
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 February 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.774467
This article is part of the Research Topic The Consequences of COVID-19 on the Mental Health of Students View all 71 articles
 Xingjie Yang1†
Xingjie Yang1† Lan Gao1†
Lan Gao1† Suoyuan Zhang1
Suoyuan Zhang1 Libin Zhang2
Libin Zhang2 Ligang Zhang1
Ligang Zhang1 Shuangjiang Zhou1
Shuangjiang Zhou1 Meng Qi3
Meng Qi3 Jingxu Chen1*
Jingxu Chen1*Background: Although professional identity is a strong predictor of career choice, only a few studies have reported on medical students' career attitude during a public health emergency. This study investigates the changes in medical students' professional identity and career attitude during the COVID-19 pandemic, evaluates their mental health and social support system under stress, and explores the relationship between their career attitude and other factors.
Methods: An online survey of 6,226 Chinese medical students was conducted to collect information on demographics, professional identity, and career attitude. The collected data were assessed using the Patient Health Questionnaire, the Generalized Anxiety Disorder Scale, and the Social Support Rating Scale.
Results: The results revealed that most (80.8%) of the participants did not change their career attitude and the professional identity of most participants strengthened, and they preferred to participate on the frontline during the COVID-19 pandemic. The prevalence of depression and anxiety among medical students was 22.86% and 35.43%. Low social support, depressive symptoms, male gender, and higher grades were factors that negatively affected career attitude.
Conclusions: After the outbreak of the pandemic, it was necessary to conduct diversified professional identity research to support medical students, especially those with low social support and depressive symptoms.
COVID-19 is considered a global pandemic and has been raging since March 11, 2020 (1), seriously threatening the health of people worldwide. In many countries, there was a serious shortage of medical workers because of the increased demand for professionals to help; consequently, retired doctors were recalled, and medical students were sent to help in the fight against the pandemic. In China, more than 42,600 medical workers went to the most seriously affected areas to help (2). In this sudden public health crisis, doctors renewed their sense of value and honor in the profession. Medical students are a major component of medical reserve forces and must also participate in ensuring the health and safety of the population (3). Therefore, it is important to assess their professional identity and psychological state during the pandemic.
Under stressful situations, individuals have different emotional, cognitive, and behavioral responses. An individual's cognitive evaluation also affects their stress responses (4). The COVID-19 pandemic has had profound mental health consequences for many people (5), especially college students (6). A previous study indicated that medical University students experienced poor mental states during the COVID-19 outbreak (7).
One's professional identity is an individual's professional self-concept based on their beliefs, values, motives, attributes, and experiences (8) and is derived from and perceived in terms of the role that individuals assume in their work. Professional identity is a factor affecting job satisfaction (9). It is an important part of nurturing professionalism among medical students (10, 11) and is related to how strongly individuals identify with their careers. Some scholars also pay attention to the formation and factors that influence medical students' professional identity (12–15). For physicians-in-training, preliminary data suggest that good virtues in medical practice are associated with a strong sense of professional identity (16). Further, career attitude refers to the tendency of medical students to pursue the medical profession in the future; It depends upon different interlinked factors (17) and formed by a matching of perceptions of specialty characteristics with personal needs (18), such as expected salary, intellectual satisfaction, workload, experience during the medical schools, the student values and professional attitude, and so on. Professional identity is an important predictor of continuing to do the job (9). Previous studies have also shown that students' career attitude would be affected by their mental health state (19), depressive symptoms were considered predictors for professional exhaustion which would affected career attitude (20).
Recently, the professional identities of medical students have gradually studied. During the COVID-19 pandemic, some scholars paid attention to the career attitudes (21, 22) and willing to volunteer (23) in medical students; medical students are motivated by a sense of purpose or duty, altruism, perception of good performance and values of professionalism. Previous studies also have focused on the tense physician-patient relationship and violent injuries in China, which may have affected medical students' professional identity (24). To the best of our knowledge, the professional identity and career attitude of medical students in China during the COVID-19 pandemic have yet to be investigated. Therefore, this study has attempted to investigate the changes in medical students' professional identity and career attitude during the COVID-19 pandemic, evaluate their mental health and social support system under stress, and explore the relationship between their career attitude and correlated factors.
We used an online survey to conduct a cross-sectional study on the professional identity and mental health of medical students from February 11 to 19, 2020. All data were collected online via a self-reported questionnaire using the Wenjuanxing platform (https://www.wjx.cn/). Participants were recruited with a snowball sampling method through wechat and social media in the form of Wenjuanxing. Participants were encouraged to forward the link to other relevant respondents. Prior to filling the questionnaire, participants were informed that they had the rights to withdraw their consents at any time, and that all information would be kept anonymous and confidential throughout the study. Inclusion criteria were full-time medical University students, including undergraduate from grade 1 to grade 5, living in mainland China, ≥18 years of age. A total of 6,318 participants took part in the survey. After excluding incomplete questionnaires and those that were completed in <3 min, 6,226 participants from 31 provinces and autonomous regions were included in the analysis.
Approval for the study was obtained from the Ethics Committee of Beijing HuiLongGuan Hospital. All participants provided informed consent online to participate in the study.
The demographic section was designed by the research team to collect the general characteristics of medical students, including gender, age, grade, hometown, and 2019-nCoV exposure (2019-nCoV exposure means being diagnosed with COVID-19 or having a history of close contact).
The questionnaire was designed to evaluate six factors (professional cognition, professional emotion, professional commitment, professional behavior, professional achievement, and professional value) of professional identity after consulting the relevant literature (25). One item was selected from each of the six dimensions of medical students' professional identity scale (25), and a simple medical students professional identity scale (see Appendix A) was developed to evaluate professional identity. The response for each item consists of five choices: from 1 (strongly disagree) to 5 (strongly agree). In this study, Cronbach's α was 0.857 and 0.890 before and after the pandemic, respectively.
Evaluation of career attitude was conducted by assessing medical students' attitude after the pandemic (the following question was asked: “Did your willingness to practice medicine change after the pandemic?” 1. unchanged; 2. enhanced; 3. weakened). Based on the results, we divided medical students into three groups: unchanged, enhanced, and weakened.
We reviewed the literatures (17, 18) and listed the reasons why medical students were willing or unwilling to continue studying medicine, the reasons were allowed multiple option. Students choose from the seven options below: The reasons for the willingness to be a doctor include: (1) “Being a doctor is my dream.” (2) “Doctors are respected.” (3) “Doctors are valuable.” (4) “Doctors are paid well.” (5) “Doctors have rich social connections.” (6) “After the outbreak, the state will provide more support to doctors.” (7) “Nothing else matters.” The reasons for not being willing to be a doctor include: (1) “Being a doctor is stressful.” (2) “The workload of doctors is too heavy.” (3) “An outbreak of infectious disease increases the risk to doctors and their families.” (4) “Doctor-patient relations are strained.” (5) “Doctors are poorly paid.” (6) “I did not like studying medicine.” (7) “I have other career options.”
Depressive symptoms were screened using the 9-item Patient Health Questionnaire (PHQ-9) (26). The PHQ-9 has been widely used in China, and the reliability and validity of the Chinese version of the PHQ-9 has been demonstrated (27). The PHQ-9 was scored from 0 to 27; Cronbach's α, in this case, was 0.87. A PHQ-9 score > 5 was considered indicative of depressive symptoms.
Anxiety symptoms were screened using the 7-item Generalized Anxiety Disorder Scale (GAD-7) (28). The GAD-7 has been widely used in China, and the reliability and validity of the Chinese version of the GAD-7 has been confirmed (29), with scores ranging from 0 to 21. Cronbach's α for this case was 0.92. A GAD-7 score > 5 was considered indicative of anxiety symptoms.
Social support was assessed using the Social Support Rating Scale (SSRS) (30), which has already been used widely in various studies in different Chinese communities and has been shown to have good validity and reliability (31) a higher score indicating more social support. Final scores were divided into three grades (high, moderate, and low).
Data analysis was performed using SPSS statistical software (version 24.0; IBM Corp). The chi-square test was used to compare the changes in the career attitude of medical students in different demographic categories. Scores obtained from the GAD-7, PHQ-9, and SSRS for the three groups of medical students were also compared. The rank sum test was used to analyze differences in the dimensions of professional identity among the three groups of medical students before and after the pandemic outbreak. Multivariate disordered logic regression was used to analyze the factors influencing changes in career attitude. The level of significance was set at 0.05 (two-sided).
A total of 6,226 full-time medical undergraduates aged 18–27 years completed the questionnaires. The median age of the participants was 21 years, of which 60.1% were female. The students came from all provinces of China, except Macau, and 98.6% took the survey at home. A total of 79.0% of the respondents revealed that they would like to participate in the frontline. And 92.0% of them has no 2019-nCoV exposure.
As shown in Table 1, the number of participants who did not change their career attitude was 4,989 (80.1%), while enhanced career attitudes accounted for 741 (11.9%) of the respondents. Students whose career attitude was weakened totaled 496 (8.0%). There were statistical differences among students from different academic years (P < 0.05) and hometowns (P < 0.05).

Table 1. The changes in career attitude among medical students with different socio-demographic characteristics (N = 6,226).
We then investigated why medical students were willing and unwilling to become doctors. As shown in Figure 1, the top three reasons for willingness to become a doctor were: (1) “Doctors are valuable.” (2) “Being a doctor is my dream.” (3) “Doctors are respected.” The top three reasons for not being willing to become a doctor were: (1) “Doctor-patient relations are strained.” (2) “The workload of doctors is too heavy.” (3) “Being a doctor is stressful.” (Figure 2).
Table 2 includes the results that were obtained using the non-parametric Wilcoxon signed-rank test. In the enhanced group, there was no significant difference in professional achievement before and after the pandemic (P = 0.494); however, the difference was statistically significant for the rest of the groups. In the weakened group, there were significant differences in professional cognition, commitment, achievement, and value.
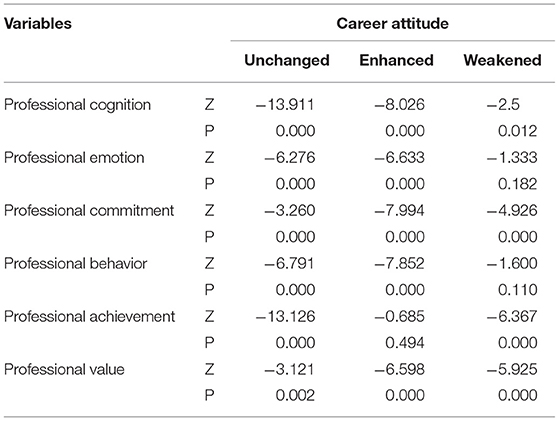
Table 2. The professional identity among medical students with different career attitudes before and after the pandemic (N = 6,226).
Scores (cutoff score 5) from GAD-7 and PHQ-9 tests were used to divide respondents into the “anxiety group” and the “depression group,” Based on the GAD-7 and PHQ-9, the prevalence of depression and anxiety among medical students was 22.86 and 35.43%, respectively. A chi-square test showed that there were significant differences in anxiety, depression, and social support among the three groups of medical students with different career attitude (summarized in Table 3).
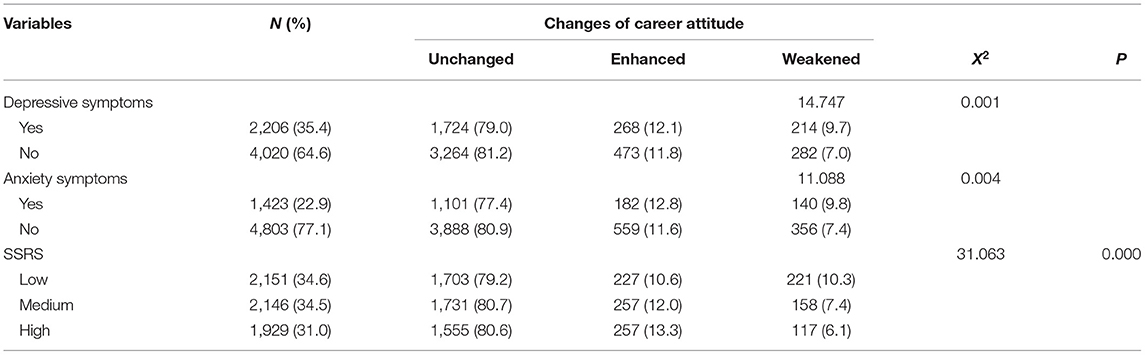
Table 3. Depressive symptoms, anxiety symptoms and social support among medical students with different changes in career attitude (N = 6,226).
We set the dependent variable of weakened, unchanged, and enhanced groups to 0, 1, and 2, respectively, and then performed an ordered multivariate logistic regression analysis. The parallel line hypothesis test showed P < 0.05, which indicated that the data could not be analyzed using this method. Therefore, we conducted a disordered multivariate logistic regression analysis. The resultant chi-square value of the model was 139.49 (P < 0.001), which indicated its statistical significance. The pseudo-R2 of Nagelkerke was 0.031, which indicated that the model corresponded, to a certain degree, with the dependent variables (Table 4).
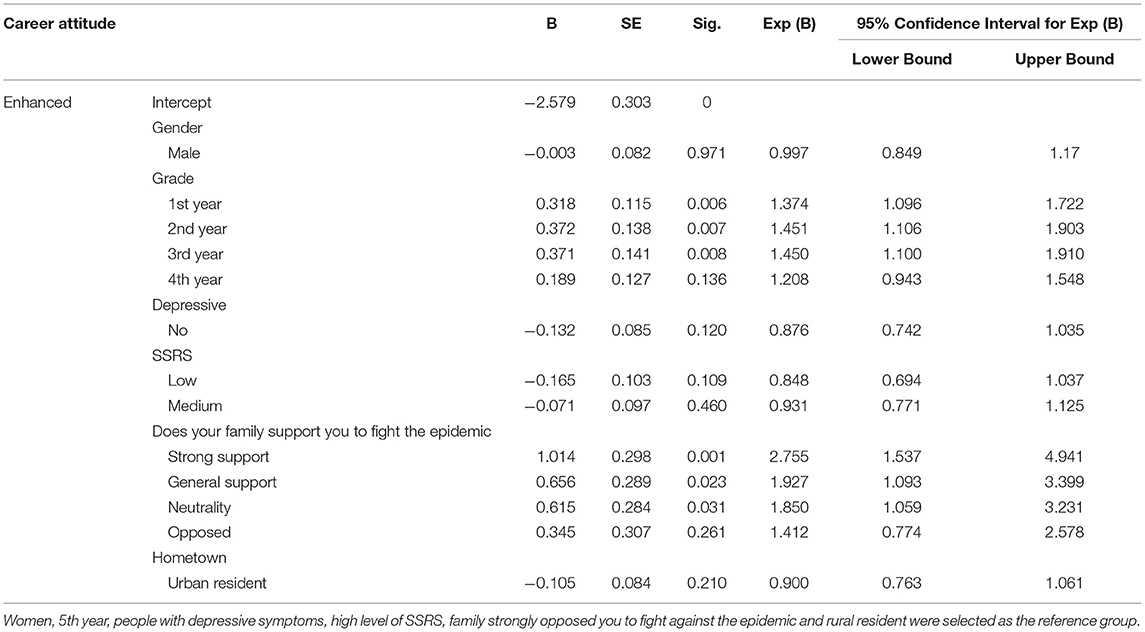
Table 4. Multivariate disordered logic regression of the factors associated with the changes in career attitude (N = 6,226).
Compared to subjects in the unchanged group, students in junior academic classes of medical school were more likely to enhance their career attitudes, whereas the attitude of freshmen was 1.374 times higher than that of fifth-year students. Subjects whose family members strongly supported them in their fight against the pandemic were more likely to enhance their career attitude than those who were strongly opposed by their family members. The number of subjects who were strongly supported by their families was 2.755 times higher than those whose family members were strongly opposed (Table 4).
Compared to subjects in the unchanged group, males were more likely to weaken their career attitude than females, and medical students with depression were more likely to weaken their attitudes than those with high social support. Students who lived in cities were 1.248 times less likely to practice medicine than those living in rural areas. The results are summarized in Table 5.
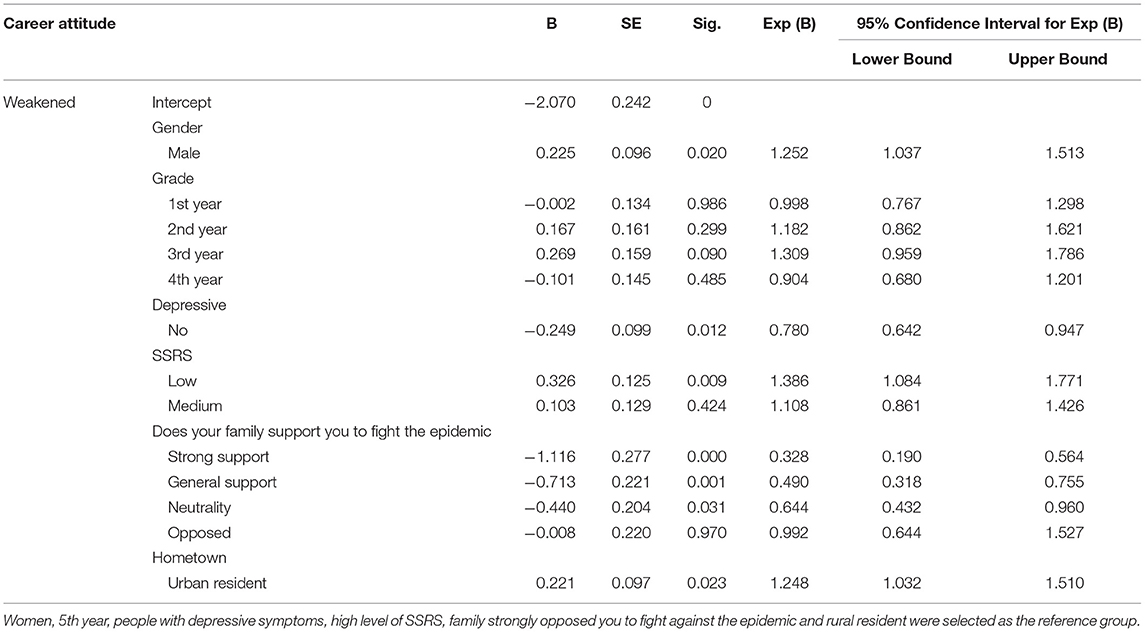
Table 5. Multivariate disordered logic regression of the factors associated with the changes in career attitude (N = 6,226).
The career attitude formed by a matching of perceptions of specialty characteristics with personal needs (18) and the characteristics of students such as age, gender, geography and study year (17). In this study, there were statistical differences among students from different academic years and hometowns. Previous studies have shown that the professional identity of medical students decreases over time (32, 33). At the time of our survey, medical students were staying in their home towns on winter vacation. And medical students from urban resident or rural resident are different, this could be explained by imbalances between economy, culture, and different publicity efforts relating to pandemic prevention knowledge between urban and rural areas (21).
In this study, most (80.8%) of the participants did not change their career attitude, and 741 (11.9%) of the total respondents enhanced their career attitude. This shows that the majority of medical students have a strong desire to become doctors, indicating that they have a strong professional identity. Professional identity is an important factor in the development of medical education and practice, and the transformation of medical students' professional identity is at the core of medical education (11). Those who possess a strong professional identity are more likely to be connected to their line of work and find a greater sense of purpose in life through it (34). In addition, medical students' career attitudes are influenced by their cognition about, attitude toward, and evaluation of their future careers. The formation and evolution of a professional identity is a dynamic process. Before and after the pandemic, most dimensions of professional identity of medical students changed. These findings revealed that COVID-19 pandemic could affect the professional identities of medical students. This finding was similar to that of a previous study, which concluded that nursing students' professional identity was enhanced after the outbreak of SARS in Hong Kong, China (35). After the outbreak of COVID-19 pandemic, one study (36) found that about one-fifth of surveyed medical students currently believe that the COVID-19 pandemic will affect their choice of specialty. Another study found that the percentage of middle-school students who wanted to study medicine increased to 55.1%, and 29.8% of middle-school students had changed from unwilling to study medicine to willing to study medicine, which indicated that middle-school students had changed their attitude toward medical work after the outbreak of COVID-19 (37). Another study (23) showed that 48.7% of Indonesian medical students were willing to volunteer, shortage of medical personnel and sense of duty were the main reasons increasing the students' willingness to volunteer. The professionalism of medical staff during the epidemic may also have been an inspiration. Some scholars (38, 39) found that the role of models and mentors had a significant impact on the professional identity of medical students. Passi and Johnson (40) also indicated that positive role modeling by doctors effectively enhanced the transformation of a student into a doctor. In this study, 79.0% of the students were likely to engage in the “battle” against the virus. This could be regarded as their “post-traumatic growth,” which suggests that exposure to critical events could lead to opportunities for growth (41). According to the survey in this study, “being a doctor is valuable,” “being a doctor is my dream,” and “being a doctor is respected” are the most popular reasons medical students choose to become a doctor. The sense of value and achievement of doctors is still the main reason medical students choose to become doctors.
This study also found that medical students with depression were more likely to weaken their attitude toward medicine, which might be due to a sense of uncertainty about themselves. Previous studies (42, 43) have shown that depression is one of the most common health problems among University students, especially among medical students who endured heavy financial burdens and study-induced stress (44). After the outbreak of COVID-19, 37.0% of Chinese University students experienced depressive symptoms and 24.9% experienced anxiety symptoms (37). The mental health of these medical students could be a predisposing factor for burnout during residency or postgraduate training (45). This might also affect their choice of future career.
Similarly, it was found that strong social support enhanced medical students' career attitudes. This study also established that the attitude of medical students' family members toward fighting the pandemic also affected students' attitudes toward medical practice. Generally speaking, people with high social support had better resources; they received more support and help coping with their working environment and were more likely to solve problems and difficulties. As a resource available to individuals, social support played an intermediary role in coping with stress, and those with good social support could cope better with it (46). The availability of social support reduced the odds of mental distress for those who experienced it (47). Degree of social support was found to be negatively correlated with anxiety and depression among residents (44). In the current COVID-19 outbreak, high social support can effectively reduce anxiety and improve self-efficacy and sleep quality in COVID-19 patients' caregivers (48). Students who lived alone or had poor relationships with their partners, classmates, or friends scored higher on the depression and anxiety scales. Thus, for medical students under stress due to the public health emergency, good social support was conducive to a positive psychological state and encouraged them to continue to engage in the medical profession.
In addition, freshmen, sophomores, juniors, and senior medical students were more likely to strengthen their career attitudes than fifth-year medical students. Previous studies have shown that the professional identity of medical students decreases over time (32, 33). Iqbal et al. (49) also indicated that higher-grade University students were more depressed and had poorer mental health. The reason might be that the higher-grade students have higher levels of stress (50), and they were affected by a heavy academic load and encountered setbacks in clinical internship. On the other hand, the lower-grade medical students had just entered medical colleges and had not yet completely started the study of clinical medicine; thus, they expected much from themselves.
Males were more likely to weaken their attitudes toward medicine. Some previous studies (32, 33, 51) concluded that females reported stronger identification than males. This might be related to the fact that males bore more social responsibilities and economic pressure (52, 53) which bring more pressure or their less seeking help and coping strategies.
The most significant advancement of this study was that it conducted the largest survey of professional identity and career attitude of medical students during the COVID-19 pandemic. Simultaneously, this study discussed the demographic factors of people with different career attitudes in depth and assessed factors related to mental health status. Further research in the field should focus on ways to improve medical students' mental health and enhance their professional identity.
However, this study has several limitations. First, the cases were recruited using snowball sampling. We could not weigh this sample to increase representativeness because statistics on national medical students were not available. Second, medical students reported their professional identity before the outbreak, and the retrospective nature of the study might have caused recall bias. Finally, although the data collection process was anonymous, online surveys could not verify the identity of respondents, and self-reporting might have been accompanied by personal biases.
The COVID-19 pandemic not only effected a crisis but reconstructed the professional identity of medical students. After such a crisis, some medical students' professional identity was enhanced, and they were proud of the profession they had chosen to pursue. However, as illustrated above, this was not the case for all medical students. We should pay more attention to medical students with depressive symptoms, low social support, and higher grades. The utilization of social support by medical students could be strengthened through group coaching, which is an effective method of support (54).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of Beijing HuiLongGuan Hospital. The patients/participants provided their written informed consent to participate in this study.
JXC and XJY designed the study, revised the manuscript, and wrote the final version. XJY and LG completed the design of the questionnaire. LBZ and JXC analyzed the data. SYZ, LGZ, and MQ have contributed to data collection. SJZ participated in the revising of the manuscript. JXC received funding support for the research. All authors contributed to the final draft of the manuscript.
This work was supported by Capital Foundation of Medicine Research and Development (Grant Number: 2018-3-2132) and the Special Foundation of Beijing Municipal Science and Technology Commission (Grant Number: Z171100001017001).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank J. L. Hou for his generous contributions to the project and thank Editage (www.editage.cn) for English language editing. We also thank all of the participants for their willingness to participate in the study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.774467/full#supplementary-material
1. World Health Organization. Novel Coronavirus-2019. (2020). Retrieved from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed July 11, 2021).
2. Agency XN. Retrieved from: http://www.gov.cn/xinwen/2020-03/09/content_5488858.htm (accessed July 03, 2021).
3. Patey DJL. The educative value of responsible history-taking by medical students. Lancet. (1955) 269:414–5. doi: 10.1016/S0140-6736(55)92640-4
5. Duan H, Yan L, Ding X, Gan Y, Kohn N, Wu J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: changes, predictors and psychosocial correlates. Psychiatry Res. (2020) 293:113396. doi: 10.1016/j.psychres.2020.113396
6. Christophers B, Nieblas-Bedolla E, Gordon-Elliott J, Kang Y, Holcomb K, Frey MK. Mental health of US medical students during the COVID-19 pandemic. J Gen Intern Med. (2021) 36:3295–7. doi: 10.1007/s11606-021-07059-y
7. Yin Y, Yang X, Gao L, Zhang S, Qi M, Zhang L, et al. The Association between social support, COVID-19 exposure, and medical students' mental health. Front Psychiatry. (2021) 12:555893. doi: 10.3389/fpsyt.2021.555893
8. Johnson M, Cowin LS, Wilson I, Young H. Professional identity and nursing: contemporary theoretical developments and future research challenges. Int Nurs Rev. (2012) 59:562–9. doi: 10.1111/j.1466-7657.2012.01013.x
9. Sabanciogullari S, Dogan S. Relationship between job satisfaction, professional identity and intention to leave the profession among nurses in Turkey. J Nurs Manag. (2015) 23:1076–85. doi: 10.1111/jonm.12256
10. Ravella KC, Curlin FA, Yoon JD. Medical school ranking and medical student vocational identity. Teach Learn Med. (2015) 27:123–12 doi: 10.1080/10401334.2015.1011644
11. Adams J, Ari M, Cleeves M, Gong J. Reflective writing as a window on medical students' professional identity development in a longitudinal integrated clerkship. Teach Learn Med. (2020) 32:117–117 doi: 10.1080/10401334.2019.1687303
12. Goldstein PA, Storey-Johnson C, Beck S. Facilitating the initiation of the physician's professional identity: Cornell's urban semester program. Perspect Med Educ. (2014) 3:492–49 doi: 10.1007/s40037-014-0151-y
13. MacLeod A. Caring, competence and professional identities in medical education. Adv Health Sci Educ Theory Pract. (2011) 16:375–37. doi: 10.1007/s10459-010-9269-9
14. Weaver R, Peters K, Koch J, Wilson I. 'Part of the team': professional identity and social exclusivity in medical students. Med Educ. (2011) 45:1220–9. doi: 10.1111/j.1365-2923.2011.04046.x
15. Wong A, Trollope-Kumar K. Reflections: an inquiry into medical students' professional identity formation. Med Educ. (2014) 48:489–4891 doi: 10.1111/medu.12382
16. Leffel GM, Oakes Mueller RA, Ham SA, Karches KE, Curlin FA, Yoon JD. Project on the good physician: further evidence for the validity of a moral intuitionist model of virtuous caring. Teach Learn Med. (2018) 30:303–303 doi: 10.1080/10401334.2017.1414608
17. Assefa T, Haile Mariam D, Mekonnen W, Derbew M. Medical students' career choices, preference for placement, and attitudes towards the role of medical instruction in Ethiopia. BMC Med Educ. (2017) 17:96. doi: 10.1186/s12909-017-0934-z
18. Querido SJ, Vergouw D, Wigersma L, Batenburg RS, De Rond ME, Ten Cate OT. Dynamics of career choice among students in undergraduate medical courses. A BEME systematic review: BEME Guide No. 33. Med Teach. (2016) 38:18–180 doi: 10.3109/0142159X.2015.1074990
19. Yousef S, Athamneh M, Masuadi E, Ahmad H, Loney T, Moselhy HF, et al. Association between depression and factors affecting career choice among jordanian nursing students. Front Public Health. (2017) 5:311. doi: 10.3389/fpubh.2017.00311
20. Oliveira AM, Silva MT, Galvao TF, Lopes LC. The relationship between job satisfaction, burnout syndrome and depressive symptoms: an analysis of professionals in a teaching hospital in Brazil. Medicine. (2018) 97:e13364. doi: 10.1097/MD.0000000000013364
21. Gao F, Jiao SX, Bi YQ, Huang ZY, Wang P, Zhang BY, et al. The impact of the SARS-COV-2 pandemic on the mental health and employment decisions of medical students in North China. Front Psychiatry. (2021) 12:641138. doi: 10.3389/fpsyt.2021.641138
22. Compton S, Sarraf-Yazdi S, Rustandy F, Radha Krishna LK. Medical students' preference for returning to the clinical setting during the COVID-19 pandemic. Med Educ. (2020) 54:943–943 doi: 10.1111/medu.14268
23. Lazarus G, Findyartini A, Putera AM, Gamalliel N, Nugraha D, Adli I, et al. Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: a cross-sectional survey in Indonesia. BMC Med Educ. (2021) 21:138. doi: 10.1186/s12909-021-02576-0
24. Xie Z, Li J, Chen Y, Cui K. The effects of patients initiated aggression on Chinese medical students' career planning. BMC Health Serv Res. (2017) 17:849. doi: 10.1186/s12913-017-2810-2
25. Zhang L. Research on Current Status and Influencing Factors of Medical Students' Professional Identity. Shanghai: East China Normal University (2013).
26. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–606 doi: 10.1046/j.1525-1497.2001.016009606.x
27. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
28. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–09 doi: 10.1001/archinte.166.10.1092
29. Yu W, Singh S, Calhoun S, Zhang H, Zhao X, Yang F. Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J Affect Disord. (2018) 234:89–96. doi: 10.1016/j.jad.2018.02.012
30. Yu Y, Yang JP, Shiu CS, Simoni JM, Xiao S, Chen WT, et al. Psychometric testing of the Chinese version of the Medical Outcomes Study Social Support Survey among people living with HIV/AIDS in China. Appl Nurs Res. (2015) 28:328–33. doi: 10.1016/j.apnr.2015.03.006
31. Xie RH, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. (2009) 19:637–637 doi: 10.1016/j.annepidem.2009.03.008
32. Burford B, Rosenthal-Stott HES. First and second year medical students identify and self-stereotype more as doctors than as students: a questionnaire study. BMC Med Educ. (2017) 17:209. doi: 10.1186/s12909-017-1049-2
33. Coster S, Norman I, Murrells T, Kitchen S, Meerabeau E, Sooboodoo E, et al. Interprofessional attitudes amongst undergraduate students in the health professions: a longitudinal questionnaire survey. Int J Nurs Stud. (2008) 45:1667–667 doi: 10.1016/j.ijnurstu.2008.02.008
34. González RA. The vocation to serve: cornerstone of health care. MEDICC Rev. (2012) 14:52. doi: 10.37757/MR2012V14.N4.1
35. Heung YY, Wong KY, Kwong WY, To SS, Wong HC. Severe acute respiratory syndrome outbreak promotes a strong sense of professional identity among nursing students. Nurse Educ Today. (2005) 25:112–8. doi: 10.1016/j.nedt.2004.11.003
36. Byrnes YM, Civantos AM, Go BC, McWilliams TL, Rajasekaran K. Effect of the COVID-19 pandemic on medical student career perceptions: a national survey study. Med Educ Online. (2020) 25:1798088. doi: 10.1080/10872981.2020.1798088
37. Hongjie M, Jingxu C, Shuangjiang Z, Ligang Z, Yunai S. Willingness to engage in medical care and related factors among middle school students during the COVID-19 epidemic. Chin Mental Health J. (2021) 35:172–6. doi: 10.3969/j.issn.1000-6729.2021.02.014
38. Hendelman W, Byszewski A. Formation of medical student professional identity: categorizing lapses of professionalism, and the learning environment. BMC Med Educ. (2014) 14:139. doi: 10.1186/1472-6920-14-139
39. Burgess A, Goulston K, Oates K. Role modelling of clinical tutors: a focus group study among medical students. BMC Med Educ. (2015) 15:17. doi: 10.1186/s12909-015-0303-8
40. Passi V, Johnson N. The impact of positive doctor role modeling. Med Teach. (2016) 38:1139–139 doi: 10.3109/0142159X.2016.1170780
41. Sattler DN, Boyd B, Kirsch J. Trauma-exposed firefighters: relationships among posttraumatic growth, posttraumatic stress, resource availability, coping and critical incident stress debriefing experience. Stress Health. (2014) 30:356–356 doi: 10.1002/smi.2608
42. Naja WJ, Kansoun AH, Haddad RS. Prevalence of depression in medical students at the lebanese University and exploring its correlation with facebook relevance: a questionnaire study. JMIR Res Protoc. (2016) 5:e96. doi: 10.2196/resprot.4551
43. Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X. A systematic review of depression and anxiety in medical students in China. BMC Med Educ. (2019) 19:327. doi: 10.1186/s12909-019-1744-2
44. Shao R, He P, Ling B, Tan L, Xu L, Hou Y, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. (2020) 8:38. doi: 10.1186/s40359-020-00402-8
45. Low ZX, Yeo KA, Sharma VK, Leung GK, McIntyre RS, Guerrero A, et al. Prevalence of burnout in medical and surgical residents: a meta-analysis. Int J Environ Res Public Health. (2019) 16:1479. doi: 10.3390/ijerph16091479
46. Thompson G, McBride RB, Hosford CC, Halaas G. Resilience among medical students: the role of coping style and social support. Teach Learn Med. (2016) 28:174–174 doi: 10.1080/10401334.2016.1146611
47. Mboya I, John B, Kibopile E, Mhando L, George J, Ngocho JS. Factors associated with mental distress among undergraduate students in northern Tanzania. BMC Psychiatry. (2020) 20:28. doi: 10.1186/s12888-020-2448-1
48. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monitor. (2020) 26:e923549. doi: 10.12659/MSM.923549
49. Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. (2015) 141:354–35 doi: 10.4103/0971-5916.156571
50. Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. (2015) 173:90–90 doi: 10.1016/j.jad.2014.10.054
51. Cleland JA, Johnston PW, Anthony M, Khan N, Scott NW. A survey of factors influencing career preference in new-entrant and exiting medical students from four UK medical schools. BMC Med Educ. (2014) 14:151. doi: 10.1186/1472-6920-14-151
52. Walter G, Soh NL, Norgren Jaconelli S, Lampe L, Malhi GS, Hunt G. Medical students' subjective ratings of stress levels and awareness of student support services about mental health. Postgrad Med J. (2013) 89:311–31 doi: 10.1136/postgradmedj-2012-131343
53. Moazam F, Shekhani S. Why women go to medical college but fail to practise medicine: perspectives from the Islamic Republic of Pakistan. Med Educ. (2018) 52:705–705 doi: 10.1111/medu.13545
Keywords: professional identity, career attitude, COVID-19 pandemic, China, medical students, health emergency
Citation: Yang XJ, Gao L, Zhang SY, Zhang LB, Zhang LG, Zhou SJ, Qi M and Chen JX (2022) The Professional Identity and Career Attitude of Chinese Medical Students During the COVID-19 Pandemic: A Cross-Sectional Survey in China. Front. Psychiatry 13:774467. doi: 10.3389/fpsyt.2022.774467
Received: 12 September 2021; Accepted: 10 January 2022;
Published: 15 February 2022.
Edited by:
Daria Smirnova, Samara State Medical University, RussiaReviewed by:
Marinos Sotiropoulos, Brigham and Women's Hospital and Harvard Medical School, United StatesCopyright © 2022 Yang, Gao, Zhang, Zhang, Zhang, Zhou, Qi and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingxu Chen, Y2hlbmp4MTExMEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.