
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 22 December 2022
Sec. Adolescent and Young Adult Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1064915
This article is part of the Research Topic Attachment, Adverse Childhood Experiences, and Affective Spectrum Disorders Among Children and Adolescents – Understanding the Impact of its Interaction and Planning Effective Intervention View all 3 articles
Introduction: Children of mothers with a history of adverse childhoods are at greater risk of behavior problems. However, the mechanisms through which a mother’s early adverse experiences (ACEs) are transmitted to her children need further study. Our goal was to examine a conceptual mediational model linking mothers’ ACEs, maternal psychopathology symptoms, and parenting behaviors with children’s internalizing and externalizing behaviors sequentially.
Methods: A sample of 153 Israeli mothers of children ages 3-12 (52% girls) participated in the study, and most of the mothers (94.7%) were cohabiting with a spouse. Mothers completed online questionnaires about their early adverse experiences, psychopathology symptoms, parenting behavior, and their children’s internalizing and externalizing behavior.
Results: Results showed that mothers with higher ACE scores reported more maternal psychopathology symptoms and more internalizing behavior in their children. The mother’s psychopathology in and of itself mediated the link between her ACEs and her child’s internalizing and externalizing behavior. Moreover, an indirect sequential path emerged linking ACEs with the mother’s psychopathology symptoms, which, in return, were linked with hostile parenting. Hostile parenting, in turn, was linked with children’s internalizing and externalizing behavior.
Discussion: These findings highlight the complicated and intertwined ways in which adverse experiences early in the mother’s life might put her child’s wellbeing at risk. The findings suggest that ACEs are linked to maternal affect dysregulation, which interferes with parenting, increasing the risk of behavior problems in children. The findings underscore the need to assess mothers’ adverse history, psychological distress, and parenting behavior, and provide treatments that can reduce the intergenerational transmission of early adverse experiences.
Exposure to adversity in early childhood can reverberate across life and jeopardize one’s health and well-being. Adverse childhood experiences (ACEs) refer to childhood abuse, neglect, and household dysfunction occurring prior to age 18 (1). Research has shown trajectories from ACEs to one’s health problems (2, 3), psychopathology (4, 5), and socioemotional obstacles (6). ACEs not only have long-term effects on those who were exposed to early traumas but are also linked with intergenerational risk. Studies from the developmental and family fields have documented links between caregivers’ ACEs and their children’s development and adaptation from birth to adolescence [e.g., (7, 8)]. For example, cumulative ACEs in parents predicted their children’s depression and/or anxiety (9) and ADHD (10). Mothers’ ACEs predicted their children’s anxiety (11), depression (12), chronic stress (13), and externalizing and internalizing behavior (14–17).
However, the hypothesized mechanisms for explaining the intergenerational link between parents’ ACEs and their children’s behavior problems are still to be explored (17–19). We proposed and examined the mediating links between mothers’ ACEs and their children’s behavioral problems through two mediators: the mothers’ psychopathology and the mothers’ parenting.
Exposure to early adversities during childhood is a well-documented risk factor for adults’ mental health. Since the pioneering study of Felitti et al. (20), a host of studies have demonstrated the association between ACE scores and depression (21), anxiety (22), PTSD (23), alcohol dependence (24), substance abuse (25), somatoform dissociation (26), dissociative symptoms (27), and suicide attempts (28). Moreover, the effect of ACEs on mental health is cumulative, meaning that exposure to a greater number of ACEs increases the risk of later mental health problems (3). Research from the parental literature that focused on maternal ACEs similarly found that mothers’ ACEs predicted their depression, anxiety, PTSD (6, 29, 30), and suicidal ideation (31).
Several explanations have been proposed for the association between ACEs and later psychopathology. Explanations have focused on the hyper-reactivity of the Hypothalamic-Pituitary-Adrenal (HPA) axis (32), dysregulation of the immune system (33), and psychological (34), and psychosocial (35) factors. Hoppen and Chalder (4) proposed a trans-diagnostic biopsychosocial r4’isk model in which exposure to early ACEs leads to the dysregulation of the autonomic nervous system and the hyper-reactivity of the HPA axis, which in turn, interfere with the stress response and immune system, increasing one’s risk for physical and emotional diseases. Given that these disturbances occur when the brain is developing, they interfere with developmental processes, creating socioemotional difficulties that lead to impaired social and psychological functioning during adulthood (4).
We conducted our study during the early stages of the COVID-19 pandemic. The outbreak of COVID-19 has led to a worldwide increase in mental health problems [e.g., (36–38)], including in Israel (39). A particularly vulnerable group are mothers of young children, who exhibited the highest level of depressive and anxiety symptoms (40). Correspondingly, studies following the pandemic’s outbreak documented an association between more ACEs and more depressive symptoms (41, 42), anxiety (43), and PTSD (44), especially among mothers (45). Taken together, these findings support the contention that early childhood adversity has a lasting negative effect on the mother’s stress response system, making her more vulnerable to emotional dysregulation during stressful times such as COVID-19.
Ample evidence has established mothers’ psychopathology as a key risk factor for their children’s development and adjustment problems [e.g., (46, 47)]. For example, mothers’ depression (48, 49), anxiety (50), and PTSD (51) increase the risk of children’s behavior problems. Moreover, the mother’s psychopathology symptoms may provide an additional explanation for the link between her early traumas and her child’s well-being [e.g., (52–54)]. Support for this argument comes from research demonstrating that maternal anxiety and depression mediate the link between maternal ACEs and children’s internalizing and externalizing problems (11, 52, 55–57). In another study from Japan mothers’ global psychological distress mediated the association between maternal ACEs and ch7’6’ildren’s mental health (12). Note that the impact of early trauma on later mental health is characterized by a broad range of symptoms rather than a unique, specific mental disorder (4). Therefore, in the current study we considered the mother’s global measure of psychopathology symptoms as a possible mediator of the link between her ACEs and her child’s internalizing and externalizing behaviors.
Early trauma may not only predict later psychopathology but could also disrupt the parental caregiving system in adulthood. In line with this argument, studies have reported that women who experienced maltreatment in childhood tended to engage in harsh parenting (58), and were more hostile (59, 60), disengaged and intrusive (60). Mothers with many ACEs also demonstrated more aggression toward their child (61). Furthermore, an adverse history of neglect and abuse increased the risk of the mother engaging in the physical abuse, psychological abuse, and neglect of her own children (62). These children may be at greater risk of experiencing ACEs (52, 63).
Research has also established that mothers who endured ACEs as children tend, as a group, to be less engaged in positive parenting behaviors (64). They exhibit less competence in parenting (59), less sensitivity (60), and less maternal self-efficacy (65), and are less available emotionally to their children (66).
Attachment theory provides a theoretical framework for the association between9’ a mother’s ACEs and her parenting. According to the attachment perspective (67), an infant who was exposed to or experienced continued maltreatment or relational trauma is likely to develop an insecure attachment style. Empirical evidence has shown links between mothers’ ACEs and the rate of insecure attachment styles in adulthood (55, 68), as well as higher rates of unresolved states of mind with regard to attachment, another aspect of insecure adult attachment (69). Insecure maternal attachment style is linked to negative parenting behavior (70). Thus, ACEs increase the risk of an insecure attachment style in the parent, which may lead to negative and insensitive parenting.
Another explanation for the association between a mother’s ACEs and her parenting is that parenting a young child may ignite painful memories in the mother about her early trauma, which may evoke affect dysregulation when faced with common, yet stressful, parenting challenges (53, 55, 71). If the mother has an insecure attachment style, her ability to regulate affective arousal effectively is likely to be compromised (72). Such a mother will also have a hard time separating her past threatening experiences from her current parenting challenges (73), activating her self-preservation instinct. This instinct, in return, may overshadow her parental caregiving system and interfere with sensitive and empathic parenting (74).
Parenting practices and behaviors, both positive and negative, are crucial in predicting children’s socioemotional adjustment [e.g., (75)]. Specifically, a large body of research has indicated a positive link between hostile, harsh maternal parenting and children’s and adolescents’ behavioral and emotional problems (76–78). In contrast, positive parenting strategies, specifically, supportive parenting and maternal warmth, are linked to fewer externalizing and internalizing behaviors (79).
Given that parenting behavior is a key factor in children’s behavior and is associated with ACEs, parenting behavior may be another mechanism accounting for the link between the mother’s ACEs and her child’s behavior problems (16). However, studies investigating this possibility have yielded inconsistent findings. On one hand, maladaptive and less responsive parenting such as shouting, slapping, and hostility mediated the association between maternal ACEs and children’s internalizing and externalizing difficulties (80, 81). On the other hand, harsh parenting such as corporal punishment and maternal sensitivity did not mediate the association between maternal ACEs and children’s internalizing and externalizing difficulties (82, 83). Therefore, more research is needed to clarify the mediating role of parenting in the link between maternal ACEs and children’s internalizing and externalizing difficulties.
In line with the efforts to identify the mediating mechanisms linking mothers’ ACEs with their children’s socioemotional adaptation, we proposed and tested two sequentially mediating links between maternal ACEs and children’s internalizing and externalizing behaviors via two mediators. The first mediator–the mother’s psychopathology symptoms–is based on previous findings associating ACEs with adults’ mental and psychological difficulties. Thus, we posited that the mother’s psychopathology symptoms may create a toxic environment for her child and increase the risk of the child’s developing internalizing and externalizing behavior. The second mediator–the mother’s parenting behavior–is grounded in attachment theory’s claim that the mother’s exposure to trauma at a young age may result in her having an insecure attachment style which may lead to more negative and less positive parenting practices.
Moreover, parental psychopathology and parenting are also interconnected. Mounting evidence from perinatal research points to maternal psychopathology as preceding parenting behaviors [e.g., (84–86)]. Therefore, we propose that a mother with a history of adverse experiences during her childhood is more likely to suffer from psychopathology symptoms. These symptoms may lead to more hostile parenting and less supportive parenting, which in turn predict her child’s internalizing and externalizing behaviors. Figure 1 presents our conceptual model.
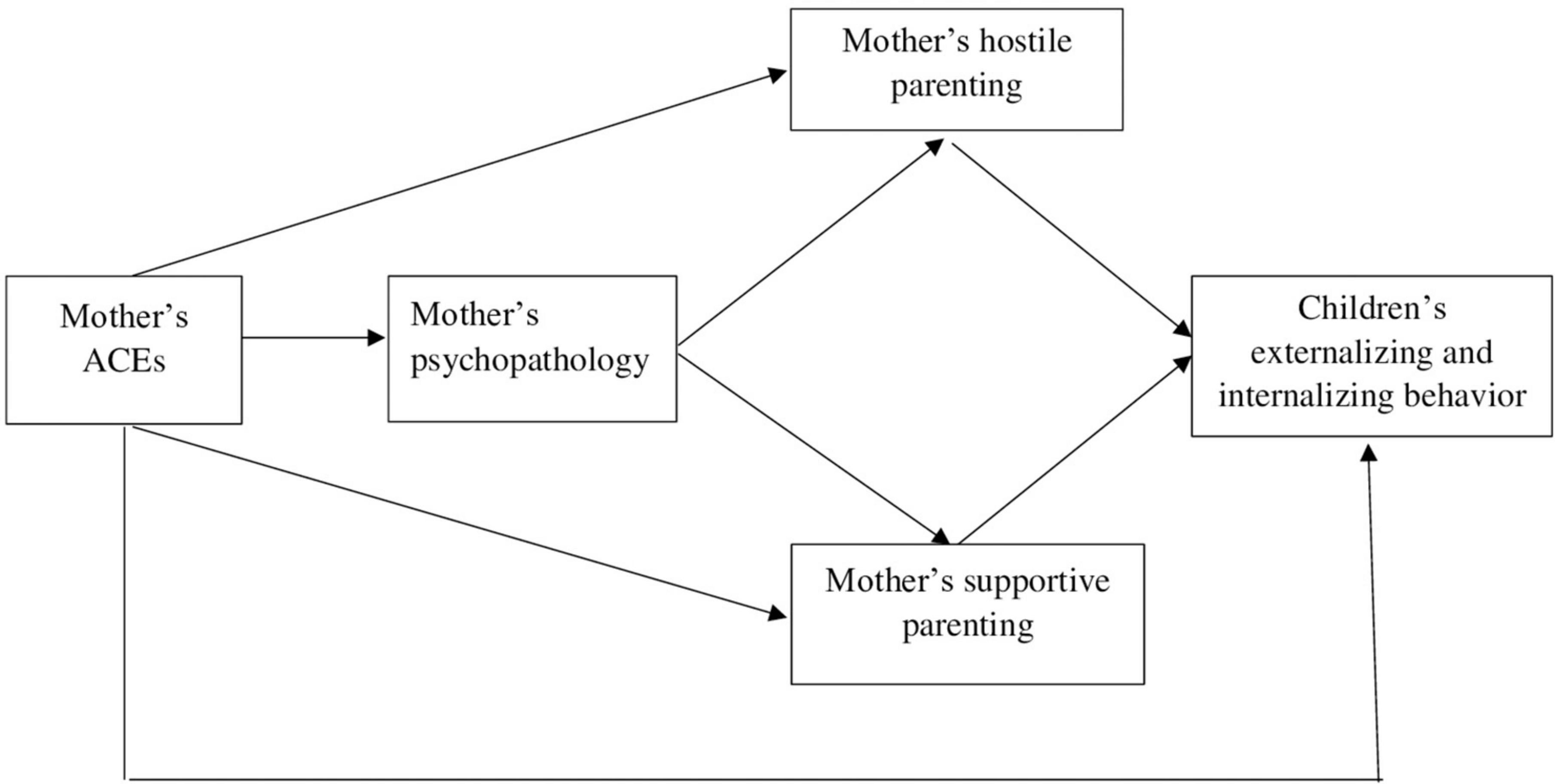
Figure 1. Theoretical mediation model for the association between the mother’s ACEs and her child’s behavior via the mother’s psychopathology and her hostile or supportive parenting.
Hence, we hypothesized that:
(1) The mother’s ACEs will be associated with higher rates of maternal psychopathology, more hostile parenting, less supportive parenting, and more internalizing and externalizing behaviors in her children.
(2) The mother’s psychopathology and hostile and supportive parenting will mediate the links between her ACEs and her children’s internalizing (H2a) and externalizing (H2b) behavior. Specifically, a mother with higher ACEs score will have more psychopathology symptoms. These symptoms will lead to both more hostile parenting and less supportive parenting, which, in turn, will lead to more internalizing and externalizing behavior in the child.
Two hundred and sixty-two Israeli mothers of children between the ages of 3 and 12 years old volunteered for the study. Of the 262, 153 mothers completed all of the study’s questionnaires and comprised the final sample. We used the respondents’ IP address to ensure that no duplicate cases were included in our sample. Independent sample t-tests and chi-squared tests found no significant differences between the main demographic variables such as age, education, income and household composition of those who completed the questionnaires entirely and those who did not. The children ranged in age from 3 to 12.8 years old (M = 7.06, SD = 2.54). Girls comprised 52% of the sample. The majority of the children (56.9%) were firstborn, healthy prior to COVID-19 (95.4%) and all attended public schools. The mothers’ mean age was 38.96 years old (SDage = 5.82). Most of them (94.7%) were cohabiting with a spouse and 57.5% of them had a post-secondary education. Most mothers (90.9%) indicated that they were in good or very good physical health before COVID-19, and none reported being sick with COVID-19 prior to or during the time of the study. The majority of mothers indicated above average (56.9%) and average (40%) pre-COVID-19 family incomes according to Israeli standards.
We used several established methods to test the factors we proposed.
The Adverse Childhood Experiences Questionnaire [ACE; (1)] was utilized. The ACE consists of 10 yes/no questions related to the respondents’ first 18 years of life. The questionnaire items are categorized into three main groups: abuse (including emotional, physical, and sexual abuse), neglect (including emotional and physical neglect), and household dysfunction (including substance use, mental illness, parental separation or divorce, mother being treated violently, and having an incarcerated household member). “Yes” answers receive 1 point and “No” answers receive 0 points, yielding a total score ranging from 0 to 10. Higher scores reflect more adverse experiences. In the current sample, 43.3% of the mothers reported zero ACE, 19.1% of the mothers reported one ACE, 13.8% reported two ACEs, 8.6% reported three ACEs and 15.2% reported four ACEs or more. Cronbach’s alpha for this sample was 0.72.
We used the Global Severity Index (GSI) of the Brief Symptom Index [BSI; (87)] questionnaire to assess the mothers’ reported psychopathology. The BSI is comprised of 53 items that measure psychopathology symptoms on a 5-point Likert-type scale, ranging from 0 (not at all) to 4 (extremely). Respondents were asked to answer questions such as: “Over the last month, to what extent did you feel no interest in things?” The GSI evaluates the combination of the number and severity of the psychopathology symptoms, with higher scores reflecting greater psychopathology. The BSI is a widely used, psychometrically validated, reliable questionnaire of adult psychopathology (88). Internal consistency of the GSI in the current study was very good (Cronbach’s alpha = 0.94).
The Parent Behavior Inventory [PBI, (89)] was used to evaluate the mothers’ parenting behavior. The PBI comprises 20 items, rated on a 6-point Likert scale from 0 (not at all or never) to 5 (always) that produces two independent scales: supportive/engaged and hostile/coercive. Each of these scales contains 10 items (e.g., “I have pleasant conversations with my child”; “I say mean things to my child that makes him/her feel bad”). The scale was designed for and has been used with parents of pre-school-age and school-age children (13, 89). In the current study the two scales had adequate internal consistency (Cronbach’s alpha = 0.78 and 0.81 for the hostile/coercive and the supportive/engaged scales, respectively).
We used the Child Behavior Checklist questionnaire to measure this outcome variable. This questionnaire has two versions, depending on the child’s age. For children 3–5, mothers completed the CBCL 11/5- 5-years-old (90), which contains 99 items, such as “can’t sit still, is restless, or hyperactive.” For children six and older, mothers completed the CBCL 6–18 years old (91), which contains 113 items, such as “not liked by other kids.” In both versions, items are presented on a 3-point Likert-type scale, ranging from 0 (not true), through 1 (somewhat or sometimes true), to 2 (very or often true). The two versions yield two identical clusters: internalizing behavior and externalizing behavior. In our study, both clusters demonstrated good internal consistency (for younger children: internalizing behavior: Cronbach’s alpha = 0.88; externalizing behavior: Cronbach’s alpha = 0.90; for older children: internalizing behavior: Cronbach’s alpha = 0.83, externalizing behavior: Cronbach’s alpha = 0.91). The CBCL has standardized scores with Israeli norms for each age category (92). There were no significant correlations between the children’s age and the raw scores of their internalizing or externalizing behavior in any age group. Thus, we converted the raw scores into t-scores for each age group and used them across the two age groups.
Mothers were recruited through social networks for parents (such as parents’ WhatsApp groups and Facebook) and through the snowball technique shortly after the outbreak of COVID-19 in Israel (from mid-March until the end of April 2020). The recruitment message described the study’s aim in general terms as the desire to learn about parenting and children, specified the required age of the children and provided a link to the online survey. The data were collected online by an open survey (via Qualtrics). The first page of the survey described the study’s aims, mentioned the investigators’ names and affiliations, and indicated the estimated length of time needed to complete the survey. The mothers were then invited to sign an informed consent. Participation was anonymous and voluntary. In addition, the mothers were informed that they could end their participation whenever they wanted to do so. There was no reward or compensation for participation. The study was approved by our institution’s Ethics Committee (ref. 2020079). Mothers were asked to consider only one of their children in the specified age range when completing the questionnaires. Based on the child’s age, they were branched to the relevant CBCL form. Only the research’s team could enter the survey by a password. The study’s questionnaires were randomized to reduce bias. Participants were not obligated to answer all of the items. However, at the end of each questionnaire a message notifying the participants about missing items appeared. Participants could go back and fill in the missing items or change their answers before proceeding to the next questionnaire.
Prior to testing the study’s hypotheses, we used Pearson’s correlations and t-tests to conduct preliminary analyses of the associations between various demographic factors and the study’s variables to identify possible confounders. To test H1 we ran Pearson’s correlations for the associations between the mothers’ ACEs, their psychopathology, and parenting, and the children’s internalizing and externalizing behavior. To test H2 we used Hayes (93) PROCESS model 81 with 5,000 bias-corrected bootstrap samples. We conducted the analyses separately for the child’s internalizing and externalizing behaviors, resulting in two models. In each model we tested the direct and indirect links between the mother’s ACEs (X) and the child’s behaviors (externalizing or internalizing; Y) with the mothers’ psychopathology symptoms as the first mediator (M1), followed by their hostile or supportive parenting as sequential parallel mediators (M2, M3, respectively). We considered the effects significant at p < 0.05. When the 95% confidence interval included 0, we inferred a significant indirect effect at the 0.05 level. All analyses were done using IBM SPSS Statistics version 27 and the PROCESS macro version 3.5 for SPSS (93).
Preliminary analyses of the associations between the demographic variables and the study’s variables revealed that the child’s age was significantly and negatively associated with the mothers’ reports of supportive parenting (r = −0.17, p = 0.03). Thus, mothers of older children reported fewer supportive and engaged parenting behaviors. The child’s gender was significantly associated with the mother’s GSI [F (151, 1) = 4.47, p = 0.04] such that mothers of boys reported more psychopathology symptoms than mothers of girls. The child’s gender was also associated with the mothers’ report of their children’s internalization behavior [F (145, 1) = 5.33, p = 0.02] indicating that girls had more internalizing behavior than boys. Thus, we included the child’s age and gender as covariates in further analyses.
To test H1, we ran Pearson’s correlations to examine the associations between the mothers’ ACEs, their psychopathology symptoms, supportive parenting, and hostile parenting, and their children’s internalizing and externalizing behaviors. Table 1 presents the descriptive information (means and standard deviations or counts and percentages, as appropriate) and correlations among the study’s variables.
As predicted, there were positive and significant correlations between the mothers’ ACE scores and their reports of their psychopathology, and their children’s internalizing behavior. Mothers who experienced more early traumas reported more psychopathology symptoms and more internalizing problems in their children. However, contrary to our hypothesis the mothers’ ACEs were not correlated with their children’s externalizing behavior or with the mothers’ reports of their hostile or supportive parenting. In addition, there were significant positive correlations between the mothers’ psychopathology and their hostile parenting and their reports of their children’s internalizing and externalizing behavior. Moreover, the mother’s parenting behaviors, be it supportive or hostile, was correlated with the child’s behavior, both internalizing and externalizing. In sum, H1 was partially confirmed.
To test H2 regarding the mediated links between the mother’s ACE and her children’s behavior via the mother’s psychopathology symptoms and her supportive or hostile parenting, we used two models: one for internalizing behavior (H2a) and one for externalizing behavior (H2b). The mediation model predicting a child’s internalizing behavior from the mother’s ACEs via the mother’s psychopathology symptoms and her hostile or supportive parenting was significant [F (6, 137) = 10.11, p < 0.001], accounting for 31% of the variance. Figure 2 depicts the links between the model’s variables. While not presented in the figure for the sake of visual clarity, the child’s age and gender were included in the models as covariates. No direct effect was found between the mother’s ACEs and the child’s internalizing behavior. Table 2 presents the indirect effects. As the table indicates, the indirect link between the mother’s ACEs and her children’s internalizing behavior via the mother’s psychopathology was significant. Moreover, as predicted, the link between the mothers’ ACEs and the children’s internalizing behavior was mediated sequentially via the mothers’ psychopathology symptoms and hostile parenting. The higher the mother scored on having experienced ACEs, the more severe her psychopathology was. This psychopathology was linked to more hostile parenting, which was linked to more internalizing behavior among the children. However, the indirect paths between the mother’s ACEs and the children’s internalizing behavior via the mother’s parenting behavior, hostile or supportive, each on its own, were not significant. Finally, the indirect sequential path through the mother’s psychopathology and her supportive parenting was not significant.
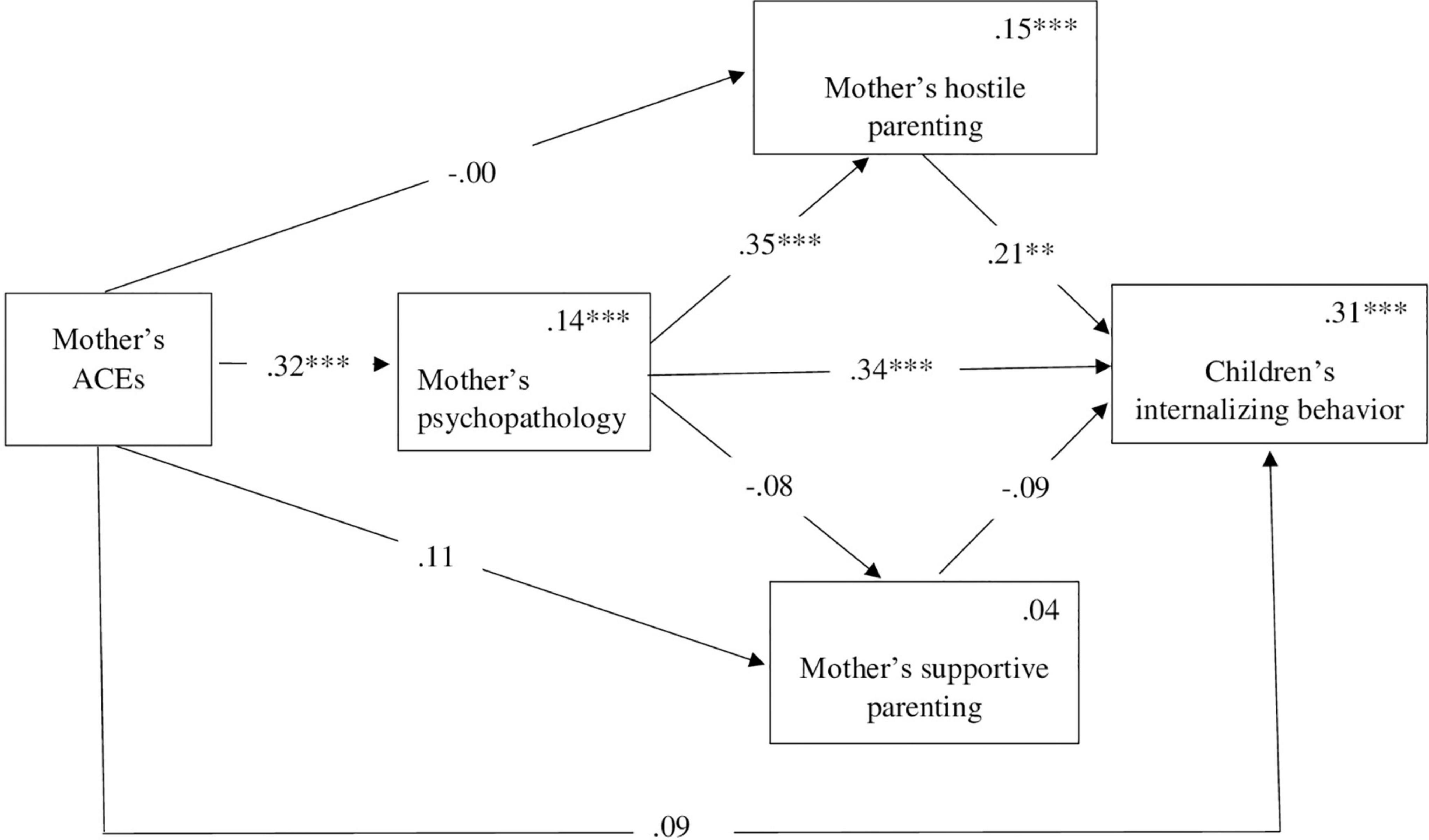
Figure 2. Mediation model for the association between the mother’s ACEs internalizing behavior via the mother’s psychopathology and her hostile or supportive parenting. Numbers above the lines are standardized coefficients. Numbers in the upper right-hand corner in the rectangles present R2. While not presented in the figure, the child’s age and gender were included as covariates in the model. **p < 0.01, ***p < 0.001.
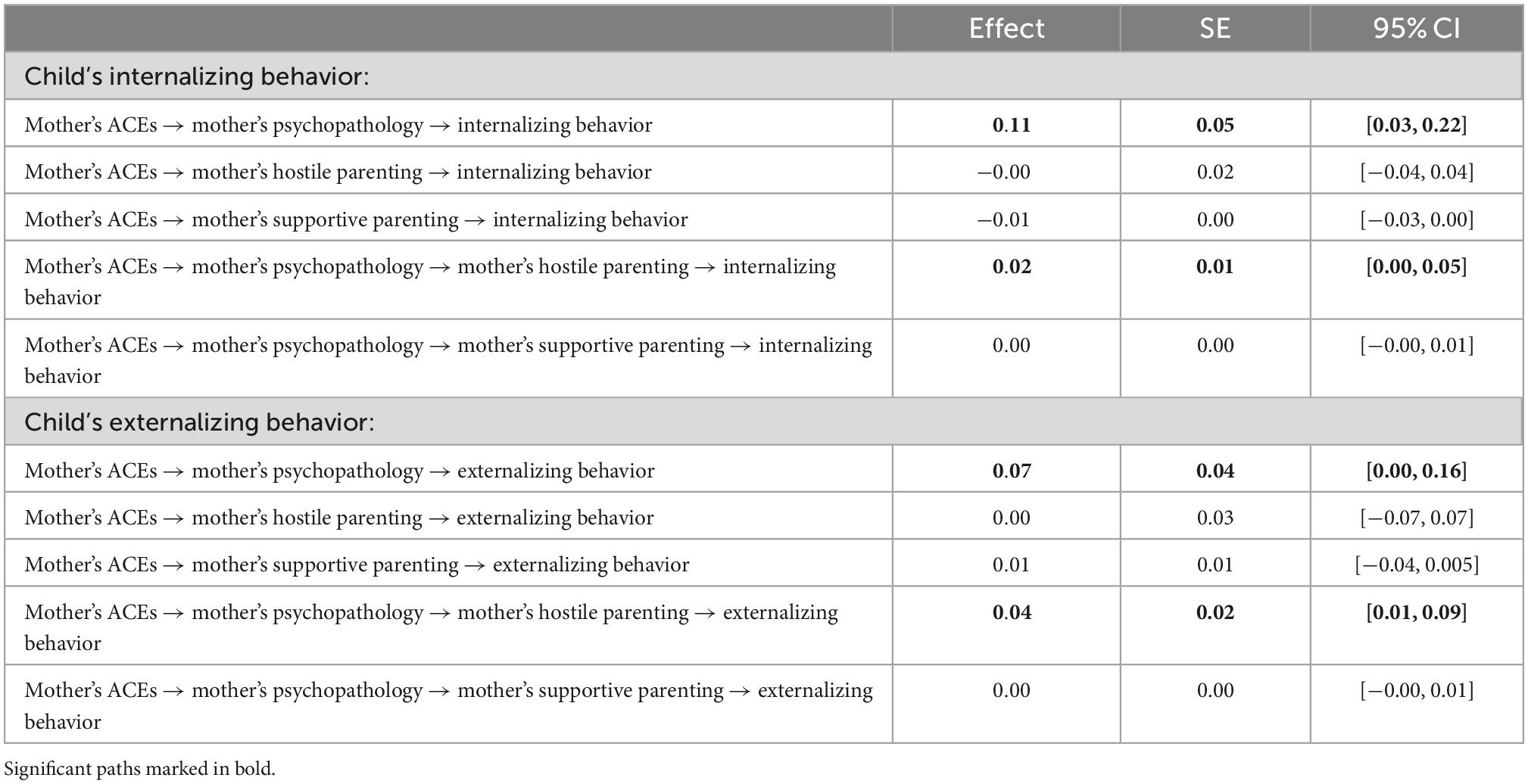
Table 2. Indirect paths between mother’s adverse childhood experiences (ACEs) and child’s behavior via mother’s psychopathology and parenting.
The model predicting the child’s externalizing behavior from the mother’s ACEs via her psychopathology symptoms and her hostile and supportive parenting was also significant [F (6, 138) = 9.64, p < 0.001] and accounted for 29% of the variance. As Table 2 indicates, the pattern of the indirect paths was similar to those for internalizing behavior. No direct effect was found between the mother’s ACEs and the child’s externalizing behavior. The indirect link between the mother’s ACEs and the children’s externalizing behavior via the mother’s psychopathology symptoms was significant. Furthermore, as predicted, the link between the mothers’ ACEs and the children’s externalizing behavior was mediated sequentially via the mothers’ psychopathology and hostile parenting. Nevertheless, the indirect sequential path through the mothers’ psychopathology symptoms and supportive parenting was not significant. Thus, the higher the mother scored on having experienced ACEs, the more severe her psychopathology was. This psychopathology was linked to more hostile parenting, which was linked to more externalizing behavior among the children. The indirect links between the mother’s ACEs and her children’s externalizing behavior via the mother’s hostile or supportive parenting, on their own, were not significant. Figure 3 presents the direct and indirect links between the model’s variables. While not presented in the figure for the sake of visual clarity, the child’s age and gender were included in the models as covariates.
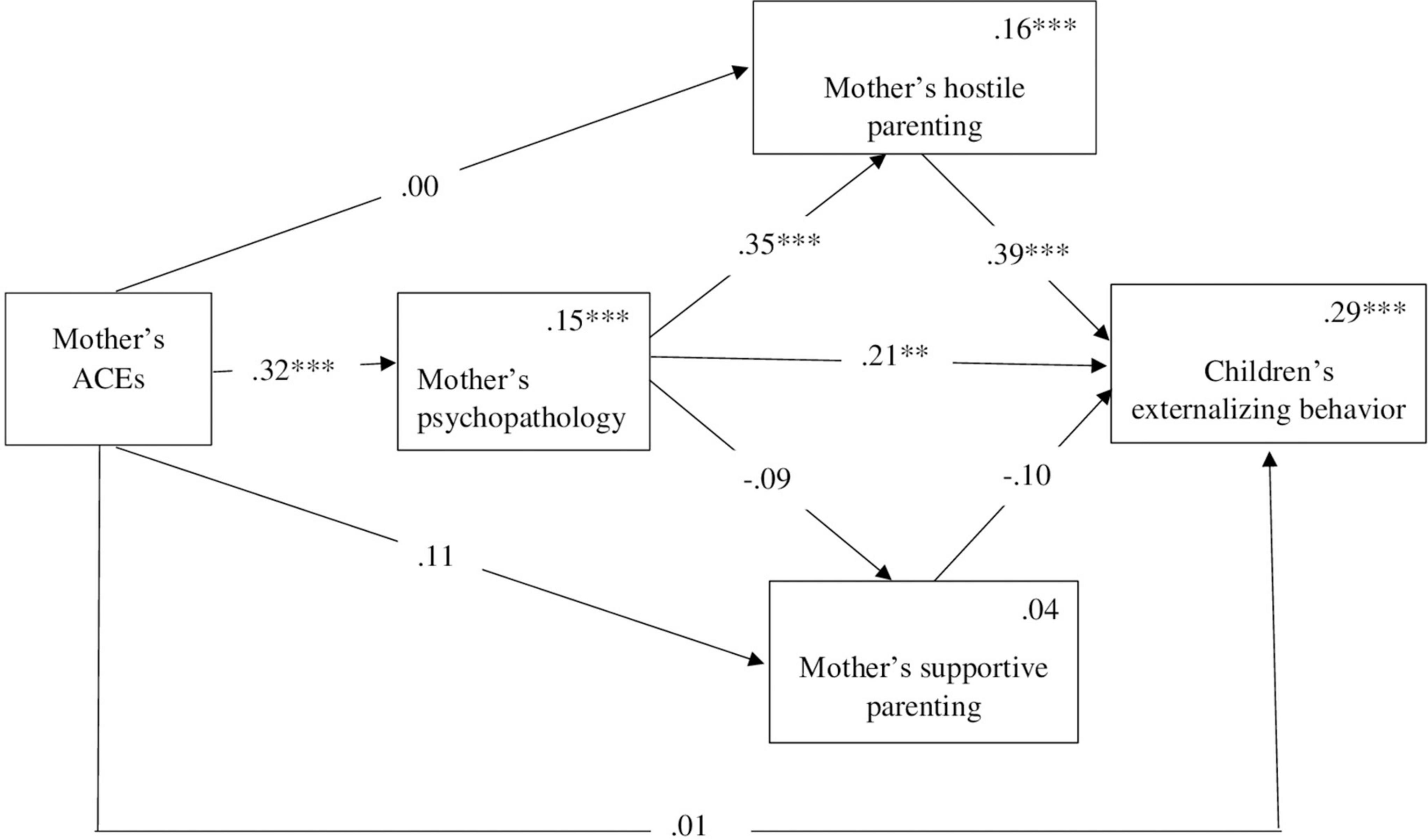
Figure 3. Mediation model for the association between the mother’s ACEs externalizing behavior via the mother’s psychopathology and her hostile or supportive parenting. Numbers above the lines are standardized coefficients. Numbers in the upper right-hand corner in the rectangles present R2. While not presented in the figure, the child’s age and gender were included as covariates in the model. **p < 0.01, ***p < 0.001.
The study’s aim was to explore the potential mediating mechanisms accounting for the intergenerational association between a mother’s early adverse experiences and her child’s behavior problems. We focused on the mother’s psychopathology and her hostile or supportive parenting behavior as mediators of this association. In support of H1 we found that mothers with higher ACE scores reported more psychopathology symptoms and more internalizing behavior in their children. However, mothers’ ACEs were not associated with their reports of their parenting behaviors style, either supportive or hostile, or with the children’s externalizing behaviors. Supporting H2, we found two indirect paths between the mother’s ACEs and the child’s behavior problems. The first indirect path was via the mother’s psychopathology. Specifically, higher ACE scores led to more psychopathology symptoms and distress, which, in turn, predicted more internalizing and externalizing behavior in the children. The second indirect path was a sequential mediation via the mother’s psychopathology and hostile parenting. The more ACEs the mother had as a child, the more psychological distress she reported as an adult. The mother’s psychological distress led to hostile parenting, which, in turn, led to more internalizing and externalizing behavior in her child. Interestingly, neither of the parenting behaviors on their own, supportive or hostile, mediated the association between the mother’s ACEs and the child’s internalizing and externalizing behavior. In addition, we found no sequential mediation via the mother’s psychopathology symptoms and supportive parenting on the association between the mother’s ACEs and the child’s internalizing and externalizing behavior.
The correlation between the mother’s ACEs and her psychopathology symptoms that we found joins substantial empirical evidence of the association between ACEs and later psychopathology (2, 3, 6, 22, 53, 94), particularly following the outbreak of COVID-19 (41, 42, 44, 45). This result suggests that experiencing abuse, neglect, and household dysfunction prior to age 18 increases the risk of later emotional difficulties for mothers, particularly during stressful times such as the outbreak of COVID-19. Notably, in the current study the association between the mother’s adverse experiences and her later distress emerged even in a low-risk sample, highlighting the profound, devastating, and long-lasting implications of early adverse circumstances even in relatively robust groups. To conclude, our findings, as well as other evidence, support current trans-diagnostic bio-socio-emotional understandings that childhood adversity interferes with the mother’s ability to self-regulate and deal with stress, increasing her risk for psychopathology (4).
The association between the mother’s ACEs and her child’s internalizing behavior resonates with previous findings about the intergenerational transmission of trauma (11, 17, 55). It confirms that children of mothers with adverse childhood experiences are at heightened risk for behavior problems. Interestingly, and contrary to previous studies, we did not find a simple correlation between the mothers’ ACEs and the child’s externalizing behavior. We suggest that this particular finding may reflect the special times of COVID-19 and its ramifications for children’s and adults’ mental health. It is possible that the pandemic-related rise in children’s fears, worries, anxiety, and depression (95–98) led mothers to report more internalizing behavior. Furthermore, it is possible that mothers with more ACEs were more distressed by the pandemic and may have projected their own fears, concerns, and negative affect onto their children, resulting in more reports of internalizing behaviors. These mothers may have also unconsciously reinforced their children’s internalizing difficulties by overanalyzing their behavior, looking for signs of distress and being overprotective of them (18). Importantly, although the simple correlation between the mother’s ACEs and her child’s externalizing behavior was not significant, the indirect links via the mother’s psychopathology symptoms and hostile parenting were significant, as we will discuss later.
The mothers’ psychopathology played a key role in mediating the association between their history of trauma and the children’s behavior. This finding accords with a growing number of studies demonstrating that the mother’s psychopathology creates a path through which her early adverse experiences impact her child (57, 99, 100). Moreover, whereas the majority of previous studies focused on young children from Western countries, our study included older children and was conducted in Israel, which is unique in its cultural composition, consisting of Westernized and non-Westernized cultural groups. Thus, our findings support and expand previous research indicating that the mother’s psychological distress is an important factor accounting for the intergenerational transmission of the adverse events she experienced during her childhood to her child.
Importantly, and as hypothesized, we found that the mother’s psychopathology symptoms not only mediated the association between her ACEs and the child’s internalizing and externalizing behaviors, but also was involved in sequential mediation with the mother’s hostile parenting. Thus, when a mother experienced more trauma as a child, she was likely to experience more distress and report more mental difficulties. These outcomes were linked with harsher, more hostile and agitated parenting, which predicted more reports about the problematic behavior of her child. Note that the mother’s hostile parenting on its own did not mediate the link between her ACEs and her child’s behavior problems. This finding highlights the importance of the mother’s psychopathology as a leading factor that can put both parenting and the child’s well-being at risk (101). In line with previous research embedded within attachment theory [see Cooke et al. and Verhage et al. (55, 102) for a review], we argue that ACEs may evoke painful attachment-related memories of trauma, loss, and unfavorable care, all contributing to the increased risk of the mother’s developing an insecure attachment style. Insecure attachment and unprocessed traumatic memories may lead to affect dysregulation, which, in turn, may interfere with the mother’s ability to provide sensitive parenting. Insensitive parenting may lead to the mother’s limited ability to regulate her child’s emotions, putting the child’s development and socioemotional adjustment at risk (103).
The sequential mediation through the mother’s psychopathology symptoms and hostile parenting we documented varies from the results of a recent longitudinal study by Shih et al. (19) that examined sequential mediation of the link between maternal ACEs and children’s internalizing behaviors at ages 4–6 via maternal anxiety and positive parenting. Shih and her colleagues reported that the mother’s anxiety and positive parenting mediated the link between the mother’s adversity and the child’s internalizing behavior separately, not sequentially. The differences in the results could be due, in part, to differences in the children’s ages and the different parenting practices that were measured. Nevertheless, our innovative finding needs further replication.
Interestingly, supportive and caring parenting, although associated with the children’s internalizing and externalizing behavior, did not mediate the association between the mother’s ACEs and the child’s internalizing and externalizing behavior on their own, or sequentially with the mother’s psychopathology symptoms. These findings echo previous results that found no associations between the mother’s ACEs and positive parenting practices (71) or sensitive and scaffolding parenting (104). However, it contradicts previous findings demonstrating that positive parenting (i.e., the fostering of cognitive growth) mediated the link between the mothers’ ACEs and their pre-schoolers’ internalizing behavior (19). (71) argued that their failure to find an association between ACEs and positive parenting reflected a social desirability bias and the over-reporting of positive parenting practices, which may be the case in our study as well. Alternatively, the lack of association may also be linked with the newly emerging empirical and clinical data regarding the suppressing effect of early childhood adversity on the dopamine system and the parental reward system, which may lead to the inability to enjoy and report positive parenting practices (74).
The current study joins and expands the literature on the possible pathways through which mothers’ ACEs might be a risk for their children’s behavior. Its main added contribution lies in identifying the sequential mediation of the link between the mother’s ACEs and the child’s internalizing and externalizing behavior first by the mother’s psychopathology and then by her hostile parenting. It highlights the complicated ways in which adversity is transferred from caregiver to offspring. Furthermore, this study emphasizes the mother’s psychological distress as a crucial factor in the association between her history of being hurt and her child’s well-being, mediated on its own, and also interfering with the mother’s parenting.
Nevertheless, these contributions need to be viewed in light of some limitations. First, although the ACE questionnaire is considered to be a reliable measure of childhood adversity (105), it is based on retrospective reports and prone to recall bias. Second, all of the study’s measures were based on the mothers’ self-reports. Thus, there is a risk of shared method variance as well as desirability bias. Future studies can benefit from using multiple informants including fathers, teachers, and the children themselves. Third, our sample was relatively modest in size and homogeneous in terms of the families’ SES, the mothers’ educational level, and two-parent households. In addition, we used a convenience sample of volunteers who felt comfortable using social media and were willing to complete an online survey. Moreover, the data were collected during the COVID-19 pandemic, which affected the socioemotional adaptation and functioning of the parents and children. These characteristics of our sample limit our ability to generalize the findings. They also make it difficult for us to draw broad-based conclusions about the intergenerational effects of the mothers’ ACEs on other family contexts among less advantaged populations and during less stressful times. Fourth, the study included only mothers. Additional studies that examine the role of fathers’ ACEs on their children’s behavior are clearly needed. Finally, the data were collected concurrently, precluding causal, directional, and reciprocal inferences. While our underlying assumption was that maternal psychopathology leads to negative parenting that is hostile and less supportive, and behavior problems in children, it is equally possible that the opposite is true: children’s difficult behavior leads to maternal psychopathology and negative parenting. Longitudinal designs with larger and more heterogeneous samples are needed to test alternative models and further understand the mechanisms that explain the association between the caregiver’s early adverse experiences and their child’s difficulties later in life. In addition, longitudinal designs that follow children who have been exposed to ACEs into adulthood and parenthood can help us better understand the developmental trajectory associated with ACEs.
Given the increased risk documented in the literature and found in our study associated with the mother’s adverse childhood experiences, her mental health, and her children’s socioemotional adjustment, healthcare providers for families and children are advised to screen and assess mothers’ (and probably fathers’) past traumatic experiences. Interventions for a parent who experienced adversity or trauma can help the parent better cope with his/her history and can also be protective for the child. For example, trauma informed care that includes validation and recognition of the effects of traumatic events, common coping strategies, and effective treatments (106) can help mothers limit the impact that their negative history has on their children.
Furthermore, treatment interventions for children need to include an assessment of the mother’s early childhood experiences, particularly her ACEs, but also her attachment-related experiences and scripts, which are linked with an increased risk of her psychopathology and, consequently, her parenting. Evidence-based treatment interventions that combine an attachment and trauma lens for young children [e.g., ABC, (107); COS, (108); CPP, (109); GABI, (110)] and adolescents [ABFT, (111)] may serve as guidelines for universal and specialized treatment plans for traumatized mothers and their children.
Finally, it is important to remember that the intergenerational transmission of childhood adversity can be broken (112). Research and clinical work have demonstrated the utility of assessing and utilizing parents’ positive childhood experiences, such as the approach of “Angels in the Nursery” (113, 114), as a source of resilience when working with parents who suffered early trauma. Furthermore, parents’ reflective functioning and mentalization skills have proven effective in breaking the link between parents’ childhood trauma and children’s insecure attachment (115). Thus, interventions such as the Family Cycle (116) or MBT-C (117) that enhance the parents’ reflective functioning and mentalization provide guidelines for intervening and can be used to improve parents’ understanding of their children’s emotional and attachment-related needs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Academic College of Tel Aviv Yaffo’s Ethics Committee approval reference #2020079. The patients/participants provided their written informed consent to participate in this study.
Both authors listed have made an equally substantial, direct, and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Centers for Disease Control and Prevention [CDC]. Adverse Childhood Experience Resources (ACEs). (2016). Available online at: https://www.cdc.gov/violenceprevention/acestudy/resources.html (accessed October 10, 2017).
2. Bellis M, Hughes K, Ford K, Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. (2019) 4:e517–28. doi: 10.1016/S2468-2667(19)30145-8
3. Hughes K, Bellis M, Hardcastle K, Sethi D, Butchart A, Mikton C Dunne M. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. (2017) 2:e356–66. doi: 10.1016/S2468-2667(17)30118-4
4. Hoppen T, Chalder T. Childhood adversity as a transdiagnostic risk factor for affective disorders in adulthood: a systematic review focusing on biopsychosocial moderating and mediating variables. Clin Psychol Rev. (2018) 65:81–151. doi: 10.1016/j.cpr.2018.08.002
5. Racine N, Byles H, Killam T, Ereyi-Osas W Madigan S. Asking about childhood adversity in the prenatal care setting: cross-sectional associations with maternal health and mental health outcomes. Mater Child Health J. (2022) 26:994–1004. doi: 10.1007/s10995-021-03301-5
6. Choi K, Sikkema K. Childhood maltreatment and perinatal mood and anxiety disorders: a systematic review. Trauma Viol Abuse. (2016) 17:427–53. doi: 10.1177/1524838015584369
7. Pasalich D, Cyr M, Zheng Y, McMahon R Spieker S. Child abuse history in teen mothers and parent–child risk processes for offspring externalizing problems. Child Abuse Neglect. (2016) 56:89–98. doi: 10.1016/j.chiabu.2016.04.011
8. Scully C, McLaughlin J Fitzgerald A. The relationship between adverse childhood experiences, family functioning, and mental health problems among children and adolescents: a systematic review. J Family Ther. (2020) 42:291–316. doi: 10.1111/1467-6427.12263
9. Haynes E, Crouch E, Probst J, Radcliff E, Bennett K Glover S. Exploring the association between a parent’s exposure to Adverse Childhood Experiences (ACEs) and outcomes of depression and anxiety among their children. Child Youth Serv Rev. (2020) 113:105013. doi: 10.1016/j.childyouth.2020.105013
10. Uddin J, Alharbi N, Uddin H, Hossain M, Hatipoglu S, Long D Carson A. Parenting stress and family resilience affect the association of adverse childhood experiences with children’s mental health and attention-deficit/hyperactivity disorder. J Affect Disord. (2020) 272:104–9. doi: 10.1016/j.jad.2020.03.132
11. McDonald S, Madigan S, Racine N, Benzies K, Tomfohr L Tough S. Maternal adverse childhood experiences, mental health, and child behaviour at age 3: the all our families community cohort study. Prevent Med. (2019) 118:286–94. doi: 10.1016/j.ypmed.2018.11.013
12. Doi S, Fujiwara T, Isumi A. Association between maternal adverse childhood experiences and mental health problems in offspring: an intergenerational study. Dev Psychopathol. (2021) 33:1041–58. doi: 10.1017/S0954579420000334
13. Condon E, Holland M, Slade A, Redeker N, Mayes L Sadler L. Maternal adverse childhood experiences, family strengths, and chronic stress in children. Nurs Res. (2019) 68:189. doi: 10.1097/NNR.0000000000000349
14. Cooke J, Racine N, Pador P, Madigan S. Maternal adverse childhood experiences and child behavior problems: a systematic review. Pediatrics. (2021) 148:e2020044131. doi: 10.1542/peds.2020-044131
15. Esteves K, Jones C, Wade M, Callerame K, Smith A, Theall K Drury S. Adverse childhood experiences: implications for offspring telomere length and psychopathology. Am J Psychiatry. (2020) 177:47–57. doi: 10.1176/appi.ajp.2019.18030335
16. Madigan S, Wade M, Plamondon A, Maguire J Jenkins J. Maternal adverse childhood experience and infant health: Biomedical and psychosocial risks as intermediary mechanisms. J Pediatr. (2017) 187:282–9. doi: 10.1016/j.jpeds.2017.04.052
17. Stepleton K, Bosk E, Duron J, Greenfield B, Ocasio K MacKenzie M. Exploring associations between maternal adverse childhood experiences and child behavior. Child Youth Serv Rev. (2018) 95:80–7. doi: 10.1016/j.childyouth.2018.10.027
18. Herbell K, Bloom T. A qualitative metasynthesis of mothers’ adverse childhood experiences and parenting practices. J Pediatr Health Care. (2020) 34:409–17. doi: 10.1016/j.pedhc.2020.03.003
19. Shih E, Ahmad S, Bush N, Roubinov D, Tylavsky F, Graff C, LeWinn K. A path model examination: maternal anxiety and parenting mediate the association between maternal adverse childhood experiences and children’s internalizing behaviors. Psychol Med. (2021) [Online ahead of print]. doi: 10.1017/S0033291721001203
20. Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V Marks J. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prevent Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
21. Gilbert L, Breiding M, Merrick M, Thompson W, Ford D, Dhingra S Parks S. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prevent Med. (2015) 48:345–49. doi: 10.1016/j.amepre.2014.09.006
22. Van der Feltz-Cornelis C, Potters E, van Dam A, Koorndijk R Elfeddali I. Adverse Childhood Experiences (ACE) in outpatients with anxiety and depressive disorders and their association with psychiatric and somatic comorbidity and revictimization. Cross-sectional observational study. J Affect Disord. (2019) 246:458–64. doi: 10.1016/j.jad.2018.12.096
23. Cloitre M, Khan C, Mackintosh M, Garvert D, Henn-Haase C, Falvey E, Saito J. Emotion regulation mediates the relationship between ACES and physical and mental health. Psychol Trauma. (2019) 11:82–9. doi: 10.1037/tra0000374
24. Pilowsky D, Keyes K Hasin D. Adverse childhood events and lifetime alcohol dependence. Am J Public Health. (2009) 99:258–63. doi: 10.2105/AJPH.2008.139006
25. Mersky J, Topitzes J Reynolds A. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the US. Child Abuse Neglect. (2013) 37:917–25. doi: 10.1016/j.chiabu.2013.07.011
26. Maaranen P, Tanskanen A, Haatainen K, Koivumaa-Honkanen H, Hintikka J Viinamäki H. Somatoform dissociation and adverse childhood experiences in the general population. J Nervous Mental Dis. (2004) 192:337–42. doi: 10.1097/01.nmd.0000126700.41047.83
27. Powers A, Cross D, Fani N Bradley B. PTSD, emotion dysregulation, and dissociative symptoms in a highly traumatized sample. J Psychiatr Res. (2015) 61:174–9. doi: 10.1016/j.jpsychires.2014.12.011
28. Merrick M, Ports K, Ford D, Afifi T, Gershoff E Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Neglect. (2017) 69:10–9. doi: 10.1016/j.chiabu.2017.03.016
29. Hinesley J, Amstadter A, Sood A, Perera R, Ramus R, Kornstein S. Adverse childhood experiences, maternal/fetal attachment, and maternal mental health. Womens Health Rep. (2020) 1:550–5. doi: 10.1089/whr.2020.0085
30. McDonnell C, Valentino K. Intergenerational effects of childhood trauma: evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat. (2016) 21:317–26. doi: 10.1177/1077559516659556
31. Muzik M, Brier Z, Menke RA, Davis MT Sexton MB. Longitudinal suicidal ideation across 18-months postpartum in mothers with childhood maltreatment histories. J Affect Disord. (2016) 204:138–45. doi: 10.1016/j.jad.2016.06.037
32. McGowan P. Epigenomic mechanisms of early adversity and HPA dysfunction: considerations for PTSD research. Front Psychiatry. (2013) 4:110. doi: 10.3389/fpsyt.2013.00110
33. Tursich M, Neufeld R, Frewen P, Harricharan S, Kibler J, Rhind S, Lanius R. Association of trauma exposure with proinflammatory activity: a transdiagnostic meta-analysis. Transl Psychiatry. (2014) 4:e413. doi: 10.1038/tp.2014.56
34. Dvir Y, Ford J, Hill M Frazier J. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Rev Psychiatry. (2014) 22:149. doi: 10.1097/HRP.0000000000000014
35. Gladstone G, Parker G, Mitchell P, Malhi G, Wilhelm K, Austin M. Implications of childhood trauma for depressed women: an analysis of pathways from childhood sexual abuse to deliberate self-harm and revictimization. Am J Psychiatry. (2004) 161:1417–25. doi: 10.1176/appi.ajp.161.8.1417
36. Gavin B, Lyne J, McNicholas F. Mental health and the COVID-19 pandemic. Ir J Psychol Med. (2020) 37:156–8. doi: 10.1017/ipm.2020.72
37. Holmes E, O’Connor R, Perry V, Tracey I, Wessely S, Arseneault L Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
38. Torales J, O’Higgins M, Castaldelli-Maia J Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
39. Central Bureau of Statistics [CBS], Israeli Central Bureau of Statistics Publication, Public Use File (PUF). (2020). Available online at: https://www.cbs.gov.il/he/Statistical/statistical-182-corona.pdf.
40. Panchal U, Salazar de Pablo G, Franco M, Moreno C, Parellada M, Arango C Fusar-Poli P. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. (2021) [Online ahead of print] doi: 10.1007/s00787-021-01856-w
41. Doom J, Seok D, Narayan A Fox K. Adverse and benevolent childhood experiences predict mental health during the COVID-19 pandemic. Advers Resilience Sci. (2021) 2:193–204. doi: 10.1007/s42844-021-00038-6
42. Gotlib I, Borchers L, Chahal R, Gifuni A, Teresi G Ho T. Early life stress predicts depressive symptoms in adolescents during the COVID-19 pandemic: the mediating role of perceived stress. Front Psychol. (2021) 11:603748. doi: 10.3389/fpsyg.2020.603748
43. Dollberg D, Hanetz-Gamliel K, Levy S. COVID-19, child’s behavior problems, and mother’s anxiety and mentalization: a mediated moderation model. Curr Psychol. (2021) [Online ahead of print] doi: 10.1007/s12144-021-02476-y
44. Chi X, Becker B, Yu Q, Willeit P, Jiao C, Huang L, Solmi M. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front Psychiatry. (2020) 11:803. doi: 10.3389/fpsyt.2020.00803
45. Wade M, Prime H, Johnson D, May S, Jenkins J Browne D. The disparate impact of COVID-19 on the mental health of female and male caregivers. Soc Sci Med. (2021) 275:113801. doi: 10.1016/j.socscimed.2021.113801
46. Trapolini T, McMahon C, Ungerer J. The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child. (2007) 33:794–803. doi: 10.1111/j.1365-2214.2007.00739.x
47. Vostanis P, Graves A, Meltzer H, Goodman R, Jenkins R Brugha T. Relationship between parental psychopathology, parenting strategies and child mental health. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:509–14. doi: 10.1007/s00127-006-0061-3
48. Goodman S. Intergenerational transmission of depression. Annu Rev Clin Psychol. (2020) 16, 213–38. doi: 10.1146/annurev-clinpsy-071519-113915
49. Hails K, Reuben J, Shaw D, Dishion T, Wilson M. Transactional associations among maternal depression, parent–child coercion, and child conduct problems during early childhood. J Clin Child Adolesc Psychol. (2018) 47:S291–305. doi: 10.1080/15374416.2017.1280803
50. Cooklin A, Giallo R, D’Esposito F, Crawford S, Nicholson J. Postpartum maternal separation anxiety, overprotective parenting, and children’s social-emotional well-being: longitudinal evidence from an Australian cohort. J Family Psychol. (2013) 27, 618–28. doi: 10.1037/a0033332
51. Hartzell G, Stenson A, van Rooij S, Kim Y, Vance L, Hinrichs R, Jovanovic T. Intergenerational effects of maternal PTSD: Roles of parenting stress and child sex. Psychol Trauma. (2020) 14:1089–98. doi: 10.1037/tra0000542
52. Letourneau N, Dewey D, Kaplan B, Ntanda H, Novick J, Thomas J APrON Study Team. Intergenerational transmission of adverse childhood experiences via maternal depression and anxiety and moderation by child sex. J Dev Origins Health Dis. (2019) 10:88–99. doi: 10.1017/S2040174418000648
53. Racine N, Devereaux C, Cooke J, Eirich R, Zhu J Madigan S. Adverse childhood experiences and maternal anxiety and depression: a meta-analysis. BMC Psychiatry. (2021) 21:28. doi: 10.1186/s12888-020-03017-w
54. Wang L, Yu Z, Chen W, Zhang J Bettencourt A. Higher exposure to childhood adversity associates with lower adult flourishing. BMC Public Health. (2022) 22:612. doi: 10.1186/s12889-022-13063-6
55. Cooke J, Racine N, Plamondon A, Tough S Madigan S. Maternal adverse childhood experiences, attachment style, and mental health: pathways of transmission to child behavior problems. Child Abuse Neglect. (2019) 93:27–37. doi: 10.1016/j.chiabu.2019.04.011
56. Ma X, Biaggi A, Sacchi C, Lawrence A, Chen P, Pollard R, Dazzan P. Mediators and moderators in the relationship between maternal childhood adversity and children’s emotional and behavioural development: a systematic review and meta-analysis. Psychol Med. (2022) 52:1817–37. doi: 10.1017/S0033291722001775
57. Roubinov D, Browne D, LeWinn K, Lisha N, Mason W Bush N. Intergenerational transmission of maternal childhood adversity and depression on children’s internalizing problems. J Affect Disord. (2022) 308:205–212. doi: 10.1016/j.jad.2022.04.030
58. Smith A, Cross D, Winkler J, Jovanovic T Bradley B. Emotional dysregulation and negative affect mediate the relationship between maternal history of child maltreatment and maternal child abuse potential. J Family Viol. (2014) 29:483–94. doi: 10.1007/s10896-014-9606-5
59. Bailey H, DeOliveira C, Wolfe V, Evans E, Hartwick C. The impact of childhood maltreatment history on parenting: a comparison of maltreatment types and assessment methods. Child Abuse Neglect. (2012) 36:236–46. doi: 10.1016/j.chiabu.2011.11.005
60. Fuchs A, Möhler E, Resch F, Kaess M. Impact of a maternal history of childhood abuse on the development of mother–infant interaction during the first year of life. Child Abuse Neglect. (2015) 48:179–89. doi: 10.1016/j.chiabu.2015.05.023
61. Rodriguez V, Are F, Madden A, Shaffer A Suveg C. Intergenerational transmission of childhood maltreatment mediated by maternal emotion dysregulation. J Child Family Stud. (2021) 30:2068–75. doi: 10.1007/s10826-021-02020-3
62. Mitani H. Effects of maternal adverse child experiences on parental maltreatment of children: An empirical study of mediating factors among Japanese mothers. Child Family Soc Work. (2022) 27:422–34. doi: 10.1111/cfs.12893
63. Larkin H, Shields J Anda R. The health and social consequences of adverse childhood experiences (ACE) across the lifespan: an introduction to prevention and intervention in the community. J Prevent Intervent Commun. (2012) 40:263–70. doi: 10.1080/10852352.2012.707439
64. Lomanowska A, Boivin M, Hertzman C, Fleming A. Parenting begets parenting: a neurobiological perspective on early adversity and the transmission of parenting styles across generations. Neuroscience. (2017) 342:120–139. doi: 10.1016/j.neuroscience.2015.09.029
65. Jiwani Z, Drylewski G, Sharma S, Ahun M, Thapa S, Steele M. Adverse childhood experiences and maternal self-efficacy: examining the mediating role of intimate partner violence and the moderating role of caste membership in rural India. Infant Mental Health J. (2022) 43:546–57. doi: 10.1002/imhj.21997
66. Rowell T Neal-Barnett A. A systematic review of the effect of parental adverse childhood experiences on parenting and child psychopathology. J Child Adolesc Trauma. (2021) 15:167–80. doi: 10.1007/s40653-021-00400-x
68. Khan M, Renk K. Mothers’ adverse childhood experiences, depressive symptoms, parenting, and attachment as predictors of young children’s problems. J Child Custody. (2019) 16:268–90. doi: 10.1080/15379418.2019.1575318
69. Murphy A, Steele M, Dube S, Bate J, Bonuck K, Meissner P Steele H. Adverse childhood experiences (ACEs) questionnaire and adult attachment interview (AAI): implications for parent child relationships. Child Abuse Neglect. (2014) 38:224–33. doi: 10.1016/j.chiabu.2013.09.004
70. Van Ijzendoorn M Bakermans-Kranenburg M. Bridges across the intergenerational transmission of attachment gap. Curr Opin Psychol. (2019) 25:31–36. doi: 10.1016/j.copsyc.2018.02.014
71. Lange B, Callinan L Smith M. Adverse childhood experiences and their relation to parenting stress and parenting practices. Commun Mental Health J. (2019) 55, 651–662. doi: 10.1007/s10597-018-0331-z
72. Mikulincer M Shaver P. Attachment, caregiving, and parenting. In: O. Taubman–Ben-Ari editor. Pathways and Barriers to Parenthood. Berlin: Springer (2019). doi: 10.1007/978-3-030-24864-2_18
73. Steele H, Bate J, Steele M, Dube S, Danskin K, Knafo H Murphy A. Adverse childhood experiences, poverty, and parenting stress. Can J Behav Sci. (2016) 48:32–8. doi: 10.1037/cbs0000034
74. Hughes D, Baylin J. (2012). Brain-Based Parenting: The Neuroscience of Caregiving for Healthy Attachment. New York, NY: W.W Norton & Company.
75. McLeod B, Weisz J, Wood J. Examining the association between parenting and childhood depression: a meta-analysis. Clin Psychol Rev. (2007) 27:986–1003. doi: 10.1016/j.cpr.2007.03.001
76. Schwartz O, Byrne M, Simmons J, Whittle S, Dudgeon P, Yap M Allen N. Parenting during early adolescence and adolescent-onset major depression: a 6-year prospective longitudinal study. Clin Psychol Sci. (2014) 2:272–86. doi: 10.1177/2167702613505531
77. Weymouth B, Buehler C, Zhou N, Henson R. A meta-analysis of parent–adolescent conflict: disagreement, hostility, and youth maladjustment. J Family Theory Rev. (2016) 8:95–112. doi: 10.1111/jftr.12126
78. Yap M Jorm A. Parental factors associated with childhood anxiety, depression, and internalizing problems: a systematic review and meta-analysis. J Affect Disord. (2015) 175:424–40. doi: 10.1016/j.jad.2015.01.050
79. Rothenberg W, Lansford J, Bornstein M, Chang L, Deater-Deckard K, Di Giunta L Bacchini D. Effects of parental warmth and behavioral control on adolescent externalizing and internalizing trajectories across cultures. J Res Adolesc. (2020) 30:835–55 doi: 10.1111/jora.12566
80. Madigan S, Wade M, Plamondon A Jenkins J. Maternal abuse history, postpartum depression and parenting: links with preschoolers’ internalizing problems. Infant Mental Health J. (2015) 36:146–155. doi: 10.1002/imhj.21496
81. Plant D, Jones F, Pariante C Pawlby S. Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. Br J Psychiatry. (2017) 211:144–50. doi: 10.1192/bjp.bp.117.198721
82. Bödeker K, Fuchs A, Führer D, Kluczniok D, Dittrich K, Reichl C, Resch F. Impact of maternal early life maltreatment and maternal history of depression on child psychopathology: mediating role of maternal sensitivity? Child Psychiatry Hum Dev. (2019) 50:278–90. doi: 10.1007/s10578-018-0839-z
83. Esteves K, Gray S, Theall K Drury S. Impact of physical abuse on internalizing behavior across generations. J Child Family Stud. (2017) 26:2753–61. doi: 10.1007/s10826-017-0780-y
84. Aktar E, Qu J, Lawrence P, Tollenaar M, Elzinga B, Bögels S. Fetal and infant outcomes in the offspring of parents with perinatal mental disorders: earliest influences. Front Psychiatry. (2019) 10:391. doi: 10.3389/fpsyt.2019.00391
85. McCabe J. Maternal personality and psychopathology as determinants of parenting behavior: a quantitative integration of two parenting literatures. Psychol Bull. (2014) 140:722–50. doi: 10.1037/a0034835
86. Røhder K, MacBeth A, Agnete Davidsen K, Gumley A, Brennan J, George C Harder S. Antenatal caregiving representations and perinatal behavior in mothers with severe lifetime psychopathology. Infant Mental Health J. (2020) 41:56–68. doi: 10.1002/imhj.21824
87. Derogatis L. Brief Symptom Inventory. Baltimore, MD: Clinical Psychometric Research (1978). doi: 10.1037/t00789-000
88. Derogatis L, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med. (1983) 13:595–605. doi: 10.1017/S0033291700048017
89. Lovejoy M, Weis R, O’Hare E, Rubin E. Development and initial validation of the Parent Behavior Inventory. Psychol Assess. (1999) 11:534. doi: 10.1037/1040-3590.11.4.534
90. Achenbach T, Rescorla L. Manual for the ASEBA preschool forms and Profiles. Burlington, VT: University of Vermont (2000).
91. Achenbach T, Rescorla L. Manual for the Achenbach System of Empirically Based Assessment School-Age Forms Profiles. Burlington, VT: ASEBA (2001).
92. Zilber N, Auerbach J, Lerner Y. Israeli norms for the achenbach child behavior checklist: comparison of clinically-referred and non-referred children. Isr J Psychiatry Relat Sci. (1994) 31:5–12.
93. Hayes A. Partial, conditional, and moderated mediation: quantification, inference, and interpretation. Commun Monogr. (2018) 85:4–40. doi: 10.1080/03637751.2017.1352100
94. Schäfer I, Fisher H. Childhood trauma and psychosis-what is the evidence? Dial Clin Neurosci. (2022) 13:360–5. doi: 10.31887/DCNS.2011.13.2/ischaefer
95. Domínguez-Álvarez B, López-Romero L, Isdahl-Troye A, Gómez-Fraguela J, Romero E. Children coping, contextual risk and their interplay during the COVID-19 pandemic: a Spanish case. Front Psychol. (2020) 11:577763. doi: 10.3389/fpsyg.2020.577763
96. Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. (2020) 14:917–20. doi: 10.1016/j.dsx.2020.05.044
97. Jiao W, Wang L, Liu J, Fang S, Jiao F, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. (2020) 221:264–266. doi: 10.1016/j.jpeds.2020.03.013
98. Orgilés M, Morales A, Delvecchio E, Mazzeschi C Espada J. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front Psychol. (2020) 11:579038. doi: 10.3389/fpsyg.2020.579038
99. Dennis C, Clohessy D, Stone A, Darnall B, Wilson A. Adverse childhood experiences in mothers with chronic pain and intergenerational impact on children. J Pain. (2019) 20, 1209–17. doi: 10.1016/j.jpain.2019.04.004
100. Zhang L, Mersky J Lee C. Intergenerational pathways linking mothers’ adverse childhood experiences and children’s social-emotional problems. Child Maltreat. (2022) [Online ahead of print] doi: 10.1177/10775595211067212
101. Hanetz-Gamliel K, Levy S, Dollberg D. Mediation of Mothers’ anxiety and parenting in Children’s behavior problems during COVID-19. J Child Family Stud. (2021) 30:2732–43. doi: 10.1007/s10826-021-02115-x
102. Verhage M, Schuengel C, Madigan S, Fearon R, Oosterman M, Cassibba R van IJzendoorn M. Narrowing the transmission gap: a synthesis of three decades of research on intergenerational transmission of attachment. Psychol Bull. (2016) 142:337–66. doi: 10.1037/bul0000038
103. Sroufe L. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev. (2005) 7:349–67. doi: 10.1080/14616730500365928
104. Coe J, Huffhines L, Contente C, Seifer R Parade S. Intergenerational effects of maternal childhood experiences on maternal parenting and infant developmental progress. J Dev Behav Pediatr. (2020) 41:619–27. doi: 10.1097/DBP.0000000000000835
105. Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. (2004) 45:260–73. doi: 10.1111/j.1469-7610.2004.00218.x
106. Oral R, Ramirez M, Coohey C, Nakada S, Walz A, Kuntz A Peek-Asa C. Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res. (2016) 79:227–33. doi: 10.1038/pr.2015.197
107. Dozier M, Roben C, Caron E, Hoye J Bernard K. Attachment and biobehavioral catch-up: an evidence-based intervention for vulnerable infants and their families. Psychother Res. (2018) 28:18–29. doi: 10.1080/10503307.2016.1229873
108. Powell B, Cooper G, Hoffman K, Marvin R. The circle of security project. In: Oppenheim D, Goldsmith DF, editors. Attachment Theory in Clinical Work with Children: Bridging the Gap Between Research and Practice. New York, NY: The Guilford Press (2007). p. 172–202.
109. Lieberman AF, Van Horn P. Psychotherapy with Infants and Young Children: Repairing the Effects of Stress and Trauma on Early Attachment. New York, NY: Guilford Press (2008).
110. Steele H, Murphy A, Bonuck K, Meissner P, Steele M. Randomized control trial report on the effectiveness of Group Attachment-Based Intervention (GABI©): improvements in the parent–child relationship not seen in the control group. Dev Psychopathol. (2019) 31:203–217. doi: 10.1017/S0954579418001621
111. Diamond G, Russon J Levy S. Attachment-based family therapy: a review of the empirical support. Family Process. (2016) 55, 595–610. doi: 10.1111/famp.12241
112. Woods-Jaeger B, Cho B, Sexton C, Slagel L Goggin K. Promoting resilience: breaking the intergenerational cycle of adverse childhood experiences. Health Educ Behav. (2018) 45:772–80. doi: 10.1177/1090198117752785
113. Lieberman A, Padrón E, Van Horn P, Harris W. Angels in the nursery: the intergenerational transmission of benevolent parental influences. Infant Mental Health J. (2005) 26:504–20. doi: 10.1002/imhj.20071
114. Narayan A, Lieberman A Masten A. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev. (2021) 85:101997. doi: 10.1016/j.cpr.2021.101997
115. Fonagy P, Steele M, Steele H, Higgitt A Target M. The Emanuel Miller memorial lecture 1992 the theory and practice of resilience. J Child Psychol Psychiatry. (1994) 35:231–57. doi: 10.1111/j.1469-7610.1994.tb01160.x
116. Stob V, Slade A, Adnopoz J Woolston J. The family cycle: Breaking the intergenerational transmission of trauma through mentalizing. J Infant Child Adolesc Psychother. (2020) 19:255–70. doi: 10.1080/15289168.2020.1786762
Keywords: mother’s ACEs, mother’s psychopathology, parenting behavior, child’s internalizing behavior, child’s externalizing behavior
Citation: Hanetz-Gamliel K and Dollberg DG (2022) Links between mothers’ ACEs, their psychopathology and parenting, and their children’s behavior problems–A mediation model. Front. Psychiatry 13:1064915. doi: 10.3389/fpsyt.2022.1064915
Received: 08 October 2022; Accepted: 07 December 2022;
Published: 22 December 2022.
Edited by:
Preeti Kandasamy, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), IndiaReviewed by:
Sowmyashree Mayur Kaku, St. John’s National Academy of Health Sciences, IndiaCopyright © 2022 Hanetz-Gamliel and Dollberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Keren Hanetz-Gamliel, ✉ a2VyZW5oYW5AbXRhLmFjLmls
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.