- Department of Acupuncture and Rehabilitation, Jiangsu Province Hospital of Chinese Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, Jiangsu, China
Objective: The number of citations to a paper represents the weight of that work in a particular area of interest. Several highly cited papers are listed in the bibliometric analysis. This study aimed to identify and analyze the 100 most cited papers in insomnia research that might appeal to researchers and clinicians.
Methods: We reviewed the Web of Science (WOS) Core Collection database to identify articles from 1985 to 24 March 2022. The R bibliometric package was used to further analyze citation counts, authors, year of publication, source journal, geographical origin, subject, article type, and level of evidence. Word co-occurrence in 100 articles was visualized using VOS viewer software.
Results: A total of 44,654 manuscripts were searched on the Web of Science. Between 2001 and 2021, the top 100 influential manuscripts were published, with a total citation frequency of 38,463. The top countries and institutions contributing to the field were the U.S. and Duke University. Morin C.M. was the most productive author, ranking first in citations. Sleep had the highest number of manuscripts published in the top 100 (n = 31), followed by Sleep Medicine Reviews (n = 9). The most cited manuscript (Bastien et al., Sleep Medicine, 2001; 3,384 citations) reported clinical validation of the Insomnia Severity Index (ISI) as a brief screening indicator for insomnia and as an outcome indicator for treatment studies. Co-occurrence analyses suggest that psychiatric disorders combined with insomnia and cognitive behavioral therapy remain future research trends.
Conclusion: This study provides a detailed list of the most cited articles on insomnia. The analysis provides researchers and clinicians with a detailed overview of the most cited papers on insomnia over the past two decades. Notably, COVID-19, anxiety, depression, CBT, and sleep microstructure are potential areas of focus for future research.
Introduction
Insomnia has been emerging with more public concerns over the past decades for affecting people’s health and well-being worldwide. The prevalence of insomnia disorder is approximately 10–20%, with approximately 50% having a chronic course (1). In America, 27.3% of adults reported insomnia 1 year, and the US annual loss of quality-adjusted life-years associated with insomnia (5.6 million) was significantly larger than that associated with any of the other 18 medical conditions assessed, including arthritis (4.94 million), depression (4.02 million), and hypertension (3.63 million) (2). The economic consequences of the disorder and the cost-effectiveness of insomnia treatments, in aggregate, exceeded $100 billion per year, with the majority being spent on indirect costs such as poorer workplace performance, increased health care utilization, and increased accident risk (3). Insomnia has been a public health issue and an extensive concern for medical practitioners. The number of insomnia-associated studies has gradually increased annually, of which 27,399 were published accumulatively in Web of Science (WoS) Core Collection from 1985 to 2021.
With a trend of research interest and explosive publication, it is worth identifying the most influential scientific achievements from an abundance of literature on insomnia related topics. So far, there is no perfect method for evaluating the scientific impact that a specific study has had on a scientific discipline, the number of citations of an article is a proxy to indicate the importance of the study (4). Bibliometric sciences offer both a statistical and quantitative analysis of published articles and provide a measure of their impact in a particular field of research. To date, no such analyses have been performed exploring the most influential works presented in the field of insomnia. In the present study, we aimed to analyze the top 100 most cited articles over the past decades in the field of insomnia with bibliometric citation analysis.
Methods
Identification of the top 100 cited articles
The Clarivate Analytics Web of Science Core Collection database was systematically searched on March 31, 2022. The search terms were “insomnia” and “disorders of initiating and maintaining Sleep,” with publication timespan (1985–2022). The publications were ranked by the number of citations, and these were reviewed to identify the top 100 papers with the most citations. Only original articles and reviews with full manuscripts that focused on insomnia as the main topic were included. Literature reviews that briefly summarized published studies were excluded; editorials and consensus statements were excluded. Two reviewers (SL and JJ) independently identified the top 100 papers according to the total citations of the papers, and any disagreement between the 2 reviewers was resolved by consensus involving a third reviewer (XM).
Analysis of the top 100 cited articles
Publications were stratified and systematically assessed according to publication year, country or institute, authors, and journal. Additionally, the frequencies of keywords extracted from the articles were assessed and then included in a network analysis of the development of insomnia.
All data were downloaded from the Web of Science and imported into the bibliometric package (Version 3.0.0) in R software (Version 4.1.3) (5), which converts and analyses automatically, including the distribution of countries/regions, years of publication, and authors. Publication quality by author was assessed based upon metrics that included the number of publications, citations in the research area, publication h-index value. The h-index is used to quantify an individual’s scientific research output and measure his citation impact (6).
Networks were constructed using VOS viewer v.1.6.18 (7) (Centre for Science and Technology Studies, Leiden University, Leiden, The Netherlands), which is commonly used to analyze and visualize relationships among authors, countries, co-citations, keywords, and the terms used in articles.
The Shapiro–Wilk test was applied to test the normality of the distribution of individual variables. We show the mean and standard deviation for data with a regularly distributed distribution and the median and range for data with a skewed distribution. The Tukey method was also employed for plotting the whiskers and outliers. The p-values from pairwise t-tests were adjusted according to either the Bonferroni post-hoc test or Mann–Whitney test to correct for the performance of multiple statistical analyses. All p-values were two-tailed, and a p-value of ≤0.05 was considered to indicate statistical significance. We used a one-way analysis of Kruskal–Wallis test for skewed data. The Mann–Kendall rank correlation was employed to test for correlations among non-parametric variables.
Results
Global trends of annual publication
A total of 44,654 eligible publications were listed in peer-reviewed journals on the ISI Web of Knowledge WoS Core on 31 March 2022. Manuscripts were screened according to inclusion and exclusion criteria and ranked according to citation frequency. The top 100 influential manuscripts were obtained. General information is detailed in Table 1.
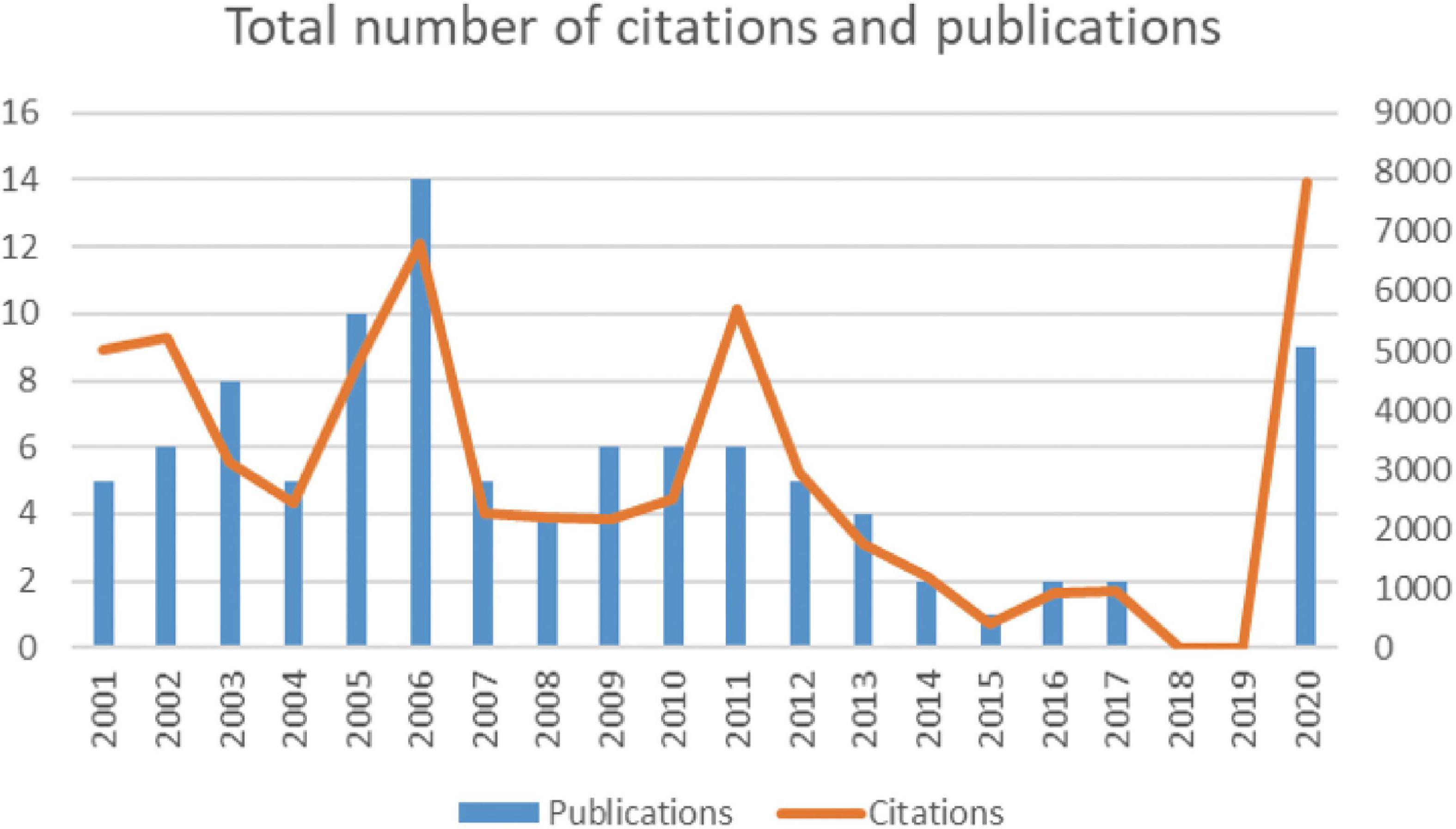
Over the course of 20 years, the total number of citations for the top 100 works of literature varied, but reached a peak in 2021 (Figure 1). The total citation frequency of the top 100 highly cited literature was 58,229 (ranging from 270 to 3,384), with a mean citation frequency of 582.29 and a median citation frequency of 427.5. To exclude the effect of year on citation volume, we analyzed the average annual citation rate of the 100 documents, the highest of which was “Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019” by Lai et al. (8) (average annual citation rate of 893.33; Table 1).
Most articles on the list were published from 2005 to 2006 (n = 24), followed by articles published from 2020 (n = 9; Figure 2A). The number of citations was high for articles published between 2001 and 2012 (mean total citations = 3762) and decreased for articles published after 2012, but reached a peak in 20 years for articles published in 2020 (citations = 7852; Figure 2B). The total citation rate of an article was not related to the date of publication (r = 0.07108, p > 0.05, Mann–Kendall test; Figure 3A). However, the current citation rate of an article (as measured by the number of citations in 2021) suggests that articles published after 2011 are more likely to have been cited in recent years. This correlation was statistically significant (r = 0.5394, p < 0.0001, Mann–Kendall test: Figure 3B).

Figure 2. (A) The total number of publications for each type of article (clinical or review article) according to publication year. (B) The total number of citations publications for each type of article (clinical or review article) according to publication year. (C) Bar graph showing the number of citations (and standard deviation) for the 100 most-cited articles according to type of article (clinical research, review article). Box: lower linee= Box: lower linee number of= Box: lower linee number of citati= median value, white points = outliers. The Tukey method was used for plotting the whiskers and outliers. *Outlier.
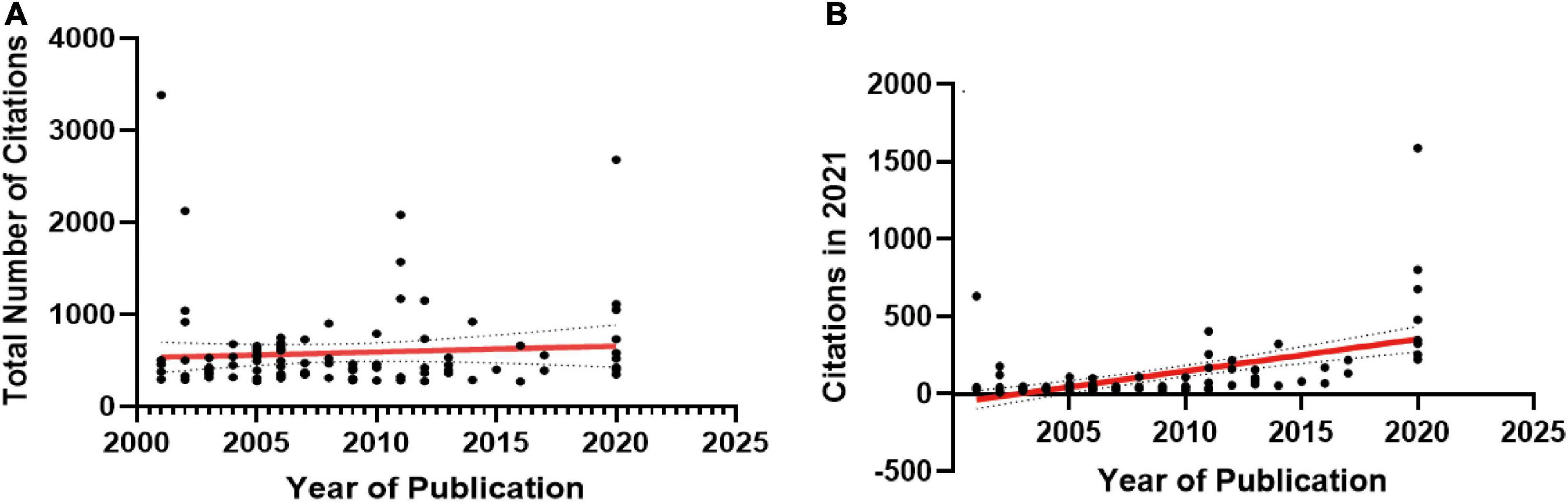
Figure 3. (A) Overall citation rate since publication, and (B) current (2021 = last full year) citation rate for the 100 most-cited articles according to the publication date of the article.
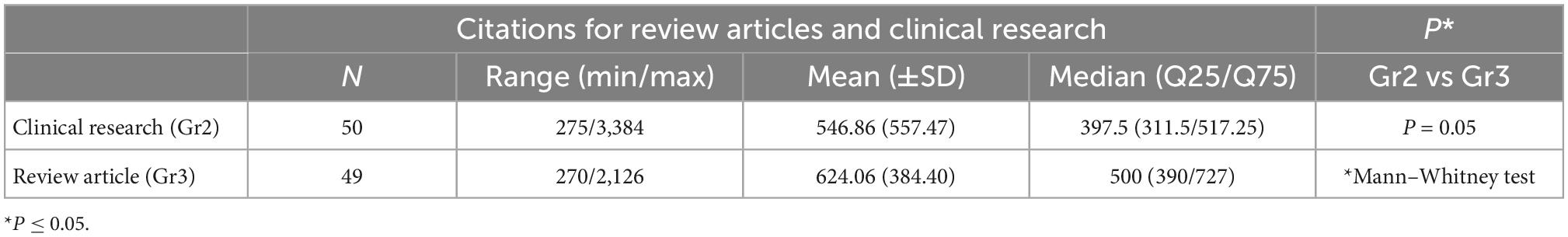
Of the 100 articles, 50 were clinical research, 49 were review articles and 1 was basic research. Due to the small sample size of the basic research, we analyzed the number of citations for review articles and clinical research (Table 2) and found that the review articles did not vary significantly with respect to total citations per article compared to the clinical research articles [Mann–Whitney test, p = 0.08; clinical research: median = 397.5 (range = 275–3384); review articles: median = 531(range = 270–2126): Figure 2C].
Distribution of countries and institutes
The global contribution of insomnia research was analyzed and represented by a blue-coded world map in the R software (Figure 4A). Of the 35 countries and territories identified for this study, the USA had the highest number of articles (n = 56), followed by Canada (n = 22), Germany (n = 11), Italy (n = 10) and the UK (n = 7) (Figure 4B). Studies from the USA were the most cited (24,423 citations), followed by Canada (11,832 citations), Germany (6,329 citations), China (5,587 citations) and the UK (3,097 citations) (Figure 4C).
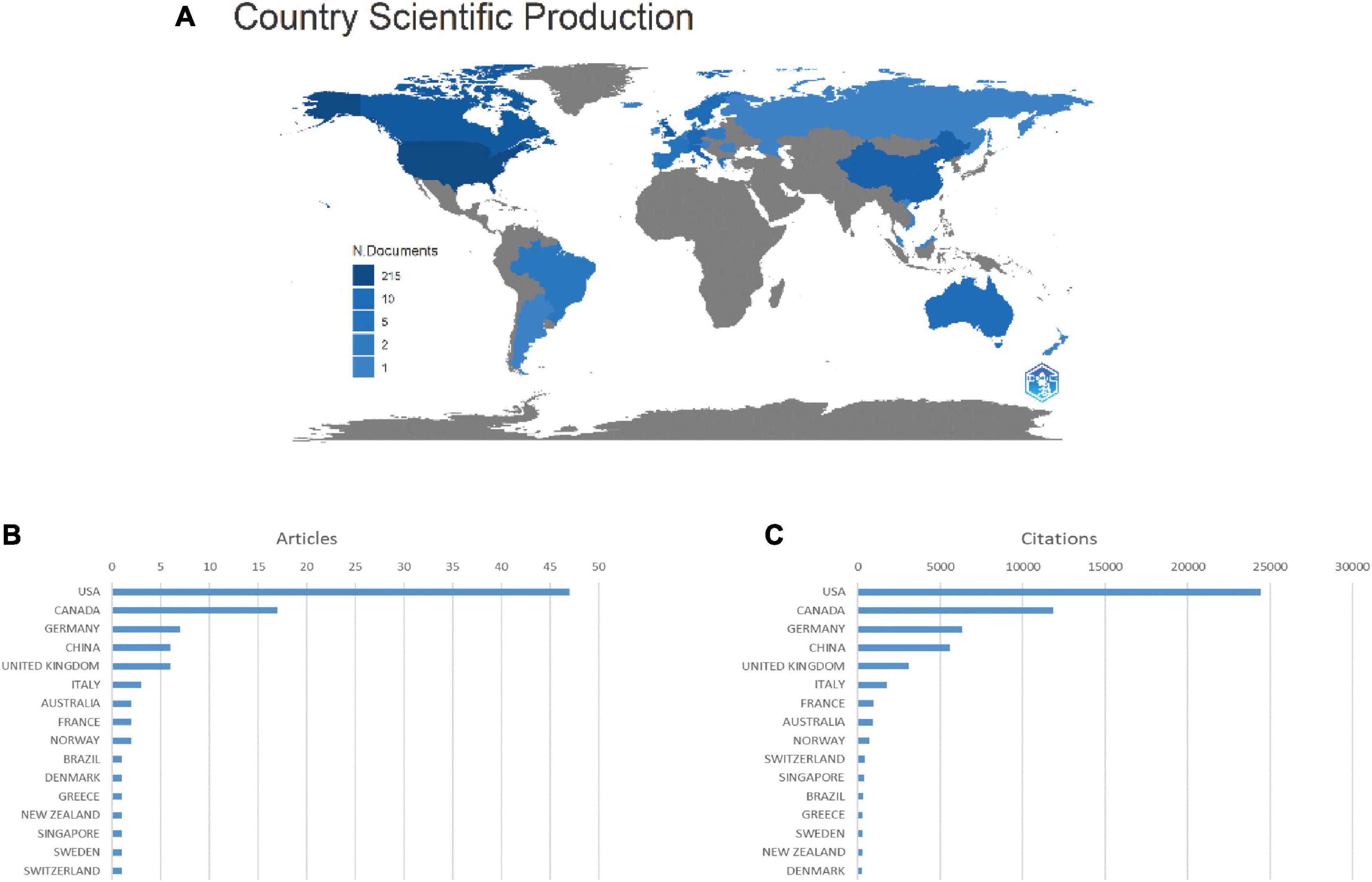
Figure 4. Countries contributing to insomnia research. (A) World map showing the distribution of countries in this field. (B) Top 15 countries with the largest number of publications. (C) Total citations of related articles from different countries.
In the co-authorship analysis, a total of eight countries with more than five publications in the field were analyzed (Figure 5A). The five countries with the highest total connection intensity were the United States (total link strength = 19 times), Germany (17 times) and Canada (15 times). A total of 235 institutions are involved in this field. Laval University (38 articles) contributed the most publications, followed by Harvard University (11 articles), Stanford University (10 articles), University of Pittsburgh (10 articles), and Duke University (9 articles). We analyzed the co-authorship of 235 institutions with more than five publications. Eight institutional collaborations are shown (Figure 5B). The strongest institutions overall were Duke University (total link strength = 14 times).
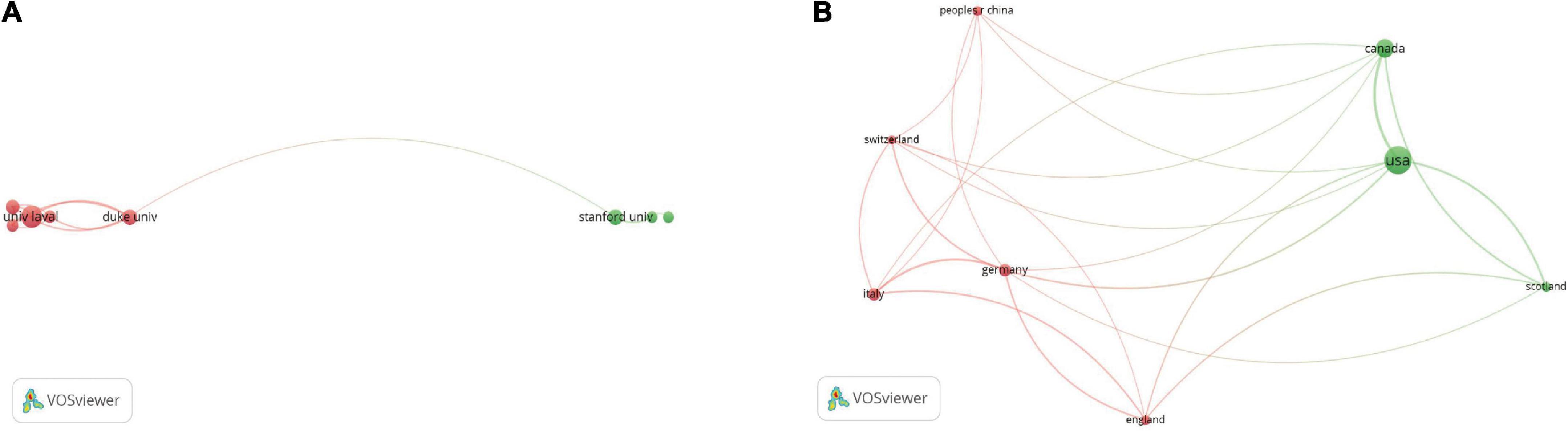
Figure 5. Co-authorship analysis of countries and institutions. (A) Network map of co-authorship between countries with more than five publications. (B) Network map of co-authorship between institutions with more than five publications. The thickness of the lines indicates the strength of the relationship.
Analysis of author
Considering the number of publications, MORIN CM. is the most productive author, with 17 articles (Figure 6A) MORIN CM. was also the top-ranked author in terms of citations in this field (108 citations) (Figure 6B).
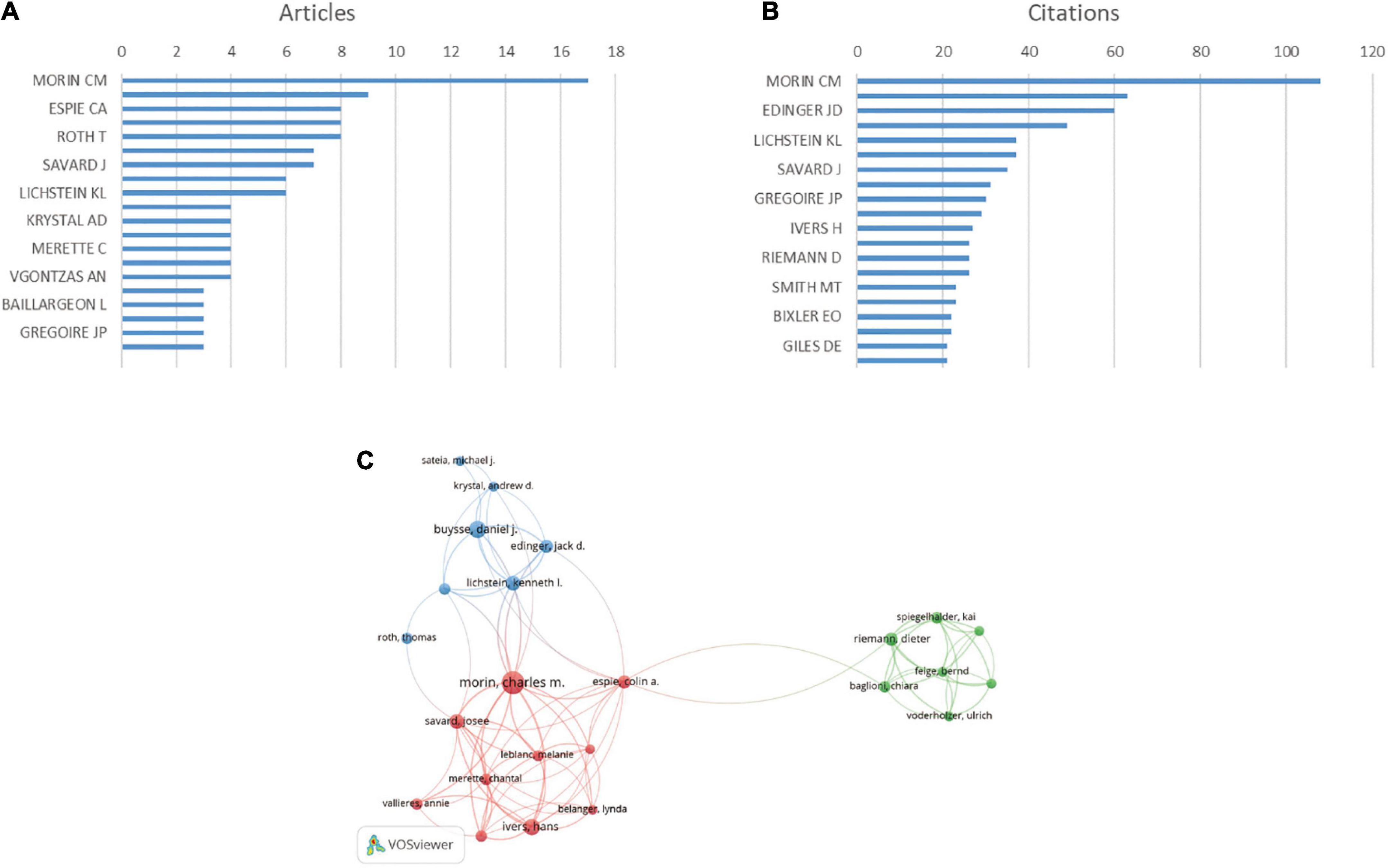
Figure 6. Analysis of authors. (A) Number of publications from different authors. (B) Total citations in the research filed from different authors. (C) Network map of co-authorship between authors with more than five publications. Size of the circles indicate the number of articles in the 100 most cited list, while the width of the curved line represents the link strength. The distance between two authors indicates approximate relatedness among the nodes.
We analyzed a total of 481 authors, 60 of whom were co-authors in more than two publications. Excluding 36 unrelated items, 24 authors were shown to have collaborated (Figure 6C). The author with the highest total linkage intensity was MORIN CM. (total link strength = 40 times).
Analysis of most cited journal
The 100 articles were published in 42 journals. Figure 7 shows the top ten h-index and cited journals that published related articles (Figures 7A, B). Of these 42 journals, the highest h-index was Sleep (h-index = 31), followed closely by Sleep Medicine Reviews (h-index = 9). Sleep was cited the most (928 times), followed by Sleep Medicine Reviews (193 times). In the co-citation analysis, we analyzed a total of 1,352 journals, and a total of 52 journals were cited more than 20 times (Figure 7C).
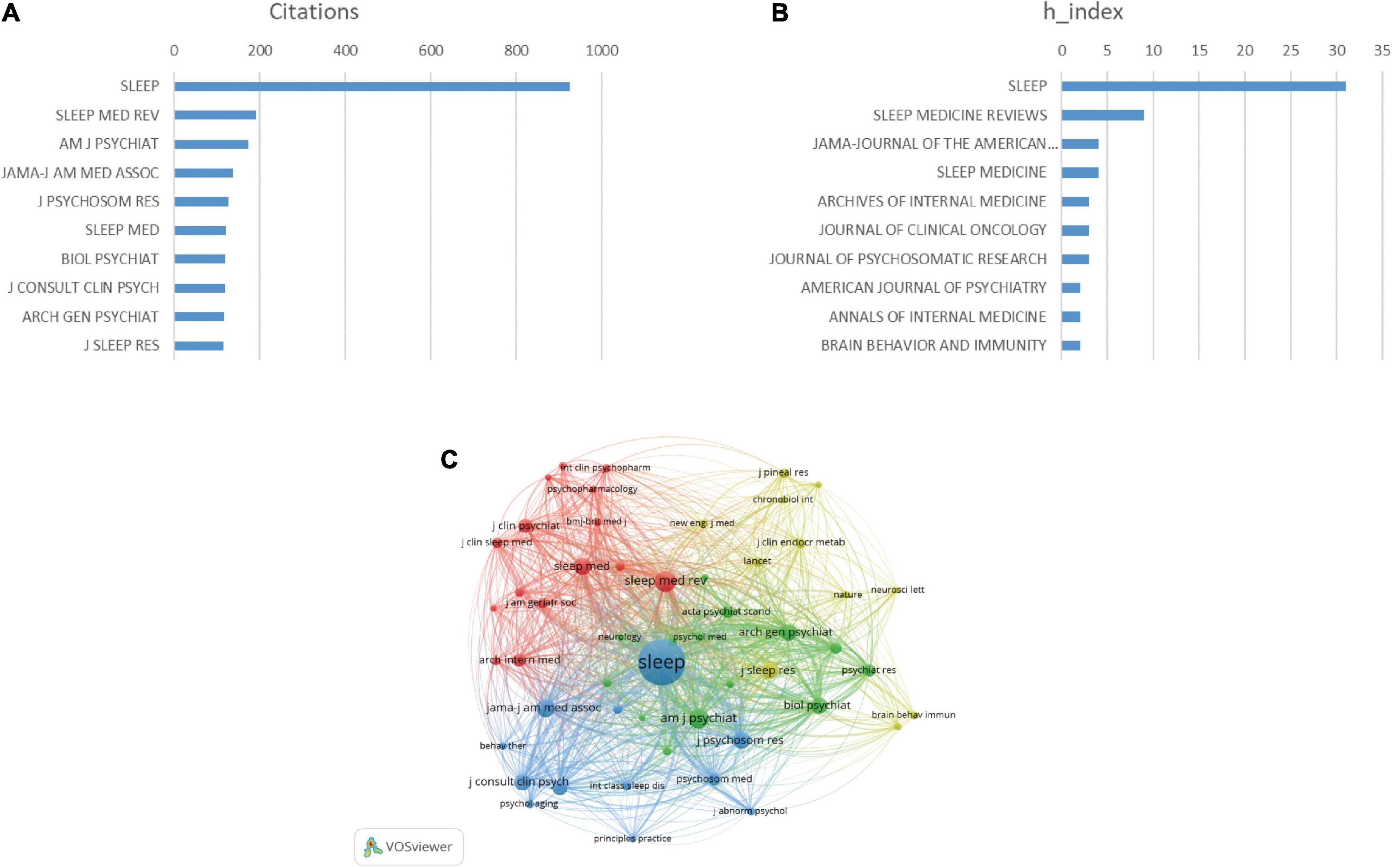
Figure 7. Analysis of journals. (A) Total citations in the research filed from different journals. (B) h-index of publications from different journals. (C) Network map of journals that were co-cited in more than 50 publications. The size of the circle represents the number of papers in the top 100 list.
Co-occurrence analysis of keywords
We analyzed a total of 33 keywords that were identified as appearing more than five times (Figure 8A). The colors in the overlay visualization shown in Figure 8B indicate the average year of publication of the identified keywords. The keywords which published after 2011 are colored more green or yellow. The density visualization shows the same identified keywords mapped by frequency of occurrence (Figure 8C).
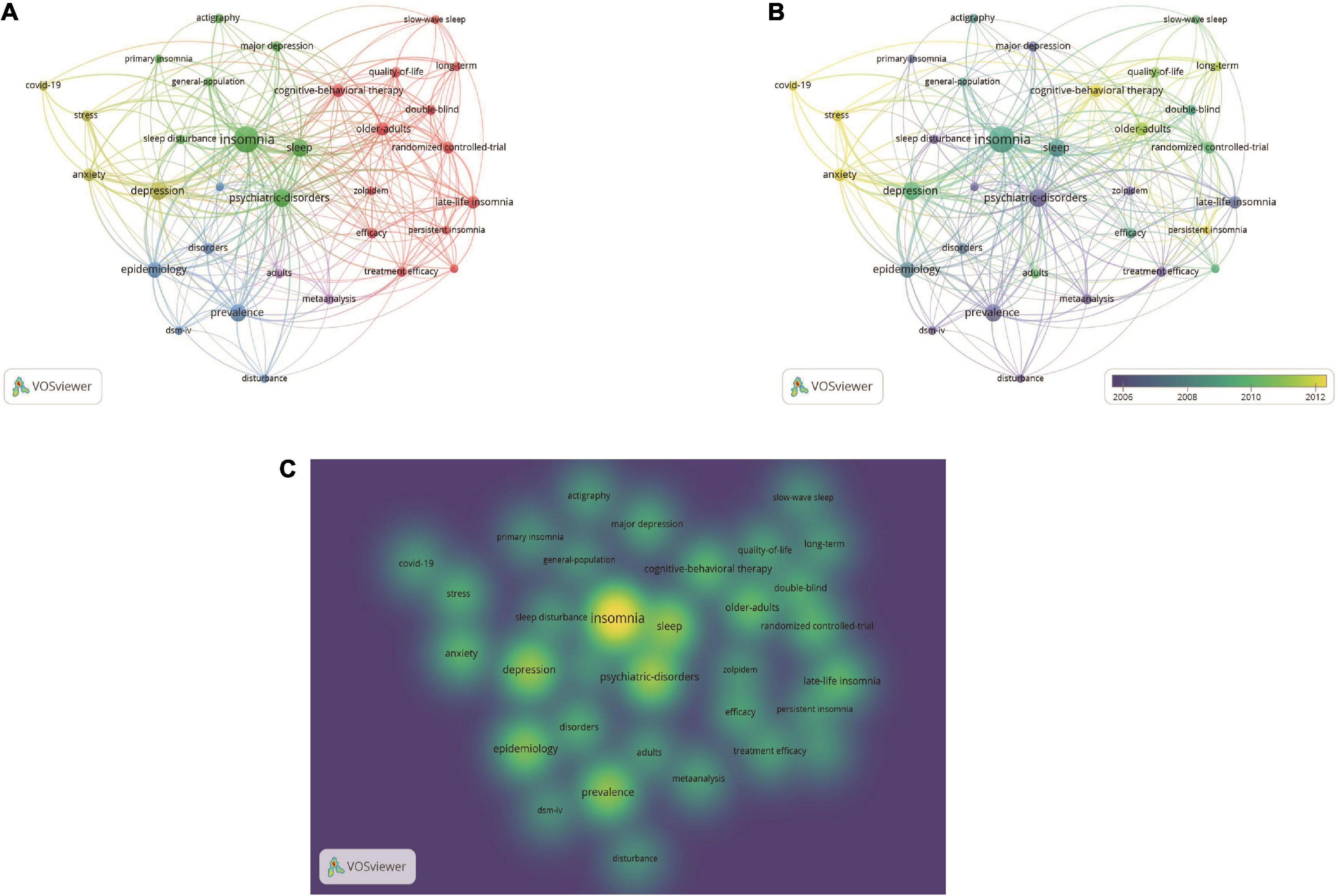
Figure 8. Co-occurrence analysis of keywords. (A) Mapping of keywords of studies. (B) Distribution of keywords according to average publication year (blue: earlier, yellow: later). (C) Distribution of keywords according to the mean frequency of appearance. Keywords in yellow occurred with the highest frequency.
Citation and co-citation analyses
The citation analysis showed 94 pieces of literature with more than 50 citations (Figure 9A). As shown in Table 1, “Validation of the Insomnia Severity Index as an outcome measure for insomnia research” [Bastien et al. (8)] was cited 3,384 times, followed by “Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019” [Lai et al. (8)] with 2,680 citations and the third most cited is “Epidemiology of insomnia: what we know and what we still need to learn” [Ohayon (10)], with 2,126 citations.
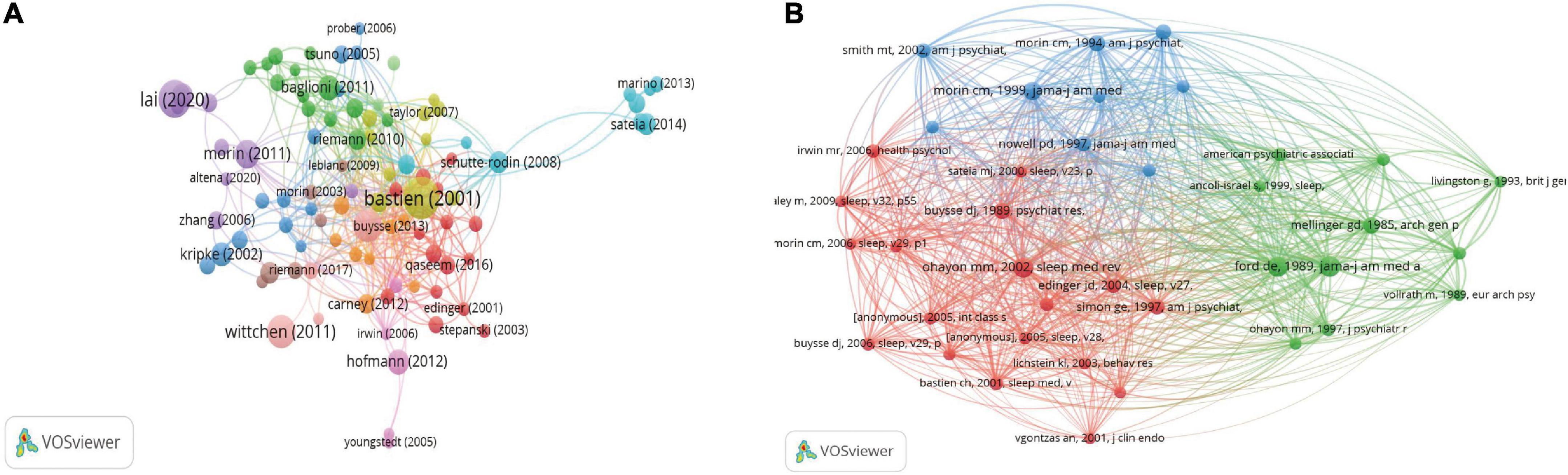
Figure 9. (A) Network map of citation analysis of documents with more than 50 citations. (B) Network map of co-citation analysis of references with more than 10 citations. The size of the circle represents the number of papers in the top 100 list.
We analyzed 38 references that were co-cited more than 10 times in total (Figure 9B). The three most cited references were Ford de. (107) (1989, JAMA-J AM MED ASSOC; 33 citations), Ohayon (10) mm. (2002, sleep med rev; 30 citations), and Breslau (108) (1996, bio psychiat; 29 citations).
Discussion
General trends in insomnia research
Bibliometrics allows for quantitative analysis of a researcher’s individual achievements, or even a country’s or institution’s contribution and international impact in the field, through a statistical analysis of the total number of academic papers published in a clinical field and the total frequency of citations (109). In this study, we combined bibliometric analysis with network visualization to identify the initial 100 most influential manuscripts in the field of insomnia based on global citation frequency, highlighting the contributions that have led to significant advances in insomnia research and pointing to current trends in the field.
With the largest number of publications and citations, and the highest co-authorship analysis ranking by country, the United States is currently the world leader in insomnia research. These results suggest that the US is likely to have a major impact on the direction of research in the field and has the strongest collaboration globally. The citations of articles from Canada, Germany, Italy and the UK have also increased significantly over the last three decades. China has a small total number of publications, but ranks fourth in total citations; it ranks sixth in collaborations with other countries, indicating that China has an influential publication in the field of insomnia and actively maintains close collaborations with other countries. The Laval University Institute is the most productive, with 38% of the publications, while Duke University ranks first in the co-authorship analysis, indicating its close cooperation with other institutes.
Influential authors and studies in insomnia
Morin, C.M. has the largest number of publications and citations and also ranks first in co-authorship analysis conducted by authors. Of these top 100 highly cited publications, Morin C.M. has published 17 articles, 8 of which he is the first author. Dr. Morin is interested in the validation of assessment scale for insomnia. Utilizing scales to evaluate the therapeutic effects of insomnia is the most convenient and widely used method, and the reliability and validity analysis results are critical for the scale to be used as an outcome indicator. Dr. Morin examined psychometric indices of the Insomnia Severity Index to evaluate treatment response in a clinical sample (9), and validated the Dysfunctional beliefs and attitudes about sleep, providing a variety of indicators for the assessment of insomnia (10). Nevertheless, the original version of the ISI and the PSQI are the most commonly used, and the original version of the ISI remains the only validated scale that is highly recommended for all insomnia research protocols. Dr. Morin has also conducted extensive research on cognitive behavioral therapy for insomnia and its comorbidities (110, 111). His team’s current efforts continue to focus on evaluating the efficacy of cognitive behavioral therapy and optimizing the procedural approach (112, 113).
According to the literature citation analysis and reference co-citation analysis, the most frequently cited Bastien et al. (8) reported clinical validation of the Insomnia Severity Index Scale (ISI) as a brief screening indicator for insomnia and an outcome indicator for treatment studies, indicating that the ISI is a reliable and valid tool for quantifying perceived insomnia severity. The ISI is a brief self-report instrument designed to assess subjective symptoms and daytime status of insomnia and the extent to which insomnia causes worry or distress. The ISI has been continually validated and the study by Bastien et al. was the first formal psychometric analysis of the reliability and validity of the ISI. Further validation of the ISI using item response theory (IRT) analysis was reported by Morin et al. (114), obtaining evidence on internal consistency, item response patterns and convergent validity, yielding new evidence on optimal sensitivity and specificity indices for case finding and assessment of minimal important changes following treatment (12). A recent meta-analysis (115) reported on the construct validity of the Insomnia Severity Index (ISI), which showed that studies reporting validated factor analyses (CFA) had more reliable results than those reporting only exploratory factor analyses (EFA), and that two-factor solution were strong expressions of dimensionality and higher reliability indicators for the ISI compared to three-factor solutions.
Future outlook
Our co-occurrence network diagram, categorized by subject area or date of publication, shows current hotspots and future directions in insomnia research (Figures 8A–C). The keywords indicate that insomnia research involves a wide range of populations (elderly, adolescents), causal factors (quality of life, coronavirus), disorders (anxiety disorders, depression) and therapies (cognitive behavioral therapy, pharmacotherapy). The most recent keywords indicating future trends in the field are as follows:
COVID-19 and insomnia
The total number of citations in the insomnia-related literature rose significantly in 2021, reaching a peak in the last 20 years. This may be related to the outbreak of the Corona Virus Disease 2019 (COVID-19). The impact of the new coronavirus pneumonia outbreak has led to an increase in psychological disorders in the population and a climb in the prevalence of insomnia, with 36.7% of adults from 13 countries having clinical symptoms of insomnia and 17.4% meeting diagnostic criteria for insomnia (24, 114). Spielman identified negative life events and other stressors as triggers for the development of insomnia (116), with up to 37% of the population experiencing insomnia in the presence of stressful events (117). During the early stage of the COVID-19 pandemic, insomnia symptoms were mainly associated with acute psychological reactions due to the rapid spread of the disease and strict enforcement of restrictions, as well as poor sleep hygiene (118). During the late stage, insomnia symptoms are associated with economic stress associated with the COVID-19 pandemic (118) and the impairment of sleep patterns (119). Recent studies have shown that into the late stages, sleep is characterized by significant objective sleep fragmentation in the presence of adequate sleep duration (120), suggesting that the adverse effects of the initial pandemic outbreak on sleep will persist. Studies of insomnia during the COVID-19 pandemic highlight the importance of focusing not only on the primary diseases, but also on the psycho-psychological issues, particularly insomnia during global public health events.
Depression, anxiety, and insomnia
In our analysis of keywords, we found that “anxiety,” “depression,” and “mental disorders” were frequently mentioned in 100 documents as the second most frequently occurring keywords after “insomnia.” Studies have shown that there is a strong relationship between insomnia, depression and anxiety, with insomnia considered a risk factor for anxiety and depression (121), with those suffering from insomnia 9.82 times more likely to have clinically significant depression and 17.35 times more likely to have clinically significant anxiety compared to those without insomnia (38). Anxiety and depression are also considered risk factors for insomnia (122), suggesting that insomnia is bilaterally associated with psychiatric disorders such as anxiety and depression (41). In terms of biological mechanisms, polymorphisms and dysregulation of the serotonin, dopamine(DA), oxytocin (OXT) and genes may be associated with the development and maintenance of insomnia and mood disorders (123), while behavior and thoughts can in turn affect the activity of the serotonin, DA, OXT, and genes (124). In terms of brain function, sleep disturbances have been shown to disrupt the function of cortical neural circuits, including the amygdala, striatum, anterior cingulate cortex and prefrontal cortex (PFC) (125), which play a key role in the regulation of the affective system (126). In addition, there is growing evidence that insomnia disrupts brain functions associated with the reward system (127, 128), and that dysfunction of the reward system is associated with a variety of neuropsychiatric disorders (129), including depression, bipolar disorder (127, 128, 130) and others.
Subtypes of insomnia
Insomnia is a heterogeneous disorder (131), and identifying clinically relevant subtypes of insomnia disorders can help reduce heterogeneity, identify etiology, and personalize treatment (132). In Ohayon (10) proposed that epidemiological studies should focus on distinguishing different subtypes of insomnia. Typing by sleep stage symptoms, such as difficulty falling asleep (DIS), difficulty maintaining sleep (DMS), early awakening (EMA), or a combination of four subtypes (133); typing by insomnia episodes and duration, such as chronic insomnia, short-term insomnia (134); and typing by primary and secondary clinical features of insomnia, such as primary insomnia, secondary insomnia (135). Although these subtypes can differ in terms of stable sleep-related characteristics, reliability and validity are lacking and heterogeneity still prevails (136). It remains difficult to find consistent insomnia features in terms of cognition, mood, personality, life history, polysomnography, and sleep microstructure, and this inconsistency suggests that different subtypes of insomnia disorder have not been fully identified (137). For a long time, researchers have been working on different aspects of the subtypes of insomnia disorders, such as natural history of insomnia (94), subjective and objective sleep duration (74), sleep microstructure (138), non-insomnia characteristics (life history, affective and personality traits) (137), and clustering subtypes of insomnia (subtyping based on subjective sleep variables as well as age at onset of insomnia, the severity of anxiety and depressive symptoms) (139). Vgontzas et al. (74) proposed that insomnia with short objective sleep duration is the most biologically severe phenotype of the disorder and is associated with a higher risk for hypertension, diabetes, and other diseases. Also, it appears that insomnia with objective short sleep duration is a biological marker of genetic predisposition to chronic insomnia. In the future, the underlying genetic, neurobiological, and neuropsychological mechanisms of insomnia with objective short sleep duration could be further explored. In terms of polysomnography (140), brain imaging (141), and genetics (142), we can also examine the association of other sleep variables with other phenotypes of insomnia.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is the most widely researched form of psychotherapy, which leads to changes in emotional distress and problem behavior by altering therapeutic strategies that are maladaptive to poor cognition (14). CBT for insomnia (CBT-I) has long been shown to be more effective than control therapy (143). Cognitive behavioral therapy for insomnia (CBT-I) is now commonly recommended as a first-line treatment for chronic insomnia because of the potential for sustained benefit from psychotherapy without the risk of tolerance or adverse effects associated with pharmacological approaches (65). Recent evidence suggests that CBTI can also be used to treat acute insomnia caused by stress (144). Many elements of this treatment approach can be applied to stressful events such as the current COVID-19 pandemic and can be adapted to treat and prevent sleep problems resulting from confinement, increased stress and changes in circadian and daily activities (78). The development of technologies such as the Internet, big data and artificial intelligence has brought about a boom in digital medicine in the healthcare industry, enabling the digitization of CBT-I (145), and the effectiveness of digital cognitive behavioral therapy (dBT-I) for insomnia has been validated (146). In recent years, dBT-I has been widely used during the COVID-19 pandemic, and Liu et al’s (147) study provides an entry point for building a dBTI platform and a theoretical basis for clinical application.
Sleep microstructure
In recent years, sleep microstructure has gradually gained widespread attention, and a number of the 100 articles we examined have begun to focus on slow-wave sleep. Slow wave sleep (SWS) is a component of non-REM sleep that is important in neurophysiological processes like memory and cognition (148). According to the “active system consolidation hypothesis,” slow oscillations, in conjunction with sleep spindle waves, drive the repetitive reactivation of newly encoded memories during slow-wave sleep, facilitating their integration into long-term memory storage sites (149). A growing body of research confirms that auditory stimulation (150), transcranial direct current stimulation (151), and medication (152) are all effective in improving memory function by enhancing slow waves of sleep (153). Slow-wave sleep is not only used for memory enhancement, but has also been widely used to improve cognitive function in patients with mental illness (154, 155) and for sensory-motor recovery in stroke patients (156). Recent studies have shown that enhancing SWS in healthy individuals profoundly affects the connections between the endocrine and autonomic nervous systems (157), opening up a wide range of potential applications for enhancing SWS.
Strengths and limitations
To the best of our knowledge, this is the first bibliometric analysis of the Insomnia research trend. Using the R bibliometric package, we conducted a comprehensive survey of the literature to perform quantitative and qualitative analyses of the publication output and quality of studies from various authors. We also used a well-known scientometric software tool (VOSviewer) to build and visualize the bibliometric networks by analyzing co-authorship, co-citation, and co-occurrence. Nevertheless, our analyses have some limitations. Firstly, the search is primarily conducted in the WoS database. Although WoS is the most commonly used database in scientometrics, it is advisable to combine the results with those from other databases, such as PubMed and Scopus. Secondly, our search did not separate mechanistic studies from clinical studies, ignoring the research progress in mechanistic studies; however, this could also indicate that mechanistic studies in the field of sleep could be strengthened. Third, the keyword analysis results may have been influenced by incomplete keyword extraction. To better display the keywords, keywords that appeared more than five times in the network were shown. Fourthly, as this is a developing area of research, we may have overlooked the contribution of analyzing recently published studies because of their low citation frequency, despite some studies being published in high quality journals.
Conclusion
In conclusion, to our knowledge, this is the first bibliometric study to identify the 100 most cited papers in insomnia research. Our results suggest that the outbreak of the COVID-19 epidemic is strongly associated with the onset of insomnia and stimulates the researcher’s interest. The key words suggest “COVID-19;” “anxiety,” “depression,” “CBT,” and “sleep microstructure” are currently hot topics in the field of insomnia and will be future research trends in the field, indicating that the focus of research has shifted from insomnia epidemiology and scale validation to the study of co-morbidities and sleep microstructure of insomnia. Despite its limitations, citation analysis provides an important quantitative approach to research in the field of comparative science. The findings of this study may provide a valuable reference for researchers to guide and implement their scientific research interests in the field of insomnia.
Author contributions
QW, KL, and WW designed the study. QW and KL wrote and revised the draft manuscript and carried out data visualization and graphical interpretation. QW, KL, SL, JJ, and XW performed the literature search, retrieval, and data collection. WW provided the critical assistance or funding. All authors contributed and approved the final draft of the manuscript before submission.
Funding
This work was supported by the National Natural Science Foundation of China (grant number: 82274631) and Jiangsu Provincial Department of Science and Technology (grant number: BE2021751).
Acknowledgments
We acknowledge the support of the Team of the Insomnia Research Team of Jiangsu Province Hospital of Chinese Medicine, Affiliated Hospital of Nanjing University of Chinese Medicine.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Olfson M, Wall M, Liu S, Morin C, Blanco C. Insomnia and impaired quality of life in the United States. J Clin Psychiatry. (2018) 79:17m12020. doi: 10.4088/JCP.17m12020
3. Wickwire E, Shaya F, Scharf S. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. (2016) 30:72–82. doi: 10.1016/j.smrv.2015.11.004
4. Landreneau J, Weaver M, Delaney C, Aminian A, Dimick J, Lillemoe K, et al. The 100 most cited papers in the history of the American surgical association. Ann Surg. (2020) 271:663–70. doi: 10.1097/SLA.0000000000003633
5. Hirsch JE. An index to quantify an individual’s scientific research output. Proc Natl Acad Sci USA. (2005) 102:16569–72. doi: 10.1073/pnas.0507655102
6. Aria M, Cuccurullo C. bibliometric: an R-tool for comprehensive science mapping analysis. J Informetr. (2018) 11:959–75. doi: 10.1016/j.joi.2017.08.007
7. van Eck N, Waltman L. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics. (2017) 111:1053–70. doi: 10.1007/s11192-017-2300-7
8. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
9. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
10. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
11. Wittchen H, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. (2011) 21:655–79. doi: 10.1016/j.euroneuro.2011.07.018
12. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
13. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
14. Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cogn Ther Res. (2012) 36:427–40. doi: 10.1007/s10608-012-9476-1
15. Pappa S, Ntella V, Giannakas T, Giannakoulis V, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
16. Torales J, O’Higgins M, Castaldelli-Maia J, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
17. Kripke D, Garfinkel L, Wingard D, Klauber M, Marler M. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. (2002) 59:131–6. doi: 10.1001/archpsyc.59.2.131
18. Sateia M. International classification of sleep disorders-third edition highlights and modifications. Chest. (2014) 146:1387–94. doi: 10.1378/chest.14-0970
19. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh sleep quality index in primary insomnia. J Psychosom Res. (2002) 53:737–40. doi: 10.1016/S0022-3999(02)00330-6
20. Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. (2008) 4:487–504. doi: 10.5664/jcsm.27286
21. Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. (2010) 14:19–31. doi: 10.1016/j.smrv.2009.04.002
22. Morin C, Bootzin R, Buysse D, Edinger J, Espie C, Lichstein K. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998-2004). Sleep. (2006) 29:1398–414. doi: 10.1093/sleep/29.11.1398
23. Carney C, Buysse D, Ancoli-Israel S, Edinger J, Krystal A, Lichstein K, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. (2012) 5:287–302. doi: 10.5665/sleep.1642
24. Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. doi: 10.1016/S2215-0366(20)30203-0
25. Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. (2007) 30:519–29. doi: 10.1093/sleep/30.4.519
26. Buysse D, Ancoli-Israel S, Edinger J, Lichstein K, Morin C. Recommendations for a standard research assessment of insomnia. Sleep. (2006) 29:1155–73. doi: 10.1093/sleep/29.9.1155
27. Edinger J, Bonnet M, Bootzin R, Doghramji K, Dorsey C, Espie C, et al. Derivation of research diagnostic criteria for insomnia: report of an american academy of sleep medicine work group. Sleep. (2004) 27:1567–96. doi: 10.1093/sleep/27.8.1567
28. Qaseem A, Kansagara D, Forciea M, Cooke M, Denberg T. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American college of physicians. Ann Intern Med. (2016) 165:125–33. doi: 10.7326/M15-2175
29. Littner M, Kushida C, Wise M, Davila D, Morgenthaler T, Lee-Chiong T, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test–an American academy of sleep medicine report–standards of practice committee of the american academy of sleep medicine. Sleep. (2005) 28:113–21. doi: 10.1093/sleep/28.1.113
30. Morin C, LeBlanc M, Daley M, Gregoire J, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. doi: 10.1016/j.sleep.2005.08.008
31. Glass J, Lanctôt K, Herrmann N, Sproule B, Busto U. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. (2005) 331:1169. doi: 10.1136/bmj.38623.768588.47
32. Pandi-Perumal S, Srinivasan V, Maestroni G, Cardinali D, Poeggeler B, Hardeland R. Melatonin–nature’s most versatile biological signal? FEBS J. (2006) 273:2813–38. doi: 10.1111/j.1742-4658.2006.05322.x
33. Zhang B, Wing Y. Sex differences in insomnia: a meta-analysis. Sleep. (2006) 29:85–93. doi: 10.1093/sleep/29.1.85
34. Gottlieb D, Redline S, Nieto F, Baldwin C, Newman A, Resnick H, et al. Association of usual sleep duration with hypertension: the sleep heart health study. Sleep. (2006) 29:1009–14. doi: 10.1093/sleep/29.8.1009
35. Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. (2005) 66:1254–69. doi: 10.4088/JCP.v66n1008
36. Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in january 2020 in China. Med Sci Monit. (2020) 26:e923921. doi: 10.12659/MSM.923921
37. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis J, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
38. Taylor DJ, Lichstein KL, Durrence HH, Reidel B, Bush A. Epidemiology of insomnia, depression, and anxiety. Sleep. (2005) 28:1457–64. doi: 10.1093/sleep/28.11.1457
39. Tsai P, Wang S, Wang M, Su C, Yang T, Huang C, et al. Psychometric evaluation of the Chinese version of the Pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res. (2005) 14:1943–52. doi: 10.1007/s11136-005-4346-x
40. Smith M, Haythornthwaite J. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. (2004) 8:119–32. doi: 10.1016/S1087-0792(03)00044-3
41. Alvaro P, Roberts R, Harris JKA. Systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
42. Ohayon M, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatry Res. (2003) 37:9–15. doi: 10.1016/S0022-3956(02)00052-3
43. Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
44. Manber R, Edinger J, Gress J, San Pedro-Salcedo M, Kuo T, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. (2008) 31:489–95. doi: 10.1093/sleep/31.4.489
45. Vgontzas A, Bixler E, Lin H, Prolo P, Mastorakos G, Vela-Bueno A, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: Clinical implications. J Clin Endocrinol Metab. (2001) 86:3787–94. doi: 10.1210/jcem.86.8.7778
46. Smith M, Perlis M, Park A, Smith M, Pennington J, Giles D, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. (2002) 159:5–11. doi: 10.1176/appi.ajp.159.1.5
47. Morgenthaler T, Kramer M, Alessi C, Friedman L, Boehlecke B, Brown T, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American academy of sleep medicine report. Sleep. (2006) 29:1415–9. doi: 10.1093/sleep/29.11.1415
48. Buckley T, Schatzberg A. Review: On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. (2005) 90:3106–14. doi: 10.1210/jc.2004-1056
49. Taylor D, Mallory L, Lichstein K, Durrence H, Riedel B, Bush A. Comorbidity of chronic insomnia with medical problems. Sleep. (2007) 30:213–8. doi: 10.1093/sleep/30.2.213
50. Buysse D, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. (2008) 31:473–80. doi: 10.1093/sleep/31.4.473
51. Vgontzas A, Liao D, Bixler E, Chrousos G, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. (2009) 32:491–7. doi: 10.1093/sleep/32.4.491
52. Bonnet M, Arand D. Hyperarousal and insomnia: State of the science. Sleep Medicine Reviews. (2010) 14:9–15. doi: 10.1016/j.smrv.2009.05.002
53. Savard J, Morin C. Insomnia in the context of cancer: a review of a neglected problem. Journal of Clinical Oncology. (2001) 19:895–908. doi: 10.1200/JCO.2001.19.3.895
54. Marino M, Li Y, Rueschman M, Winkelman J, Ellenbogen J, Solet J, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. (2013) 36:1747–55. doi: 10.5665/sleep.3142
55. Drake C, Roehrs T, Richardson G, Walsh J, Roth T. Shift work sleep disorder: Prevalence and consequences beyond that of symptomatic day workers. Sleep. (2004) 27:1453–62. doi: 10.1093/sleep/27.8.1453
56. Johnson E, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J Psychiatr Res. (2006) 40:700–8. doi: 10.1016/j.jpsychires.2006.07.008
57. Nofzinger E, Buysse D, Germain A, Price J, Miewald J, Kupfer D. Functional neuroimaging evidence for hyperarousal in insomnia. Am J Psychiatry. (2004) 161:2126–8. doi: 10.1176/appi.ajp.161.11.2126
58. Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. (2020) 11:790. doi: 10.3389/fpsyt.2020.00790
59. Littner M, Kushida C, Anderson W, Bailey D, Berry R, Davila D, et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002–an American academy of sleep medicine report. Sleep. (2003) 26:337–41. doi: 10.1093/sleep/26.3.337
60. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. (2010) 14:227–38. doi: 10.1016/j.smrv.2009.10.007
61. Morin C, Benca R. Chronic insomnia. Lancet. (2012) 379:1129–41. doi: 10.1016/S0140-6736(11)60750-2
62. Cajochen C, Kräuchi K, Wirz-Justice A. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. (2003) 15:432–7. doi: 10.1046/j.1365-2826.2003.00989.x
63. Morin C, Vallières A, Guay B, Ivers H, Savard J, Mérette C, et al. cognitive behavioral therapy, singly and combined with medication, for persistent insomnia a randomized controlled trial. JAMA. (2009) 301:2005–15. doi: 10.1001/jama.2009.682
64. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
65. Trauer J, Qian M, Doyle J, Rajaratnam S, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. (2015) 163:191–204. doi: 10.7326/M14-2841
66. Morin C, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. (2003) 65:259–67. doi: 10.1097/01.PSY.0000030391.09558.A3
67. Daley M, Morin C, LeBlanc M, Grégoire J, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. (2009) 32:55–64.
68. Sateia M, Buysse D, Krystal A, Neubauer D, Heald J. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med. (2017) 13:307–49. doi: 10.5664/jcsm.6470
69. National Institutes of Health. National institutes of health state of the science conference statement–manifestations and management of chronic insomnia in adults June 13-15, 2005. Sleep. (2005) 28:1049–57. doi: 10.1093/sleep/28.9.1049
70. Edinger J, Wohlgemuth W, Radtke R, Marsh G, Quillian R. Cognitive behavioral therapy for treatment of chronic primary insomnia–a randomized controlled trial. JAMA. (2001) 285:1856–64. doi: 10.1001/jama.285.14.1856
71. Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord. (2003) 76:255–9. doi: 10.1016/S0165-0327(02)00072-1
72. Neckelmann D, Mykletun A, Dahl A. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. (2007) 30:873–80. doi: 10.1093/sleep/30.7.873
73. Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin C. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. (2012) 16:83–94. doi: 10.1016/j.smrv.2011.03.008
74. Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. (2013) 17:241–54. doi: 10.1016/j.smrv.2012.09.005
75. Lichstein K, Stone K, Donaldson J, Nau S, Soeffing J, Murray D, et al. Actigraphy validation with insomnia. Sleep. (2006) 29:232–9.
76. Morin CM, Vallières A, Hans I. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16). Sleep. (2011) 30:1547–54. doi: 10.1093/sleep/30.11.1547
77. Stepanski E, Wyatt J. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. (2003) 7:215–25. doi: 10.1053/smrv.2001.0246
78. Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. (2020) 29:e13052. doi: 10.1111/jsr.13052
79. Morphy H, Dunn K, Lewis M, Boardman H, Croft P. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. (2007) 30:274–80.
80. Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik O, Kvale G, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults–a randomized controlled trial. JAMA. (2006) 295:2851–8. doi: 10.1001/jama.295.24.2851
81. Espie C. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. (2002) 53:215–43. doi: 10.1146/annurev.psych.53.100901.135243
82. Johnson E, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. (2006) 117:e247–56. doi: 10.1542/peds.2004-2629
83. Bertolazi A, Fagondes S, Hoff L, Dartora E, Miozzo I, de Barba M, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. (2011) 12:70–5. doi: 10.1016/j.sleep.2010.04.020
84. Irwin M, Cole J, Nicassio P. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+years of age. Health Psychol. (2006) 25:3–14. doi: 10.1037/0278-6133.25.1.3
85. Jacobs G, Pace-Schott E, Stickgold R, Otto M. Cognitive behavior therapy and pharmacotherapy for insomnia– randomized controlled trial and direct comparison. Arch Intern Med. (2004) 164:1888–96. doi: 10.1001/archinte.164.17.1888
86. Soldatos C, Dikeos D, Paparrigopoulos T. The diagnostic validity of the athens insomnia scale. J Psychosom Res. (2003) 55:263–7. doi: 10.1016/S0022-3999(02)00604-9
87. Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. (2008) 64:443–9. doi: 10.1016/j.jpsychores.2007.10.016
88. Krystal A, Walsh J, Laska E, Caron J, Amato D, Wessel T, et al. Sustained efficacy of eszopiclone over 6 months of nightly treatment: results of a randomized, double-blind, placebo-controlled study in adults with chronic insomnia. Sleep. (2003) 26:793–9. doi: 10.1093/sleep/26.7.793
89. Prober D, Rihel J, Onah A, Sung R, Schier A. Hypocretin/orexin overexpression induces an insomnia-like phenotype in zebrafish. J Neurosci. (2006) 26:13400–10. doi: 10.1523/JNEUROSCI.4332-06.2006
90. Savard J, Simard S, Ivers H, Morin C. Randomized study on the efficacy of cognitive-bahavioural therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. J Clin Oncol. (2005) 23:6083–96. doi: 10.1200/JCO.2005.09.548
91. Youngstedt S. Effects of exercise on sleep. Clin Sports Med. (2005) 24:355–65,xi. doi: 10.1016/j.csm.2004.12.003
92. Fava M, McCall W, Krystal A, Wessel T, Rubens R, Caron J, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiatry. (2006) 59:1052–60. doi: 10.1016/j.biopsych.2006.01.016
93. Vgontzas A, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler E. Insomnia with objective short sleep duration is associated with type 2 diabetes a population-based study. Diabetes Care. (2009) 32:1980–5. doi: 10.2337/dc09-0284
94. Morin CM, Bélanger L, LeBlanc M, Ivers H, Savard J, Espie C, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. (2009) 169:447–53. doi: 10.1001/archinternmed.2008.610
95. Perlis M, Smith M, Andrews P, Orff H, Giles D. Beta/gamma EEG activity in patients with primary and secondary insomnia and good sleeper controls. Sleep. (2001) 24:110–7. doi: 10.1093/sleep/24.1.110
96. Leger D, Guilleminault C, Bader G, Lévy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. (2002) 25:625–9. doi: 10.1093/sleep/25.6.621
97. Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini G. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. (2014) 21:57–64. doi: 10.1177/2047487312460020
98. Buysse D, Germain A, Moul D, Franzen P, Brar L, Fletcher M, et al. Efficacy of brief behavioral treatment for chronic insomnia in older adults. Arch Intern Med. (2011) 171:887–95. doi: 10.1001/archinternmed.2010.535
99. LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin C. Incidence and risk factors of insomnia in a population-based sample. Sleep. (2009) 32:1027–37. doi: 10.1093/sleep/32.8.1027
100. Wilson S, Anderson K, Baldwin D, Dijk D, Espie A, Espie C, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J Psychopharmacol. (2010) 33:923–47. doi: 10.1177/0269881119855343
101. Palesh O, Roscoe J, Mustian K, Roth T, Savard J, Ancoli-Israel S, et al. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: university of rochester cancer center-community clinical oncology program. J Clin Oncol. (2010) 28:292–8. doi: 10.1200/JCO.2009.22.5011
102. Kessler R, Berglund P, Coulouvrat C, Hajak G, Roth T, Shahly V, et al. Insomnia and the performance of US workers: results from the America insomnia survey. Sleep. (2011) 34:1161–71. doi: 10.5665/SLEEP.1230
103. Reid K, Baron K, Lu B, Naylor E, Wolfe L, Zee P. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. (2010) 11:934–40. doi: 10.1016/j.sleep.2010.04.014
104. Espie C, Kyle S, Williams C, Ong J, Douglas N, Hames P, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. (2012) 35:769–81. doi: 10.5665/sleep.1872
105. Harrison T, Keating G. Zolpidem–a review of its use in the management of insomnia. CNS Drugs. (2005) 19:65–89. doi: 10.2165/00023210-200519010-00008
106. Zachariae R, Lyby M, Ritterband L, O’Toole M. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia–a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2016) 30:1–10. doi: 10.1016/j.smrv.2015.10.004
107. Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. (1989) 262:1479–84. doi: 10.1001/jama.262.11.1479
108. Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. (1996) 39:411–8. doi: 10.1016/0006-3223(95)00188-3
109. Guo J, Gu D, Zhao T, Zhao Z, Xiong Y, Sun M, et al. Trends in piezo channel research over the past decade: a bibliometric analysis. Front Pharmacol. (2021) 12:668714. doi: 10.3389/fphar.2021.668714
110. Ji X, Ivers H, Beaulieu-Bonneau S, Morin C. Complementary and alternative treatments for insomnia/insomnia -depression-anxiety symptom cluster: meta-analysis of English and Chinese literature. Sleep Med Rev. (2021) 58:101445. doi: 10.1016/j.smrv.2021.101445
111. Selvanathan J, Pham C, Nagappa M, Peng PW, Englesakis M, Espie CA, et al. Cognitive behavioral therapy for insomnia in patients with chronic pain–a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. (2021) 60:101460. doi: 10.1016/j.smrv.2021.101460
112. Lancee J, Harvey AG, Morin CM, Ivers H, Zweerde T v, Blanken TF. Network intervention analyses of cognitive therapy and behavior therapy for insomnia: symptom specific effects and process measures. Behav Res Ther. (2022) 153:104100. doi: 10.1016/j.brat.2022.104100
113. Ritterband LM, Thorndike FP, Morin CM, Gerwien R, Enman NM, Xiong R, et al. Real-world evidence from users of a behavioral digital therapeutic for chronic insomnia. Behav Res Ther. (2022) 153:104084. doi: 10.1016/j.brat.2022.104084
114. Morin CM, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. (2021) 87:38–45. doi: 10.1016/j.sleep.2021.07.035
115. Manzar M, Jahrami H, Bahammam A. Structural validity of the insomnia severity index: a systematic review and meta-analysis. Sleep Med Rev. (2021) 60:101531. doi: 10.1016/j.smrv.2021.101531
116. Spielman A, Caruso L, Glovinsky P. A behavior perspective on insomnia treatment. Psychiatr Clin North Am. (1987) 10:541–53. doi: 10.1016/S0193-953X(18)30532-X
117. Su T, Lien T. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
118. Li Y, Chen B, Hong Z, Sun Q, Dai Y, Basta M, et al. Insomnia symptoms during the early and late stages of the COVID-19 pandemic in China: a systematic review and meta-analysis. Sleep Med. (2022) 91:262–72. doi: 10.1016/j.sleep.2021.09.014
119. Šljivo A, Juginovi A, Ivanovi K, Quraishi I, Mula A, Kovaèevi Z, et al. Sleep quality and patterns of young West Balkan adults during the third wave of COVID-19 pandemic: a cross-sectional study. BMJ Open. (2022) 12:e060381. doi: 10.1136/bmjopen-2021-060381
120. Conte F, De Rosa O, Rescott ML, Arabia TP, D’Onofrio P, Lustro A, et al. High sleep fragmentation parallels poor subjective sleep quality during the third wave of the Covid-19 pandemic: an actigraphic study. J Sleep Res. (2022) 31:e13519. doi: 10.1111/jsr.13519
121. Taylor D, Lichstein K, Durrence H. Insomnia as a health risk factor. Behav Sleep Med. (2003) 1:227. doi: 10.1207/S15402010BSM0104_5
122. Sforza M, Galbiati A, Zucconi M, Casoni F, Hensley M, Ferini-Strambi L, et al. Depressive and stress symptoms in insomnia patients predict group cognitive-behavioral therapy for insomnia long-term effectiveness: a data-driven analysis. J Affect Disord. (2021) 289:117–24. doi: 10.1016/j.jad.2021.04.021
123. Esposito E, Di Matteo V, Di Giovanni G. Serotonin-dopamine interaction: an overview. Prog Brain Res. (2008) 172:3–6. doi: 10.1016/S0079-6123(08)00901-1
124. Hamann C, Bankmann J, Mora Maza H, Kornhuber J, Zoicas I, Schmitt-Böhrer A. Social fear affects limbic system neuronal activity and gene expression. Int J Mol Sci. (2022) 23:8228. doi: 10.3390/ijms23158228
125. Blake M, Trinder J, Allen N. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin Psychol Rev. (2018) 63:25–40. doi: 10.1016/j.cpr.2018.05.006
126. Sabbah S, Worden MS, Laniado DD, Berson DM, Sanes JN. Luxotonic signals in human prefrontal cortex as a possible substrate for effects of light on mood and cognition. Proc Natl Acad Sci USA. (2022) 119:e2118192119. doi: 10.1073/pnas.2118192119
127. Liverant G, Arditte Hall K, Wieman S, Pineles S, Pizzagalli D. Associations between insomnia and reward learning in clinical depression. Psychol Med. (2021) 26:1–10. doi: 10.1017/S003329172100026X
128. Wieman ST, Hall KA, MacDonald HZ, Gallagher MW, Suvak MK, Rando AA, et al. Relationships among sleep disturbance, reward system functioning, anhedonia, and depressive symptoms. Behav Ther. (2022) 53:105–18. doi: 10.1016/j.beth.2021.06.006
129. Schiller CE, Walsh E, Eisenlohr-Moul TA, Prim J, Dichter GS, Schiff L, et al. Effects of gonadal steroids on reward circuitry function and anhedonia in women with a history of postpartum depression. J Affect Disord. (2022) 314:176–84. doi: 10.1016/j.jad.2022.06.078
130. Kirschner M, Cathomas F, Manoliu A, Habermeyer B, Simon JJ, Seifritz E, et al. Shared and dissociable features of apathy and reward system dysfunction in bipolar I disorder and schizophrenia. Psychol Med. (2020) 50:936–47. doi: 10.1017/S0033291719000801
131. Bjorvatn B, Jernelöv S, Pallesen S. Insomnia–a heterogenic disorder often comorbid with psychological and somatic disorders and diseases: a narrative review with focus on diagnostic and treatment challenges. Front Psychol. (2021) 12:639198. doi: 10.3389/fpsyg.2021.639198
132. Fietze I, Laharnar N, Koellner V, Penzel T. The different faces of insomnia. Front Psychiatry. (2021) 12:683943. doi: 10.3389/fpsyt.2021.683943
133. Reynolds CF III, Kupfer DJ, Buysse DJ, Coble PA, Yeager A. Subtyping DSM-III-R primary insomnia: a literature review by the DSM-IV work group on sleep disorders. Am J Psychiatry. (1991) 148:432–8. doi: 10.1176/ajp.148.4.432
134. American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine (2014).
135. American Academy of Sleep Medicine. International Classification of Sleep Disorders. 2nd ed. Darien, IL: American Academy of Sleep Medicine (2005).
136. Blanken T, Benjamins J, Borsboom D, Vermunt J, Paquola C, Ramautar J, et al. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. (2019) 6:151–63. doi: 10.1016/S2215-0366(18)30464-4
137. Benjamins JS, Migliorati F, Dekker K, Wassing R, Moens S, Blanken TF, et al. Insomnia heterogeneity: characteristics to consider for data-driven multivariate subtyping. Sleep Med. Rev. (2017) 36:71–81. doi: 10.1016/j.smrv.2016.10.005
138. Dang-Vu TT, Hatch B, Salimi A, Mograss M, Boucetta S, O’Byrne J, et al. Sleep spindles may predict response to cognitive-behavioral therapy for chronic insomnia. Sleep Med. (2017) 39:54–61. doi: 10.1016/j.sleep.2017.08.012
139. van de Laar M, Leufkens T, Bakker B, Pevernagie D, Overeem S. Phenotypes of sleeplessness: stressing the need for psychodiagnostics in the assessment of insomnia. Psychol Heal Med. (2017) 22:902–10. doi: 10.1080/13548506.2017.1286360
140. Baglioni C, Regen W, Teghen A, Spiegelhalder K, Feige B, Nissen C, et al. Sleep changes in the disorder of insomnia: a meta-analysis of polysomnographic studies. Sleep Med Rev. (2014) 18:195–213. doi: 10.1016/j.smrv.2013.04.001
141. Van Someren EJW, Altena E, Ramauter JR, Stoffers D, Benjamins J, Moens S, et al. Imaging Causes and Consequences of Insomnia and Sleep Complaints. Cambridge: Cambridge University Press (2013). p. 187–96.
142. Harvey C, Gehrman P, Espie C. Who is predisposed to insomnia: a review of familial aggregation, stress-reactivity, personality and coping style. Sleep Med Rev. (2014) 18:237–47. doi: 10.1016/j.smrv.2013.11.004
143. Okajima I, Komada Y, Inoue Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep Biol Rhythms. (2011) 9:24–34. doi: 10.1111/j.1479-8425.2010.00481.x
144. Randall C, Nowakowski S, Ellis JG. Managing acute insomnia in prison: evaluation of a “One-Shot” cognitive behavioral therapy for insomnia (CBT-I) intervention. Behav Sleep Med. (2019) 17:827–36. doi: 10.1080/15402002.2018.1518227
145. Luik A, van der Zweerde T, van Straten A, Lancee J. Digital delivery of cognitive behavioral therapy for insomnia. Curr Psychiatry Rep. (2019) 21:50. doi: 10.1007/s11920-019-1041-0
146. Vedaa Ø, Kallestad H, Scott J, Smith O, Pallesen S, Morken G, et al. Effects of digital cognitive behavioral therapy for insomnia on insomnia severity: a large-scale randomised controlled trial. Lancet Digit Health. (2020) 2:e397–406. doi: 10.1016/S2589-7500(20)30135-7
147. Liu X, Li Y, Yan R, Timo H, Li D, Liu S, et al. The platform development, adherence and efficacy to a digital Brief therapy for insomnia (dBTI) during the COVID-19 pandemic. Methods. (2022) 205:39–45. doi: 10.1016/j.ymeth.2022.04.016
148. Léger D, Debellemaniere E, Rabat A, Bayon V, Benchenane K, Chennaoui M. Slow-wave sleep: from the cell to the clinic. Sleep Med Rev. (2018) 41:113–32. doi: 10.1016/j.smrv.2018.01.008
149. Rasch B, Born J. About sleeps role in memory. Physiol Rev. (2013) 93:681–766. doi: 10.1152/physrev.00032.2012
150. Ong J, Patanaik A, Chee N, Lee X, Poh J, Chee M. Auditory stimulation of sleep slow oscillations modulates subsequent memory encoding through altered hippocampal function. Sleep (Basel). (2018) 5:1–11. doi: 10.1093/sleep/zsy031
151. Marshall L. Transcranial direct current stimulation during sleep improves declarative memory. J Neurosci. (2004) 44:9985–92. doi: 10.1523/JNEUROSCI.2725-04.2004
152. Walsh J. Enhancement of slow wave sleep: implications for insomnia. J Clin Sleep Med. (2009) 5(Suppl. 2):S27–32. doi: 10.5664/jcsm.5.2S.S27
153. Zhang Y, Gruber R. Can slow-wave sleep enhancement improve memory? A review of current approaches and cognitive outcomes. Yale J Biol Med. (2019) 92:63–80.
154. Scholes S, Santisteban J, Zhang Y, Bertone A, Gruber R. Modulation of Slow-wave sleep: implications for psychiatry. Curr Psychiatry Rep. (2020) 22:52. doi: 10.1007/s11920-020-01175-y
155. Wood KH, Memon AA, Memon RA, Joop A, Pilkington J, Catiul C, et al. Slow wave sleep and EEG delta spectral power are associated with cognitive function in Parkinson’s disease. J Parkinsons Dis. (2021) 11:703–14. doi: 10.3233/JPD-202215
156. Facchin L, Schöne C, Mensen A, Bandarabadi M, Pilotto F, Saxena S, et al. Slow waves promote sleep-dependent plasticity and functional recovery after stroke. J Neurosci. (2020) 40:8637–51. doi: 10.1523/JNEUROSCI.0373-20.2020
Keywords: bibliometric analysis, citations, insomnia, trends, VOSviewer
Citation: Wan Q, Liu K, Wang X, Luo S, Yuan X, Wang C, Jiang J and Wu W (2023) The top 100 most cited papers in insomnia: A bibliometric analysis. Front. Psychiatry 13:1040807. doi: 10.3389/fpsyt.2022.1040807
Received: 09 September 2022; Accepted: 08 December 2022;
Published: 04 January 2023.
Edited by:
Mehmet Y. Agargün, Van Yüzüncü Yıl University, TurkeyReviewed by:
David Neubauer, Johns Hopkins Medicine, United StatesCélyne H. Bastien, Laval University, Canada
Copyright © 2023 Wan, Liu, Wang, Luo, Yuan, Wang, Jiang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenzhong Wu, ✉ bWFlcnRhX3pob25nYWN1QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Qingyun Wan†
Qingyun Wan† Kai Liu
Kai Liu Shuting Luo
Shuting Luo