
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 09 November 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1026032
Background: The relationship between allergic diseases (AD) and mental disorders (MD) in women has not been fully systematically evaluated. We aimed at validating this correlation.
Methods: The relevant cohort and case-control studies from the establishment of the database to February 18, 2022 in PubMed, Embase, and Cochrane library were searched by computer. The researchers conducted the quality evaluation of the included articles by reviewing and discussing with reference to relevant standards, and conducted the analysis of the correlation between female patients with AD and MD by using Review Manager 5.4.
Results: Six observational studies from 2631 studies (n = 1160858 women) were assessed as medium and high-quality studies. The meta-analysis demonstrated that AD was correlated with MD in female patients (OR = 1.21, 95%CI: 1.14–1.29), including asthma (OR = 1.16, 95%CI: 1.11–1.22), allergic rhinitis (OR = 1.31, 95%CI: 1.06–1.63), and atopic dermatitis in women (OR = 1.37, 95%CI: 1.24–1.50) were associated with MD. At the same time, subgroup analysis was performed according to region, study design, criteria of AD and MD, and the results demonstrated that both AD and MD were correlated in these different conditions.
Conclusion: Allergic diseases in female patients do have an association with mental disorders.
Systematic review registration: [https://www.crd.york.ac.uk/PROSPERO/], identifier [CRD42022311146].
Allergic diseases (AD) are a series of health issues that are widely concerned worldwide. The incidence rate of AD is increasing year by year. Heredity and environment are the main pathogenic factors, while pathogenesis is mainly “T helper type 2 immune response” (1). In addition, “atopic march” is more common in AD (2). Among these, the global incidence rate of allergic rhinitis (AR) is 10–40% (3), atopic dermatitis and asthma also affect 230 million and 300 million people worldwide (4, 5). According to existing research, allergies gradually become serious with the growing of girls, so lifelong allergic diseases are more obvious in women (6).
Mental disorders (MD) are a global problem, which have a crucial impact on human health. They usually include depression, anxiety, etc. (7). The prevalence of depression and anxiety in women is 1.5–2.5 times higher than that in men (8). Additionally, gender-specific disorders are more significant in women, such as perinatal MD (9). It is reported that the disease mechanism of inflammatory dysregulation may lead to MD (10, 11). Thus, the possible association between AD and MD has been widely concerned by society.
The association between AD and MD has been controversial in recent years. One study showed a correlation between AR and depression (5). Another studies illustrated that patients with atopic dermatitis had a higher incidence of depression than those with non-atopic dermatitis (12). In addition, the study found that women with depression or anxiety had a higher incidence of uncontrolled asthma during pregnancy than women without depression or anxiety. The incidence of uncontrolled asthma during at least one or more than two study visits was 52.9% vs. 32.7% and 23.5% vs. 9.6%, respectively (13). It was reported that major depressive disorder had more adverse effects on the severity of asthma and AR than non-major depressive disorder (14). Nevertheless, a systematic evaluation found that asthma did not have an association with depression (15). Another prospective study found no association between AD and depression (16). In conclusion, the existing systematic evaluation mainly targets a class of diseases in AD and MD, and there is a lack of studies specifically on women. At present, the relationship between female AD and MD has not been clarified. Therefore, this study intends to examine the association by analyzing existing observational studies.
The preferred reporting items for systematic review and meta-analysis (PRISMA) were used in this study (17). We registered on the PROSPERO (NO. CRD42022311146).
English articles published in PubMed, Embase and Cochrane Library from inception to February 18, 2022, were searched. The combination of subject words and free words is adopted. Search terms include mental disorder terms (“mental disorder,” “psychiatric disorder,” “psychiatric diagnosis,” etc.) and terms of allergy and atopic diseases (“allergic rhinitis,” “asthma,” “hay fever,” “Eczema,” “atopic dermatitis,” etc.) and female terms (“women,” “girls,” “women’s group,” etc.) and related terms (“risk,” “mortality,” “cohort,” etc.). Meanwhile, we also discuss the references in the main study with peer experts for additional reference information.
After eliminating the repeated and irrelevant articles, two researchers screened out the articles that met the standard by reading the title, the abstract, and the full text to finally determine the included articles. In case of disagreement and consensus cannot be resolved, a third researcher will assist in the review. Furthermore, if more information is required, we will contact the relevant authors to obtain it. We formulated the following inclusion criteria: (1) the type of study was an observational study (cohort study and case-control study); (2) the subjects were female patients with AD and MD; (3) comparison with the control group was involved; (4) it had scientific disease diagnostic criteria; (5) data such as odds ratio (OR) or relative rate (RR) and 95% confidence interval (CI) could be obtained. We excluded studies under the following circumstances: (1) articles published repeatedly or unable to obtain the full text; (2) data was incomplete or cannot be converted; (3) review, conference abstract, case report, and animal experiments; (4) study design, outcome indicators, and themes were inconsistent with the study; (5) there was no scientific diagnostic criteria for the disease.
A researcher extracted the information included in the study, including (1) basic information such as author, year, country, participant, and age; (2) study design and source of case samples; (3) diagnostic criteria for AD and MD. It was subsequently reviewed by another researcher, and differences were resolved through discussion, with the assistance of a third researcher. The quality of the included studies was evaluated by the Newcastle Ottawa scale (NOS) (18). There were three parts, including eight items, with a total score of 9 points. A score of ≥7 was rated as high quality, otherwise as low to medium quality. The evaluation was accomplished by two researchers reaching a consensus through discussion.
Review Manager 5.4 was used for meta-analysis of the included studies. Effect sizes of OR were pooled using generic inverse variance. Heterogeneity was indicated by I2 test. For low-degree heterogeneity (P < 0.10 and I2< 50%), the fixed-effects model was used. Otherwise, the random-effects model was selected (P < 0.10 and I2≥ 50%). Meanwhile, the source of heterogeneity was determined by subgroup and sensitivity analysis. If more than ten articles were included, the funnel plot was used to analyze the risk of bias.
A total of 2631 articles (Embase 2498, Cochrane 96, PubMed 37) were initially detected through database retrieval, of which 23 duplicate articles were excluded. After reading the title and abstract, 2564 articles were excluded, and the remaining 44 articles were reviewed in full text. Finally, a total of 6 articles were included for analysis (Figure 1) (13, 19–23).
The 6 articles were published for 2014-2021 years, and all participants were women, with 189-846155 participants, respectively, from North America (Canada and USA) (19, 21, 23), Asia (Korea and Taiwan, China) (20, 22), and Oceania (Australia) (13). The age is 15-50 years old (19–22), but this information went unreported in 2 articles (13, 23). The included studies are all observational studies, five of which were cohort studies (13, 19, 21–23), and one was case-control study (20). Furthermore, the diagnostic criteria for AD include physician diagnosis (19–23) and questionnaire (13). The diagnostic criteria for MD include self-report (13), questionnaire (13, 22, 23) and physician diagnosis (19–21) (Table 1).
The quality of included studies was evaluated according to NOS. There were 5 articles of high quality, and the other one (22) was rated as medium quality, due to the exposed group was not representative and merely Korean feminine nurses were taken as the research object (Tables 2, 3).
The correlation between AD and MD was analyzed for the 6 included articles (13, 19–23), and significant heterogeneity was found through test (I2 = 81%, P < 0.001). The analysis of random-effects model showed that AD in female patients was correlated with MD (OR = 1.21, 95%CI: 1.14–1.29, P < 0.001) (Figure 2). Considering that the causes of significant heterogeneity were related to different types of included diseases and low quality of literature. Therefore, a moderate-quality study of Kim (22) was excluded by the sensitivity analysis, and the results showed that OR = 1.17, 95%CI: 1.11–1.23, P < 0.001, and heterogeneity decreased (I2 = 72%, P = 0.007) (Figure 3). Excluding the studies of Yang and Kim (20, 22) with inconsistent disease types, the sensitivity analysis showed that OR = 1.14, 95%CI: 1.10–1.18, P < 0.001, and heterogeneity significantly decreased (I2 = 58%, P = 0.07) (Figure 4).
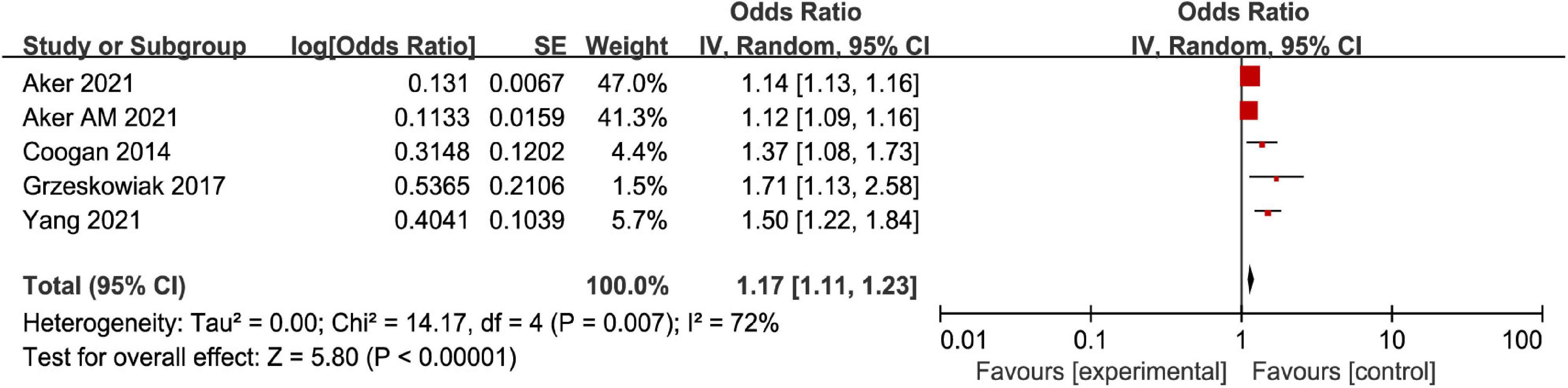
Figure 3. Forest map of association meta-analysis between AD and MD—Only relatively high-quality studies were included.
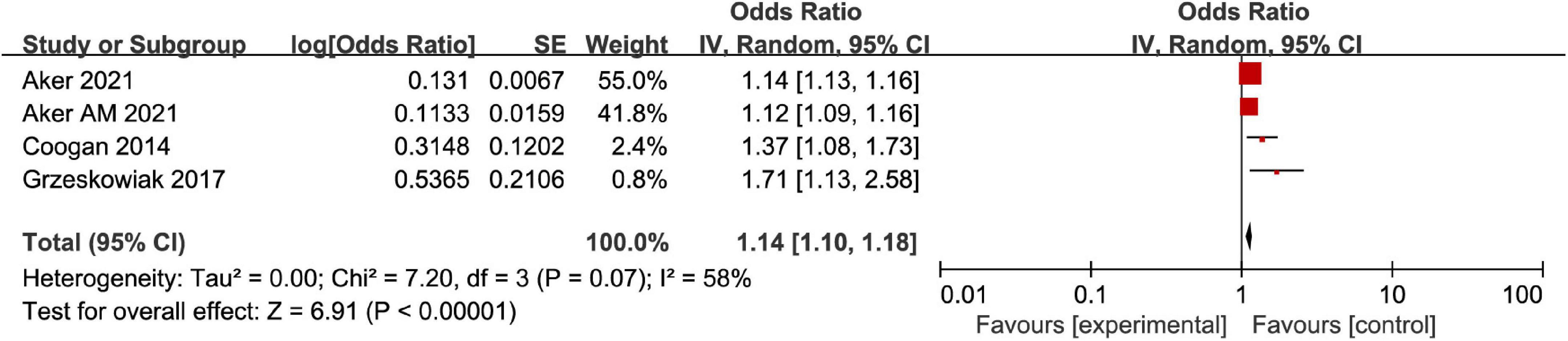
Figure 4. Forest map of association meta-analysis between AD and MD—Only studies of the same disease type were included.
For different disease types of AD, the subgroup analysis illustrated heterogeneity in the asthma group (I2 = 69%, P = 0.01), and asthma was associated with MD (OR = 1.16, 95%CI: 1.11–1.22, P < 0.001). There was heterogeneity in AR group (I2 = 74%, P = 0.05), and the incidence of mental disorders in AR group was higher than that in non-AR control group (OR = 1.31, 95%CI: 1.06–1.63, P = 0.01). There was no significant heterogeneity in the atopic dermatitis group (I2 = 0%, P = 0.38), and atopic dermatitis was associated with MD (OR = 1.37, 95%CI: 1.24–1.50, P < 0.001). Therefore, female patients with AD were correlated with MD (Figure 5).
Meanwhile, we conducted subgroup analysis of region, study design, criteria of AD and MD, and the results demonstrated that under the different conditions mentioned above, AD and MD were correlated. Furthermore, in the region and criteria of MD subgroup analysis, we found that Asian region (OR = 1.38, 95%CI: 1.26–1.50, P < 0.00; I2 = 0%) and questionnaire for diagnosis of MD (OR = 1.37, 95%CI: 1.25–1.49, P < 0.001; I2 = 0%) without significant heterogeneity (Table 4).
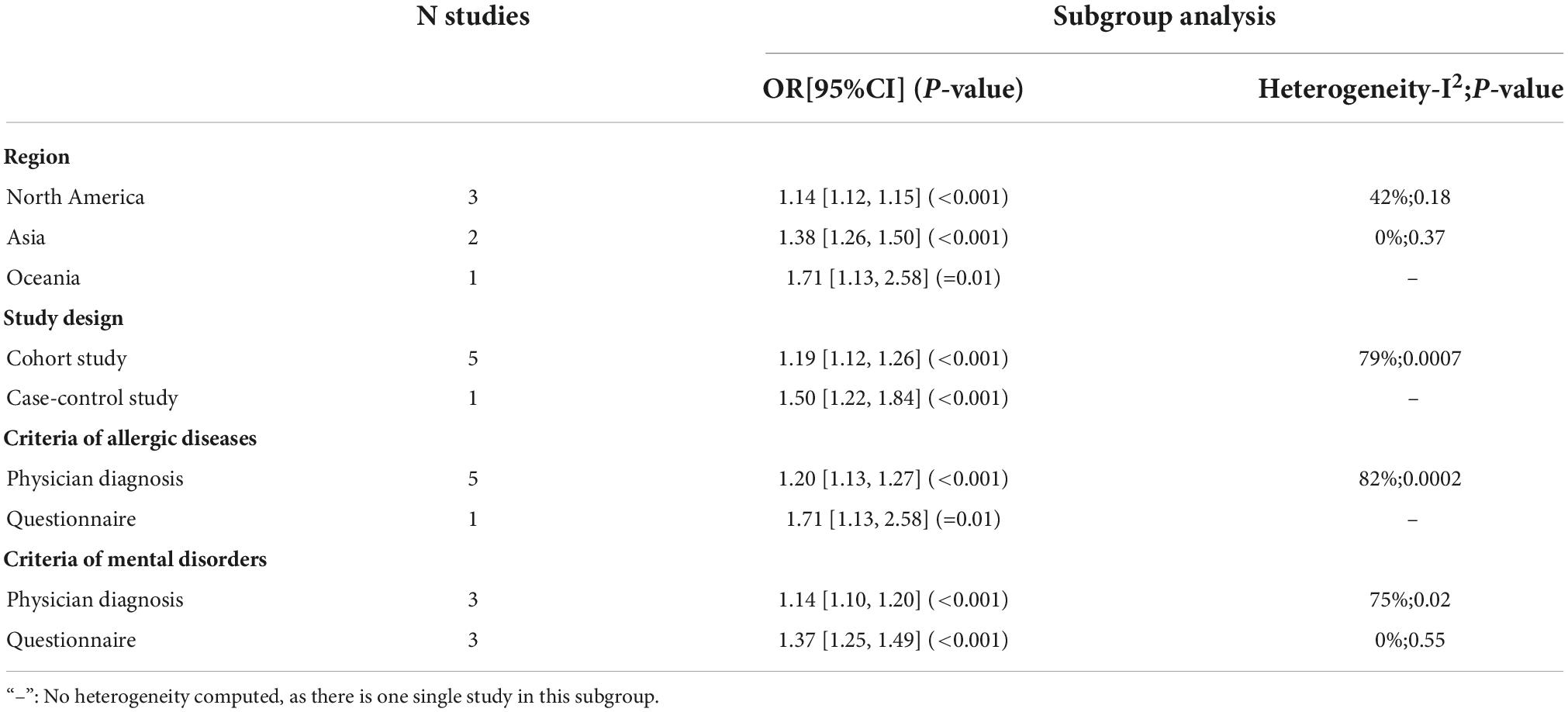
Table 4. Meta-analytical results and results of the subgroup analyses on the association between allergic diseases and mental disorders.
A previous meta-analysis found that adolescents with atopic dermatitis took a higher risk of MD in comparison with non-atopic dermatitis (OR = 1.652; 95% CI: 1.463–1.864) (24). Another systematic evaluation found that AR was associated with MD, and the risk of anxiety and depression in AR patients was higher than that in the non-AR group (25). Moreover, a systematic evaluation of the association between asthma and anxiety was conducted in 2021 based on observational studies, which found the association between asthma and anxiety disorders (OR = 2.08; 95% CI: 1.70–2.56) (26). Nevertheless, the above meta-analysis was limited to one or two types of diseases and failed to conduct a comprehensive review of a series of disease problems and gender factors. At present, there is still a lack of comprehensive evaluation of the relationship between AD and MD in women. Therefore, based on six observational studies, the systematic evaluation in this work found a correlation between AD and MD in women. In addition, subgroup analysis also illustrated that women with AD did have an association with MD. Among them, asthma, atopic dermatitis and AR were mainly associated with depression (13, 19, 20, 22, 23). Secondly, AR and atopic dermatitis would also be combined with sleep disorders (22). Women with asthma were also accompanied by other MD, such as anxiety disorders (13, 19). In addition, depression/anxiety in MD had the strongest correlation with uncontrolled asthma during pregnancy (RR = 1.71, 95%CI: 1.13–2.58) (13).
At present, the pathogenesis of AD is still being explored. Some theories suggest that inflammatory cytokines (tumor necrosis factor-α, interleukin, etc.) in AD bound to receptors on nerve cells, which can reduce the volume of gray matter in the hippocampus and thus have an impact on depression (27). Besides, the hypothalamic-pituitary-adrenal (HPA) axis activated in the course of inflammation is also associated with MD such as depression (28). Moreover, α-amylase and salivary cortisol, as well as a common NR3C1 gene, are found to correlate asthma with anxiety (29, 30). Of course, the sex-specific disease is also more and more apparent in women, particularly perinatal women. With the change in hormone level and immune function, the susceptibility to MD is gradually obvious (31). Therefore, society pays special attention to the relationship between female AD patients and MD. Clinically, we should first understand whether women with AD have a medical history and family history related to MD, so as to carry out comprehensive treatment. Secondly, especially for perinatal women, AD should be monitored and intervened in time to avoid the emergence of postpartum MD. Furthermore, treatment modalities that may cause side effects on the mental system should be avoided when treating AD. Finally, in addition to the use of medication, effective psychological intervention measures should be taken to prevent the emergence of self-harm or suicide.
This systematic evaluation is mainly aimed at the female group at first. The perinatal women and professional women are comprehensive evaluated, so as to explore the impact of disease on women. Secondly, the diseases studied are not limited to a single type, but a larger range of diseases are discussed for AD and MD, and a series of diseases such as AR, anxiety, and depression are comprehensively analyzed. Thirdly, all the included studies were rated as medium and high quality after NOS quality evaluation. Fourthly, compared with the 106813 samples studied by Ye et al. (26), we analyzed more than 1.16 million participants, involving Asia, North America, Oceania and other regions around the world, which provided a reliable and sufficient basis for this meta-analysis.
This study also has the following limitations. First, the observational studies principally focused on cohort studies and involved merely one case-control study. Second, AD was predominant in asthma. The relevant AR and atopic dermatitis solely involved two studies respectively, and the severity of the disease was not analyzed. Third, the OR, RR and 95%CI obtained from the paper failed to completely exclude relevant confounding factors. Fourth, there may be some bias in reviewing only those published in English and excluding other forms of reporting. Fifth, three of the six articles used questionnaire assessment in the criteria of MD.
In conclusion, our meta-analysis finds a significant association between AD (AR, asthma, and atopic dermatitis) and MD in women. Future studies require adjusting for confounding variables and include a larger number of high-quality studies. Additionally, multi-center randomized controlled trials are needed to further explore pathogenesis and clinical prevention and treatment of the disease.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
LL and SP participated in the design of this study. MZ, XA, and HL discussed and screened the literature. LL was responsible for data analysis and writing. CL and SP were responsible for revising and reviewing the manuscript. All authors contributed to the article and approved the submitted version.
This project was supported by Sichuan Provincial Administration of Traditional Chinese Medicine Science and Technology Research Special Project (2021MS098), Technology Innovation Research and Development Project of Chengdu Science and Technology Bureau (2021-YF05-01940-SN), and the Key R&D Project of Science and Technology Department of Sichuan Province (2022YFS0414).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Stark JM, Coquet JM, Tibbitt CA. The role of PPAR-γ in Allergic Disease. Curr Allergy Asthma Rep. (2021) 21:45. doi: 10.1007/s11882-021-01022-x
2. Paller AS, Spergel JM, Mina-Osorio P, Irvine AD. The atopic march and atopic multimorbidity: Many trajectories, many pathways. J Allergy Clin Immunol. (2019) 143:46–55. doi: 10.1016/j.jaci.2018.11.006
3. Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. (2017) 140:950–8. doi: 10.1016/j.jaci.2017.03.050
4. Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. (2018) 4:1. doi: 10.1038/s41572-018-0001-z
5. Lu Z, Chen L, Xu S, Bao Q, Ma Y, Guo L, et al. Allergic disorders and risk of depression: A systematic review and meta-analysis of 51 large-scale studies. Ann Allergy Asthma Immunol. (2018) 120:310–7. doi: 10.1016/j.anai.2017.12.011
6. Rosário CS, Cardozo CA, Neto HJC, Filho NAR. Do gender and puberty influence allergic diseases? Allergol Immunopathol (Madr). (2021) 49:122–5. doi: 10.15586/aei.v49i2.49
7. Aftab A, Joshi Y, Sewell D. Conceptualizations of mental disorder at a US Academic Medical Center. J Nerv Ment Dis. (2020) 208:848–56. doi: 10.1097/NMD.0000000000001227
8. Cantwell R. Mental disorder in pregnancy and the early postpartum. Anaesthesia. (2021) 76:76–83. doi: 10.1111/anae.15424
9. Silva BPD, Neves PAR, Mazzaia MC, Gabrielloni MC. Common mental disorders and perinatal depressive symptoms: an integrative review. Rev Bras Enferm. (2020) 73:e20190823. doi: 10.1590/0034-7167-2019-0823
10. Hussain S, Ronaldson A, Arias de la Torre J, Sima RM, Hatch S, Hotopf M, et al. Depressive and anxiety symptomatology among people with asthma or atopic dermatitis: A population-based investigation using the UK Biobank data. Brain Behav Immun. (2020) 90:138–44. doi: 10.1016/j.bbi.2020.08.003
11. Trikojat K, Luksch H, Rösen-Wolff A, Plessow F, Schmitt J, Buske-Kirschbaum A. “Allergic mood” - Depressive and anxiety symptoms in patients with seasonal allergic rhinitis (SAR) and their association to inflammatory, endocrine, and allergic markers. Brain Behav Immun. (2017) 65:202–9. doi: 10.1016/j.bbi.2017.05.005
12. Patel KR, Immaneni S, Singam V, Rastogi S, Silverberg JI. Association between atopic dermatitis, depression, and suicidal ideation: A systematic review and meta-analysis. J Am Acad Dermatol. (2019) 80:402–10. doi: 10.1016/j.jaad.2018.08.063
13. Grzeskowiak LE, Smith B, Roy A, Schubert KO, Baune BT, Dekker GA, et al. Impact of a history of maternal depression and anxiety on asthma control during pregnancy. J Asthma. (2017) 54:706–13. doi: 10.1080/02770903.2016.1258080
14. Oyamada HAA, Cafasso MOSD, Vollmer CM, Alvim F, Lopes LM, Castro C, et al. Major depressive disorder enhances Th2 and Th17 cytokines in patients suffering from allergic rhinitis and asthma. Int Arch Allergy Immunol. (2021) 182:1155–68. doi: 10.1159/000517478
15. Gao YH, Zhao HS, Zhang FR, Gao Y, Shen P, Chen RC, et al. The relationship between depression and asthma: A meta-analysis of prospective studies. PLoS One. (2015) 10:e0132424. doi: 10.1371/journal.pone.0132424
16. Brunner WM, Schreiner PJ, Sood A, Jacobs DR Jr. Depression and risk of incident asthma in adults. The CARDIA study. Am J Respir Crit Care Med. (2014) 189:1044–51. doi: 10.1164/rccm.201307-1349OC
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
18. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
19. Aker AM, Vigod SN, Dennis CL, Kaster T, Brown HK. The association between asthma and perinatal mental illness: a population-based cohort study. Int J Epidemiol. (2022) 51:964–73.
20. Yang ZC, Wang LX, Yu Y, Lin HY, Shih LC. Increased risk of postpartum depression in women with allergic rhinitis during pregnancy: A population-based case-control study. Ann Otol Rhinol Laryngol. (2022) 131:1137–43. doi: 10.1177/00034894211058135
21. Aker AM, Stephenson AL, Wilton AS, Vigod SN, Dennis CL, Guttmann A, et al. Asthma severity and control and their association with perinatal mental illness. Can J Psychiatry. (2022) 67:156–9.
22. Kim B, Jung H, Kim J, Lee J, Kim O. Depressive symptoms and sleep disturbance in female nurses with atopic dermatitis: The Korea Nurses’ Health Study. Int J Environ Res Public Health. (2020) 17:2743.
23. Coogan PF, Yu J, O’Connor GT, Brown TA, Palmer JR, Rosenberg L. Depressive symptoms and the incidence of adult-onset asthma in African American women. Ann Allergy Asthma Immunol. (2014) 112:333–8. doi: 10.1016/j.anai.2013.12.025
24. Xie QW, Dai X, Tang X, Chan CHY, Chan CLW. Risk of mental disorders in children and adolescents with atopic dermatitis: A systematic review and meta-analysis. Front Psychol. (2019) 10:1773. doi: 10.3389/fpsyg.2019.01773
25. Rodrigues J, Franco-Pego F, Sousa-Pinto B, Bousquet J, Raemdonck K, Vaz R. Anxiety and depression risk in patients with allergic rhinitis: a systematic review and meta-analysis. Rhinology. (2021) 59:360–73. doi: 10.4193/Rhin21.087
26. Ye G, Baldwin DS, Hou R. Anxiety in asthma: a systematic review and meta-analysis. Psychol Med. (2021) 51:11–20. doi: 10.1017/S0033291720005097
27. Castillo EF, Zheng H, Yang XO. Orchestration of epithelial-derived cytokines and innate immune cells in allergic airway inflammation. Cytokine Growth Factor Rev. (2018) 39:19–25. doi: 10.1016/j.cytogfr.2017.11.004
28. Rivest S. Interactions between the immune and neuroendocrine systems. Prog Brain Res. (2010) 181:43–53. doi: 10.1016/S0079-6123(08)81004-7
29. Yang CJ, Liu D, Xu ZS, Shi SX, Du YJ. The pro-inflammatory cytokines, salivary cortisol and alpha-amylase are associated with generalized anxiety disorder (GAD) in patients with asthma. Neurosci Lett. (2017) 656:15–21. doi: 10.1016/j.neulet.2017.07.021
30. Zhu Z, Zhu X, Liu CL, Shi H, Shen S, Yang Y, et al. Shared genetics of asthma and mental health disorders: a large-scale genome-wide cross-trait analysis. Eur Respir J. (2019) 54:1901507. doi: 10.1183/13993003.01507-2019
Keywords: allergic diseases, mental disorders, women, relationship, meta-analysis
Citation: Liu L, Luo C, Zhang M, Ao X, Liu H and Peng S (2022) Relationship between allergic diseases and mental disorders in women: A systematic review and meta-analysis. Front. Psychiatry 13:1026032. doi: 10.3389/fpsyt.2022.1026032
Received: 23 August 2022; Accepted: 19 October 2022;
Published: 09 November 2022.
Edited by:
Sy Duong-Quy, Lam Dong Medical College, VietnamReviewed by:
Mai Nguyen Thi Phuong, Hanoi Medical University, VietnamCopyright © 2022 Liu, Luo, Zhang, Ao, Liu and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shunlin Peng, c2h1bmxpbl9wQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.