- 1Freemasons Centre for Male Health and Wellbeing, South Australian Health and Medical Research Institute, School of Medicine, The University of Adelaide, Adelaide, SA, Australia
- 2School of Psychology, The University of Adelaide, Adelaide, SA, Australia
- 3Department of Cardiology, Basil Hetzel Institute, The Queen Elizabeth Hospital, Adelaide, SA, Australia
- 4Department of Psychiatry, University of Münster, Münster, Germany
- 5Department of Psychiatry, Melbourne Medical School, The University of Melbourne, Melbourne, VIC, Australia
- 6The Florey Institute of Neuroscience and Mental Health, The University of Melbourne, Parkville, VIC, Australia
- 7Department of Psychology, University of Kentucky, Lexington, KY, United States
- 8Department of Clinical Psychology and Psychotherapy, Institute of Psychology and Education, Ulm University, Ulm, Germany
- 9School of Psychology, The University of New England, Armidale, NSW, Australia
Objective: The aim of the Cardiovascular Health in Anxiety and Mood Problems Study (CHAMPS) is to pilot the Unified Protocol (UP) for the transdiagnostic treatment of depression and anxiety disorders in patients recently hospitalized for cardiovascular diseases (CVDs) and evaluate the feasibility.
Methods: The present study is a controlled, block randomized pragmatic pilot-feasibility trial incorporating qualitative interview data, comparing UP (n = 9) with enhanced usual care (EUC, n = 10). Eligible trial participants had a recent CVD-cause admission and were above the severity threshold for depression or anxiety denoted by Patient Health Questionnaire (PHQ-9) total scores ≥10 and/or Generalized Anxiety Disorder (GAD-7) total scores ≥7 respectively on two occasions, and met criteria for one or more depression or anxiety disorders determined by structured clinical interview. Study outcomes were analyzed as intention-to-treat using linear mixed models and qualitative interview data were analyzed with content analysis.
Results: Quantitative and qualitative measured indicated acceptability of the transdiagnostic CBT intervention for CVD patients with depression or anxiety disorders. Satisfaction with UP was comparable to antidepressant therapy and higher than general physician counseling. However, there were difficulties recruiting participants with current disorders and distress on two occasions. The UP was associated with a reduction in total number of disorders determined by blinded raters. Linear mixed models indicated that a significantly greater reduction in anxiety symptoms was evident in the UP group by comparison to the EUC group (GAD-7, p between groups = 0.011; Overall Anxiety Severity and Impairment Scale, p between groups = 0.013). Results favored the UP group by comparison to EUC for change over 6 months on measures of physical quality of life and harmful alcohol use. There was no difference between the two groups on changes in depression symptoms (PHQ-9), stress, metacognitive worry beliefs, physical activity, or adherence.
Discussion: In conclusion, this feasibility trial indicates acceptability of transdiagnostic CBT intervention for CVD patients with depression or anxiety disorders that is tempered by difficulties with recruitment. Larger trials are required to clarify the efficacy of transdiagnostic depression and anxiety disorder CBT in populations with CVDs and depressive or anxiety disorders.
Clinical Trial Registration: https://www.australianclinicaltrials.gov.au/anzctr/trial/ACTRN12615000555550, identifier: ACTRN12615000555550.
Background
Depressive disorders are prevalent in 10–15% of the population with cardiovascular diseases (CVD) such as coronary heart disease and heart failure (1, 2). Comorbid depression in patients with CVD portends an increased risk for morbidity and mortality (3, 4) and higher healthcare costs (5). To date, antidepressant and cognitive-behavioral therapy (CBT) interventions have resulted in significant reductions in depression symptoms, albeit inconsistent reductions on major adverse cardiac outcomes (MACE) (6, 7). One limitation of past interventions is the predominant focus on depression in isolation of other psychosocial risk factors. Psychosocial risk factors for CVD tend to cluster together within individuals or groups (8–10). These interrelated psychosocial factors include anxiety disorders, hostility, anger, stress, worry, rumination, anxiety sensitivity, phobic anxiety, distress tolerance, and the specific combination of negative affect and social inhibition (11–17). Anxiety disorders in particular are associated with onset of CVD and adverse cardiovascular prognosis (18–22). Moreover, anxiety disorders have high concurrent and lifetime comorbidity rates with depression disorders in the general population (23) and those with CVD (15, 24). Collectively, these findings point to the likelihood that common processes underlying negative emotions generally elevate CVD risk and vice versa (12). This raises the possibility that an intervention transcending diagnostic boundaries, targeting core emotional processes, would be a step toward improving mental health interventions amongst CVD populations.
Indeed, parallel trends in clinical psychology are exploring the tenet that CBT interventions transcending diagnostic boundaries may offer advantages over disorder-specific treatments (25, 26). For example, transdiagnostic interventions may be more appropriate in the common clinical situation of comorbid disorders, without the need to prioritize one disorder over another (i.e., selecting one single-disorder protocol over another) (27). To date, few studies have examined transdiagnostic CBT interventions for depression and anxiety disorders in CVD populations. A RCT of meta-cognitive therapy in cardiac rehabilitation patients showed that results favored the meta-cognitive therapy arm for reduction in Hospital Anxiety and Depression Scale total score at 4 and 12 months post-intervention compared to usual care (standardized effect size 0.52 and 0.33 respectively) (28). Moreover, transdiagnostic approaches have been successfully applied to other health conditions including functional gastrointestinal diseases (29, 30), cancer (31), HIV (32), headache (33).
The aim of the Cardiovascular Health in Anxiety and Mood Problems Study (CHAMPS) is to prospectively study the feasibility and acceptability of the Unified Protocol (UP) for the Transdiagnostic Treatment of Emotional Disorders (34) in patients with a recent CVD hospitalization and comorbid depression or anxiety disorder. A feasibility study is considered preliminary work undertaken to estimate important parameters necessary for the design of a larger clinical trial.
Methods
Study Design
This prospective study is a feasibility randomized controlled trial, of parallel design, comparing the UP for emotional disorders vs. enhanced usual care (EUC). A trial protocol was registered (ACTRN12615000555550) and summarized elsewhere (35). This study was approved by Human Research Ethics Committee of the Queen Elizabeth Hospital (Approval #HREC/15/TQEH47). A power calculation was not performed for this feasibility trial with the self-rated outcome measures collected to provide the standard deviation of patient outcomes which is necessary to perform a power calculation in a larger and more definitive trial.
Study Population
Participant eligibility criteria were: (1) age ≥ 18 years; (2) a primary hospital admission for CVD (specified by relevant International Classification of Disease codes (36) for myocardial infarction, coronary revascularization, symptomatic coronary disease, heart failure, heart valve disease, atrial or ventricular arrhythmia); (3) above the threshold for depression and/or anxiety denoted by Patient Health Questionnaire (PHQ-9) total scores ≥10 (37) and/or Generalized Anxiety Disorder (GAD-7) total scores ≥7 (38) respectively on two occasions (index admission and 2 weeks later); and a MINI International Neuropsychiatric Interview (MINI) 5.0.0 diagnosis of any major depression ± melancholic features, dysthymia, panic disorder, agoraphobia, social anxiety disorder, generalized anxiety disorder (GAD) or post-traumatic stress disorder (PTSD); and (4) fluency in English. Participants who were no longer above the threshold for depression and anxiety symptoms on the PHQ-9 and GAD-7 at the second assessment were invited to continue their involvement in an observational sub-study as a non-distressed control group.
Participant exclusion criteria were: (1) psychosis or bipolar disorder determined by medical history or randomization naïve assessors; (2) high suicide risk; (3) cognitive impairment or dementia impeding delivery of psychotherapy or provision of informed consent; (4) neurodegenerative condition such as Parkinson's Disease; (5) receiving psychologist or psychiatrist counseling elsewhere or psychotropic treatment at enrollment; (6) a diagnosis of drug and alcohol dependence or abuse determined by randomization naïve assessors; (7) a medical condition likely to be fatal within 1 year.
Participants were recruited from the Queen Elizabeth Hospital, a public hospital in the Western urban area of Adelaide, South Australia. Parallel to the main trial, a non-distressed control group was recruited, comprised of patients below the severity threshold for depression or anxiety denoted by PHQ-9 and GAD-7 2 weeks post-admission, or not meeting criteria for a depression or anxiety disorder specified by inclusion criterion #3 (Figure 1). The non-distressed control group were recruited to evaluate screening procedures (39) and determine longer-term symptom trajectories similar to previous trials (40), and are not described further here.
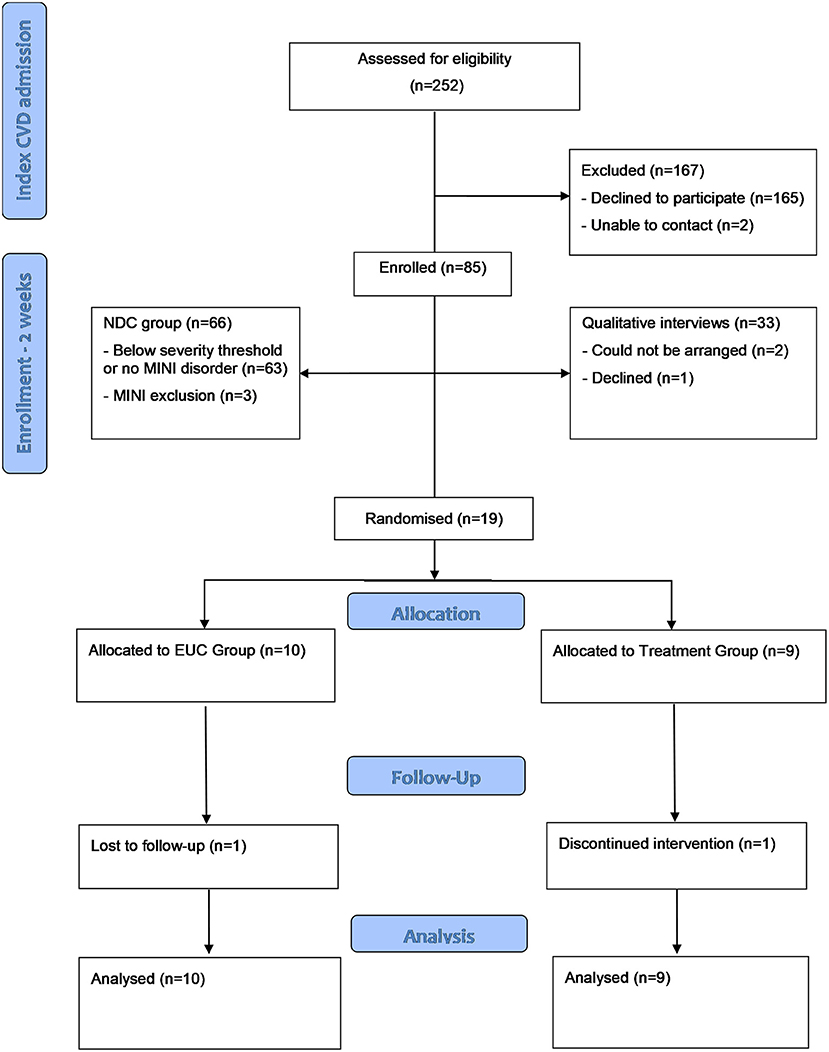
Figure 1. Flow chart of CHAMPS participants through the study. CVD, cardiovascular disease; CHAMPS, Cardiovascular health in Anxiety or Mood Problems Study; EUC, enhanced usual care; GAD-7, generalized anxiety disorder-7; MINI, MINI international Neuropsychiatric Interview; NDC, non-distressed control; PHQ, Patient Health Questionnaire; UP, unified protocol.
Protocol Deviations
In contrast to the published protocol (35), participants were only included if they met criteria for a current depression and/or anxiety disorder and had elevated symptoms on two occasions, as opposed to the original criteria of elevated symptoms ± a depression or anxiety disorder. Consequently, randomization was not stratified by primary CVD-cause admission and the target recruitment of 50 patients was revised to 20 participants due to recruitment difficulties of severe mental disorders among the CVD population as other trials have noted (41). Also, during the roll-out phase, an amendment was made to include a questionnaire measuring meta-worry, along with a qualitative sub-study. During the ethics amendment process, trial recruitment was suspended as the ethics committee mandated, for all patients with a severe depressive symptoms in the control group (i.e., PHQ-9 scores ≥ 20) at any stage of the study, that a community based acute crisis mental health triage service was contacted as part of duty of care. Similarly, for any control patients with moderate to moderately severe depressive symptoms (i.e. PHQ scores ≥10 and ≤ 19) at any stage of the study, that the patient and their general physician be notified.
Randomization and Masking
An independent statistician generated the randomization codes. Patients were block randomized according to a random number generator in alternating block sizes of four and six. After baseline measures were completed, an electronic and automated email was sent to the clinical trial manager containing a code for randomization to either the UP or EUC. In psychotherapy trials, the patients, therapist, and clinical trial manager are aware of treatment allocation. The research assistants who performed the assessments, data extraction and entry remained blind to treatment allocation through all stages of the study and follow-up.
Transdiagnostic Unified Protocol Intervention
The UP is a type of CBT explicitly designed to address the full range of emotional disorders (anxiety, depressive, and related disorders) by targeting core and underlying emotional processes that lead to the development and maintenance of symptoms across disorders. The UP was designed by Barlow et al. for weekly and face-to-face delivery up to a maximum of 18 weeks (42). The UP comprises eight modules: (1) enhancing motivation for change and treatment engagement, (2) facilitating better understanding of patients' emotional experiences, (3) increasing present focused emotion awareness, (4) increasing cognitive flexibility, (5) identifying and preventing patterns of emotion avoidance and maladaptive emotion driven behaviors, (6) increasing awareness and tolerance of emotion-related physical sensations, (7) interoceptive and situation-based emotion focused exposure, and (8) the final module was devoted to summarizing the relevant techniques attained and developing relapse prevention strategies. Owing to the highly medicalized nature of treating anxiety and depression in CVD populations and patient preference for shorter therapies (43), during piloting we refined the UP from 18 sessions, covering 8 modules (and the preliminary module), down to 12 sessions, opting for 50 to 90 min weekly sessions (see eSupplement1 in Supplementary Material). An experienced psychologist (CGB), who was trained in both the manualized UP (42) and on common CVDs, delivered the intervention. Intervention fidelity was maintained by weekly supervision with a senior psychologist and discussion of cases.
Enhanced Usual Care
Patients randomized to the EUC group received an education package which was delivered by the clinical trial manager, consisting of the beyondblue® fact sheet regarding anxiety, depression and coronary heart disease (44), conforming with the National Heart Foundation of Australia's® guidelines (37). Participants and their general physician were informed of the baseline depression severity results and directed to available clinical services (psychologist, psychiatrist, telephone counseling), advising participants to seek assistance for achieving mental wellbeing. As abovementioned, additional duty of care practices and general physician notification was implemented for patients with depressive symptoms at the request of the ethics committee. There were no other restrictions placed on usual care.
Procedure
Potentially eligible patients were identified 1–4 days after the index CVD admission by the clinical trial manager in the cardiology department. Eligible and consenting participants underwent a basic screening procedure consisting of the PHQ-9 and GAD-7. Participants were re-assessed at 2 weeks post-index CVD admission to complete the PHQ-9, GAD-7, and a structured clinical interview to confirm symptom severity and study eligibility, as well as complete the baseline patient rated measures (see eSupplement 2 in Supplementary Material). After confirmation of study eligibility and completion of baseline study measures, the allocation was revealed to the clinical trial manager, and arrangements made for either the UP or EUC arm. Patients ineligible for the trial at 2 weeks due to low symptom severity on the PHQ-9 or GAD-7 were invited to participate in the non-distressed control group. The qualitative sub-study sampled equally from the UP, EUC, and non-distressed control group.
Patient Rated Measures
The complete battery of measures and their timing of assessment is described in eSupplement 2 in Supplementary Material.
Generalized Anxiety Symptoms
The GAD-7 approximates Diagnostic and Statistical Manual 5 (DSM-5) criteria for GAD (45). The GAD-7 is scored on a scale of 0–3 (not at all, several days, more days than half the days, and nearly every day). The GAD-7 is considered valuable for use the detection of anxiety disorders in medical and primary care populations because the measure does not contain any somatic items (45). The GAD-7 severity threshold for clinically relevant symptoms are total GAD scores ≥ 7 (38) which has favorable validity to identify depression and anxiety disorders in medical patients (38).
Anxiety Severity
The Overall Anxiety Severity and Impairment Scale (OASIS) was developed as a self-report measure that assesses clinical severity and functional impairment of anxiety disorders (46, 47). Participants respond to 5 items that best describe their experience on a five-point scale (0, little or none; 1, mild; 2, moderate; 3, severe; 4, extreme). Scores >8 are indicative of severe anxiety in primary care and psychiatric samples (47).
Depression Symptoms
The PHQ-9 is a standardized instrument that incorporates DSM-5 major depression disorder criteria (48). Each item of the PHQ-9 is scored from 0 to 3, with scores ranging from 0 to 27. Scores of 10, 15, and 20 represent the thresholds for moderate-, moderately severe-, and severe-depression respectively (48). The PHQ-9 is recommended for depression screening in CVD populations because of its specificity to detect depression and sensitivity to clinical change (14, 37, 49).
Stress
The Depression, Anxiety and Stress Scales (DASS-21) is a 21 item measure validated in adults to age 90 years (50, 51). Scores range from 0 to 21 for the stress subscale with higher scores denoting higher stress symptoms. The DASS-21 factor structure approximates a tripartite structure, with stress broadly indicative of negative affectivity shared between depression and anxiety disorders (52).
Meta-Cognitions
The Metacognitions about Symptoms Control Scale (MaSCS) assesses metacognitive beliefs pertaining to symptoms in chronic health conditions (53). The MaSCS is a 17-item questionnaire, asking participants to rate on a 4-point Likert scale (1 = Do not agree, 4 = Agree strongly) how much a statement applies to them (e.g., “If I focus on the symptom, I can take the appropriate action to get better”). In line with conceptualizations of meta-worry, the MaSCS has two subscales, one each tapping into positive metacognitive worry beliefs and negative metacognitive worry beliefs. The MaSCS was developed for a variety of chronic conditions. The MaSCS instructions were adapted to state “This scale is concerned with how people with cardiovascular disease experience and cope with their symptoms.”
Quality of Life and Health Behaviors
Quality of life (QOL) was assessed with the 12-item short-form health survey (SF-12) (54). The SF-12 is one of the most commonly utilized and generalizable measures of QOL in general populations as well as CVD populations (55). The SF-12 sub-scale scores were arranged into the Physical Components Scale (PCS) and Mental Components Scale (MCS) in accordance with the manual. The PCS and MCS are weighted summary scales (range width 0–100) with higher scores representing higher QOL.
Behavioral factors such as alcohol use and smoking are pertinent to cardiovascular functioning, and are potential emotion-driven behaviors under the UP conceptualization of responses to anxiety and depression. Harmful alcohol use was measured by the Alcohol Use Disorders Identification Test Shortened Clinical (AUDIT-C) version which provides favorable sensitivity and specificity for the detection of problematic drinking (56). The physical activity questions from the Australian National Health Surveys was used to classify participants level of physical activity (57). Due to inconsistent reporting and missing data, it was not possible to calculate metabolic equivalents and thus only total activity (in minutes) is reported. Lifetime and current tobacco use was measured by items from the Global Adult Tobacco Survey (GATS) (58).
Adherence
Adherence was measured by 5 items from the Medical Outcomes Study Specific Adherence Scale (MOS SAS) (59). The items used in CHAMPS covered adherence to diet, exercise, stress management, cardiac rehabilitation and medication.
Mental Disorders
The MINI version 5.0.0 is a brief structured interview to diagnose common depression and anxiety disorders as well as alcohol and substance abuse and psychosis as outlined in the inclusion and exclusion criteria (60, 61). The MINI modules utilized in this study covered; major depressive disorder, major depressive disorder with melancholic features, dysthymia, hypomanic and manic episode (bi-polar I and II), panic disorder, agoraphobia, social anxiety disorder, obsessive-compulsive disorder (OCD), PTSD, alcohol dependence/abuse, substance dependence/abuse (non-alcohol), psychotic disorders, mood disorders with psychotic features, GAD, and antisocial personality disorder. Specific phobias are not assessed by the MINI 5.0.0 and the modules relating to anorexia and bulimia nervosa were omitted. Assessments were performed to determine the mental health diagnosis at baseline and remission at the end of the study by qualified junior psychologist assessors who were blinded to treatment allocation and the timing of the assessment (e.g. pre-, post).
Medical Outcomes, Intervention Acceptability and Feasibility, Qualitative Analyses
These methods are described in the eSupplement 3 in Supplementary Material.
Statistical Analysis
For participants missing any self-reported data at 18 weeks or 6 months, data were imputed to increase statistical power using multiple imputation procedures based on demographic and medical comorbidities. All analyses were performed based on intention-to-treat. Comparisons between UP and EUC were made at baseline on demographics and clinical risk factors using independent samples t-tests, Kruskal–Wallis test, and the chi-square statistic with Fisher's exact test where appropriate. Continuous data were analyzed with linear mixed models to assess between UP and EUC group differences in the change of a given variable from baseline to 6 months follow-up (62). Mixed model data assumptions were met and each mixed model specified correlated residuals within subjects, random effects with restricted maximum likelihood function, and robust covariance estimation, utilizing a random slope and random intercept. Mixed model data are reported with M ± SD at each observation point to assist with effect size estimates in future studies or meta-analyses. For depression and anxiety disorder diagnoses at 6-month follow-up, the total number of disorders were tallied to calculate the change in number of baseline and follow-up disorders. For hospital readmissions, MACE and psychiatric admissions were analyzed with the chi-square statistic with Fisher's exact test. For satisfaction with care, only descriptive statistics are reported. As a feasibility trial and largely exploratory study to help inform the power calculations of a larger trial, no adjustment was made for multiple comparisons.
Results
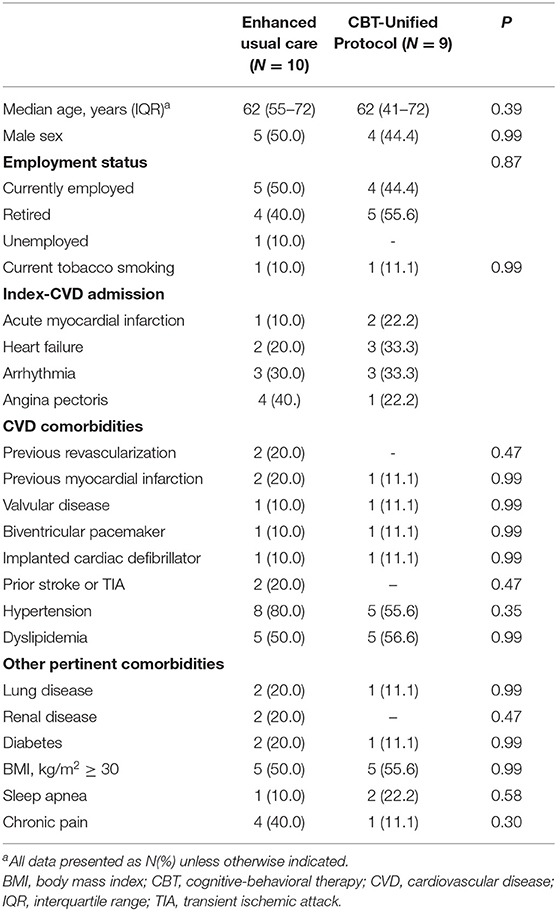
A total of 19 participants were randomized to either UP (n = 9) or EUC (n = 10). Two participants dropped out (1 from each arm) by 6 months. There were no differences between UP and EUC patients in any baseline demographic, cardiovascular or mental health variables (Tables 1, 2). The most common mental disorders at baseline were major depressive disorder, agoraphobia, and GAD. At baseline, 5 patients met criteria for 1 disorder (26.3%), 4 met criteria for 2 disorders (21.1%), 8 met criteria for 3 disorders (42.1%), and 2 met criteria for 4 disorders (10.5%).
Psychological and QOL Outcomes
The number of disorders determined by blinded MINI raters was significantly lower in the UP group by comparison to the EUC (Table 3). Linear mixed models indicated that a significantly greater reduction in anxiety symptoms was evident in the UP group by comparison to the EUC group on the GAD-7 (p between groups = 0.011) and also the Overall Anxiety Severity and Impairment Scale (p between groups = 0.013). There was no difference between the UP and EUC groups on change in depression symptoms (PHQ-9), stress (DASS-21) or metacognitive worry beliefs. There was evidence favoring the UP group for greater improvement over 6 months in physical QOL, but not mental QOL.

Table 3. Change in psychological outcomes for patients randomized to unified protocol vs. enhanced usual care.
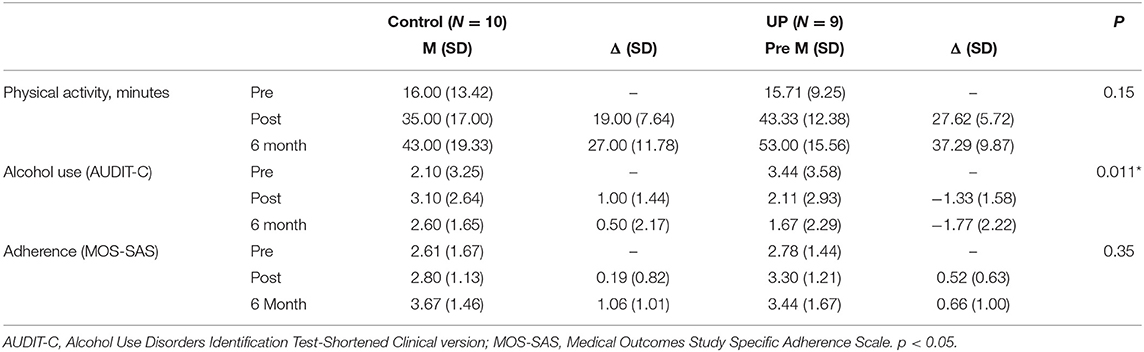
CVD Health Behaviors and Adherence
The CVD health behavior and adherence data are reported in Table 4. Linear mixed models indicated that a significantly greater reduction in harmful alcohol was evident in the UP group by comparison to the EUC group on the AUDIT-C. There were no differences between the UP group by comparison to the EUC group in physical activity or adherence. There were only two current smokers in the study and therefore GATS data was not analyzed.
Hospital Admissions
Hospital admissions for CVD causes at 6 months follow-up were comparable (UP 20.0% vs. EUC 22.2%, p = 0.99). One psychiatric admission occurred in the study (UP group 11.1% vs. EUC 0%, p = 0.47). This admission occurred in the context of concerns over cognitive function and personality change that was subsequently identified as a transient ischemic attack.
Satisfaction With Care
Participants randomized to UP reported high satisfaction with the psychologist delivered UP intervention, median satisfaction = 4 “quite a bit satisfied,” and low satisfaction with psychological care provided by their GP, median = 1 “not at all satisfied.” However, EUC participants reported equally high satisfaction with antidepressants, median satisfaction = 4 “quite a bit satisfied” and equally low satisfaction with GP psychological care, median = 1 “not at all satisfied.”
Qualitative Analysis
The CVD participants discussed numerous factors that contributed to their satisfaction or dissatisfaction with care. These were categorized into two overarching themes: characteristics of the treatment and of health professionals. Pertaining to CVD treatment, themes included identifying the problem and fixing it. Hence, accurate diagnoses and a successful outcome led to improvements in CVD symptom severity. By contrast, psychological treatment under the UP related to reducing severity, which impacted on overall satisfaction with medical care. With regard to medical professionals in general, including the psychologist, two main themes were developed. Firstly, the practitioner's personal characteristics which included subthemes of competence, efficiency, and personality. Competence was discussed in association with knowledge and expertise. Finally, being caring, helpful, and kind were crucial elements of practitioners' personal characteristics. The second theme pertaining to medical professionals was the practitioner-patient interaction. An important subtheme was quality of communication as perceived by patients, specifically—as mentioned by nearly all participants—receiving comprehensive information. Taken altogether, for patients to be satisfied, professionals must not only be competent (i.e., have knowledge and expertise), but also communicate effectively and explain information in a caring, helpful, and kind manner. Respect for the patient was identified as a subtheme that overlapped across practitioners' personal characteristics and practitioner-patient interactions.
Discussion
This feasibility RCT showed that the UP intervention for emotional disorders was associated with greater change, by comparison to the EUC, on the total number of psychiatric disorders, anxiety, harmful alcohol use, and improvement in physical QOL. The UP was not associated with reductions in depression, stress, or metacognitive worry about symptoms. Likewise, the UP was not associated with changes in pertinent health behaviors such as physical activity level, adherence, or major hospitalization rates. As a feasibility study, the trial was not powered to detect significant clinical effects, thus all results need to be interpreted as preliminary. Moreover, there were difficulties with recruiting CVD patients who met criteria for current disorders and were distressed after the index admission which points to low feasibility of an outpatient intervention for patients with severe mental health concerns.
This study is perhaps the first CBT intervention in CVD populations to target anxiety disorders as part of its inclusion criteria. The current study indicated that the UP was associated with reductions in GAD-7 and OASIS scores, as well as cumulative number of disorders as adjudicated by blinded raters. The findings are highly significant because less is known about the treatment of anxiety disorders in CVD populations. Given that access to community mental health services is often limited to persons with a verified mental disorder (e.g., better access initiatives in Australia and Improving Access to Psychological Therapies in UK) (63, 64), the study findings support the referral of these patients with comorbid CVDs to mental healthcare professionals for transdiagnostic CBT. Indeed, as little empirical data currently exists pertaining to anxiety disorder treatment in CVD populations, it remains largely unknown whether transdiagnostic approaches are equivalent to single-disorder protocols in general (65) and in chronic diseases specifically (66). Recently, the UP has been tested in diverse health conditions including functional gastrointestinal diseases (30), cancer (31), HIV (32), and headache (33). The UP was particularly effective for emotional disorder and disease-related symptoms across multiple measures in functional gastrointestinal diseases (30), cancer (31), and HIV populations (32). Not all findings concerning the UP have been supportive, with this type of CBT found to be less effective across multiple outcomes among youth with anxiety disorders and headache (33). Similarly, in the present study there was no evidence of significant difference by comparison to EUC on depression, adherence, stress, metacognitive worry, physical activity, or adherence. The findings may raise preliminary questions of the suitability of UP to certain health conditions, or alternatively point to the need for refinements in intervention delivery and the results of larger more definitive trials.
One clinical implication of these findings is that the treatment of depressive symptoms and mental QoL in CVD may require a treatment approach other than the UP or in combination with other interventions. A recent Cochrane review (10) showed that both psychotherapy and pharmacological interventions have moderate to large effects on end of treatment depression scores though RCT evidence on the impact upon QoL remains sparse. Emerging data suggests that the sequential delivery of pharmacotherapy in the acute phase of depression and a short-term course of cognitive-behavioral therapy in the residual phase may be a suitable approach (67). Furthermore, the combination of CBT with other therapies such as wellbeing therapy could be optimal to enhance psychological wellbeing and improve quality of life (68, 69).
There is limited use of transdiagnostic interventions in CVD populations however past interventions have utilized collaborative care to treat depression and anxiety symptoms simultaneously in CVDs. For example, the Management of Sadness and Anxiety in Cardiology (MOSAIC) RCT (70) screened patients with the PHQ-9, GAD-7, and a panic-attack questionnaire to enroll participants into a multicomponent collaborative care intervention. Contrasting to the current findings, the MOSAIC trial showed that participants exposed to the intervention displayed significant reductions in depressive but not anxiety symptoms (70). A possible explanation is that the EUC group here were provided with enhanced monitoring at the recommendation of the ethics committee, though large trials have called into question the effectiveness of depression screening in patients with CVD (71). An alternative explanation is that the UP intervention group consisted of patients with GAD, panic disorder, agoraphobia, social anxiety disorder, OCD and PTSD, whereas the MOSAIC trial did not report anxiety disorder prevalence other than for GAD-7 symptom severity and responses to the panic attack screening question.
CBT may lead to improvements in health behaviors and adherence pertinent to CVD. A past CBT intervention combined with motivational interviewing as part of cardiac rehabilitation led to improvements in physical activity, dietary fat intake, medication adherence, and smoking abstinence (72). Here there was only a reduction in harmful alcohol intake, thus paralleling a transdiagnostic CBT intervention for eating disorders that led to reductions in alcohol intake (73). Concomitant reductions in harmful alcohol intake are theorized to relate to the UP's modules covering emotion-driven behaviors, which may include alcohol and illicit drug intake, smoking, and binge-eating behaviors pertinent to cardiovascular health (27). However, we emphasize that there is insufficient data from our trial to support the UP as a means to target binge-eating and smoking.
Participants randomized to UP reported high satisfaction with the psychologist delivered CBT intervention though this level of satisfaction was comparable to the EUC groups rating of satisfaction with antidepressants. In both cases, satisfaction with UP or antidepressants was higher than general physician counseling for mental health. The qualitative interviews suggested that medical and psychological care was viewed as related to the practitioner's personal characteristics, which included subthemes of competence, efficiency, and personality. Respect for the patient was identified as a subtheme that overlapped across practitioners' personal characteristics and practitioner-patient interactions. However, these themes likely parallel the therapeutic alliance, which is not specific to any particular psychotherapy, whether UP or otherwise.
This study is presented with several strengths including use of a manualized and transdiagnostic CBT intervention, blinded outcome ratings, and use of qualitative interviews to determine acceptability. There are several limitations of this feasibility trial including changes to the study protocol and difficulties recruiting similar to other recent trials in the CVD population (41), which points toward low feasibility for outpatient, face-to-face, and individual therapy. Consequently, a small sample size was obtained, thereby precluding definitive conclusions on UP treatment efficacy in CVD populations. Also, the small sample size precludes stratification of the findings by sex or age. The findings will require replication in adequately powered samples and potentially more homogenous samples such as post-acute coronary syndromes where depression treatment effect sizes are well characterized. The UP intervention is designed for multiple emotional disorders, likely resulting in heterogeneity in study participants' treatment needs that may be less related to the index CVD admission. For example, though depression and anxiety frequently occur in CVD populations, it is perhaps less likely that disorders such as social anxiety disorder would result from a CVD admission. A related limitation is that only 1 patient met criteria for PTSD thus it is unknown if the UP could be extended to PTSD in CVD populations. This is an important limitation to reconcile in future research as there are few RCT interventions for PTSD in CVD populations (74).
Another limitation of this study is that implementation of usual care was not possible, and the EUC design likely resulted in a level of monitoring and treatment greatly exceeding usual depression care (75). The increased intervention in EUC could potentially explain the lack of difference in PHQ-9 scores between UP and EUC groups. This somewhat parallels the findings of the 2 × 2 factorial CREATE trial where interpersonal therapy was not superior over clinical management in terms of depression outcomes (76). Other limitations concern the procedural challenges during the roll-out and intervention phase which included recruitment postponement, as well as staff unavailability and turnover which may have contributed to acceptability, attrition, and contaminate the feasibility of the intervention. Finally, the follow-up was limited to 6 months after the intervention period and longer-term follow-up would be required to examine durability of the intervention and the impact on CVD events and psychiatric readmissions.
In conclusion, our feasibility trial indicates acceptability of transdiagnostic CBT intervention for CVD patients with depression or anxiety disorders. The feasibility trial of UP intervention suggested superiority over enhanced usual care regarding the total number of disorders, anxiety symptoms, alcohol intake, and improvements in physical QOL. CVD patients with depression and anxiety disorders however may not benefit from UP with regards to depression, mental QOL, adherence, physical activity or hospitalization rates. Satisfaction with UP was comparable to antidepressant therapy and higher than general physician counseling. Future trials of the UP in CVD populations are warranted to confirm if treatment benefits are restricted to anxiety symptoms or might extend to depressive symptoms.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee of the Queen Elizabeth Hospital (Approval #HREC/15/TQEH47). The patients/participants provided their written informed consent to participate in this study.
Champs Investigators
Linley A. Denson1, Megan Grech1, Marilyn Black2, Peter Cheung2, Alisson Barret3, Nathan Harrison3, Terina Selkow2 and Elizabeth Markwick4
1School of Psychology, University of Adelaide, Adelaide, SA, Australia; 2Department of Cardiology, Queen Elizabeth Hospital, Woodville, SA, Australia; 3Freemasons Foundation Centre for Men's Health, The University of Adelaide, Adelaide, SA, Australia; 4Department of Psychiatry, Queen Elizabeth Hospital, Woodville, SA, Australia.
Author Contributions
PT, DT, JH, JB, BB, SS-Z, HB, and GW: study design. CB and RP: data collection. PT and HB: drafting manuscript. PT, DT, JH, JB, BB, SS-Z, HB, CB, RP, SC, and GW: critical revision of manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Heart Foundation of Australia Vanguard Grant (100593) and the Menzies Foundation Allied Health Scholars Grant (AHS_004). PT was supported by the National Health and Medical Research Council of Australia (Neil Hamilton Fairley—Clinical Overseas Fellowship #1053578).
Conflict of Interest
Advisory Board—Lundbeck, Janssen-Cilag; Grant/Research Support—AstraZeneca; Sanofi, Lundbeck; Honoraria—AstraZeneca, Bristol-Myers Squibb, Lundbeck, Pfizer, Servier Laboratories, Wyeth Pharmaceuticals, Takeda, Janssen, LivaNova PLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank Marg McGee for their assistance with the study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.741039/full#supplementary-material
References
1. Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. (2006) 48:1527–37. doi: 10.1016/j.jacc.2006.06.055
2. Thombs BD, De Jonge P, Coyne JC, Whooley MA, Frasure-Smith N, Mitchell AJ, et al. Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA. (2008) 300:2161–71. doi: 10.1001/jama.2008.667
3. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. (2004) 66:802–13. doi: 10.1097/01.psy.0000146332.53619.b2
4. Samartzis L, Dimopoulos S, Tziongourou M, Nanas S. Effect of psychosocial interventions on quality of life in patients with chronic heart failure: a meta-analysis of randomized controlled trials. J Card Fail. (2013) 19:125–34. doi: 10.1016/j.cardfail.2012.12.004
5. Baumeister H, Haschke A, Munzinger M, Hutter N, Tully PJ. Inpatient and outpatient costs in patients with coronary artery disease and mental disorders: a systematic review. Biopsychosoc Med. (2015) 9:1–16. doi: 10.1186/s13030-015-0039-z
6. Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, et al. Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Eur J Prev Cardiol. (2018) 25:247–59. doi: 10.1177/2047487317739978
7. Pizzi C, Rutjes AW, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol. (2011) 107:972–9. doi: 10.1016/j.amjcard.2010.11.017
8. Pogosova N, Kotseva K, De Bacquer D, von Känel R, De Smedt D, Bruthans J, et al. (2017). Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol. (2017) 24:1371–80. doi: 10.1177/2047487317711334
9. Kozela M, Doryńska A, Bobak M, Pajak A. Accumulation of psychosocial risk factors and cardiovascular disease incidence. Prospective observation of the Polish HAPIEE cohort. Kardiol Pol. (2019) 77:535–40. doi: 10.33963/KP.14814
10. Tully PJ, Ang SY, Lee EJ, Bendig E, Bauereiß N, Bengel J, et al. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst Rev. (2021) 12:CD008012. doi: 10.1002/14651858.CD008012.pub4
11. Dreher H. Psychosocial factors in heart disease: a process model. Adv Mind Body Medicine. (2004) 20:20–31.
12. Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. (2005) 131:260–300. doi: 10.1037/0033-2909.131.2.260
13. Pogosova N, Saner H, Pedersen SS, Cupples ME, McGee S, Höfer F, et al. Psychosocial aspects in cardiac rehabilitation: From theory to practice. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Eur J Prevent Cardiol. (2015) 22:1290–306. doi: 10.1177/2047487314543075
14. Ladwig KH, Lederbogen F, Albus C, Angermann C, Borggrefe M, Fischer D, et al. Position paper on the importance of psychosocial factors in cardiology: Update 2013. German Med Sci. (2014) 12:Doc09. doi: 10.3205/000194
15. Tully PJ, Cosh SM, Baumeister H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. J Psychosom Res. (2014) 77:439–48. doi: 10.1016/j.jpsychores.2014.10.001
16. Tully PJ, Winefield H, Baker RA, Denollet J, Pedersen SS, Wittert GA, et al. Depression, anxiety and major adverse cardiovascular and cerebrovascular events in patients following coronary artery bypass graft surgery: a five year longitudinal cohort study. BioPsychoSocial medicine 9(14). (2015). doi: 10.1186/s13030-015-0041-5
17. Luberto CM, Crute S, Wang A, Yeh GY, Celano CM, Huffman JC, et al. Lower distress tolerance is associated with greater anxiety and depression symptoms among patients after acute coronary syndrome. Gen Hosp Psychiatry. (2021). doi: 10.1016/j.genhosppsych.2021.01.011
18. Phillips AC, Batty GD, Gale CR, Deary IJ, Osborn D, MacIntyre K. Generalized anxiety disorder, major depressive disorder, and their comorbidity as predictors of all-cause and cardiovascular mortality: the Vietnam experience study. Psychosom Med. (2009) 71:395–403. doi: 10.1097/PSY.0b013e31819e6706
19. Barger SD, Sydeman SJ. Does generalized anxiety disorder predict coronary heart disease risk factors independently of major depressive disorder? J Affect Disord. (2005) 88:87–91. doi: 10.1016/j.jad.2005.05.012
20. Tully PJ, Baune BT. Comorbid anxiety disorders alter the association between cardiovascular diseases and depression: the German National Health Interview and Examination Survey. Soc Psych Psychiatr Epidemiol. (2014) 49:683–91. doi: 10.1007/s00127-013-0784-x
21. Roest AM, de Jonge P, Lim CW, Stein DJ, Al-Hamzawi A, Alonso J, et al. Scott, fear and distress disorders as predictors of heart disease: a temporal perspective. J Psychosom Res. 96:67–75. doi: 10.1016/j.jpsychores.2017.03.015
22. Roest AM, Zuidersma M, de Jonge P. Myocardial infarction and generalised anxiety disorder: 10-year follow-up. Br J Psychiatry. (2012) 200:324–9. doi: 10.1192/bjp.bp.111.103549
23. Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2011) 68:90–100. doi: 10.1001/archgenpsychiatry.2010.180
24. Tully PJ, Cosh SM. Generalized anxiety disorder prevalence and comorbidity with depression in coronary heart disease: a meta analysis. J Health Psychol. (2013) 18:1601–16. doi: 10.1177/1359105312467390
25. Andersen P, Toner P, Bland M, McMillan D. Effectiveness of transdiagnostic cognitive behaviour therapy for anxiety and depression in adults: a systematic review and meta-analysis. Behav Cogn Psychother. (2016) 44:673–90. doi: 10.1017/S1352465816000229
26. Norton PJ, Roberge P. Transdiagnostic therapy. Psychiatr Clin North Am. (2017) 40:675–87. doi: 10.1016/j.psc.2017.08.003
27. Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety. (2010) 27:882–90. doi: 10.1002/da.20735
28. Wells A, Reeves D, Capobianco L, Heal C, Davies L, Heagerty A, et al. Improving the effectiveness of psychological interventions for depression and anxiety in cardiac rehabilitation: PATHWAY-A single-blind, parallel, randomized, controlled trial of group metacognitive therapy. Circulation. (2021) 144:23–33. doi: 10.1161/CIRCULATIONAHA.120.052428
29. Dear BF, Fogliati VJ, Fogliati R, Gandy M, McDonald S, Talley N, et al. Transdiagnostic internet-delivered cognitive-behaviour therapy (CBT) for adults with functional gastrointestinal disorders (FGID): a feasibility open trial. J Psychosom Res. (2018) 108:61–9. doi: 10.1016/j.jpsychores.2018.02.015
30. Mohsenabadi H, Zanjani Z, Shabani MJ, Arj A. A randomized clinical trial of the Unified Protocol for Transdiagnostic treatment of emotional and gastrointestinal symptoms in patients with irritable bowel syndrome: evaluating efficacy and mechanism of change. J Psychosom Res. (2018) 113:8–15. doi: 10.1016/j.jpsychores.2018.07.003
31. Weihs KL, McConnell MH, Wiley JF, Crespi CM, Sauer-Zavala S, Stanton AL. A preventive intervention to modify depression risk targets after breast cancer diagnosis: design and single-arm pilot study. Psycho-oncology. (2019) 28:880–7. doi: 10.1002/pon.5037
32. Parsons JT, Rendina HJ, Moody RL, Gurung S, Starks TJ, Pachankis JE. Feasibility of an emotion regulation intervention to improve mental health and reduce HIV transmission risk behaviors for HIV-positive gay and bisexual men with sexual compulsivity. AIDS Behav. (2017) 21:1540–9. doi: 10.1007/s10461-016-1533-4
33. Sharma P, Mehta M, Sagar R. Efficacy of transdiagnostic cognitive-behavioral group therapy for anxiety disorders and headache in adolescents. J Anxiety Disord. (2017) 46:78–84. doi: 10.1016/j.janxdis.2016.11.001
34. Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: protocol development and initial outcome data. Cogn Behav Pract. (2010) 17:88–101. doi: 10.1016/j.cbpra.2009.06.002
35. Tully PJ, Turnbull DA, Horowitz JD, Beltrame JF, Selkow T, Baune BT, et al. Cardiovascular Health in Anxiety or Mood Problems Study (CHAMPS): study protocol for a RCT. Trials. (2016) 17:18. doi: 10.1186/s13063-015-1109-z
36. World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision Version for 2007 (2007). Available online at http://www.who.int/classifications/apps/icd/icd10online/ (accessed September 26, 2017).
37. Colquhoun DM, Bunker SJ, Clarke DM, Glozier N, Hare DL, Hickie IB, et al. Screening, referral and treatment for depression in patients with coronary heart disease. Med J Aust. (2013) 198:483–4. doi: 10.5694/mja13.10153
38. Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psych. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
39. Grech M, Turnbull DA, Wittert GA, Tully PJ, Horowitz JD, Beltrame JF, et al. Identifying the internalizing disorder clusters among recently hospitalized cardiovascular disease patients: a receiver operating characteristics study. Front Psychol. (2019) 10:2829. doi: 10.3389/fpsyg.2019.02829
40. Rollman BL, Belnap BH, LeMenager MS, Mazumdar S, Schulberg HC, Reynolds III CF. The Bypassing the Blues treatment protocol: stepped collaborative care for treating post-CABG depression. Psychosom Med. (2009) 71:217–30. doi: 10.1097/PSY.0b013e3181970c1c
41. Bendig E, Bauereiß N, Buntrock C, Habibović M, Ebert DD, Baumeister H. Lessons learned from an attempted randomized-controlled feasibility trial on “WIDeCAD” - An internet-based depression treatment for people living with coronary artery disease (CAD). Internet Interv. (2021) 24:100375. doi: 10.1016/j.invent.2021.100375
42. Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, et al. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. New York, NY: Oxford University Press (2011).
45. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
46. Norman SB, Cissell SH, Means-Christensen AJ, Stein MB. Development and validation of an overall anxiety severity and impairment scale (OASIS). Depress Anxiety. (2006) 23:245–9. doi: 10.1002/da.20182
47. Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, et al. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS). J Affect Disord. (2009) 112:92–101. doi: 10.1016/j.jad.2008.03.014
48. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
49. Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, et al. Depression and coronary heart disease: a science advisory from the American Heart Association. Circulation. (2008) 118:1768–75. doi: 10.1161/CIRCULATIONAHA.108.190769
50. Crawford J, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychol. (2011) 46:3–14. doi: 10.1111/j.1742-9544.2010.00003.x
51. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavior Research Therapy. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
52. Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther. (1997) 35:79–89. doi: 10.1016/S0005-7967(96)00068-X
53. Fernie BA, Maher-Edwards L, Murphy G, Nikcevic AV, Spada MM. The Metacognitions about Symptoms Control Scale: development and concurrent validity. Clin Psychol Psychother. (2015) 22:443–9. doi: 10.1002/cpp.1906
54. Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
55. Muller-Nordhorn J, Roll S, Willich SN. Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart. (2004) 90:523–7. doi: 10.1136/hrt.2003.013995
56. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. (1998) 158:1789–95. doi: 10.1001/archinte.158.16.1789
57. Australian Bureau of Statistics. National Health Survey: Users' Guide. Canberra: Australian Bureau of Statistics (2003).
58. Global Adult Tobacco Survey Collaborative Group. Tobacco Questions for Surveys: A Subset of Key Questions From the Global Adult Tobacco Survey Centers for Disease Control and Prevention. Atlanta, GA: Global Adult Tobacco Survey Collaborative Group (2011).
59. Hays RD. The medical outcomes study (mos) measures of patient adherence. J Behav Med. (1994) 17:361–7.
60. Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSM-IH-R Psychotic Disorders: procedural validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. (1998) 13:26–34. doi: 10.1016/S0924-9338(97)86748-X
61. Sheehan DV, Lecrubier Y, Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59(Supplement 20):22–33.
62. Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, et al. The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry. (2017) 74:875–84. doi: 10.1001/jamapsychiatry.2017.2164
63. McGarry H, Hegarty K, Johnson C, Gunn J, Blashki G. Managing depression in a changing primary mental healthcare system: comparison of two snapshots of Australian GPs' treatment and referral patterns. Mental Health Fam Med. (2009) 6:75.
64. Clark DM. Realizing the mass public benefit of evidence-based psychological therapies: the IAPT program. Annu Rev Clin Psychol. (2018) 14:159–83. doi: 10.1146/annurev-clinpsy-050817-084833
65. Domhardt M, Geßlein H, von Rezori RE, Baumeister H. Internet- and mobile-based interventions for anxiety disorders: A meta-analytic review of intervention components. Depress Anxiety. (2019) 36:213–24. doi: 10.1002/da.22860
66. Tully PJ, Sardinha A, Nardi AE. A new CBT model of panic attack treatment in comorbid heart diseases (PATCHD): how to calm an anxious heart and mind. Cog Behav Pract. (2017) 24:329–41. doi: 10.1016/j.cbpra.2016.05.008
67. Guidi J, Tomba E, Cosci F, Park SK, Fava GA. The role of staging in planning psychotherapeutic interventions in depression. J Clin Psychiatry. (2017) 78:456–63. doi: 10.4088/JCP.16r10736
68. Rafanelli C, Gostoli S, Buzzichelli S, Guidi J, Sirri L, Gallo P, et al. Sequential combination of cognitive-behavioral treatment and well-being therapy in depressed patients with acute coronary syndromes: a randomized controlled trial (TREATED-ACS Study). Psychother Psychosom. (2020) 89:345–56. doi: 10.1159/000510006
69. Mansueto G, Cosci F. Well-being therapy in depressive disorders. Adv Exp Med Biol. (2021) 1305:351–74. doi: 10.1007/978-981-33-6044-0_19
70. Huffman JC, Mastromauro CA, Beach SR, Celano CM, Dubois CM, Healy BC, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: The Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. (2014) 174:927–36. doi: 10.1001/jamainternmed.2014.739
71. Kronish IM, Moise N, Cheung YK, Clarke GN, Dolor RJ, Duer-Hefele J, et al. Effect of depression screening after acute coronary syndromes on quality of life: CODIACS-QoL RCT. JAMA Intern Med. (2020) 180:45–53. doi: 10.1001/jamainternmed.2019.4518
72. Turner A, Murphy BM, Higgins RO, Elliott PC, Le Grande MR, Goble AJ, et al. An integrated secondary prevention group programme reduces depression in cardiac patients. Eur J Prev Cardiol. (2014) 21:153–62. doi: 10.1177/2047487312467747
73. Karacic M, Wales JA, Arcelus J, Palmer RL, Cooper Z, Fairburn CG. Changes in alcohol intake in response to transdiagnostic cognitive behaviour therapy for eating disorders. Behav Res Ther. (2011) 49:573–7. doi: 10.1016/j.brat.2011.05.011
74. Shemesh E, Annunziato RA, Weatherley BD, Cotter G, Feaganes JR, Santra M, et al. A randomized controlled trial of the safety and promise of cognitive-behavioral therapy using imaginal exposure in patients with posttraumatic stress disorder resulting from cardiovascular illness. J Clin Psychiatry. (2011) 72:168–74. doi: 10.4088/JCP.09m05116blu
75. Freedland KE, Mohr DC, Davidson KW, Schwartz JE. Usual and unusual care: existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom Med. (2011) 73:323–35. doi: 10.1097/PSY.0b013e318218e1fb
76. Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. (2007) 297:367–79. doi: 10.1001/jama.297.4.367
Keywords: depression, major depression (MDD), anxiety, anxiety disorders, cardiovascular disease, coronary heart disease, randomized controlled trial, cognitive-behavioral therapy (CBT)
Citation: Tully PJ, Turnbull DA, Horowitz JD, Beltrame JF, Baune BT, Sauer-Zavala S, Baumeister H, Bean CG, Pinto RB, Cosh S and Wittert GA (2022) Transdiagnostic Cognitive-Behavioral Therapy for Depression and Anxiety Disorders in Cardiovascular Disease Patients: Results From the CHAMPS Pilot-Feasibility Trial. Front. Psychiatry 13:741039. doi: 10.3389/fpsyt.2022.741039
Received: 14 July 2021; Accepted: 24 March 2022;
Published: 14 April 2022.
Edited by:
Marlies Elizabeth Alvarenga, Victorian Heart Institute, AustraliaReviewed by:
Jibril I. M. Handuleh, Amoud University, SomaliaGiovanni Mansueto, University of Florence, Italy
Copyright © 2022 Tully, Turnbull, Horowitz, Beltrame, Baune, Sauer-Zavala, Baumeister, Bean, Pinto, Cosh and Wittert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Phillip J. Tully, cGhpbGxpcC50dWxseUBhZGVsYWlkZS5lZHUuYXU=
 Phillip J. Tully
Phillip J. Tully Deborah A. Turnbull
Deborah A. Turnbull John D. Horowitz
John D. Horowitz John F. Beltrame
John F. Beltrame Bernhard T. Baune
Bernhard T. Baune Shannon Sauer-Zavala7
Shannon Sauer-Zavala7 Harald Baumeister
Harald Baumeister Christopher G. Bean
Christopher G. Bean Ronette B. Pinto
Ronette B. Pinto Suzie Cosh
Suzie Cosh on behalf of the CHAMPS Investigators
on behalf of the CHAMPS Investigators