- 1Department of Neurology, Joint Research Institute of Altitude Health, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Project Design and Statistics, West China Hospital, Sichuan University, Chengdu, China
- 3Department of Clinical Research Management, West China Hospital, Sichuan University, Chengdu, China
Loneliness is a growing public health problem that threatens physical and mental health to a large extent. Compelling evidence has shown that premature parental death is strongly associated with many mental health disorders in adulthood, but whether it increases the risk of loneliness remains unclear. In this large community-based study, we included 32,682 adult participants (20–93 years old) from Southwest China and used the three-item short version of University of California, Los Angeles, Loneliness Scale to identify participants with loneliness. A total of 1,975 participants reported loneliness, which resulted in a loneliness prevalence of 6.0% in Southwest China. Logistic regression was used to evaluate the association between early parental death and loneliness after adjusting for age, gender, education level, marital status, smoking and drinking status, living status, and chronic diseases. We found that early parental death was significantly associated with loneliness [odds ratio (OR) = 1.21, 95% confidence interval (CI), 1.03–1.42]. A Sensitivity analysis excluding those with mental health disorders (796 participants) yielded similar results (OR = 1.26, 95% CI = 1.06–1.49). We also found that being younger, single, divorced, or widowed, and more educated; living alone; and having chronic disorders were associated with loneliness. We conclude that childhood parental death is associated with loneliness in adulthood, suggesting the need for early intervention in affected children to prevent long-term adverse neuropsychiatric effects.
Introduction
Loneliness is a distressful feeling of social isolation, even if the person is not alone. This is a pervasive mental health condition that has attracted great attention worldwide in recent years (1, 2). Various epidemiological studies have shown that the prevalence of loneliness in middle-aged and older adults ranges from 10.5% up to 78.1% (3–5). Meanwhile, loneliness increases the risk of premature death by 26%, and continues to increase (1). Loneliness has been found to be closely associated with depression (4, 6, 7) and many chronic diseases, such as dementia (8, 9), cardiovascular disease and stroke (10, 11), diabetes, obesity, and respiratory diseases (6, 12). An in-depth understanding of the risk factors for loneliness is essential to better intervene in this condition.
There is compelling evidence suggesting that adverse childhood experiences can generate long-term negative effects on mental health. For example, it increases the risk of alcoholism, problematic drug substance use, depression, anxiety, and other mental health disorders in adulthood (6, 7). Parental death is a traumatic event in childhood that has been associated with depression, suicide, and other chronic illnesses in adulthood (13, 14). However, research on the relationship between early parental death and adulthood loneliness remains limited, and results are inconsistent (15, 16).
To investigate the prevalence of loneliness in Southwest China and to further our understanding of the relationship between childhood parental loss and loneliness in adulthood, we conducted this community-based study of more than 30,000 adults from Sichuan Province, China.
Materials and Methods
Participants
Individual-level data were obtained from the Natural Population Cohort Study of West China Hospital of Sichuan University, an ongoing prospective cohort study conducted in communities, with approval from the Ethics Committee of West China Hospital of Sichuan University. Participants older than 20 years from multiple communities (Longquan, Mianzhu, and Pidu) were encouraged to participant in this project. Communities were distributed in rural, urban, and urban–rural borders. The cohort study started in Longquan in 2019 (with the first wave in 2019 and the second in 2020), in Mianzhu in 2020, and in Pidu in 2021. Annual follow-ups were conducted after initiation. This study used data from Longquan (collected in 2020), Mianzhu, and Pidu (collected in 2021), and data analysis was completed in August 2021.
Loneliness Assessment
Loneliness in adulthood was assessed using the three-item short version of the University of California, Los Angeles (UCLA), Loneliness Scale (17). The scale evaluated the frequency of lack of companionship, exclusion, and isolated from others. Response categories ranged from “never” = 1, “sometimes” = 2, to “too often” = 3. The total score ranges from 3 to 9, with higher scores indicating greater loneliness and a score of 6 or above being classified as lonely (18).
Parental Death and Covariates
All participants were asked whether they had experienced parental death before the age of 17 years, and the answers were yes and no. The following factors were used as covariates: age, gender, marital status, education level, living status, drinking and smoking status, and chronic diseases. Marital statuses included married, single, divorced, and widowed. Educational levels were categorized as elementary school, middle school, high school, and college (or above). Smoking statuses were categorized as yes and no, similar to drinking statuses. Chronic diseases prediagnosed by physicians, including hypertension, diabetes (including intermediate hyperglycemia and prediabetes), hyperlipidemia, stroke, cancer, heart diseases (including coronary heart disease, myocardial ischemia, bundle branch block, and heart failure), respiratory diseases (including chronic obstructive pulmonary disease, asthma, chronic bronchitis, and emphysema), and mental health disorders (depression and anxiety).
Depression and Anxiety
Considering that anxiety and depression are largely underdiagnosed and underreported in China (19, 20), we also used validated scales in this study to screen participants with anxiety (or depression). The 9-item Patient Health Questionnaire (PHQ-9) was used to screen participants for depression, and the 7-item Generalized Anxiety Disorder Scale (GAD-7) was used for anxiety screening. The total score of PHQ-9 ranges from 0 to 27, with a score of 10 or more for major depressive disorder (21). The total score of GAD-7 ranges from 0 to 21 points, and participants with a score of 10 or higher were considered to have anxiety disorders (22).
Statistical Analysis
Continuous variables were presented as mean and standard deviation; categorical variables were described as frequencies and percentages. Student t-test was used to analyze continuous variables; a χ2 test was used for categorical variable. Logistic regression models were used to evaluate odds ratios (ORs) and 95% confidence intervals (CIs) for the association between early parental death and loneliness. Two models were performed: model 1 adjusted for age and gender and model 2 adjusted for all potential confounders, including age, gender, marital status, education level, living status, smoking and drinking status, and chronic diseases. We adjusted for age and gender only in model 1 to avoid overadjustment.
Considering that loneliness symptoms (lack of companionship, having been left out, and isolated from others) screened with UCLA-3 may also be present in some participants with depression or other mental health disorders, we conducted sensitivity analyses excluding participants with depression and anxiety in addition to primary analyses. In this study, those who had been previously diagnosed by physicians or screened positive for the scale were excluded.
We also performed subgroup analyses to explore the relationships between early parental loss and loneliness in the younger (<60 years) and older (≥60 years) groups. In these subgroup analyses, logistic regression models were adjusted for all confounders. Statistical analyses were performed using SPSS (IBM, version 25) and R 4.0 (R Project for Statistical Computing), and a two-sided p < 0.05 was considered statistically significant.
Results
Characteristics of the Participants
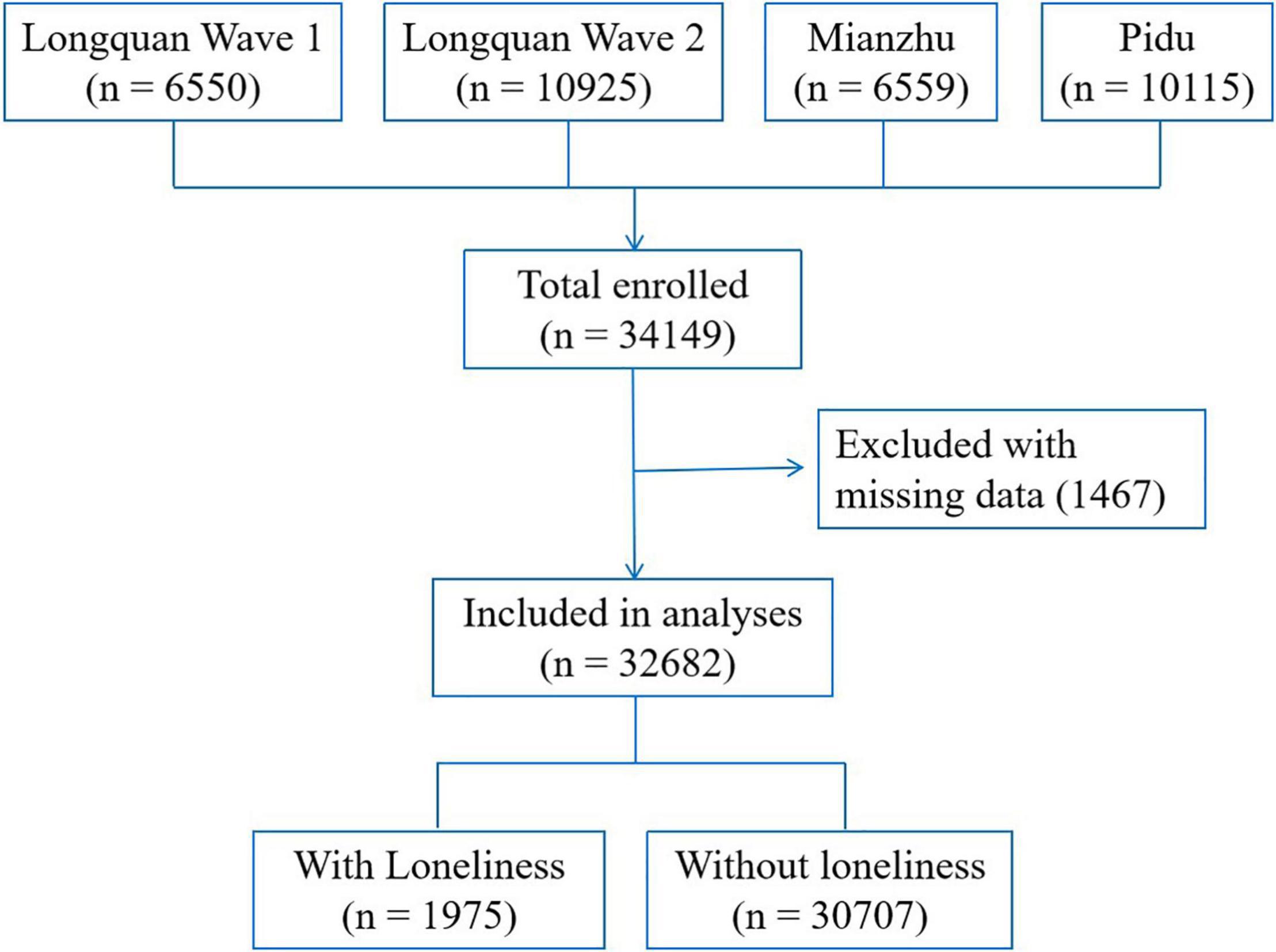
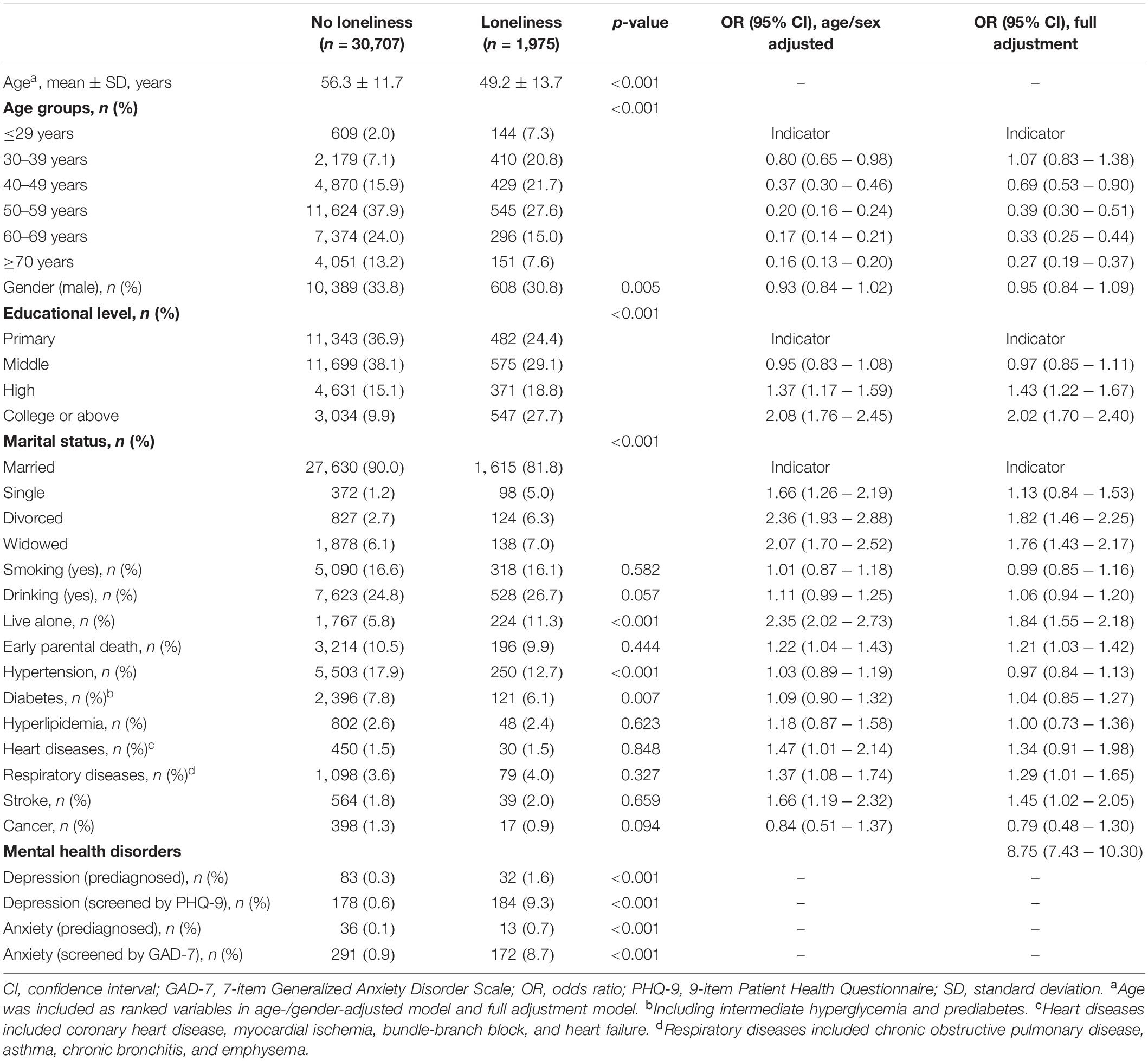
The current cohort enrolled 34,149 participants (including 6,550 participants in the first wave of Longquan, 10,925 participants in the second wave of Longquan, 6,559 from Mianzhu, and 10,115 in Pidu). A total of 1,467 (4.3%) were excluded because of missing data. Finally, 32,682 participants (21,685 female and 10,997 male, age range = 20–93 years) were enrolled in the study, of whom 3,410 (10.4%) reported early parental death. The participant inclusion flowchart is shown in Figure 1. Among all included participants, 1,975 [6.0% 95% CI (5.8–6.3%)] felt lonely, and those who felt lonely were younger than those who did not (49.2 ± 13.7 vs. 56.3 ± 11.7 years, p < 0.001) (Table 1).
Association Between Early Parental Death and Loneliness
From the results, it can be seen that in the age- and sex-adjusted model (OR = 1.22, 95% CI = 1.04–1.43) and the fully adjusted model (OR = 1.21, 95% CI = 1.03–1.42) (Table 1), those whose parents died early were more likely to feel lonely. In sensitivity analyses that excluded people with mental health disorders (796 participants, including 477 participants for depression and 512 participants for anxiety), parental death was still found to be associated with loneliness in age- and sex-adjusted model (OR = 1.29, 95% CI = 1.09–1.52) as well as fully adjusted model (OR = 1.26, 95% CI = 1.06–1.49).
Subgroup analyses showed that early parental death was significantly associated with loneliness in younger adults (OR = 1.34, 95% CI = 1.09–1.65), whereas this effect faded in older adults (OR = 1.06, 95% CI = 0.82–1.36).
Other Factors Associated With Loneliness
In age- and gender-adjusted model, several factors were found to be associated with loneliness. Older participants tended to feel less lonely than younger participants (OR = 0.16, 95% CI = 0.13–0.20 for participants aged ≥70 vs. ≤29 years). People with higher education were more likely to feel lonely (OR = 1.37, 95% CI = 1.17–1.59 for those who attended high school and OR = 2.08, 95% CI = 1.76–2.45 for those who attended a college or above compared with those who attended elementary school or illiterate). Individuals who were single, divorced, or widowed had a higher risk of feeling lonely (OR = 1.66, 95% CI = 1.26–2.19; OR = 2.36, 95% CI = 1.93–2.88; and OR = 2.07, 95% CI = 1.70–2.52, respectively) compared with those who were married. People living alone were more likely to feel lonely (OR = 2.35, 95% CI = 2.02–2.73). Smoking and drinking were not found to be associated with loneliness. For chronic diseases, heart diseases, respiratory diseases, and stroke were significantly associated with a higher risk of loneliness (OR = 1.47, 95% CI = 1.01–2.14; OR = 1.37, 95% CI = 1.08–1.74; and OR = 1.66, 95% CI = 1.19–2.32, respectively). Hypertension, diabetes, hyperlipidemia, and cancer were not found to be associated with loneliness (Table 1).
Discussion
The study, based on more than 30,000 community participants, demonstrated that the prevalence of loneliness in Southwest China was close to 6.0% and that early parental death was associated with loneliness in adulthood, even accounting for other potential risk factors.
The prevalence of loneliness in our study is relatively lower than most previous studies, such as 10.5% reported in German (3), 21.7% reported in Sweden (4), 43% reported in the United States (23), and 78.1% reported in Anhui, China (5). These results are similar to those for other mental disorders. For example, previous surveys, together with our results, suggest that the prevalence of depression and anxiety in Sichuan is much lower than in other provinces (24, 25) and other countries (26, 27). Taken together, these results may suggest that people in Sichuan are more optimistic than those in other regions, leading to a relatively lower rate of loneliness. What is more, the relatively lower prevalence of loneliness in our study could be partly explained by the timing of this study. Our survey was conducted in 2020 and 2021, nearly one year after the COVID-19 pandemic. People during this time may be more united and value their lives than ever before, which may also lead to lower rates of loneliness than studies from other periods.
The most important finding in our study is that we found that early parental death is associated with loneliness. There is growing evidence suggesting that, in addition to parental death, adverse childhood experiences, such as sexual abuse, physical abuse, and neglect, can significantly impair long-term physical and psychological health and increase the risk of loneliness and mental disorders in adulthood (6, 7, 13, 14, 28, 29). Loneliness has also been found to mediate the association between adverse childhood experiences and mental diseases, such as depression and anxiety (29). Vice versa, mental health problems can also increase the risk of loneliness; for example, having depression, anxiety, or other mental disorders can cause people to feel stigmatized and reduce their social interactions with others (28).
Importantly, in this study, the association between parental death and loneliness remained statistically significant after excluding people with mental illness, suggesting that early parental death may be an independent risk factor for adulthood loneliness. Previous researches have shown that parent–infant attachment and healthy early experiences are vital for the development of self-confidence, resilience, social competence, optimism, and trust during one’s growth, whereas negative experiences can affect social support systems in adulthood (29, 30). Thus, people may be more likely to develop certain personality traits that affect their ability to form other relationships (30), resulting in higher rates of loneliness. Interestingly, we found that the effects of early parental death on loneliness were not significant in older adults compared with younger adults, suggesting that the effects of negative childhood experiences on mental health may diminish with age.
Given the profound and long-term health effects of early parental death, those affected need professional support to increase their resilience and reduce the impact of negative impacts on them. In China, all children are required to receive 9 years of compulsory education (i.e., mostly from the age 6 to 15 years). Therefore, schools are where young children stay the most and are the ideal place for intervention. Specialized departments can be set up to provide psychological counseling and support for children whose parents have passed away.
Consistent with previous study, we found that being single, divorced, or widowed; living alone; and having cardiocerebrovascular diseases were associated with loneliness (5, 28, 31). However, previous findings on the association between age and loneliness have been inconsistent across studies (3, 32, 33). Consistent with two previous studies (3, 32), we found that age was negatively correlated with loneliness. As older adults are more satisfied with their friendships and life (34, 35), this may explain why older adults are less likely to feel lonely. We also found an inverse association between education level and loneliness, which is consistent with a recent study conducted in Turkey (36), but contrary to the findings of several previous studies (5, 31). Considering that older and less educated individuals are more likely to be satisfied with their lives (35), increased overall life satisfaction may also be associated with a reduction in their loneliness.
There are some limitations needed to be mentioned in this study. First, recall bias and reporting bias could not be eliminated because of the cross-sectional nature of the study. Second, we did not collect information on the gender and number of parents who died. The lack of this information limited our further analysis. Finally, the results of this study, conducted in Southwest China do not represent the whole picture of the country.
Conclusion
The findings of this study suggest that parental death in childhood is associated with loneliness in adulthood, suggesting the need for early intervention to prevent long-term detrimental neuropsychiatric effects.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the West China Hospital of Sichuan University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AP designed the study, conducted the study, carried out the statistical analysis, and drafted the manuscript. WLi, TS, and XZ collected the information of participants. WLa and SH drafted the manuscript. SJ carried out the statistical analysis. LC designed the study and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Outstanding Youth Scientific and Technological Foundation project, Science and Technology Department of Sichuan Province (No. 2020JDJQ0018), 1⋅3⋅5 Project for Disciplines of Excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (No. 2021HXFH012), and Postdoctoral Research and Development Fund of West China Hospital, Sichuan University (No. 2020HXBH030).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all staff in the department of clinical research management who helped to recruit participants and all study participants.
References
1. Cacioppo JT, Cacioppo S. The growing problem of loneliness. Lancet. (2018) 391:426. doi: 10.1016/S0140-6736(18)30142-9
2. Fried L, Prohaska T, Burholt V, Burns A, Golden J, Hawkley L, et al. A unified approach to loneliness. Lancet. (2020) 395:114. doi: 10.1016/S0140-6736(19)32533-4
3. Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. (2017) 17:97. doi: 10.1186/s12888-017-1262-x
4. Henriksen J, Larsen ER, Mattisson C, Andersson NW. Loneliness, health and mortality. Epidemiol Psychiatr Sci. (2019) 28: 234–9.
5. Wang G, Zhang X, Wang K, Li Y, Shen Q, Ge X, et al. Loneliness among the rural older people in Anhui, China. Prevalence and associated factors. Int J Geriatr Psychiatry. (2011) 26:1162–8. doi: 10.1002/gps.2656
6. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. (2017) 2:e356–66. doi: 10.1016/S2468-2667(17)30118-4
7. Selous C, Kelly-Irving M, Maughan B, Eyre O, Rice F, Collishaw S. Adverse childhood experiences and adult mood problems: evidence from a five-decade prospective birth cohort. Psychol Med. (2020) 50:2444–51. doi: 10.1017/S003329171900271X
8. Lara E, Martín-María N, De la Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, et al. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res Rev. (2019) 52:7–16. doi: 10.1016/j.arr.2019.03.002
9. Yin J, Lassale C, Steptoe A, Cadar D. Exploring the bidirectional associations between loneliness and cognitive functioning over 10 years: The English longitudinal study of ageing. Int J Epidemiol. (2019) 48:1937–48. doi: 10.1093/ije/dyz085
10. Hakulinen C, Pulkki-Råback L, Virtanen M, Jokela M, Kivimäki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479 054 men and women. Heart. (2018) 104:1536–42. doi: 10.1136/heartjnl-2017-312663
11. Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. Eur J Prev Cardiol. (2018) 25:1387–96. doi: 10.1177/2047487318792696
12. Hackett RA, Hudson JL, Chilcot J. Loneliness and type 2 diabetes incidence: findings from the English Longitudinal Study of Ageing. Diabetologia. (2020) 63:2329–38. doi: 10.1007/s00125-020-05258-6
13. Agid O, Shapira B, Zislin J, Ritsner M, Hanin B, Murad H, et al. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol Psychiatry. (1999) 4:163–72. doi: 10.1038/sj.mp.4000473
14. Silverman GK, Johnson JG, Prigerson HG. Preliminary explorations of the effects of prior trauma and loss on risk for psychiatric disorders in recently widowed people. Isr J Psychiatry Relat Sci. (2001) 38:202–15.
15. Ellis J, Dowrick C, Lloyd-Williams M. The long-term impact of early parental death: Lessons from a narrative study. J R Soc Med. (2013) 106:57–67. doi: 10.1177/0141076812472623
16. Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkälä KH. Loss of parents in childhood - associations with depression, loneliness, and attitudes towards life in older Finnish people. Int J Older People Nurs. (2006) 1:17–24. doi: 10.1111/j.1748-3743.2006.00001.x
17. Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. (1980) 39:472–80. doi: 10.1037//0022-3514.39.3.472
18. Mullen RA, Tong S, Sabo RT, Liaw WR, Marshall J, Nease DJ, et al. Loneliness in primary care patients: a prevalence study. Ann Fanm Med. (2019) 17:108–15. doi: 10.1370/afm.2358
19. Gupta S, Goren A, Dong P, Liu D. Prevalence, awareness, and burden of major depressive disorder in urban China. Expert Rev Pharmacoecon Outcomes Res. (2016) 16:393–407. doi: 10.1586/14737167.2016.1102062
20. Yang F, Yang BX, Stone TE, Wang XQ, Zhou Y, Zhang J, et al. Stigma towards depression in a community-based sample in China. Compr Psychiatry. (2020) 97:152152. doi: 10.1016/j.comppsych.2019.152152
21. Levis B, Benedetti A, Thombs BD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
22. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
23. Perissinotto CM, Stijacic CI, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. (2012) 172:1078–83. doi: 10.1001/archinternmed.2012.1993
24. Gu L, Xie J, Long J, Chen Q, Chen Q, Pan R, et al. Epidemiology of major depressive disorder in mainland china: a systematic review. PLoS One. (2013) 8:e65356. doi: 10.1371/journal.pone.0065356
25. Guo X, Meng Z, Huang G, Fan J, Zhou W, Ling W, et al. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015. Sci Rep. (2016) 6:28033. doi: 10.1038/srep28033
26. Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. (1994) 151:979–86. doi: 10.1176/ajp.151.7.979
27. Ohayon MM, Priest RG, Guilleminault C, Caulet M. The prevalence of depressive disorders in the United Kingdom. Biol Psychiatry. (1999) 45:300–7. doi: 10.1016/s0006-3223(98)00011-0
28. Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. (2015) 10:238–49. doi: 10.1177/1745691615570616
29. Murphy S, Murphy J, Shevlin M. Negative evaluations of self and others, and peer victimization as mediators of the relationship between childhood adversity and psychotic experiences in adolescence: the moderating role of loneliness. Br J Clin Psychol. (2015) 54:326–44. doi: 10.1111/bjc.12077
30. Johnson CL, Barer BM. Life course effects of early parental loss among very old African Americans. J Gerontol B Psychol Sci Soc Sci. (2002) 57:S108–16. doi: 10.1093/geronb/57.2.s108
31. Lim MH, Eres R, Vasan S. Understanding loneliness in the twenty-first century: An update on correlates, risk factors, and potential solutions. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:793–810. doi: 10.1007/s00127-020-01889-7
32. Shovestul B, Han J, Germine L, Dodell-Feder D. Risk factors for loneliness: The high relative importance of age versus other factors. PLoS One. (2020) 15:e229087. doi: 10.1371/journal.pone.0229087
33. Lavrič M, Gomboc V, Krohne N, Podlogar T, Poštuvan V, Zadravec ŠN, et al. Loneliness within the general population of Slovenia. Int J Soc Psychiatry. (2021) 67:182–7. doi: 10.1177/0020764020943230
34. Nicolaisen M, Thorsen K. Who are lonely? Loneliness in different age groups (18-81 years old), using two measures of loneliness. Int J Aging Hum Dev. (2014) 78:229–57. doi: 10.2190/AG.78.3.b
35. Pan Y, Chan S, Xu Y, Yeung KC. Determinants of life satisfaction and self-perception of ageing among elderly people in China: an exploratory study in comparison between physical and social functioning. Arch Gerontol Geriatr. (2019) 84:103910. doi: 10.1016/j.archger.2019.103910
Keywords: early parental death, loneliness, adverse childhood experiences, mental health disorders, mental health problems
Citation: Peng A, Lai W, He S, Li W, Song T, Ji S, Zhao X and Chen L (2022) Association Between Early Parental Death and Loneliness in Adulthood: A Community-Based Study in Southwest China. Front. Psychiatry 13:784000. doi: 10.3389/fpsyt.2022.784000
Received: 27 September 2021; Accepted: 28 February 2022;
Published: 31 March 2022.
Edited by:
Lawrence T. Lam, University of Technology Sydney, AustraliaReviewed by:
Ellen E. Lee, University of California, San Diego, United StatesSarah Stahl, University of Pittsburgh, United States
Copyright © 2022 Peng, Lai, He, Li, Song, Ji, Zhao and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Chen, bGVpbGVpXzI1QDEyNi5jb20=
†ORCID: Anjiao Peng, orcid.org/0000-0002-8074-0812; Lei Chen, orcid.org/0000-0001-5263-5540
 Anjiao Peng1†
Anjiao Peng1† Lei Chen
Lei Chen