
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 26 April 2022
Sec. Mood Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.760521
This article is part of the Research Topic Insights in Mood and Anxiety Disorders: 2021 View all 18 articles
 Qing Chang1,2,3†
Qing Chang1,2,3† Han Su1,3†
Han Su1,3† Yang Xia1,3
Yang Xia1,3 Shanyan Gao1,3
Shanyan Gao1,3 Ming Zhang4
Ming Zhang4 Xiaoyu Ma1,3
Xiaoyu Ma1,3 Yashu Liu1,3
Yashu Liu1,3 Yuhong Zhao1,3*
Yuhong Zhao1,3*Background: In China, mental health of frontline medical staff might be influenced by clinicians' ability to handle the outbreak of coronavirus disease 2019 (COVID-19). Few studies to-date have addressed the association between clinicians' competencies and mental health in this context. This cross-sectional study was to examine the prevalence of mental health symptoms among frontline medical staff that fought against the COVID-19 outbreak, and explore the associations between their competencies, and separate and concurrent depressive and anxiety symptoms.
Methods: A total of 623 frontline medical staff was included in this study. Competencies, depressive symptoms, and anxiety symptoms were assessed using a self-reported short form of the Chinese clinical physicians' competency model, Patient Health Questionnaire-9, and Generalized Anxiety Disorder-7 questionnaire, respectively. Logistic regression models were used to evaluate the associations between one SD increase in competency scores and the prevalence of mental health problems.
Results: The prevalence of depressive, anxiety, and comorbid depressive and anxiety symptoms was 40.93, 31.78, and 26.00%, respectively. Among the medical staff with higher total competency scores, the prevalence of depressive [odds ratios (ORs) = 0.67, 95% confidence intervals (CIs): 0.55–0.81], anxiety (OR = 0.68, 95% CI: 0.56–0.83), and comorbid anxiety and depressive symptoms (OR = 0.69, 95% CI: 0.55–0.83) was lower than among their lower-scoring counterparts. Subgroup analyses stratified by core competency scores revealed similar associations as the main analyses.
Conclusion: The present findings highlight the association between high core competency scores and lower prevalence of depressive, anxiety, and comorbid anxiety and depressive symptoms.
Coronavirus disease 2019 (COVID-19), was initially reported in Wuhan, the capital of Hubei Province in China, has rapidly spread globally (1–4). The World Health Organization Emergency Committee declared COVID-19 outbreak an international public health emergency in late January 2020 (5). Wuhan soon became an epicenter of COVID-19 in China. By March 1, 2020, there have been 79,968 confirmed COVID-19 cases, including 2,873 associated deaths in China (6). The entire health care system in Wuhan, even in Hubei Province was almost paralyzed by then due to this rapidly evolving epidemic. The government of China took active measures to call for support to fight against the rapid transmission of COVID-19. Thus, over 30,000 volunteered healthcare workers from all over China were sent to Hubei Province and provided medical support to combat the COVID-19 outbreak (7, 8).
Such large-scale public health threat associated with infectious disease poses several challenges to frontline healthcare workers, who are generally medical workers treating patients with major contagious diseases. For instance, frontline medical workers are under tremendous physical and psychological pressure, higher risk of being infected, considerable work intensity, in particular, and have to cope with unknown causes and pathogens of the diseases, especially in the early stage of the COVID-19 outbreak (9, 10). The present COVID-19 epidemic has features comparable to the 2003 outbreak of severe acute respiratory syndrome (SARS-CoV), which was caused by another coronavirus, resulting in 349 deaths out of 5,327 confirmed cases in China (11). Previous studies have reported that in the initial phase of the SARS outbreak, medical staff felt vulnerable, uncertain, and concerned for their lives, which manifested with physical and psychological symptoms (12–16). It is demonstrated that frontline medical workers fighting against COVID-19 are susceptible to mental illnesses, such as depression and anxiety (10). Another study found that during the COVID-19 outbreak, frontline healthcare workers were more likely to have psychosocial issues and risk factors for developing them (17). A study carried out in Wuhan indicated that poor mental health status and sleep quality were common among frontline medical workers during the COVID-19 outbreak (18). Another survey reported that the prevalence of depression, anxiety, insomnia, and distress symptoms was 50.7, 44.7, 36.1, and 73.4%, respectively, among frontline healthcare workers in China (19). Moreover, frontline medical workers who experienced symptoms of depression were at increased risk of making errors in patient care (20). Maintaining good mental health among medical staff is essential to prevent infectious disease from spreading and ensure long-term wellbeing of staff (21, 22). Therefore, the mental health of frontline medical staff should be placed more emphasis during the outbreak of COVID-19.
Competence is a concept that refers to the ability to perform a specific activity, integrating knowledge, skills, values, and attitudes, often used to distinguish average and outstanding performance of a role (23, 24). Competence is measurable and can be developed through training. In the early stages of the COVID-19 outbreak, frontline medical workers have experienced substantial challenges with their competencies (25). Evidence shows that the core competencies are essential for healthcare workers to combat major infectious diseases outbreak (26, 27). It is demonstrated that the core competencies of nursing personnel are identified as a important factor affecting nursing effectiveness (28). Another study indicates that core competencies of nurse, including their knowledge, skills and experiences to handle unknown infectious disease, have a substantial impact on the prevention and control of the COVID-19 outbreak in China (29). In addition, it is suggested that a training program is required to improve core competencies of healthcare providers in regard to infectious disease outbreaks (30). Therefore, it is hypothesized that the high prevalence of mental disorders among frontline healthcare workers might be influenced by their competencies to handle the outbreak of COVID-19 in China. However, to the best of our knowledge, the association between competencies and mental health symptoms among frontline medical workers during the COVID-19 outbreak still remains unknown.
Therefore, the present cross-sectional study intends to examine the prevalence of mental health problems among frontline medical staff responding to the COVID-19 outbreak, and explore the associations between core competency scores and prevalence of depressive, anxiety, and comorbid anxiety and depressive symptoms in this population.
According to the COVID-19 pandemic isolation regulations, this cross-sectional study avoided the face to face interview and adopted online survey using an electronic questionnaire tool named “Questionnaire Star”, which was a mini-programme based on WeChat (a social media app widely used in China). Participants were able to fill out the questionnaire after scanning a quick response (QR) code by their mobile phones. Questionnaires were distributed by the directors of the medical aiding teams in WeChat group. In order to guarantee quality control of answering questionnaire, a 5-min time-frame was set in Questionnaire Star. In the pilot study, the average time of finishing the questionnaire was 5 min. Those who completed the questionnaire within 5 min would not be able to submit. Those who did not answer the questionnaire in the opening hours, or exceed the time limit for questionnaire, or have incomplete answer for the questions would be ruled out. In addition, several simple repeated questions, including age, years of service, marriage status, were set automatically in questionnaire. If the answers of the repeated questions were inconsistent, the questionnaire would be considered invalid. The entry criteria were as follows: (1) individuals aged 18 years or older; (2) frontline healthcare workers who were volunteers from different hospitals in Liaoning Province and offered medical support to cope with COVID-19 in Hubei Province; (3) without serious mental illness, such as schizophrenia. The exclusion criteria were as follows: (1) Those who did not answer the questionnaire in the opening hours; (2) Exceeding the time limit for questionnaire; (3) incomplete answer for the questions. (4) Those who failed to answer the repeated questions correct. From January 20, 2020 to February 20, 2020, which basically was the early stage of COVID-19 outbreak in China, a total of 669 frontline medical staff coping with the COVID-19 outbreak participated in the present study. Participants who failed to provide information on any of the variables were ruled out (n = 46). Overall, data from 623 participants were collected in the analyses. The study protocol was approved by the ethics committee of Shengjing Hospital of China Medical University, and all participants provided written informed consent to participate. The study protocol conformed to the principles of the 1975 Declaration of Helsinki.
Depressive symptoms were assessed using the Chinese version of the Patient Health Questionnaire-9 (PHQ-9), a nine-item questionnaire designed to screen for depression in primary care and other medical settings (31). Questionnaire items were scored from 0 (not at all) to 3 (nearly every day). The sum of these scores produced an overall score, ranging from 0 to 27; higher scores indicated greater depressive symptoms. The degree of depressive symptoms was classified into four categories according to the score: 0–4 points: no depression; 5–9 points: mild depression; 10–14 points: moderate depression and ≥ 15 points: severe depression (31). Those participants with an overall PHQ-9 score ≥ 5 were considered to suffer depressive symptoms (31).
Anxiety symptoms were assessed using the Chinese version of the Generalized Anxiety Disorder-7 (GAD-7) questionnaire, which consists of 7 questions and reflects the frequency of symptoms during the preceding 2 weeks (32). Questionnaire items were scored from 0 (not at all) to 3 (nearly every day). The sum of these scores produced an overall score, ranging from 0 to 21, with higher scores indicating greater anxiety symptoms. The degree of anxiety was evaluated in accordance with the score: 0–4 points: no anxiety: 5–9 points: mild anxiety; 10–14 points: moderate anxiety and ≥ 15 points or above: severe anxiety (32). Those individuals with an overall GAD-7 score ≥ 5 were considered to suffer anxiety symptoms (32).
Competencies among frontline medical staff were assessed using the short version of the Chinese clinical physicians' competency model, which was comprised of 12 items, classified into 8 components: clinical skills and patient care, mastery of medical knowledge, information and management, professionalism, interpersonal communication, health promotion and disease prevention, academic research, and teamwork (33, 34). In general, the items of abundant clinical experiences, skills of curing respiratory diseases, skills of treating infectious disease, skills of dealing with critical illnesses, nursing operating skills were classified into the dimension of clinical skills and patient care. The items of teamwork abilities, communication skills, good work ethic, knowledge and skills of public health, scientific research ability, accumulated medical knowledge, ability in organization and coordination and management, were categorized into the components of teamwork, interpersonal communication, professionalism, health promotion and disease prevention, academic research, mastery of medical knowledge, Information and management, respectively. Each component was weighed from 1 to 9, generating a global score from 8 to 72. Higher scores indicated greater competencies. The overall scale reliability (Cronbach's alpha) of the short version (12 items) of the Chinese Clinical physicians' competency model was 0.874 with dimensions ranged from 0.737 to 0.892. The test-retest reliability examined after 2 weeks was 0.905. The validity of the short version of the Chinese Clinical physicians' competency model was also examined. The Spearman correlation coefficient with the full version (103 items) was 0.833. Correlation coefficients at the item level between the two versions of scale ranged from 0.810 to 0.975.
All confounding factors (age, gender, profession, department, marital status, relative infected by COVID-19, working location, household income, years of service, working time after the COVID-19 outbreak, and sleeping time after COVID-19) were collected using a questionnaire. For analyses, profession was classified as “physician”, “nurse”, or “public health practitioner”; department was classified as “intensive care unit”, “general ward”, or “other”; household income was classified as “≥1,00,000 Yuan/year” or below; marital status was classified as “currently married” or “currently unmarried”; working location was classified as “Hubei province” or “other”.
Participant characteristics were reported stratified by depressive or anxiety symptoms status. Continuous variables were presented as least-square means and 95% confidence intervals (CIs); categorical variables were presented as counts and percentages. Logistic regression models were used to estimate the associations between one standard deviation increase in clinicians' competency scores, and the prevalence of depressive and anxiety symptoms. Odds ratios (ORs) and 95% CIs were calculated. The crude model was used to calculate the crude OR (95% CI) without any adjustments. Model 1 was adjusted for age and sex. Model 2 was further adjusted for profession, department, marital status, relative infected by COVID-19, working location, household income, years of service, working time after COVID-19, and sleeping time after COVID-19. Moreover, in order to increase analytic rigor, we also conducted the Benjamini-Hochberg procedure to calculate adjusted P-values. All analyses were performed using the Statistical Analysis System 9.3 edition for Windows (SAS Institute Inc., Cary, NC, USA). All P-values were two-tailed, and P-values < 0.05 were considered statistically significant.
Among 623 participants, the prevalence of depressive, anxiety, and comorbid depressive and anxiety symptoms was 40.93, 31.78, and 26.00%, respectively. The mean age was 33.93 (95% CI: 33.74–34.49) years.
Participant characteristics are presented in Tables 1, 2, divided by depressive and anxiety symptoms status, respectively. Participants with depressive or anxiety symptoms had lower clinicians' competency scores. Participants with depressive symptoms tended to be younger (P = 0.01), not married (P = 0.03), and have a shorter length of service (P = 0.01). Moreover, participants with anxiety symptoms were more likely to be men (P = 0.02), younger (P < 0.01), working at departments other than intensive care or general wards (P < 0.001), based in provinces other than Hubei (P < 0.001), with a shorter length of service (P < 0.01), and a higher likelihood of having a relative infected by COVID-19 (P = 0.02).
Associations between clinicians' competency scores and prevalence of depressive symptoms are presented in Table 3. Among participants with higher total competency scores, the prevalence of depressive symptoms was lower. The multivariate-adjusted OR (95% CI) for depressive symptoms per one standard deviation increase in total scores of competencies was 0.67 (0.55–0.81). Furthermore, subgroup analyses stratified by eight core competency categories revealed similar associations as the total score. After corrected for multiple comparisons, the results were not changed.
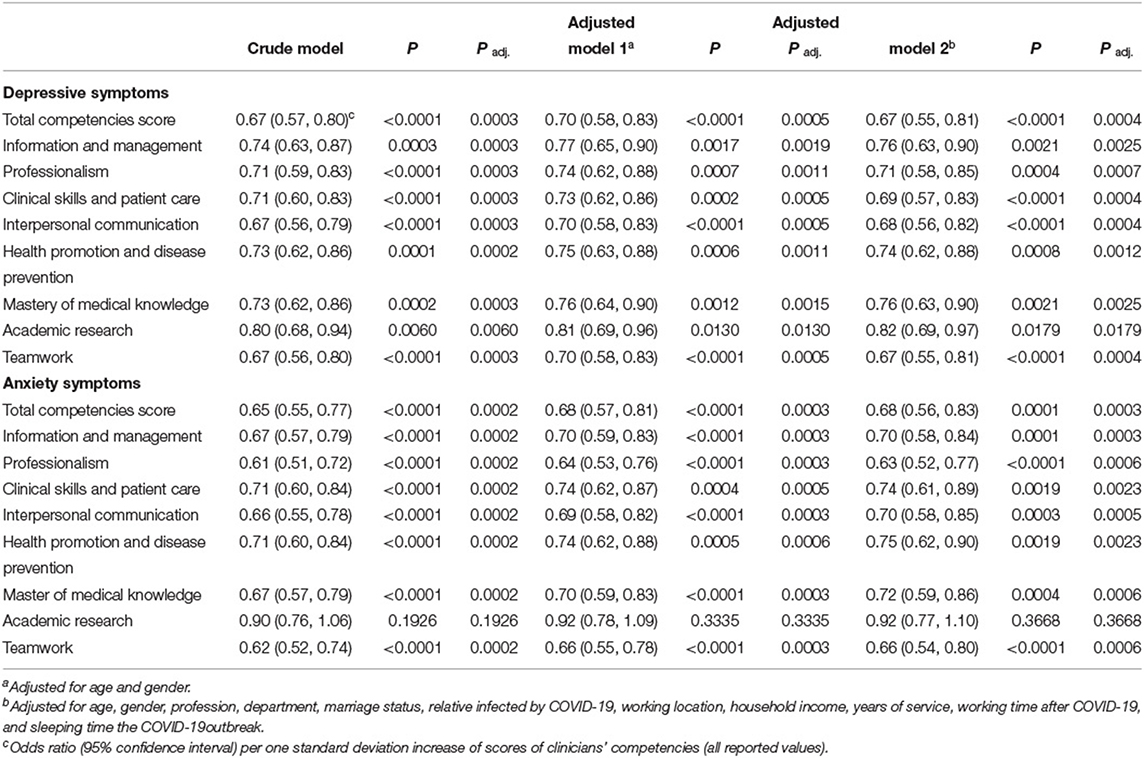
Table 3. Associations between competencies, anxiety, and depressive symptoms among frontline medical staff during the COVID-19 outbreak.
As shown in Table 3, total clinicians' competency scores were negatively associated with the prevalence of anxiety symptoms. After adjustments for confounding factors, the OR (95% CI) for anxiety symptoms per one standard deviation increase in the total competency score was 0.68 (0.56–0.83). Moreover, scores on seven core competency categories (all except academic research) were negatively associated with the prevalence of anxiety symptoms. After corrected for multiple comparisons, the results were not changed.
We examined associations between clinicians' competency scores and comorbid anxiety and depressive symptoms (Table 4). Among participants with higher total competency scores, the prevalence of comorbid anxiety and depressive symptoms was lower than among their counterparts. The OR (95% CI) for comorbid anxiety and depressive symptoms per one standard deviation increase in total clinicians' competency score was 0.68 (0.55–0.83). Seven core competency categories (all except academic research) were negatively associated with the prevalence of comorbid anxiety and depressive symptoms. After corrected for multiple comparisons, the results were not changed.
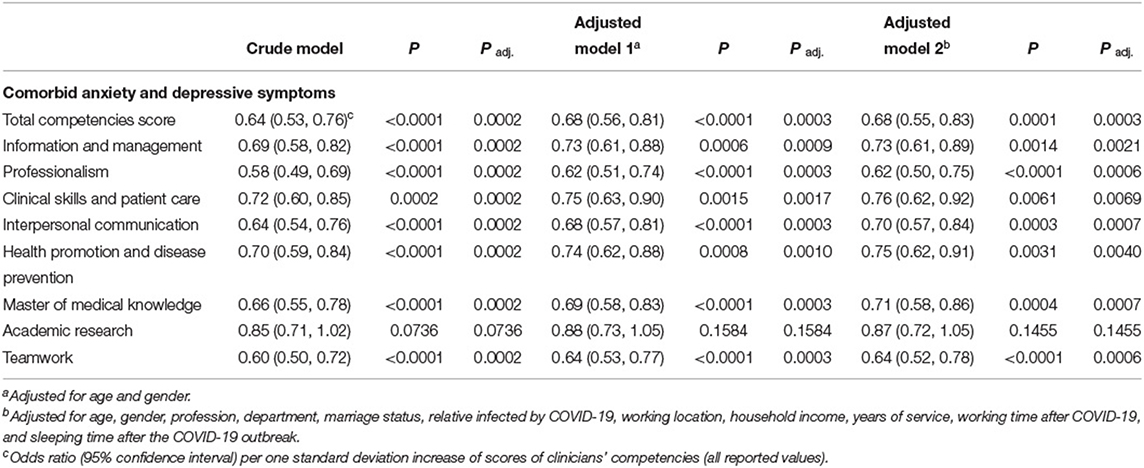
Table 4. Associations between competencies, and comorbid anxiety and depressive symptoms among frontline medical staff during the COVID-19 outbreak.
To the best of our knowledge, the present study is the first study to explore the associations between competencies and mental health symptoms among frontline healthcare workers fighting against the COVID-19 outbreak. Mental health problems, including depressive, anxiety, and comorbid depressive and anxiety symptoms are highly prevalent in frontline healthcare workers. Our findings suggest that higher competency scores are associated with lower prevalence of depressive, anxiety, and comorbid depressive and anxiety symptoms. Subgroup analyses stratified by different domains of competencies yielded results similar to the results of the main analyses.
It is well established that the outbreak of severe infectious diseases may exert adverse psychological impact on ordinary people and healthcare staff. A number of studies have confirmed that medical staff suffered mental illnesses during the outbreak of SARS in 2003 (14–16). The present findings suggest that frontline healthcare workers with depressive and anxiety symptoms tend to be younger and have a shorter length of service. The risk of depressive and anxiety symptoms appears to be influenced by frontline healthcare workers' age and length of service (35, 36). Possible factors that account for these findings are age- and service duration-related decrease in emotional responsiveness, and increase in emotional control and psychological resilience.
In the present study, the prevalence of depressive, anxiety, and comorbid depressive and anxiety symptoms among Chinese frontline medical workers fighting against the COVID-19 outbreak was 40.93, 31.78, and 26.00%, respectively, which was higher than reported peacetime estimates as well as estimates from the initial phase of the SARS epidemic (37–41). A previous study conducted in southern China has reported that 28.13% of physicians had depressive symptoms, 25.67% had anxiety symptoms, and 19.01% had comorbid depressive and anxiety symptoms (38). Another study has explored the impact of the SARS epidemic on healthcare workers in Taiwan, reporting the prevalence of depressive symptoms at 17.3% during the SARS epidemic (41). In a recent multi-center survey, high prevalence of depressive (50.7%) and anxiety (44.7%) symptoms of frontline medical workers has been reported during the COVID-19 outbreak in China (21). Mental health problems among medical staff might hinder their professional performance and affect the quality of response to COVID-19. Concurrently, deterioration in medical workers' wellbeing is likely to negatively affect on patients and professionals' overall health. Protecting mental health of medical staff is crucial for epidemic control and maintaining staff wellbeing.
In recent years, clinical core competencies, including clinical skills and patient care, mastery of medical knowledge, health promotion and disease prevention, information and management, professionalism, interpersonal communication, academic research, and teamwork have played a key role in defining medical staff's ability worldwide (42–45). High competency scores indicate good clinical performances.
Moreover, the present study found that lower competency scores have been associated with increased prevalence of anxiety, depressive, and comorbid anxiety and depressive symptoms. Competency scores were negatively associated with the prevalence of mental health problems among frontline medical staff. These findings suggest that improving core competencies among frontline medical workers coping with the epidemic might help contain the spread of COVID-19. To control the epidemic, health authorities would ensure that frontline workers are competent and equipped with up-to-date knowledge and information.
To the best of our knowledge, the present study is the first to use a competency-based survey to investigate the associations between core competency scores and the prevalence of mental health problems among frontline medical workers. The present findings highlight the importance of clinicians' competencies in maintaining mental health. Suitable training should be provided to frontline medical workers. Nevertheless, this study has several limitations, which should be considered when interpreting its findings. Firstly, the cross-sectional design of the present study limits discussions about causality and generalizability of the findings. For example, participants with worse mental health may assess their competencies more negatively. Secondly, the use of an online survey might have resulted in a biased participant sample. However, given the high transmission rate of the virus, which has restricted the opportunities to conduct face-to-face surveys, WeChat-based survey programme Questionnaire Star has been widely implemented in China (21). Thirdly, unmeasured confounding factors might have affected the observed findings. Fourthly, in the present study, considering the heavy work for the frontline medical staff in the early stage of COVID-19 outbreak, we used a short version of the Chinese Clinical physicians' competency model to evaluate the competencies. Even though the short version has been validated in medical staff (including doctor, nurse and other types of medical staff), comparing to the full version, it cannot reflect all the characteristics of frontline medical staff's competencies. Fifthly, due to the COVID-19 pandemic isolation regulations and the risk of virus transmission, a self-reported clinical competency scale was used in the present study. Even though the scale showed decent reliability and validity, due to the nature of self-reported questionary, recall bias and reporting bias exist and the associations between clinical competency and depression may be overestimated. Future cohort studies with objective assessments of clinical competencies are needed to classify the results.
In conclusion, mental health problems associated with core competencies are highly prevalent among frontline medical workers combating the COVID-19 outbreak. Protecting mental health of medical workers is of great importance for epidemic control. Our study has highlighted the importance of clinicians' core competencies in maintaining staff well-being during an epidemic. Providing additional training to frontline medical staff might help prevent the onset of mental health problems and make efforts to contain COVID-19. To address the COVID-19 epidemic, health authorities would ensure competent staff, equipped with up-to-date information are volunteered to combat in the frontline.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of Shengjing Hospital of China Medical University. The patients/participants provided their written informed consent to participate in this study.
QC and YZ designed the study and formulated the clinical question. YZ had full access to all data in the study and is responsible for data integrity and the accuracy of data analysis. All authors collected, managed, analyzed the data, prepared, reviewed, revised, and read and approved the final manuscript.
This work was supported by the National Key R&D Program of China (No. 2017YFC0907404 to YZ), Liaoning Revitalization Talents Program (No. XLYC1802095 to YZ), the Science and Technology Project of Liaoning Province (No. 2019JH6/10400002 to YZ), the Young Faculty support program of China Medical University (No. QGRA2018002 to QC), the Natural Science Foundation of Liaoning Province of China (No. 2020-MS-184 to QC), the 345 Talent Project of Shengjing Hospital of China Medical University (No. M0715 to QC), and the Young Talents of Education Ministry of Liaoning Province (No. QN2019011 to HS).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ribeiro EM, Alves M, Costa J, Ferreira JJ, Pinto FJ, Caldeira D. Safety of coffee consumption after myocardial infarction: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. (2020) 30:2146–58. doi: 10.1016/j.numecd.2020.07.016
2. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. (2020) 382:1199–207. doi: 10.1056/NEJMoa2001316
3. Day M. Covid-19: surge in cases in Italy and South Korea makes pandemic look more likely. BMJ. (2020) 368:m751. doi: 10.1136/bmj.m751
4. The Lancet. COVID-19: too little, too late? Lancet. (2020) 395:755. doi: 10.1016/S0140-6736(20)30522-5
5. Xu X, Hu J, Song N, Chen R, Zhang T, Ding X. Hyperuricemia increases the risk of acute kidney injury: a systematic review and meta-analysis. BMC Nephrol. (2017) 18:27. doi: 10.1186/s12882-016-0433-1
6. Borghi C, Rosei EA, Bardin T, Dawson J, Dominiczak A, Kielstein JT, et al. Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens. (2015) 33:1729–41; discussion 1741 doi: 10.1097/HJH.0000000000000701
7. Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. (2020) 88:916–9. doi: 10.1016/j.bbi.2020.03.007
8. Xiang YT, Jin Y, Wang Y, Zhang Q, Zhang L, Cheung T. Tribute to health workers in China: A group of respectable population during the outbreak of the COVID-19. Int J Biol Sci. (2020) 16:1739–40. doi: 10.7150/ijbs.45135
9. Chen H, Sun L, Du Z, Zhao L, Wang L. A cross-sectional study of mental health status and self-psychological adjustment in nurses who supported Wuhan for fighting against the COVID-19. J Clin Nurs. (2020) 29:4161–70. doi: 10.1111/jocn.15444
10. Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. (2020) 11:386. doi: 10.3389/fpsyt.2020.00386
11. Xiang YT Yu X, Ungvari GS, Correll CU, Chiu HF. Outcomes of SARS survivors in China: not only physical and psychiatric co-morbidities. East Asian Arch Psychiatry. (2014) 24:37–8.
12. Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. (2004) 185:127–33. doi: 10.1192/bjp.185.2.127
13. Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
14. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. (2007) 52:241–7. doi: 10.1177/070674370705200406
15. Tam CW, Pang EP, Lam LC, Chiu HF. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. (2004) 34:1197–204. doi: 10.1017/S0033291704002247
16. Grace SL, Hershenfield K, Robertson E, Stewart DE. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. (2005) 46:385–91. doi: 10.1176/appi.psy.46.5.385
17. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
18. Zhou Y, Ding H, Zhang Y, Zhang B, Guo Y, Cheung T, et al. Prevalence of poor psychiatric status and sleep quality among frontline healthcare workers during and after the COVID-19 outbreak: a longitudinal study. Transl Psychiatry. (2021) 11:223. doi: 10.1038/s41398-020-01190-w
19. Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
20. Garrouste-Orgeas M, Perrin M, Soufir L, Vesin A, Blot F, Maxime V, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. (2015) 41:273–84. doi: 10.1007/s00134-014-3601-4
21. Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e17–8. doi: 10.1016/S2215-0366(20)30077-8
22. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
23. Holmboe ES, Call S, Ficalora RD. Milestones and competency-based medical education in internal medicine. JAMA Intern Med. (2016) 176:1601–2. doi: 10.1001/jamainternmed.2016.5556
24. McClelland DC. Testing for competence rather than for “intelligence”. Am Psychol. (1973) 28:1–14. doi: 10.1037/h0034092
25. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
26. Hung KKC, Mashino S, Chan EYY, MacDermot MK, Balsari S, Ciottone GR, et al. Health workforce development in health emergency and disaster risk management: the need for evidence-based recommendations. Int J Environ Res Public Health. (2021) 18:3382. doi: 10.3390/ijerph18073382
27. Hsu EB, Thomas TL, Bass EB, Whyne D, Kelen GD, Green GB. Healthcare worker competencies for disaster training. BMC Med Educ. (2006) 6:19. doi: 10.1186/1472-6920-6-19
28. Song S, Li X, Bell SA, Yang X, Zhang W, Shanghai C, et al. Emergency response: a cross-sectional study of core competencies for nurses regarding major infectious disease outbreaks. J Emerg Nurs. (2021) 47:902–13. doi: 10.1016/j.jen.2021.04.010
29. Li H, Dong S, He L, Wang R, Long S, He F, et al. Nurses' core emergency competencies for COVID-19 in China: a cross-sectional study. Int Nurs Rev. (2021) 68:524–32. doi: 10.1111/inr.12692
30. Karnjus I, Prosen M, Licen S. Nurses' core disaster-response competencies for combating COVID-19-A cross-sectional study. PLoS ONE. (2021) 16:e0252934. doi: 10.1371/journal.pone.0252934
31. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
32. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
33. Liu Z, Tian L, Chang Q, Sun B, Zhao Y. A competency model for clinical physicians in China: a cross-sectional survey. PLoS ONE. (2016) 11:e0166252. doi: 10.1371/journal.pone.0166252
34. Liu Z, Zhang Y, Tian L, Sun B, Chang Q, Zhao Y. Application of latent class analysis in assessing the competency of physicians in China. BMC Med Educ. (2017) 17:208. doi: 10.1186/s12909-017-1039-4
35. Kessler RC, Foster C, Webster PS, House JS. The relationship between age and depressive symptoms in two national surveys. Psychol Aging. (1992) 7:119–26. doi: 10.1037/0882-7974.7.1.119
36. Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. (2000) 30:11–22. doi: 10.1017/S0033291799001452
37. Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association between physician depressive symptoms and medical errors: a systematic review and meta-analysis. JAMA Netw Open. (2019) 2:e1916097. doi: 10.1001/jamanetworkopen.2019.16097
38. Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. (2015) 314:2373–83. doi: 10.1001/jama.2015.15845
39. Gong Y, Han T, Chen W, Dib HH, Yang G, Zhuang R, et al. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS ONE. (2014) 9:e103242. doi: 10.1371/journal.pone.0103242
40. Wang JN, Sun W, Chi TS, Wu H, Wang L. Prevalence and associated factors of depressive symptoms among Chinese doctors: a cross-sectional survey. Int Arch Occup Environ Health. (2010) 83:905–11. doi: 10.1007/s00420-010-0508-4
41. Lu YC, Shu BC, Chang YY, Lung FW. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom. (2006) 75:370–5. doi: 10.1159/000095443
42. Natesan P, Batley NJ, Bakhti R, El-Doueihi PZ. Challenges in measuring ACGME competencies: considerations for milestones. Int J Emerg Med. (2018) 11:39. doi: 10.1186/s12245-018-0198-3
43. Santen SA, Hemphill RR, Pusic M. The responsibility of physicians to maintain competency. JAMA. (2020) 323:117–8. doi: 10.1001/jama.2019.21081
44. Daouk-Oyry L, Zaatari G, Sahakian T, Rahal Alameh B, Mansour N. Developing a competency framework for academic physicians. Med Teach. (2017) 39:269–77. doi: 10.1080/0142159X.2017.1270429
Keywords: COVID-19, competency, frontline staff, medical staff, mental health
Citation: Chang Q, Su H, Xia Y, Gao S, Zhang M, Ma X, Liu Y and Zhao Y (2022) Association Between Clinical Competencies and Mental Health Symptoms Among Frontline Medical Staff During the COVID-19 Outbreak: A Cross-Sectional Study. Front. Psychiatry 13:760521. doi: 10.3389/fpsyt.2022.760521
Received: 18 August 2021; Accepted: 22 March 2022;
Published: 26 April 2022.
Edited by:
Paul Stokes, King's College London, United KingdomReviewed by:
Jing-Xu Chen, Peking University, ChinaCopyright © 2022 Chang, Su, Xia, Gao, Zhang, Ma, Liu and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuhong Zhao, emhhb3l1aG9uZ0Bzai1ob3NwaXRhbC5vcmc=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.