- 1Department of Psychiatry and Behavioral Sciences, School of Medicine, Stanford University, Stanford, CA, United States
- 2School of Psychological Sciences, University of Melbourne, Melbourne, VIC, Australia
- 3Aspect Research Centre for Autism Practice, French's Forest, Sydney, NSW, Australia
- 4Department of Psychology, John Carroll University, University Heights, OH, United States
Autistic individuals and individuals with a range of other neurodevelopmental conditions (NDD) often present with lower levels of daily living skills (DLS) when compared to their neurotypical peers. Importantly, lower levels of DLS have been linked to a range of negative outcomes, including lower rates of post-secondary education, lower employment rates, and higher daily support needs across autism and NDD. However, there are currently no open-source informant-reported instruments for capturing key aspects of DLS. This study describes the development, refinement, and initial psychometric evaluation of a new, relatively brief (53-item). Daily Living Skills Scale (DLSS) in a sample of 1,361 children aged 2–17 years, Confirmatory Factor Analysis demonstrated an excellent fit of unidimensional model to the data (CFI = 0.953, TLI = 0.951, RMSEA = 0.073 [95% CI: 0.071–0.074]). The single-factor CFA model showed evidence of measurement invariance of factor loadings, thresholds, and residual variance (strict invariance) across sex, age, race, and ethnicity. Model reliability and internal consistency were excellent (ω = 0.98; α = 0.97). Conditional reliability estimates indicated very good reliability (= 0.80) for the total DLS scale from very low (θ = −4.2) to high (θ = +2.4) scores. Conceptually derived self-care, homecare, and community participation subscales also showed strong reliability and internal consistency. With further replication, the EFS has excellent potential for wide adoption across research and clinical contexts.
1. Introduction
In addition to core diagnostic characteristics, autistic individuals and individuals with a range of other neurodevelopmental conditions (NDD), including, but not limited to, attention-deficit hyperactivity disorder (ADHD), intellectual disabilities (ID), and neurogenetic conditions, often present with lower levels of daily living skills (DLS) when compared to their neurotypical peers (1–4). Importantly, lower levels of DLS have been linked to lower rates of post-secondary education, lower employment rates, increased likelihood of living with parents, and higher daily support needs in individuals with NDD, in particular in autistic individuals with and without co-occurring ID (5–7). Conversely, higher DLS are predictive of more positive adult outcomes, including better subjective wellbeing (8) and higher education rates, employment, and independent living (9). Consequently, DLS have been recognized as a crucial target for clinical intervention and support by both research and clinical community as well as by autistic individuals and stakeholders (10–12).
DLS are typically acquired across development and are defined as the ability to perform the everyday tasks and activities necessary for independent living. They fall into three main domains: personal (e.g., dressing, showering, and taking medication), domestic (e.g., cooking, cleaning, and laundry), and community DLS [e.g., managing time, money, and employment; (13)]. Autistic individuals and individuals with other NDD demonstrate significant heterogeneity in these skills that cannot be accounted for by cognitive functioning alone (1, 14, 15). In fact, although higher cognitive functioning is broadly associated with higher DLS (16), autistic individuals with average or above average IQs often show considerably lower DLS than would be expected given their cognitive functioning, whereas DLS has been identified as a relative strength of many individuals with co-occurring ID (17–21). Further, although some core autism characteristics, such as communication barriers or rigid routines, may play a role in the reduced acquisition of these skills, research has shown that the autism characteristics alone are poor predictors of DLS (1, 3, 21, 22). Therefore, DLS represent a distinct and crucial target for more individualized research and support that is stakeholder-informed and reflects a shift toward a more dimensional and trans-diagnostic understanding of support needs.
Although current measures of DLS, with the Vineland Adaptive Behavior Scale [VABS-3; (13)] and the Adaptive Behavior Assessment System [ABAS-3; (23)] being the most widely adopted instruments, have provided important insights into presentations of DLS across neurodevelopmental conditions, they are not without limitations. Firstly, although relatively comprehensive, both instruments are lengthy and can be burdensome for participants, limiting their use in clinical contexts and research studies with longer assessment batteries. Further, high cost prohibits their use among research and clinical communities with less funding or could decrease the collection of adaptive functioning in situations where money must be allocated to more expensive measurement types (e.g., multi-omic data collections). Therefore, despite stakeholder calls to better contextualize autism research in terms of specific challenges requiring support, the expense and length of current instruments could preclude the inclusion of DLS assessments from being more widely adopted. Additionally, the current measures of DLS have demonstrated psychometric limitations. For example, despite the complexity and noted heterogeneity of DLS (1, 9, 13, 16, 21), most commonly used measures either provide only a total DLS score based solely on theoretical or practical concerns, limiting the clinical utility of these measures in terms of identifying specific targets for intervention and monitoring the progress of specific skills, or have not been comprehensively and stringently factorized, raising concerns about their construct validity. Additionally, measurement invariance and factor structures of current measures are largely unexplored and remain poorly understood, despite their wide use. This is a significant issue given that measurement invariance is crucial for ensuring that a measure is applicable across a wide demographic spectrum. Further, several studies evaluating VABS psychometric properties have reported low internal consistency for subscale scores as well as low interrater and test-retest reliability (13, 24–26). Finally, despite increasing recognition of the utility of regression-based norms to improve the precision and individualization of clinical assessment (27), current measures do not provide regression-based norms across autistic, neurotypical, and other developmental disorder populations. Thus, there is an urgent need for new, freely-available, comprehensive DLS instruments developed and validated based on state-of-the-art measurement development and psychometric principles.
The current paper outlines the development and psychometric evaluation of the Daily Living Skills Scale (DLSS)—a relatively brief (53-items) yet comprehensive, open-source informant-reported instrument for capturing key aspects of DLS that was specifically developed to be appropriate for use across full developmental (age and cognitive functioning) and demographic range and to be applicable across a range of NDD. DLSS was designed to specifically address the limitations of current DLS measures by providing a robust factor structure and measurement invariance across key parameters, including age, sex, and diagnostic status. The development process included a literature review of current DLS measures and item evaluation by stakeholders. Preliminary validation was conducted with a large, representative US sample spanning autistic children, children with other NDD, and neurotypical controls and included evaluation of the factor structure, measurement invariance, classical test theory and item response theory-derived reliability, and convergent and discriminant validity.
2. Materials and methods
2.1. Participants
Parent informants were recruited using the Prolific online data collection service (https://prolific.co/). Data was collected from 05/03/2022 to 07/20/2022. The final sample included 1,361 informants who completed the survey on their children. Based on informant-reported clinical diagnoses, 116 children had autism, 356 had neurodevelopmental conditions, and 889 were neurotypical (no neurodevelopmental or neuropsychiatric diagnosis). Inclusion criteria for both exploratory and confirmatory samples included: residence in the US, having a dependent child aged 2–17, and informant proficiency in English. Detailed characteristics across exploratory and confirmatory samples are presented in Table 1.
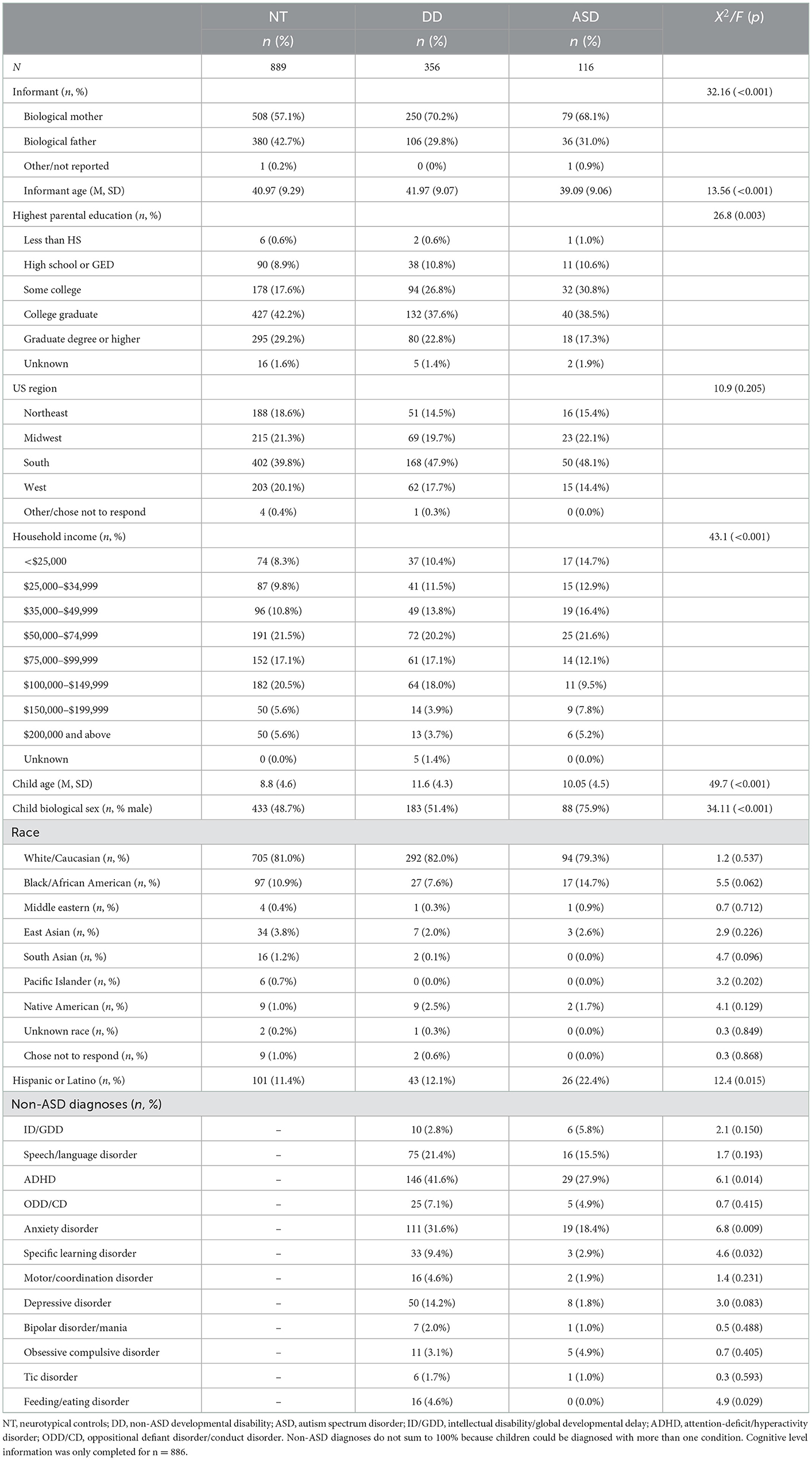
Table 1. Demographic and clinical characteristics across autism spectrum disorder (ASD), developmental disability (DD), and neurotypical (NT) controls.
2.2. Measures
Daily Living Skills Scale (DLSS). DLSS was developed and refined through an iterative series of steps embodied in the Patient-Reported Outcomes Measurement Information System (PROMIS) framework. Firstly, the DLS conceptual model was generated based on a systematic review of the existing DLS instruments and existing conceptual models of both broader adaptive functioning and more specific DLS frameworks. The following key content areas were identified: Personal Hygiene and Grooming, Dressing and Undressing, Meal Preparation and Feeding, Toileting, Housekeeping, Health and Medication, Leisure Time, Safe Environment, Transportation and Mobility. Following the generation of the conceptual map, a review of the literature was conducted to identify existing scales relevant to each content area. Reviewed scales included: the Vineland Adaptive Behavior Scales, third edition [VABS-3; (13)], the Adaptive Behavior Assessment System [ABAS-3; (23)], the Scales of Independent Behavior—Revised [SIB-R; (28)], and Waisman Activities of Daily Living [W-ADL; (29)]. Instruments were then reviewed by the first and senior author, and at least three items were written to ensure that each content area is adequately assessed with particular emphasis on capturing the full ability range, from very low to high (capturing very high levels was deemed not crucial for most clinical and research contexts). A preliminary item bank was evaluated by 10 neurodevelopmental disability clinician-scientist experts and 10 neurodevelopmental disability caregiver/patient informants. Both experts and caregivers/patient informants evaluated whether each item (i) effectively evaluated the given DLS content area (experts and informants), (ii) was relevant to patients (experts) or child (informants), (iii) was relevant to the full developmental (age and IQ) and functional range of patients (experts), and (iv) was easy/difficult to understand and rate (experts and informants). Following the feedback, minor clarifications and changes in terms of the wording were made to several items. Given that neither experts nor caregivers/patient informants indicated that any of the items should be removed and that no specific behaviors, skills, or content areas were missing, no further changes were made to the scale. The final scale consisted of 53 items that were rated on a 4-point Likert scale with the choices being: “Not able to complete (total assistance needed),” “Requires significant prompting or assistance,” “Requires minimal prompting or assistance,” “Completely independent (does not require any assistance or prompting)”. This scale was chosen given that being able to differentiate between significant prompting/assistance and only minimal prompting/assistance should add discrimination to each item and is consistent with behavioral intervention approaches that attempt to decrease the level of prompting needed when building functional skills. No time frame was included in the instructions because daily living skills are rated according to whether the skill has been acquired at the time of rating.
Demographic and health information. Informants provided age, sex, race, ethnicity, time spent living with the informant, household income, and highest level of parental education, and reported all prior clinical diagnoses for each participant.
Vineland Adaptive Behavior Scales, third edition [VABS-3; (13)]. VABS-3 is an informant-report scale designed to comprehensively capture different aspects of adaptive functioning. Each item is rated on a 3-point Likert scale (0 = Never, 1 = Sometimes, 2 = Usually), with higher rating indicating better performance/ability/skill level. For the present study, the total Daily Living Skills domain (143 items) score was used. VABS-3 Daily Living Skills domain encompasses Personal, Domestic, and Community subdomains. For the present study, the total domain score was used.
DSM-5 attention-deficit/hyperactivity disorder (ADHD) Checklist. DSM-5 ADHD Checklist is an 18-item informant report scale designed to capture DSM-5 ADHD symptoms of inattention, hyperactivity, and impulsivity. Each item is rated on a 4-point Likert scale (0 = Not at all; 1 = Just a Little; 2 = Often; and 3 = Very Often) with a higher rating indicating more severe symptoms.
Developmental Coordination Disorder Questionnaire [DCDQ; (30)]. DCDQ is a 15-item informant-report measure designed to capture fine and gross motor skills as well as general coordination in children and adolescents. Each item is rated on a 5-point Likert scale, with higher scores reflecting better performance. Total score was used in this study.
Spence Children's and Preschool Anxiety Scales [SCAS and SPAS; (31, 32)]. SCAS and SPAS are informant-report measures of anxiety designed to capture overall anxiety levels and specific anxiety subdomains. Each item is rated on a 4-point Likert scale (0 = Neve, 1 = Sometimes, 2 = Often, and 3 = Always) where higher rating indicates higher symptom severity. The SPAS was administered to ages 2–6 and the SCAS was administered to ages 7–17. The total scores were used for the current study.
Executive Functioning Skills scale [EFS; (33)]. EFS is a 52-item scale designed to comprehensively characterize non-affective (e.g., sequencing/working memory, response inhibition and set-shifting) and affective (e.g., emotion regulation, and risk-taking) facets of executive functioning. Total EFS score is strongly correlated with the 24-item Behavior Rating Inventory of Executive Functioning (r = 0.85) and shows excellent model reliability and internal consistency (ω = 0.98; α = 0.97) and excellent conditional reliability estimates (≥0.90) from extremely low (θ ~ −4.2) to very high (θ ~ +2.6) scores.
2.3. Statistical analyses
Descriptive statistics for demographic and clinical factors were computed to characterize the sample.
2.3.1. Factor structure
Confirmatory Factor Analysis was first used to explore the fit of the unidimensional model. Model fit was evaluated using the comparative fit index (CFI), Tucker–Lewis index (TLI), root mean square error of approximation (RMSEA), and the 95% confidence interval of RMSEA were used to examine model fit (34, 35). If the unidimensional model showed poor fit, we planned to estimate exploratory structural equation models [ESEM; (36)] using geomin rotation and weighted least squares mean and variance adjusted estimation and specifying two to 8 specific factors with an additional general bifactor that included estimation of loadings from all items.
2.3.2. Measurement invariance
The optimal model derived from the factor analyses described above was used as the basis for the evaluation of measurement invariance (37) across age groups (ages 2–4, 5–11, and 12–17 years), sex (male, female), race (Caucasian, other), and ethnicity (Hispanic, non-Hispanic). To examine measurement invariance (equivalence), a series of multi-group confirmatory factor analyses were computed using the theta parameterization and WLSMV estimation for categorical indicators, following recommended conventions (38) and our prior work (39). Model comparisons for measurement invariance analyses were based on empirical work indicating that a drop in CFI or TLI > 0.01 or an increase in RMSEA > 0.01 implies measurement non-equivalence (40, 41).
2.3.3. Reliability
Using the optimal factor model, items with substantive loadings were assigned to scales and classical test theory (CTT) reliability (internal consistency and correct item-total correlations) (42) and item response theory (IRT) analyses were conducted (43) in the full sample (n = 2004). Analyses used maximum likelihood estimation with robust standard errors and a logit link with the single factor mean and variance fixed to 0 and 1, respectively. Reliability estimates falling in the ranges 0.70–0.79, 0.80–0.89, and >0.90 were considered fair, good, and excellent (44). Average corrected item-total correlations ≥0.30 were considered adequate or better (42). Differential item and test functioning were evaluated by examining differences in item characteristic curves and test information curves across age groups, sex, race, and ethnicity.
2.3.4. Convergent and discriminant validity
Convergent and discriminant validity were computed using bivariate correlations (Pearson or Spearman's non-parametric, where applicable).
3. Results
3.1. Factor structure and measurement invariance
The CFA single-factor model based on the final 53 items showed good fit to the data (CFI = 0.953, TLI = 0.951, RMSEA = 0.073 [95% CI: 0.071–0.074]). All items had strong loading on the single factor (Figure 1). The single-factor CFA model was used to evaluate measurement invariance, model reliability, and variance accounted for by the specific and general DLS factors. Given that other daily living skills (Vineland-3) or practical domain (ABAS-3) measures include content subareas and that there is value in helping clinicians understand what types of skills might be strengths or weaknesses, we also computed three subscales: self-care (28 items), home-care (10 items), and community participation (15 items). Scale reliability information is also provided for these conceptual subscales.
The single-factor CFA model presented above showed evidence of measurement invariance of factor loadings, thresholds, and residual variance (strict invariance) across sex, age, race, and ethnicity (Table 2).
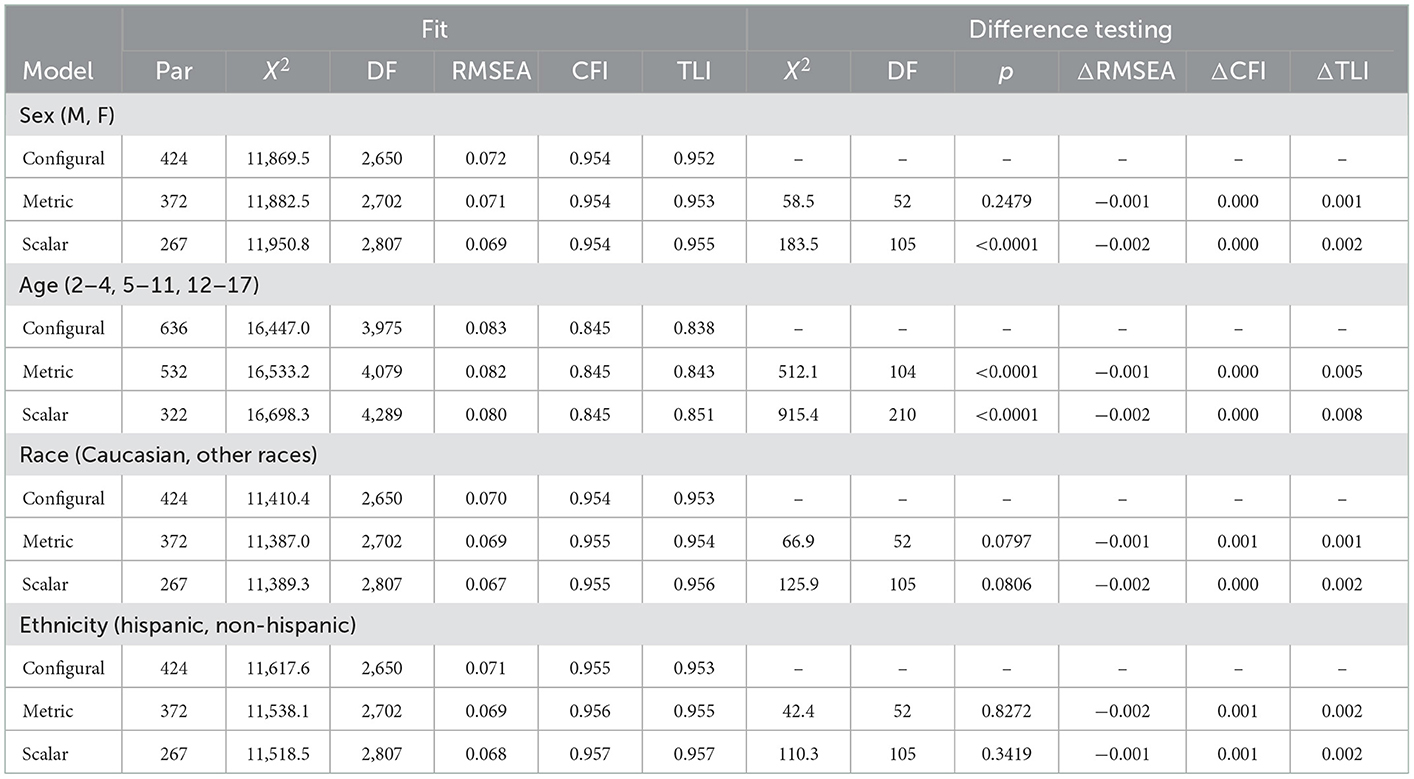
Table 2. Measurement invariance analyses for the final DLS factor model across sex, age, race, and ethnicity.
3.2. Model and scale reliability
Model reliability was high for the general DLS factor (ω = 0.98) and comparable to the Vineland-3 Daily Living Skills domain reliability in this sample (ω = 0.99). Using item scores, internal consistency reliability was excellent for the total scale (α = 0.97) and comparable to the Vineland-3 Daily Living Skills domain (α = 0.99) in this sample. Internal consistency reliability of the conceptual scores was also excellent (self-care α = 0.96; home-care α = 0.94; community participation α = 0.94).
3.3. Conditional reliability derived from item response theory analyses
Conditional reliability estimates indicated very good reliability (≥0.80) for the total DLS scale from very low (θ = −4.2) to high (θ = +2.4) scores. Importantly, a comparison of conditional reliability from the 53-item DLS scale and the 143-item Vineland-3 Daily Living Skills domain in this sample indicated highly comparable curves (Figure 2). The average difference in conditional reliability from theta = −4 to +4 was trivial (Δrxx = 0.02). This indicates that the DLS is showing good precision of measurement across key score ranges for monitoring intervention progress (equivalent to standard scores of 37–136) and that the DLS and Vineland Daily Living Skills domain are showing equivalent measurement precision in this sample.
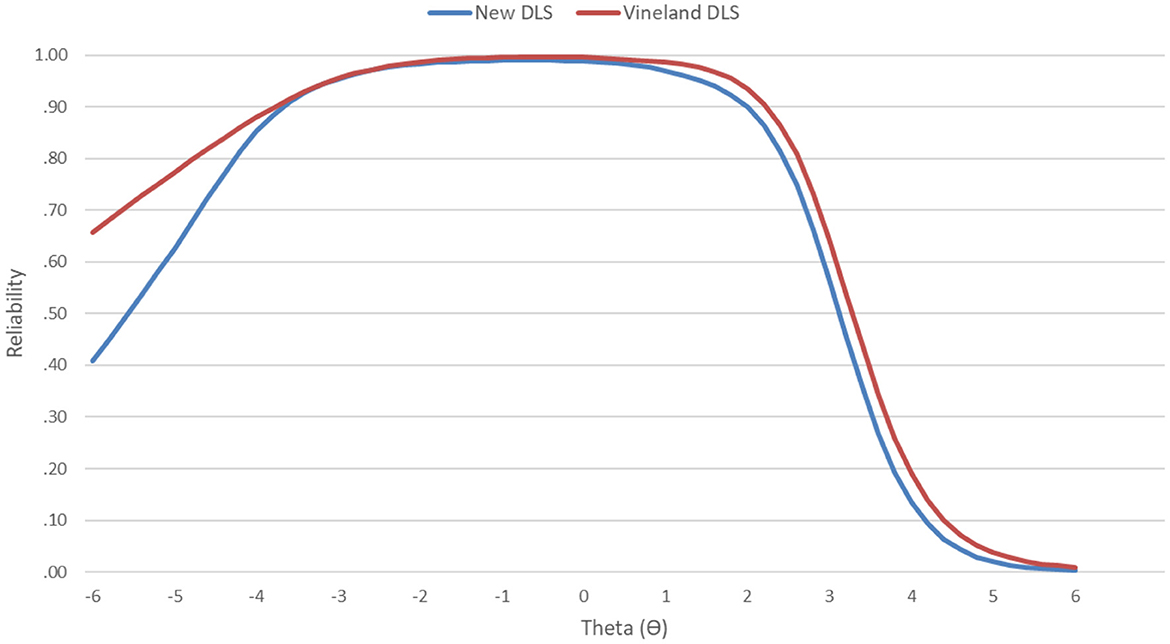
Figure 2. Item response theory-derived conditional reliability across the latent trait for the total DLS scale and the Vineland Daily Living Skills domain.
3.4. Convergent and discriminant validity
The expected pattern of convergent and discriminant validity was observed. More specifically, DLS total scores showed strong correlations with VABS-3 Total Daily Living Skills domain raw scores (r = 0.94) and the DLS and Vineland-3 Daily Living Skills domain subscale scores showed the expected strong correlations (Self-Care with Personal: r = 0.88; Home-Care with Domestic: r = 0.88; Community Participation with Community: r = 0.91). The DLS total score showed a moderate and expected negative correlation with ASD diagnosis (r = −0.22) and IQ (r = −0.22). As anticipated, correlations with other measures that do not assess daily functioning but that evaluate clinical domains which could reduce adaptive function were also in the moderate range (DSM-5 ADHD scale r = −0.35; Spence Children's Anxiety Scale r = −0.40, Spence Children's Anxiety Scale r = −0.03). Not surprisingly, given the importance of executive functioning for daily living skills and the close relationship between motor functioning and daily living skills, the correlations between DLS total scores and measures of these constructs were higher (DLS with EFS r = 0.59 and DLS with DCDQ r = −0.75), however, correlations with these measures were significantly lower than correlations with the Vineland-3 Daily Living Skills scores as indexed by the Fisher r-to-z transformation (for DLS with EFS vs. Vineland-3 z = 27.63, p < 0.001; for DLS with DCDQ vs. Vineland 3 z = 19.94, p < 0.001).
4. Discussion
The DLSS is an open-source, informant-report measure that was developed to comprehensively assess key facets of daily living skills (DLS) across the full ability and cognitive range in children and adolescents with autism, other neurodevelopmental conditions and across normative development. Findings from this preliminary validation study demonstrate that the DLSS has excellent psychometric properties, which combined with the fact that it free and relatively brief (53 items), suggest that it is potentially a good choice for capturing DLS across different contexts, both in terms of research and potentially clinical practice. Crucially, despite having slightly more than a third of the items compared to the Vineland Adaptive Behavior Scales, third edition (DLSS = 53 vs. Vineland DLS domain = 143 items), DLSS shows equivalent reliability, internal consistency, and measurement precision.
The DLSS was developed to capture a range of different daily living skills that could be broadly divided into self-care, homecare, and community participation subdomains and encompass a diverse range of skills and behaviors, including personal hygiene and grooming, dressing and undressing, meal preparation and feeding, toileting, housekeeping, health and medication, leisure time, safe environment, and transportation and mobility. In keeping with other DLS measures such as Vineland-3, latent variable modeling indicated that the unidimensional model showed an excellent fit to the data, indicating a unidimensional factor structure. Further, a single-factor model showed evidence of measurement invariance of factor loadings, thresholds, and residual variance (strict invariance) across sex, age, race, and ethnicity. Model reliability and internal consistency were high, and conditional reliability estimates indicated very good reliability for the total DLS scale from very low to high scores. Finally, there was good preliminary evidence for convergent and discriminant validity. Although self-care (28 items), homecare (10 items), and community participation (15 items) subscales were conceptually-derived as analogs to Vineland-3 subscales, they nevertheless showed strong reliability and internal consistency. Thus, given in-depth coverage of these DLS subareas, the DLSS might be useful in helping clinicians understand types of skills that might be strengths or weaknesses for a particular child. Future studies are needed to better understand the potential value of these conceptually-derived subscales.
Although several DLS measures, including ABAS, SIB-R, and Vineland-3, have been specifically designed and widely used for capturing individual differences in DLS among autistic individuals and individuals with a range of neurodevelopmental conditions, their limited psychometric evaluation, together with significant length and cost, limit their utility. More specifically, demonstrated invariance across diverse sex, age, race, ethnicity, and clinical groups is a key assumption that must be met for widespread measure adoption of any instrument. However, there is little evidence for the invariance of other DLS scales, including ABAS, SIB-R and Vineland-3. In contrast, as noted, the DLSS showed strong evidence for invariance, indicating that it can be interpreted consistently when implemented across populations with diverse developmental levels and demographics. Good conditional reliability is a key feature necessary for capturing and tracking very high and very low levels of a particular trait with good precision; however, with the exception of Vineland-3, other measures of daily living skills lack evidence for conditional reliability. Conversely, DLSS conditional reliability estimates indicated very good measurement precision across key score ranges for monitoring intervention progress. Thus, robust evidence of invariance and conditional reliability provide tentative support for DLSS as being more useful for assessing adaptive behavior in many research contexts where brevity, rater burden, equivalent measurement across demographic groups, and cost are key considerations.
Despite a large, representative validation sample, stringent analytical approaches and comprehensive convergent and discriminant validity indicators, the findings reported here need to be considered in the light of several limitations. In particular, this study was limited by the reliance on informant reports and the lack of direct clinical diagnostic, cognitive, and symptom severity assessments. Further, even though online data collection does not allow independent confirmation of diagnostic status and administration of gold standard diagnostic assessments and dedicated cognitive assessments, it is important to note that prior online studies collecting parent-reported diagnoses have shown very high rates of ASD verification from clinical reports (45, 46) and high concordance (>97%) with clinician best estimate diagnoses and with standardized instruments (47). Further, with regards to cognitive functioning, parent-reported levels of children's IQ/cognitive functioning level have been shown to strongly correspond with in-person IQ testing [e.g., (48)]. In addition, even though the Vineland-3 DLS section was used, a more comprehensive set of additional measures is needed. Despite the large sample size, our cohort included a mainly white and well-educated sample. Given the noted limitations, it will be crucial to further validate the DLSS in a more diverse sample and clinical settings through in-person clinical and cognitive assessments and utilize longitudinal and treatment designs to investigate its predictive validity and sensitivity to change. Finally, it will be important to develop regression-based norms that take into account age, sex, and developmental and cognitive level.
In summary, despite noted limitations, the present data provide preliminary evidence that the DLSS is a valid and reliable new, freely available and relatively brief instrument for the comprehensive characterization of individual differences in different facets of DLS in autism and a range of other NDD. Further, DLSS shows excellent measurement precision for capturing a wide range of abilities, which suggests the excellent potential for its use for characterizing change over time and for treatment tracking. Thus, with further replication, the DLSS has excellent potential for wide adoption across research and clinical contexts.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. And I did not detect any particular expressions.
Ethics statement
The studies involving human participants were reviewed and approved by John Carroll University IRB. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
TF, MU, and AH designed the study. TF and MU collected the data and had full access to the data and conducted the analyses. MU, ES, TF, RC, KP, and AH drafted the initial manuscript. All authors critically reviewed, provided feedback on the initial version of the manuscript, and approved the final version of the manuscript.
Funding
The study was supported by Simons Foundation Autism Research Initiative—Director's Award #831500 (PI: TF), PTEN Research Foundation Grant #JCU-20-001 (PI: TF), and #UOM-20-001 (PI: MU).
Acknowledgments
We are sincerely indebted to the generosity of the participants who contributed their time and effort to this study. We would also like to thank the PTEN Research Foundation for their continued support.
Conflict of interest
MU has equity options and an advisory role in Quadrant Biosciences and has an investor stake in iSCAN-R. AH has equity options and an advisory role in Quadrant Biosciences, has an investor stake in iSCAN-R and is a consultant/advisor for Jazz Pharmaceuticals, Beaming Health, and IAMA Therapeutics. TF is employed by and has equity options in Quadrant Biosciences/Autism Analytica, has equity options in MaraBio and SpringTide, and has an investor stake in Autism EYES LLC and iSCAN-R.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Duncan AW, Bishop SL. Understanding the gap between cognitive abilities and daily living skills in adolescents with autism spectrum disorders with average intelligence. Autism Int J Res Pract. (2015) 19:64–72. doi: 10.1177/1362361313510068
2. Gillham JE, Carter AS, Volkmar FR, Sparrow SS. Toward a developmental operational definition of autism. J Autism Dev Disord. (2000) 30:269–78. doi: 10.1023/A:1005571115268
3. Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, Saulnier CA. The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. J Autism Dev Disord. (2011) 41:1007–18. doi: 10.1007/s10803-010-1126-4
4. Scandurra V, Emberti Gialloreti L, Barbanera F, Scordo MR, Pierini A, Canitano R. Neurodevelopmental disorders and adaptive functions: a study of children with autism spectrum disorders (ASD) and/or attention deficit and hyperactivity disorder (ADHD). Front Psychiatry. (2019) 10:673. doi: 10.3389/fpsyt.2019.00673
5. Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Res Off J Int Soc Autism Res. (2009) 2:109–18. doi: 10.1002/aur.69
6. Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Post-secondary education and employment among youth with an autism spectrum disorder. Pediatrics. (2012) 129:1042–9. doi: 10.1542/peds.2011-2864
7. Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: the case of daily living skills. J Am Acad Child Adolesc Psychiatry. (2012) 51:622–31. doi: 10.1016/j.jaac.2012.03.001
8. Scheeren AM, Buil JM, Howlin P, Bartels M, Begeer S. Objective and subjective psychosocial outcomes in adults with autism spectrum disorder: a 6-year longitudinal study. Autism. (2022) 26:243–55. doi: 10.1177/13623613211027673
9. Clarke EB, McCauley JB, Lord C. Post–high school daily living skills in autism spectrum disorder. J Am Acad Child Adoles Psychiatry. (2021) 60:978–85. doi: 10.1016/j.jaac.2020.11.008
10. Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. J Am Acad Child Adolesc Psychiatry. (2015) 54:369–76. doi: 10.1016/j.jaac.2015.02.005
11. Ghanouni P, Quirke S, Blok J, Casey A. Independent living in adults with autism spectrum disorder: stakeholders' perspectives and experiences. Res Dev Disabil. (2021) 119:104085. doi: 10.1016/j.ridd.2021.104085
12. Roche L, Adams D, Clark M. Research priorities of the autism community: a systematic review of key stakeholder perspectives. Autism. (2021) 25:336–48. doi: 10.1177/1362361320967790
13. Sparrow SS, Cicchetti DV, Saulnier CA. Vineland-3: Vineland Adaptive Behavior Scales. New York, NY: PsychCorp (2016).
14. Baker E, Stavropoulos KK, Baker BL, Blacher J. Daily living skills in adolescents with autism spectrum disorder: implications for intervention and independence. Res Autism Spect Disord. (2021) 83:101761. doi: 10.1016/j.rasd.2021.101761
15. Tam JYC, Barrett EA, Ho AYH. Narrative intervention in school-aged children with autism spectrum disorder: a systematic review. Speech Lang Hear. (2021) 19:1–18. doi: 10.1080/2050571X.2021.1985893
16. Bal VH, Kim SH, Cheong D, Lord C. Daily living skills in individuals with autism spectrum disorder from 2 to 21 years of age. Autism Int J Res Pract. (2015) 19:774–84. doi: 10.1177/1362361315575840
17. Alvares GA, Bebbington K, Cleary D, Evans K, Glasson EJ, Maybery MT, et al. The misnomer of “high functioning autism”: intelligence is an imprecise predictor of functional abilities at diagnosis. Autism Int J Res Pract. (2020) 24:221–32. doi: 10.1177/1362361319852831
18. Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, et al. Predictors and correlates of adaptive functioning in children with developmental disorders. J Autism Dev Disord. (2001) 31:219–30. doi: 10.1023/A:1010707417274
19. Bradshaw J, Gillespie S, Klaiman C, Klin A, Saulnier C. Early emergence of discrepancy in adaptive behavior and cognitive skills in toddlers with autism spectrum disorder. Autism. (2019) 23:1485–96. doi: 10.1177/1362361318815662
20. Matthews NL, Smith CJ, Pollard E, Ober-Reynolds S, Kirwan J, Malligo A. Adaptive functioning in autism spectrum disorder during the transition to adulthood. J Autism Dev Disord. (2015) 45:2349–60. doi: 10.1007/s10803-015-2400-2
21. Tillmann J, San José Cáceres A, Chatham CH, Crawley D, Holt R, Oakley B, et al. Investigating the factors underlying adaptive functioning in autism in the EU-AIMS Longitudinal European Autism Project. Autism Res. (2019) 12:645–57. doi: 10.1002/aur.2081
22. Klin A, Saulnier CA, Sparrow SS, Cicchetti DV, Volkmar FR, Lord C. Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: the Vineland and the ADOS. J Autism Dev Disord. (2007) 37:748–59. doi: 10.1007/s10803-006-0229-4
24. Perry A, Factor DC. Psychometric validity and clinical usefulness of the Vineland adaptive behavior scales and the AAMD adaptive behavior scale for an autistic sample. J Autism Dev Disord. (1989) 19:41–55.
25. Floyd RG, Shands EI, Alfonso VC, Phillips JF, Autry BK, Mosteller JA, et al. A systematic review and psychometric evaluation of adaptive behavior scales and recommendations for practice. J Appl School Psychol. (2015) 31:83–113. doi: 10.1080/15377903.2014.979384
26. De Bildt A, Sytema S, Kraijer D, Sparrow S, Minderaa R. Adaptive functioning and behaviour problems in relation to level of education in children and adolescents with intellectual disability. J Intell Disabil Res. (2005) 49:672–81. doi: 10.1111/j.1365-2788.2005.00711.x
27. Timmerman ME, Voncken L, Albers CJ. A tutorial on regression-based norming of psychological tests with GAMLSS. Psychol Methods. (2021) 26:357–73. doi: 10.1037/met0000348
28. Bruininks RH, Woodcock RW, Weatherman RF, Hill BK. Scales of Independent Behavior-Revised SIB-R. Itasca: Riverside Publishing (1996).
29. Maenner MJ, Smith LE, Hong J, Makuch R, Greenberg JS, Mailick MR. Evaluation of an activities of daily living scale for adolescents and adults with developmental disabilities. Disabil Health J. (2013) 6:8–17. doi: 10.1016/j.dhjo.2012.08.005
30. Wilson BN, Crawford SG, Green D, Roberts G, Aylott A, Kaplan BJ. Psychometric properties of the revised developmental coordination disorder questionnaire. Phys Occup Therapy Pediat. (2009) 29:182–202. doi: 10.1080/01942630902784761
31. Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children's anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Therapy. (2004) 42:813–39. doi: 10.1016/S0005-7967(03)00200-6
32. Spence SH. Spence Children's Anxiety Scale (Parent Version). Brisbane: University of Queensland (1999).
33. Uljarević M, Cai R-Y, Hardan AY, Frazier TW. Development and validation of the executive functioning scale. Front Psychiatry. (2022) 13:2998. doi: 10.3389/fpsyt.2022.1078211
34. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria vs. new alternatives. Struct Equ Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
35. Marsh HW, Hau K-T, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct Equ Model. (2004) 11:320–41. doi: 10.1207/s15328007sem1103_2
36. Marsh HW, Morin AJ, Parker PD, Kaur G. Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Ann Rev Clin Psychol. (2014) 10:85–110. doi: 10.1146/annurev-clinpsy-032813-153700
37. Chiorri C, Hall J, Casely-Hayford J, Malmberg L-E. Evaluating measurement invariance between parents using the strengths and difficulties questionnaire (SDQ). Assessment. (2016) 23:63–74. doi: 10.1177/1073191114568301
38. Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. (2016) 41:71–90. doi: 10.1016/j.dr.2016.06.004
39. Frazier TW, Hardan AY. Equivalence of symptom dimensions in females and males with autism. Autism Int J Res Pract. (2017) 21:749–59. doi: 10.1177/1362361316660066
40. Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model. (2007) 14:464–504. doi: 10.1080/10705510701301834
41. Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. (2002) 9:233–55. doi: 10.1207/S15328007SEM0902_5
42. Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to their Development and Use. 2nd ed. Oxford: Oxford University Press (1995).
43. Embretson SE, Reise SP. Item Response Theory for Psychologists. Mahwah, NJ: Lawrence Erlbaum Associates (2000).
45. Daniels AM, Rosenberg RE, Anderson C, Law JK, Marvin AR, Law PA. Verification of parent-report of child autism spectrum disorder diagnosis to a web-based autism registry. J Autism Dev Disord. (2012) 42:257–65. doi: 10.1007/s10803-011-1236-7
46. Feliciano P, Zhou X, Astrovskaya I, Turner TN, Wang T, Brueggeman L, et al. Exome sequencing of 457 autism families recruited online provides evidence for autism risk genes. NPJ Genom Med. (2019) 4:19. doi: 10.1038/s41525-019-0093-8
47. Lee H, Marvin AR, Watson T, Piggot J, Law JK, Law PA, et al. Accuracy of phenotyping of autistic children based on Internet implemented parent report. Am J Med Genet B Neuropsych Genet B. (2010) 153:1119–26. doi: 10.1002/ajmg.b.31103
Keywords: assessment, daily living skills, adaptive functioning, neurodevelopmental, neuropsychiatric, autism
Citation: Uljarević M, Spackman EK, Cai RY, Paszek KJ, Hardan AY and Frazier TW (2023) Daily living skills scale: Development and preliminary validation of a new, open-source assessment of daily living skills. Front. Psychiatry 13:1108471. doi: 10.3389/fpsyt.2022.1108471
Received: 26 November 2022; Accepted: 30 December 2022;
Published: 23 January 2023.
Edited by:
Antonio Narzisi, Stella Maris Foundation (IRCCS), ItalyReviewed by:
Ricardo Canal-Bedia, University of Salamanca, SpainCecilia Montiel Nava, The University of Texas Rio Grande Valley, United States
Copyright © 2023 Uljarević, Spackman, Cai, Paszek, Hardan and Frazier. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mirko Uljarević,  bWlya291bGpAc3RhbmZvcmQuZWR1
bWlya291bGpAc3RhbmZvcmQuZWR1
 Mirko Uljarević
Mirko Uljarević Emily K. Spackman
Emily K. Spackman Ru Ying Cai
Ru Ying Cai Katherine J. Paszek1
Katherine J. Paszek1 Antonio Y. Hardan
Antonio Y. Hardan Thomas W. Frazier
Thomas W. Frazier