- 1Department of Psychology, Brooklyn College, City University of New York, New York, NY, United States
- 2Program in Psychology, The Graduate Center, City University of New York, New York, NY, United States
- 3Psycho-Oncology, Monter Cancer Center, Northwell Health Cancer Institute, New York, NY, United States
Background: Depression is a heterogenous disorder with both cognitive and somatic symptom dimensions that may differentially relate to systemic inflammation. Diet, which has the potential to modulate both inflammation levels and mood, is yet to be studied within the context of individual depression dimensions. This study examined the associations between inflammatory cytokines and dietary patterns with depressive symptom dimension profiles among a sample of women recruited in a non-clinical setting.
Methods: Inflammatory cytokines (IL-6 and TNF-α), inflammatory diet (Diet Inflammatory Index; DII), and depressive symptoms (Beck Depression Inventory-II; BDI-II) were measured in 136 females (Mage = 22.01 ± 4.02, range 18–59 years). Multiple linear regressions were used to investigate the relationships between inflammatory cytokines and diet with self-reported cognitive, somatic, and total depressive symptoms, adjusting for demographic factors.
Results: Findings showed that increased somatic dimension scores were positively associated with IL-6 (ß = 0.273, p = 0.002) and TNF-α (ß = 0.215, p = 0.017), but not inflammatory diet (p = 0.300). Total BDI-II scores were only positively associated with IL-6 (ß = 0.221, p = 0.012), and cognitive dimension scores were not associated with any inflammation measures.
Conclusions: These findings contribute to existing evidence that inflammatory cytokines are associated with the somatic symptoms of depression. Inflammatory diet index was not associated with depression measures.
Introduction
Emerging evidence suggests that a subgroup of individuals with depression have elevated inflammation (1, 2). Inflammation, a biological process that fights infection, is brought on by groups of secreted proteins called cytokines (3, 4). Research has demonstrated positive correlations between cytokines interleukin (IL)-6 and tumor necrosis factor (TNF)-α and symptoms of depression in meta-analyses of both community samples (5, 6) and adults diagnosed with major depressive disorder (MDD) (2, 5, 7–11).
The evident relation between inflammation and depression is commonly explained by the sickness behavior model. Sickness behaviors are depression-like symptoms (fatigue, anhedonia, changes in sleep and appetite, and decreased interest in sex) resulting from infection or injury and subsequent rise in inflammation (12–15). These behaviors are evolutionary advantageous in that they promote sedentary behavior and eventual recovery from infection or injury. However, prolonged exposure to inflammation, and consequent sickness behaviors, may influence the development and maintenance of MDD (16).
In addition to infection or injury, a growing body of literature shows that an unhealthy diet may contribute to low-grade, prolonged systemic inflammation via pathways within the gut (17–19). An inflammatory diet has been associated with increased risk for depressive symptoms and diagnosis of MDD in a handful of studies (20–23), and thus, may be an important factor to consider when studying inflammation-associated depression (24). An unhealthy, inflammatory diet typically consists of highly processed foods such as white bread, sweets, sugary beverages, and large amounts of animal products high in saturated fats (25, 26). In contrast, a healthy, anti-inflammatory diet typically consisting of foods such as fruits, vegetables, whole grains, nuts, seeds, and fish, have been associated with low levels of depression (27–29). Based on these findings, diet may be one source of inflammation that contributes to sickness behaviors. Investigation of dietary intake that can contribute to inflammation is needed to better understand how lifestyle associated inflammation is associated with depression.
Historically, depression, as it relates to inflammation, has been examined as a global construct (30). In this way, prior research is limited, as depression encompasses a broad, heterogenous range of symptoms that may be differentially related to inflammation (31–34). Specifically, symptoms can be conceptualized as cognitive-affective (e.g., maladaptive beliefs or thinking patterns and sad mood) or somatic (e.g., fatigue, appetite, or sleep changes) (35). This distinction is relevant when considering the inflammation-depression link given that sickness behavior symptoms predominately overlap with somatic symptoms of depression, as opposed to cognitive symptoms of depression (33). Thus a dimensional analysis of depressive symptoms is a more nuanced approach to disentangle biological mechanisms of depression and their behavioral manifestations (31, 32). The somatic dimension has been shown to be associated with various inflammatory measures in both clinical (36, 37) and non-clinical samples (6, 34, 38, 39). However, not all studies demonstrate this association (40–44), and still others find equal associations between both dimensions and inflammation (6, 42). These inconsistent findings may be due to heterogeneity in methodology of how somatic symptoms are measured (45). Furthermore, depression research mostly measures inflammatory cytokines using blood samples. However, preliminary data shows that cytokine levels measured via saliva sampling, a non-invasive and more economical approach, (46) may be related to depression as well (47, 48).
A more multifaceted investigation, which includes measures of salivary cytokines, dietary patterns, and a dimensional assessment of depressive symptoms which has been validated by meta-analysis in previous research, is utilized in the current study to better elucidate the relationship between inflammation and depression. This study aimed to test the association between inflammatory cytokines and diet with depressive symptom dimensions (i.e., somatic and cognitive) in a community sample of women. It was predicted that inflammation measures would be associated with somatic symptoms of depression.
Materials and Methods
Participants and Procedure
We performed a secondary data analysis of baseline data collected from a randomized trial (RCT) testing the efficacy of a 12-week daily dose of supplements (i.e., omega-3 fatty acids, probiotics, combination, placebo) to reduced depressive, anxiety, and stress symptoms (49). This study was conducted at a college in Brooklyn, New York. Participants were recruited via flyers posted on campus, snowball sampling, and online advertisements. Inclusion criteria included self-reporting as a cisgender female, at least 18 years of age, and English fluency. Exclusion criteria included self-reported of any of the following: current pregnancy, a diagnosis of chronic inflammatory or endocrine related illnesses, a diagnosis of current schizophrenia or bipolar disorder, current psychoactive drug use, treatment (psychopharmacology or psychotherapy) for any psychiatric illness within 6 months prior to study recruitment, excessive alcohol or cigarette intake, more than occasional use of marijuana, or any use of other recreational drugs.
The research was approved by the university's institutional review board, and all participants provided informed, written consent prior to participation in research activities. In the lab, participants completed self-report assessments (demographic information, depressive symptoms, and diet), provided 0.5–2.0 ml of saliva via passive drool, and were compensated $25. Immediately after saliva collection, samples were placed in a −20 degrees Celsius freezer for approximately 3–6 months. They were then mailed to Salimetrics Laboratory on dry ice for analysis (Salimetrics, LLC, State College, Pennsylvania).
Measures
Demographic Variables
Participants were asked to report their age, race/ethnicity, and income. Age was measured on a continuous scale. For race/ethnicity, participants had the option of choosing Caucasian, Hispanic/Latina, Black/African American, Asian/Pacific Islander, or Mixed/Other. Income was assessed using seven income brackets ranging from < $25,000 to $150,000 or more.
Beck Depression Inventory (BDI-II)
The BDI-II assesses severity of depressive symptoms using a 21-items questionnaire (45). Total scores can range from 0 to 63, with higher scores indicative of more severe depression symptoms. Established clinical cutoff scores include normal ranges (0–13), mild depression (14–19), moderate depression (20–28), and severe depression (29 or above). The BDI-II has adequate validity (50). In the current sample, total scores had good internal consistency (Cronbach's α = 0.89).
To calculate somatic and cognitive dimensions of depression, Huang & Chen's (51) method was used. Briefly, the authors conducted a meta-analysis of the factor structure of the BDI-II's depression dimensions which resulted in the following two-factor structure. The somatic dimension is a summed score of 11 items on the BDI-II (items 4, 11–13, and 15–21). The cognitive dimension is a summed score of nine items on the BDI-II (items 1–3, 5–9, and 14). Scores obtained in the current study suggest that the somatic and cognitive dimensions have good internal consistency (Cronbach's α = 0.81 and 0.86, respectively).
Salivary Cytokines
Prior to initiating in-person data collection, participants were instructed to refrain from drinking alcohol and smoking 12 h prior to their study appointment, and to refrain from eating, consuming caffeine, and brushing their teeth within 1 h of their appointment to ensure more accurate measurement of salivary inflammatory cytokines. Instruction compliance was verified before initiating any study procedures. Salivary inflammation was measured via passive drool.
A total of 136 saliva samples were analyzed by Salimetrics Laboratory (Salimetrics, LLC, State College, Pennsylvania). Samples were centrifuged at 3,500 rpm for 15 min, and supernatant was transferred away from the resultant mucin and debris. Next, supernatant samples were mixed again by inversion and vortexing and then stored in a laboratory freezer set at −80 degrees Celsius until they were assayed. Enzyme-linked immunosorbent assay (ELISA) was used to detect each participant's average levels of IL-6 and TNF-α in pg/mL. Minimum detection limits for IL-6 were 0.07 pg/mL. IL-6 values in the sample ranged from 0.07 to 92 pg/mL, mean (SD) = 5.79 (11.52) pg/mL, which is comparable to other, larger samples (36, 42, 52). Minimum detection limits for TNF-α were 0.04 pg/mL. TNF-α values in the sample ranged from 0.22 to 336.98 pg/mL, mean (SD) = 10.42 (43.53) pg/mL, which is comparable to other, larger samples (52, 53). ELISA procedures performed by Salimetrics were reported to be reliable via several parameters including linearity, spike and recovery testing, intra- and inter- assay precision, and freeze/thaw stability (54).
Inflammatory Diet
Measurement of the inflammatory potential of participants' diets was based on self-reported dietary intake using the Diet History Questionnaire-II [DHQ-II; (55)]. The DHQ-II (56) is a web-based, self-reported food frequency questionnaire that assesses intake of 134 food and beverage items and eight dietary supplements over the past month in terms of both frequency and portion size. DHQ-II items were transformed using the U.S. Department of Agriculture's (USDA) Food and Nutrient Database for Dietary Studies and USDA's MyPyramid Equivalents Database (MPED) to produce an average daily amount for food items and nutrients. This method is commonly used in nutrition research that uses the DHQ-II (57). A software program, Diet*Calc PC [Version 1.5, (58)] was utilized to convert data generated by the DHQ-II into an estimated value of daily nutrient consumption in grams (59, 60).
The Diet Inflammatory Index (DII) was used to determine the inflammatory potential of participants' diets (61). Briefly, the DII is a validated, literature-derived index used to calculate the inflammatory potential of participants' self-reported dietary patterns (62, 63). The methods outlined by Shivappa et al. (61) to calculate the total DII scores were used. A total of 27 food and nutrient items obtained from the DHQ-II were used in this study, including alcohol, beta-carotene, caffeine, carbohydrates, cholesterol, total fat, fiber, folic acid, iron, magnesium, monounsaturated fatty acids, niacin, omega-3, protein, polyunsaturated fatty acids, riboflavin, saturated fats, selenium, thiamin, trans fats, vitamins A, B12, B6, C, D, E, and zinc. These items were adjusted for total energy intake using the residual method (64), and then summed. DII scores closer to −5 indicate a more anti-inflammatory diet, and scores closer to +5 indicate a more pro-inflammatory diet.
Data Analysis
Statistical analysis was conducted using Statistical Package for the Social Sciences (SPSS) version 27 (65). First, data was examined for normality and outliers. While depression variables were normally distributed, distributions of IL-6 and TNF-α values were significantly skewed (Skapiro-Wilk = 0.40 and 0.55, respectively), these scores were transformed using a natural logarithmic transformation to normalize the data. Two outliers were identified for IL-6 (92 and 60 pg/mL), and 1 for TNF-α (44 pg/mL). Outliers were windsorized by replacing values at or above 3 standard deviations above the mean with the next highest value (66). These transformation methods for cytokines are commonly used within the literature (52, 67). Alpha was set at 0.05 for all analyses.
Two-tailed Pearson correlations tested preliminary associations between the three predictor variables (DII, IL-6, and TNF-α) and the depression dimensions and total BDI-II scores. The univariate relationship between depression and inflammation was studied by hierarchical linear regression analyses. The somatic dimension, cognitive dimension, and total BDI-II scores were examined as separate dependent variables. First, inflammation level (IL-6, TNF-α) and DII score were entered as the independent variables separately, and then entered together. For models with independent variables entered together, multicollinearity was ruled out by calculating variance inflation factors (VIF). VIFs for IL-6, TNF-α, and DII were 1.96, 2.00, and 1.06, respectively.
Regression models were adjusted for demographic factors (age, income, and race/ethnicity). For all regression analyses, demographic factors were entered into the first step and inflammation measures were entered in the second step. Income was represented as a scale of 1–7, with each point representing one of the seven income groups. Racial/ethnic groups were represented as dummy variables with White as the reference group.
Results
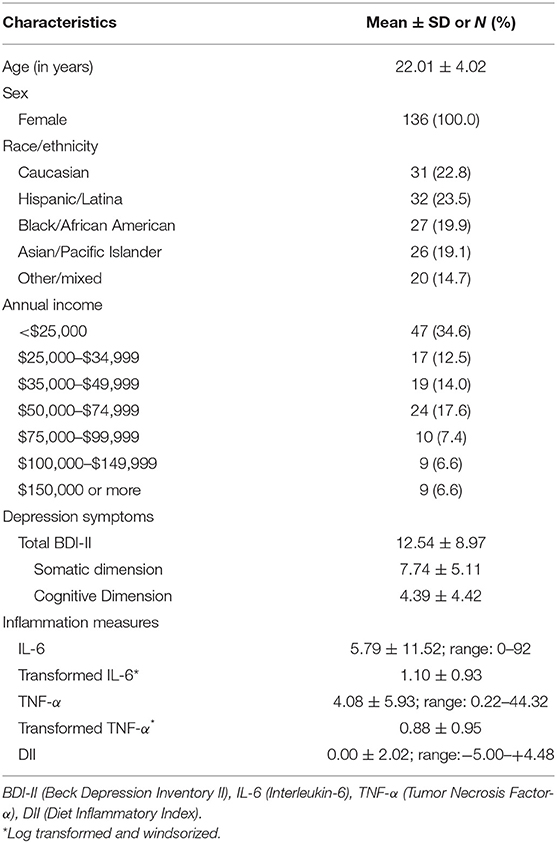
The sample included 136 adult female participants with ages ranging from 18 to 59 years old (M = 22.24, SD = 4.96). Table 1 shows a description of participants' demographic characteristics, and the descriptive statistics for depression, inflammation, and diet measures. Participants were racially/ethnically and economically diverse, with more than three-quarters of the participants identifying as Latina (23.5%), Black (19.9%), or Asian/Pacific Islander (19.1%) and a wide range of annual household income levels. Total BDI-II scores ranged from 0 to 51, the somatic dimension ranged from 0 to 26, and the cognitive dimension ranged from 0 to 22. Although this sample was recruited in a non-clinical setting, 40.4% (N = 55) of participants scored within the clinically significant range of symptom severity in the BDI-II. More specifically, based on clinical cutoff scores on the BDI-II, 29 (21.3%) participants reported mild clinical depressive symptoms, 20 (14.7%) reported moderate clinical depressive symptoms, and 6 (4.4%) scored in the severe clinical depressive symptom range. Participants had a mean DII score of 0.0 (SD = 2.02) with a range of −5 to +4.48, indicating that the average diet reported was neither pro- or anti-inflammatory.
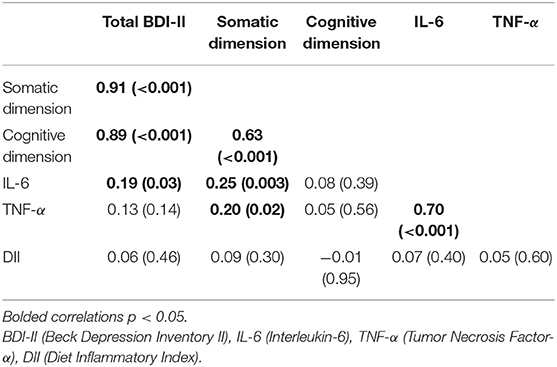
Table 2 shows bivariate correlations between depression and inflammation variables. Depression variables were positively correlated with each other, and inflammatory cytokines were positively correlated with each other. Inflammatory cytokines IL-6 and TNF-α were positively correlated with the somatic dimension, but not cognitive. IL-6 was positively correlated with total BDI-II scores. DII scores were not correlated with any measure.
Associations Between Inflammation and Depression
Results of demographic-adjusted models for the association between salivary cytokines and DII scores entered separately, and depression variables are presented in Table 3. Multiple regression results show that higher IL-6 was associated with report of more somatic symptoms of depression (ß = 0.273, p = 0.002) and higher total BDI-II scores (ß = 0.221, p = 0.012). IL-6 was not associated with cognitive symptoms of depression. Likewise, increased TNF-α was positively associated with the presence of more somatic symptoms (ß = 0.215, p = 0.017). TNF-α was not associated with the cognitive dimension nor total BDI-II scores. No significant association was observed between the DII and depression measures.
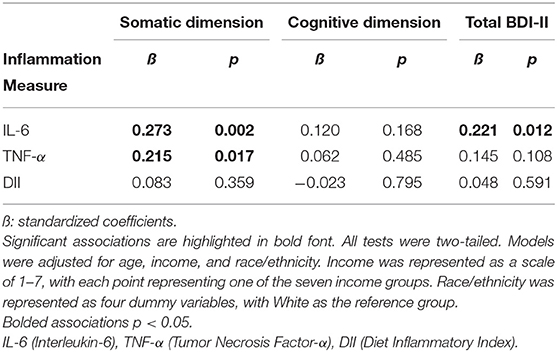
Table 3. Summary of multiple regression analysis examining the adjusted relationship between inflammation measures and dimensions of depression and total BDI-II scores.
Tables 4–6 show the results of demographic-adjusted models for the association between salivary cytokines and DII scores entered together, and depression variables. Overall, no model examining inflammation variables together were associated with depression variables. No covariates were significantly associated with depression variables in these models, although IL-6 approached significance (ß = 0.235, p = 0.052).
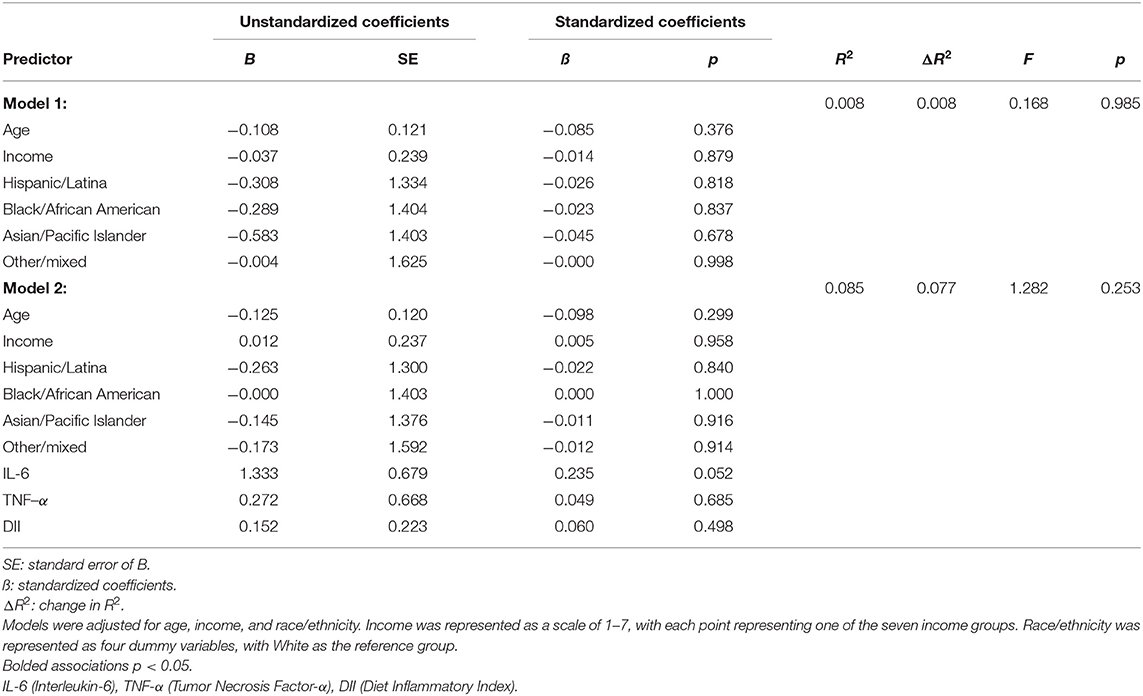
Table 4. Summary of multiple regression analysis examining the adjusted relationship between inflammation variables and the somatic dimension.
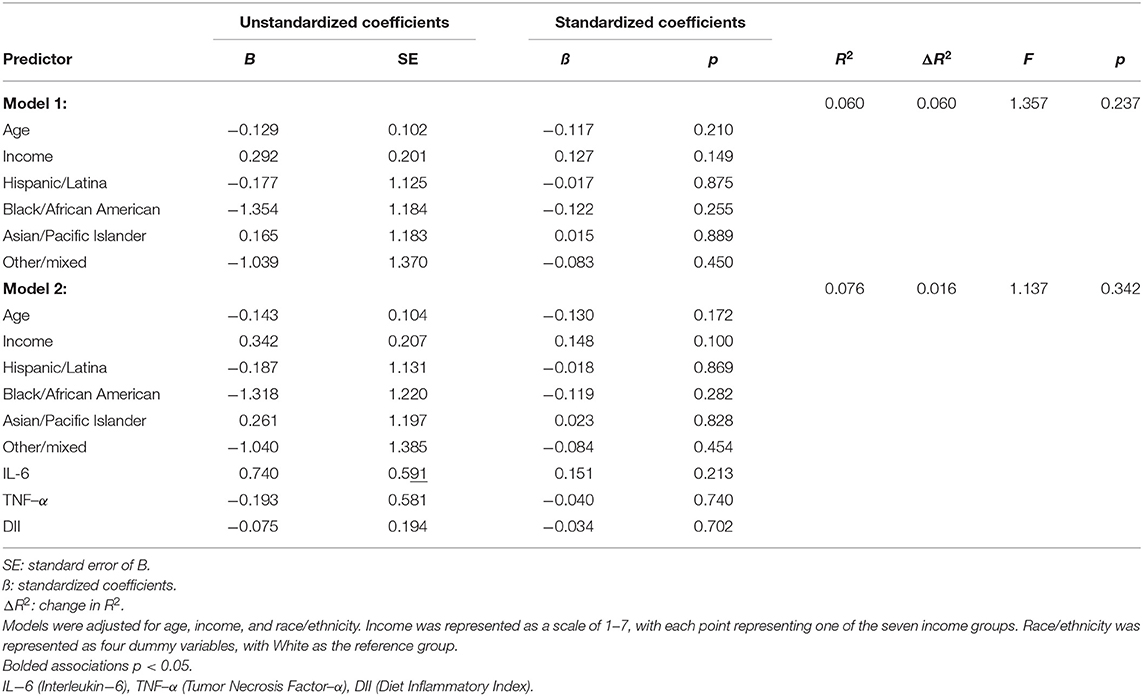
Table 5. Summary of multiple regression analysis examining the adjusted relationship between inflammation variables and the cognitive dimension.
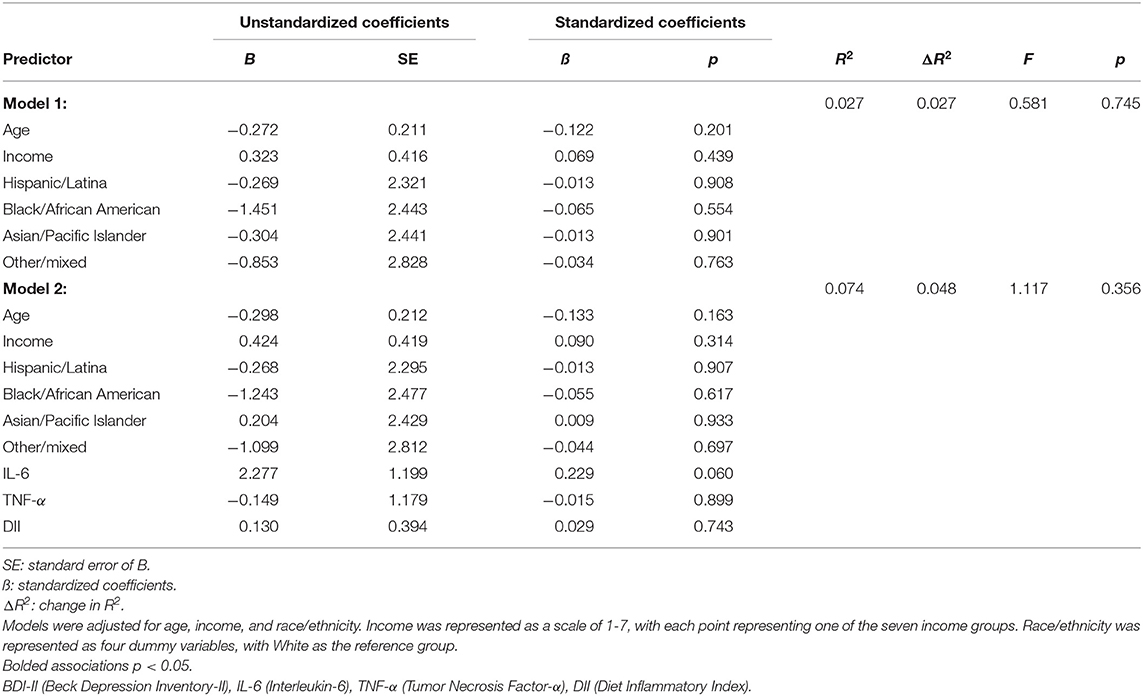
Table 6. Summary of multiple regression analysis examining the adjusted relationship between inflammation variables and total BDI-II scores.
Discussion
This study investigated the relationships between inflammatory cytokines and diet with dimensions of depressive symptoms among a diverse (i.e., socio-economic, race, and ethnicity) sample of women recruited in a non-clinical setting. Salivary inflammatory markers were found to be positively associated with the somatic dimension of depression when examined as separate independent variables. This finding parallels the results of other studies utilizing majority-White samples that found increased somatic symptoms, but not cognitive symptoms, to be associated with blood levels of IL-6 (39), TNF-α (36), and other inflammatory cytokines (6, 40, 68–71). These findings are also in concordance with the sickness behavior model, which posits that somatic depressive symptoms (sickness behavior) are related to immune system activity (12–15). After accounting for overlapping contributions, no inflammatory marker remained significant.
This study is the first to examine the relationship between dimensions of depressive symptoms and a measure of dietary patterns. Varying levels of an inflammatory diet pattern were not associated with depressive symptoms nor salivary cytokines. These findings contradict a review of six studies which found the DII to be positively associated with depressive symptoms in women (23), as well as existing research showing a relationship between the DII and biological markers for inflammation (62, 63, 72, 73). However, the present sample is racially and ethnically diverse, which has limited representation in the previous research, and signal the need for further attention. For instance, existing self-report measures of diet may not accurately or equally assess food consumption across different races or ethnicities (74–79) because diet composition can vary by culture (80); thus, future research with racially and ethnically diverse samples should include diet assessments that can capture culturally specific foods that have inflammatory potential. Furthermore, this study is of the first to examine salivary inflammation markers in relation to the DII. Future research comparing blood and salivary measures of inflammatory markers is needed. Of note, diet quality, inflammatory biomarkers, and depression are also associated with oxidative stress (81), absorption of specific vitamins (82, 83), psychological stress (84), gut microbiome health (85), and preferences for unhealthy foods (86). Collectively, this suggests that the relationships between the inflammatory potential of a diet, the actual level of inflammatory biomarkers observed, and depression is complex.
The current study is one of few that has examined the relationships between multiple inflammatory measures and meta-analysis derived depression dimensions of the BDI-II (87–89). There is a large amount of heterogeneity across research methods measuring somatic symptoms of depression within studies, making it challenging to draw distinct conclusions (51). For example, when using the BDI-II, some researchers rely on dimensions established in early dimension analyses of the BDI-II (38, 40) and others use dimensions that arise from data reduction techniques within their individual study (90, 91). Operationalizing dimensions consistently across studies is necessary to draw valid conclusions about the relationships between inflammatory markers and the somatic dimension of depression.
As this sample included only females, sex was controlled for. Prior research found females to be more susceptible to elevated inflammation (92), major depressive disorder (93), as well as inflammation-associated depressive symptoms (92, 94) which points to the importance of controlling for sex when studying the relationship between diet, inflammation, and depression. One limitation to an all-female sample, however, is that results may not be generalizable to males. This study was conducted in a non-clinical setting and examined the full range of depressive symptoms. However, 40% of participants reported scores above the clinical cutoff on the BDI-II, suggesting that they possibly meet criteria for a mood disorder. Community rates of individuals scoring above the clinical cutoff on the BDI-II ranged from 26% in racially/ethnically diverse student samples (95) to 30% in samples of Black adults (96). Rates may be higher in this current sample due to the intersectionality between female gender and racial/ethnic identity, as both are associated with greater vulnerability to depressive symptoms related to socio-cultural factors (97).
Several additional limitations should be considered. First, this study was cross-sectional precluding conclusions or interpretations about causality. This study did not account for time of day nor acute infection related to oral health, or otherwise, when collecting saliva samples. Salivary cytokine concentrations have been shown to have a diurnal rhythm (98) and be influenced by acute infection in the mouth such as gingivitis (99). There are known biases in self-report measures of dietary consumption including recall errors and social desirability factors (100, 101). Another limitation of this study is that it did not assess tobacco use, alcohol intake, or body mass index (BMI) as covariates.
In conclusion, this study provides support that both IL-6 and TNF-α are related to a meta-analysis derived somatic dimension of depression. A self-reported measure for an inflammatory diet pattern may be a less robust predictor of “inflamed depression” than salivary cytokines. Research aimed at phenotyping inflamed-depression subtypes should consider using consistent dimensions of depression, testing these relationships longitudinally, and examining additional biological factors such as gut microbiome health and nutrient absorption.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Brooklyn College Institution Review Board Human Research Protection Program. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DH contributed to conceptualization, writing (original draft, reviewing, and editing), formal analysis, and data curation. AP contributed to methodology, writing (reviewing and editing), investigation, and funding acquisition. LR contributed to conceptualization, methodology, writing (reviewing and editing), and supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Heppelmann Wacek Charitable Gift Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Raison CL, Miller AH. Is depression an inflammatory disorder? Curr Psychiatry Rep. (2011) 13:467–75. doi: 10.1007/s11920-011-0232-0
2. Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-Analysis of CRP levels. Psychol Med. (2019) 49:1958–70. doi: 10.1017/S0033291719001454
3. Opal SM, Depalo VA. Anti-inflammatory cytokines. Chest. (2000) 117:1162–72. doi: 10.1378/chest.117.4.1162
4. Zunszain PA, Hepgul N, Pariante CM, Zunszain PA, Hepgul ÁN, Pariante ÁCM. Inflammation and depression. Curr Top Behav Neurosci. (2013) 14:135–51. doi: 10.1007/7854_2012_211
5. Howren MB, Lamkin DM, Suls J. Associations of depression with c-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med. (2009) 71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
6. Duivis HE, Vogelzangs N, Kupper N, De Jonge P, Penninx B. Differential association of somatic and cognitive symptoms of depression and anxiety with inflammation: findings from the netherlands study of depression and anxiety (NESDA). Psychoneuroendocrinology. (2013) 38:1573–85. doi: 10.1016/j.psyneuen.2013.01.002
7. Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. Meta-analysis of cytokines in major depression. Biol Psychiatry. (2010) 67:446–57. doi: 10.1016/j.biopsych.2009.09.033
8. Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: a systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav Immun. (2019) 81:24–40. doi: 10.1016/j.bbi.2019.06.015
9. Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun. (2015) 49:206–15. doi: 10.1016/j.bbi.2015.06.001
10. Liu Y, Ho RCM, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: A meta-analysis and meta-regression. J Affect Disord. (2012) 139:230–9. doi: 10.1016/j.jad.2011.08.003
11. Köhler-Forsberg O, Buttenschøn HN, Tansey KE, Maier W, Hauser J, Dernovsek Z, et al. Association between C-reactive protein (CRP) with depression symptom severity and specific depressive symptoms in major depression. Brain Behav Immun. (2017) 62:344–50. doi: 10.1016/j.bbi.2017.02.020
12. Dantzer R. Cytokine, sickness behavior, and depression. Immunol Allergy Clin North Am. (2009) 29:247–64. doi: 10.1016/j.iac.2009.02.002
13. Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. (2008) 9. doi: 10.1038/nrn2297
14. Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. (1988) 12:123–37. doi: 10.1016/S0149-7634(88)80004-6
15. Smith RS. The macrophage theory of depression. Med Hypotheses. (1991) 35:296–306. doi: 10.1016/0306-9877(91)90272-Z
16. Charlton B. The malaise theory of depression: major depressive disorder is sickness bnehavior and antidepressants are analgenic. Med Hypotheses. (2000) 54:126–30. doi: 10.1054/mehy.1999.0986
17. Liu L, Zhu G. Gut-brain axis and mood disorder. Front Psychiatry. (2018) 9:1–8. doi: 10.3389/fpsyt.2018.00223
18. Petra AI, Panagiotidou S, Hatziagelaki E, Stewart JM, Conti P, Theoharides TC, et al. Gut-microbiota-brain axis and effect on neuropsychiatric disorders with suspected immune dysregulation HHS public access author manuscript. Clin Ther. (2015) 37:984–95. doi: 10.1016/j.clinthera.2015.04.002
19. Thorburn AN, Macia L, Mackay CR. Diet, metabolites, and “western-lifestyle” inflammatory diseases. Immunity. (2014) 40:833–42. doi: 10.1016/j.immuni.2014.05.014
20. Adjibade M, Andreeva VA, Lemogne C, Touvier M, Shivappa N, Hébert JR, et al. The inflammatory potential of the diet is associated with depressive symptoms in different subgroups of the general population. J Nutr. (2017) 147:879–87. doi: 10.3945/jn.116.245167
21. Lucas M, Chocano-Bedoya P, Shulze MB, Mirzaei F, O'Reilly ÉJ, Okereke OI, et al. Inflammatory dietary pattern and risk of depression among women. Brain Behav Immun. (2014) 36:46–53. doi: 10.1016/j.bbi.2013.09.014
22. Shivappa N, Hébert JR, Veronese N, Caruso MG, Notarnicola M, Maggi S, et al. The relationship between the dietary inflammatory index (DII(®)) and incident depressive symptoms: a longitudinal cohort study. J Affect Disord. (2018) 235:39–44. doi: 10.1016/j.jad.2018.04.014
23. Wang J, Zhou Y, Chen K, Jing Y, He J, Sun H, et al. Dietary inflammatory index and depression: a meta-analysis. Public Health Nutr. (2019) 22:654–60. doi: 10.1017/S1368980018002628
24. Firth J, Veronese N, Cotter J, Shivappa N, Hebert JR, Ee C, et al. What is the role of dietary inflammation in severe mental illness? A review of observational and experimental findings. Front psychiatry. (2019) 10:350. doi: 10.3389/fpsyt.2019.00350
25. Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. (2005) 81:341–54. doi: 10.1093/ajcn.81.2.341
26. Carrera-Bastos P, Fontes O'Keefe Lindeberg Cordain. The western diet and lifestyle and diseases of civilization. Res Reports Clin Cardiol. (2011) 15. doi: 10.2147/RRCC.S16919
27. Akbaraly TN, Brunner EJ, Ferrie JE, Marmot MG, Kivimaki M, Singh-Manoux A. Dietary pattern and depressive symptoms in middle age. Br J Psychiatry. (2009) 195:408–13. doi: 10.1192/bjp.bp.108.058925
28. Jacka FN, Pasco JA, Williams LJ, Meyer BJ, Digger R, Berk M. Dietary intake of fish and PUFA, and clinical depressive and anxiety disorders in women. Br J Nutr. (2013) 109:2059–66. doi: 10.1017/S0007114512004102
29. Lai JS, Hiles S, Bisquera A, Hure AJ, Mcevoy M, Attia J, et al. systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. (2014) 99:181–97. doi: 10.3945/ajcn.113.069880
30. Shattuck EC, Muehlenbein MP. Towards an integrative picture of human sickness behavior. Brain Behav Immun. (2016) 57:255–62. doi: 10.1016/j.bbi.2016.05.002
31. Parker G, Fletcher K, Paterson A, Anderson J, Hong M. Gender differences in depression severity and symptoms across depressive sub-types. J Affect Disord. (2014) 167:351–7. doi: 10.1016/j.jad.2014.06.018
32. Fried EI, Nesse RM. Depression sum-scores don't add up: why analyzing specific depression symptoms is essential. BMC Med. (2015) 13:72. doi: 10.1186/s12916-015-0325-4
33. Maes M, Berk M, Goehler L, Song C, Anderson G, Gałecki P, Leonard B. Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. (2012) 10. doi: 10.1186/1741-7015-10-66
34. Majd M, Saunders EFH, Engeland CG. Inflammation and the dimensions of depression: a review. Front Neuroendocrinol. (2020) 56. doi: 10.1016/j.yfrne.2019.100800
35. Whisman MA, Perez JE, Ramel W. Factor structure of the beck depression inventory-second edition (bdi-ii) in a student sample. J Clin Psychol. (2000) 56:545–51. doi: 10.1002/(sici)1097-4679(200004)56:4<545::aid-jclp7>3.0.co;2-u
36. Dannehl K, Rief W, Schwarz MJ, Hennings A, Riemer S, Selberdinger V, et al. The predictive value of somatic and cognitive depressive symptoms for cytokine changes in patients with major depression. Neuropsychiatr Dis Treat. (2014) 10:1191–7. doi: 10.2147/NDT.S61640
37. Euteneuer F, Schwarz MJ, Dannehl K, Hartung A, Westermann S, Rief W. Increased soluble interleukin-2 receptor levels are related to somatic but not to cognitive-affective features in major depression. Brain Behav Immun. (2012) 26:1244–8. doi: 10.1016/j.bbi.2012.06.007
38. Elovainio M, Aalto AM, Kivimäki M, Pirkola S, Sundvall J, Lönnqvist J, et al. Depression and C-reactive protein: population-based health 2000 study. Psychosom Med. (2009) 71:423–30. doi: 10.1097/PSY.0b013e31819e333a
39. Stewart JC, Rand KL, Muldoon MF, Kamarck TW. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain Behav Immun. (2009) 23:936–44. doi: 10.1016/j.bbi.2009.04.011
40. Euteneuer F, Dannehl K, del Rey A, Engler H, Schedlowski M, Rief W. Peripheral immune alterations in major depression: The role of subtypes and pathogenetic characteristics. Front Psychiatry. (2017) 8:8–13. doi: 10.3389/fpsyt.2017.00250
41. Bremmer MA, Beekman ATF, Deeg DJH, Penninx BWJH, Dik MG, Hack CE, et al. Inflammatory markers in late-life depression: Results from a population-based study. J Affect Disord. (2008) 106:249–55. doi: 10.1016/j.jad.2007.07.002
42. Chu AL, Stochl J, Lewis G, Zammit S, Jones PB, Khandaker GM. Longitudinal association between inflammatory markers and specific symptoms of depression in a prospective birth cohort. Brain Behav Immun. (2019) 76:74–81. doi: 10.1016/j.bbi.2018.11.007
43. Einvik G, Vistnes M, Hrubos-Strøm H, Randby A, Namtvedt SK, Nordhus IH, et al. Circulating cytokine concentrations are not associated with major depressive disorder in a community-based cohort. Gen Hosp Psychiatry. (2012) 34:262–7. doi: 10.1016/j.genhosppsych.2012.01.017
44. Krogh J, Benros ME, Jørgensen MB, Nordentoft M. The association between depressive symptoms, cognitive function, and inflammation in major depression. Brain Behav Immun. (2013) 35:70–6. doi: 10.1016/j.bbi.2013.08.014
45. Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio. (1996) 78:490–8. doi: 10.1037/t00742-000
46. Granger DA, Kivlighan KT, Fortunato C, Harmon AG, Hibel LC, Schwartz EB, et al. Integration of salivary biomarkers into developmental and behaviorally-oriented research: problems and solutions for collecting specimens. Physiol Behav. (2007) 92:583–90. doi: 10.1016/j.physbeh.2007.05.004
47. Walsh E, Eisenlohr-Moul T, Baer R. Brief mindfulness training reduces salivary IL-6 and TNF. J Consult Clin Psychol. (2016) 887–97. doi: 10.1037/ccp0000122
48. Keller PS, El-Sheikh M, Vaughn B, Granger DA. Relations between mucosal immunity and children's mental health: the role of child sex. Physiol Behav. (2010) 101:705–12. doi: 10.1016/j.physbeh.2010.08.012
49. Reigada LC, Buchanan EM, Hazeltine DB. Shakil H, Polokowski AR. A pilot randomized controlled trial testing supplements of omega-3 fatty acids, probiotics, combination or placebo on symptoms of depression, anxiety and stress. J Affect Disord Reports. (2021) 5:100141. doi: 10.1016/j.jadr.2021.100141
50. Osman MA, Barrios FX, Gutierrez PM, Williams JE, Bailey J, Osman A. Psychometric properties of the beck depression inventory-II in nonclinical adolescent samples. J Clin Psychol. (2008) 64:83–102. doi: 10.1002/jclp.20433
51. Huang C, Chen JH. Meta-analysis of the factor structures of the beck depression inventory–II. Assessment. (2015) 22:459–72. doi: 10.1177/1073191114548873
52. Riis JL, Ahmadi H, Hamilton KR, Hand T, Granger DA. Best practice recommendations for the measurement and interpretation of salivary proinflammatory cytokines in biobehavioral research. Brain Behav Immun. (2020)0−1. doi: 10.1016/j.bbi.2020.09.009
53. Glaus J, Vandeleur CL, von Känel R, Lasserre AM, Strippoli MPF, Gholam-Rezaee M, et al. Associations between mood, anxiety or substance use disorders and inflammatory markers after adjustment for multiple covariates in a population-based study. J Psychiatr Res. (2014) 58:36–45. doi: 10.1016/j.jpsychires.2014.07.012
54. Stebbins J, Granger S. Validation Report: Inflammatory Cytokine Multiplex Validation Report Item NO. 5209 Research Use Only. Carlsbad, CA: Salimetrics (2017).
55. National Cancer Institute. Diet History Questionnaire, Version 2.0. Bethesda, MD: National Cancer Institute (2010).
56. Diet History Questionnaire. National Institutes of Health, Epidemiology and Genomics Research Program. Bethesda, MD: National Cancer Institute (2010).
57. Ahuja JKC, Moshfegh AJ, Holden JM, Harris E. USDA food and nutrient databases provide the infrastructure for food and nutrition research, policy, and practice. J Nutr. (2013) 143:241S−9S. doi: 10.3945/jn.112.170043
58. DHQ Nutrient Database. dhq2.database.092914.csv. Bethesda, MD: National Cancer Institute (2012).
59. Thompson FE, Subar AF. Dietary Assessment Methodology. (2017). doi: 10.1016/B978-0-12-802928-2.00001-1
60. Subar A, Thompson F. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America's table study. Am J Epidemiol. (2001) 154:1089–99. doi: 10.1093/aje/154.12.1089
61. Shivappa N, Steck S, Hurley T. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. (2014) 17:1689–96. doi: 10.1017/S1368980013002115
62. Shivappa N, Hebert JR, Marcos A, Diaz L-E, Gomez S, Nova E, et al. Association between dietary inflammatory index and inflammatory markers in the HELENA study. Mol Nutr Food Res. (2017) 61:1600707. doi: 10.1002/mnfr.201600707
63. Tabung FK, Steck SE, Zhang J, Ma Y, Liese AD, Agalliu I, et al. Construct validation of the dietary inflammatory index among postmenopausal women. Ann Epidemiol. (2015) 25:398–405. doi: 10.1016/j.annepidem.2015.03.009
64. Willett W, Stampfer MJ. Total energy intake: Implications for epidemiologic analyses. Am J Epidemiol. (1986) 124:17–27. doi: 10.1093/oxfordjournals.aje.a114366
67. Riis JL, Out D, Dorn LD, Beal SJ, Denson LA, Pabst S, et al. Salivary cytokines in healthy adolescent girls: Intercorrelations, stability, and associations with serum cytokines, age, and pubertal stage. Dev Psychobiol. (2014)
68. White Phd J, Kivimäki Phd M, Phd MJ, David G, Dsc B. Association of inflammation with specific symptoms of depression in a general population of older people: the English Longitudinal Study of Ageing. Brain Behav Immun. (2016) 61:27–30. doi: 10.1016/j.bbi.2016.08.012
69. Case SM, Stewart JC. Race/ethnicity moderates the relationship between depressive symptom severity and C-reactive protein: 2005-2010 NHANES data. Brain Behav Immun. (2014) 41:101–8. doi: 10.1016/j.bbi.2014.04.004
70. Michal M, Wiltink J, Kirschner Y, Wild PS, Mü Nzel T. Differential associations of depressive symptom dimensions with cardio-vascular disease in the community: results from the gutenberg health study. PLoS ONE. (2013) 8:72014. doi: 10.1371/journal.pone.0072014
71. Iob E, Kirschbaum C. Persistent depressive symptoms, HPA-axis hyperactivity, and inflammation: the role of cognitive-affective and somatic symptoms. Mol Psychiatry. (2020) 25:1130–40. doi: 10.1038/s41380-019-0501-6
72. Shivappa N, Hébert JR, Rietzschel ER, De Buyzere ML, Langlois M, Debruyne E, et al. Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br J Nutr. (2015) 113:665–71. doi: 10.1017/S000711451400395X
73. Phillips CM, Shivappa N, Hébert JR, Perry IJ. Dietary inflammatory index and biomarkers of lipoprotein metabolism, inflammation and glucose homeostasis in adults. Nutrients. (2018) 10:1–13. doi: 10.3390/nu10081033
74. Coates RJ, Serdula MK, Byers T, Mokdad A, Jewell S, Leonard SB, et al. brief, telephone-administered food frequency questionnaire can be useful for surveillance of dietary fat intakes. J Nutr. (1995) 125:1473–83.
75. Davis JN, Nelson MC, Ventura EE, Lytle LA, Goran MI. A brief dietary screener: appropriate for overweight Latino adolescents? J Am Diet Assoc. (2009) 109:725–9. doi: 10.1016/j.jada.2008.12.025
76. Jensen MK, Koh-Banerjee P, Hu FB, Franz M, Sampson L, Grønbæk M, et al. Intakes of whole grains, bran, and germ and the risk of coronary heart disease in men. Am J Clin Nutr. (2004) 80:1492–9. doi: 10.1093/ajcn/80.6.1492
77. Liu F, Malaval L, Gupta AK, Aubin JE. Simultaneous detection of multiple bone-related mRNAs and protein expression during osteoblast differentiation: polymerase chain reaction and immunocytochemical studies at the single cell level. Dev Biol. (1994) 166:220–34. doi: 10.1006/dbio.1994.1309
78. Stram DO, Hankin JH, Wilkens LR, Pike MC, Monroe KR, Park S, et al. Calibration of the dietary questionnaire for a multiethnic cohort in Hawaii and Los Angeles. Am J Epidemiol. (2000) 151:358–70. doi: 10.1093/oxfordjournals.aje.a010214
79. Reigada LC, Buchanan EM, Hazeltine DB. Shakil H, Polokowski AR. Assessment of polyunsaturated fatty acids: A self-report and biomarker assessment with a racially and ethnically diverse sample of women. Prostaglandins Leukot Essent Fat Acids. (2021) 164:102214. doi: 10.1016/j.plefa.2020.102214
80. Akbar JA, Jaceldo-Siegl K, Fraser G, Herring RP, Yancey A. The contribution of soul and Caribbean foods to nutrient intake in a sample of Blacks of US and Caribbean descent in the Adventist Health Study-2: a pilot study. Ethn Dis. (2007) 17:244–9. doi: 10.1093/aje/163.suppl_11.S31-c
81. Huang Q, Liu H, Suzuki K, Ma S, Liu C. Linking what we eat to our mood: A review of diet, dietary antioxidants, and depression. Antioxidants. (2019) 8. doi: 10.3390/antiox8090376
82. Huang X, Fan Y, Han X, Huang Z, Yu M, Zhang Y, et al. Association between serum vitamin levels and depression in U.S. adults 20 years or older based on national health and nutrition examination survey 2005-2006. Int J Environ Res Public Health. (2018) 15. doi: 10.3390/ijerph15061215
83. Mitchell ES, Conus N, Kaput J. B vitamin polymorphisms and behavior: Evidence of associations with neurodevelopment, depression, schizophrenia, bipolar disorder and cognitive decline. Neurosci Biobehav Rev. (2014) 47:307–20. doi: 10.1016/j.neubiorev.2014.08.006
84. Bremner JD, Moazzami K, Wittbrodt MT, Nye JA, Lima BB, Gillespie CF, et al. Diet, stress and mental health. Nutrients. (2020) 12:2428. doi: 10.3390/nu12082428
85. Bastiaanssen TFS, Cussotto S, Claesson MJ, Clarke G, Dinan TG, Cryan JF. Gutted! unraveling the role of the microbiome in major depressive disorder. Harv Rev Psychiatry. (2020) 28:26–39. doi: 10.1097/HRP.0000000000000243
86. Bartkiene E, Steibliene V, Adomaitiene V, Juodeikiene G, Cernauskas D, Lele V, et al. Factors affecting consumer food preferences: food taste and depression-based evoked emotional expressions with the use of face reading technology. Biomed Res Int. (2019) 2019. doi: 10.1155/2019/2097415
87. Schmidt FM, Schröder T, Kirkby KC, Sander C, Suslow T, Holdt LM, et al. Pro- and anti-inflammatory cytokines, but not CRP, are inversely correlated with severity and symptoms of major depression. Psychiatry Res. (2016) 239:85–91. doi: 10.1016/j.psychres.2016.02.052
88. Schmidt FM, Sander C, Minkwitz J, Mergl R, Dalton B, Holdt LM, et al. Serum markers of inflammation mediate the positive association between neuroticism and depression. Front Psychiatry. (2018) 9:609. doi: 10.3389/fpsyt.2018.00609
89. Jeon YJ, Cho SMJ, Lee YJ, Kim HC, Jung SJ. Depressive symptoms, its sub-factors, and augmentation index: the modifying effects according to inflammatory markers. J Affect Disord. (2020) 272:380–7. doi: 10.1016/j.jad.2020.03.174
90. Marijnissen RM, Bus BAA, Holewijn S, Franke B, Purandare N, De Graaf J, et al. Depressive symptom clusters are differentially associated with general and visceral obesity. J Am Geriatr Soc. (2011) 59:67–72. doi: 10.1111/j.1532-5415.2010.03228.x
91. Uher R, Tansey KE, Dew T, Maier W, Mors O, Hauser J, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry. (2014) 171:1278–86. doi: 10.1176/appi.ajp.2014.14010094
92. Lasselin J, Lekander M, Axelsson J, Karshikoff B. Sex differences in how inflammation affects behavior: What we can learn from experimental inflammatory models in humans. Front Neuroendocrinol. (2018) 50:91–106. doi: 10.1016/j.yfrne.2018.06.005
93. Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. (2015) 40:219–21. doi: 10.1503/jpn.150205
94. Derry HM, Padin AC, Kuo JL, Hughes S, Kiecolt-Glaser JK. Sex Differences in Depression: Does Inflammation Play a Role? Curr Psychiatry Rep. (2015) 17:1–10. doi: 10.1007/s11920-015-0618-5
95. Whisman MA, Richardson ED. Normative data on the beck depression inventory - second edition (BDI-II) in college students. J Clin Psychol. (2015) 71:898–907. doi: 10.1002/jclp.22188
96. Hambrick JP, Rodebaugh TL, Balsis S, Woods CM, Mendez JL, Heimberg RG. Cross-ethnic measurement equivalence of measures of depression, social anxiety, and worry. Assessment. (2010) 17:155–71. doi: 10.1177/1073191109350158
97. Patil PA, Porche M V, Shippen NA, Dallenbach NT, Fortuna LR. Which girls, which boys? The intersectional risk for depression by race and ethnicity, and gender in the US. Clin Psychol Rev. (2018) 66:51–68. doi: 10.1016/j.cpr.2017.12.003
98. Izawa S, Miki K, Liu X, Ogawa N. The diurnal patterns of salivary interleukin-6 and C-reactive protein in healthy young adults. Brain Behav Immun. (2013) 27:38–41. doi: 10.1016/j.bbi.2012.07.001
99. Diesch T, Filippi C, Fritschi N, Filippi A, Ritz N. Cytokines in saliva as biomarkers of oral and systemic oncological or infectious diseases: A systematic review. Cytokine. (2021) 143:155506. doi: 10.1016/j.cyto.2021.155506
100. Freedman LS, Carroll RJ, Wax Y. Estimating the relation between dietary intake obtained from a food frequency questionnaire and true average intake. Am J Epidemiol. (1991) 134:310–20. doi: 10.1093/oxfordjournals.aje.a116086
Keywords: depression, inflammation, diet, cytokines, somatic, neurovegetative, nutrition
Citation: Hazeltine DB, Polokowski AR and Reigada LC (2022) Inflammatory Cytokines, but Not Dietary Patterns, Are Related to Somatic Symptoms of Depression in a Sample of Women. Front. Psychiatry 13:822466. doi: 10.3389/fpsyt.2022.822466
Received: 25 November 2021; Accepted: 04 March 2022;
Published: 16 May 2022.
Edited by:
Karen Tabb, University of Illinois at Urbana-Champaign, United StatesReviewed by:
Sylvie Vancassel, INRA Centre Bordeaux-Aquitaine, FranceAlina Wilkowska, Medical University of Gdansk, Poland
Eric Shattuck, University of Texas at San Antonio, United States
Copyright © 2022 Hazeltine, Polokowski and Reigada. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Christine Reigada, bHJlaWdhZGFAYnJvb2tseW4uY3VueS5lZHU=
 Danielle Belden Hazeltine
Danielle Belden Hazeltine Ashley Rose Polokowski1,2,3
Ashley Rose Polokowski1,2,3 Laura Christine Reigada
Laura Christine Reigada