
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry, 22 February 2022
Sec. Psychological Therapy and Psychosomatics
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.813506
This article is part of the Research TopicPsychocardiology: Exploring the Brain-Heart InterfaceView all 27 articles
 Da-Hee Park1,2*
Da-Hee Park1,2* Tanja Meltendorf3
Tanja Meltendorf3 Kai G. Kahl3
Kai G. Kahl3 Jan C. Kamp1,2
Jan C. Kamp1,2 Manuel J. Richter4,5
Manuel J. Richter4,5 Marius M. Hoeper1,2
Marius M. Hoeper1,2 Karen M. Olsson1,2†
Karen M. Olsson1,2† Jan Fuge1,2†
Jan Fuge1,2†Introduction: Mental disorders are common in patients with pulmonary arterial hypertension (PAH) and contribute to impaired quality of life (QoL). The impact of mental disorders on access to health care, differences in clinical parameters and treatment in patients with PAH is unclear. In this study we sought to assess the impact of mental disorders and other health disparities on health-care-utilization in patients with PAH.
Methods: In a cross-sectional observational study of patients with PAH, mental disorders were characterized using a structed clinical interview. In addition, patients completed a self-administered questionnaire to assess QoL, symptoms of anxiety and depression, lifestyle-factors and educational status. Number of outpatient visits and communication events per year were calculated as a surrogate for health-care-utilization and were compared by the presence of mental disorder. Linear regression analysis was conducted to assess the impact on health-care-utilization.
Results: 117 patients with PAH participated in this study (70% female, median age 59 (interquartile range, 49–70) years). Significant differences between patients with or without mental disorders were found in anxiety, depression and QoL. There were no significant differences in clinical parameters. Patients with mental disorders had higher rates of outpatient visits and communication events than patients without mental disorders. Linear regression revealed a gain of 2.2 communication events per year in the presence of any mental disorders.
Conclusion: Mental disorders in patients with PAH are common and significantly affect health-care-utilization. This higher demand in patients with mental disorder needs to be addressed by physicians, psychiatrists and specialized nurses offering therapeutic strategies.
Pulmonary arterial hypertension (PAH) is a rare disease characterized by increased pulmonary vascular resistance due to remodeling of pulmonary vasculature (1, 2). Symptoms of PAH include clinical signs of heart failure, dyspnea on exertion, syncope leading to impaired physical activities and a reduced quality of life (QoL) (3). Therapy of PAH has greatly advanced over the last decades improving clinical outcomes and survival of PAH patients. However, PAH remains a fatal illness with right heart failure being the primary cause of death (4).
Mental disorders such as major depression disorder (MDD) or panic disorder (PD) are common in patients with PAH, and patient's quality of life, mental health, and access to medical care have been addressed in recent studies (5–10). The prevalence of anxiety, depression and adjustment disorders in patients with PAH correlate with disease progression, intensity of symptoms as well as functional impairment (11, 12). Mental disorders such as major depression disorder, panic disorder or adjustment disorder are common in patients with PAH (13).
Health disparities are defined as significant differences in health or outcomes with correlation to greater obstacles to healthcare based on ethnicity, sex, age, socioeconomic status, occupation, mental health, cognitive or physical disability (14). Health disparities can impact quality of life, disease treatment and outcomes (15, 16). With only few studies addressing health disparities in patients with PAH, the American Thoracic Society encouraged further research to achieve more equitable care, improve advocacy efforts and public health policy for patients with PAH (8). Health disparities, in particular mental disorders may contribute to differences in clinical parameters, treatment and survival in patients with PAH. Thus, in this study, we sought to assess possible implications of mental disorders in patients with PAH leading to differences in PAH treatment and health-care utilization.
This cross-sectional observational study included patients with a confirmed diagnosis of PAH from one PH referral center (Hannover Medical School in Germany). This patient cohort is a subsample of a larger cohort that was originally described by Olsson et al. (13). All patients gave written informed consent and the study was approved by the local institutional review board (Nr. 8540_BO_K_2019). Patients were contacted and interviewed between September 2019 and March 2020 to perform a structured clinical interview. This study further comprised self-administrated questionnaires and data was enriched using a clinical research database.
Patients were selected from a clinical research database based on diagnosis of PAH according to current criteria (1) and age ≥ 18 years. Assessment included hemodynamics from right heart catherization at time of diagnosis, 6-minute walk distance (6MWD), serum levels of N-terminal fragment of pro-brain natriuretic peptide (NT-proBNP), WHO functional class (FC) and diffusing capacity of the lung for carbon monoxide (DLCO). Lifestyle factors included smoking status (active smoker, former smoker or never-smoker), duration of smoking and mean number of cigarettes per day to calculate the number of packyears (17) as well as alcohol abuse as drinks per week.
Psychiatric characterization was performed using the Structured Clinical Interview (SCID) for Diagnostic and Statistical Manual of Mental Disorders, fifth Edition (DSM-V) by a medical student carefully trained and under the supervision of a senior physician to determine the presence of MDD and PD and covered the past 4 weeks prior to the interview (18). The Hospital Anxiety and Depression Scale (HADS) was used to assess symptoms of anxiety and depression (19). The HADS questionnaire comprises two subscales for anxiety (HADS-A) and depression (HADS-D), each containing 7 questions for a maximum of 21 points per subscale. Higher scores indicating a more severe anxiety or depression. A score > 11 per subscale was proposed by Bjelland et al. and Lowe to be associated with significant anxiety or depression while a cut-off score of > 8 for both subscores showing probable signs of anxiety or depression (20, 21). The World Health Organization Quality of Life [WHO-QoL-BREF (22)] questionnaire was used to assess quality of life. To assess patients educational status, the sociodemographic standards of the German Federal Statistical Office (destatis) (23) were applied. Further educational status was categorized in low (no education), moderate (non-academic education) and high (academic education) educational status.
Total number of outpatient visits and patient communication datasets were derived from a clinical research database as well as the date from first and last outpatient visit or communication event respectively. Patient communication is defined as any kind of unscheduled communication event (e.g., e-mail, mail, phone calls or other correspondence) documented in the clinical research database by a physician or a specialized nurse. Time-variables comprising the time in years between first and last date of outpatient visit or communication event were calculated and set into relation to the number of visits and communications. This allowed us to calculate outpatient visits and communication events per year for each patient.
IBM SPSS Statistics (version 28.0, IBM Corp., Armonk, New York) and Stata 13.0 (State Corp LP, College Station, Texas, USA) statistical software programs were used for statistical analysis. Continuous parameters are presented as median and interquartile range (Q25-Q75) or as mean and standard deviation (SD). Categorical variables are presented as number (n) and percent (%). Comparisons of continuous parameters were conducted using t-test or Mann-Whitney U test and comparison of categorical parameters by using Chi-square-test or fisher's exact test, unless indicated otherwise. Linear regression models calculated on dependent variables outpatient visits per year and correspondences per year in a stepwise forward setting. Independent variables were age, sex, packyears, HADS-A and HADS-D scores, QoL, education, WHO FC, 6MWD and the diagnosis of any MDD or PD. All tests were two-sided, p-values < 0.05 were considered statistically significant.
A total of 117 patients were enrolled in this study. Patient characteristics are shown in Table 1. The majority of patients were female (n=82, 70%); median age was 59 (interquartile range, 49–70) years. Twenty six patients presented with MDD and 10 patients with PD resulting in 31 (27%) patients (five patients had a combination of MDD or PD). All patients were treated with PAH medications, most of them (73%) with combination therapy. Disease severity indicated by WHO FC, 6MWD, NT-proBNP, DLCO, hemodynamics at time of diagnosis as well as PAH treatment did not differ between patients with or without mental disorders (Table 1). In addition, there were no differences in drinking habits or exercise scores but patients with any form of mental disorder were nearly two-times more likely to be active smokers (23 vs. 12%). Patients with MDD or PD had significantly worse HADS-A and HADS-D scores. Psychological and physical QoL was worse in patients with MDD or PD (all p < 0.001).
Detailed results are stated in Table 2. Grouped together, the patients had a median number of 2.2 outpatient visits and 1.8 communication events per year. Comparison of visits and communication revealed significant differences between patients with and without MDD or PD. Patients with MDD or PD had significantly more outpatient visits per year compared to patients without MDD or PD (2.4 vs. 2.2 visits per year, p = 0.022, Figure 1A). The number of communication events also differed significantly (Figure 1B), with 2.8 (interquartile range, 1.8–6.2) communication events per year in patients with MDD or PD compared to 2.1 (interquartile range, 1.0–2.9) communication events in patients without MDD or PD (p = 0.001).
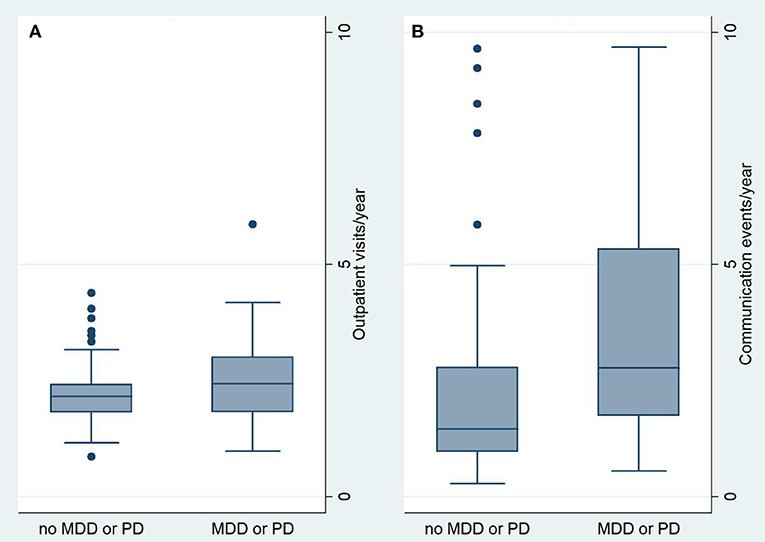
Figure 1. Comparison of Outpatient visits/year (A) and communication events/year (B). MDD, major depressive disorder; PD, panic disorder.
Impact on number of outpatient visits and communication events was tested using clinical parameters, the presence of MDD or PD, QoL and lifestyle factors. Linear regression analysis showed a significant impact of age and 6MWD on the number of visits per year. Per 10 years of patients age there was a loss of 0.2 visits per year (p = 0.003) and per 50 m 6MWD there was a loss of 0.1 visits per year (p = 0.007). Impact on communication events per year was only determined by the presence of MDD or PD. If a patient had any current MDD or PD, correspondence increased by 2.2 communication events per year (p = 0.001) with the linear regression analysis stating a constant of 2.4 communication events per year. This results in a near two-fold number of communication events in the presence of MDD or PD. The other covariates sex, packyears, HADS-A and HADS-D scores, QoL, education and WHO FC had no significant impact on the number of outpatient visits or communication events per year.
The main finding of this study can be summarized as follows: patients with MDD or PD have a higher need for patient care with a higher demand for extracurricular communication. The presence of MDD or PD was the only factor significantly influencing the rate of communication events. Patients with MDD or PD had worse QoL and HADS-scores while no differences in PAH medication or lifestyle factors were found. Education had no impact on number of outpatient visits or communication events nor were there any differences in education between patients with or without MDD or PD.
Impact on outpatient visits was determined by age and 6MWD while communication events were impacted by the presence of MDD or PD. While the association of age and 6MWD on outpatient visits was significant, absolute differences in number of outpatient visits were small suggesting only limited impact on clinical practice. Overall, the difference of 0.2 or 0.1 visits per year respectively might not result in an impaired health-care-utilization for patients with MDD or PD.
The only determinant for an increased number of communication events was the presence of MDD or PD. These patients had an almost two-fold increase in communication events while there were no differences in therapy strategies or disease severity (Table 1). This is in line with previous studies showing that the presence of a mental health disorder is associated with significantly higher health care resource utilization and costs independent of disease severity (24, 25).
Communication events beyond outpatient visits seem to be a valuable instrument for patients with mental disorders to facilitate health-care-utilization. Recent data have shown that the use of telecommunications such as video consultations reduced the need for onsite outpatients visits with increased use during the COVID-19 pandemic (26). While established patients had no worsening of mental disorders during the Covid-19 pandemic (27), health care utilization in form of diagnostic delay and increased time to referral in patients with PAH was impaired (28). Thus, future strategies and technologies are needed to fulfill patient's health-care-needs.
Our findings raise questions about optimizing the management of patients with PAH especially in the setting of mental disorders. First, mental disorders such as major depressive disorders or panic disorders need to be assessed in routine care. However, a SCID maybe not be feasible for screening purposes. The HADS was recently proven to detect anxiety and depression in patients with PAH (13) but also other tools such as the Hamilton Anxiety- or Depression Scale (HAM-A or HAM-D) might be feasible. Further, studies have shown that poor access to coordinated mental health care had impact on acute health-care-utilization. Different models of care such as a multidisciplinary approach with the integration of medical and psychiatric health care have been described in primary as well as specialty care such as is PAH care (29). Recent studies have shown a higher prevalence of adjustment disorders among mental disorders in patients with PAH (13). Metacognitive treatment, a cognitive behavioral therapy, has been successfully applied to a patient with newly diagnosed PAH suffering from severe adjustment disorder (30, 31). With only limited data on psychiatric treatment options in patients with PAH, further studies are needed. This preliminary report on health disparities and health care utilization raises the question of improved patient care for patients with PAH. Knowledge, deeper understanding, and education of psychiatric disorders is key to prevent further stigma, increase awareness for patients challenges and needs and improve QoL beyond the physical burden of PAH. We suggest a specialized approach to address the needs of patients with MDD or PD through available treatment programs. PAH patients with MDD or PD have an increased need for assistance of social workers, physiotherapist and occupational therapist which should be a valuable asset in PAH patient's care. Further the availability of fast-track psychiatric consultations and acute crisis management should be of importance. In summery we suggest a comprehensive multidisciplinary psychiatric medical care for patients with MDD or PD and conclude that further research is needed to inform clinicians on the differences in health care utilization in the presence of psychiatric disorders.
This study has limitations and strength. One limitation is the monocentric cross-sectional design of the study and the use of outpatients visits and another that communication events per year as a surrogate for health-care-utilization has not been validated. Further no economical evaluation has been conducted. However, for a rare disease the analyzed sample size is high and the SCID-derived diagnosis of mental disorders is considered the gold standard of psychiatric assessment.
Compared to PAH patients without mental disorders, patients with MDD or PD are more likely to seek communication with their health care provider and health care systems should address the higher need of patients with MDD or PD. These findings were independent of disease severity or therapy. Future studies are needed to inform clinicians, psychiatrists and specialized nurses on differences in health care utilization as well as patients' individual needs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Hannover Medical School. The patients/participants provided their written informed consent to participate in this study.
DHP was responsible for study design, implementation of the study, data collection, data interpretation and drafting the manuscript. TM was responsible for data collection and revising the manuscript. KK was responsible for study design, data interpretation, and revising the manuscript. JK was responsible for data interpretation and revising the manuscript. MR was responsible for implementation of the study and critically revising the manuscript. MH was responsible for implementation of the study, data interpretation, and critically revising the manuscript. KO was responsible for study design, implementation of the study, data interpretation, and critically revising the manuscript. JF was responsible for study design, implementation of the study, data collection, statistical analysis, data interpretation, and drafting the manuscript. All authors contributed to the article and approved the submitted version.
DHP has received honoraria for lectures and/or consultations from Janssen. KK has received honoraria for consultations and/or lectures from Eli Lilly, Janssen, Lundbeck, Neuraxpharm, Otsuka, Pfizer, Servier, Schwabe, Takeda, and Trommsdorff/Ferrer, Alexion, and CannaXan (advisory board). MH has received honoraria for lectures and/or consultations from Acceleron, Actelion, Bayer, GSK, Janssen, MSD and Pfizer, all outside the present study. KO has received honoraria for lectures and/or consultations from Acceleron, Actelion, Bayer, GSK, Janssen, MSD, United Therapeutics and Pfizer, all outside the present study.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We wish to thank all patients who participated in this project as well as Stefanie Konwert for her profound knowledge on the German healthcare sector and the discussion about social and medical inequalities.
6MWD, 6-minute walk distance; DLCO, diffusing capacity of the lung for carbon monoxide; DSM-V, Diagnostic and Statistical Manual of Mental Disorders V; FC, World Health Organization Functional Class; HADS, Hospital Anxiety and Depression Scale; NT-proBNP, N-terminal fragment of probrain natriuretic peptide; PAH, pulmonary arterial hypertension; QoL, quality of life; SCID, structed clinical interview for DSM-V, Structured Clinical Interview; SD, standard deviation.
1. Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J. (2015) 46:903–75. doi: 10.1183/13993003.01032-2015
2. Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med. (2016) 4:306–22. doi: 10.1016/S2213-2600(15)00543-3
3. Shafazand S, Goldstein MK, Doyle RL, Hlatky MA, Gould MK. Health-related quality of life in patients with pulmonary arterial hypertension. Chest. (2004) 126:1452–9. doi: 10.1378/chest.126.5.1452
4. Sommer N, Ghofrani HA, Pak O, Bonnet S, Provencher S, Sitbon O, et al. Current and future treatments of pulmonary arterial hypertension. Br J Pharmacol. (2021) 178:6–30. doi: 10.1111/bph.15016
5. Armstrong I, Billings C, Kiely DG, Yorke J, Harries C, Clayton S, et al. The patient experience of pulmonary hypertension: a large cross-sectional study of UK patients. BMC Pulm Med. (2019) 19:67. doi: 10.1186/s12890-019-0827-5
6. Guillevin L, Armstrong I, Aldrighetti R, Howard LS, Ryftenius H, Fischer A, et al. Understanding the impact of pulmonary arterial hypertension on patients' and carers' lives. Eur Respir Rev. (2013) 22:535–42. doi: 10.1183/09059180.00005713
7. Zhai Z, Zhou X, Zhang S, Xie W, Wan J, Kuang T, et al. The impact and financial burden of pulmonary arterial hypertension on patients and caregivers: results from a national survey. Medicine (Baltimore). (2017) 96:e6783. doi: 10.1097/MD.0000000000006783
8. Talwar A, Garcia JGN, Tsai H, Moreno M, Lahm T, Zamanian RT, et al. Health disparities in patients with pulmonary arterial hypertension: a blueprint for action. An official American thoracic society statement. Am J Respir Crit Care Med. (2017) 196:e32–47. doi: 10.1164/rccm.201709-1821ST
9. Von Visger TT, Kuntz KK, Phillips GS, Yildiz VO, Sood N. Quality of life and psychological symptoms in patients with pulmonary hypertension. Heart Lung. (2018) 47:115–21. doi: 10.1016/j.hrtlng.2017.12.004
10. Larisch A, Neeb C, de Zwaan M, Pabst C, Tiede H, Ghofrani A, et al. [Mental distress and wish for psychosomatic treatment of patients with pulmonary hypertension]. Psychother Psychosom Med Psychol. (2014) 64:384–9. doi: 10.1055/s-0034-1377013
11. Lowe B, Grafe K, Ufer C, Kroenke K, Grunig E, Herzog W, et al. Anxiety and depression in patients with pulmonary hypertension. Psychosom Med. (2004) 66:831–6. doi: 10.1097/01.psy.0000145593.37594.39
12. Bussotti M, Sommaruga M. Anxiety and depression in patients with pulmonary hypertension: impact and management challenges. Vasc Health Risk Manag. (2018) 14:349–60. doi: 10.2147/VHRM.S147173
13. Olsson KM, Meltendorf T, Fuge J, Kamp JC, Park D-H, Richter MJ, et al. Prevalence of mental disorders and impact on quality of life in patients with pulmonary arterial hypertension. Front Psychiatry. (2021) 12:667602. doi: 10.3389/fpsyt.2021.667602
14. Celedon JC, Burchard EG, Schraufnagel D, Castillo-Salgado C, Schenker M, Balmes J, et al. An American thoracic society/National heart, lung, and blood institute workshop report: addressing respiratory health equality in the United States. Ann Am Thorac Soc. (2017) 14:814–26. doi: 10.1513/AnnalsATS.201702-167WS
15. Khariton Y, Nassif ME, Thomas L, Fonarow GC, Mi X, DeVore AD, et al. Health status disparities by sex, race/ethnicity, and socioeconomic status in outpatients with heart failure. JACC Heart Fail. (2018) 6:465–73. doi: 10.1016/j.jchf.2018.02.002
16. Bowen DJ, Alfano CM, McGregor BA, Kuniyuki A, Bernstein L, Meeske K, et al. Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res Treat. (2007) 106:85–95. doi: 10.1007/s10549-006-9479-2
17. Tammemagi MC, Katki HA, Hocking WG, Church TR, Caporaso N, Kvale PA, et al. Selection criteria for lung-cancer screening. N Engl J Med. (2013) 368:728–36. doi: 10.1056/NEJMoa1211776
18. Shankman SA, Funkhouser CJ, Klein DN, Davila J, Lerner D, Hee D. Reliability and validity of severity dimensions of psychopathology assessed using the Structured Clinical Interview for DSM-5 (SCID). Int J Methods Psychiatr Res. (2018) 27:e1590. doi: 10.1002/mpr.1590
19. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
20. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. J Psychosom Res. (2002) 52:69–77. doi: 10.1016/S0022-3999(01)00296-3
21. Lowe B. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians? Diagnoses. J Affect Disord. (2004) 78:131–40. doi: 10.1016/S0165-0327(02)00237-9
22. Harper A, Power M. Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. (1998) 28:551–8. doi: 10.1017/S0033291798006667
23. Beckmann K, Glemser A, Heckel C, von der Heyde C, Hoffmeyer-Zlotnik JHP, Hanefeld U, et al. Demographische Standards. Wiesbaden: Statistisches Bundesamt (2016).
24. Sporinova B, Manns B, Tonelli M, Hemmelgarn B, MacMaster F, Mitchell N, et al. Association of mental health disorders with health care utilization and costs among adults with chronic disease. JAMA Netw Open. (2019) 2:e199910. doi: 10.1001/jamanetworkopen.2019.9910
25. Egede LE, Bishu KG, Walker RJ, Dismuke CE. Impact of diagnosed depression on healthcare costs in adults with and without diabetes: United States, 2004-2011. J Affect Disord. (2016) 195:119–26. doi: 10.1016/j.jad.2016.02.011
26. Kayser MZ, Valtin C, Greer M, Karow B, Fuge J, Gottlieb J. Video consultation during the COVID-19 pandemic: a single center's experience with lung transplant recipients. Telemed J E Health. (2020) 27:807–15. doi: 10.1089/tmj.2020.0170
27. Park DH, Fuge J, Meltendorf T, Kahl KG, Richter MJ, Gall H, et al. Impact of SARS-CoV-2-pandemic on mental disorders and quality of life in patients with pulmonary arterial hypertension. Front Psychiatry. (2021) 12:668647. doi: 10.3389/fpsyt.2021.668647
28. Yogeswaran A, Gall H, Tello K, Grunig E, Xanthouli P, Ewert R, et al. Impact of SARS-CoV-2 pandemic on pulmonary hypertension out-patient clinics in Germany: a multi-centre study. Pulm Circ. (2020) 10:2045894020941682. doi: 10.1177/2045894020941682
29. Stiebel V, Schwartz C. Physicians at the medicine/psychiatric interface: what do internist/psychiatrists do? Psychosomatics. (2001) 42:377–81. doi: 10.1176/appi.psy.42.5.377
30. Winter L, Naumann F, Olsson K, Fuge J, Hoeper MM, Kahl KG. Metacognitive therapy for adjustment disorder in a patient with newly diagnosed pulmonary arterial hypertension: a case report. Front Psychol. (2020) 11:143. doi: 10.3389/fpsyg.2020.00143
Keywords: pulmonary arterial hypertension, mental health, quality of life, health disparities, health-care-utilization
Citation: Park DH, Meltendorf T, Kahl KG, Kamp JC, Richter MJ, Hoeper MM, Olsson KM and Fuge J (2022) Health Disparities and Differences in Health-Care-Utilization in Patients With Pulmonary Arterial Hypertension. Front. Psychiatry 13:813506. doi: 10.3389/fpsyt.2022.813506
Received: 11 November 2021; Accepted: 13 January 2022;
Published: 22 February 2022.
Edited by:
Domenico De Berardis, Azienda Usl Teramo, ItalyReviewed by:
Mariusz Stanisław Wiglusz, Medical University of Gdansk, PolandCopyright © 2022 Park, Meltendorf, Kahl, Kamp, Richter, Hoeper, Olsson and Fuge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Da-Hee Park, cGFyay5kYS1oZWVAbWgtaGFubm92ZXIuZGU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.