
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 22 December 2022
Sec. Psychopharmacology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1033019
This article is part of the Research Topic Bridging the Gap: An Interdisciplinary Perspective on Ketamine in Psychiatric Disorders View all 11 articles
Objectives: Melancholic depression may respond differently to certain treatments. The aim of this study was to compare the antianhedonic effects of six intravenous injections of 0.5 mg/kg ketamine in patients with melancholic and non-melancholic depression, which remain largely unknown.
Methods: Individuals experiencing melancholic (n = 30) and non-melancholic (n = 105) depression were recruited and assessed for anhedonic symptoms using the Montgomery–Åsberg Depression Rating Scale (MADRS). The presence of melancholic depression was measured with the depression scale items at baseline based on DSM-5 criteria.
Results: A total of 30 (22.2%) patients with depression fulfilled the DSM-5 criteria for melancholic depression. Patients with melancholic depression had a non-significant lower antianhedonic response (43.3 vs. 50.5%, t = 0.5, p > 0.05) and remission (20.0 vs. 21.0%, t = 0.01, p > 0.05) to repeated-dose ketamine infusions than those with non-melancholic depression. The melancholic group had significantly lower MADRS anhedonia subscale scores than the non-melancholic group at day 26 (p < 0.05).
Conclusion: After six ketamine infusions, the improvement of anhedonic symptoms was found in both patients with melancholic and non-melancholic depression, and the efficacy was similar in both groups.
Melancholic features were classified by the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) as a particular subtype of major depressive disorder (MDD), which may coexist with other patterns of depressive symptoms (1). This concept of melancholic depressive symptoms primarily originated from the historic concept of “endogenous depression” (2). Melancholia can occur in either MDD or major depressive episodes (MDEs) of bipolar depression (BD) (3). Melancholic depression may be associated with a relatively severe clinical manifestation of mood disorder (3).
Patients with melancholic depressive are differentiated from patients with non-melancholic depressive with regard to clinical characteristics, neurocognitive dysfunctions, treatment response patterns, and neuroimaging findings. For example, a recent meta-analysis found that acute episodes of MDD with melancholic features had greater neurocognitive deficits than episodes with non-melancholic features (4). A prospective study reported that subjects with melancholic features have higher excess all-cause mortality than those without melancholic features (5). However, findings on the treatment responses to psychotropic drug treatments between patients with melancholic and non-melancholic features were inconsistent. For example, when compared to those with non-melancholic depression, patients with melancholic depression had similar responses to antidepressants (3, 6) and quetiapine (7), had stronger responses to lithium (8) and electroconvulsive therapy (ECT) (9), and had weaker responses to psychotherapy (10).
Apart from the rapid and robust antisuicidal and antidepressant effects (11–15), accumulating evidence has shown that both single and repeated ketamine injections at a subanaesthetic dose (0.5 mg/kg over 40 min) have rapid and robust antianhedonic effects in individuals suffering from MDD and BD (16–19). Notably, ketamine's antianhedonic effects were independent of other depressive symptoms (16). A recent study found that a single dose of ketamine appears to be effective in treating both melancholic/typical and atypical depressive symptoms (1). However, the differences in the antianhedonic effects of repeated ketamine infusions in patients with melancholic and non-melancholic depression have remained unknown.
In this exploratory study, we divided the participants into melancholic and non-melancholic subtypes and sought to comparatively investigate the antianhedonic effects of multiple intravenous injections of 0.5 mg/kg ketamine in individuals with melancholic and non-melancholic depression. Based on the findings of a recent study (1), we hypothesized that multiple intravenous injections of ketamine effectively treated anhedonic symptoms in both melancholic and non-melancholic depression.
In this post hoc analysis, data were drawn from an ongoing real-world open-label study investigating the efficacy and safety of adjunctive multiple ketamine infusions for the treatment of patients with depression with TRD and/or suicidal ideation, which was initiated in November 2016 and registered in the Chinese Clinical Trail Registry (Clinical Trials Identifier: ChicCTR-OOC-17012239). All patients provided written informed consent, and approval was obtained from the Affiliated Brain Hospital of Guangzhou Medical University respective Institutional Review Board (IRB) (Ethical Application Ref: 2016030).
Patients with depression were recruited from the Affiliated Brain Hospital of Guangzhou Medical University. The inclusion criteria for this real-world open-label study were as follows: (1) a diagnosis of MDD or BD without hallucinations or delusions according to the DSM-5 criteria; (2) experiencing a MED with a baseline score ≥17 on the Hamilton Depression Rating Scale-17 (HAMD-17); (3) aged 18–65 years; and (4) suffering from suicidal ideation with a Beck Scale for Suicide Ideation-part I (SSI-part I) scores of 2 or higher and/or TRD, defined as having failed attempts to achieve a response to two trials of antidepressants. The exclusion criteria were as follows: (1) patients fulfilling the DSM-5 criteria for other serious mental disorders, such as schizophrenia or alcohol/substance use disorder; (2) patients with a positive urine toxicology screen; (3) patients with any serious or unstable somatic diseases, such as cancer or infectious disease; and (4) patients who were pregnant or breast feeding.
The procedures for subanaesthetic intravenous ketamine have been detailed previously (11). In brief, as recommended previously (12), all participants received a course of six intravenous infusions of ketamine hydrochloride (0.5 mg/kg over 40 min) administered thrice weekly over the course of 2 weeks following overnight fasting. A psychiatrist recorded vital signs, including pulse frequency, blood pressure and heart rate, every 10 min throughout the infusion and monitoring period. All subjects remained on stable type and dosage of concomitant psychotropic medication during the infusion treatment.
A detailed demographic questionnaire was conducted for patients with melancholic and non-melancholic depression, recording general information and socio-demographic characteristics, such as age, gender, and marital status. Clinical ratings of the severity of anhedonic symptoms measured in a sample of individuals with melancholic and non-melancholic depression at baseline, at 4 and 24 h after each infusion of the study agent, and at 2 weeks postinfusion (day 26) using the Montgomery–Åsberg Depression Rating Scale (MADRS). Following the methodology of previous studies (20–22), the anhedonia items of the MADRS, including assessments of apparent sadness, concentration difficulties, lassitude, reported sadness, and inability to feel, were utilized to assess the severity of anhedonic symptoms (23, 24). The coprimary endpoints were the comparison of antianhedonic response and remission (≥50 and ≥75% reduction of the MADRS anhedonia subscale scores at day 13, respectively) (25, 26) between individuals with melancholic and non-melancholic depression. The secondary endpoint was the comparison of the severity of anhedonic symptoms between individuals with melancholic and non-melancholic depression. The intraclass correlation coefficient (ICC) for the MADRS anhedonia subscale scores was >0.9, suggesting excellent interrater reliability.
As recommended previously (7), baseline scores on the HAMD-17 and MADRS were used to split the population into two subgroups (patients with melancholic and non-melancholic depression). The presence of melancholic depression was defined based on DSM-5 criteria (7), which require anhedonia in nearly all activities (MADRS item 8 ≥ 4) and/or non-reactive mood (MADRS items 1 or 2 = 6), and at least three of the following: significant psychomotor retardation or agitation (HAMD-17 items 8 or 9 ≥ 2), marked appetite/weight loss (HAMD-17 items 12 or 16 = 2), terminal insomnia (HAMD-17 item 6 ≥ 1), and unwarranted or disproportionate guilt (HAMD-17 item 2 ≥ 2).
In this study, we used SPSS version 24.0 (SPSS Inc., Chicago, United States) for all statistical analyses. Intent-to-treat analysis was conducted in this study. The demographic and clinical variables of individuals with melancholic and non-melancholic depression were compared with Student's t-test for continuous variables (including age, body mass index, education, depressive symptoms, anxiety symptoms, and suicidal ideation) and the Chi-square test for categorical variables (including gender, marital status, and rates of antianhedonic response, and remission). The rates of antianhedonic response and remission between individuals with melancholic and non-melancholic depression were analyzed by the Chi-square test. The comparisons of the rates of antianhedonic response and remission between the two groups were performed using odds ratios derived from logistic regression analyses after adjusting for the sociodemographic confounding variables. A linear mixed-effects model was utilized to determine the difference in anhedonic symptoms over time between groups. The covariates in the linear mixed-effects model analysis included baseline demographic and clinical variables that differed between the two groups. We utilized Bonferroni correction to adjust for multiple comparisons and set the significance level α at 0.05.
Among 135 patients with depression receiving repeated ketamine infusions, 30 (22.2%) fulfilled the DSM-5 criteria for melancholic depression, and 105 (77.8%) did not. The demographic and clinical characteristics of patients with melancholic depression vs. non-melancholic depression are summarized in Table 1. As expected, the melancholic subgroup had higher baseline HAMD-17 scores (t = 10.5, p < 0.001), baseline MADRS scores (t = 7.8, p < 0.001), and baseline MADRS anhedonia subscale scores (t = 17.4, p < 0.001) (Table 1). The subgroups did not differ with regard to age, sex, education level, or age of onset (all p > 0.05).
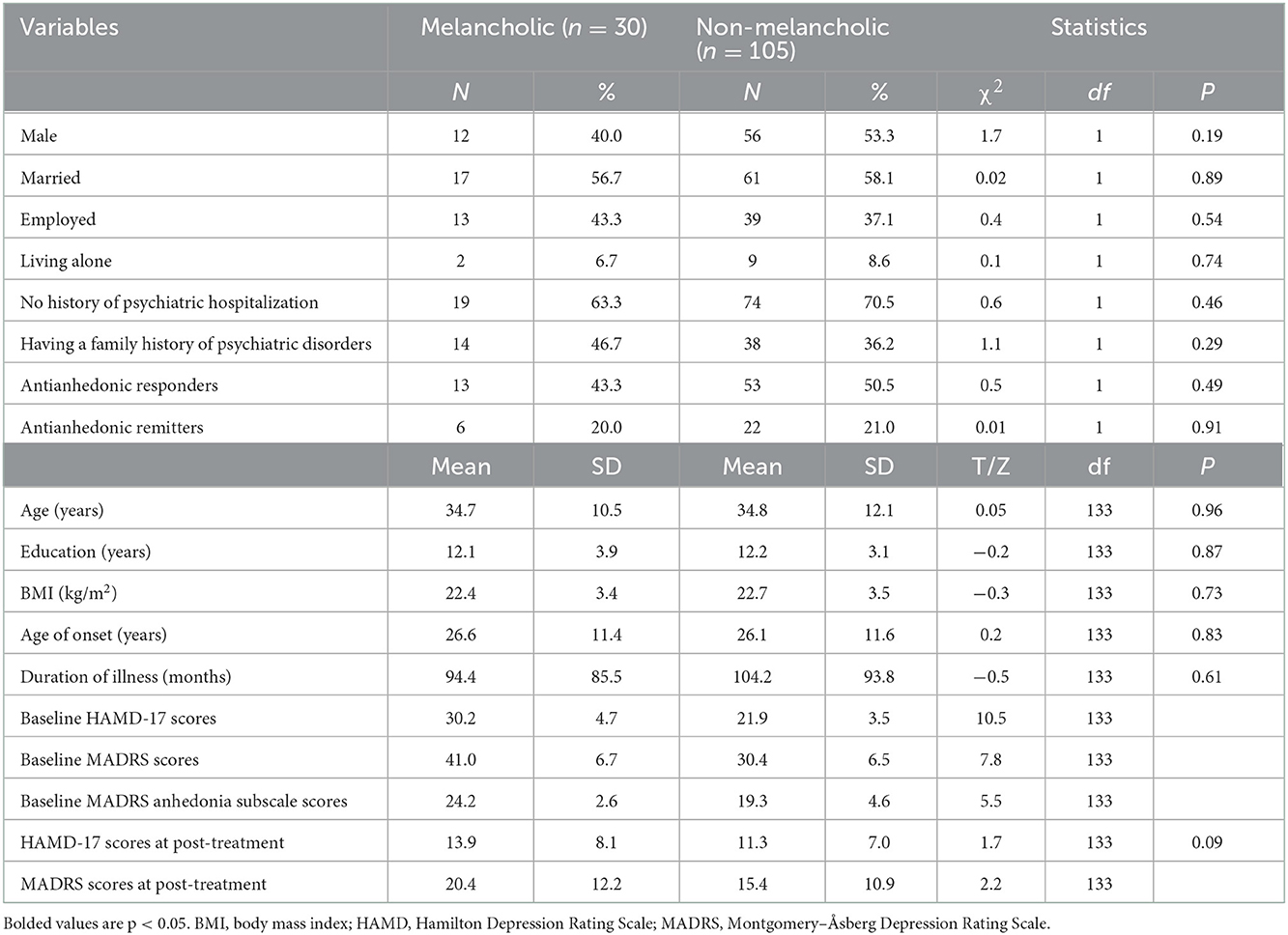
Table 1. Comparison of demographic and clinical characteristics between patients with melancholic depression and non-melancholic depression.
As shown in Table 1, patients with non-melancholic depression had significantly lower MADRS scores at post-treatment (15.4 ± 10.9 vs. 20.4 ± 12.2, p < 0.05) than those with melancholic depression, but significance disappeared after controlling for baseline MADRS scores (p > 0.05). Patients with non-melancholic depression had non-significantly lower HAMD scores at post-treatment (11.3 ± 7.0 vs. 13.9 ± 8.1, p > 0.05) than those with melancholic depression. Patients with melancholic depression achieved a non-significant lower antianhedonic response to repeated-dose ketamine infusions than those with non-melancholic depression [43.3% (13/30) vs. 50.5% (53/105), t = 0.5, p > 0.05]. Similarly, patients with melancholic depression met a non-significant lower antianhedonic remission criteria than those with non-melancholic depression [20.0% (6/30) vs. 21.0% (22/105), t = 0.01, p > 0.05]. No significant differences between the two groups were observed regarding antianhedonic response and remission rates after controlling for confounds (all p > 0.05).
The linear mixed model with MADRS anhedonia subscale scores showed significant main effects for group-by-time interaction (F = 3.0, p < 0.001) and time (F = 64.4, p < 0.001) but not for group (F = 0.6, p = 0.46). Compared with baseline, significant improvements in anhedonic symptoms were found from day 1 to 26 and from day 3 to 26 in the non-melancholic and melancholic groups, respectively (all p < 0.05). As shown in Figure 1, the melancholic group had significantly lower MADRS anhedonia subscale scores than the non-melancholic group at day 26 (p < 0.05).
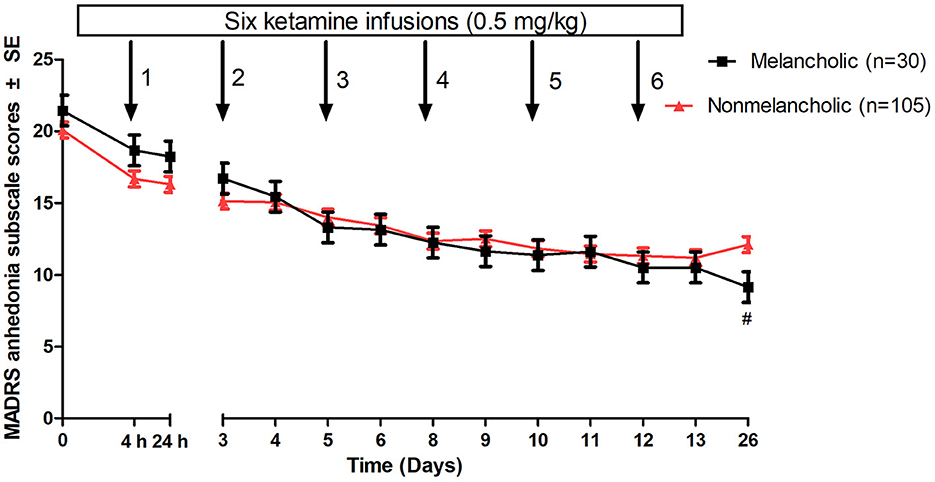
Figure 1. Change in ahedonic symptoms in patients with melancholic and non-melancholic depression following multiple ketamine infusions. Values covaried for baseline MADRS anhedonia subscale scores. #A significant difference was found at a given time point between patients with melancholic and non-melancholic depression (p < 0.05). MADRS, Montgomery-Åsberg Depression Rating Scale; SE, standard error.
To the best of our knowledge, this is the first study to examine the differences in antianhedonic response and remission to six intravenous injections of 0.5 mg/kg ketamine over 40 min in individuals with non-melancholic and melancholic depression. The following major findings were obtained: (1) 22.2% (30/135) of subjects reported melancholic depression; (2) similar antianhedonic response and remission rates were found in individuals with or without melancholic depression after six injections of ketamine; and (3) the reduction of anhedonic symptoms in patients with melancholic depression was greater at day 26 than in patients with non-melancholic depression.
Based on the DSM-5 criteria, 22% of participants suffer from melancholic depression, which is relatively lower than the figure (31.7%) reported in a previous study (7). Another study (27) found that 13 of 33 (39.3%) participants were classified as having melancholic depression according to the CORE measure (28). The differences in the presence of melancholic depression between our findings and Spanemberg et al.'s study (27) are mainly attributed to differential diagnosis criteria for melancholic depression. Furthermore, Joyce et al. found that the CORE criteria for melancholia, but not the Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV), had greater neuroendocrine dysfunction (29).
In this post hoc secondary analysis, significant rapid improvements in anhedonic symptoms in both patients with and without melancholic depression were observed in response to six ketamine infusions in this group of individuals suffering from either MDD or BD. Furthermore, the antianhedonic response and remission to repeated intravenous administration of subanaesthetic doses of ketamine were similar in patients with and without melancholic depression. The fact that this difference did not achieve statistical significance may be due to the relatively small number of melancholic patients in the sample. The potential for a superior result with melancholic patients deserves further study with a larger sample. Similarly, a single ketamine infusion effectively reduced depressive symptoms in patients with melancholic/typical and atypical depression, with similar efficacy in both groups (1). However, the differences in antianhedonic effects of a single ketamine infusion between the two groups should be investigated in future studies.
The present study has several strengths and limitations. The largest strength of this study is that it is the first to compare the antianhedonic effects of ketamine between patients with melancholic depression and those with non-melancholic depression. The limitations of this study are as follows: (1) open-label design; (2) the sample size for the melancholic group (n = 30) was relatively small; (3) the pooling of individuals with MDD and BD increasing sample heterogeneity; (4) the anhedonia items of the MADRS were used to assess anhedonic symptoms rather than a specific scale for anhedonia, such as the Snaith–Hamilton Pleasure Scale (SHAPS) (30–32); and (5) the secondary/post hoc analysis of melancholic depression based on scale items.
After six ketamine infusions, an improvement in anhedonic symptoms was observed in patients with melancholic and non-melancholic depression, but with similar efficacy in both groups. These findings are still exploratory, and future studies with a randomized, active placebo-controlled design are warranted.
• The prevalence of melancholic depression was 22.2%.
• Ketamine effectively relieved anhedonic symptoms in both patients with melancholic and non-melancholic depression.
• The antianhedonic effects of ketamine was similar in patients with melancholic than non-melancholic depression.
• This study was a post hoc secondary analysis.
• Participants were pooled across diagnoses (bipolar depression and major depressive disorder).
• This study was conducted based on an open-label design.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Affiliated Brain Hospital of Guangzhou Medical University respective Institutional Review Board (IRB) (Ethical Application Ref: 2016030). The patients/participants provided their written informed consent to participate in this study.
Y-PN: study design and critical revision of the manuscript. WZ, Y-LZ, and C-YW: data collection. WZ, X-HY, and L-MG: analysis and interpretation of data. WZ and J-QT: drafting of the manuscript. All authors: approval of the final version for publication.
This study was funded by the Scientific Research Project of Guangdong Provincial Bureau of Traditional Chinese Medicine (20201273), the National Natural Science Foundation of China (82101609), Scientific Research Project of Guangzhou Bureau of Education (202032762), Science and Technology Program Project of Guangzhou (202102020658), Guangzhou Health Science and Technology Project (20211A011045), Guangzhou Science and Technology Project of Traditional Chinese Medicine and Integrated Traditional Chinese and Western medicine (20212A011018), China International Medical Exchange Foundation (Z-2018-35-2002), Guangzhou Clinical Characteristic Technology Project (2019TS67), and Science and Technology Program Project of Guangzhou (202102020658). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Park LT, Luckenbaugh DA, Pennybaker SJ, Hopkins MA, Henter ID, Lener MS, et al. The effects of ketamine on typical and atypical depressive symptoms. Acta Psychiatr Scand. (2020) 142:394–401. doi: 10.1111/acps.13216
2. Dold M, Bartova L, Fugger G, Kautzky A, Mitschek MMM, Fabbri C, et al. Melancholic features in major depression - a European multicenter study. Progr Neuro-Psychopharmacol Biol Psychiatr. (2021) 110:110285. doi: 10.1016/j.pnpbp.2021.110285
3. Undurraga J, Vázquez GH, Tondo L, Baldessarini RJ. Antidepressant responses in direct comparisons of melancholic and non-melancholic depression. J Psychopharmacol. (2020) 34:1335–41. doi: 10.1177/0269881120953983
4. Valerio MP, Szmulewicz AG, Lomastro J, Martino DJ. Neurocognitive performance in melancholic and non-melancholic major depressive disorder: a meta-analysis of comparative studies. Psychiatr Res. (2021) 303:114078. doi: 10.1016/j.psychres.2021.114078
5. Rantanen AT, Kallio MM, Korkeila JJA, Kautiainen H, Korhonen PE. Relationship of non-melancholic and melancholic depressive symptoms with all-cause mortality: a prospective study in a primary care population. J Psychosomat Res. (2020) 133:110107. doi: 10.1016/j.jpsychores.2020.110107
6. Bobo WV, Chen H, Trivedi MH, Stewart JW, Nierenberg AA, Fava M, et al. Randomized comparison of selective serotonin reuptake inhibitor (escitalopram) monotherapy and antidepressant combination pharmacotherapy for major depressive disorder with melancholic features: a CO-MED report. J Affect Disord. (2011) 133:467–76. doi: 10.1016/j.jad.2011.04.032
7. Peters EM, Bowen R, Balbuena L. Melancholic depression and response to quetiapine: a pooled analysis of four randomized placebo-controlled trials. J Affect Disord. (2020) 276:696–8. doi: 10.1016/j.jad.2020.07.071
8. Valerio MP, Martino DJ. Differential response to lithium between melancholic and non-melancholic unipolar depression. Psychiatr Res. (2018) 269:183–4. doi: 10.1016/j.psychres.2018.08.077
9. Pinna M, Manchia M, Oppo R, Scano F, Pillai G, Loche AP, et al. Clinical and biological predictors of response to electroconvulsive therapy. (ECT): a review. Neurosci Lett. (2018) 669:32–42. doi: 10.1016/j.neulet.2016.10.047
10. Boschloo L, Bekhuis E, Weitz ES, Reijnders M, DeRubeis RJ, Dimidjian S, et al. The symptom-specific efficacy of antidepressant medication vs. cognitive behavioral therapy in the treatment of depression: results from an individual patient data meta-analysis. World Psychiatr. (2019) 18:183–91. doi: 10.1002/wps.20630
11. Zheng W, Zhou YL, Liu WJ, Wang CY, Zhan YN, Li HQ, et al. Rapid and longer-term antidepressant effects of repeated-dose intravenous ketamine for patients with unipolar and bipolar depression. J Psychiatr Res. (2018) 106:61–8. doi: 10.1016/j.jpsychires.2018.09.013
12. Shiroma PR, Johns B, Kuskowski M, Wels J, Thuras P, Albott CS, et al. Augmentation of response and remission to serial intravenous subanesthetic ketamine in treatment resistant depression. J Affect Disord. (2014) 155:123–9. doi: 10.1016/j.jad.2013.10.036
13. Zhan Y, Zhang B, Zhou Y, Zheng W, Liu W, Wang C, et al. A preliminary study of anti-suicidal efficacy of repeated ketamine infusions in depression with suicidal ideation. J Affect Disord. (2019) 251:205–12. doi: 10.1016/j.jad.2019.03.071
14. Hu YD, Xiang YT, Fang JX, Zu S, Sha S, Shi H, et al. Single i.v. ketamine augmentation of newly initiated escitalopram for major depression: results from a randomized, placebo-controlled 4-week study. Psychol Med. (2016) 46:623–35. doi: 10.1017/S0033291715002159
15. Murrough JW, Perez AM, Pillemer S, Stern J, Parides MK, aan het Rot M, et al. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatr. (2013) 74:250–6. doi: 10.1016/j.biopsych.2012.06.022
16. Lally N, Nugent AC, Luckenbaugh DA, Ameli R, Roiser JP, Zarate CA. Anti-anhedonic effect of ketamine and its neural correlates in treatment-resistant bipolar depression. Transl Psychiatr. (2014) 4:e469. doi: 10.1038/tp.2014.105
17. Lally N, Nugent AC, Luckenbaugh DA, Niciu MJ, Roiser JP, Zarate CA, Jr. Neural correlates of change in major depressive disorder anhedonia following open-label ketamine. J Psychopharmacol. (2015) 29:596–607. doi: 10.1177/0269881114568041
18. Rodrigues NB, McIntyre RS, Lipsitz O, Cha DS, Lee Y, Gill H, et al. Changes in symptoms of anhedonia in adults with major depressive or bipolar disorder receiving IV ketamine: Results from the Canadian Rapid Treatment Center of Excellence. J Affective Disord. (2020) 276:570–5. doi: 10.1016/j.jad.2020.07.083
19. Zheng W, Gu LM, Sun CH, Zhou YL, Wang CY, Lan XF, et al. Comparative effectiveness of repeated ketamine infusions in treating anhedonia in bipolar and unipolar depression. J Affective Disord. (2022) 300:109–13. doi: 10.1016/j.jad.2021.12.105
20. McIntyre RS, Loft H, Christensen MC. Efficacy of vortioxetine on anhedonia: results from a pooled analysis of short-term studies in patients with major depressive disorder. Neuropsychiatr Dis Treat. (2021) 17:575–85. doi: 10.2147/ndt.s296451
21. Cao B, Park C, Subramaniapillai M, Lee Y, Iacobucci M, Mansur RB, et al. The efficacy of vortioxetine on anhedonia in patients with major depressive disorder. Front Psychiatr. (2019) 10:17. doi: 10.3389/fpsyt.2019.00017
22. Zheng W, Gu LM, Zhou YL, Wang CY, Lan XF, Zhang B, et al. Association of VEGF with antianhedonic effects of repeated-dose intravenous ketamine in treatment-refractory depression. Front Psychiatr. (2021) 12:780975. doi: 10.3389/fpsyt.2021.780975
23. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatr. (1979) 134:382–9. doi: 10.1192/bjp.134.4.382
24. Zhong BL, Wang Y, Chen HH, Wang XH. Reliability, validity and sensitivity of Montgomery-Åsberg Depression Rating Scale for patients with current major depressive disorder [in Chinese]. Chinese J Behav Med Brain Sci. (2011) 20:85–7. doi: 10.3760/cma.j.issn.1674-6554.2011.01.032
25. Zheng W, Yang XH, Gu LM, Tan JQ, Zhou YL, Wang CY, et al. Gender differences in the antianhedonic effects of repeated ketamine infusions in patients with depression. Front Psychiatr. (2022) 13:981981. doi: 10.3389/fpsyt.2022.981981
26. Zheng W, Yang XH, Gu LM, Tan JQ, Zhou YL, Wang CY, et al. Antianhedonic effects of serial intravenous subanaesthetic ketamine in anxious versus nonanxious depression. J Affect Disord. (2022) 313:72–6. doi: 10.1016/j.jad.2022.06.081
27. Spanemberg L, Caldieraro MA, Vares EA, Wollenhaupt-Aguiar B, Kauer-Sant'Anna M, Kawamoto SY, et al. Biological differences between melancholic and nonmelancholic depression subtyped by the CORE measure. Neuropsychiatr Dis Treat. (2014) 10:1523–31. doi: 10.2147/NDT.S66504
28. Parker G, Hadzi-Pavlovic D, Wilhelm K, Hickie I, Brodaty H, Boyce P, et al. Defining melancholia: properties of a refined sign-based measure. Br J Psychiatr. (1994) 164:316–26. doi: 10.1192/bjp.164.3.316
29. Joyce PR, Mulder RT, Luty SE, McKenzie JM, Sullivan PF, Abbott RM, et al. Melancholia: definitions, risk factors, personality, neuroendocrine markers and differential antidepressant response. Austral N Z J Psychiatr. (2002) 36:376–83. doi: 10.1046/j.1440-1614.2001.01025.x
30. Franken IH, Rassin E, Muris P. The assessment of anhedonia in clinical and non-clinical populations: further validation of the Snaith-Hamilton Pleasure Scale. (SHAPS). J Affect Disord. (2007) 99:83–9. doi: 10.1016/j.jad.2006.08.020
31. Liu WH, Wang LZ, Zhu YH, Li MH, Chan RC. Clinical utility of the Snaith-Hamilton-Pleasure scale in the Chinese settings. BMC Psychiatr. (2012) 12:184. doi: 10.1186/1471-244X-12-184
Keywords: clinical trial, ketamine, depression, melancholia, response
Citation: Zheng W, Yang X-H, Gu L-M, Tan J-Q, Zhou Y-L, Wang C-Y and Ning Y-P (2022) A comparison of the antianhedonic effects of repeated ketamine infusions in melancholic and non-melancholic depression. Front. Psychiatry 13:1033019. doi: 10.3389/fpsyt.2022.1033019
Received: 31 August 2022; Accepted: 05 December 2022;
Published: 22 December 2022.
Edited by:
Sherry-Anne Muscat, Alberta Hospital Edmonton, CanadaReviewed by:
Rodrigo Simonini Delfino, Federal University of São Paulo, BrazilCopyright © 2022 Zheng, Yang, Gu, Tan, Zhou, Wang and Ning. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Ping Ning,  bmluZ2plbnlAMTI2LmNvbQ==
bmluZ2plbnlAMTI2LmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.