- 1School of Pharmacy and Medical Sciences, Griffith University, Gold Coast, QLD, Australia
- 2Centre for Mental Health, Griffith University, Brisbane, QLD, Australia
- 3Menzies Health Institute Queensland, Griffith University, Brisbane, QLD, Australia
- 4The University of Sydney School of Pharmacy, Faculty of Medicine and Health, The University of Sydney, Camperdown, NSW, Australia
- 5Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand
Introduction: Goal planning is routinely employed in mental health service delivery to identify priorities for treatment and support the achievement and evaluation of outcomes. Previous systematic reviews of the literature have focused on the use of goal planning in a range of physical and cognitive disability settings, but there is a lack of information regarding how goal planning is used in mental healthcare.
Aims: This systematic integrative review aimed to understand the types of goals, effectiveness of goal planning, the experience of goal planning and barriers and facilitators to effective goal planning in mental healthcare settings.
Methods: Five databases were systematically searched using key terms related to mental health AND goal planning. The search was supplemented through citation chaining. Due to the heterogeneity of the studies, a narrative synthesis approach to data analysis was undertaken.
Results: Fifty-four studies were identified through the search of the literature following the PRISMA guidelines. Data was systematically extracted and thematically organized. There was a high level of heterogeneity among the studies, originating from a range of countries and with diverse characteristics and focus. Four themes emerged from the data analysis and included: (i) goal planning as a central aspect of interventions; (ii) types of goals planned; (iii) factors that influenced goal planning and/or attainment; and (iv) collaboration and concordance in goal planning.
Conclusion: This review found some support for the use of goal planning to improve outcomes in mental healthcare although there was no identified standardized approach to the use of goal planning. Individualized, recovery-oriented and collaborative goal planning was recommended but not always used in practice. Further research to understanding the most appropriate skills and training needed to support collaborative and effective goal planning is needed.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/], identifier [CRD42020220595].
Key messages
- This systematic review identified themes regarding the use of goal planning in mental healthcare, increasing our understanding of how goal planning is used in service delivery.
- Four themes emerged from the data and included (i) goal planning as a central aspect of interventions; (ii) types of goals planned; (iii) factors that influenced goal planning and/or attainment; and (iv) collaboration and concordance in goal planning.
- Overall, findings suggest that there are benefits associated with the use of goal planning in mental healthcare settings, and goals are important in supporting change and achieving outcomes.
- Goals prioritized by practitioners and service users were not always well-aligned and shared decision making and collaborative approaches improved engagement, satisfaction, and outcomes for service users.
- Goal planning is a complex process and a better understanding of the skills required by practitioners to support recovery-oriented goal planning is needed.
1 Introduction
Goal planning is widely recognized as an integral component of psychiatric rehabilitation (1), with evidence suggesting that goal planning facilitates behavioral change (2). It is seen as a process of discussion and negotiation through which service users and health practitioners identify priorities for treatment to support the achievement of desired future states (3). A range of terminology in relation to goal planning has been used in the literature and includes goal setting and care planning, along with action planning, in which plans are made to operationalize and assist achievement of goals (4). Given the close relationship between the process of goal setting and action planning, these terms are often used interchangeably. Within mental healthcare, terms such as recovery planning and shared decision making are common. Goal planning has been shown to enhance service user motivation, adherence, self-efficacy, and health related quality of life (5).
Goal planning processes support individuals to identify desired outcomes, specific behaviors to change and how to go about making changes (6) and should be intentionally developed in negotiation with those who will be directly impacted (3). Goal planning theory suggests that goals that are conscious and specific as well as sufficiently difficult produce better results (7, 8), and can be influenced by factors such as intrinsic motivation and self-efficacy (7).
Current mental healthcare is focused on promoting recovery, utilizing interventions that focus on increasing competencies or skills and providing environmental supports to assist service users achieve a meaningful life (9). Shared decision making is seen as an essential process in supporting personal recovery and self-determination, occurring when all participants are informed, involved, and influential in the decision making and goal planning process (10). Whilst shared decision making is promoted in mental healthcare, several barriers have been identified including concerns regarding service user capacity, complicated by power imbalances due to statutory provisions for involuntary treatment in many countries (11). Previous literature reviews regarding the use of goal planning in healthcare have focused on the rehabilitation context for acquired disability (5), acquired brain injury (12, 13), spinal cord injury (14), and older patients (15). Given the theoretical and practical differences in service delivery for those with physical injuries as compared with people experiencing mental illnesses, it is important to understand any differences in goal planning processes and outcomes.
The involvement of people with mental illness in goal planning is generally seen as beneficial, however information regarding what makes goal planning effective is lacking. The purpose of this review was to systematically examine and synthesize the literature regarding goal planning in mental healthcare.
1.1 Objectives
The purpose of this systematic integrative review was to locate, access, compile, and map the published studies that exist about the use of goal planning within the context of mental health service delivery. This review aimed to understand (i) the types of goals being developed; (ii) the effectiveness of goal planning in improving mental health outcomes; (iii) how service users and practitioners experience goal planning processes, and (iv) the barriers and facilitators to effective goal planning in mental health service delivery from the perspectives of service users and practitioners.
For the purpose of this review, the definition of a rehabilitation goal by Siegert and Levack was applied in that goals are “actively selected, intentionally created, have purpose and are shared (where possible) by the people participating in the activities and interventions” (3).
2 Materials and methods
This integrative review process was developed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (16) and was registered with PROSPERO (CRD42020220595). The PRISMA checklist is attached (Supplementary material).
2.1 Search strategy
Six electronic databases [Medline (Ebsco), CINAHL, Embase, PsycINFO (Ovid), and Scopus] were searched in March 2022. The PICO framework (17) structured the search strategy with the population (“P”) identified as adults experiencing mental illness, the intervention (“I”) defined as goal planning, the comparison group (“C”) was not relevant for this study, and outcomes (“O”) were not limited. The search strategies were developed with assistance from an academic librarian and combined MESH terms and keywords related to mental health (e.g., mental illness, mental health condition, and psychiatric diagnosis) AND goal planning (e.g., goal setting, care planning, and shared decision-making). Additional studies were identified through reviewing the reference lists and citations of retrieved articles. Further details regarding the search strategy is provided (Supplementary material). The main inclusion criterion was that the study included adults diagnosed with a mental illness or practitioners working with this population and reported on the impact or experience of goal planning. Empirical studies also needed to be published in a peer-reviewed journal in English, with no restriction on the study methodology used. Conceptual, commentary and review papers were excluded, as were studies focused on specific cohorts such as forensic, substance use or dementia populations. Further details regarding the inclusion and exclusion criteria can be found in the published protocol (18).
2.2 Study selection
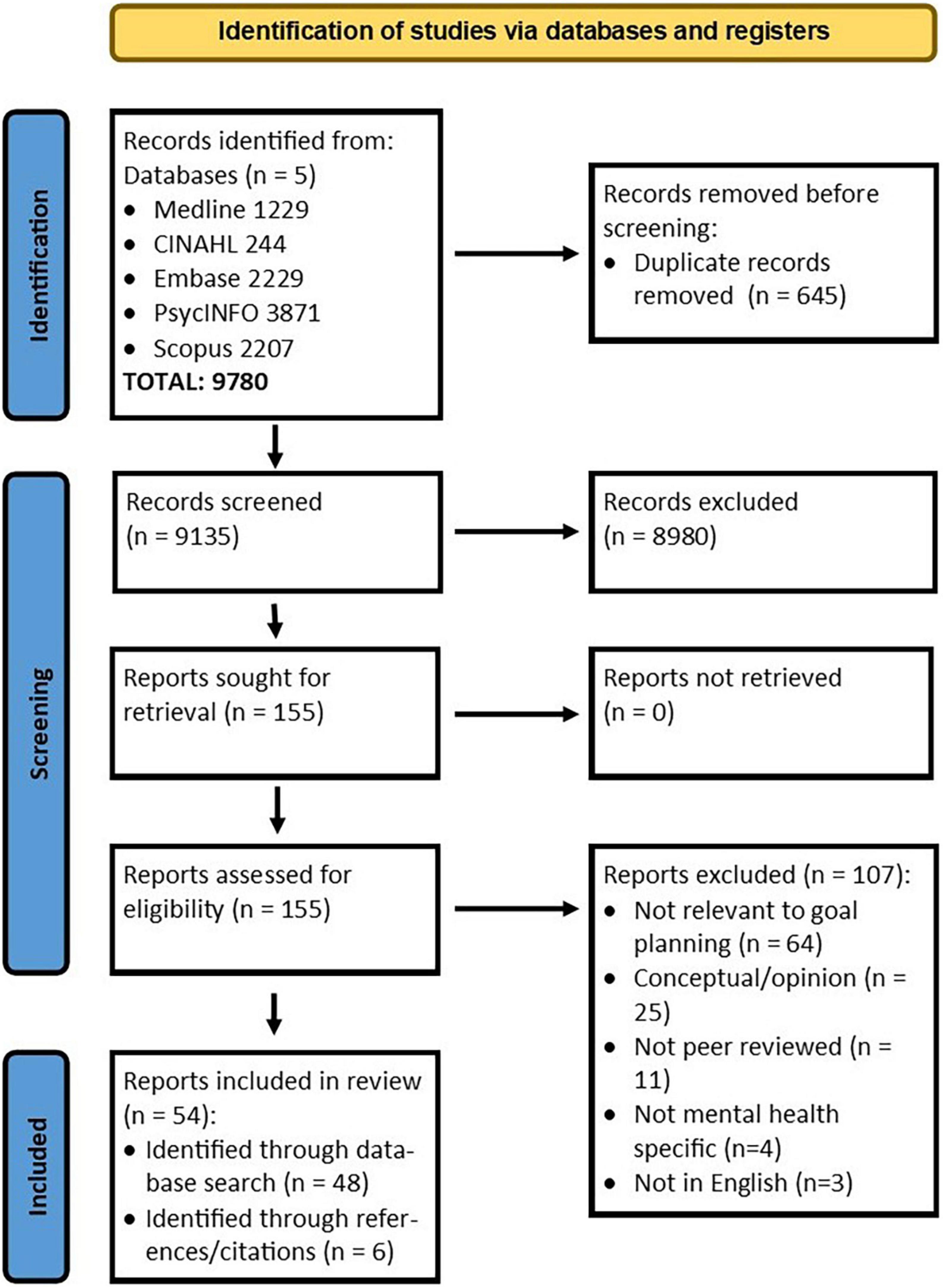
First, one author (VS) conducted a preliminary screening of titles to exclude any irrelevant studies (e.g., focused on different populations) or duplications. Articles were then imported into the Covidence review management tool (19) with titles and abstracts independently screened for relevance by two authors (VS and RN). An over-inclusive approach was utilized with full-text articles obtained for any abstracts in doubt. The same authors then screened all full-text articles for inclusion in the final review. Consensus on inclusion was reached by discussion between the authors, with a third author (SM) arbitrating on those in doubt (n = 3). Further details for study exclusion can be found in Figure 1.
2.3 Critical appraisal
The quality of the included studies was assessed using the Mixed-Methods Appraisal Tool (MMAT), which was designed to appraise the methodological quality of five different study categories (qualitative research, randomized controlled trials, non-randomized studies, quantitative descriptive studies, and mixed methods studies) (20). The MMAT scale comprises two screening questions, followed by individual items for the five different methodologies. Initially, three authors (VS, JH, and SM) independently reviewed a selection of 20 studies, with a consensus on scoring reached through discussion. Another author (AW) arbitrated disagreements (n = 2). Two authors (VS and JH) then independently completed the appraisal of the final 34 studies, again reaching a consensus on any disagreements (n = 6). The methodological quality of included studies ranged from 20 to 100% (M = 66.3%). For qualitative studies, the methodological quality ranged from 60 to 100% (M = 92.7%), randomized controlled trials ranged from 20 to 100% (M = 64.4%), and quantitative studies ranged from 40 to 80% (M = 60.0%). Following MMAT author guidelines, the overall quality score for mixed methods studies was identified as the lowest score achieved (M = 56%, range 20–80) across the study components (20). As integrative reviews consider a wide range of evidence, studies were not excluded on the appraised level of quality. However, consideration of study quality was taken into account during the interpretation of the data. A summary of the quality of studies is presented (Supplementary material) and should be considered alongside the findings of this review.
2.4 Data extraction and analysis
This process aimed to analyze and synthesize the information from included studies to develop new knowledge and insights about mental healthcare goal planning, which were not visible through reading each study in isolation. An integrative literature review method was undertaken, following the process described by Whittemore and Knafl (21). An integrative approach was selected as it allows for the inclusion of studies from diverse methodologies and captures the complexity of varied perspectives (21, 22).
Initially, an Excel spreadsheet was used by one author (VS) to extract descriptive data on the author, publication date, country, study design, aims, study setting, sample characteristics, goal planning method, healthcare practitioner, description of intervention(s), goal planning outcome measure(s), service user, and practitioner results (18). A second author (SM) completed a quality check (20% of included studies) of data extraction. Next, an in-depth analysis of the eligible studies was undertaken by one author (VS) in consultation with another author (SM). Due to the heterogeneity of the studies included in this review, a narrative synthesis approach (23) was identified as an appropriate approach to understanding and presenting the findings of the included studies. First, data were extracted according to the review questions (e.g., use of goal planning and experiences of goal planning) and presented in tabular form. These results were then reviewed by the same author (VS) and manually added to tables that structured the study themes based on the aims and outcomes described within each study. The included studies were summarized within this thematic framework by one author (VS).
3 Results
3.1 Study characteristics
Fifty-four studies were identified (Figure 1) and published between 1982 and 2021. Studies showed heterogeneity in characteristics and outcomes (Tables 1–4). The majority of studies were quantitative (n = 29), 16 utilized mixed methods and nine involved a qualitative study design. Studies were undertaken in the USA (n = 17), Europe (n = 12) Australia (n = 9), UK (n = 9), Israel (n = 3), Brazil (n = 2), Canada (n = 1), and India (n = 1). Recruitment occurred in a range of settings including outpatient settings (e.g., primary health; n = 23), specialized psychiatric rehabilitation programs (n = 16), inpatient settings (n = 6), residential settings (n = 3), recovery college (n = 1), and recovery camp (n = 1), with four studies recruiting from general community forums. Studies reported on participants diagnosed with schizophrenia/psychotic disorder (n = 10), depression (n = 9), borderline personality disorder (n = 1), bipolar disorder (n = 1), and post-traumatic stress disorder (n = 1). The remaining 32 studies reported on groups of participants diagnosed with a range of mental illnesses (n = 15) or what the authors described as severe and persistent mental illness (n = 17). Forty-eight of the studies included health practitioners from backgrounds described as multidisciplinary teams (n = 21), psychotherapists (n = 5), psychologists (n = 5), case managers or care coordinators (n = 4), occupational therapists (n = 2), peer workers (n = 2), student (n = 1), or undefined backgrounds (e.g., mental health worker; n = 8).
3.2Goal planning themes
After analyzing the extracted data, four themes emerged and included: (i) goal planning as a central aspect of interventions; (ii) types of goals planned; (iii) factors that influenced goal planning and/or attainment; and (iv) collaboration and concordance in goal planning. As many studies reported information that could have fit into more than one theme category, the study’s primary focus was used in determining the most appropriate discrete theme category. Whilst it is acknowledged that this is not an ideal process, it was identified as the best way to synthesize a diverse range of results in a brief and manageable form and provide meaningful insights on how goal planning could be used in mental health service delivery. For example, Proctor et al. (24) utilized a range of data collected in a community mental health setting to explore the content of practitioner-developed and service user goals, goal achievement, benefits of therapy, and satisfaction with service delivery. When discussing the implications for practice, the results particularly highlighted the lack of agreement between practitioner and service user goals and the need for services to routinely collect this information to inform improvements. As such, this study was coded to the theme of exploring concordance in goal planning.
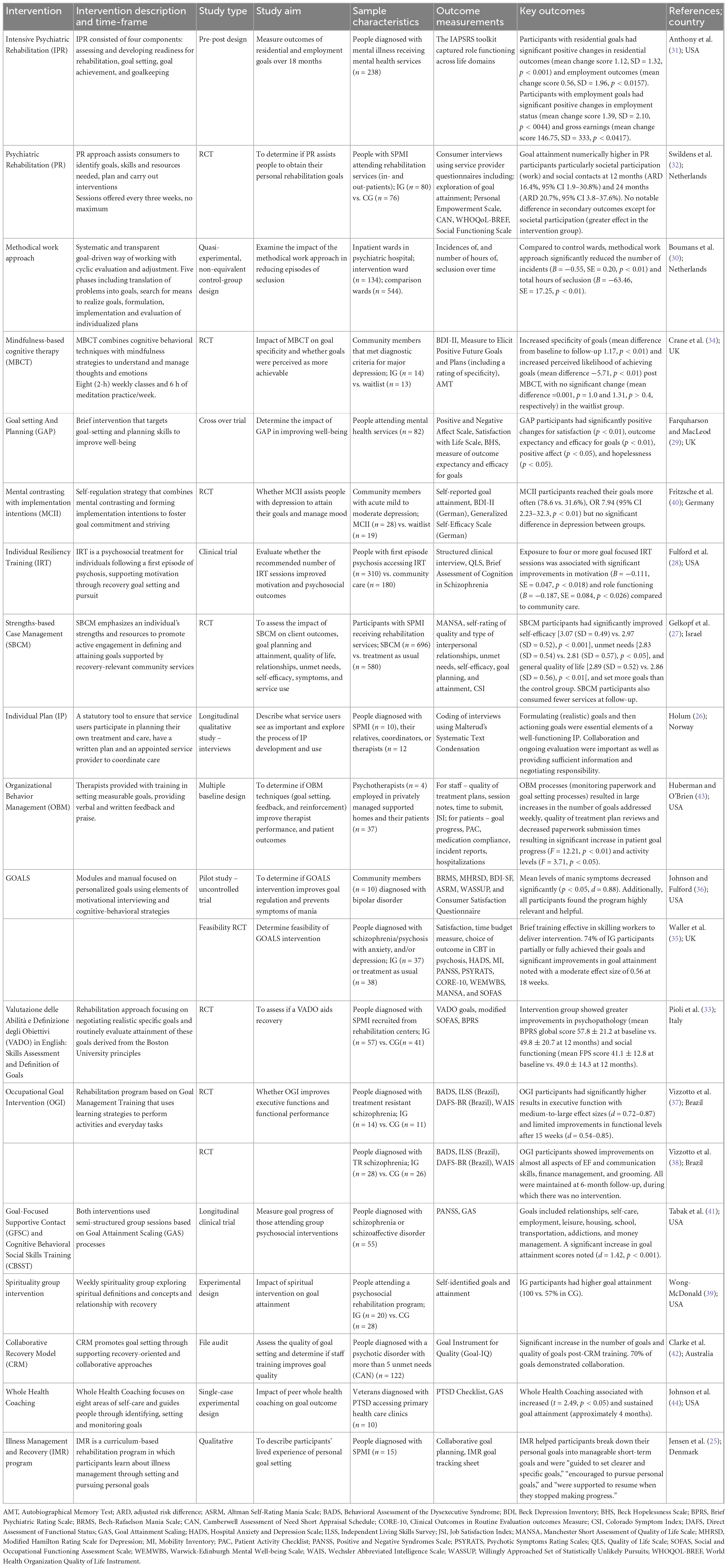
3.2.1 Goal planning as a central aspect of interventions
Eighteen rehabilitation and therapy interventions in 20 studies were described in the literature (Table 1). The interventions were based on individual goal planning approaches (25–30), psychiatric rehabilitation principles (31–33), cognitive-behavioral techniques (34–36), learning strategies (37, 38), spirituality (39), self-regulation (40), Goal Attainment Scaling (GAS) (41), recovery (42), Organizational Behavior Management (OBM) (43), and coaching (44). Fourteen of the interventions reported on goal attainment, which was assessed using a variety of methods, including a range of clinical and functional scales (27, 29, 31, 33, 35–38), GAS (41, 44), self-reporting (32, 40, 43), or an unreported measure (39). Other studies reported on the experiences of goal planning (25, 26), collaboration (42), and outcomes, including specificity of goals (34), motivation levels (36), and episodes of seclusion (30). Interventions were reported to support goal achievement for participants’ general well-being and quality of life (27, 35, 39, 40, 44) and in a range of areas, including housing and employment (31, 32, 39, 41), social participation (32, 33, 39–41), symptom management (29, 33, 35–38, 40), and executive functioning (37, 38). No instances of interventions having a negative effect on goal achievement, i.e., worsening of service user outcome measures, were reported.
Due to the variability in study designs and outcome measures, direct comparisons of results were not possible. In terms of outcomes, studies that reported on the process of goal planning identified that formulating and actioning specific goals, along with collaboration, ongoing evaluation of goal progress, and the provision of sufficient information to enable informed choice in regards to treatment or intervention options was determined by participants as necessary in supporting goal achievement (26, 30, 34). One quality RCT identified that goal-based interventions improved attainment of work and social goals (32), another with a large sample size but poor quality found improved self-efficacy and quality of life, with fewer unmet needs (27), whilst another reported greater improvements in psychopathology (33). Participants reported goal planning as a process or structure encouraging change by identifying specific steps to enable achievement (28). Good quality qualitative studies identified that involvement in goal planning resulted in improved motivation and increased goal-directed behaviors (27) and decreased hopelessness (25), while a well-powered clinical trial demonstrated enhanced confidence in achievement (28). Additionally, a small RCT reported that structured goal planning interventions improved rehabilitation practitioners’ confidence and motivation to support service users (33). Focusing on positive outcomes rather than deficits or obstacles was also an essential element of interventions (29, 40).
Additionally, training staff in goal planning interventions increased the number and quality of goals generated by promoting participant and practitioner collaboration in the goal planning process (31, 35, 42, 43). Studies also identified that interventions that promoted an individualized approach to goal planning (27, 41, 43, 44), spanning a range of life domains (31, 32, 39), were preferred by participants.
Whilst goal planning interventions were identified as effective in promoting positive outcomes for those experiencing mental illness, it was recommended that further research to determine which aspects of the process were most effective in supporting positive results is needed (37, 38).
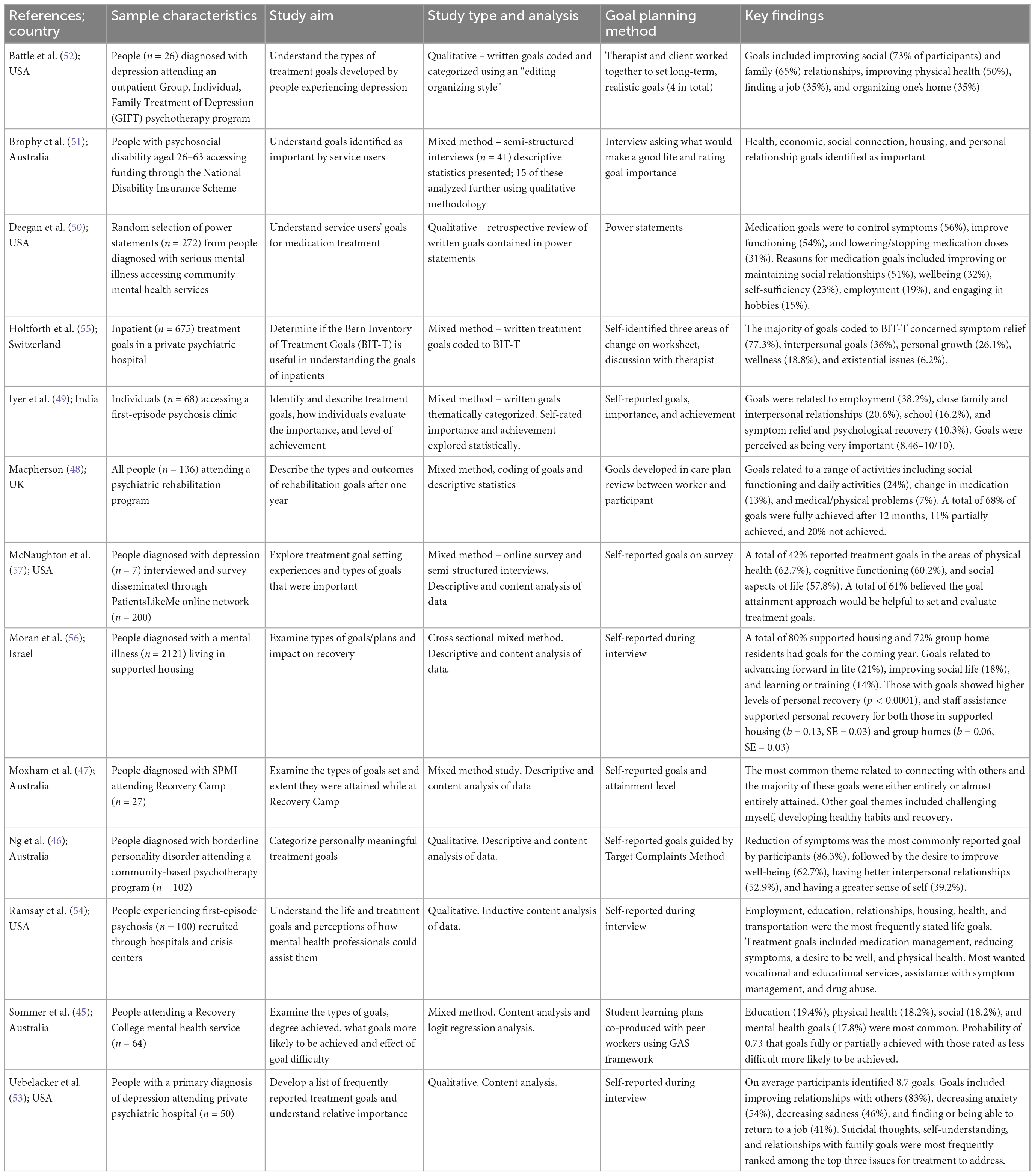
3.2.2 Types of goals planned
Thirteen studies primarily described the goals identified and prioritized by people experiencing mental illness (Table 2). Goals were developed in community-based treatment and rehabilitation programs (n = 8) (45–52), inpatient (n = 3) (53–55), supported housing (n = 1) (56) settings and with people living in the community (n = 1) (57). Data were collected through interviews (n = 6) (46, 51–54, 56), surveys (n = 1) (55, 57), treatment notes (n = 1) (48), worksheets (n = 1) (47), and assessment scales (n = 2) (45, 49). One study used power statements, an approach assisting clients prepare goal statements regarding medication treatment prior to medication visits (50). Studies used qualitative (n = 5) (46, 50, 52–54) or mixed methods (descriptive statistics and content analysis) (n = 7) (45, 47–49, 51, 56, 57) approaches to categorize, code, or describe the types of goals identified by participants. One study (55) utilized the Bern Inventory of Treatment Goals (BIT-T), a previously published goal taxonomy developed for psychotherapy goals (58).
Overall, participants experiencing a range of mental illnesses identified a broad range of goals from different life domains, including, but not limited to, employment/education, housing, relationships, mental health, physical health, symptom relief, medication use, and living skills. Researchers recognized that the goals identified by participants were largely developmentally appropriate, realistic, and did not stem from psychotic symptoms (49, 54). Generally, life and personal recovery goals were more prevalent and prioritized by service users, with symptom control seen as a means to achieving life goals (45, 50, 53, 55).
Given the diverse range of goals identified by those experiencing mental illness, some qualitative study authors raised concerns regarding the required scope of expertise or skills practitioners would need to support service users to achieve their prioritized goals (51, 52, 54). A high quality qualitative study recommended that practitioners focus on assessing whether the service user experienced difficulty with motivation to make changes or whether additional skills and knowledge were required to assist them in achieving their goals (52). As such, communicating and coordinating care with other professionals was deemed necessary, which was reinforced by study participants reporting a preference for support from practitioners with diverse skills (51, 52). In addition to partnering with other practitioners to address goals, working in partnership with service users (51) and ensuring treatments were appropriate to support goal achievement were identified as important practitioner skills by service users (49). In line with recommendations from studies included in the above theme, structured goal planning processes were seen as necessary; fostering collaboration and shared decision making, promoting understanding, engagement and retention with services, improving adherence to treatments, increasing satisfaction, and enhancing outcomes (49, 53, 57).
3.2.3 Factors influencing goal planning and/or attainment
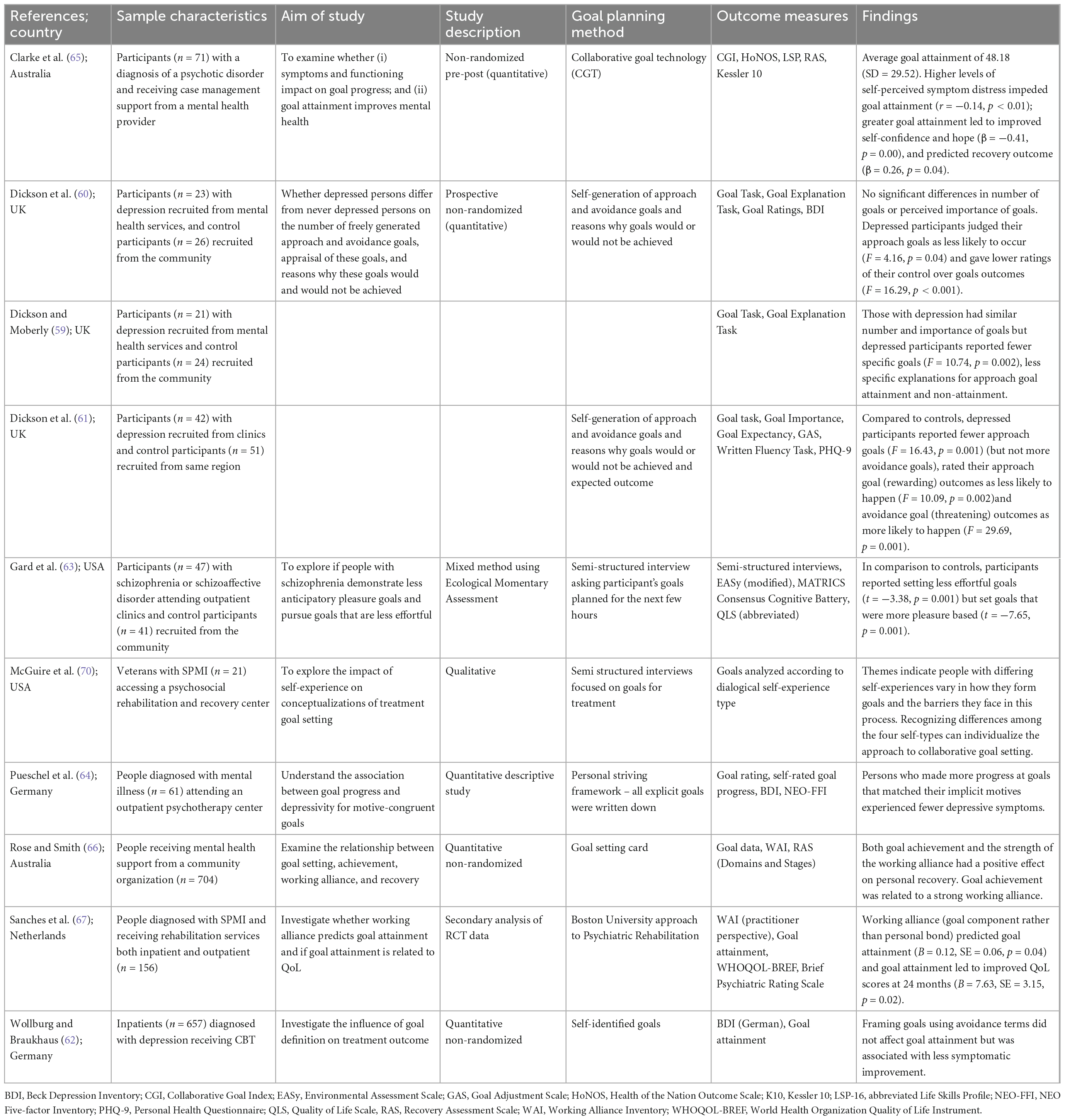
Ten studies investigated aspects of the goal planning process that may influence the type of goals planned or outcomes achieved (Table 3). Studies explored factors such as whether the goals used avoidance or approach to formulation (59–62), how effortful goals were (63), whether goals were pleasure-based (63), as well as participant factors such as an individual’s dialogical self-experience (1), severity of symptoms (64, 65), and the quality of a participant’s working alliance with the practitioner (66, 67). Participants diagnosed with depression (1, 59–62), schizophrenia (63), or a range of mental illnesses (1, 64, 65, 67) were included and recruited from community-based services (59–61, 63–67) and/or hospitals (62, 67).
Service users who reported fewer symptoms or distress obtained greater goal progress, particularly if the goals were congruent with personal motives (64, 65). One moderately powered study (61) identified that a person’s self-experience or self-narrative impacted goal formation and the barriers faced in goal planning processes, recommending that practitioners use approaches appropriate for different levels of self-experience. Goal achievement was also related to a strong working alliance between service users and practitioners, suggesting greater collaboration and agreement in goal planning resulted in an improved quality of life and positive personal recovery for participants (66, 67).
Five studies explored the goal planning of people diagnosed with depression (59–62, 64). These studies reported that generally, participants identified more approach (moving to a desirable state) than avoidance (moving away from undesirable end state) goals, with no differences in types of goals found between those diagnosed with depression and control groups (59–61). A large study identified that framing goals as approach or avoidance did not influence goal attainment, although less symptomatic improvement was seen in service users identifying avoidance goals (62). Whilst a smaller study reported that participants diagnosed with depression rated approach goals as less likely to be achieved, undesirable goal outcomes more likely to occur, and perceived less control over their goal outcomes (60). Additionally, participants diagnosed with depression generated fewer specific goals and reasons for and against goal attainment (59), with a greater inclination to disengage with goals they viewed as unattainable (61). These outcomes suggest that people experiencing depression have a more pessimistic view of goal planning. As such, other authors recommended that practitioners focus on challenging negative thinking to support goal attainment (46) and promote goal specificity and perseverance to sustain motivation to participate in goal activities for this specific population (59, 61).
A medium sized study investigated the goal planning behaviors of participants diagnosed with schizophrenia (63). These service users planned less effortful goals and activities and engaged in goals and activities that were more pleasure-based. As a result, the authors recommended that practitioners support service users to break down more extensive and complex goals into smaller, lower-effort steps and engage in pleasurable activities or rewards to promote goal attainment (63).
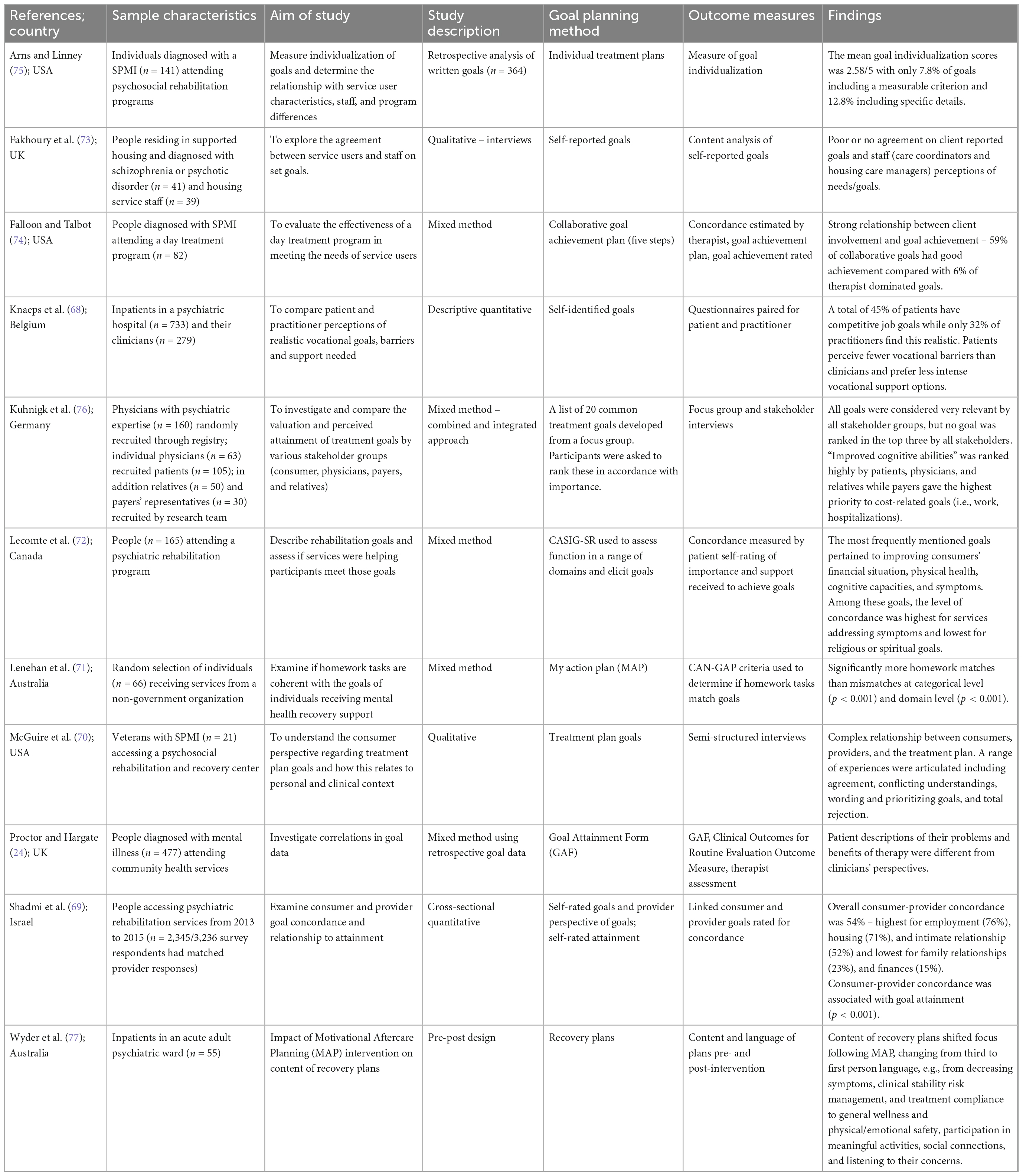
3.2.4 Collaboration and concordance in goal planning
Eleven studies evaluated collaboration and concordance between participant and practitioner perspectives regarding goal planning (Table 4). Seven of these studies were focused on the agreement between participant-identified goals, and the treatment plan developed or services provided (24, 68–73), whilst one study reviewed the level of collaboration in goal planning (74), one assessed the individualization of written goals (75), one examined and compared the goal priorities of participants, families, and practitioners (76), and one reviewed the effectiveness of a collaborative training intervention for practitioners (77). Goal planning processes in rehabilitation programs (69, 70, 72, 74, 75), community-based mental health services (24, 71, 76), supported housing (73), and hospitals (68, 77) were identified through existing treatment/rehabilitation plans (70, 71, 74, 75, 77), questionnaires (24, 68, 69, 76), and interviews (72, 73).
Several studies reported limited agreement between the goals that participants identified, and goals developed by practitioners (24, 69, 73, 74, 76), with the highest levels of agreement for goals addressing symptoms and the lowest level of agreement for religious or spiritual goals (72). One large study (68) reported that nearly half of the inpatient participants had competitive employment goals, with only a third of practitioners agreeing these goals were realistic; practitioners identified more barriers and more significant support needs to be required. In particular, one large qualitative study (75) noted that whilst 70% of written goals included observable behaviors, only 7.8% of these goals contained a measurable criterion. These differences in the individualization of goals were attributed to variances in practices, both between programs and among staff within programs (75). A small qualitative study (70) identified the complexity of creating collaborative treatment plans that recorded individual goals in a way that was actionable, understandable by other practitioners, and met regulatory requirements. As a result, authors highlighted the need for practitioner training (73, 75), with particular attention paid to supporting practitioners to apply motivational approaches to goal and treatment planning (70). A study reporting on the impact of a practitioner training program focused on increasing collaboration in goal planning resulted in a shift in both the content of the goals (increased focus on individual priorities) and the use of first-person language (77), indicating that practitioner training can be effective in improving collaboration and concordance in goal planning.
In all studies, service users were able to identify and set realistic goals. Diagnosis or severity of illness did not appear to impact the ability of participants to plan goals (74). Given these outcomes, authors highlighted difficulties with current service delivery using psychiatric diagnoses to guide the development of interventions (24), recommending that service users’ goals and priorities should guide how services are delivered (69, 72). High levels of service user involvement in goal planning and concordance between participant and practitioner goals resulted in higher levels of goal achievement (69, 74, 75).
4 Discussion
This review is, to the best of our knowledge, the first systematic review exploring the use of goal planning in mental health service delivery, and it aimed to provide a better understanding of the types, effectiveness, and experiences of goal planning, as well as the barriers and facilitators to goal planning in mental healthcare. Data from 54 studies were synthesized, demonstrating that goal planning was used in a range of settings, by health practitioners from varied professional backgrounds, and with people experiencing a range of mental illnesses. Overall, findings suggest that there are benefits associated with the use of goal planning in mental healthcare settings.
Interventions that utilized goal planning tended to be complex and varied substantially in approach and application, thus making it challenging to isolate goal planning from the other activities undertaken in mental health service delivery settings. For example, interventions based on psychiatric rehabilitation principles (31–33) provided participants or staff with training to identify goals, describe the skills and resources needed to attain goals, plan, and carry out interventions and access ongoing support to maintain goal attainment. Other studies (66, 67, 70) focused on the impact of the quality of relationships between staff and participants (working alliance), how psychopathology or symptoms effect goal planning and attainment (33, 36, 40, 59–62, 64, 65), or the quality of written goals (42, 77).
The heterogeneity in goal planning processes and measurement of goal attainment precluded direct comparisons across studies or a clear understanding of the impact of goal planning on mental health outcomes. However, studies identified goal planning as an important element in supporting change for people experiencing mental illness, providing a structure that encouraged change and supported motivation to achieve outcomes (28) and improved quality of life (27, 67).
This review highlighted the broad range of goals identified and prioritized by service users and recognized that there was often a divergence between the priorities and goals planned by service users and health practitioners. Goals designed by health practitioners were often focused on symptom management whilst service users prioritized goals for other areas of their everyday lives, including employment, education, relationships, physical health, and living skills, in addition to symptom relief and medication use (45, 49). Service users also valued goals that were individualized to their particular needs, consistent with principles of recovery and recovery-oriented care. Improving goal alignment through shared decision making and collaboration in goal planning promoted increased engagement and retention with services, improved adherence to treatments, increased satisfaction, and enhanced outcomes for service users (49, 53, 57). Factors related to recovery such as focusing on strengths and positive outcomes (29, 40), individualized and personal goals (27, 41–45, 50, 53, 55), collaborative relationships and goal planning (31, 35, 42, 43, 66, 67), informed choice (26), recovery language (77), and partnerships with service users (51) were highlighted across the studies. Whilst some interventions focused on increasing aspects of these in goal planning processes, further research is needed to understand how best to incorporate individual goals into recovery-oriented interventions and service delivery, particularly how best to measure effectiveness and outcomes. The disparity in practitioner and personal understandings of goals and priorities is an important issue that needs review across all levels of service delivery to better align treatment with service user needs (24, 54). This may lead to the development of new and more acceptable treatment options for people experiencing mental illnesses.
Creating collaborative treatment plans that could be individually recorded and understandable by service users and other health practitioners was identified as a complex process (70), one that may have intrinsic therapeutic value in itself (27). As a result, the need for practitioner training was highlighted (73, 75), with particular attention paid to supporting practitioners to develop strong working alliances with service users (66, 69) and apply motivational approaches to goal and treatment planning (70). Studies identified that health practitioners who were provided with training demonstrated increased collaboration during goal planning (31, 42, 43, 77) and improved practitioner confidence in goal planning processes (33). Additionally, due to the individual and diverse goals prioritized by service users, it was identified that practitioners required skills in communicating and coordinating care to ensure that service users were able to access support relevant to their goal outcomes (51, 52, 54). Further understanding of appropriate skills and training needed to support collaborative and effective goal planning is needed.
A number of common aspects of goal planning were identified through this review that mapped easily to the stages reported in the Goal Setting and Action Planning Framework (78). Whilst this practice framework was developed to support the achievement of rehabilitation goals (78), these findings support the applicability of this framework to mental healthcare settings. Stage 1 (goal negotiation) was supported by the provision of appropriate information to allow informed decision-making by service users (26, 30, 34), service user involvement and collaboration in goal planning (67, 69, 74, 75), and shared decision making approaches (49, 53, 57). Stage 2 (goal setting) required an individualized approach (27, 41, 43, 44) that identified the priorities and personal motivations of service users (45, 50, 53, 55, 64, 65) and resulted in the planning of specific goals (28, 59, 61). Stage 3 (planning and action) needed the identification of specific steps that broke complex goals into smaller, achievable steps that enabled achievement (25, 28, 63), focused on positive outcomes rather than obstacles (29, 40), and was supported by a strong working alliance (66), that utilized motivational support approaches (70). Stage 4 (appraisal and feedback) required ongoing evaluation of goal progress and adjustment of goals as needed (30).
4.2 Strengths and limitations
The findings from this review need to be considered within the context of its strengths and limitations. This review followed the process outlined in a peer-reviewed protocol (18) and adhered to the PRISMA guidelines (16). Additionally, quality checking of screening and data extraction along with a quality assessment of the studies, added transparency and rigor to the research. The synthesis of data concentrated on both the effects and experiences of goal planning, examining these aspects regarding the use of goal planning in mental healthcare. This focus has enabled recommendations that are specific to the use of goal planning in mental healthcare.
Both a strength and limitation of this review were that evidence was systematically collected from a range of studies, including those with quantitative, qualitative, and mixed method designs. The breadth of studies provided an enhanced understanding of the different contexts in which goal planning is utilized as well as providing insights into the experiences of goal planning from practitioner and service user perspectives. Whilst the inclusion of a diverse range of studies added depth to our understanding; the authors acknowledge the inherent weaknesses of mixed methods systematic reviews (79). Only studies published in English were included, which may have resulted in the loss of important information in different cultural contexts. During synthesis, the study’s primary focus was used to determine the most appropriate theme category for each study. Whilst this allowed for better management of data, the authors recognize the limiting data extraction impacts of this process including the possibility of bias in coding decisions made by researchers and loss of information that could have added to other themes. Given the range of diagnoses and health practitioners within the included studies, the transferability of recommendations is limited. Additionally, a major limitation was a lack of comparability between studies due to heterogeneity of research aims and methods, resulting in difficulty in confidently identifying factors that contributed to effective outcomes. Further research comparing different goal planning interventions is needed to understand which approaches are most effective.
5 Conclusion
In conclusion, our systematic integrative review examined the use of goal planning in mental healthcare and found some support for the use of goal planning to improve outcomes in mental healthcare. Individualized, recovery-oriented and collaborative goal planning has been identified as best practice but does not always occur. Goal planning can be a complex process, and mental health practitioners require a range of skills to collaborate and appropriately identify and support service user goal priorities. Additionally, there does not appear to be one standardized approach to goal planning in mental healthcare. Therefore, more research is required to clarify best practice methods for goal planning and required professional education to implement appropriate, recovery-oriented goal planning.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
VS: study design, title and abstract screen, full-text screen, quality appraisal, data extraction and analysis, and write manuscript. SM: study design, quality appraisal, data analysis, and write manuscript. JH: quality appraisal and comment on manuscript. RN: title and abstract screen, and comment on manuscript. SE-D and CO’R: study design, comment, and edit manuscript. AW: study design, quality appraisal, and write manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was part of VS’s Ph.D. supported by a Griffith University scholarship.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1057915/full#supplementary-material
References
1. McGuire A, Lysaker P, Wasmuth S. Altered self-experience and goal setting in severe mental Illness. Am J Psychiatr Rehabil. (2015) 18:333–62.
2. Epton T, Currie S, Armitage C. Unique effects of setting goals on behavior change: systematic review and meta-analysis. J Consult Clin Psychol. (2017) 85:1182–98. doi: 10.1037/ccp0000260
3. Siegert R, Levack W. Rehabilitation Goal Setting: Theory, Practice and Evidence. Boca Raton, FL: CRC press, Taylor & Francis Group (2015).
4. Scobbie L, Wyke S, Dixon D. Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin Rehabil. (2009) 23:321–33. doi: 10.1177/0269215509102981
5. Levack W, Weatherall M, Hay-Smith E, Dean S, McPherson K, Siegert R. Goal Setting and Strategies to Enhance Goal Pursuit for Adults with Acquired Disability Participating in Rehabilitation. London: Cochrane Library (2015). doi: 10.1002/14651858.cd009727.pub2
6. Bailey R. Goal setting and action planning for health behavior change. Am J Lifestyle Med. (2019) 13:615–8. doi: 10.1177/1559827617729634
7. Locke E, Latham G. Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol. (2002) 57:705–17. doi: 10.1037//0003-066X.57.9.705
9. Farkas M, Anthony W. Psychiatric rehabilitation interventions: a review. Int Rev Psychiatry. (2010) 22:114–29. doi: 10.3109/09540261003730372
10. Stacey G, Felton A, Hui A, Stickley T, Houghton P, Diamond B, et al. Informed, involved and influential: three is of shared decision making. Ment Health Pract. (2015) 19:31–5. doi: 10.7748/mhp.19.4.31.s20
11. Farrelly S, Lester H, Rose D, Birchwood M, Marshall M, Waheed W, et al. Barriers to shared decision making in mental health care: qualitative study of the joint crisis plan for psychosis. Health Expect. (2016) 19:448–58. doi: 10.1111/hex.12368
12. Knutti K, Björklund Carlstedt A, Clasen R, Green D. Impacts of goal setting on engagement and rehabilitation outcomes following acquired brain injury: a systematic review of reviews. Disabil Rehabil. (2022) 44:2581–90. doi: 10.1080/09638288.2020.1846796
13. Sugavanam T, Mead G, Bulley C, Donaghy M, van Wijck F. The effects and experiences of goal setting in stroke rehabilitation – a systematic review. Disabil Rehabil. (2013) 35:177–90. doi: 10.3109/09638288.2012.690501
14. Maribo T, Jensen C, Madsen L, Handberg C. Experiences with and perspectives on goal setting in spinal cord injury rehabilitation: a systematic review of qualitative studies. Spinal Cord. (2020) 58:949–58. doi: 10.1038/s41393-020-0485-8
15. Smit E, Bouwstra H, Hertogh C, Wattel E, van der Wouden J. Goal-setting in geriatric rehabilitation: a systematic review andmeta-analysis. Clin Rehabil. (2019) 33:395–407. doi: 10.1177/0269215518818224
16. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
18. Stewart V, McMillan S, Roennfeldt H, El-Den S, Ng R, Wheeler A. Exploring goal planning in mental health service delivery: a systematic review protocol. BMJ Open. (2021) 11:e047240. doi: 10.1136/bmjopen-2020-047240
19. Veritas Health Innovation. Better Systematic Review Management. Deerfield, IL: Veritas Health Innovation (2022).
20. Hong Q, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the mixed methods appraisal tool (Mmat). J Eval Clin Pract. (2018) 24:459–67. doi: 10.1111/jep.12884
21. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. (2005) 52:546–53. doi: 10.1111/j.1365-2648.2005.03621.x
22. Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. (2016) 30:662–9. doi: 10.1111/scs.12327
23. Ryan R, Cochrane Consumers and Communication Review Group. Cochrane Consumers and Communication Review Group: Data Synthesis and Analysis. London: Cochrane (2013).
24. Proctor G, Hargate R. Quantitative and qualitative analysis of a set of goal attainment forms in primary care mental health services. Couns Psychother Res. (2013) 13:235–41. doi: 10.1080/14733145.2012.742918
25. Jensen S, Eplov L, Mueser K, Petersen K. Participants’ lived experience of pursuing personal goals in the illness management and recovery program. Int J Soc Psychiatry. (2021) 67:360–8. doi: 10.1177/0020764020954471
26. Holum L. Individual plan in a user-oriented and empowering perspective: a qualitative study of individual plans in Norwegian mental health services. Nord Psychol. (2012) 64:44–57. doi: 10.1080/19012276.2012.693725
27. Gelkopf M, Lapid L, Werbeloff N, Levine S, Telem A, Zisman-Ilani Y, et al. A Strengths-based case management service for people with serious mental illness in Israel: a randomized controlled trial. Psychiatry Res. (2016) 241:182–9. doi: 10.1016/j.psychres.2016.04.106
28. Fulford D, Meyer-Kalos P, Mueser K. Focusing on recovery goals improves motivation in first-episode psychosis. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:1629–37. doi: 10.1007/s00127-020-01877-x
29. Farquharson L, MacLeod A. A brief goal-setting and planning intervention to improve well-being for people with psychiatric disorders. Psychother Psychosom. (2014) 83:122–4. doi: 10.1159/000356332
30. Boumans C, Egger J, Souren P, Hutschemaekers G. Reduction in the use of seclusion by the methodical work approach. Int J Ment Health Nurs. (2014) 23:161–70. doi: 10.1111/inm.12037
31. Anthony W, Ellison M, Rogers E, Mizock L, Lyass A. Implementing and evaluating goal setting in a statewide psychiatric rehabilitation program. Rehabil Couns Bull. (2014) 57:228–37. doi: 10.1177/0034355213505226
32. Swildens W, van Busschbach J, Michon H, Kroon H, Koeter M, Wiersma D, et al. effectively working on rehabilitation goals: 24-month outcome of a randomized controlled trial of the Boston psychiatric rehabilitation approach. Can J Psychiatry. (2011) 56:751–60. doi: 10.1177/070674371105601207
33. Pioli R, Vittorielli M, Gigantesco A, Rossi G, Basso L, Caprioli C, et al. Outcome assessment of the vado approach in psychiatric rehabilitation: a partially randomised multicentric trial. Clin Pract Epidemiol Ment Health. (2006) 2:1–8. doi: 10.1186/1745-0179-2-5
34. Crane C, Winder R, Hargus E, Amarasinghe M, Barnhofer T. Effects of mindfulness-based cognitive therapy on specificity of life goals. Cognit Ther Res. (2012) 36:182–9. doi: 10.1007/s10608-010-9349-4
35. Waller H, Landau S, Fornells-Ambrojo M, Jolley S, McCrone P, Halkoree R, et al. Improving implementation of evidence based practice for people with psychosis through training the wider workforce: results of the goals feasibility randomised controlled trial. J Behav Ther Exp Psychiatry. (2018) 59:121–8. doi: 10.1016/j.jbtep.2017.12.004
36. Johnson S, Fulford D. Preventing mania: a preliminary examination of the goals program. Behav Ther. (2009) 40:103–13. doi: 10.1016/j.beth.2008.03.002
37. Vizzotto A, Celestino D, Buchain P, Oliveira A, Oliveira G, Di Sarno E, et al. A pilot randomized controlled trial of the occupational goal intervention method for the improvement of executive functioning in patients with treatment-resistant schizophrenia. Psychiatry Res. (2016) 245:148–56. doi: 10.1016/j.psychres.2016.05.011
38. Vizzotto A, Celestino D, Buchain P, Oliveira A, Oliveira G, Di Sarno E, et al. Occupational goal intervention method for the management of executive dysfunction in people with treatment-resistant schizophrenia: a randomized controlled trial. Am J Occup Ther. (2021) 75:7503180050. doi: 10.5014/ajot.2021.043257
39. Wong-McDonald A. Spirituality and psychosocial rehabilitation: empowering persons with serious psychiatric disabilities at an inner-city community program. Psychiatr Rehabil J. (2007) 30:295–300. doi: 10.2975/30.4.2007.295.300
40. Fritzsche A, Schlier B, Oettingen G, Lincoln T. Mental contrasting with implementation intentions increases goal-attainment in individuals with mild to moderate depression. Cognit Ther Res. (2016) 40:557–64. doi: 10.1007/s10608-015-9749-6
41. Tabak N, Link P, Holden J, Granholm E. Goal attainment scaling: tracking goal achievement in consumers with serious mental Illness. Am J Psychiatr Rehabil. (2015) 18:173–86. doi: 10.1080/15487768.2014.954159
42. Clarke S, Crowe T, Oades L, Deane F. Do goal-setting interventions improve the quality of goals in mental health services? Psychiatr Rehabil J. (2009) 32:292–9. doi: 10.2975/32.4.2009.292.299
43. Huberman W, O’Brien R. Improving therapist and patient performance in chronic psychiatric group homes through goal-setting, feedback, and positive reinforcement. J Organ Behav Manage. (1999) 19:13–36. doi: 10.1300/J075v19n01_04
44. Johnson E, Possemato K, Martens B, Hampton B, Wade M, Chinman M, et al. Goal attainment among veterans with Ptsd enrolled in peer-delivered whole health coaching: a multiple baseline design trial. Coaching. (2022) 15:197–213. doi: 10.1080/17521882.2021.1941160
45. Sommer J, Gill K, Stein-Parbury J, Cronin P, Katsifis V. The role of recovery colleges in supporting personal goal achievement. Psychiatr Rehabili J. (2019) 42:394–400. doi: 10.1037/prj0000373
46. Ng F, Carter P, Bourke M, Grenyer B. What do individuals with borderline personality disorder want from treatment? A study of self-generated treatment and recovery goals. J Psychiatr Pract. (2019) 25:148–55. doi: 10.1097/PRA.0000000000000369
47. Moxham L, Taylor E, Patterson C, Perlman D, Brighton R, Heffernan T, et al. Goal setting among people living with mental illness: a qualitative analysis of recovery camp. Issues Ment Health Nurs. (2017) 28:420–4. doi: 10.1080/01612840.2016.1271067
48. Macpherson R, Jerrom B, Lott G, Ryce M. The outcome of clinical goal setting in a mental health rehabilitation service. A model for evaluating clinical effectiveness. J Ment Health. (1999) 8:95–102. doi: 10.1080/09638239917670
49. Iyer S, Mangala R, Anitha J, Thara R, Malla A. An examination of patient-identified goals for treatment in a first-episode programme in Chennai, India. Early Interv Psychiatry. (2011) 5:360–5. doi: 10.1111/j.1751-7893.2011.00289.x
50. Deegan P, Carpenter-Song E, Drake R, Naslund J, Luciano A, Hutchison S. Enhancing clients’ communication regarding goals for using psychiatric medications. Psychiatr Serv. (2017) 68:771–5. doi: 10.1176/appi.ps.201600418
51. Brophy L, Bruxner A, Wilson E, Cocks N, Stylianou M. How social work can contribute in the shift to personalised, recovery-oriented psycho-social disability support services. Br J Soc Work. (2015) 45:98–116. doi: 10.1093/bjsw/bcv094
52. Battle C, Uebelacker L, Friedman M, Cardemil E, Beevers C, Miller I. Treatment goals of depressed outpatients: a qualitative investigation of goals identified by participants in a depression treatment trial. J Psychiatr Pract. (2010) 16:425–30. doi: 10.1097/01.pra.0000390763.57946.93
53. Uebelacker L, Battle C, Friedman M, Cardemil E, Beevers C, Miller I. The importance of interpersonal treatment goals for depressed inpatients. J Nerv Ment Dis. (2008) 196:217–22. doi: 10.1097/NMD.0b013e3181663520
54. Ramsay C, Broussard B, Goulding S, Cristofaro S, Hall D, Kaslow N, et al. Life and Treatment goals of individuals hospitalized for first-episode nonaffective psychosis. Psychiatry Res. (2011) 189:344–8. doi: 10.1016/j.psychres.2011.05.039
55. Holtforth M, Reubi I, Ruckstuhl L, Berking M, Grawe K. The value of treatment-goal themes for treatment planning and outcome evaluation of psychiatric inpatients. Int J Soc Psychiatry. (2004) 50:80–91. doi: 10.1177/0020764004040955
56. Moran G, Westman K, Weissberg E, Melamed S. Perceived assistance in pursuing personal goals and personal recovery among mental health consumers across housing services. Psychiatry Res. (2017) 249:94–101. doi: 10.1016/j.psychres.2017.01.013
57. McNaughton E, Curran C, Granskie J, Opler M, Sarkey S, Mucha L, et al. Patient attitudes toward and goals for Mdd treatment: a survey study. Patient Prefer Adherence. (2019) 13:959–67. doi: 10.2147/PPA.S204198
58. Holtforth M, Grawe K. Bern inventory of treatment goals: part 1. Development and first application of a taxonomy of treatment goal themes. Psychother Res. (2002) 12:79–99. doi: 10.1080/713869618;10.1093/ptr/12.1.79
59. Dickson J, Moberly N. Reduced specificity of personal goals and explanations for goal attainment in major depression. PLoS One. (2013) 8:e64512. doi: 10.1371/journal.pone.0064512
60. Dickson J, Moberly N, Kinderman P. Depressed people are not less motivated by personal goals but are more pessimistic about attaining them. J Abnorm Psychol. (2011) 120:975–80. doi: 10.1037/a0023665
61. Dickson J, Moberly N, O’Dea C, Field M. Goal fluency, pessimism and disengagement in depression. PLoS One. (2016) 11:e0166259. doi: 10.1371/journal.pone.0166259
62. Wollburg E, Braukhaus C. Goal setting in psychotherapy: the relevance of approach and avoidance goals for treatment outcome. Psychother Res. (2010) 20:488–94. doi: 10.1080/10503301003796839
63. Gard D, Sanchez A, Cooper K, Fisher M, Garrett C, Vinogradov S. Do people with schizophrenia have difficulty anticipating pleasure, engaging in effortful behavior, or both? J Abnorm Psychol. (2014) 123:771–82. doi: 10.1037/abn0000005
64. Pueschel O, Schulte D, Michalak J. Be careful what you strive for: the significance of motive-goal congruence for depressivity. Clin Psychol Psychother. (2011) 18:23–33. doi: 10.1002/cpp.697
65. Clarke S, Oades L, Crowe T, Caputi P, Deane F. The role of symptom distress and goal attainment in promoting aspects of psychological recovery for consumers with enduring mental illness. J Ment Health. (2009) 18:389–97. doi: 10.3109/09638230902968290
66. Rose G, Smith L. Mental health recovery, goal setting and working alliance in an Australian community-managed organisation. Health Psychol Open. (2018) 15:1–9. doi: 10.1177/2055102918774674
67. Sanches S, van Busschbach J, Michon H, van Weeghel J, Swildens W. The role of working alliance in attainment of personal goals and improvement in quality of life during psychiatric rehabilitation. Psychiatri Serv. (2018) 69:903–9. doi: 10.1176/appi.ps.201700438
68. Knaeps J, Neyens I, van Weeghel J, Van Audenhove C. Perspectives of hospitalized patients with mental disorders and their clinicians on vocational goals, barriers, and steps to overcome barriers. J Mental Health. (2015) 24:196–201. doi: 10.3109/09638237.2015.1036972
69. Shadmi E, Gelkopf M, Garber-Epstein P, Baloush-Kleinman V, Dudai R, Scialom S, et al. Relationship between psychiatric-service consumers’ and providers’ goal concordance and consumers’ personal goal attainment. Psychiatri Serv. (2017) 68:1312–4. doi: 10.1176/appi.ps.201600580
70. McGuire A, Oles S, White D, Salyers M. Perceptions of treatment plan goals of people in psychiatric rehabilitation. J Behav Health Serv Res. (2016) 43:494–503. doi: 10.1007/s11414-015-9463-x
71. Lenehan P, Deane F, Wolstencroft K, Kelly P. Coherence between Goals and therapeutic homework of clients engaging in recovery-oriented support. Psychiatri Rehabili J. (2019) 42:201–5. doi: 10.1037/prj0000335
72. Lecomte T, Wallace C, Perreault M, Caron J. Consumers’ goals in psychiatric rehabilitation and their concordance with existing services. Psychiatri Serv. (2005) 56:209–11. doi: 10.1176/appi.ps.56.2.209
73. Fakhoury W, Priebe S, Quraishi M. Goals of new long-stay patients in supported housing: a Uk study. Int J Soc Psychiatry. (2005) 51:45–54. doi: 10.1177/0020764005053273
74. Falloon I, Talbot R. Achieving the goals of day treatment. J Nerv Ment Dis. (1982) 170:279–85. doi: 10.1097/00005053-198205000-00005
75. Arns P, Linney J. The relationship of service individualization to client functioning in programs for severely mentally ill persons. Community Ment Health J. (1995) 31:127–37. doi: 10.1007/BF02188762
76. Kuhnigk O, Slawik L, Meyer J, Naber D, Reimer J. Valuation and attainment of treatment goals in schizophrenia: perspectives of patients, relatives, physicians, and payers. J Psychiatr Pract. (2012) 18:321–8. doi: 10.1097/01.pra.0000419816.75752.65
77. Wyder M, Kisely S, Meurk C, Dietrich J, Fawcett T, Siskind D, et al. The language we use– the effect of writing mental health care plans in the first person. Australas Psychiatry. (2018) 26:496–502. doi: 10.1177/1039856218772251
78. Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clin Rehabil. (2011) 25:468–82. doi: 10.1177/0269215510389198
Keywords: goal planning, goal setting, mental health, mental illness, recovery planning, rehabilitation, systematic integrative review
Citation: Stewart V, McMillan SS, Hu J, Ng R, El-Den S, O’Reilly C and Wheeler AJ (2022) Goal planning in mental health service delivery: A systematic integrative review. Front. Psychiatry 13:1057915. doi: 10.3389/fpsyt.2022.1057915
Received: 30 September 2022; Accepted: 02 December 2022;
Published: 19 December 2022.
Edited by:
Hector Wing Hong Tsang, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Frank Deane, University of Wollongong, AustraliaFrances Louise Dark, Metro South Addiction and Mental Health Services, Australia
Devashish Konar, Mental Health Care Centre, India
Copyright © 2022 Stewart, McMillan, Hu, Ng, El-Den, O’Reilly and Wheeler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Victoria Stewart, ✉ di5zdGV3YXJ0QGdyaWZmaXRoLmVkdS5hdQ==
 Victoria Stewart
Victoria Stewart Sara S. McMillan
Sara S. McMillan Jie Hu
Jie Hu Ricki Ng4
Ricki Ng4