as fasting glucose levels and that HbA1C should also be monitored, as increases occur several years before fasting glucose is elevated, signaling prediabetes or diabetes earlier (94).
Benzodiazepines
Benzodiazepines (BZDs) are frequently being prescribed for anxiety disorders, insomnia, and alcohol withdrawal and agitation (141–143). Due to their potential for abuse and their addictive properties, short-term use is recommended (144). Of note, some patients may have paradoxical effects of BZD medication, leading to confusion and an increase in agitation and delirium (145). In the context of CVD, BZDs may play a particular role in calming patients quickly who suffer from chest pain and acute myocardial infarction, reducing cardiac stress (146, 147). The addition of BZDs to standard cardiac medication in patients post myocardial infarction was associated with lower rates of re-infarction (148).
Recommendations
Benzodiazepines are generally considered safe in patients comorbid with CVD and mental disorders, when given as short-term acute treatment to relieve anxiety and agitation. Long-term use should be avoided due to inherent risks for iatrogenic BZD addiction, and caution should be given to elderly patients who are at greater risk of falls.
Mood Stabilizers
Mood stabilizers are given in the context of bipolar disorders to prevent further depressive/manic episodes (88–90), and in MDD as augmentation (91, 149) and, possibly prophylactic treatment (particularly lithium) (150). Lithium has been associated with sinus bradycardia, sinus node dysfunction, atrioventricular lock and ventricular irritability, and sick sinus syndrome is considered a cardiac contraindication for its use (151, 152). Valproic acid is a frequently given drug in epilepsy, and in bipolar disorders. Valproic acid is associated with thrombocytopenia, abnormal platelet function, bleeding risk, and with severe fetal abnormalities, restricting its use in female patients (153–157).
Lamotrigine is an anticonvulsant used in the treatment of bipolar disorder. Lamotrigine is known to bear the risk for toxic epidermal necrolysis (158), which is titration-speed dependent, but is considered safe concerning cardiac complications.
Recommendations
Mood stabilizers are generally considered safe concerning cardiovascular side effects in the absence of cardiac conduction delay. Lithium should be avoided in cases of atrioventricular block and sick sinus syndrome.
Psychological Interventions
Psychotherapy, in particular cognitive behavioral therapy (CBT), is established in the treatment of most major mental disorders, and is also applied to treat patients with mental disorders in the context of an underlying physical disease as well as in cardiometabolic disorders themselves (90, 159–163). In particular, adjustment disorder, anxiety and depressive disorders are frequent comorbidities in CVD, leading to decreased quality of life and in part worsen the disease course of the underlying physical illness (164–166).
Adjustment disorder represents an abnormal stress response to a stressor, such as acute myocardial infarction or chronic heart failure, and is reported to be common in primary care with rates ranging from 1% to 18% (167, 168). MDD also has been associated with a significant bidirectional comorbidity with CVD (169). Compared to MDD, adjustment disorder is almost three times more common in physically ill patients (13% versus 5%) (170) and is also frequently present in conjunction with chronic and potentially life-threatening diseases such as cancer (171). In the context of CVD, rates as high 38% have been reported, particular in acute and potentially life-threatening diseases such as peripartum cardiomyopathy and pulmonary artery hypertension (165, 166).
Different psychological treatments, such as CBT, low intensity psychological interventions, mindfulness-based techniques, metacognitive therapy (172) and e-mental health interventions, have been proposed for the treatment of adjustment disorder. Common components of these treatment strategies are the enabling of patients to reduce or remove the stressor, interventions to improve stress coping, and stress reduction strategies (173). Although there is limited empirical evidence, CBT and CBT-derived strategies are promising treatment interventions in patients with CVD and adjustment disorders (172, 173) and for CVD disorders per se (160, 161).
Major depressive disorder and anxiety disorders (particularly panic disorders) are more frequent in patients with CVD compared to the general population (3, 4, 165, 166, 169). Different psychotherapeutic methods are available to treat these disorders including CBT, “third wave” CBT [such as Acceptance and Commitment Treatment (174)] or psychodynamic psychotherapy. CBT is based on the principles established by Aaron T. Beck (175), focusing on dysfunctional believes, maladaptive schemes, and avoidance behavior to counteract mental disorders. Recent meta-analyses revealed that CBT presents an effective treatment to reduce depression and anxiety in patients with CVD (176) and acute coronary syndrome (177).
CBT as a treatment option is often limited by its accessibility. For example, in Germany the time period until a first visit with a psychotherapist takes place lasts up to 3 months, and the duration to the start of psychotherapy may be as long as 6–9 months (178). Therefore, internet-based self-help programs and internet-based psychotherapy have been developed during the last two decades, and efficacy has been proven in the context of anxiety and depressive disorders. These programs are most often based on CBT strategies, and are frequently offered as blended treatments, meaning that a real-life psychotherapist supports the program on demand. A recent meta-analysis demonstrated that internet-based self-help/psychotherapeutic programs have a similar efficacy as face-to-face psychotherapy, although their use has been limited to mild to moderate disease severity (179). Less research has been done for the treatment of patients comorbid with anxiety/depression and CVD. Recently, an internet-based CBT treatment adapted to persons with heart failure was compared to a web-based discussion forum, demonstrating small effects of internet-based CBT (180). In a secondary analysis of the data, improvement of depressive symptoms was demonstrated to be associated with improved autonomous-based self-care (181).
Recommendations
Face-to-face CBT and “third wave CBT” interventions have been proven effective in frequent mental disorders that are associated with cardiovascular diseases, and should be considered as treatment options. Due to the mere quantity of CVD patients in need for psychotherapy, and the limited number of psychotherapists, internet-based psychotherapeutic interventions may become a field of growing interest.
Clinical Summary
Due to the bidirectional association between cardiac and mental diseases, knowledge about treatment interventions and their limitations is important. According to recent research, adjustment disorder, anxiety disorder and MDD are the most frequent mental disorders in patients with CVD; all of them are addressable by psychotherapeutic interventions. Therefore, particularly CBT and its related “third wave CBT” are recommended in patients with CVD and mental disorders of mild to moderate severity. Furthermore, CBT can be recommended in patients with CVD and severe mental disorder as an augmentation of psychopharmacological treatment. If CBT is not accessible, internet-based psychological interventions may also be considered, although more research is needed to prove the effectiveness of internet-based psychotherapy in this population.
In more severe cases, psychopharmacological drugs can be recommended. Although well tolerated and efficacious in general, drug- and dose-dependent side effects have to be considered. Among antidepressants, SSRIs, SNRIs, and newer antidepressants, such as mirtazapine, bupropion, agomelatine and vortioxetine, can be recommended, while TCAs should be avoided due to their cardiac side effects. Mood stabilizers have been associated with arrhythmias, and some first- and second-generation antipsychotic drugs can increase the risk of QTc prolongation and metabolic side effects, although substantial differences exist between individual drugs. BDZs are generally considered safe in CVD when administered short-term. Of note, laboratory and ECG monitoring is always recommended in patients with CDV who are treated with psychopharmacological drugs, starting before the beginning of a drug treatment, and continuing on a regular basis.
Knowledge about effective psychological and safer pharmacological treatment options for mental disorders that are frequently comorbid with CVD can help clinicians optimize the biopsychosocial outcome of patients suffering from both mental and cardiovascular disorders. Importantly, since CVD increases the risk for mental disorders and vice versa, both physical and mental health care providers need to screen for the presence of the common comorbidity to consider the patient in their somato-psychiatric totality, which can help improve overall outcomes.
Author Contributions
KK: conceptualization, investigation, writing—original draft, and supervision. BS: writing—review and editing. CC: investigation and writing—original draft. All authors contributed to the article and approved the submitted version.
Conflict of Interest
KK received speaker honoraria by Janssen, Otsuka, Neuraxpharm, EliLilly, Schwabe, Servier, and Trommsdorff/Ferrer; he received an unrestricted grant by Ferrer, ADDISCA. CC has been a consultant and/or advisor to or has received honoraria from: AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Axsome, Cardio Diagnostics, Compass, Damitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Medscape, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Noven, Otsuka, Pfizer, Pharmabrain, Recordati, Relmada, Reviva, Rovi, Seqirus, Servier, SK Life Science, Sumitomo Dainippon, Sunovion, Supernus, Takeda, Teva, and Viatris. He provided expert testimony for Janssen and Otsuka. He served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, and Teva. He has received grant support from Janssen and Takeda. He received royalties from UpToDate and is also a stock option holder of Cardio Diagnostics, Mindpax, and LB Pharma.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. (2017) 16:163–80. doi: 10.1002/wps.20420
2. Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. (2014) 35:1365–72. doi: 10.1093/eurheartj/eht462
3. Celano CM, Huffman JC. Depression and cardiac disease: a review. Cardiol Rev. (2011) 19:130–42. doi: 10.1097/CRD.0b013e31820e8106
4. Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. (2003) 54:227–40. doi: 10.1016/s0006-3223(03)00587-0
5. Strik JJ, Denollet J, Lousberg R, Honig A. Comparing symptoms of depression and anxiety as predictors of cardiac events and increased health care consumption after myocardial infarction. J Am Coll Cardiol. (2003) 42:1801–7. doi: 10.1016/j.jacc.2003.07.007
6. Davidson KW, Kupfer DJ, Bigger JT, Califf RM, Carney RM, Coyne JC, et al. Assessment and treatment of depression in patients with cardiovascular disease: national heart, lung, and blood institute working group report. Ann Behav Med. (2006) 32:121–6. doi: 10.1097/01.psy.0000233233.48738.22
7. Todaro JF, Shen B-J, Raffa SD, Tilkemeier PL, Niaura R. Prevalence of anxiety disorders in men and women with established coronary heart disease. J Cardiopulm Rehabil Prev. (2007) 27:86–91. doi: 10.1097/01.HCR.0000265036.24157.e7
8. de Jonge P, Spijkerman TA, van den Brink RH, Ormel J. Depression after myocardial infarction is a risk factor for declining health related quality of life and increased disability and cardiac complaints at 12 months. Heart. (2006) 92:32–9. doi: 10.1136/hrt.2004.059451
9. Fauerbach JA, Bush DE, Thombs BD, McCann UD, Fogel J, Ziegelstein RC. Depression following acute myocardial infarction: a prospective relationship with ongoing health and function. Psychosomatics. (2005) 46:355–61. doi: 10.1176/appi.psy.46.4.355
10. Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry. (2003) 54:241–7. doi: 10.1016/s0006-3223(03)00111-2
11. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. (2000) 284:2606–10. doi: 10.1001/jama.284.20.2606
12. Jakobsen AS, Speyer H, Norgaard HCB, Karlsen M, Hjorthoj C, Krogh J, et al. Dietary patterns and physical activity in people with schizophrenia and increased waist circumference. Schizophr Res. (2018) 199:109–15. doi: 10.1016/j.schres.2018.03.016
13. Wadhera RK, Bhatt DL, Kind AJH, Song Y, Williams KA, Maddox TM, et al. Association of outpatient practice-level socioeconomic disadvantage with quality of care and outcomes among older adults with coronary artery disease: implications for value-based payment. Circ Cardiovasc Qual Outcomes. (2020) 13:e005977. doi: 10.1161/CIRCOUTCOMES.119.005977
14. Veru-Lesmes F, Rho A, King S, Joober R, Pruessner M, Malla A, et al. Social determinants of health and preclinical glycemic control in newly diagnosed first-episode psychosis patients. Can J Psychiatry. (2018) 63:547–56. doi: 10.1177/0706743718762097
15. Veru-Lesmes F, Rho A, Joober R, Iyer S, Malla A. Socioeconomic deprivation and blood lipids in first-episode psychosis patients with minimal antipsychotic exposure: implications for cardiovascular risk. Schizophr Res. (2020) 216:111–7. doi: 10.1016/j.schres.2019.12.019
16. Halaris A. Inflammation-associated co-morbidity between depression and cardiovascular disease. Curr Top Behav Neurosci. (2017) 31:45–70. doi: 10.1007/7854_2016_28
17. Rosmond RA, Björntorp P. The hypothalamic–pituitary–adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. (2000) 247:188–97. doi: 10.1046/j.1365-2796.2000.00603.x
18. Marano G, Harnic D, Lotrionte M, Biondi-Zoccai G, Abbate A, Romagnoli E, et al. Depression and the cardiovascular system: increasing evidence of a link and therapeutic implications. Expert Rev Cardiovasc Ther. (2009) 7:1123–47. doi: 10.1586/erc.09.78
19. Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry. (2016) 15:166–74. doi: 10.1002/wps.20309
20. Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease - a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. (2014) 5:137. doi: 10.3389/fpsyt.2014.00137
21. Mitchell AJ, Lord O, Malone D. Differences in the prescribing of medication for physical disorders in individuals with v. without mental illness: meta-analysis. Br J Psychiatry. (2012) 201:435–43. doi: 10.1192/bjp.bp.111.094532
22. Ayerbe L, Forgnone I, Addo J, Siguero A, Gelati S, Ayis S. Hypertension risk and clinical care in patients with bipolar disorder or schizophrenia; a systematic review and meta-analysis. J Affect Disord. (2018) 225:665–70. doi: 10.1016/j.jad.2017.09.002
23. Schneider F, Härter M, Schorr S. S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression. Berlin: Springer-Verlag (2017).
24. Bandelow B, Aden I, Alpers GW, Benecke A, Benecke C, Beutel ME, et al. Deutsche S3-Leitlinie Behandlung von Angststörungen, Version 2. (2021). Available online at: www.awmf.org/leitlinien/detail/ll/051-028.html (accessed November 01, 2021).
25. Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. (2015) 14:119–36. doi: 10.1002/wps.20204
26. Pacher P, Kecskemeti V. Cardiovascular side effects of new antidepressants and antipsychotics: new drugs, old concerns? Curr Pharm Des. (2004) 10:2463–75. doi: 10.2174/1381612043383872
27. Marano G, Traversi G, Romagnoli E, Catalano V, Lotrionte M, Abbate A, et al. Cardiologic side effects of psychotropic drugs. J Geriatr Cardiol. (2011) 8:243–53. doi: 10.3724/SP.J.1263.2011.00243
28. American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. (2010). Available online at: https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf (accessed November 01, 2021).
29. National Institute for Health and Care Excellence. Depression in Adults: Recognition and Management. (2009). Available online at: https://www.nice.org.uk/guidance/cg90/chapter/Recommendations (accessed November 01, 2021).
30. National Institute for Health and Care Excellence. Generalised Anxiety Disorder and Panic Disorder in Adults: Management. (2011). Available online at: https://www.nice.org.uk/guidance/cg113/chapter/1-Guidance#stepped-care-for-people-with-gad (accessed November 01, 2021).
31. Mazza M, Lotrionte M, Biondi-Zoccai G, Abbate A, Sheiban I, Romagnoli E. Selective serotonin reuptake inhibitors provide significant lower re-hospitalization rates in patients recovering from acute coronary syndromes: evidence from a meta-analysis. J Psychopharmacol. (2010) 24:1785–92. doi: 10.1177/0269881109348176
32. Beach SR, Kostis WJ, Celano CM, Januzzi JL, Ruskin JN, Noseworthy PA, et al. Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. J Clin Psychiatry. (2014) 75:e441–9. doi: 10.4088/JCP.13r08672
33. Maljuric NM, Noordam R, Aarts N, Niemeijer MN, van den Berg ME, Hofman A, et al. Use of selective serotonin re-uptake inhibitors and the heart rate corrected QT interval in a real-life setting: the population-based Rotterdam study. Br J Clin Pharmacol. (2015) 80:698–705. doi: 10.1111/bcp.12681
34. Qirjazi E, McArthur E, Nash DM, Dixon SN, Weir MA, Vasudev A, et al. Risk of ventricular arrhythmia with citalopram and escitalopram: a population-based study. PLoS One. (2016) 11:e0160768. doi: 10.1371/journal.pone.0160768
35. Haritos VS, Ghabrial H, Ahokas JT, Ching MS. Role of cytochrome P450 2D6 (CYP2D6) in the stereospecific metabolism of E- and Z-doxepin. Pharmacogenetics. (2000) 10:591–603. doi: 10.1097/00008571-200010000-00003
36. Crone CC, Gabriel GM. Treatment of anxiety and depression in transplant patients: pharmacokinetic considerations. Clin Pharmacokinet. (2004) 43:361–94. doi: 10.2165/00003088-200443060-00002
37. Thase ME, Larsen KG, Reines E, Kennedy SH. The cardiovascular safety profile of escitalopram. Eur Neuropsychopharmacol. (2013) 23:1391–400. doi: 10.1016/j.euroneuro.2013.05.011
38. Castro VM, Clements CC, Murphy SN, Gainer VS, Fava M, Weilburg JB, et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ. (2013) 346:f288. doi: 10.1136/bmj.f288
39. Funk KA, Bostwick JR. A comparison of the risk of QT prolongation among SSRIs. Ann Pharmacother. (2013) 47:1330–41. doi: 10.1177/1060028013501994
40. EMA. Pharmacovigilance Working Party (PhVWP). (2011). Available online at: https://www.ema.europa.eu/en/documents/report/monthly-report-pharmacovigilance-working-party-phvwp-october-2011-plenary-meeting_en.pdf (accessed November 10, 2021).
41. FDA. FDA Drug Safety Communication: Revised Recommendations for Celexa (Citalopram Hydrobromide) Related to a Potential Risk of Abnormal Heart Rhythms with High Doses. (2012). Available online at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-recommendations-celexa-citalopram-hydrobromide-related (accessed November 10, 2021).
42. De Picker L, Van Den Eede F, Dumont G, Moorkens G, Sabbe BG. Antidepressants and the risk of hyponatremia: a class-by-class review of literature. Psychosomatics. (2014) 55:536–47. doi: 10.1016/j.psym.2014.01.010
43. Liu BA, Mittmann N, Knowles SR, Shear NH. Hyponatremia and the syndrome of inappropriate secretion of antidiuretic hormone associated with the use of selective serotonin reuptake inhibitors: a review of spontaneous reports. CMAJ. (1996) 155:519–27.
44. Coupland CA, Dhiman P, Barton G, Morriss R, Arthur A, Sach T, et al. A study of the safety and harms of antidepressant drugs for older people: a cohort study using a large primary care database. Health Technol Assess. (2011) 15:1–202, iii–iv. doi: 10.3310/hta15280
45. Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. (2011) 343:d4551. doi: 10.1136/bmj.d4551
46. Letmaier M, Painold A, Holl AK, Vergin H, Engel R, Konstantinidis A, et al. Hyponatraemia during psychopharmacological treatment: results of a drug surveillance programme. Int J Neuropsychopharmacol. (2012) 15:739–48. doi: 10.1017/S1461145711001192
47. Degner D, Grohmann R, Kropp S, Ruther E, Bender S, Engel RR, et al. Severe adverse drug reactions of antidepressants: results of the German multicenter drug surveillance program AMSP. Pharmacopsychiatry. (2004) 37(Suppl. 1):S39–45. doi: 10.1055/s-2004-815509
48. Kirby D, Harrigan S, Ames D. Hyponatraemia in elderly psychiatric patients treated with selective serotonin reuptake inhibitors and venlafaxine: a retrospective controlled study in an inpatient unit. Int J Geriatr Psychiatry. (2002) 17:231–7. doi: 10.1002/gps.591
49. Cherin P, Colvez A, Deville de Periere G, Sereni D. Risk of syncope in the elderly and consumption of drugs: a case-control study. J Clin Epidemiol. (1997) 50:313–20. doi: 10.1016/s0895-4356(96)00385-x
50. Joo JH, Lenze EJ, Mulsant BH, Begley AE, Weber EM, Stack JA, et al. Risk factors for falls during treatment of late-life depression. J Clin Psychiatry. (2002) 63:936–41. doi: 10.4088/jcp.v63n1012
51. Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs Aging. (2009) 26:381–94. doi: 10.2165/00002512-200926050-00002
52. Pollock BG. Adverse reactions of antidepressants in elderly patients. J Clin Psychiatry. (1999) 60(Suppl. 20):4–8.
53. Akoudad S, Aarts N, Noordam R, Ikram MA, Tiemeier H, Hofman A, et al. Antidepressant use is associated with an increased risk of developing microbleeds. Stroke. (2016) 47:251–4. doi: 10.1161/STROKEAHA.115.011574
54. Andrade C, Sandarsh S, Chethan KB, Nagesh KS. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry. (2010) 71:1565–75. doi: 10.4088/JCP.09r05786blu
55. Cheng YL, Hu HY, Lin XH, Luo JC, Peng YL, Hou MC, et al. Use of SSRI, but not SNRI, increased upper and lower gastrointestinal bleeding: a nationwide population-based cohort study in Taiwan. Medicine (Baltimore). (2015) 94:e2022. doi: 10.1097/MD.0000000000002022
56. Quinn GR, Singer DE, Chang Y, Go AS, Borowsky LH, Udaltsova N, et al. Effect of selective serotonin reuptake inhibitors on bleeding risk in patients with atrial fibrillation taking warfarin. Am J Cardiol. (2014) 114:583–6. doi: 10.1016/j.amjcard.2014.05.037
57. Shin JY, Park MJ, Lee SH, Choi SH, Kim MH, Choi NK, et al. Risk of intracranial haemorrhage in antidepressant users with concurrent use of non-steroidal anti-inflammatory drugs: nationwide propensity score matched study. BMJ. (2015) 351:h3517. doi: 10.1136/bmj.h3517
58. Kahl KG, Westhoff-Bleck M, Kruger THC. Effects of psychopharmacological treatment with antidepressants on the vascular system. Vascul Pharmacol. (2017) 96–98:11–8. doi: 10.1016/j.vph.2017.07.004
59. Kahl KG. Direct and indirect effects of psychopharmacological treatment on the cardiovascular system. Horm Mol Biol Clin Investig. (2018) 36. doi: 10.1515/hmbci-2018-0054
60. Stahl SM, Grady MM, Moret C, Briley M. SNRIs: the pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. (2005) 10:732–47. doi: 10.1017/s1092852900019726
61. Alvares GA, Quintana DS, Hickie IB, Guastella AJ. Autonomic nervous system dysfunction in psychiatric disorders and the impact of psychotropic medications: a systematic review and meta-analysis. J Psychiatry Neurosci. (2016) 41:89–104. doi: 10.1503/jpn.140217
62. Danjou P, Hackett D. Safety and tolerance profile of venlafaxine. Int Clin Psychopharmacol. (1995) 10(Suppl. 2):15–20. doi: 10.1097/00004850-199503002-00004
63. Rudolph RL, Derivan AT. The safety and tolerability of venlafaxine hydrochloride: analysis of the clinical trials database. J Clin Psychopharmacol. (1996) 16:54S–9S. doi: 10.1097/00004714-199606002-00011
64. Feighner JP. Cardiovascular safety in depressed patients: focus on venlafaxine. J Clin Psychiatry. (1995) 56:574–9.
65. Gahimer J, Wernicke J, Yalcin I, Ossanna MJ, Wulster-Radcliffe M, Viktrup L. A retrospective pooled analysis of duloxetine safety in 23 983 subjects. Curr Med Res Opin. (2007) 23:175–84. doi: 10.1185/030079906X162719
66. Jasiak NM, Bostwick JR. Risk of QT/QTc prolongation among newer non-SSRI antidepressants. Ann Pharmacother. (2014) 48:1620–8. doi: 10.1177/1060028014550645
67. Tisdale JE. Drug-induced QT interval prolongation and torsades de pointes: role of the pharmacist in risk assessment, prevention and management. Can Pharm J (Ott). (2016) 149:139–52. doi: 10.1177/1715163516641136
68. Mease PJ, Zimetbaum PJ, Duh MS, Vekeman F, Guerin A, Boerstoel-Streefland M, et al. Epidemiologic evaluation of cardiovascular risk in patients receiving milnacipran, venlafaxine, or amitriptyline: evidence from French health data. Ann Pharmacother. (2011) 45:179–88. doi: 10.1345/aph.1P391
69. Deardorff WJ, Grossberg GT. A review of the clinical efficacy, safety and tolerability of the antidepressants vilazodone, levomilnacipran and vortioxetine. Expert Opin Pharmacother. (2014) 15:2525–42. doi: 10.1517/14656566.2014.960842
70. Asnis GM, Henderson MA. Levomilnacipran for the treatment of major depressive disorder: a review. Neuropsychiatr Dis Treat. (2015) 11:125–35. doi: 10.2147/NDT.S54710
71. Leth-Møller KB, Hansen AH, Torstensson M, Andersen SE, Ødum L, Gislasson G, et al. Antidepressants and the risk of hyponatremia: a Danish register-based population study. BMJ Open. (2016) 6:e011200. doi: 10.1136/bmjopen-2016-011200
72. Sala M, Coppa F, Cappucciati C, Brambilla P, d’Allio G, Caverzasi E, et al. Antidepressants: their effects on cardiac channels, QT prolongation and torsade de pointes. Curr Opin Investig Drugs. (2006) 7:256–63.
73. Thanacoody HK, Thomas SH. Tricyclic antidepressant poisoning : cardiovascular toxicity. Toxicol Rev. (2005) 24:205–14. doi: 10.2165/00139709-200524030-00013
74. Kim J, Phongsamran P, Park S. Use of antidepressant drugs in transplant recipients. Prog Transplant. (2004) 14:98–104. doi: 10.7182/prtr.14.2.40w9186064m78653
75. Lee YC, Lin CH, Lin MS, Lin JW, Chang CH, Lai MS. Effects of selective serotonin reuptake inhibitors versus tricyclic antidepressants on cerebrovascular events: a nationwide population-based cohort study. J Clin Psychopharmacol. (2013) 33:782–9. doi: 10.1097/JCP.0b013e31829c970e
76. Mago R, Tripathi N, Andrade C. Cardiovascular adverse effects of newer antidepressants. Expert Rev Neurother. (2014) 14:539–51. doi: 10.1586/14737175.2014.908709
77. Salvi V, Mencacci C, Barone-Adesi F. H1-histamine receptor affinity predicts weight gain with antidepressants. Eur Neuropsychopharmacol. (2016) 26:1673–7. doi: 10.1016/j.euroneuro.2016.08.012
78. Honig A, Kuyper AM, Schene AH, van Melle JP, de Jonge P, Tulner DM, et al. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med. (2007) 69:606–13. doi: 10.1097/PSY.0b013e31814b260d
79. Orsolini L, Tomasetti C, Valchera A, Iasevoli F, Buonaguro EF, Fornaro M, et al. Current and future perspectives on the major depressive disorder: focus on the new multimodal antidepressant vortioxetine. CNS Neurol Disord Drug Targets. (2017) 16:65–92. doi: 10.2174/1871527315666161025140111
80. Wagner G, Schultes MT, Titscher V, Teufer B, Klerings I, Gartlehner G. Efficacy and safety of levomilnacipran, vilazodone and vortioxetine compared with other second-generation antidepressants for major depressive disorder in adults: a systematic review and network meta-analysis. J Affect Disord. (2018) 228:1–12. doi: 10.1016/j.jad.2017.11.056
81. Salagre E, Sole B, Tomioka Y, Fernandes BS, Hidalgo-Mazzei D, Garriga M, et al. Treatment of neurocognitive symptoms in unipolar depression: a systematic review and future perspectives. J Affect Disord. (2017) 221:205–21. doi: 10.1016/j.jad.2017.06.034
82. Kiev A, Masco HL, Wenger TL, Johnston JA, Batey SR, Holloman LC. The cardiovascular effects of bupropion and nortriptyline in depressed outpatients. Ann Clin Psychiatry. (1994) 6:107–15. doi: 10.3109/10401239409148989
83. Roose SP, Dalack GW, Glassman AH, Woodring S, Walsh BT, Giardina EG. Cardiovascular effects of bupropion in depressed patients with heart disease. Am J Psychiatry. (1991) 148:512–6. doi: 10.1176/ajp.148.4.512
84. Rigotti NA, Thorndike AN, Regan S, McKool K, Pasternak RC, Chang Y, et al. Bupropion for smokers hospitalized with acute cardiovascular disease. Am J Med. (2006) 119:1080–7. doi: 10.1016/j.amjmed.2006.04.024
85. Balit CR, Lynch CN, Isbister GK. Bupropion poisoning: a case series. Med J Aust. (2003) 178:61–3. doi: 10.5694/j.1326-5377.2003.tb05064.x
86. Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Focus (Am Psychiatr Publ). (2020) 18:443–55. doi: 10.1176/appi.focus.18306
87. Kishimoto T, Hagi K, Nitta M, Kane JM, Correll CU. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry. (2019) 18:208–24. doi: 10.1002/wps.20632
88. Kishi T, Ikuta T, Matsuda Y, Sakuma K, Okuya M, Mishima K, et al. Mood stabilizers and/or antipsychotics for bipolar disorder in the maintenance phase: a systematic review and network meta-analysis of randomized controlled trials. Mol Psychiatry. (2021) 26:4146–57. doi: 10.1038/s41380-020-00946-6
89. Kishi T, Sakuma K, Okuya M, Matsuda Y, Esumi S, Hashimoto Y, et al. Effects of a conventional mood stabilizer alone or in combination with second-generation antipsychotics on recurrence rate and discontinuation rate in bipolar I disorder in the maintenance phase: a systematic review and meta-analysis of randomized, placebo-controlled trials. Bipolar Disord. (2021) 23:789–800. doi: 10.1111/bdi.13053
90. Nestsiarovich A, Gaudiot CES, Baldessarini RJ, Vieta E, Zhu Y, Tohen M. Preventing new episodes of bipolar disorder in adults: systematic review and meta-analysis of randomized controlled trials. Eur Neuropsychopharmacol. (2022) 54:75–89. doi: 10.1016/j.euroneuro.2021.08.264
91. Nunez NA, Joseph B, Pahwa M, Kumar R, Resendez MG, Prokop LJ, et al. Augmentation strategies for treatment resistant major depression: a systematic review and network meta-analysis. J Affect Disord. (2022) 302:385–400. doi: 10.1016/j.jad.2021.12.134
92. Ventriglio A, Gentile A, Stella E, Bellomo A. Metabolic issues in patients affected by schizophrenia: clinical characteristics and medical management. Front Neurosci. (2015) 9:297. doi: 10.3389/fnins.2015.00297
93. De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. (2011) 8:114–26. doi: 10.1038/nrendo.2011.156
94. Firth J, Siddiqi N, Koyanagi A, Siskind D, Rosenbaum S, Galletly C, et al. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. (2019) 6:675–712. doi: 10.1016/S2215-0366(19)30132-4
95. Beach SR, Celano CM, Noseworthy PA, Januzzi JL, Huffman JC. QTc prolongation, torsades de pointes, and psychotropic medications. Psychosomatics. (2013) 54:1–13. doi: 10.1016/j.psym.2012.11.001
96. Hasnain M, Vieweg WV. QTc interval prolongation and torsade de pointes associated with second-generation antipsychotics and antidepressants: a comprehensive review. CNS Drugs. (2014) 28:887–920. doi: 10.1007/s40263-014-0196-9
97. Wenzel-Seifert K, Wittmann M, Haen E. QTc prolongation by psychotropic drugs and the risk of torsade de pointes. Dtsch Arztebl Int. (2011) 108:687–93. doi: 10.3238/arztebl.2011.0687
98. van Noord C, Straus SM, Sturkenboom MC, Hofman A, Aarnoudse AJ, Bagnardi V, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol. (2009) 29:9–15. doi: 10.1097/JCP.0b013e318191c6a8
99. DeDea L. QT prolongation: a critical adverse effect of some medications. JAAPA. (2013) 26:11. doi: 10.1097/01720610-201302000-00002
100. Fusar-Poli P, Kempton MJ, Rosenheck RA. Efficacy and safety of second-generation long-acting injections in schizophrenia: a meta-analysis of randomized-controlled trials. Int Clin Psychopharmacol. (2013) 28:57–66. doi: 10.1097/YIC.0b013e32835b091f
101. Shah AA, Aftab A, Coverdale J. QTc prolongation with antipsychotics: is routine ECG monitoring recommended? J Psychiatr Pract. (2014) 20:196–206. doi: 10.1097/01.pra.0000450319.21859.6d
102. Chohan PS, Mittal R, Javed A. Antipsychotic medication and QT prolongation. Pak J Med Sci. (2015) 31:1269–71. doi: 10.12669/pjms.315.8998
103. Takeuchi H, Suzuki T, Remington G, Uchida H. Antipsychotic polypharmacy and corrected QT interval: a systematic review. Can J Psychiatry. (2015) 60:215–22. doi: 10.1177/070674371506000503
104. Wu CS, Tsai YT, Tsai HJ. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Assoc. (2015) 4:e001568. doi: 10.1161/JAHA.114.001568
105. Barbui C, Bighelli I, Carra G, Castellazzi M, Lucii C, Martinotti G, et al. Antipsychotic dose mediates the association between polypharmacy and corrected QT interval. PLoS One. (2016) 11:e0148212. doi: 10.1371/journal.pone.0148212
106. Carra G, Crocamo C, Bartoli F, Lax A, Tremolada M, Lucii C, et al. First-generation antipsychotics and QTc: any role for mediating variables? Hum Psychopharmacol. (2016) 31:313–8. doi: 10.1002/hup.2540
107. Polcwiartek C, Kragholm K, Schjerning O, Graff C, Nielsen J. Cardiovascular safety of antipsychotics: a clinical overview. Expert Opin Drug Saf. (2016) 15:679–88. doi: 10.1517/14740338.2016.1161021
108. Acciavatti T, Martinotti G, Corbo M, Cinosi E, Lupi M, Ricci F, et al. Psychotropic drugs and ventricular repolarisation: the effects on QT interval, T-peak to T-end interval and QT dispersion. J Psychopharmacol. (2017) 31:453–60. doi: 10.1177/0269881116684337
109. Kano M, Toyoshi T, Iwasaki S, Kato M, Shimizu M, Ota T. QT PRODACT: usability of miniature pigs in safety pharmacology studies: assessment for drug-induced QT interval prolongation. J Pharmacol Sci. (2005) 99:501–11. doi: 10.1254/jphs.qt-c13
110. Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. (2009) 360:225–35. doi: 10.1056/NEJMoa0806994
111. Haddad PM, Anderson IM. Antipsychotic-related QTc prolongation, torsade de pointes and sudden death. Drugs. (2002) 62:1649–71. doi: 10.2165/00003495-200262110-00006
112. Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart. (2003) 89:1363–72. doi: 10.1136/heart.89.11.1363
113. Mehtonen OP, Aranko K, Malkonen L, Vapaatalo H. A survey of sudden death associated with the use of antipsychotic or antidepressant drugs: 49 cases in Finland. Acta Psychiatr Scand. (1991) 84:58–64. doi: 10.1111/j.1600-0447.1991.tb01421.x
114. Harrigan EP, Miceli JJ, Anziano R, Watsky E, Reeves KR, Cutler NR, et al. A randomized evaluation of the effects of six antipsychotic agents on QTc, in the absence and presence of metabolic inhibition. J Clin Psychopharmacol. (2004) 24:62–9. doi: 10.1097/01.jcp.0000104913.75206.62
115. Potkin SG, Preskorn S, Hochfeld M, Meng X. A thorough QTc study of 3 doses of iloperidone including metabolic inhibition via CYP2D6 and/or CYP3A4 and a comparison to quetiapine and ziprasidone. J Clin Psychopharmacol. (2013) 33:3–10. doi: 10.1097/JCP.0b013e31827c0314
116. Vandael E, Vandenberk B, Vandenberghe J, Willems R, Foulon V. Risk factors for QTc-prolongation: systematic review of the evidence. Int J Clin Pharm. (2017) 39:16–25. doi: 10.1007/s11096-016-0414-2
117. Liperoti R, Pedone C, Lapane KL, Mor V, Bernabei R, Gambassi G. Venous thromboembolism among elderly patients treated with atypical and conventional antipsychotic agents. Arch Intern Med. (2005) 165:2677–82. doi: 10.1001/archinte.165.22.2677
118. Zornberg GL, Jick H. Antipsychotic drug use and risk of first-time idiopathic venous thromboembolism: a case-control study. Lancet. (2000) 356:1219–23. doi: 10.1016/S0140-6736(00)02784-7
119. Werring D, Hacking D, Losseff N, Jager HR, Walsh M, Foong J. Cerebral venous sinus thrombosis may be associated with clozapine. J Neuropsychiatry Clin Neurosci. (2009) 21:343–5. doi: 10.1176/jnp.2009.21.3.343a
120. Thomassen R, Vandenbroucke JP, Rosendaal FR. Antipsychotic medication and venous thrombosis. Br J Psychiatry. (2001) 179:63–6. doi: 10.1192/bjp.179.1.63
121. Stansby G, Noble S, Howes O. The importance of venous thromboembolism – a physical consequence of psychiatric treatments. Int J Clin Pract. (2010) 64:1005–6. doi: 10.1111/j.1742-1241.2010.02435.x
122. Shulman M, Jennifer Njoku I, Manu P. Thrombotic complications of treatment with antipsychotic drugs. Minerva Med. (2013) 104:175–84.
123. Ray JG, Mamdani MM, Yeo EL. Antipsychotic and antidepressant drug use in the elderly and the risk of venous thromboembolism. Thromb Haemost. (2002) 88:205–9.
124. Parker C, Coupland C, Hippisley-Cox J. Antipsychotic drugs and risk of venous thromboembolism: nested case-control study. BMJ. (2010) 341:c4245. doi: 10.1136/bmj.c4245
125. Pantel J, Schroder J, Eysenbach K, Mundt C. Two cases of deep vein thrombosis associated with a combined paroxetine and zotepine therapy. Pharmacopsychiatry. (1997) 30:109–11. doi: 10.1055/s-2007-979493
126. Numata S, Kato O, Misawa H, Tokuda H, Kasahara T, Ohmori T. Left atrial thrombosis associated with antipsychotic drugs. Prog Neuropsychopharmacol Biol Psychiatry. (2005) 29:153–5. doi: 10.1016/j.pnpbp.2004.08.010
127. Matsumoto M, Konno T, Tamba K, Abe T, Kato S, Kajii E. Two cases of deep vein thrombosis associated with antipsychotic drug use. Psychiatry Clin Neurosci. (2004) 58:450–1. doi: 10.1111/j.1440-1819.2004.01284.x
128. Maly R, Masopust J, Hosak L, Konupcikova K. Assessment of risk of venous thromboembolism and its possible prevention in psychiatric patients. Psychiatry Clin Neurosci. (2008) 62:3–8. doi: 10.1111/j.1440-1819.2007.01773.x
129. Hagg S, Spigset O. Antipsychotic-induced venous thromboembolism: a review of the evidence. CNS Drugs. (2002) 16:765–76. doi: 10.2165/00023210-200216110-00005
130. Hägg S, Tätting P, Spigset O. Olanzapine and venous thromboembolism. Int Clin Psychopharmacol. (2003) 18:299–300. doi: 10.1097/01.yic.0000085241.99018.30
131. Knudson JF, Kortepeter C, Dubitsky GM, Ahmad SR, Chen M. Antipsychotic drugs and venous thromboembolism. Lancet. (2000) 356:252–3. doi: 10.1016/S0140-6736(05)74504-9
132. Benkert O, Hippius H. Kompendium der Psychiatrischen Pharmakotherapie. Berlin: Springer (2021).
133. Nielsen J, Skadhede S, Correll CU. Antipsychotics associated with the development of type 2 diabetes in antipsychotic-naive schizophrenia patients. Neuropsychopharmacology. (2010) 35:1997–2004. doi: 10.1038/npp.2010.78
134. Pillinger T, Beck K, Gobjila C, Donocik JG, Jauhar S, Howes OD. Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry. (2017) 74:261–9. doi: 10.1001/jamapsychiatry.2016.3803
135. Pillinger T, Beck K, Stubbs B, Howes OD. Cholesterol and triglyceride levels in first-episode psychosis: systematic review and meta-analysis. Br J Psychiatry. (2017) 211:339–49. doi: 10.1192/bjp.bp.117.200907
136. Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders–a systematic review and meta-analysis. Schizophr Bull. (2013) 39:306–18. doi: 10.1093/schbul/sbr148
137. Gugger JJ. Antipsychotic pharmacotherapy and orthostatic hypotension: identification and management. CNS Drugs. (2011) 25:659–71. doi: 10.2165/11591710-000000000-00000
138. Correll CU, Harris J, Figen V, Kane JM, Manu P. Antipsychotic drug administration does not correlate with prolonged rate-corrected QT interval in children and adolescents: results from a nested case-control study. J Child Adolesc Psychopharmacol. (2011) 21:365–8. doi: 10.1089/cap.2011.0024
139. Nielsen J, Correll CU, Manu P, Kane JM. Termination of clozapine treatment due to medical reasons: when is it warranted and how can it be avoided? J Clin Psychiatry. (2013) 74:603–13; quiz 613. doi: 10.4088/JCP.12r08064
140. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. (2004) 27:596–601. doi: 10.2337/diacare.27.2.596
141. Gerlach LB, Wiechers IR, Maust DT. Prescription benzodiazepine use among older adults: a critical review. Harv Rev Psychiatry. (2018) 26:264–73. doi: 10.1097/HRP.0000000000000190
142. Abad VC, Guilleminault C. Insomnia in elderly patients: recommendations for pharmacological management. Drugs Aging. (2018) 35:791–817. doi: 10.1007/s40266-018-0569-8
143. Correll CU, Yu X, Xiang Y, Kane JM, Masand P. Biological treatment of acute agitation or aggression with schizophrenia or bipolar disorder in the inpatient setting. Ann Clin Psychiatry. (2017) 29:92–107.
144. Peng L, Morford KL, Levander XA. Benzodiazepines and related sedatives. Med Clin North Am. (2022) 106:113–29. doi: 10.1016/j.mcna.2021.08.012
145. Champion C, Novais T, Dorey JM, Krolak-Salmon P, Lepetit A. Paradoxical reactions to benzodiazepines in the elderly. Geriatr Psychol Neuropsychiatr Vieil. (2021) 35:8–10. doi: 10.1684/pnv.2021.0982
146. Janeway D. An integrated approach to the diagnosis and treatment of anxiety within the practice of cardiology. Cardiol Rev. (2009) 17:36–43. doi: 10.1097/CRD.0b013e3181867fe3
147. Wu CK, Huang YT, Lee JK, Jimmy Juang JM, Tsai CT, Lai LP, et al. Anti-anxiety drugs use and cardiovascular outcomes in patients with myocardial infarction: a national wide assessment. Atherosclerosis. (2014) 235:496–502. doi: 10.1016/j.atherosclerosis.2014.05.918
148. Wheatley D. Psychological stress and cardiovascular diseases. Scand J Work Environ Health. (1984) 10:415–7. doi: 10.5271/sjweh.2319
149. Solmi M, Veronese N, Zaninotto L, van der Loos ML, Gao K, Schaffer A, et al. Lamotrigine compared to placebo and other agents with antidepressant activity in patients with unipolar and bipolar depression: a comprehensive meta-analysis of efficacy and safety outcomes in short-term trials. CNS Spectr. (2016) 21:403–18. doi: 10.1017/S1092852916000523
150. Baethge C, Gruschka P, Smolka MN, Berghofer A, Bschor T, Muller-Oerlinghausen B, et al. Effectiveness and outcome predictors of long-term lithium prophylaxis in unipolar major depressive disorder. J Psychiatry Neurosci. (2003) 28:355–61.
151. Freeman MP, Freeman SA. Lithium: clinical considerations in internal medicine. Am J Med. (2006) 119:478–81. doi: 10.1016/j.amjmed.2005.11.003
152. Beach SR, Celano CM, Huffman JC, Stern TA. Psychopharmacology in the treatment of patients with cardiovascular disease. In: ME Alvarenga, D Byrne editors. Handbook of Psychocardiology. Singapore: Springer Singapore (2016). p. 1043–59.
153. Jentink J, Loane MA, Dolk H, Barisic I, Garne E, Morris JK, et al. Valproic acid monotherapy in pregnancy and major congenital malformations. N Engl J Med. (2010) 362:2185–93. doi: 10.1056/NEJMoa0907328
154. Kumar R, Vidaurre J, Gedela S. Valproic acid-induced coagulopathy. Pediatr Neurol. (2019) 98:25–30. doi: 10.1016/j.pediatrneurol.2019.04.019
155. Ko CH, Kong CK, Tse PW. Valproic acid and thrombocytopenia: cross-sectional study. Hong Kong Med J. (2001) 7:15–21.
156. Koenig S, Gerstner T, Keller A, Teich M, Longin E, Dempfle CE. High incidence of vaproate-induced coagulation disorders in children receiving valproic acid: a prospective study. Blood Coagul Fibrinolysis. (2008) 19:375–82. doi: 10.1097/MBC.0b013e3282f3f9ec
157. Johnston JP, Nerenberg SF. Valproic acid-induced thrombocytopenia-related spontaneous systemic bleeding. Am J Case Rep. (2020) 21:e927830. doi: 10.12659/AJCR.927830
158. Gleghorn KL, Voigt C, Kelly B. Toxic epidermal necrolysis and Stevens-Johnson syndrome/toxic epidermal necrolysis overlap in pediatric patients with a focus on newer antiepileptic drugs: a 25-year retrospective study at a single tertiary care center. Pediatr Dermatol. (2021) 38:812–8. doi: 10.1111/pde.14598
159. Yang X, Li Z, Sun J. Effects of cognitive behavioral therapy-based intervention on improving glycaemic, psychological, and physiological outcomes in adult patients with diabetes mellitus: a meta-analysis of randomized controlled trials. Front Psychiatry. (2020) 11:711. doi: 10.3389/fpsyt.2020.00711
160. Li YN, Buys N, Ferguson S, Li ZJ, Sun J. Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease: a meta-analysis. World J Psychiatry. (2021) 11:1147–66. doi: 10.5498/wjp.v11.i11.1147
161. Li Y, Buys N, Li Z, Li L, Song Q, Sun J. The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: a systematic review and meta-analysis. Prev Med Rep. (2021) 23:101477. doi: 10.1016/j.pmedr.2021.101477
162. Li X, Feng Y, Xia J, Zhou X, Chen N, Chen Z, et al. Effects of cognitive behavioral therapy on pain and sleep in adults with traumatic brain injury: a systematic review and meta-analysis. Neural Plast. (2021) 2021:6552246. doi: 10.1155/2021/6552246
163. McMain S, Newman MG, Segal ZV, DeRubeis RJ. Cognitive behavioral therapy: current status and future research directions. Psychother Res. (2015) 25:321–9. doi: 10.1080/10503307.2014.1002440
164. Westhoff-Bleck M, Lemke LH, Bleck JS, Bleck AC, Bauersachs J, Kahl KG. Depression associated with reduced heart rate variability predicts outcome in adult congenital heart disease. J Clin Med. (2021) 10:1554. doi: 10.3390/jcm10081554
165. Pfeffer TJ, Herrmann J, Berliner D, Konig T, Winter L, Ricke-Hoch M, et al. Assessment of major mental disorders in a German peripartum cardiomyopathy cohort. ESC Heart Fail. (2020) 7:4394–8. doi: 10.1002/ehf2.12967
166. Olsson KM, Meltendorf T, Fuge J, Kamp JC, Park DH, Richter MJ, et al. Prevalence of mental disorders and impact on quality of life in patients with pulmonary arterial hypertension. Front Psychiatry. (2021) 12:667602. doi: 10.3389/fpsyt.2021.667602
167. Casey P. Adjustment disorder: new developments. Curr Psychiatry Rep. (2014) 16:451. doi: 10.1007/s11920-014-0451-2
168. Blacker CVR, Clare AW. The prevalence and treatment of depression in general practice. Psychopharmacology. (1988) 95:S14–7. doi: 10.1007/BF00172624
169. Gold SM, Kohler-Forsberg O, Moss-Morris R, Mehnert A, Miranda JJ, Bullinger M, et al. Comorbid depression in medical diseases. Nat Rev Dis Primers. (2020) 6:69. doi: 10.1038/s41572-020-0200-2
170. Silverstone PH. Prevalence of psychiatric disorders in medical inpatients. J Nerv Ment Dis. (1996) 184:43–51. doi: 10.1097/00005053-199601000-00008
171. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. (2011) 12:160–74. doi: 10.1016/S1470-2045(11)70002-X
172. Winter L, Naumann F, Olsson K, Fuge J, Hoeper MM, Kahl KG. Metacognitive therapy for adjustment disorder in a patient with newly diagnosed pulmonary arterial hypertension: a case report. Front Psychol. (2020) 11:143. doi: 10.3389/fpsyg.2020.00143
173. O’Donnell ML, Metcalf O, Watson L, Phelps A, Varker T. A systematic review of psychological and pharmacological treatments for adjustment disorder in adults. J Trauma Stress. (2018) 31:321–31. doi: 10.1002/jts.22295
174. Kahl KG, Winter L, Schweiger U. The third wave of cognitive behavioural therapies: what is new and what is effective? Curr Opin Psychiatry. (2012) 25:522–8. doi: 10.1097/YCO.0b013e328358e531
175. Beck AT. A 60-year evolution of cognitive theory and therapy. Perspect Psychol Sci. (2019) 14:16–20. doi: 10.1177/1745691618804187
176. Reavell J, Hopkinson M, Clarkesmith D, Lane DA. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease: a systematic review and meta-analysis. Psychosom Med. (2018) 80:742–53. doi: 10.1097/PSY.0000000000000626
177. Magan I, Casado L, Jurado-Barba R, Barnum H, Redondo MM, Hernandez AV, et al. Efficacy of psychological interventions on psychological outcomes in coronary artery disease: systematic review and meta-analysis. Psychol Med. (2021) 51:1846–60. doi: 10.1017/S0033291720000598
178. BPTK. Bundes Psychotherapeuten Kammer: Ein Jahr Nach der Reform der Psychotherapie-Richtlinie – Wartezeiten 2018. (2018). Available online at: https://www.bptk.de/wp-content/uploads/2019/01/20180411_bptk_studie_wartezeiten_2018.pdf (accessed November10, 2021).
179. Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. (2014) 13:288–95. doi: 10.1002/wps.20151
180. Lundgren JG, Dahlstrom O, Andersson G, Jaarsma T, Karner Kohler A, Johansson P. The effect of guided web-based cognitive behavioral therapy on patients with depressive symptoms and heart failure: a pilot randomized controlled trial. J Med Internet Res. (2016) 18:e194. doi: 10.2196/jmir.5556
181. Johansson P, Jaarsma T, Andersson G, Lundgren J. The impact of internet-based cognitive behavioral therapy and depressive symptoms on self-care behavior in patients with heart failure: a secondary analysis of a randomised controlled trial. Int J Nurs Stud. (2021) 116:103454. doi: 10.1016/j.ijnurstu.2019.103454
Keywords: psychocardiology, psychological intervention, psychopharmacological intervention, cardiovascular disease, antidepressant, antipsychotic, psychotherapy
Citation: Kahl KG, Stapel B and Correll CU (2022) Psychological and Psychopharmacological Interventions in Psychocardiology. Front. Psychiatry 13:831359. doi: 10.3389/fpsyt.2022.831359
Received: 08 December 2021; Accepted: 18 February 2022;
Published: 16 March 2022.
Edited by:
Georgios Paslakis, Ruhr University Bochum, Medical Faculty, University Clinic for Psychosomatic Medicine and Psychotherapy, GermanyReviewed by:
Marianna Mazza, Agostino Gemelli University Polyclinic (IRCCS), ItalyCopyright © 2022 Kahl, Stapel and Correll. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai G. Kahl, a2FobC5rYWlAbWgtaGFubm92ZXIuZGU=
 Kai G. Kahl
Kai G. Kahl Britta Stapel
Britta Stapel Christoph U. Correll2,3,4
Christoph U. Correll2,3,4