- Department of Psychiatry, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Background: Posttraumatic stress disorder (PTSD) may develop as a serious long-term consequence of traumatic experiences, even many years after trauma exposure. Dessie town residents have experienced prolonged armed conflict due to inter-communal conflict in 2021. Those people are exposed to different kinds of trauma, and violence, making them more prone to psychological disorders. Despite the highest number of people affected due to conflict and its negative impact on mental health, post-traumatic stress disorders among people are overlooked in Ethiopia. This study aimed to assess the prevalence and associated factors of post-traumatic stress disorder among people who experienced traumatic events in Dessie town, Ethiopia, 2022.
Materials and methods: Community based cross-sectional study was conducted on June 8–July 7, 2022, by using a multi-stage cluster sampling with a total sample of 785. Pretested, structured questionnaires and face-to-face interviews were used for data collection. PTSD was assessed by the Post-traumatic stress disorder Checklist for DSM-5 (PCL-5). Data was entered using Epi-data version 3.1 and, then exported to SPSS version 26 for analysis. The association between outcome and independent variables was analyzed with bi-variable and multivariable logistic regression. P-values less than 0.05 was considered statistically significant.
Result: The prevalence of PTSD among Dessie town residents was found to be 19.4% (95% CI, 16.7, 22.0). In multivariable analysis, being females (AOR = 1.63, 95% CI 1.10–2.44), previous history of mental illness (AOR = 3.14, 95% CI 1.14–7.06) depressive symptoms (AOR = 3.12, 95% CI 1.92–5.07), witnessing a serious physical injury of a family member or friend (AOR = 2.82, 95% CI 1.18–6.70) and high perceived life threats (AOR = 5.73, 95% CI 3.05–10.78) were found to be significant predictors of PTSD.
Conclusion: The prevalence of PTSD among Dessie town residents was found to be huge. Being female, having a previous history of mental illness, depressive symptoms, witnessing a serious physical injury of a family member or friend, and high perceived life threats were variables that are independent predictors of PSTD. People who have experienced such a severe traumatic event require psychosocial support to aid in their recovery from the terrible experiences.
Background
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Posttraumatic stress disorder (PTSD) is one of the mental disorder related to the following exposure to a traumatic or stressful event which is characterized by the symptoms of intrusion, avoidance, alternation of mood and cognition and hyperarousal lasts for more than a month after the stressful event (1). Experiencing or witnessing traumatic events including murder, threats, kidnapping, the death of loved ones or friends, the loss of a home, or malnutrition can lead to PTSD (2). The global economic burden of stress-related mental illness is expected to rise in the coming decade (3). The world health organization (WHO) global disease of burden survey estimates that mental illness, including stress-related disorders, will be the second leading cause of disability by the year 2023 (4). In a given year, PTSD affected about 8 million adults worldwide (5). PTSD was followed by 0.4% of all years lived with disability, and the estimated burden increased to 0.6% of years of healthy life lost due to disability (YLD). globally, according to the world health report (3). In the upcoming decade, it is anticipated that trauma-related mental illness will have a greater economic impact and raises the risk of physical illness (diabetes, obesity, pain, etc.) globally, leading to disability and compromising the quality of life.
In post-conflict and conflict-ridden societies, the prevalence rates in the general population can be much higher (6). According to statistical estimates, the prevalence of PTSD ranges from 1 and 5% in studies of the general population (7, 8), and from 3 and 58% in high-risk groups such as conflict areas (9, 10). Northern Ethiopia went through one of the worst civil conflicts that attracted the world’s attention in 2021. The civil conflict was between the Ethiopian National Defence Forces (ENDF) and The Tigray People’s Liberation Front (TPLF) party (11). Due to this thousands of people died, and many people were injured and were subjected to traumatic events due to this conflict while they were trying to survive. Additionally, nearly 2 million people were displaced into internally displaced people’s camps (IDPs) as a result of violent threats that included rape, torture, mutilation, and destruction of property and many of them people including children were abducted, rendering them more susceptible to psychological disorders, particularly post-traumatic stress disorder (PTSD) (11).
A meta-analysis study conducted on a global population of adult war survivors that looked at all countries that suffered at least one war within their territory between 1989 and 2015 found that 23.81% of adult war survivors met the diagnostic criteria for PTSD (12). Another systematic review undertaken revealed that the prevalence of PTSD in the community ranges from 3 to 88% (13, 14). In addition, a cross-sectional survey was conducted among community levels in Nepal during armed conflict and the reported prevalence of PTSD was 53.4% (15). In another research conducted on Palestinian people who were living in refugee camps during the Al-Aqsa intifada, the estimated prevalence of post-traumatic stress disorder was 68.9% (16). Furthermore, studies showed in Africa, internally displaced victims in Nigeria 63% (17), Morocco 19.3% (18), and South Sudan 28% (19). Some studies report from Ethiopia showed Maikadra Massacre Suffer in North West, Ethiopia 59.8% (16), and internally displaced people in South Ethiopia 58.4% (20). Another study finding from West of Ethiopia showed the overall prevalence rate of PTSD among traumatic Patients was 17.1% (21). In a community-based, cross-sectional study conducted on landslide survivors, in Addis Ababa, Ethiopia the prevalence of PTSD was 37.3% (22).
Many studies have shown a link between PTSD and various risk factors before the injury like sex, low educational status, low social support, unemployment, lower socioeconomic status, younger age, childhood abuse, history of depressive symptoms, and history of mental illnesses (23–25). Also, factors during the traumatic events such as witnessing the death and serious physical injury of a family member or friend, the property being destroyed during the conflict, serious physical injury during the conflict, and alcohol use (12, 16–18, 20, 22, 26). Additionally, factors after the injury like high perceived life threats, and the property being destroyed after the conflict (16) have been frequently reported as predictors of posttraumatic stress disorder.
Conflicts reportedly killed over three times more people during the past decade than natural disasters (27). In Ethiopia, where armed conflict, ethnic violence, and terrorist attacks are on the rise, only a few studies with highly variable estimates of the prevalence of post-traumatic stress disorder have been published, despite mounting evidence of its high prevalence in conflict-affected nations around the world. Moreover, it was reported that the number of reports that dealt with the prevalence of mental illnesses among people who were living in areas of conflict is limited. Therefore this study is aimed at assessing the prevalence of post-traumatic stress disorder and its predictors among people who experienced traumatic events in Dessie town situated in the area of armed conflict. The findings of this study will help health professionals, NGOs, and psychological centers to develop appropriate plans and interventions to provide evidence-based treatment for patients with PTSD. Additionally, it can also serve as baseline data for those who wish to conduct studies in this area.
Materials and methods
Study setting, design, and period
A community-based cross-sectional study was conducted in Dessie Town, Northeast Ethiopia, from June 8 to July 7/2022. The administrative center of Dessie Town in the Amhara Region; is located from Addis Ababa to Northeast Ethiopia 401 Km. It sits at a latitude and longitude of 11°8′N 39°38′E, with an elevation between 2,470 and 2,550 meters above sea level. It has 18 kebeles and has a 350,000 population. Among those populations 186,571 males and 163,429 females according to 2016 to 2017 South Wollo Zone statistics office data. The two governmental hospitals have psychiatric outpatient and inpatient services.
Source of population
All residents of Dessie town, North East, Ethiopia.
Study population
Households live in the Menafesha sub-city who are in the selected kebele and available during the study period.
Inclusion and exclusion criteria
All households in selected kebeles and one individual from each household who was 18 years old and above, living in Dessie town during the time of the study were included, while participants who were not available during wartime, severely ill, and unable to communicate during data collection time and those residents less than 6 months were excluded from the study.
Sample size determination and sampling technique
Sample size determination
To calculate the maximum estimated sample size, the single population proportion formula was used at 95% CI and 5% marginal error and by taking the P-value of 58.4% from the previous study in Southern Ethiopia (20). Then the sample size was calculated as follows;
where: n = sample size, P = prevalence of previous study (58.4%), d = degree of precision (assumed to be 5%), (z α/2)2 = 1.96 = the value of standard normal variable that corresponds to be 95% confidence levels (1.96).
Since we have employed a multi-stage sampling technique to consider the designing effect, the calculated sample size by two to correct the sampling error. After all, by adding a 10% non-response rate, the final sample size was 821.
Sampling technique and procedure
A multi-stage probability sampling technique was employed. There are five sub-cities in Dessie town, and one sub-city was selected from the entire, employing a simple random sampling technique, then within this chosen sub-city there are three kebeles, and therefore the numbers of participants were selected from each kebele using the proportional allocation of the sample size. Then, a systematic random sampling technique was employed to select study units. the primary study unit was selected randomly between 1st and Kth and study subjects in every Kth household. When more than one study subject was found in one household, a lottery method was used to select a participant. If the chosen house is closed during data collection, the subsequent household participant was interviewed. i.e., Kj = Nj/nj where; Kj = sampling interval, Nj = total number of households, nj = total number of sample size. There are three kebeles within the Menafesha sub-city and having a total of 3,832 households, K or interval was decided by N/n (K = 3832/821 = 4). They interviewed one individual from every four households consecutively (Figure 1).
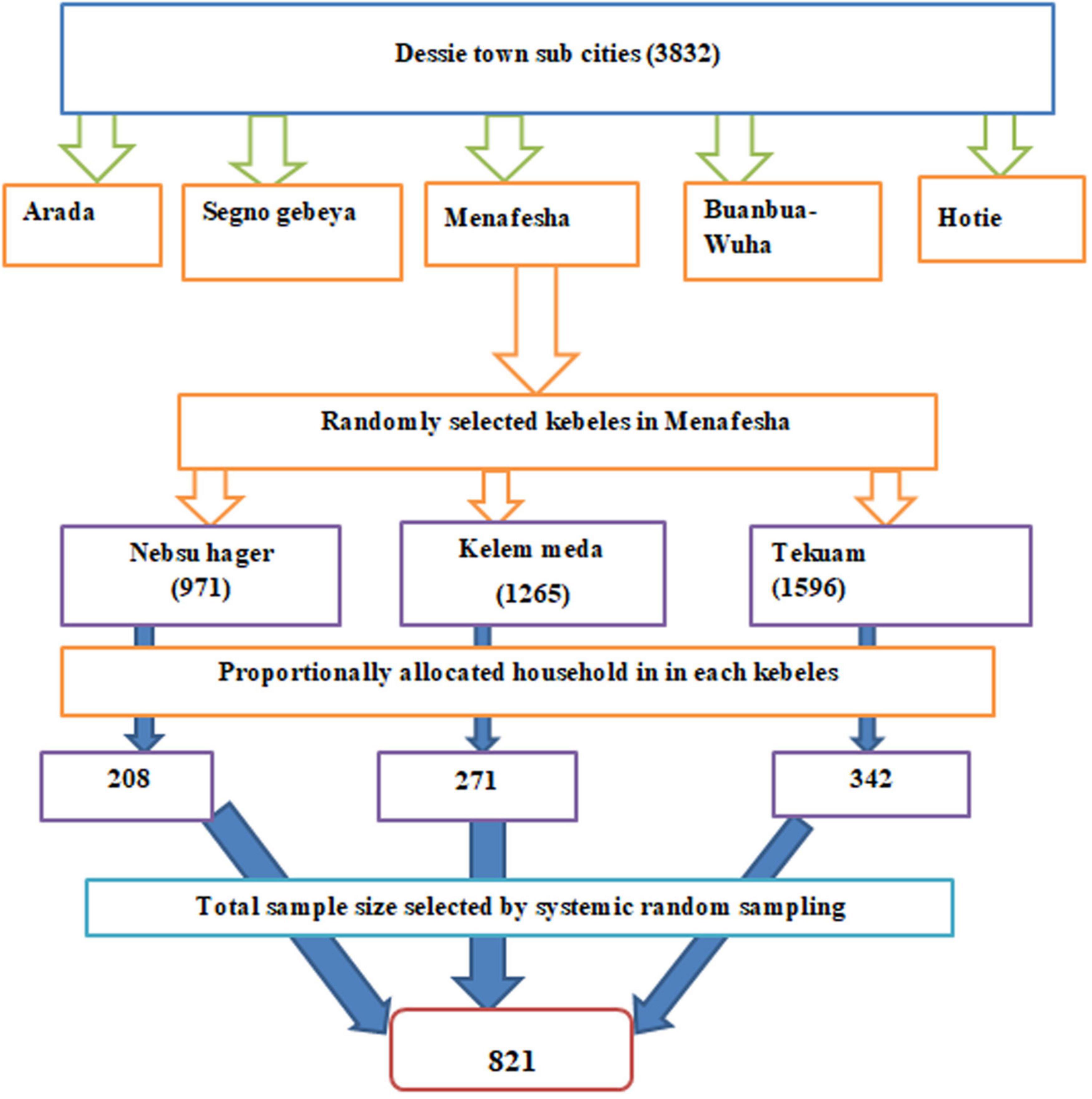
Figure 1. Schematic representation of sampling technique showing the number of selected samples from each sub-city of Dessie city, 2022 G. C.
Data collection method and technique
Data were collected by face-to-face interviews using a structured questionnaire. PTSD was measured by using a 20-item post-traumatic checklist (PCL-5) with scores ranging from 0 to 80 with a five-point Likert scale (0 = Not at all, 1 = A little bit, 2 = moderately, 3 = Quite a bit, 4 = extremely). A score of ≥ 33 was considered a symptom of PTSD (28). The PCL-5’s validity and reliability have been examined and demonstrated in several nations, including Iraq (Cronbach’s alpha = 0.85) (29), and Zimbabwe (Cronbach’s alpha = 0.92) (30). The internal consistency (Cronbach alpha) of (PCL-5s) in this study was 0.87.
The Patient Health Questionnaire (PHQ-9) was used to assess depression, with a score of 10 or higher indicating depression (31). In several nations, the PHQ-9 validity and reliability have been evaluated and verified for usage in community studies (16). The perceived stress (PSS) scale, which has a 0–40 range, was used to quantify felt life threats. According to the PSS, respondents with scores between 0 and 13 had low perceived stress, those between 14 and 26 had moderate perceived stress, and those between 27 and 40 had high felt perceived stress (8). The internal consistency (Cronbach alpha) of (PHQ-9) and perceived stress scale (PSS) were 0.82, and 0.84, respectively.
The Social Support Scale (The Oslo three-items) (OSSS-3) was used to collect data regarding the strength of social support. It was categorized into three broad categories of social support; 3–8 poor social support, 9–11 moderate social support, and 12–14 strong social support (32). The internal consistency (Cronbach alpha) of Oslo-3 social support was 0.79. Anxiety was measured by a sub scale adapted from the Depression, Anxiety, and Stress Scale (DASS -21) with a score of 8 or more suggesting anxiety symptom (bib1). The WHO student drug-use questionnaire was used to measure substances (34). Socio-demographic factors, substance use history, clinical factors, and trauma-related factors were used on “yes/no” response questionnaires and were operationalized according to different works of literature.
Data collection procedures
The questionnaire was initially written in English, then translated into Amharic, and finally back into English to ensure uniformity. Additionally, we use standard tools to determine the outcome variable by giving 2 days of training for data collectors and supervisors. In the Hotie sub-city, 5% (n = 41) of the participants took part in the pre-test, which aimed to identify any potential issues with the data collection methods and suggest changes to the questionnaire. The principal investigator and supervisor regularly oversaw and assisted the data collectors. Every day during the period of data collection, supervisors and primary investigators verified the data for consistency and completeness.
Data processing and analysis
Data were checked and cleaned before being entered into the computer system using Epi-data version 3.1, and they were then exported to SPSS version 26 statistical software for additional analysis. The researchers employed frequency, proportion, and other descriptive statistics. To account for potential confounding effects, independent variables with a bivariable model p-value of less than 0.25 were added to the multivariable regression model. Hosmer and Lemeshow examined the fitness model to ensure its accuracy. The strength of the association was demonstrated by an odds ratio with a 95% CI for all factors in the multivariable model that had a p-value of less than 0.05. The final result was to report the findings in text, a table, or a graph. Tolerance and variance inflation factors were checked to test multicollinearity or to see the unique effect of predictors on outcome variables.
Results
Socio-demographic factors of the respondents
A total of 785 participants were involved in this study and the response rate was 95.6%. The mean age (SD) of the participants was 36.01 (± 11.29 years), and the majority of 447 (56.9%) were males. The majority of the participants, 521 (66.4%), 519 (66.1%), and 203 (25.9%) were married, Muslim, and had a University degree and above, respectively. The majority of the community were 249 (31.7%) merchants by occupation. According to the participant’s responses, 460 (58.6%) of respondents earned monthly income ≥ 2166 (ETB) (Table 1).
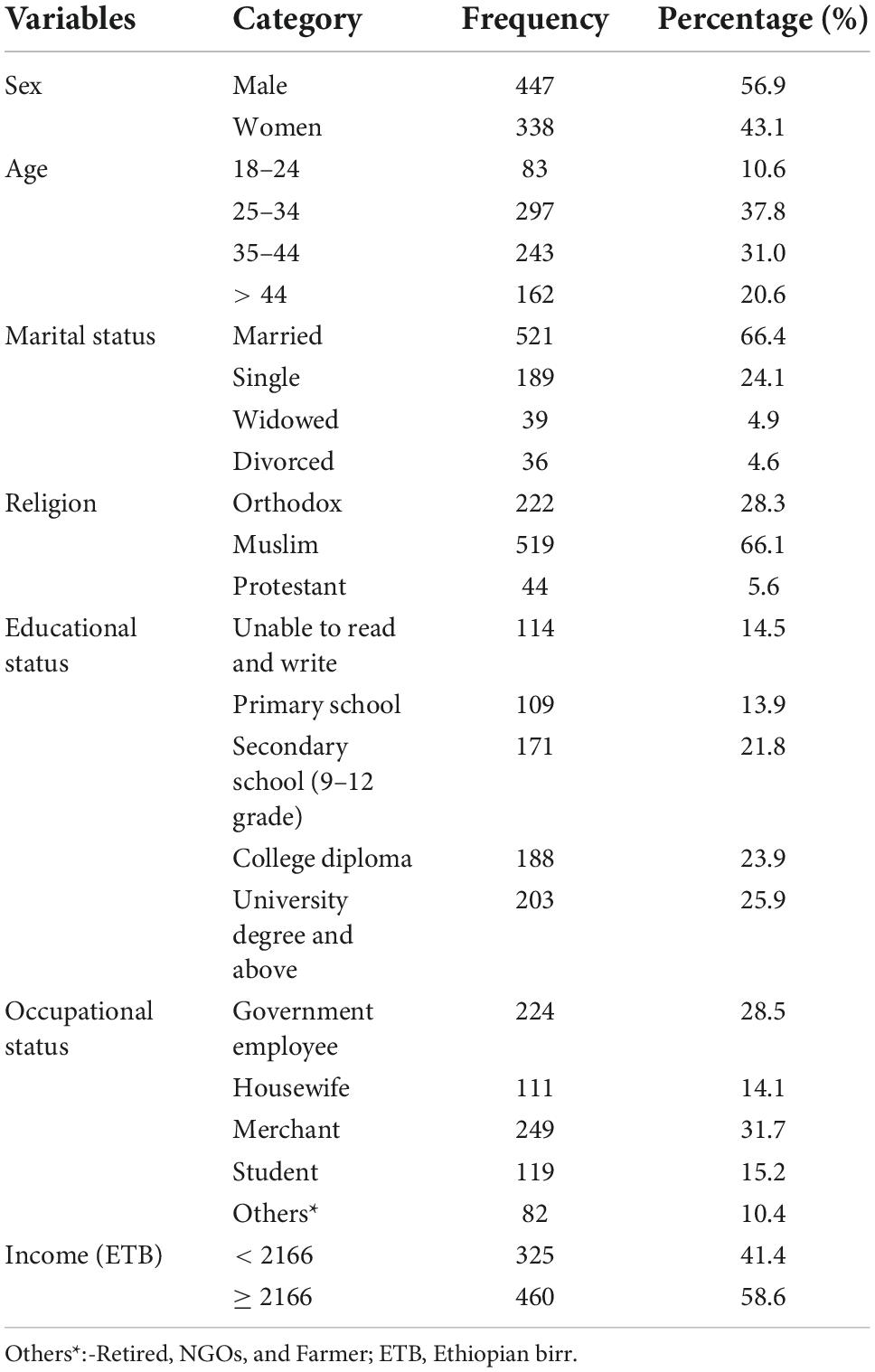
Table 1. Distribution of socio-demographic factors of Dessie town residents, Ethiopia, 2022 (N = 785).
Clinical related factors of the respondents
According to the current study, 40 (5.1%) of respondents had a history of mental illness. Among participants, 39 (5.0%) respondents had a family history of mental illness and 88 (11.2%) participants reported a history of chronic medical illness. Of the participants, 192 (24.5%), and 262 (33.4%) had depressive symptoms and anxiety symptoms, respectively (Table 2).
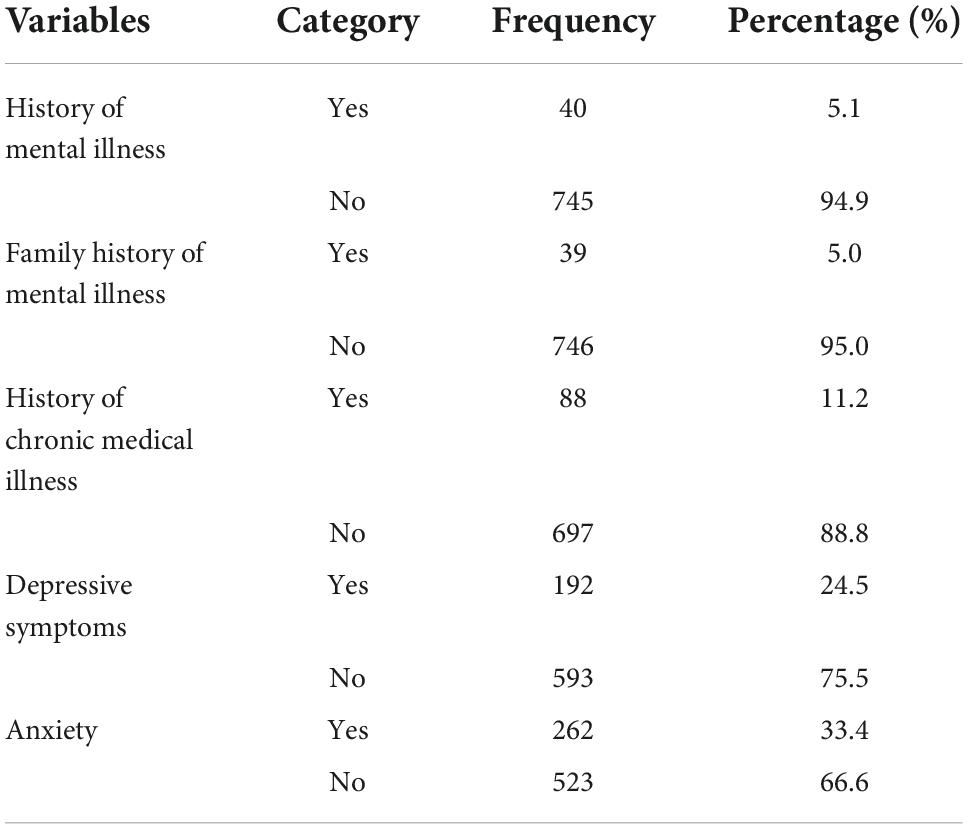
Table 2. Description of Clinical related factors of respondents among Dessie town residents, Ethiopia, 2022 (N = 785).
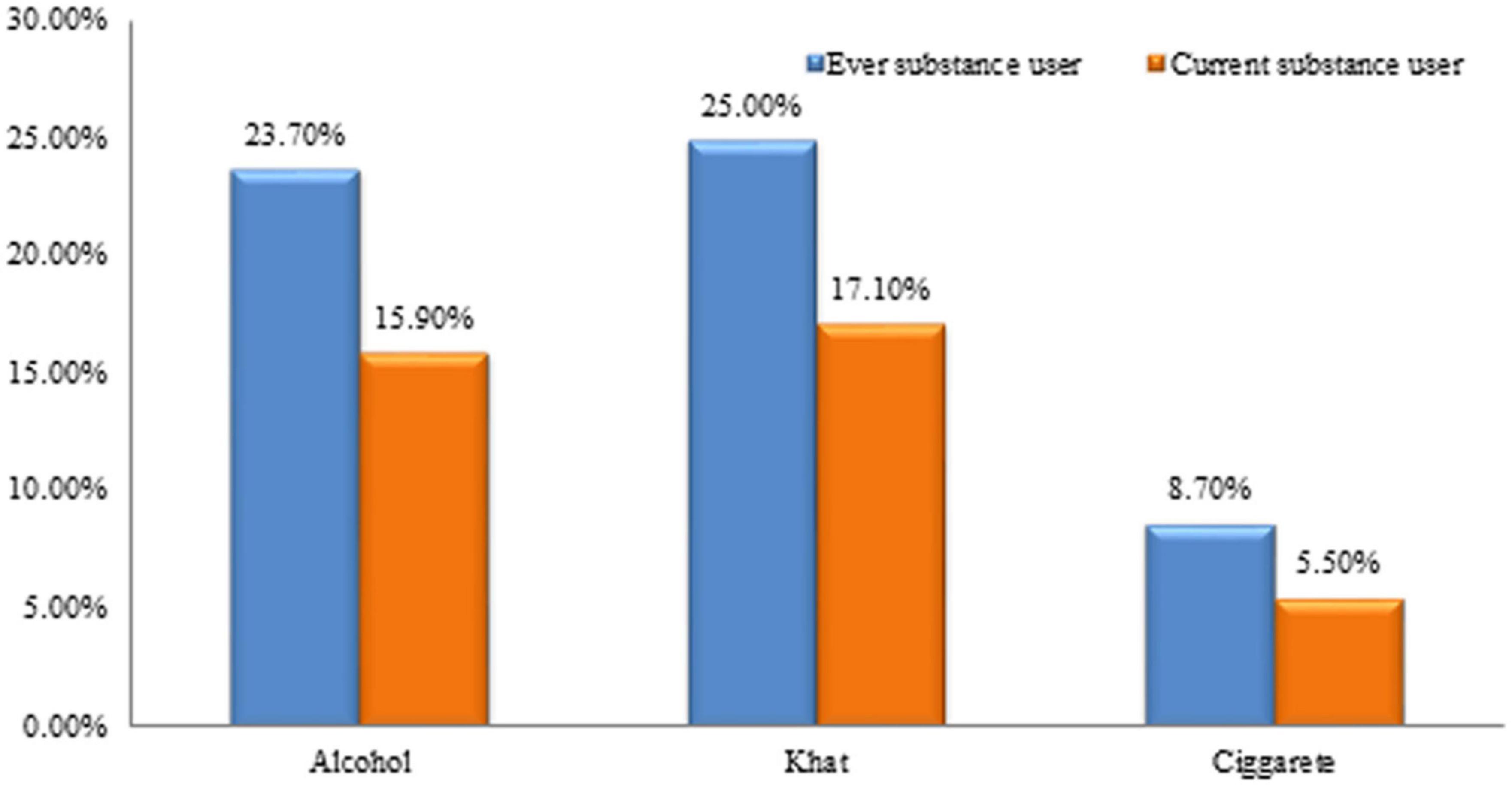
Substance-related factors of the respondents
Regarding the use of the substance, nearly one-fourth 186 (23.7%) had consumed alcohol, 196 (25%) had used khat, and 8.7% had smoked cigarettes in their lifetime. Whereas, 125 (15.9%) consumed alcohol, 134 (17.1%) use khat, and 43 (5.5%) smoke cigarette currently (Figure 2).
Trauma-related and psychosocial factors
Regarding individual trauma type, the type of trauma experienced by the community 72 (9.2%), 33 (4.2%), 66 (8.4%), and 116 (14.8%) were serious physical injury during the conflict, witness the death of a family member, witness a serious physical injury of a family member or friend, and property destroyed during the conflict, respectively. From this study, 120 (15.3%) had experienced childhood abuse, 357 (45.5%), had moderate perceived life threats and 420 (53.5%) had received threat intermittent social support (Table 3).
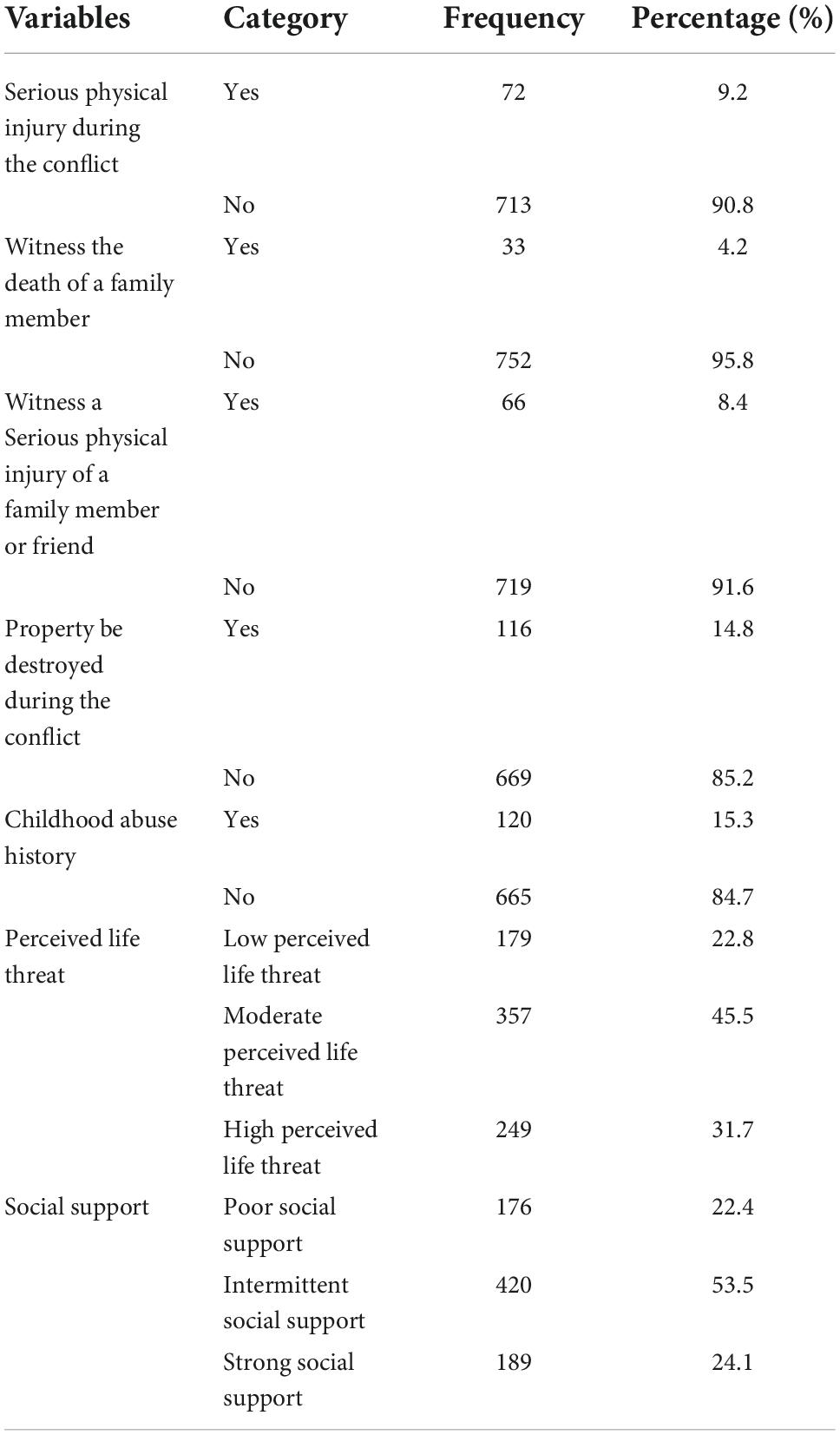
Table 3. Description of Trauma-related and psychosocial factors among Dessie town residents, Ethiopia, 2022 (N = 785).
Prevalence of posttraumatic disorder and associated factors among Dessie town residents
In this study, the overall prevalence of PTSD among people who experienced traumatic events in Dessie town was 19.4% [(95% CI, 16.7, 22.0)].
Factors associated with posttraumatic stress disorder factors among Dessie town residents
In the bivariate analysis, age, sex, history of mental illness, family history of mental illness, history of chronic medical illness, childhood abuse history, ever alcohol use, current alcohol use, serious physical injury during the conflict, witness the death of a family member, witness a serious physical injury of a family member or friend, the property be destroyed during the conflict, depressive symptoms, perceived life threat, and low social support showed a P–value of < 0.25 and became a candidate for multivariable analysis. Variables such as, being female, history of mental illness, depressive symptoms, witnessing a serious physical injury of a family member or friend, and high perceived life threat were found to be significantly associated with PTSD at a p-value less than 0.05. in multivariable analysis.
Females were 1.63 times more likely to develop PTSD than males (AOR = 1.63, 95% CI 1.10–2.44). Those participants who had a previous history of mental illness were 3.14 times more likely to develop PTSD as compared with respondents who did not have a history of mental illness (AOR = 3.14, 95% CI 1.14–7.06). Likewise, the odds of developing PTSD among those with depressive symptoms were 3.12 times higher as compared to their counterparts (AOR = 3.12, 95% CI 1.92–5.07). Those who had witnessed a serious physical injury of a family member or friend were 2.82 times more likely to develop PTSD than those who had not witnessed a serious physical injury of a family member or friend (AOR = 2.82, 95% CI 1.18–6.70). Finally, the odds of developing PTSD among participants who had experienced high perceived life threats were five times higher than those who had low perceived life threats (AOR = 5.73, 95% CI 3.05–10.78) (Table 4).
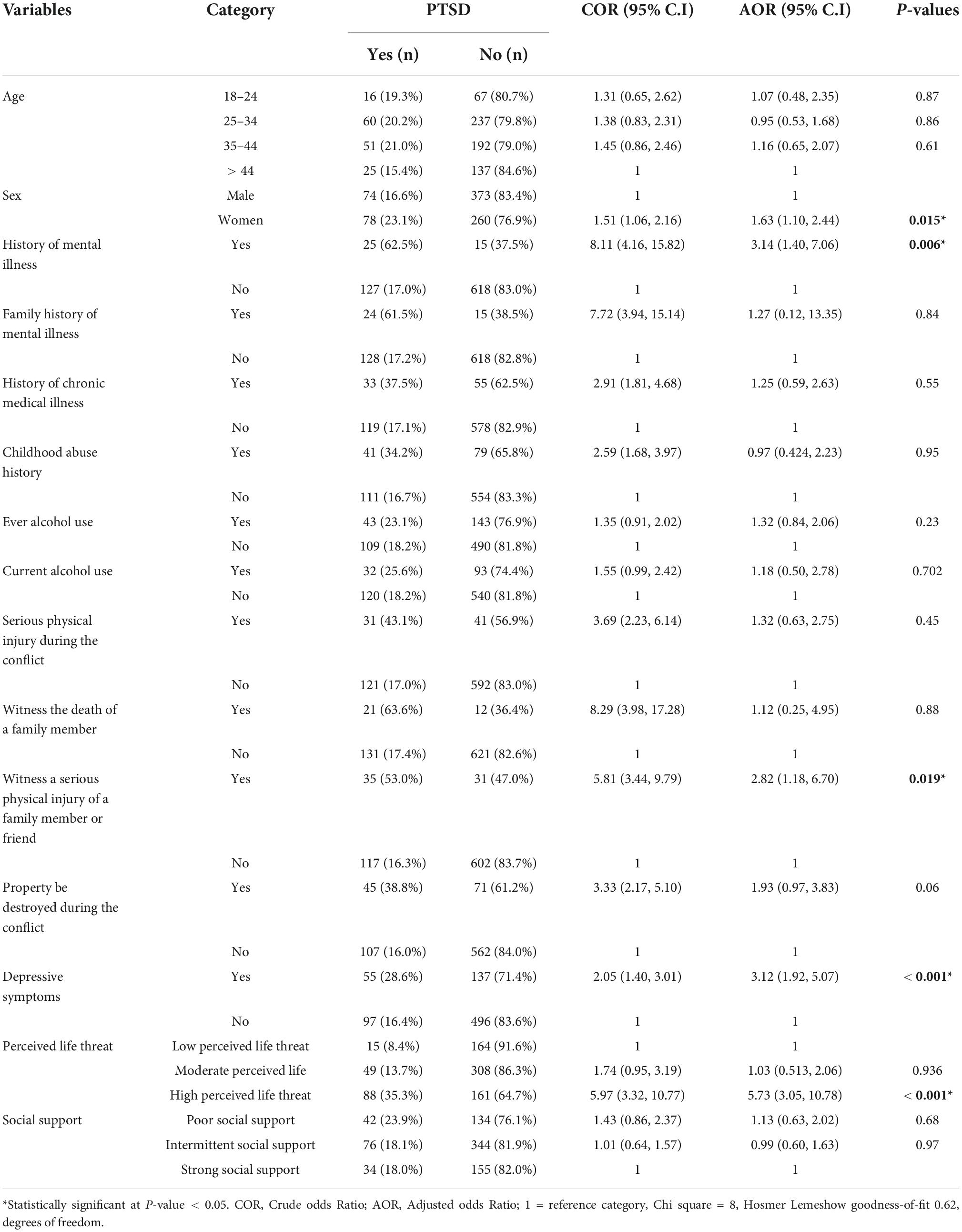
Table 4. Bivariate and multivariable logistic regression analysis results of posttraumatic stress disorder (PTSD) among Dessie town residents, Ethiopia, 2022 (N = 785).
Discussion
War is complex and potentially leads to ever-lasting trauma in the population (27). This population-based study aimed to assess the prevalence of PTSD in northern Etiopia following the civil war. The study showed a higher prevalence of PTSD in the study communities. Additionally, given the high prevalence of PTSD in the study communities, well-coordinated public mental health initiatives should be implemented. Since mental problems can impair people’s ability to operate normally and be productive members of society, reducing the burden of mental disorders, especially (PTSD), is essential (35).
The result of the current study indicated that the magnitude of PTSD among people who experienced traumatic events in Dessie town was 19.4% [(95% CI, 16.7, 22.0)]. The finding was congruent with the study carried out among traumatic Patients in West Ethiopia 17.1% (21), Serbia 18.8% (35), Diyarbakir, Turkey 21.4% (36), and Morocco 19.3% (18). On the other hand, this study’s finding was lower when compared with studies done in North West, Ethiopia 59.8% (16), internally displaced victims in Nigeria 63% (17), a community-based, cross-sectional study landslide survivors, Addis Ababa, Ethiopia 37.3% (22), South Sudan 28% (19), internally displaced people in South Ethiopia 58.4% (20), Palestine 68.9% (37), and Medellin Colombia 88% (26). The disparity could be explained by the population makeup of the participants. For instance, the Palestinian study was restricted to young people who were living in refugee camps during the Al-Aqsa intifada and who had significant injuries as a result of ongoing hostilities. Since the trauma was severe and persisted for a long time, this made the young people more vulnerable. Hence, numerous research has shown that the prevalence of PTSD increases along with the level of exposure to traumatic events, such as the quantity or intensity of the experienced events (16). Other potential causes of this discrepancy include the use of various measurement tools and cut-off points for PTSD, exposure to numerous trauma, study design, and the type and degree of the magnitude of the accidents exposed in the study.
This result was higher than those found in studies in Uganda 11.8% (23), Southern Brazil 9.1% (24), Sri Lanka 2.3% (25), and Sindh 9% (38). The discrepancy in the instruments could be the cause of this variation; in which in Uganda the mini-international neuropsychiatric interview (MINI) was used (23), Composite International Diagnostic Interview (CIDI) in Sri Lanka (25), structured interview using DSM-IV-TR in Sindh (38), whereas in this study the PCL-C was used, and extended standards criteria A which was modified with a better internal consistent in order to measure PTSD (28). Another reason might be the duration of exposure to traumatic events; the study was conducted in Uganda 7 years after the conflict, Sri Lanka was after 20 years of forced displacement, but the current study was conducted after 6 months of exposure to trauma. As a result, the lengthened exposure to the traumatic event was more likely to result in a reduction in magnitude due to recall bias. Furthermore the different types of trauma exposure, the sample methods, and sociocultural aspects. could be a reason for their variation.
Regarding the associated factors, females were 1.63 times more likely to develop PTSD than males. This finding was in agreement with different studies in South Africa (39), and two different studies in Ethiopia (16, 20). This might be because women are more likely than men to experience a lower threshold from exposure to psychotrauma, which increases their chance of developing PTSD (26). It may also be a result of the psychological effects of rape or sexual abuse, violent partner loss, higher rates of poverty, children, and being a single parent or widow than men (35). Another factor might be that females react to stress more emotionally and ruminatively than males do. This could make getting PTSD more likely (25).
In the current study, we found that participants who had a previous history of mental illness were 3.14 times more likely to develop PTSD as compared to those who did not have a history of mental illness. Similar to a finding of different studies from Kenya (40), and South Korea (41). In comparison to participants without a history of mental illness, individuals with a history may have higher neurochemical imbalance and neuronal damage. Therefore, stressful situations that persons who have neuron-chemical imbalance due to a history of psychiatric illness encounter speed up the onset of PTSD (35).
The odds of developing PTSD among those with depressive symptoms were 3.12 times higher as compared to their counterparts. This is similar to findings done in Kenya (40), Maikadra, Ethiopia 59.8% (16), and South Ethiopia (20). This may be due to the fact that participants with depressive symptoms are more likely than responders without depressive symptoms to have experienced traumatic events, which in turn raises the risk of developing PTSD (26). Another factor contributing to the higher likelihood of developing PTSD is having previously experienced depressive symptoms and other psychological problems (25).
This finding also revealed that participants who had witnessed a serious physical injury of a family member or friend were nearly three times more likely to develop PTSD than those who had not witnessed a serious physical injury of a family member or friend. This was supported by the study conducted in Bangladesh (39), and the Wenchuan earthquake in China (42). It is now widely recognized that witnessing traumatic events directly can lead to the development of post-traumatic stress disorder (PTSD). This may be the case because witnessing traumatic events can have effects that are similar to those of other trauma victims, such as re-experiencing the event, intrusive negative thoughts including ideas of retaliation, and it may have a big influence on emotional health (17).
Finally, the odds of developing PTSD among participants who had experienced high perceived life threats were five times higher than those who had low perceived life threats. A current study finding was congruent with a finding from North West, Ethiopia 59.8% (16), Koshe landslide in Addis Ababa, Ethiopia 37.3% (22), and South Korea (41). The onset and persistence of PTSD will be accelerated by negative views about the detrimental implications of the ongoing threat (43).
Limitations of the study
The use of a high response rate and the inclusion of significant variables that were left out of earlier research. Also, for measuring PTSD, we employed an updated standardized tool even it is not validated in Ethiopia. Additionally, to evaluate independent variables including depressive symptoms and perceived stress, validated and standardized instruments were used. Whereas; we were unable to conclude the causes of the connections we discovered because of the study’s cross-sectional nature. The research could not include the afflicted demographic as children in traumatic events, this is recommended for future researchers to perform their studies among this affected population. In addition, recall bias and social desirability may potentially be further limitations. Because the data was collected through a face-to-face interview, which could influence participants’ responses to socially acceptable questions about substances, people with PTSD symptoms may be more motivated to remember earlier exposure than those without the symptoms.
Conclusion
The current study showed a high prevalence of PTSD among people who experienced traumatic events in Dessie town. Being female, a previous history of mental illness, depressive symptoms, witnessing a serious physical injury of a family member or friend, and high perceived life threats were found to be significant predictors of PTSD. Therefore, mental health programs by local officials, psychologists, and non-governmental groups should be expanded for screening and providing treatment for all people suffering from PTSD to minimize the prevalence of this condition. In addition, mental health awareness campaigns for trauma victims to seek mental health treatment and intense and persistent psychosocial interventions should be provided.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee of Wollo University College of Medicine and Health Science with an ethical review board with an ethical review number (RCSPG-205/14). All study participants were told that participation was completely voluntary, that written informed consent was obtained, and that they could withdraw from the study at any time if they were not comfortable. A participant’s confidentiality and privacy were ensured by not including a personal identifier. All methods were performed in accordance with the relevant guidelines and regulations. The patients/participants provided their written informed consent to participate in this study.
Author contributions
TA was the principal investigator of the study and involved from inception to design acquisition of data analysis, interpretation, and drafting and preparing of the manuscript. YZ, MS, AA, and NB were involved in the reviewing of the proposal and critical review of the draft manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by Wollo University. The funders had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We would like to acknowledge Wollo University, the Dessie Town administration office for their cooperation to provide the necessary data about the study area. Finally, would like to say thank the study participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; DSM, Diagnostic Statistical Manual; ICD, International Classification of Disease; NGOs, Non-governmental organizations; OSSS-3, Social Support Scale; PCL, Post-traumatic Stress Disorder Checklist; PHQ-9, Patient Health Questionnaire; PSS, Perceived Stress Scale; PTSD, Post-traumatic Stress Disorder; SD, Standard deviation; SPSS, Statistical Package for Social Science; WHO, World Health Organization; YLD, Years of healthy life lost due to disability.
References
1. APA. Diagnostic and Statistical Manual of Mental Disorders Fifth Edition DSM-5. EDISI KE-5. Washington, DC: American Psychiatric Association (2013).
2. Monson CM, Shnaider P. Treating PTSD with Cognitive-Behavioral Therapies: Interventions that Work. Washington, DC: American Psychological Association (2014). doi: 10.1037/14372-000
3. Ayuso-Mateos JL. Global Burden of Post-Traumatic Stress Disorder in the Year 2000: Version 1 Estimates. Geneva: World Health Organization (2002).
4. Fortes S, Lopes CS, Villano LA, Campos MR, Gonçalves DA, Mari JJ. Common mental disorders in Petrópolis-RJ: a challenge to integrate mental health into primary care strategies. Braz J Psychiatry. (2011) 33:150–6. doi: 10.1590/S1516-44462011000200010
5. Hg L, Heather Graham L. How Common is PTSD. Washington, DC: National Center for PTSD (2015). 1 p.
6. Farhood L, Dimassi H, Lehtinen T. Exposure to war-related traumatic events, prevalence of PTSD, and general psychiatric morbidity in a civilian population from Southern Lebanon. J Transcult Nurs. (2006) 17:333–40. doi: 10.1177/1043659606291549
7. Hapke U, Schumann A, Rumpf H-J, John U, Meyer C. Post-traumatic stress disorder. Eur Arch Psychiatry Clin Neurosci. (2006) 256:299–306. doi: 10.1007/s00406-006-0654-6
8. Frans Ö, Rimmö PA, Åberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand. (2005) 111:291–9. doi: 10.1111/j.1600-0447.2004.00463.x
9. Hobfoll SE, Canetti-Nisim D, Johnson RJ, Palmieri PA, Varley JD, Galea S. The Association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to repeated acts of terrorism in Israel. J Trauma Stress. (2008) 21:9–21. doi: 10.1002/jts.20307
10. Silove D, Steel Z, Bauman A, Chey T, McFarlane A. Trauma, PTSD and the longer-term mental health burden amongst Vietnamese refugees. Soc Psychiatry Psychiatr Epidemiol. (2007) 42:467–76. doi: 10.1007/s00127-007-0194-z
11. Plaut M. The International Community Struggles to Address the Ethiopian Conflict. London: RUSI Newsbrief RUSI (2021).
12. Hoppen TH, Morina N. The prevalence of PTSD and major depression in the global population of adult war survivors: a meta-analytically informed estimate in absolute numbers. Eur J Psychotraumatol. (2019) 10:1578637. doi: 10.1080/20008198.2019.1578637
13. Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. (2009) 302:537–49. doi: 10.1001/jama.2009.1132
14. Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: a systematic review. Front Psychiatry. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
15. Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:672–9. doi: 10.1007/s00127-005-0943-9
16. Ali D, Azale T, Wondie M, Tadesse J. About six in ten survivors of the november 2020 Maikadra massacre suffer from posttraumatic stress disorder, Northwest Ethiopia. Psychol Res Behav Manag. (2022) 15:251. doi: 10.2147/PRBM.S338823
17. Taru MY, Bamidele LI, Makput DM, Audu MD, Philip TF, John DF, et al. Posttraumatic stress disorder among internally displaced victims of Boko Haram terrorism in north-eastern Nigeria. Jos J Med. (2018) 12:8–15.
18. Astitene K, Barkat A. Prevalence of posttraumatic stress disorder among adolescents in school and its impact on their well-being: a cross-sectional study. Pan Afr Med J. (2021) 39:54. doi: 10.11604/pamj.2021.39.54.27419
19. Ayazi T, Lien L, Eide AH, Ruom MM, Hauff E. What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BMC Psychiatry. (2012) 12:175. doi: 10.1186/1471-244X-12-175
20. Madoro D, Kerebih H, Habtamu Y, Mokona H, Molla A, Wondie T, et al. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. (2020) 16:2317. doi: 10.2147/NDT.S267307
21. Golja EA, Labata BG, Mekonen GF, Dedefo MG. Post-traumatic stress disorder and associated factors among traumatic patients attended in four government hospitals, West Ethiopia. Open Public Health J. (2020) 13:576–81. doi: 10.2174/1874944502013010576
22. Asnakew S, Shumet S, Ginbare W, Legas G, Haile K. Prevalence of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ Open. (2019) 9:e028550. doi: 10.1136/bmjopen-2018-028550
23. Mugisha J, Muyinda H, Wandiembe P, Kinyanda E. Prevalence and factors associated with posttraumatic stress disorder seven years after the conflict in three districts in northern Uganda (The Wayo-Nero Study). BMC Psychiatry. (2015) 15:170. doi: 10.1186/s12888-015-0551-5
24. Brunnet AE, Bolaséll LT, Weber JL, Kristensen CH. Prevalence and factors associated with PTSD, anxiety and depression symptoms in Haitian migrants in southern Brazil. Int J Soc Psychiatry. (2018) 64:17–25. doi: 10.1177/0020764017737802
25. Husain F, Anderson M, Cardozo BL, Becknell K, Blanton C, Araki D, et al. Prevalence of war-related mental health conditions and association with displacement status in postwar Jaffna District, Sri Lanka. JAMA. (2011) 306:522–31. doi: 10.1001/jama.2011.1052
26. Richards A, Ospina-Duque J, Barrera-Valencia M, Escobar-Rincón J, Ardila-Gutiérrez M, Metzler T, et al. Posttraumatic stress disorder, anxiety and depression symptoms, and psychosocial treatment needs in Colombians internally displaced by armed conflict: a mixed-method evaluation. Psychol Trauma. (2011) 3:384. doi: 10.1037/a0022257
27. Hankins MS. International Federation of Red Cross and Red Crescent Societies. Geneva: IFRC (2015).
28. Ben-Zion Z, Fine NB, Keynan NJ, Admon R, Green N, Halevi M, et al. Cognitive flexibility predicts PTSD symptoms: observational and interventional studies. Front Psychiatry. (2018) 9:477. doi: 10.3389/fpsyt.2018.00477
29. Ibrahim H, Ertl V, Catani C, Ismail AA, Neuner F. The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry. (2018) 18:259. doi: 10.1186/s12888-018-1839-z
30. Verhey R, Chibanda D, Gibson L, Brakarsh J, Seedat S. Validation of the posttraumatic stress disorder checklist–5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry. (2018) 18:109. doi: 10.1186/s12888-018-1688-9
31. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
32. Lecic-Tosevski D, Pejuskovic B, Miladinovic T, Toskovic O, Priebe S. Posttraumatic stress disorder in a Serbian community: Seven years after trauma exposure. J Nerv Ment Dis. (2013) 201:1040–4.
33. Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-u
34. Essizoglu A, Keser I. Post-traumatic stress disorder in internally displaced people subjected to displacement by armed forces. J Trauma Stress Disor Treat. 2014 3:2–6.
35. Lecic-Tosevski D, Pejuskovic B, Miladinovic T, Toskovic O, Priebe S. Posttraumatic stress disorder in a Serbian community: seven years after trauma exposure. J Nervous Mental Dis. (2013) 201:1040–4. doi: 10.1097/NMD.0000000000000051
36. Essizoglu A, Keser I. Post-traumatic stress disorder in internally displaced people subjected to displacement by armed forces. J Trauma Stress Disor Treat. (2014) 3:2–6.
37. Pham PN, Weinstein HM, Longman T. Trauma and PTSD symptoms in Rwanda: implications for attitudes toward justice and reconciliation. JAMA. (2004) 292:602–12. doi: 10.1001/jama.292.5.602
38. Rahman, A, Akhtar, P, Siddiqui, M. Psychological effects among internally displaced persons (IDPS) residing in two districts of Sindh. Med Forum Mon. (2013) 24:82–4.
39. Ndungu J, Ramsoomar L, Willan S, Washington L, Ngcobo-Sithole M, Gibbs A. Depression, posttraumatic stress disorder (PTSD) and their comorbidity: implications of adversity amongst young women living in informal settlements in Durban. South Africa. J Affect Disord Rep. (2020) 1:100022. doi: 10.1016/j.jadr.2020.100022
40. Jenkins R, Othieno C, Omollo R, Ongeri L, Sifuna P, Mboroki JK, et al. Probable post traumatic stress disorder in Kenya and its associated risk factors: a cross-sectional household survey. Int J Environ Res Public Health. (2015) 12:13494–509. doi: 10.3390/ijerph121013494
41. Song JY, Jeong K-S, Choi K-S, Kim M-G, Ahn Y-S. Psychological risk factors for posttraumatic stress disorder in workers after toxic chemical spill in Gumi, South Korea. Workplace Health Saf. (2018) 66:393–402. doi: 10.1177/2165079917750168
42. Zhou X, Kang L, Sun X, Song H, Mao W, Huang X, et al. Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Compr Psychiatry. (2013) 54:493–9. doi: 10.1016/j.comppsych.2012.12.010
Keywords: Dessie town, post-traumatic stress disorder, depression, Ethiopia, stress
Citation: Anbesaw T, Zenebe Y, Asmamaw A, Shegaw M and Birru N (2022) Post-traumatic stress disorder and associated factors among people who experienced traumatic events in Dessie town, Ethiopia, 2022: A community based study. Front. Psychiatry 13:1026878. doi: 10.3389/fpsyt.2022.1026878
Received: 24 August 2022; Accepted: 06 October 2022;
Published: 25 October 2022.
Edited by:
S. M. Yasir Arafat, Enam Medical College, BangladeshReviewed by:
Mohammed Abdu Seid, Debre Tabor University, EthiopiaAmir Mohsen Rahnejat, AJA University of Medical Sciences, Iran
Copyright © 2022 Anbesaw, Zenebe, Asmamaw, Shegaw and Birru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tamrat Anbesaw, dGFtcmF0YW5iZXNhd0BnbWFpbC5jb20=
 Tamrat Anbesaw
Tamrat Anbesaw Yosef Zenebe
Yosef Zenebe Amare Asmamaw
Amare Asmamaw Maregu Shegaw
Maregu Shegaw Nahom Birru
Nahom Birru