
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 01 April 2022
Sec. Child and Adolescent Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.796384
This article is part of the Research Topic Paternal Health and Offspring Psychological Development: From Preconception to Adolescence View all 4 articles
Evaluating the resolution of parents of ill children can help in taking measures to alleviate their distress in a timely manner and promote children's rehabilitation. This study aims to develop and validate a nomogram for predicting the unresolved risk of parents of adolescents with psychiatric diagnoses. The data for 130 parents (modeling dataset = 90; validation dataset = 40) were collected. A nomogram was first developed to predict the unresolved risk for parents based on the logistic regression analysis in the modeling dataset. The internal and external validation then were conducted through quantifying the performance of the nomogram with respect to discrimination and calibration, respectively, in the modeling and validation datasets. Finally, the clinical use was evaluated through decision curve analyses (DCA) in the overall dataset. In the results, the nomogram consisted of six risk factors and provided a good discrimination with areas under the curve of 0.920 (95% CI, 0.862–0.978) in internal validation and 0.886 (95% CI, 0.786–0.986) in external validation. The calibration with good consistency between the observed probability and predicted probability was also found in both internal and external validation. DCA showed that the nomogram had a good clinical utility. In conclusion, the proposed nomogram exhibited a favorable performance with regard to its predictive accuracy, discrimination capability, and clinical utility, and, thus, can be used as a convenient and reliable tool for predicting the unresolved risk of parents of children with psychiatric diagnoses.
The arrival of a new child into the family is usually received with immense elation, and parents generally have optimistic expectations of what their child will become and how they will be as parents (1, 2). Parents usually invest a large amount of energy and time in childrearing, while also enjoying their parenting role. When facing with children's diagnoses of an illness or a disability, parents can suffer from disappointment and distress because of failing to achieve their hopes of a healthy offspring or a “perfect child” (3). Moreover, the process of accepting or adjusting a disease diagnosis is most challenging for parents because changing previous expectations to more realistic ones can be as painful as losing a loved one (4–6).
Coming to fully accept a child's diagnosis requires parents to cognitively and emotionally process the experience of children with an illness or a disability. Cognitively, parents need to understand the implications of their child's diagnosis for themselves and their child. Emotionally, they need to acknowledge the feelings associated with the child's diagnosis and comprehend the meaning of parenting a child with a medical condition (7, 8). Parents who accepted their children's diagnoses were found to be more likely to build secure attachment with children, be more sensitive to children's cues, and better adjust their reactions to children, even when children's responses were inappropriate (9, 10). Studies have shown that parents' reactions to children's diagnoses were the premise of providing support for children, which had a major influence on the disease progress, treatment, and rehabilitation (11). Thus, professionals should be aware of the significance of assessing parents' reactions and identifying the challenges faced by parents in the process of adaptation (7, 12, 13).
An important progress in assessing parents' reactions to children's diagnoses has been made by Marvin and Pianta (10) with the introduction of the model of the resolution of the diagnosis based on the attachment theory. Resolution represents a process that parents change their working models of the anticipated perfect child into conceptions that are more aligned with the reality of child with specific abilities and limitations (14). Then a standardized, reliable procedure named the Reaction to Diagnosis Interview (RDI) was developed to identify individual differences in the process of the parents' resolution (8, 10, 15). The resolution status of parents was classified as two main classifications: “resolved” or “unresolved” according to RDI. Resolved parents can quickly cease active grieving and reorient current realities and future possibilities, which is characterized by acknowledging feelings associated with diagnoses, controlling their emotional responses, and moving on in life. On the contrary, unresolved parents display an absence of these characteristics. They are described as emotionally “stuck in the past” and tend to preoccupy themselves with negative aspects of their children's condition (10).
In recent years, studies have investigated the resolution of parents of children with various medical conditions, including autism spectrum disorder (13, 16), epilepsy (10), developmental delay (17), cerebral palsy (2, 10, 18), diabetes (19), preterm birth (20), and phenylketonuria (12). These literatures showed that the rates of “resolved” were diverse with a range between 33% (13) and 82% (2), supporting the view that the resolution was related to the illness itself. Except for the type of illness, some other demographic variables were also found to be associated with parents' resolution. An earlier study has shown that parents' stress and burden became greater as children's age progresses, making it more difficult for parents to resolve the children's diagnoses (17). The same was true as the parents got older. Some studies have revealed that fathers were more likely to resolve children's diagnoses than mothers, yet these differences did not reach significance (12, 21). Parents with lower education levels reported a heavier burden and higher unresolved status. Besides, family function and social support were also related to the parents' resolution (22, 23).
At present, parents' resolution to their children's psychiatric diagnosis did not receive a great deal of attention. Adolescence is the vital period for most people to pursue their education, seek for suitable job, and establish friendships and romantic relationships. Psychiatric disorder, often beginning at adolescence, cannot only potentially limit the achievement of these objects but also lead to high rates of disability, mortality, and suicide (24, 25). Hence, like parents of children with other medical conditions, parents of adolescents with psychiatric disorders may also experience strong emotional distress and have difficulties in resolving their children's diagnoses (26). Besides, obvious behavior problems, stigma, and stereotypes of psychiatric disorders may also prevent parents from resolving their children's diagnoses (11, 27). Therefore, identifying the high-risk unresolved parents and developing targeted interventions for them should become an integral part of the clinical care of adolescents with psychiatric diagnoses.
Nomogram is a statistics-based tool that can quickly predict the probability of a specific event through approximate complicated calculation without a computer or calculator (28, 29). As a simple and convenient mathematical model, nomograms have recently attracted increasing attention for their substantial clinical utility. This study aims to establish and validate a nomogram for predicting the unresolved risk of parents of adolescents with psychiatric diagnoses in an intuitive, visual, and convenient way.
It was a cross-sectional study incorporating both interview and questionnaire with a sample of parents of adolescents with psychiatric diagnoses.
A convenience sample was employed to recruit participants from a mental health center between November 2019 and February 2021 in China. The inclusion criteria for parents were (a) having a child (10–18 years old) meeting the diagnostic criteria (DSM-IV) for psychiatric disorder, (b) spending more time with their child than other family members, and (c) willing to be interviewed and share their experiences of caring for their child. Parents with a mental illness or lack of cognitive capacity were excluded. The total sample comprised 130 parents of adolescents with psychiatric diagnoses, and these parents were randomly divided into modeling dataset (90 cases) and validation dataset (40 cases) with a split ratio of 7:3 (30, 31).
Ethical approval was obtained from the Institutional Review Board of Wuhan University School of Medicine prior to the study. Research assistants spoke with parents who met the criteria about the goals, significance, and methods of the study, and asked if they and their child would like to participate. Upon parents' consent to participate, appointments were made for interviews in an unoccupied ward. All interviews were audio-recorded by a minirecording device. Notes were made on behavioral characteristics (i.e., body language and facial expression) during the interview in order that the parents' perspectives were correctly stated and comprehended. Appropriate pauses or changes in topic were applied whenever participants seemed to feel uncomfortable and upset during the interview. After completing of the RDI, parents were asked to independently complete the self-report questionnaire including the sociodemographic characteristics, the Family Adaptability and Cohesion Evaluation Scales (FACESII), the Parenting Stress Index—Short Form (PSI-SF), and the Social Support Rating Scale (SSRS). The researchers remained quiet when the patients filled out the questionnaire. All data were anonymous and only accessible to the researchers.
Reaction to Diagnosis Interview (RDI) is used to assess the resolution status of parents of children with medical conditions (15, 32). It is a standardized, videotaped, and structured interview consisting of five questions. The interview may last from a few minutes to approximately 15 min. In the interview, parents were asked (1) to recall the period of time they began noticing that their children had a medical problem; (2) how they felt at that time and if there were changes to those feelings; (3) to describe the events and experiences surrounding the time they received the diagnosis; (4) how their feelings changed since the time of the diagnosis; (5) to detail whether they have been searching for other reasons for their experiences. Each interview was videotaped, transcribed, and classified as “resolved” or “unresolved” (8). Reliability and validity of the RDI have been confirmed, with inter-rater agreement ranging from 88 to 96% (3, 15). The coding was completed by two trained coders, and each trained coder rated all interviews and was blinded to each other's ratings. Researchers had an intercoder agreement of 90% on the “resolved” or “unresolved” classification in the study.
The questionnaire was designed based on the purpose of this study. It provided data on sociodemographic variables of the parents including age, gender, marital status, education level, and status of employment, as well as data of the children including age, gender, one child, and time since diagnosis.
The family functioning is evaluated by the Family Adaptability and Cohesion Evaluation Scales (FACESII). The 30-item self-report scale consists of two subscales, namely, coherence (16 items) and adaptability (14 items). All items are scored based on a five-point Likert scale (ranging from 1 = almost never to 5 = almost always). A higher score indicates better family functioning. The validity and reliability of the FACESII of the Chinese version have been well established (33), and its internal consistency was acceptable (Cronbach's α = 0.73–0.85), and the test–retest reliability was also satisfactory (r = 0.84–0.91).
The Parenting Stress Index—Short Form (PSI-SF) (34) is a 36-item self-report scale designed to identify the experiencing stress of the parent–child system and the sources of that stress. The scale is organized into three subscales consisting of 12 items each: parental distress (PD), parent–child dysfunctional interaction (PCDI), and difficult child (DC) (34). All items are scored based on a five-point Likert scale (ranging from 1 = strongly agree to 5 = strongly disagree). A higher score indicates higher parenting stress. The PSI-SF has been translated into Chinese and previously used in the Chinese population, and has been tested to have good reliability and validity (35–37).
Originally developed in Chinese by Xiao, the Social Support Rating Scale (SSRS) is a self-rated scale used to measure social support, with a good test–retest reliability of 0.92 (38). It has already been widely used in different Chinese communities and showed good validity and reliability (39–41). The 10-item scale contains three dimensions including objective support, subjective support, and support usage to evaluate social support. A higher score indicates higher social support.
The decision analysis curves (DCA) was introduced by Vickers and Elkin to estimate clinical utility of prediction models based on the threshold probability (probability that triggers a medical intervention, equating to the probability at which the harm of a false-positive intervention exceeds the harm of a false-negative non-intervention) (42). The threshold probability is used to derive the net benefit (defined as the fraction of true positives subtracted by the fraction of false positives weighted by the relative harm of a false-positive and false-negative result) (43). Graphical analysis of the net benefit and the threshold probability yields a decision analysis curve, which can then be used to assess the net benefit of nomogram-assisted decisions at different threshold probabilities, compared with the net benefit of decisions made with the assumption that either all or no patient has the outcome of interest (42–44).
All statistical analyses were conducted using R Environment for Statistical Computing (version 4.0.2, http://www.r-project.org/). Univariable and multivariable logistic regression analysis was performed to identify independent risk factors for the unresolved parents of adolescents with psychiatric diagnoses. All tests were two sided, and values of p < 0.05 were considered statistically significant. Then a nomogram was created using the “rms” package based on the independent risk factors of logistic regression analysis. The performance of the nomogram was evaluated through measuring discrimination and calibration in both the modeling and validation datasets. Discrimination was evaluated by using a receiver operating characteristic (ROC) curve and the area under the curve (AUC). The calibration was assessed by observing the goodness of fit between the observed probability and the predicted probability in the calibration plot. Finally, the decision curve analysis (DCA) was performed to evaluate the clinical utility of the nomogram based on net benefits at different threshold probabilities in the overall dataset (modeling and validation datasets).
A total of 150 parents of adolescents with mental illness were invited to participate in our study; 20 parents rejected to participate for the main reasons that they “do not want” and “have no time.” In the end, the study included 130 eligible parents, including 90 parents in the modeling dataset and 30 parents in the validation dataset. The characteristics of parents and adolescents in the modeling dataset, validation dataset, and overall dataset are shown in Table 1.
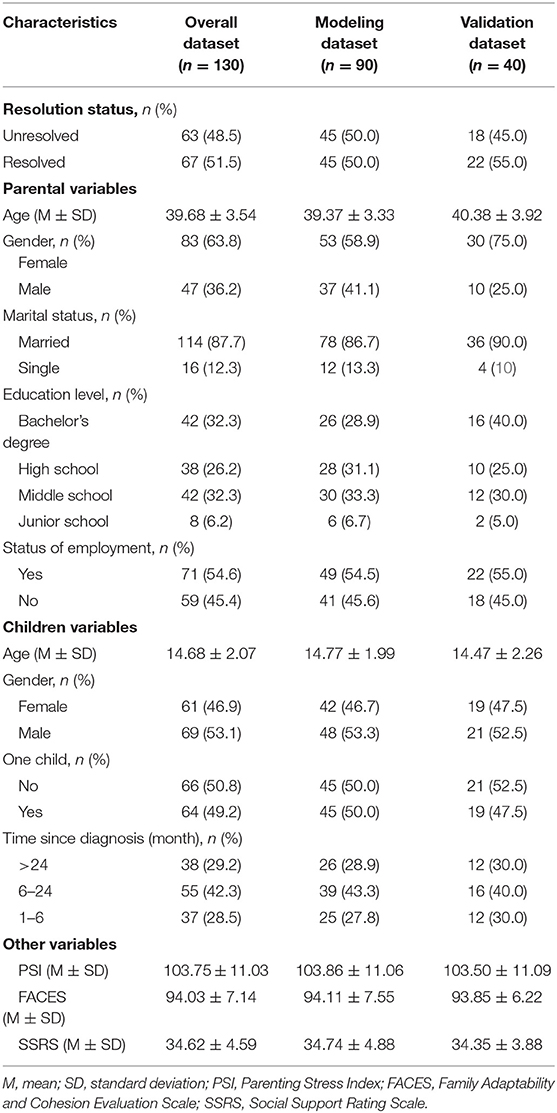
Table 1. Characteristics of parents and adolescents in the modeling, validation, and overall datasets.
In the modeling dataset, the univariable and multivariable analysis showed that parents' gender, status of employment, adolescents' age, one child, time since diagnosis, and social support were the independent risk factors related to the unresolved risk of parents of adolescents with psychiatric diagnoses (see Table 2).
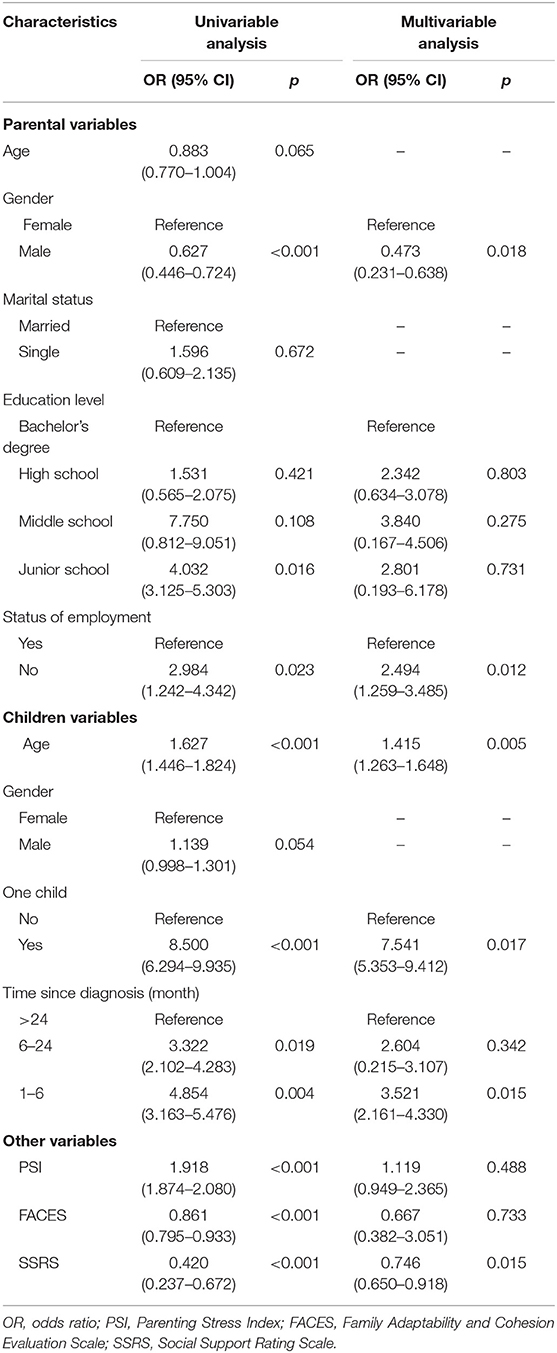
Table 2. Risk factors for unresolved status by univariable and multivariable logistic regression analysis in the modeling dataset.
Based on the significant variables in the logistic regression analysis, a nomogram for predicting the unresolved risk of parents of adolescents with the psychiatric diagnoses was developed in the modeling dataset (see Figure 1). The internal validation was conducted in the modeling dataset to assess the performance of the nomogram including calibration and discrimination. The calibration plot of the nomogram showed a good consistency between the predicted probability and observed probability (see Figure 2). The receiver operating characteristic (ROC) and the area under the curve (AUC) was 0.920, indicating favorable discrimination (see Figure 3).
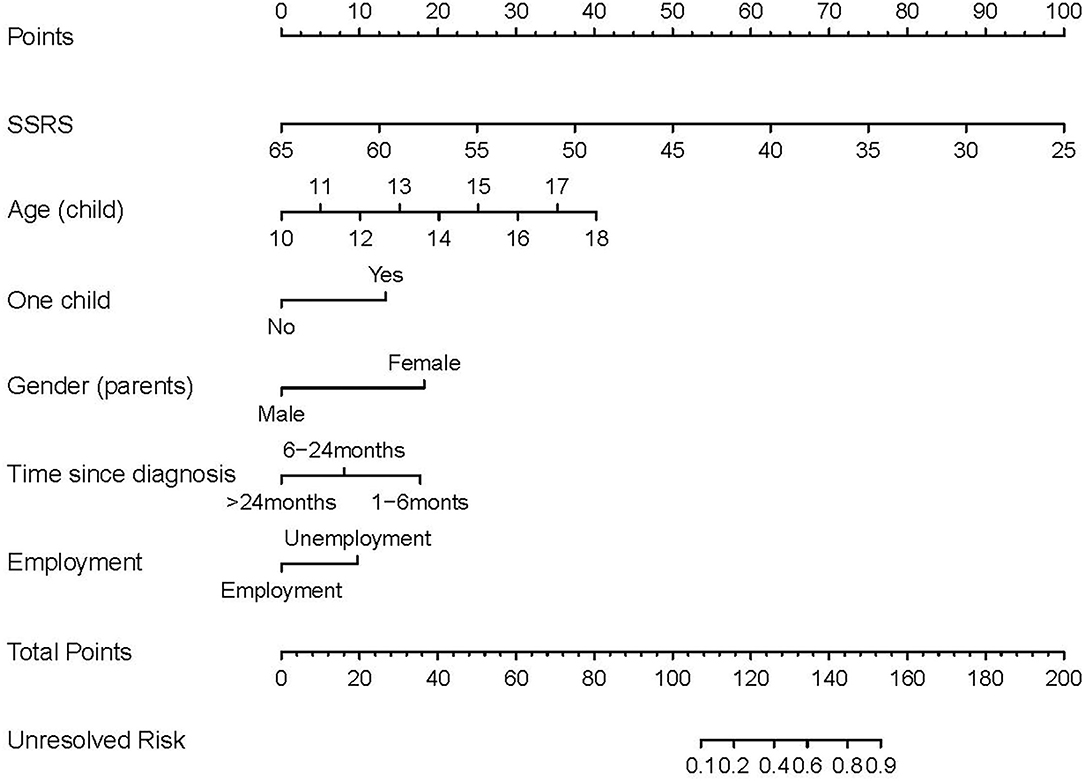
Figure 1. Nomogram for predicting the unresolved risk of parents of children with psychiatric diagnoses. Each risk factor of the parents has a value on its variable axis, and vertical lines are drawn upward to the point axis to obtain the corresponding scores for the value of each risk factor. A total score can be easily calculated by adding each single score. The total score is plotted on the bottom total point axis, and a vertical line is drawn downward to the unresolved risk axis to estimate the unresolved risk.
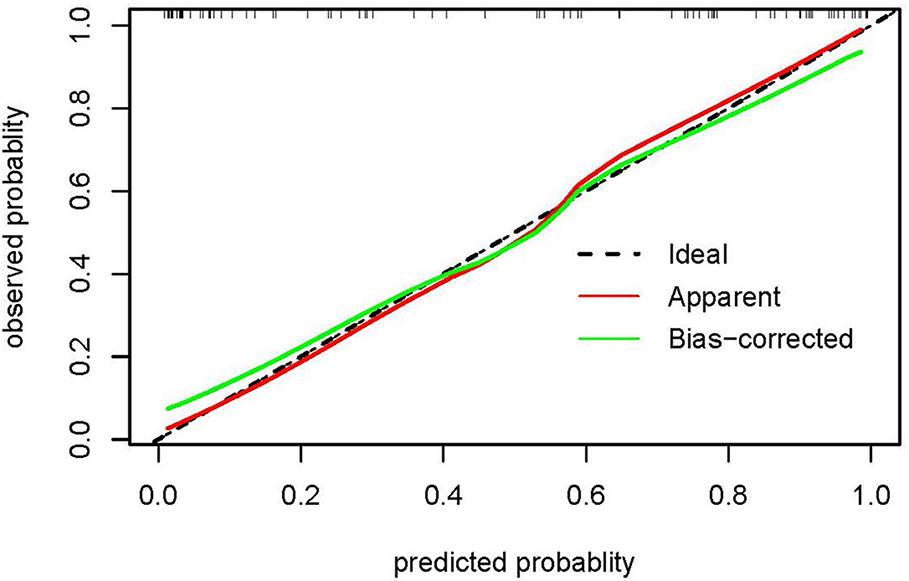
Figure 2. The calibration plot of the nomogram in the modeling dataset. The x-axis shows the nomogram-predicted probability of unresolved risk, and the y-axis shows the actual observed probability of unresolved risk. The ideal line (45°) in the calibration plots represents perfect consistency between the nomogram-predicted probabilities and the observed probabilities. The apparent line represents the model calibrated with the modeling dataset, and the bias-corrected line represents the model calibrated using the bootstrap method.
The validation of the nomogram was performed in the validation dataset to further evaluate the performance of the proposed nomogram. The calibration plot for the nomogram showed a good consistency between the predicted probability and observed probability (see Figure 4). The receiver operating characteristic (ROC) and the area under the curve (AUC) was 0.886, indicating good discrimination (see Figure 5).
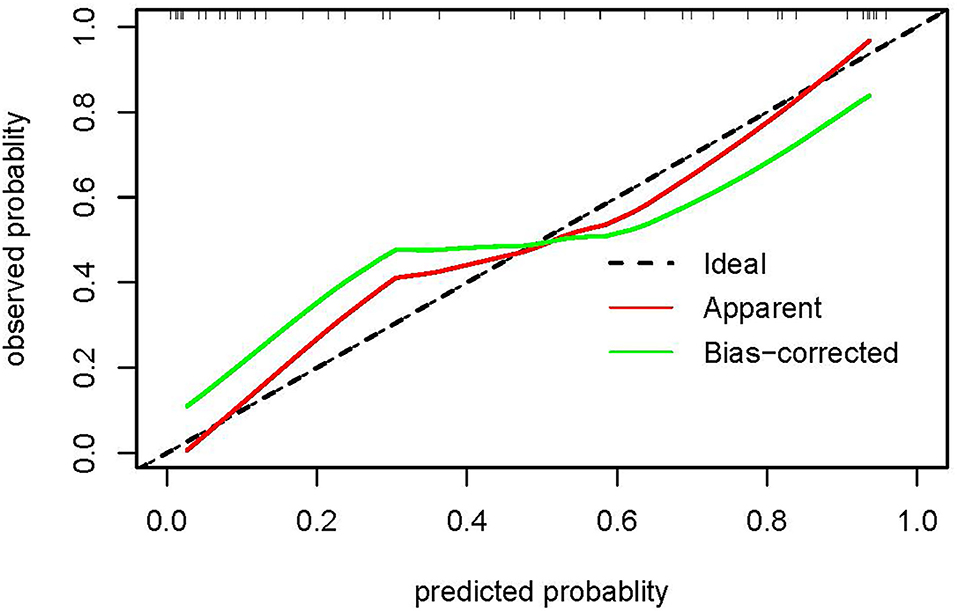
Figure 4. The calibration plot of the nomogram in the validation dataset. The x-axis shows the nomogram-predicted probability of unresolved risk, and the y-axis shows the actual observed probability of unresolved risk. The ideal line (45°) in the calibration plots represents perfect consistency between the nomogram-predicted probabilities and the observed probabilities. The apparent curve represents the model calibrated with the validation dataset, and the bias-corrected curve represents the model calibrated using the bootstrap method.
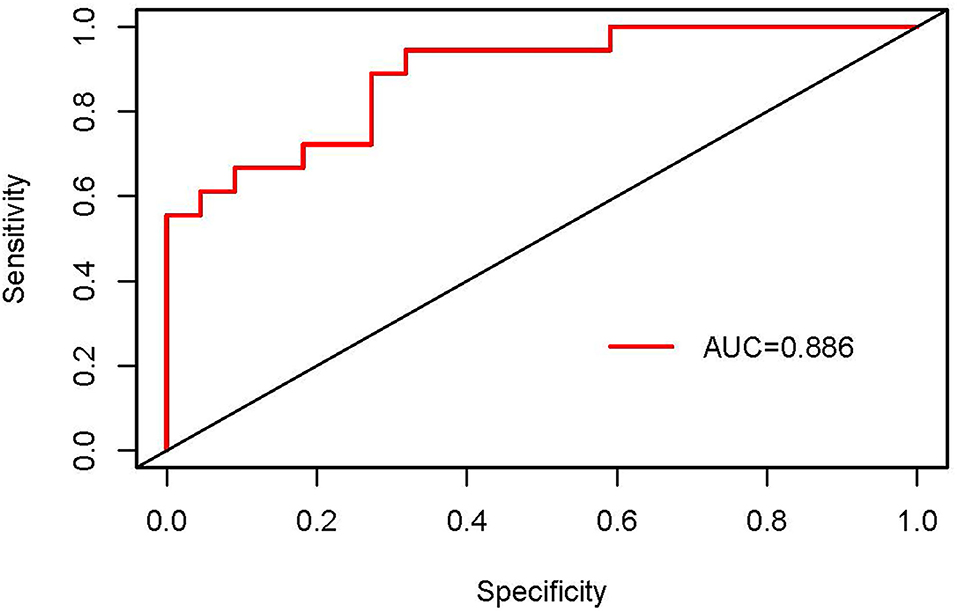
Figure 5. The receiver operating characteristic (ROC) curves of the nomogram in the validation dataset.
The decision curve analyses (DCA) was used to evaluate the clinical utility of the nomogram in all 130 parents. As shown in Figure 6, the nomogram provided greater benefits than the treat-all-parents scheme and treat-none scheme when the threshold probability was >13% and <54%. Therefore, the nomogram had a good clinical utility.
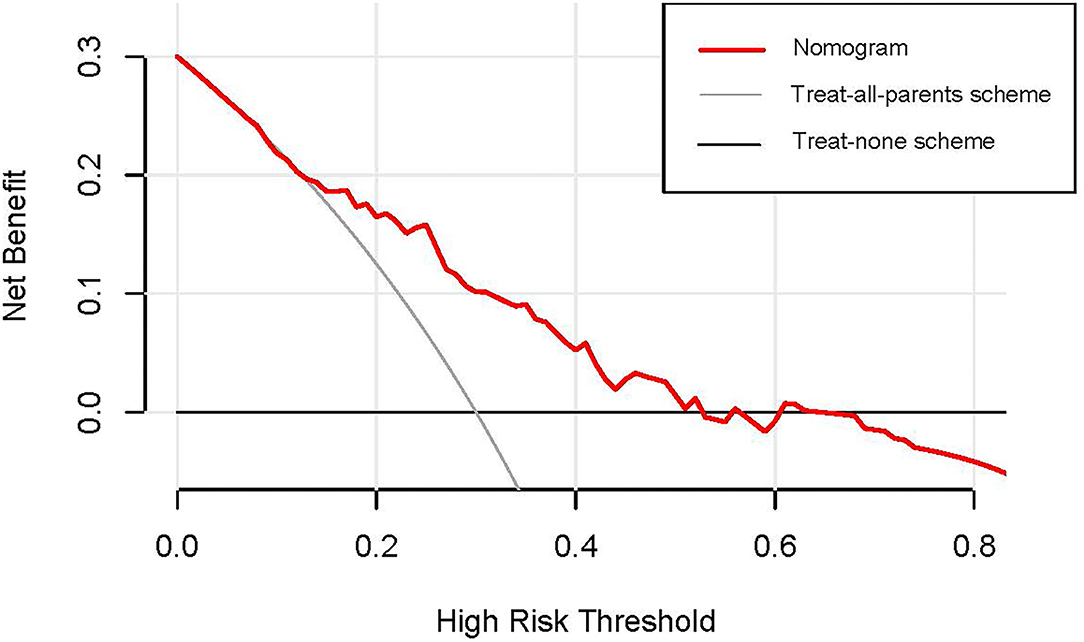
Figure 6. The decision curve analysis of the nomogram in the entire dataset. The y-axis measures the net benefit, and the x-axis measures the probability threshold. The red line represents the nomogram. The black line (treat-none scheme line) represents the assumption that all parents are unresolved statuses. The gray line (treat-all-parents scheme line) represents the assumption that no parent is unresolved status. The decision curve analysis (DCA) indicated that the nomogram provided more benefits than the treat-all-parents scheme and treat-none scheme when the threshold probability of unresolved status was >13% and <54%.
In the current study, the percentage of unresolved parents (50%) in the modeling dataset was higher than the mean percentage (40%) found in a previous study (45), which indicated that parents of adolescents with psychiatric diagnoses had higher rates of unresolved status. Therefore, evaluating the unresolved risk of parents in the process of resolution and making targeted interventions are vital in clinical care. In the current study, a nomogram was developed to predict the unresolved risk of parents of adolescents with psychiatric diagnoses based on the logistic regression analysis. It showed favorable discrimination, calibration, and clinical utility through internal and external validation. The proposed nomogram can be used as a tool to help professionals identify high-risk unresolved parents and take targeted interventions to promote parents' resolution of diagnoses.
Improving the accuracy of a model needs comprehensive and reasonable evaluation of all possible related variables, which is complicated and tedious work (46). In addition, it is hard to keep a balance between comprehensiveness and comprehensibility when creating the nomogram (46). Given the busy and complex clinical work, we, thus, only collected variables with clinical importance and easy accessibility to develop an easy-to-use prediction model. Based on the logistic regression analysis, we finally identified six independent risk factors including parents' gender, employment status, children's ages, one child, time since diagnosis, and social support, and developed the nomogram.
Consistent with previous studies (12, 17, 21), it was found that the mother had a higher unresolved risk than the father in our study. The gender roles theory indicates that women prefer to cope with the problem with personal emotion, and men are more stoic and logically driven. Therefore, mothers had more intense negative feelings than fathers in the interview and, thus, were more likely to be classified as an unresolved status. Employment status induced a positive effect for parents to resolve the children's psychiatric diagnoses in the study. It enabled parents to obtain stable financial resources and better medical resources, which can reduce parents' stress and promote the resolution of diagnoses (3). Parents of adolescents with shorter time since diagnosis had higher unsolved risk. It can be explained by Blacher's phase theory (47) describing that parents' reactions to their children's diagnoses gradually progress and finally achieve adaptation. As the only child in the family, the one child usually receives more attention from parents (48). Therefore, parents are more likely to immerse in distress and have difficulties in resolving the diagnosis. Moreover, caring for children with mental illness can be a challenging experience because of the special nature of the psychiatric disorder, such as obvious behavior problem, unclear prognosis, and lack of a radical cure. Formal and informal support can help parents to alleviate distress and stress, and, thus, are beneficial to the process of resolution (49). As for the children' ages, older children had more pronounced differences in abilities of independent living and communication than typical developing children, and thus, parents had more difficulties in resolving the diagnoses.
Validating the nomogram is essential to ensure that it can be applied generally and avoid overfitting. In the internal validation, the nomogram provided favorable discrimination with an AUC of 0.920 and a good calibration with goodness of fit between the predicted probability and observed probability. Research has indicated that the performance of a nomogram, such as discrimination and calibration, can vary when applied to different datasets (43). As a result, the external validation, validating in a dataset with similar characteristics to the population to which the nomogram will be applied, is generally regarded as the gold standard. In the current study, the external validation showed reasonable discrimination based on an AUC of 0.886 and a favorable calibration based on acceptable goodness of fit between the predicted probability and observed probability in the calibration plot. Although the performance of the nomogram in the validation dataset was slightly worse than those in the modeling dataset, the degraded performance metrics were still in the clinically acceptable range (43). Therefore, it was appropriate to recommend the nomogram for routine use in clinical practice.
However, even if the nomogram had a perfect performance, it was possible to lack clinical utility. The essential criterion to evaluate the utility of a model is whether the model benefits patients. When the threshold probability of the net benefit is impractical, the model with good performance may also have limited utility (46, 50). The decision analysis curve (DCA) was used to estimate the clinical utility of the nomogram based on the net benefit and the threshold probability in the present study. The results indicated that when the threshold probability of unresolved risk was 13%−54%, intervention for parents added more benefit compared with the treat-all-parents scheme or the treat-none scheme. Therefore, the nomogram can assist in decision making and have good clinical utility (51).
Kearney (26) designed the logistic prediction model for assessing the resolution of parents of young children with psychiatric disorders based on the data of 33 parents, but the model showed worse prediction ability for unresolved parents, indicating a need for further model development. Compared with the abovementioned logistic prediction model, the proposed nomogram in the current study showed some strengths. At first, the study expanded the resolution of the diagnosis to the adolescent psychiatric population and first established the nomogram for predicting the unresolved risk of parents of adolescents with psychiatric diagnoses in the context of the Chinese culture. Second, the nomogram had good calibration, discrimination, and clinical utility through internal and external validation. Third, the majority of variables identified by the nomogram were easily obtained and can reflect the clinically relevant information, which helped the medical staff to quickly identify the parents at high unresolved risk. Finally, this nomogram had a good cultural representation because it was created based on the Chinese population.
The limitations of this study should be acknowledged. First, selection bias was an issue in the study because there was no systematic sampling method, i.e., anyone who met the inclusion criteria was invited to participate. Second, the small size of the sample impacted the power of the analysis and the effect size, which was directly linked with the predictive ability of the model in logistic regression. Finally, participants were from a single institution, and the generalization of the nomogram to the other cities in China, or even the global population, was still unclear. Therefore, it is necessary for future studies to further explore the risk factors related to the unresolved status of parents and develop a model with universal applicability in the future. Regardless of the limitation of the nomogram, the study offered new perspective and research foundation for evaluating the parents' reactions to psychiatric diagnosis of their children.
To our knowledge, we developed the first nomogram for predicting the unresolved risk of parents of adolescents with psychiatric diagnoses based on the routine medical information of parents and their adolescents. The proposed nomogram showed a favorable performance in predictive accuracy, discrimination, capability, and clinical utility. As a result, the nomogram can be considered as a prediction tool to guide medical staff to identify the high-risk unresolved parents and take personalized measures to assist them to resolve the diagnosis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Institutional Review Board of the Researchers' Institution granted approval for this study. Written informed consent was obtained from all participants.
QS, CC, and PL designed the study and wrote the research protocol. QS, CC, XZ, XW, and PL performed the literature, quality control, and collected and checked the data. QS, LC, YG, and PL analyzed the data, interpretation of data, and contributed to the in-depth revision of the manuscript. QS, PL, LC, YG, and XW prepared the manuscript. All authors contributed to and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank all the parents who participated in this study and the medical staff for helping us implement the study in the Mental Health Center.
1. Leerkes EM, Burney RV. The development of parenting efficacy among new mothers and fathers. Infancy. (2007) 12:45–67. doi: 10.1111/j.1532-7078.2007.tb00233.x
2. Schuengel C, Rentinck IC, Stolk J, Voorman JM, Loots GM, Ketelaar M, et al. Parents' reactions to the diagnosis of cerebral palsy: associations between resolution, age and severity of disability. Child Care Health Dev. (2009) 35:673–80. doi: 10.1111/j.1365-2214.2009.00951.x
3. Barnett D, Clements M, Kaplan-Estrin M, McCaskill JW, Hunt KH, Butler CM, et al. Maternal resolution of child diagnosis: stability and relations with child attachment across the toddler to preschooler transition. J Fam Psychol. (2006) 20:100–7. doi: 10.1037/0893-3200.20.1.100
4. Bowlby J. A Secure Base: Parent-Child Attachment and Healthy Human Development. New York: Basic Books (1988).
5. Chen JY, Clark MJ. Family resources and parental health in families of children with Duchenne muscular dystrophy. J Nurs Res. (2010) 18:239–48. doi: 10.1097/JNR.0b013e3181fbe37b
6. Luther EH, Canham DL, Fau-Young Cureton V, Young Cureton V. Coping and social support for parents of children with autism. J School Nurs. (2005) 21:40–7. doi: 10.1177/10598405050210010901
7. Barnett D, Clements M, Kaplan-Estrin M, Fialka J. Building new dreams: Supporting parents' adaptation to their child with special needs. Infants Young Child. (2003) 16:184–200. doi: 10.1097/00001163-200307000-00002
8. Pianta RC, Marvin RS. Manual for Classification of the Reaction to Diagnosis Interview. Charlottesville: University of Virginia (1993).
9. Feniger-Schaal R, Oppenheim D. Resolution of the diagnosis and maternal sensitivity among mothers of children with Intellectual Disability. Res Dev Disabil. (2013) 34:306–13. doi: 10.1016/j.ridd.2012.08.007
10. Marvin RS, Pianta RC. Mothers' reactions to their child's diagnosis: relations with security of attachment. J Clin Child Psychol. (1996) 25:436–45. doi: 10.1207/s15374424jccp2504_8
11. Oruche UM, Gerkensmeyer J, Fau-Stephan L, Stephan L, Fau-Wheeler CA, Wheeler Ca Fau-Hanna KM, Hanna KM. The described experience of primary caregivers of children with mental health needs. Arch Psychiatric Nurs. (2012) 26:382–91. doi: 10.1016/j.apnu.2011.12.006
12. Lord B, Ungerer J, Wastell C. Implications of resolving the diagnosis of PKU for parents and children. J Pediatric Psychol. (2008) 33:855–66. doi: 10.1093/jpepsy/jsn020
13. Oppenheim D, Koren-Karie N, Dolev S, Yirmiya N. Maternal insightfulness and resolution of the diagnosis are associated with secure attachment in preschoolers with autism spectrum disorders. Child Dev. (2009) 80:519–27. doi: 10.1111/j.1467-8624.2009.01276.x
14. Krstic T, Mihic L, Mihic I. Stress and resolution in mothers of children with cerebral palsy. Res Dev Disabil. (2015) 47:135–43. doi: 10.1016/j.ridd.2015.09.009
15. Pianta RC, Marvin RS, Britner PA, Borowitz KC. Mother's resolution of their children's diagnosis: organized patterns of caregiving representations. Infant Mental Health Journal. (1996) 17:239–56. doi: 10.1002/(SICI)1097-0355(199623)17:3<239::AID-IMHJ4>3.0.CO;2-J
16. Dolev S, Sher-Censor E, Baransi N, Amara K, Said M. Resolution of the child's ASD diagnosis among Arab–Israeli mothers: associations with maternal sensitivity and wellbeing. Res Autism Spectr Disord. (2016) 21:73–83. doi: 10.1016/j.rasd.2015.09.004
17. Barak-Levy Y, Atzaba-Poria N. Paternal versus maternal coping styles with child diagnosis of developmental delay. Res Dev Disabil. (2013) 34:2040–6. doi: 10.1016/j.ridd.2013.02.026
18. Rentinck IC, Ketelaar M, Schuengel C, Stolk J, Lindeman E, Jongmans MJ, et al. Short-term changes in parents' resolution regarding their young child's diagnosis of cerebral palsy. Child Care Health Dev. (2010) 36:703–8. doi: 10.1111/j.1365-2214.2010.01077.x
19. Goldberg A, Wiseman H. Parental resolution and the adolescent's health and adjustment: The case of adolescents with type 1 diabetes. Social Work Health Care. (2016) 55:87–100. doi: 10.1080/00981389.2015.1073209
20. Shah PE, Clements M, Poehlmann J. Maternal resolution of grief after preterm birth: implications for infant attachment security. Pediatrics. (2011) 127:284–92. doi: 10.1542/peds.2010-1080
21. Milshtein S, Yirmiya N, Oppenheim D, Koren-Karie N, Levi S. Resolution of the diagnosis among parents of children with autism spectrum disorder: associations with child and parent characteristics. J Autism Dev Disord. (2010) 40:89–99. doi: 10.1007/s10803-009-0837-x
22. Baiocco R, Castelli GP, Cioccetti G, Ioverno S. Parents' Reactions to the diagnosis of Duchenne Muscular Dystrophy: associations between resolution, family functioning, and child behavior problems. J Nurs Res. (2017) 25:455–63. doi: 10.1097/JNR.0000000000000186
23. Rentinck I, Ketelaar M, Jongmans M, Lindeman E, Gorter JW. Parental reactions following the diagnosis of cerebral palsy in their young child. J Pediatr Psychol. (2009) 34:671–6. doi: 10.1093/jpepsy/jsn103
24. Brown J. Parents' experiences of their adolescent's mental health treatment: Helplessness or agency-based hope. Clin Child Psychol Psychiatry. (2018) 23:644–62. doi: 10.1177/1359104518778330
25. Crouch LA-O, Reardon T, Farrington A, Glover F, Creswell C. Just keep pushing“: Parents' experiences of accessing child and adolescent mental health services for child anxiety problems. Child Care Health Dev. (2019) 45:491–9. doi: 10.1111/cch.12672
26. Kearney JA, Britner PA, Farrell AF, Robinson JL. Mothers' resolution of their young children's psychiatric diagnoses: associations with child, parent, and relationship characteristics. Child Psychiatry Hum Dev. (2011) 42:334–48. doi: 10.1007/s10578-011-0217-6
27. Johansson A, Anderzén-Carlsson A, Ewertzon M. Parents of adult children with long-term mental disorder: Their experiences of the mental health professionals' approach and feelings of alienation—a cross sectional study. Arch Psychiatric Nurs. (2019) 33:129–37. doi: 10.1016/j.apnu.2019.10.002
28. Park SY. Nomogram: An analogue tool to deliver digital knowledge. J Thorac Cardiovasc Surg. (2018) 155:1793. doi: 10.1016/j.jtcvs.2017.12.107
29. Xie W, Liu J, Huang X, Wu G, Jeen F, Chen S, et al. A nomogram to predict vascular invasion before resection of colorectal cancer. Oncol Lett. (2019) 18:5785–92.
30. Huang X, Liu J, Wu G, Chen S, Pc FJ, Xie W, et al. Development and validation of a nomogram for preoperative prediction of perineural invasion in colorectal cancer. Med Sci Monitor. (2019) 25:1709–17. doi: 10.12659/MSM.914900
31. Liu J, Huang X, Chen S, Wu G, Xie W, Franco JPC, et al. Nomogram based on clinical characteristics for preoperative prediction of perineural invasion in gastric cancer. J Int Med Res. (2020) 48:300060519895131. doi: 10.1177/0300060519895131
32. Pianta RC, Marvin RS. Manual for Classification of the Reaction to Diagnosis Interview. Virginia: University of Virginia, Charlottesville (1992).
33. Fei L, Shen Q, Zheng Y. Preliminary evaluation of the family adaptability and cohesion evaluation scale and the family environment scale. Chin J Mental Health. (1991) 5:198–203.
34. Abidin RR. Parenting Stress Index, Third Edition: Professional Manual. Odessa, FL: Psychological Assessment Resources (1995).
35. Chan YC. Parenting stress and social support of mothers who physically abuse their children in Hong Kong. Child Abuse Neglect. (1994) 18:261–9. doi: 10.1016/0145-2134(94)90110-4
36. Pearson V, Chan TW. The relationship between parenting stress and social support in mothers of children with learning disabilities: a Chinese experience. Soc Sci Med. (1993) 37:267–74. doi: 10.1016/0277-9536(93)90461-C
37. Yeh CH, Chen ML, Li W. The Chinese version of the parenting stress index: a psychometric study. Acta Paediatr. (2001) 90:1470–7. doi: 10.1111/j.1651-2227.2001.tb01615.x
39. Cheng Y, Liu C, Mao C, Qian J, Liu K, Ke G. Social support plays a role in depression in Parkinson's disease: a cross-section study in a Chinese cohort. Parkinsonism Related Disorders. (2008) 14:43–5. doi: 10.1016/j.parkreldis.2007.05.011
40. Ke X, Liu C, Li N. Social support and quality of life: a cross-sectional study on survivors eight months after the 2008 Wenchuan earthquake. BMC Public Health. (2008) 10:573. doi: 10.1186/1471-2458-10-573
41. Xie RH, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. (2009) 19:637–43. doi: 10.1016/j.annepidem.2009.03.008
42. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Mak. (2006) 26:565–74. doi: 10.1177/0272989X06295361
43. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. (2015) 16:173–80. doi: 10.1016/S1470-2045(14)71116-7
44. Vickers AJ, Cronin AM, Elkin EB, Gonen M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak. (2008) 8:53. doi: 10.1186/1472-6947-8-53
45. Poslawsky IE, Naber FB, Van Daalen E, Van Engeland H. Parental reaction to early diagnosis of their children's autism spectrum disorder: an exploratory study. Child Psychiatry Hum Dev. (2014) 45:294–305. doi: 10.1007/s10578-013-0400-z
46. Wu J, Zhou Q, Pan Z, Wang Y, Hu L, Chen G, et al. Development and validation of a nomogram for predicting long-term overall survival in nasopharyngeal carcinoma: a population-based study. Medicine. (2020) 99:e18974.
47. Blacher J. The sequential stages of parental adjustment to the birth of a child with handicaps: Fact or artifact? Ment Retard. (1984) 22:55–68.
48. Lu L, Lin YY. Family roles and happiness in adulthood. Pers Individ Dif. (1998) 25:195–207. doi: 10.1016/S0191-8869(98)00009-9
49. Krstić T, Batić S, Mihić L, Milankov V. Mothers' reactions to the diagnosis of cerebral palsy: associations with their educational level. Int J Disabil Dev Educ. (2016) 63:467–83. doi: 10.1080/1034912X.2016.1142068
50. Rouprêt M, Hupertan V, Fau-Seisen T, Seisen T, Fau-Colin P, Colin P, et al. Prediction of cancer specific survival after radical nephroureterectomy for upper tract urothelial carcinoma: development of an optimized postoperative nomogram using decision curve analysis. J Urol. (2013) 189:1662–9. doi: 10.1016/j.juro.2012.10.057
Keywords: psychiatric diagnoses, nomogram, parents, resolution, prediction model, unresolved risk
Citation: Sheng Q, Cai C, Li P, Chen L, Zhang X, Wang X and Gong Y (2022) Development and Validation of a Nomogram for Predicting the Unresolved Risk of Parents of Adolescents With Psychiatric Diagnoses. Front. Psychiatry 13:796384. doi: 10.3389/fpsyt.2022.796384
Received: 16 October 2021; Accepted: 01 February 2022;
Published: 01 April 2022.
Edited by:
Ruoqing Chen, Sun Yat-Sen University, ChinaReviewed by:
Richard S. Lee, Johns Hopkins University, United StatesCopyright © 2022 Sheng, Cai, Li, Chen, Zhang, Wang and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingqing Sheng, ODc3ODgyNjQ0QHFxLmNvbQ==; Yucui Gong, Z29uZ3l1Y3VpZmFuZ0Bzb2h1LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.