
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 03 November 2022
Sec. Addictive Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1047280
This article is part of the Research TopicBehavioral addictions: Emerging scienceView all 10 articles
The prevalence of buying/shopping disorder (B/SD) has been increasing in the last two decades, and this disorder has a substantial negative impact on general functioning and quality of life. Therefore, a systematic review of the studies dedicated to the efficacy and tolerability of therapeutic interventions, both psychological and pharmacological, might help clinicians to decide on the most evidence-based treatment for these patients. In order to further increase the clinical usefulness of the current review, GRADE-based recommendations were formulated, where enough evidence was found to support such an approach. A number of five electronic databases were searched for single case reports, case series, open-label and double-blind, placebo/active intervention-controlled trials, but other secondary reports (i.e., systematic reviews and meta-analyses) were also included in this analysis. Studies with unspecified designs or those that do not report either qualitatively or quantitively the evolution of B/SD core manifestations were excluded. All data included in the secondary analysis were evaluated using the Joanna Briggs Institute critical appraisal checklists. A total number of 24 manuscripts (i.e., 12 clinical trials, eight case reports, and four reviews) were included. Most of the reviewed studies were of moderate quality, representing a certain limitation of this review and preventing the formulation of high-validity recommendations. Psychotherapy, especially cognitive behavioral therapy (CBT) seems to be the main intervention supported by the current evidence, followed by the combination of antidepressants and CBT, and serotoninergic antidepressants as monotherapy. There is an obvious need to further develop good-quality trials with a more significant number of participants with B/SD and longer follow-up periods.
“Compulsive shopping/buying” (CS/CB), also known as “buying/shopping dependence/addiction,” “pathological buying,” or “oniomania” represents a behavioral addiction defined by excessive financial investments (either online or in the real world), which cause distress or significant dysfunctions to the patients (1, 2).
While some authors consider CS/CB an addiction, others include this condition in the “impulse-control disorders” category or within the obsessive-compulsive disorders (OCD) spectrum (Figure 1) (1–3). For the objectives of this review, the term “buying/shopping disorder” (B/SD) will be used in order to avoid insufficiently proven categorizations and to highlight that reviewed therapies are dedicated to patients with significant impairments due to their behaviors, not to the shoppers who may occasionally overbuy and later regret their investments. This terminology is far from being redundant because of the continuum model several authors suggested, a model that states the difference between normality and pathology is based on the frequency and intensity of the problematic behavior and on its various dysfunctional consequences (e.g., professional, social, academic, legal, financial) (4). Also, the DSM-5 uses the same terminology, i.e., “gambling disorder” and “Internet gaming disorder” for other pathologies with intricate, addictive, compulsive, and impulsive mechanisms (5).
B/SD may be conceptualized as a behavioral addiction (BA) due to the shared core manifestations between this pathology and substance use disorders (SUDs), and also based on the presumed common hyperstimulation of the dopamine reward system (6). The overvaluation of the shopping process/objects purchased was considered similar to the high importance attributed to the drugs by patients with SUD. Also, impulsivity and lack of inhibition during drug use or shopping are shared features of these two disorders (6). This rationale is similar to other BAs, e.g., food addiction, physical exercise addiction, Internet addiction, etc. (7). Cultural factors might contribute to the pathogenesis of B/SD because it has been reported mainly in developed countries (3), but this could be a bias due to the higher income and increased accessibility to the products when compared to low and medium-income countries. According to the tenth version of the International Classification of Mental Disorders (ICD-10), B/SD may be considered an “impulse control disorder, not otherwise specified” because of the repeated acts of buying without a well-defined motivation, lack of control over these behaviors, and the presence of functional negative consequences (8). There is no mention of the B/SD in the last edition of the same classification (9).
Diagnostic criteria for B/SD have been created (10), with the accent being placed upon irresistible impulses and frequent preoccupation with buying, but also on discomfort, and time-consuming or negative financial and social consequences, in the absence of mania or hypomania. Also, a type of “co-dependent buyer” has been described in the literature, and this term is reserved for those who are driven by the desire to purchase items for other individuals based on their wish to obtain approval, to be validated emotionally, or to avoid rejection (11).
B/SD has been diagnosed as a comorbidity in patients who have SUDs, mood disorders, personality disorders, or obsessive-compulsive spectrum disorders (OCSD) (1). Compulsive hoarding, anxiety disorders, and various other impulse control disorders may also be diagnosed in patients with B/SD (12). This pathology has been associated with a high prevalence of suicidal ideation, reaching 18.4% in a study that included 4,404 patients with different behavioral addictions (out of which 158 presented B/SD) (13). Suicide attempts were detected in 7.6% of the B/SD patients, and female gender, lack of family support, and unemployment were associated with the greater risk for suicide (13). According to a case series (N = 20 patients) that used structured evaluation for patients with problematic buying behavior, 95% had lifetime diagnoses of major mood disorders, 80% associated anxiety disorders, 40% presented impulse control disorders, and 35% also suffered from eating disorders (14). Also, it was observed that first-degree relatives presented a high prevalence of mood disorders (14).
The prevalence of B/SD in the United States was estimated to be 5%, and the most vulnerable individuals to B/SD onset were adolescents and young adults (1). Women are dominant in this group, with a proportion reaching 80% in clinical samples (10). Some authors consider this difference artificial, based on research that women are more open to admitting their pathological behavior (15). A meta-analysis with 49 articles included focused on the prevalence of CS in 16 countries (N = 32,000) and reported a 4.9% pooled prevalence in adults, with higher rates in university students (up to 11.5%) (16). The prevalence of CS in shopping-specific populations (e.g., individuals shopping in supermarkets or malls) had a value of up to 27.8% (16). European surveys reported an increase in B/SD in the adult population over the last two decades, indicating the necessity to develop adequate strategies for early detection and treatment (17).
Several instruments have been created for the structured evaluation of the B/SD, e.g., the Compulsive Buying Scale (CBS), Yale-Brown Obsessive-Compulsive Scale-Shopping version (YBOCS-SV), Pathological Buying Screener (PBS), and Compulsive Buying Follow-up Scale (CBFS) (18–22). CBS includes seven items representing activities, motivations, and feelings associated with buying, and a score ≤ -1.34 indicates a possible compulsive nature of this behavior (18). Another version of the CBS included 29 items, distributed on five factors (“tendency to spend,” “compulsion/drive to spend,” “feelings about shopping and spending,” “dysfunctional spending,” and “post-purchase guilt”), and allows the classification of individuals across a compulsive buying spectrum- from normal, recreational, or borderline, to compulsive, or addictive shopping patients (19). YBOCS-SV was designed to evaluate the cognitions and behaviors related to compulsive buying, instead of assessing obsessions and compulsion, as in the original YBOCS, and it includes 10 items, with a total score interval between 0 and 40 (20). PBS has 20 items, but another, 13-item version with two factors (“loss of control/consequences” and “excessive buying behavior”), has also been created (21). CBFS is a self-administered instrument with six self-reported items that evaluate aspects of CS in the last 4 weeks, and it proved a strong sensitivity to change and recovery, with a cut-off score of 22 (22).
Regarding the pathogenesis, elevated impulsivity due to poor response inhibition was found to play an important role in experimental conditions, assessed by patients themselves or investigators, both in CS and in pathological gambling (PG) vs. healthy controls (2). Another trial (N = 103 patients with B/SD) supported a closer relationship between B/SD and BA than between B/SD and obsessive-compulsive symptoms, based on two delayed discounting tasks as markers of behavioral impulsivity (23). Mental disengagement could significantly predict vulnerability toward B/SD, according to a study based on an online questionnaire (N = 189 participants), which evaluated the main coping mechanisms used by these patients (24). Denial and substance use were also dysfunctional coping methods with predictive value for B/SD onset (24). A poorly developed, ambivalent, or contradictory self-image may create a vulnerable terrain for dysfunctional object attachment behaviors that may predict the B/SD onset (25). This disorder may be considered a chronic and repetitive failure in self-regulation, with cognitive, affective, and behavioral factors involved in different phases of the pathogenesis (26). Although these observations may have a significant impact on the therapy, there are many confounding factors that may limit their relevance for B/SD patients (e.g., research in laboratory settings vs. real-life conditions, lack of control for significant variables in the case of online questionnaires, or absence of culturally-defined variables that may contribute to the onset of B/SD in the explored studies). However, it is expected that the analysis of these outcomes (e.g., dysfunctional coping mechanisms, self-image distortions, and behavioral impulsivity) could be useful from the perspective of finding the most evidence-based therapies for patients with B/SD.
The neurobiological dimensions of B/SD have been hypothesized to involve serotoninergic, dopaminergic, and opioidergic neurotransmission, similar to other behavioral addictions, OCD, and substance use disorders (10). Based on these presumed mechanisms, the potential benefits of psychopharmacological agents (i.e., selective serotonin reuptake inhibitors-SSRIs, serotonin and norepinephrine reuptake inhibitors—SNRIs, opioid receptors antagonists—ORAs, or mood stabilizers) have been inferred. However, studies exploring the direct correlations between specific neurotransmitters or neuroanatomic pathways and the onset of B/SD are still lacking.
A genetic component of B/SD has been suggested, even if the available data support more of a vulnerability toward psychiatric disorders in first-degree relatives of B/SD patients than a specific tendency for CS (10). For example, CS/CB has been reported more frequently in descendants of individuals presenting with depression or substance use disorders (10).
In conclusion, the necessity of investigating the available treatments for B/SD is derived from multiple factors: the use of excessive buying as a way to cope with stress or isolation (27); negative functional consequences and risk of a chronic course (28); and the relatively high and increasing prevalence of problematic buying in the general population (1, 16). The need to assess the efficacy of psychotherapeutic, pharmacological and combined therapies in BAs or SUDs is also motivated by the high societal and personal costs associated with healthcare in B/SD, high risk of psychiatric or somatic comorbidity, and lower quality of life (29).
The main objective was to review the available data regarding the efficacy and tolerability of therapeutic interventions in the treatment of B/SD.
The second objective was to assess the validity of evidence-based recommendations, according to the GRADE system (30), for the therapeutic management of B/SD.
A systematic review was conducted in order to find the effects of therapeutic interventions dedicated to adult patients with B/SD. Primary and secondary reports, i.e., clinical reports, clinical and epidemiological studies, and reviews, were included in the analysis. The data extraction was guided by the PRISMA 2020 statements (31–33), and the corresponding steps are represented in Table 1. No automation tool was used in the process of data extraction.
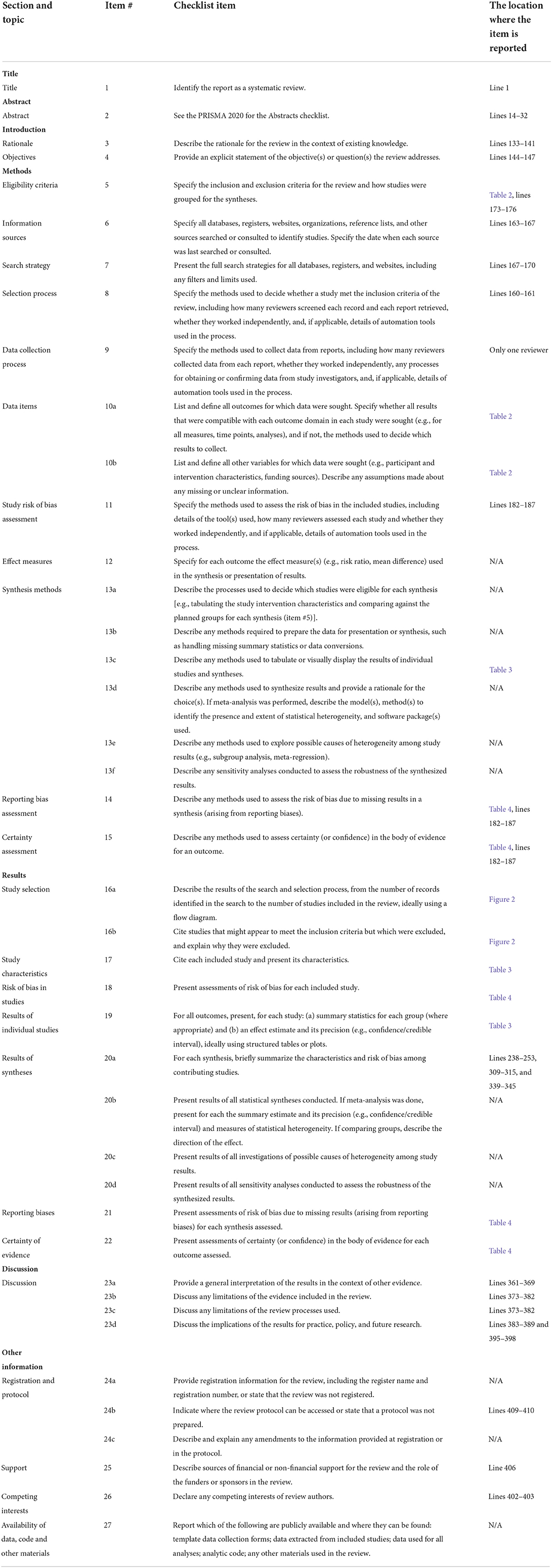
Table 1. PRISMA 2020 checklist (31).
Five electronic databases (PubMed, PsychInfo, Cochrane, EMBASE, Clarivate/Web of Science) were included in the primary search. Also, the register of clinical trials run by the US National Library of Medicine (NLM) (www.clinicaltrials.gov) was explored for potential data regarding clinical trials dedicated to this topic. Also, websites and organizational websites dedicated to patients with B/SD were included in the sources exploration, and citation searching was also allowed.
The search paradigm used was “compulsive buying” OR “buying addiction” OR “shopping addiction” OR “shopping/buying dependence” AND “psychotherapy” OR “pharmacotherapy” OR “antidepressants” OR “mood stabilizers” OR “opioid antagonists” OR “medication”. All papers published between January 1990 and July 2022 were included in the primary search.
Based on the SPIDER criteria (34), the retrieved sources were evaluated to see if they may be considered suitable for review (Table 2). The main sets of criteria referred to the characteristics of the sample, type of intervention, design of the research, methods of outcomes evaluation, and type of study (34).
The quality of trials, case reports, and systematic reviews included in this analysis was assessed according to the Joanna Briggs Institute (JBI) critical appraisal checklists (57). These criteria were preferred because primary and secondary reports were allowed to enter the reviewing stage, and both qualitative and quantitative data were expected to result from the primary search. According to the JBI checklists, the sources may be included, excluded, or seeking further information is recommended (35, 36).
The GRADE criteria for assessing the strength of recommendations based on the found evidence were applied to the final conclusions (31–33).
Out of the initial 861 papers collected through the primary search, only 24 reached the final stage of selection (Figure 2). Eight case reports, 12 clinical studies, and four systematic reviews/meta-analyses were reviewed in detail, and the results are presented in Table 3. JBI Critical Appraisal Checklists for Case Reports, Randomized Studies, Quasi-experimental design studies, and Systematic Reviews were used in order to evaluate the quality of the research (35, 36).
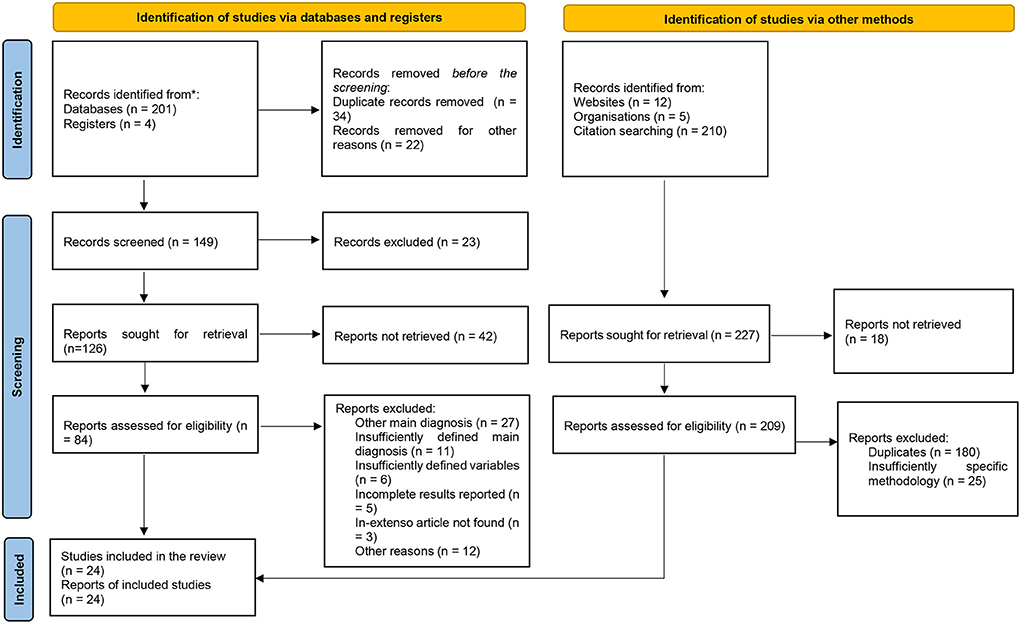
Figure 2. PRISMA 2020 flow diagram for systematic reviews (31).
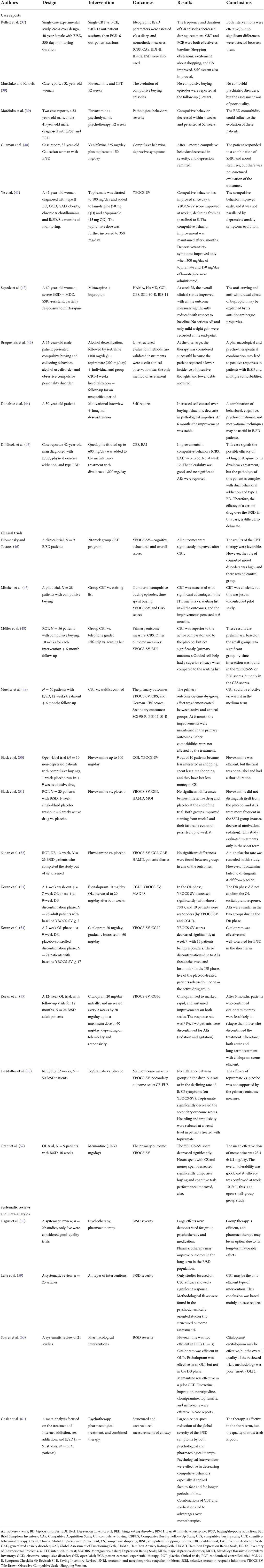
Table 3. The main data reviewed for the evaluation of the efficacy and tolerability of therapeutic interventions in patients with B/SD.
A case study with a cross-over design that compared cognitive-behavioral therapy (CBT) and person-centered experiential therapy (PCE) in a 40-year-old B/SD patient found beneficial results for both interventions (37). These favorable effects were detected on ideographic (i.e., amount of money spent daily, time invested in B/SD, time spent on talking about buying, and B/SD-related cognitions and emotions) and nomothetic (i.e., scores on CBS, Compulsive Acquisition Scale, Beck Depression Inventory-II, Inventory of Interpersonal Problems-32, and Brief Symptom Inventory) outcomes related to B/SD severity, with no relapse over the follow-up period (99 days) (37). Another single-case report supports the therapeutic effect of the fluvoxamine and CBT combination in a female patient with B/SD during 52 weeks of unstructured monitoring, but no information about the duration of the psychotherapy or the antidepressant treatment was provided in this report (38). The same authors reported positive effects of the fluvoxamine (up to 150 and 200 mg daily, respectively) and psychodynamically-oriented psychotherapy (weekly sessions) in two female patients with B/SD and binge eating disorder (BED) after 3 weeks of combined treatment (39). No systematic methods were used to assess B/SD, but craving for buying and compulsive acts (e.g., shopping for large quantities of food, designer clothes or jewelry, acquiring antique objects, and compulsive eating) decreased based on patient self-report and clinician's observation (39).
Topiramate was explored as a potential treatment for B/SD in a 37-year-old female diagnosed with persistent B/SD and depression who was non-responsive to fluoxetine and venlafaxine. Topiramate was also selected based on previous reports of its efficacy in treating mood disorders and OCD (40). In this study, topiramate was added to venlafaxine up to 150 mg/day. The compulsive behavior (i.e., excessive shopping, mainly clothes) subsided in a month (but no objective measurement was provided by the authors), while depression was fully remitted (according to the Beck Depression Inventory scores) (40). Another case study explored the effect of topiramate (titrated up to 350 mg/day) as an augmenting agent in a 42-year-old female diagnosed with OCD, type II bipolar disorder, generalized anxiety disorder, obesity, trichotillomania, and B/SD (41). This patient also received lamotrigine and aripiprazole, which were added to topiramate, and the compulsive behaviors declined gradually for 6 months (according to the YBOCS-SV scores), with a slower pace of improvement for the anxiety and depressive manifestations (41).
The augmentation of mirtazapine (30 mg/day) with bupropion (300 mg/day) in a 60-year-old female patient diagnosed with a severe form of B/SD (i.e., high CBS score, spent family's money, ran into debt) and comorbid MDD led to clinical and psychometric improvements by week 8 (42). The compulsive behavior (assessed with CBS) remained significantly decreased at the end-point (week 28) (42). The assessment of the associated symptoms included the use of the Hamilton Anxiety Rating Scale (HAMA), Hamilton Depression Rating Scale (HAMD), Symptom Checklist-90-Revised (SCL-90-R), and Barratt Impulsiveness Scale (BIS-11) (42). All these scales recorded improvements (i.e., the severity of associated anxiety, depressive, and impulsive symptoms decreased). Also, the global overall clinical status, determined by the use of Clinical Global Impression (CGI), improved significantly at the final visit (42). The overall tolerability was good, with only a 4% increase in weight gain (42).
A combination of sertraline, topiramate, and group and individual CBT was associated with favorable results after discharge in a 53-year-old patient diagnosed with pathological buying and collecting behaviors, obsessive-compulsive personality disorder, and alcohol use disorder (43). The initial stage of the therapeutic management consisted of alcohol detoxification, followed by the combined intervention previously mentioned, that targeted both addictive and compulsive behaviors (43). No clinically validated scales were used to assess either hoarding or B/SD; the authors based their conclusions solely on clinical observation and patient reports (i.e., involvement in excessive shopping and hoarding, debt amount, and obsessions) (43).
Motivational interviewing and imaginal desensitization were successfully combined in a 30-year-old patient diagnosed with B/SD because they succeeded in increasing self-control over buying behaviors while decreasing the manifestation of pathological impulses (44). At 6 months, the improvement of the overall status was considered stable, assessed by clinicians' observations (44). Motivational interviewing helped the patient to develop intrinsic motivation for change, while the desensitization techniques were useful for confrontation and controlling impulsive behaviors (44).
The combination of quetiapine and divalproex was used as maintenance treatment in a 47-year-old male patient who presented with type I bipolar disorder comorbid with two behavioral addictions- B/SD and physical exercise addiction (45). After 12 weeks, the CS severity decreased under quetiapine (titrated up to 600 mg/day), according to the CBS scores, and the overall tolerability of this antipsychotic was good (45). The physical exercise addiction severity also decreased, according to the Exercise Addiction Inventory (EAI) scores (45).
Based on eight case reports, which evaluated the efficacy of pharmacological, psychotherapeutic, or combined interventions in nine patients presenting B/SD with psychiatric comorbidities (bipolar disorder N = 2, other BAs N = 2, personality disorders N = 1, substance use disorders N = 1, depressive disorders N = 2, OCD N = 1, anxiety disorders N = 1, impulse control disorders N = 1, eating disorders N = 1)/without such comorbidities (N = 1), the short-term prognosis of these individuals may be improved if treatment is initiated. The overall quality of data is low because there was no control group, not all reports have used structured and validated instruments for the monitoring of B/SD severity, concomitant medication was added in several cases, and there is a high degree of comorbidity, which may lead to a number of biases. Fluvoxamine combined with psychotherapy is supported by most data in this chapter, followed by various antidepressants (i.e., mirtazapine, venlafaxine, bupropion, and sertraline) either administered alone or in combinations, were associated with improved B/SD symptoms. Mood stabilizers (e.g., lamotrigine, topiramate, and divalproex) and atypical antipsychotics (i.e., aripiprazole and quetiapine) have been used especially in patients with B/SD and mood disorders, which make difficult to distinguish the impact of each disorder's impact over the clinical evolution. Very few reports on psychotherapy as the only intervention for these patients exist, therefore it is impossible to draw any conclusion on this topic for now.
A 20-week group CBT program was evaluated in a pilot study (N = 9 B/SD patients, mean age 41.8 years old) (46). Group therapy dedicated to the detection of specific shopping cognitive distortions and restructuring led to improvements in the cognitive, behavioral, and total scores of the YBOCS-SV after the therapy ended (46). Seven of the included patients currently presented with comorbid depression, and two of them had bipolar disorder, therefore, the results may be influenced by these comorbidities, which is impossible to establish without a control group (46).
The authors state, however, that “loss of control over shopping was not better explained by mood disorders since shopping bouts also occurred during periods of euthymia” (46).
A pilot study enrolled 28 compulsive buyers recruited through mass-media advertisements who subsequently received 12 sessions of group CBT over 10 weeks. Participants undergoing CBT had superior outcomes compared to the wait-list control in all the outcomes (both clinical variables and structured evaluation scores) at the end of treatment and 6-month follow-up (47). The main outcomes assessed were the number of compulsive buying episodes, time spent buying, YBOCS-SV, and CBS scores (47). Although this was just a pilot study, the results support the efficacy of group CBT on compulsive buying in outpatients with B/SD. Its main limitation is the absence of a comparison treatment, which prevents the causal correlation between this specific intervention (i.e., group CBT) and the outcome (i.e., improvement of the B/SD severity) (47).
Another pilot study included 56 patients with B/SD who were randomized on group CBT, telephone-guided self-help, or waiting list and monitored for the 10 weeks of the treatment, with a 6-month follow-up (48). Group CBT was superior to the self-help intervention and to the waiting list in reducing compulsive behaviors, and the favorable results were still present after 6 months (48). The CBS and YBOCS-SV scores declined significantly when compared to the baseline values for both active interventions, but the end-point differences between groups were not significant (48).
Another CBT trial focused on interruption and control of CS behaviors, training of healthy coping skills, and cognitive restructuring and enrolled 60 B/SD patients who were monitored for 12 weeks, with a 6-month follow-up (49). Significant improvement was detected in patients who received CBT vs. patients assigned to a waiting list at week 12, according to the primary outcome variables (YBOCS-SV, CBS, German-CBS) (49). Also, the improvement persisted at 6 months, but other psychopathology variables (i.e., compulsive hoarding, general psychopathology, impulsivity) were not significantly changed by the CBT vs. placebo (49).
A 9-week open-label trial with fluvoxamine (up to 300 mg/day) had a 1-week placebo run-in phase and included 10 non-depressed patients with CS (50). At the end of the trial, 9 patients presented improvements in their preoccupations, time spent, and money spent with these compulsive behaviors (50). Another 9-week trial, this time with a randomized, double-blind design following a 1-week single-blind placebo washout phase, did not find significant differences between fluvoxamine and placebo in any of the outcome measures, except for Maudsley Obsessive-Compulsive Inventory (MOCI) (51). In this second trial, fluvoxamine was associated with more adverse events than placebo, mainly nausea, insomnia/sedation, and decreased motivation (51). Yet another trial that evaluated fluvoxamine used a randomized, double-blind, placebo-controlled design and recruited 42 patients, out of which 23 completed the study after 13 weeks (52). No significant differences between groups were detected in any of the outcomes- YBOCS-SV, CGI, Global Assessment of Functioning (GAF), HAMD, and patients' self-reported compulsive behaviors (52).
In two trials conducted by the same team that used the same design (7-week open-label phase of active drug administration, followed by 9 weeks of double-blind, active drug vs. placebo), citalopram proved itself efficient in decreasing the YBOCS-SV scores and inducing higher response rate than placebo, but escitalopram was associated with favorable results only in the open-label phase (53, 54). However, these trials included small groups for each arm and relatively short durations of monitoring, therefore, their results should be interpreted with caution. In yet another trial, citalopram was administered open-label for 12 weeks in B/SD patients (N = 24), and it led to rapid, significant, and sustained improvements in both YBOCS-SV and CGI-I scores (55). Citalopram was associated with positive effects at 12 months of follow-up when compared to lack of treatment due to discontinuation (55).
A randomized, double-blind, controlled trial evaluated the efficacy of topiramate (up to 300 mg/day in the ninth week, if tolerated) vs. placebo for 12 weeks in 50 patients with B/SD (56). The superiority of topiramate vs. placebo was not confirmed by the main outcome measure (YBOCS-SV), and only clinical variables (hoarding, impulsivity) and Compulsive Buying Follow-Up Scale (CB-FUS) scores confirmed the efficacy of topiramate vs. placebo (56). However, the follow-up analysis suggested that topiramate may begin to distinguish itself from placebo after 10 weeks, which indicates the need for a longer duration of monitoring (56).
Memantine (23.4 ± 8.1 mg/day mean effective dose) improved the YBOCS-SV scores in a 10-week open-label trial that enrolled nine B/SD patients (57). The overall tolerability of memantine was good (57), but it should be mentioned that this was an open-label, small-group study, therefore, the efficacy results should be confirmed in larger trials.
According to the analysis of 12 clinical trials (N = 153 patients), mostly of moderate quality, group CBT benefits from consistent evidence of efficacy at 6 months, while the results supporting pharmacological interventions are scarce. Fluvoxamine led to negative results (n = 3 trials, N = 56 patients) on the main outcomes (i.e., CS severity and related variables, determined by either self-reported or clinician-rated scales) and possible low tolerability (reported in one trial), while citalopram and escitalopram (N = 74 participants) were associated with mixed results. Topiramate and memantine were evaluated only in one trial each (50 and nine patients, respectively), therefore, it is difficult to formulate clear conclusions about their efficacy in B/SD patients.
A systematic review of the psychotherapy (n = 17 studies) and drug treatmentsn=12 studies) concluded, based on mostly moderate and low-quality data (according to the criteria applied by the authors), that large effects were present for group psychotherapy and medication (58). Long-term treatment was correlated with better outcomes during pharmacotherapy but not when psychotherapy was administered (58).
Another review (n = 23 studies) concluded that CBT might be the only efficient method for the treatment of B/SD patients (59). However, this conclusion was based on case reports, and it must be mentioned that other psychotherapies did not use structured and validated instruments for the outcome measurements.
A review of 21 studies evaluating different pharmacological interventions found that placebo-controlled trials with fluvoxamine did not show effectiveness vs. placebo in B/SD patients, open-label trials with citalopram favored the active intervention vs. placebo, escitalopram was effective in an open-label trial, but not in the double-blind phase, and memantine was efficient only in a pilot open-label study (60). The authors of this review concluded that there is not enough evidence to support the recommendation of a specific agent for B/SD treatment (60).
In a meta-analysis dedicated to the pharmacological and psychological interventions for various behavioral addictions (Internet/sex/shopping dependence) that included 91 studies (N = 3531 participants), the results supported the efficacy of both types of therapy in the short-term (61). For B/SD, a large-sized pre-post decrease in the global severity of pathological behaviors was calculated: Hedge's g = 1.00 for psychotherapy and 1.52 for pharmacotherapy (61). The combined psychotherapy and pharmacological approach led to superior results to monotherapies, but the efficacy was demonstrated only in the short term (61).
The four systematic reviews/meta-analyses previously presented have formulated contradictory conclusions: while one found psychotherapy to be associated with the highest effect size (based on the results of 29 studies), another reported a superior effect size for pharmacotherapy (based on 91 studies) (58, 61). In the two reviews that evaluated only psychotherapeutic interventions and only pharmacotherapy respectively (based on 23 and 21 studies), CBT was considered the only efficient method (59), while no pharmacological agent could be recommended yet as monotherapy for B/SD patients (60).
B/SD is a very complex pathology, which integrates elements from BAs, OCD spectrum, and impulse control disorders, which raises the question of the heterogeneity of the populations included in the reviewed reports. It could be conceived that some of them are more close to a BA, some of them are more impulsive, while still others associate elements from the OCD spectrum. Various combinations of these dimensions in the same patient are also theoretically possible, and the high rate of comorbidity reported in this population may support this perspective.
Based on reviewing 24 distinct sources, representing case reports (n = 8), clinical trials (n = 12), and systematic reviews/meta-analyses (n = 4), it may be concluded that psychotherapy, and especially group CBT may be recommended for B/SD patients (supported by the results of two reviews, one case study, and four clinical trials) (Table 5). Combined, pharmacotherapy and psychotherapy, may be recommended, but the data in favor of this strategy is less significant (supported by three case reports, and one meta-analysis). No specific recommendations for pharmacological agents could be made, although positive results with serotonergic antidepressants and topiramate exist. In patients with associated mood disorders, mood stabilizers (topiramate, lamotrigine, divalproex) and atypical antipsychotics (aripiprazole, quetiapine) have been correlated with positive results in case studies.
The GRADE recommendations formulated were A (high), B (moderate), C (low), or D (very low) (42, 55), according to the level of confidence that therapeutic interventions will improve the outcome of patients with B/SD.
The strengths of the current review rely on the inclusion of both primary and secondary reports detected through a systematic literature search and on the formulation of evidence-based recommendations with potential clinical utility. The reports were assessed for methodological quality using validated checklists (JBI), and the recommendations were made in accordance with GRADE criteria.
As limitations of the current review, it must be mentioned that conclusions integrated data derived from studies with multiple comorbidities, but since not all the researchers have made a thorough screening for psychiatric comorbidity at baseline, it is possible that other pathologies might be escaped, and yet influenced the outcomes. Due to the high rate of dual diagnosis in B/SD, screening for other psychiatric disorders is needed initially and periodically in this population. The high rate of SUDs and behavioral addictions with other psychiatric disorders has been reported in many sources (1, 15, 18, 19, 36, 62). It is difficult to interpret data resulting from the treatment of patients with multiple comorbidities, especially in case reports. The quality of the reviewed data is heterogenous, with case reports not using structured methods of monitoring, and a short duration of observation. Another limitation derives from the fact that data extraction and quality assessment were conducted by only one researcher.
Regarding the specifics of the recommendations for patients with B/SD, fewer sessions of group therapy and more severe pre-treatment hoarding features were significant predictors for nonresponse to the CBT (63). The risk of poor adherence to the individual CBT program was 28% in a study that enrolled 97 B/SD patients (63). Also, a significant discontinuation rate of 46.4% was reported, and the predictors of poor therapy adherence were male gender, more severe depression and obsessive-compulsive symptoms, lower anxiety level, high persistence, high harm avoidance, and low self-transcendence (63).
The prognosis of B/SD management is dependent on the adequate treatment of comorbid psychiatric conditions, psychological vulnerability factors, and sufficient time for monitoring. Therefore, an initial comprehensive evaluation of the patients presenting CS/CB is granted.
It is expected that further research will evaluate larger populations and more homogeneous participants. Also, a longer duration of clinical trials is needed, in order to confirm the efficacy of therapeutic interventions in patients with a known high rate of relapse.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
OV contributed to the article and approved the submitted version.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Black DW. Compulsive shopping: a review and update. Curr Opin Psychol. (2022) 46:101321. doi: 10.1016/j.copsyc.2022.101321
2. Williams AD. Are compulsive buyers impulsive? Evidence for poor response inhibition and delay discounting. J Exp Psychopathol. (2012) 3:794–806. doi: 10.5127/jep.025211
4. d'Astous A. An inquiry into the compulsive side of “normal” consumers. J Consumer Policy. (1990) 13:15–31. doi: 10.1007/BF00411867
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Arlington: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
6. Hartston H. The case for compulsive shopping as an addiction. J Psychoact Drugs. (2012) 44:64–7. doi: 10.1080/02791072.2012.660110
7. Vasiliu O. Current status of evidence for a new diagnosis: food addiction—a literature review. Front Psychiatry. (2022) 12:824936. doi: 10.3389/fpsyt.2021.824936
8. World Health Organization. The ICD-10 classification of mental and behavioral disorders. Geneva: WHO (1993).
9. World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th Edn. Geneva: ICD-11. WHO (2019). Available online at: https://icd.who.int/browse11/l-m/en (accessed September 17, 2022).
10. Tavares H, Lobo DSS, Fuentes D, Black DW. Compulsive buying disorder: a review and a case vignette. Rev Bras Psiquiatr. (2008) 30(Suppl.1):S16–23. doi: 10.1590/S1516-44462008005000002
11. Boundy D. When money is the drug. In:Benson AL, , editor. I Shop, Therefore I Am: A Compulsive Buying and the Search for Help. Northrade, NJ: Aronson (2000), pp. 3–16.
12. Mueller A, de Zwaan M. Treatment of compulsive buying. Fortschr Neurol Psychiatr. (2008) 76:478–83. doi: 10.1055/s-2008-1038227
13. Valenciano-Mendoza E, Fernandez-Aranda F, Granero R, Gomez-Peña M, Moragas L, Mora-Maltas B, et al. Prevalence of suicidal behavior and associated clinical correlates in patients with behavioral addictions. Int J Environ Res Public Health. (2021) 18:11085. doi: 10.3390/ijerph182111085
14. Mc Elroy SL, Keck PE, Pope HG, Smith JM, Strakowski SM. Compulsive buying: a report of 20 cases. J Clin Psychiatry. (1994) 55:242–8.
15. Koran LM, Faber RJ, Aboujaoude E, Large MD, Serpe RT. Estimated prevalence of compulsive buying in the United States. Am J Psychiatry. (2006) 163:1806–12. doi: 10.1176/ajp.2006.163.10.1806
16. Maraz A, Griffiths MD, Demetrovics Z. The prevalence of compulsive buying: a meta-analysis. Addiction. (2016) 111:408–19. doi: 10.1111/add.13223
17. Muller A, Mitchell JE, de Zwaan M. Compulsive buying. Am J Addict. (2015) 24:132–7. doi: 10.1111/ajad.12111
18. Faber RJ, O'Guinn TC, A. clinical screener for compulsive buying. J Consum Res. (1992) 19:459–69. doi: 10.1086/209315
19. Edwards EA. Development of a new scale to measure compulsive buying behavior. Finan Counsel Plan. (1993) 4:67–84.
20. Monahan P, Black DW, Gabel J. Reliability and validity of a scale to measure change in persons with compulsive buying. Psychiatry Res. (1996) 64:59–67. doi: 10.1016/0165-1781(96)02908-3
21. Müller A, Trotzke P, Mitchell JE, de Zwaan M, Brand M. The pathological buying screener: Development and psychometric properties of a new screening instrument for the assessment of pathological buying symptoms. PLoS ONE. (2015) 10:e0141094. doi: 10.1371/journal.pone.0141094
22. de Mattos CN, Kim HS, Filomensky TZ, Tavares H. Development and validation of the compulsive-buying follow-up scale: a measure to assess treatment improvements in compulsive buying disorder. Psychiatry Res. (2019) 282:112009. doi: 10.1016/j.psychres.2018.12.078
23. Nicolai J, Moshagen M. Dissociating pathological buying from obsessive-compulsive symptoms using delay discounting. Zeitschrift für Psychologie. (2017) 225:244–51. doi: 10.1027/2151-2604/a000308
24. Lawrence LM, Elphinstone B. Coping associated with compulsive buying tendency. Stress Health. (2021) 37:263–71. doi: 10.1002/smi.2994
25. Moulding R, Kings C, Knight T. The things that make us: self and object attachment in hoarding and compulsive buying-shopping disorder. Curr Opin Psychol. (2021) 39:100–4. doi: 10.1016/j.copsyc.2020.08.016
26. Kellett S, Bolton JV. Compulsive buying: a cognitive-behavioural model. Clin Psychol Psychother. (2009) 16:83–99. doi: 10.1002/cpp.585
27. Vasiliu O, Vasile D, Vasiliu DG, Ciobanu OM. Quality of life impairments and stress coping strategies during the Covid-19 pandemic isolation and quarantine: a web-based survey. Rom J Milit Med. (2021) CXXIV(1):10–21. doi: 10.55453/rjmm.2021.124.1.2
28. Aboujaoude E. Compulsive buying disorder: a review and update. Curr Pharm Des. (2014) 20:4021–5. doi: 10.2174/13816128113199990618
29. Vasiliu O. Current trends and perspectives in the immune therapy for substance use disorders. Front Psychiatry. (2022) 13:882491. doi: 10.3389/fpsyt.2022.882491
30. Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidem. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015
31. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
32. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:89. doi: 10.1186/s13643-021-01626-4
33. Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis finding-paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci. (2018) 13(Suppl.1):10. doi: 10.1186/s13012-017-0689-2
34. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. (2012) 22:1435–43. doi: 10.1177/1049732312452938
35. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In:Aromataris E, Munn Z, , editors. JBI Manual for Evidence Synthesis. Miami: JBI (2020). doi: 10.46658/JBIMES-20-08
36. The University of Adelaide. JBI's Critical Appraisal Tools Assist in Assessing the Trustworthiness, Relevance and Results of Published Papers. Adelaide: The University of Adelaide. Available online at: https://jbi.global/critical-appraisal-tools (accessed September 10, 2022).
37. Kellett S, Oxborough P, Gaskell C. Treatment of compulsive buying disorder: comparing the effectiveness of cognitive behavioural therapy with person-centered experiential counselling. Behav Cogn Psychother. (2021) 49:370–84. doi: 10.1017/S1352465820000521
38. Marčinko D, Kalovič D. Oniomania-successful treatment with fluvoxamine and cognitive-behavioral psychotherapy. Psychiatr Danub. (2005) 17:97–100.
39. Marčinko D, Bolanča M, Rudan V. Compulsive buying and binge eating disorder: a case vignette. Prog Neuro-Psychopharmacol Biol Psychiatry. (2006) 30:1542–4. doi: 10.1016/j.pnpbp.2006.05.009
40. Guzman CS, Filomensky T, Tavares H. Compulsive buying treatment with topiramate, a case report. Rev Bras Psiquiatr. (2007) 29:380–5. doi: 10.1590/S1516-44462007000400016
41. Ye L, Kadia S, Lippman S. Topiramate and compulsive buying disorder. Topiramate and compulsive buying disorder. J Clin Psychopharmacol. (2014) 34:174–5. doi: 10.1097/JCP.0b013e3182aa0139
42. Sepede G, Di Iorio G, Sarchione F, Fiori F, Di Giannantonio M. Bupropion augmentation in a case of compulsive buying disorder. Clin Neuropharmacol. (2017) 40:189–91. doi: 10.1097/WNF.0000000000000232
43. Braquehais MD, Valls DM, Sher L, Cass M. Pathological collecting: a case report. Int J Disabil Hum Dev. (2012) 11:81–3. doi: 10.1515/ijdhd.2012.001
44. Donahue CB, Odlaug B, Grant JE. Compulsive buying treated with motivational interviewing and imaginal desensitization. Ann Clin Psychiatry. (2011) 23:226–7.
45. Di Nicola M, Martinotti G, Mazza M, Tedeschi D, Pozzi G, Janiri L. Quetiapine as add-on treatment for bipolar I disorder with comorbid compulsive buying and physical exercise addiction. Prog Neuropsychopharmacol Biol Psychiatry. (2010) 34:713–4. doi: 10.1016/j.pnpbp.2010.03.013
46. Filomensky TZ, Tavares H. Cognitive restructuring for compulsive buying. Rev Bras Psiquiatr. (2009) 31:76–81. doi: 10.1590/S1516-44462009000100018
47. Mitchell JE, Burgard M, Faber R, Crosby RD, de Zwaan M. Cognitive behavioral therapy for compulsive buying disorder. Behav Res Ther. (2006) 44:1859–65. doi: 10.1016/j.brat.2005.12.009
48. Müller A, Arikian A, de Zwaan M, Mitchell JE. Cognitive-behavioural group therapy vs. guided self-help for compulsive buying disorder: a preliminary study. Clin Psychol Psychother. (2013) 20:28–35. doi: 10.1002/cpp.773
49. Mueller A, Mueller U, Silbermann A, Reinecker H, Bleich S, Mitchell JE, et al. randomized, controlled trial of group cognitive-behavioral therapy for compulsive buying disorder: posttreatment and 6-month follow-up results. J Clin Psychiatry. (2008) 69:1131–8. doi: 10.4088/JCP.v69n0713
50. Black DW, Monahan P, Gabel J. Fluvoxamine in the treatment of compulsive buying. J Clin Psychiatry. (1997) 58:159–63.
51. Black DW, Gabel J, Hansen J, Schlosser S, A. double-blind comparison of fluvoxamine vs. placebo in the treatment of compulsive buying disorder. Ann Clin Psychiatry. (2000) 12:205–11. doi: 10.3109/10401230009147113
52. Ninan PT, McElroy SL, Kane CP, Knight BT, Casuto LS, Rose SE, et al. Placebo-controlled study of fluvoxamine in the treatment of patients with compulsive buying. J Clin Psychopharmacol. (2000) 20:362–6. doi: 10.1097/00004714-200006000-00012
53. Koran LM, Aboujaoude EN, Solvason B, Gamel NN, Smith EH. Escitalopram for compulsive buying disorder; a double-blind discontinuation study. J Clin Psychopharmacol. (2007) 27:225–7. doi: 10.1097/01.jcp.0000264975.79367.f4
54. Koran LM, Chuong HW, Bullock KD, Smith SC. Citalopram for compulsive shopping disorder: an open-label study followed by double-blind discontinuation. J Clin Psychiatry. (2003) 64:793–8. doi: 10.4088/JCP.v64n0709
55. Koran LM, Bullock KD, Hartston HJ, Elliott MA, D'Andrea V. Citalopram treatment of compulsive shopping: an open-label study. J Clin Psychiatry. (2002) 63:704–8. doi: 10.4088/JCP.v63n0808
56. de Mattos CN, Kim HS, Marasaldi RF, Requião MG, de Oliveira EC, Filomensky TZ, et al. A 12-week randomized, double-blind, placebo-controlled clinical trial of topiramate for the treatment of compulsive buying disorder. J Clin Psychopharmacol. (2020) 40:186–90. doi: 10.1097/JCP.0000000000001183
57. Grant JE, Odlaug BL, Mooney M, O'Brien R, Kim SW. Open-label pilot study of memantine in the treatment of compulsive buying. Ann Clin Psychiatry. (2012) 24:119–26.
58. Hague B, Hall J, Kellett S. Treatments for compulsive buying: a systematic review of the quality, effectiveness and progression of the outcome evidence. J Behav Addict. (2016) 5:379–94. doi: 10.1556/2006.5.2016.064
59. Leite PL, Pereira VM, Nardi AE, Silva AC. Psychotherapy for compulsive buying disorder: a systematic review. Psychiatry Res. (2014) 219:411–9. doi: 10.1016/j.psychres.2014.05.037
60. Soares C, Fernandes N, Morgado P. A review of pharmacologic treatment for compulsive buying disorder. CNS Drugs. (2016) 30:281–91. doi: 10.1007/s40263-016-0324-9
61. Goslar M, Leibetseder M, Muench HM, Hofmann SG, Laireiter AR. Treatments for internet addiction, sex addiction and compulsive buying: a meta-analysis. J Behav Addict. (2020) 9:14–43. doi: 10.1556/2006.2020.00005
62. Vasiliu O. Maintenance pharmacologic therapies for opioid use disorders: beyond opioid agonists. Rom J Military Med. (2019) CXXII:52–70. doi: 10.55453/rjmm.2019.122.1.8
Keywords: compulsive buying, shopping addiction, behavioral addictions, psychotherapy, antidepressants, mood stabilizers, atypical antipsychotics
Citation: Vasiliu O (2022) Therapeutic management of buying/shopping disorder: A systematic literature review and evidence-based recommendations. Front. Psychiatry 13:1047280. doi: 10.3389/fpsyt.2022.1047280
Received: 17 September 2022; Accepted: 19 October 2022;
Published: 03 November 2022.
Edited by:
Hyoun S. Kim, Ryerson University, CanadaReviewed by:
Vanessa Montemarano, Ryerson University, CanadaCopyright © 2022 Vasiliu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Octavian Vasiliu, b2N0YXZ2YXNpbGl1QHlhaG9vLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.