- 1Department of Medicine, Universidade Estadual de Mato Grosso do Sul, Campo Grande, Brazil
- 2Care Policy and Evaluation Centre, Department of Health Policy, London School of Economics and Political Science, London, United Kingdom
- 3Department of Neuropsychiatry, Universidade Federal de Santa Maria, Santa Maria, Brazil
- 4Graduate Program in Psychiatry and Behavioral Sciences, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil
- 5Departamento de Psiquiatria, Universidade Federal de São Paulo, São Paulo, Brazil
- 6Department of Medicine, Universidade Federal de Alagoas, Maceió, Brazil
- 7Department of Public Health, Universidade do Extremo Sul Catarinense, Criciúma, Brazil
Background: Implementation of interventions to treat child and adolescent mental health problems in schools could help fill the mental health care gap in low- and middle-income countries (LMICs). Most of the evidence available come from systematic reviews on mental health prevention and promotion, and there is less evidence on treatment strategies that can be effectively delivered in schools. The aim of this review was to identify what school-based interventions have been tested to treat children and adolescents in LMICs, and how effective they are.
Methods: We conducted a systematic review including seven electronic databases. The search was carried out in October 2022. We included randomised or non-randomised studies that evaluated school-based interventions for children or adolescents aged 6–18 years living in LMICs and who had, or were at risk of developing, one or more mental health problems.
Results: We found 39 studies with 43 different pairwise comparisons, treatment for attention-deficit and hyperactivity (ADHD), anxiety, depression, and posttraumatic stress disorder (PTSD), Conduct disorder (CD). Pooled SMD were statistically significant and showed that, overall, interventions were superior to comparators for PTSD (SMD = 0.61; 95% CI = 0.37–0.86), not statistically significant for anxiety (SMD = 0.11; 95% CI = −0.13 to 0.36), ADHD (SMD = 0.36; 95% CI = −0.15 to 0.87), and for depression (SMD = 0.80; 95% CI = −0.47 to 2.07). For CD the sample size was very small, so the results are imprecise.
Conclusion: A significant effect was found if we add up all interventions compared to control, suggesting that, overall, interventions delivered in the school environment are effective in reducing mental health problems among children and adolescents.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=129376], identifier [CRD42019129376].
Introduction
The global prevalence of mental health conditions in children and adolescents is estimated to be around 13.4% (1) and half of the adults diagnosed with one had their first episode during childhood and adolescence (2). Moreover, young people are presenting increasing levels of mental health problems related to increasingly stressful environments (3, 4), particularly in low- and middle-income countries (LMICs), where young people are exposed to several vulnerability factors for the development of mental health conditions, such as violence and material deprivation (5).
Most of the world’s population (80%) live in LMICs, and, yet, only 6% of research on mental health come from these countries (6). Despite the likelihood of positive and consistent effects from high-income countries for decision making, there is a shortage of trained mental health professionals according to reports from the World Health Organisation (WHO), mental health systems in LMICs are not properly equipped/resourced to deliver appropriate mental health care. Therefore, a mental health care gap remains in these countries, which could be filled through the implementation of mental health programmes that could be delivered by non-specialist professionals (7, 8).
As schooling is compulsory in most LMICs (9), this brings opportunities for delivering mental health care and support. Schools are as settings where youth spend a significant proportion of their time–from at least 4 h/day reaching a maximum of 8 h/day and a place where they learn and develop (10). Therefore, schools are a key setting where mental health could be effectively treated, as some evidence has suggested (11, 12). Indeed, a few systematic reviews have shown the potential of school-based interventions in preventing the development of mental health problems. However, such interventions are focussed mostly on anxiety and depression with low to middle Standardized mean difference (SMD) (13–15). Another systematic review on effectiveness of mental health promotion interventions for young people found that some interventions had a positive impact on children and adolescents’ externalising and internalising problem scores and in improving social and emotional wellbeing (16). However, other interventions had no effect on anxiety, depression and PTSD symptoms (16). Additionally, there is a significant return on investment, as some estimates show that for each $1 invested in universal school-based interventions aiming at mental health prevention and promotion, there is an expected $24 economic return in 80 years, resulting from savings in further health/mental health care, improved school outcomes, productivity, and better life chances (17).
Nonetheless, evidence on interventions to treat mental health problems in the school setting, particularly in LMICs, is scarce. Such interventions, if proven to be effective, could help fill the mental health care gap in low resources settings. Therefore, the aim of this review was to identify what are and how effective are school-based interventions used to treat children and adolescents in LMICs.
Methods
Protocol and registration
The protocol for this systematic review was previously published in Medicine (Baltimore) (18) and is registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the number CRD42019129376 (19).
Eligibility criteria
This study is part of a broader systematic review that has been carried out to identify effective interventions to treat child and adolescent mental health problems in LMIC (18). However, for this specific review, only studies on school-based interventions were included.
In summary, we carried out a systematic review of studies published in scientific journals and grey literature, considering the following inclusion criteria:
1. Population: children and adolescents aged 6–18 years, school-age child and adolescent, living in LMIC based on criteria of World Bank Country and Lending Groups (20).
2. Intervention: any school-based intervention.
3. Condition: the systematic review included any child and adolescent mental health problems.
4. Outcome: primary outcomes were defined as the improvement of participants’ mental health symptoms. Studies that did not assess primary outcomes were still included if their interventions targeted the following secondary outcomes: hospitalisation, wellbeing, quality of life, physical social, or occupational functioning/impairment.
5. Study design: we included randomised and non-randomised controlled trials.
6. Language: there were no language restrictions.
7. Timeframe: studies published from 2007 to 2022 were included.
Information resource
Only studies published from 2007 onwards were included because this is the year in which child and adolescent mental health became prominent as a global public health challenge (7). Our research was limited to studies published until October 2022.
Search
An electronic search was carried out in the following databases: MEDLINE Ovid, EMBASE Ovid, PsycINFO Ovid, CINAHL plus, LILACS (Latin American and Caribbean Health Sciences), BDENF (Brazilian Nursing Database), and IBECS (The Spanish Bibliographic Index of the Health Sciences). We also checked reference lists of all included studies and relevant review articles identified through our search for additional references. We emailed experts in the field about other published and unpublished studies that might be eligible for inclusion. No unpublished data were included in this review.
Details on our search strategy and other relevant methodological aspects of our review can be found in our study protocol, which has been previously published (18).
Study selection
To ensure reliability between reviewers, we performed a screening team training phase, in which 5% of all references were independently screened by 2 different reviewers. An expert in mental health researcher (WSR) resolved divergences independently and made the final decision when it was necessary. Based on the identification of the main reasons for divergences between reviewers, a meeting was held with the review team to clarify potential doubts and solve any systematic error when screening references.
After divergences in the pilot phase were solved and the screening team was retrained, the remaining 95% of references were equally split among the reviewers to finalise the screening phase. Based on our inclusion and exclusion criteria, reviewers read titles and abstracts and classified references into three categories: “no,” “yes,” and “maybe.” References classified as “no” were excluded. Those classified as “yes” or “maybe” were selected for the full-text screening phase, and were analysed again against inclusion/exclusion criteria after full texts have been obtained and read.
The selection process was documented with a Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flowchart (21).
The web based Covidence (covidence.org) tool will be used to perform the management and screening of references, and data extraction from eligible studies.
Data collection process
Data items
We first extracted relevant data from studies, including key characteristics of studies and parameters of interventions’ efficacy/effectiveness.
Study details
Aim, study design, design details, country in which study was conducted, details on location of intervention delivery, target condition, or risk factor (i.e., subthreshold symptoms, experience of child maltreatment).
Participants
Sample size (intervention and control groups at baseline and follow-up), sociodemographic characteristics (e.g., age, gender, ethnicity, socioeconomic status).
Interventions
Description of intervention including frequency and duration, number of sessions, mode of delivery (e.g., face to face, internet), format (e.g., one to one or group), cost of intervention.
Delivery of the intervention
Setting in which intervention was delivered (e.g., school), who delivered the intervention (e.g., medical doctor, nurse, psychologist, teacher, lay health worker, etc.) and whether it was delivered by 1 practitioner or a team of individuals, whether there was intersectoral collaboration (e.g., between health and education or guardianship councils).
Comparison groups
Characteristics of and procedures for selection comparison groups (e.g., matching vs. randomisation).
Outcomes
Primary outcomes will include reduction of mental health symptoms, or improvement in mental health functioning. Secondary outcomes will include, economic impact, reduction of hospitalisations, or improvement in wellbeing, quality of life, resilience, social, physical, and occupational functioning, including educational outcomes.
Studies with missing data were excluded after two unsuccessful attempts of contacting authors. Then, based on pre- and post-intervention scores we estimated within-group mean differences, as well as between-groups (intervention vs. control) mean differences and pooled standard deviations (SD). Mean differences were, then, divided by pooled SDs to be converted into standardized mean differences (SMD).
Data analyses
We started our analytical approach by carrying out a descriptive analysis, in which we reported the number of references that were found and dealt with—from number of references retrieved by our search to the number of studies included in the study—, according to the updated version of the PRISMA guideline for reporting systematic reviews (21). Afterwards, we reported key characteristics of studies included in our review by summarising the frequency and proportions of studies in each category of relevant variables—e.g., country, types of interventions, outcomes etc.
For our pairwise meta-analysis, we grouped individual studies into the following emerged conditions: ADHD, PTSD, anxiety, depression, and conduct disorder, interventions have been tested in the school setting. For all other conditions included in our search strategy, interventions were tested only in clinical settings.
Risk of bias within individual studies
Two review authors (AG and WR) independently critically appraised the studies, all disagreements were resolved by discussion. We used the Cochrane Collaboration’s risk of bias tool, version 2.0. Six parameters were used to assess included studies: (1) Bias arising from the randomisation process; (2) bias due to deviations from intended intervention; (3) bias due to missing outcome data; (4) bias in measurement of the outcome; (5) bias in selection of the reported result; and (6) overall risk of bias of included studies. Based on these parameters, studies were classified into three categories: low risk of bias; some concerns; and high risk of bias (22).
Summary measures
For our data synthesis, we performed a random-effect pairwise meta-analysis using Stata’s metan command, stratified by conditions. Therefore, we estimated pooled standardised mean differences with 95% confidence intervals for each one of the conditions, and an overall pooled mean difference and 95% confidence interval for the combined effect of all comparisons included in the meta-analysis. This approach also allowed us to estimate I2 parameters of heterogeneity for each one of the subgroups and for the overall pooled analysis.
Results
Key characteristics of included studies
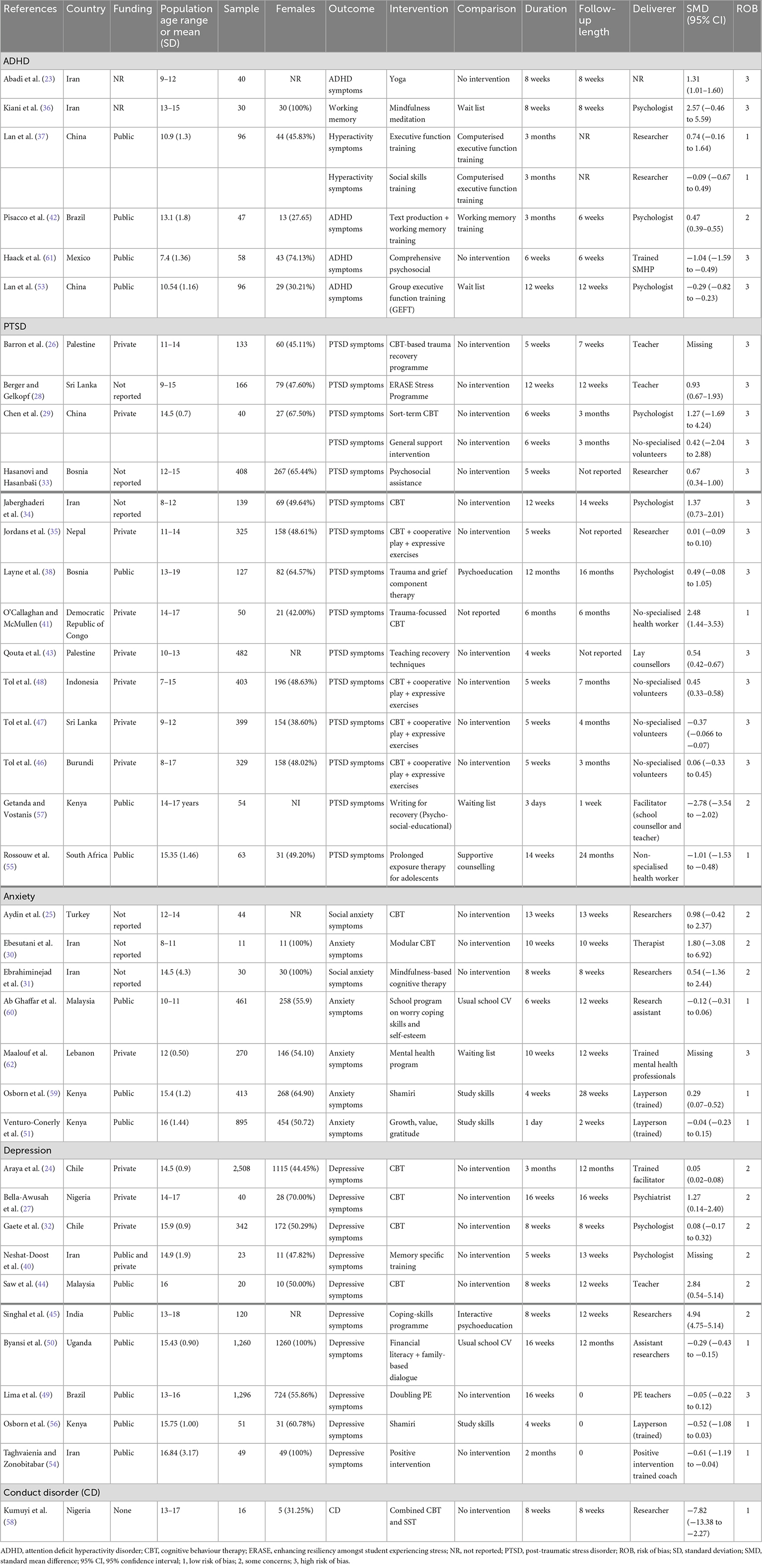
A total of 133,568 references were identified through our search strategy. After the screening of titles and abstracts, and eligibility assessment, 166 studies were in LMIC (Figure 1), 127 were excluded with reason and 39 were on school-based interventions (23–61). We excluded, therefore, 166 studies that were not conducted in schools.
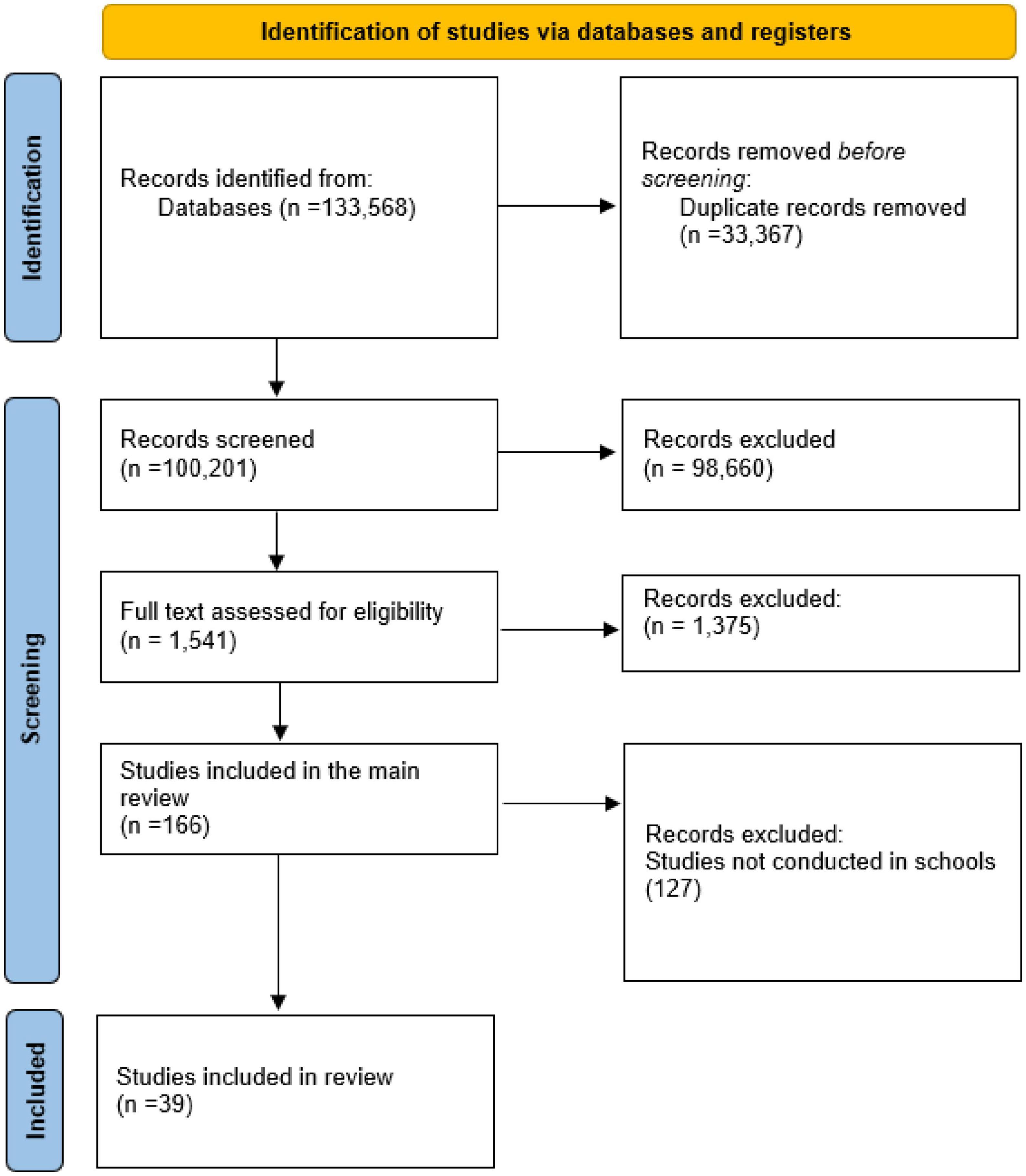
Figure 1. PRISMA flow-chart of systematic review on school-based interventions for children and adolescent in LMIC.
Some of these studies had multiple intervention groups (29, 37), thus a total of 6 interventions were compared in which a total of 9,017 participants were allocated between intervention and control groups.
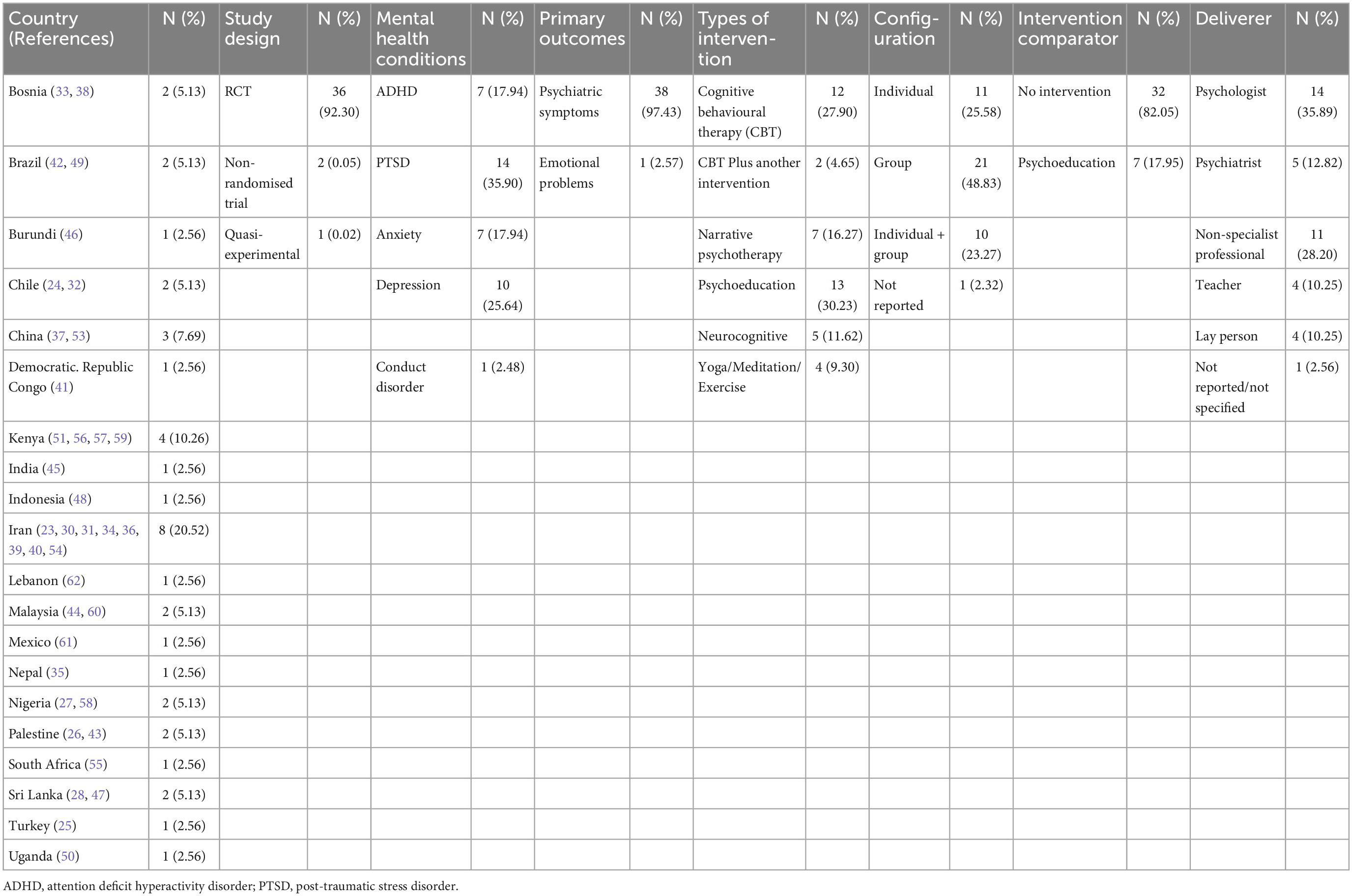
The included studies were from: Bosnia (34, 39) (N = 2–5.13%), Brazil (42, 49) (N = 2–5.13%), Burundi (46) (N = 1–2.56%), Chile (24, 32) (N = 2–5.13%), China (37, 53) (N = 2–5.13%), Congo (41) (N = 1–2.56%), Kenya (51, 56, 57, 59) (N = 4–10.26%) India (45) (N = 1–2.56%), Indonesia (48) (N = 1–2.56%), Iran (23, 30, 31, 34, 36, 39, 40, 54) (N = 8–20.52%), Lebanon (62) (N = 1–2.56%), Malaysia (44, 60) (N = 2–5.13%), Mexico (61) (N = 1–2.56%), Nepal (35) (N = 1–2.56%), Nigeria (27, 58) (N = 2–5.13%), Palestine (26) (N = 1–2.56%), South Africa (55) (N = 1–2.56%), Sri Lanka (28, 47) (N = 2–5.13%), Turkey (25) (N = 1–3.85%), Uganda (50) (N = 1–2.56%). Table 1 shows the characteristics of individual included studies.
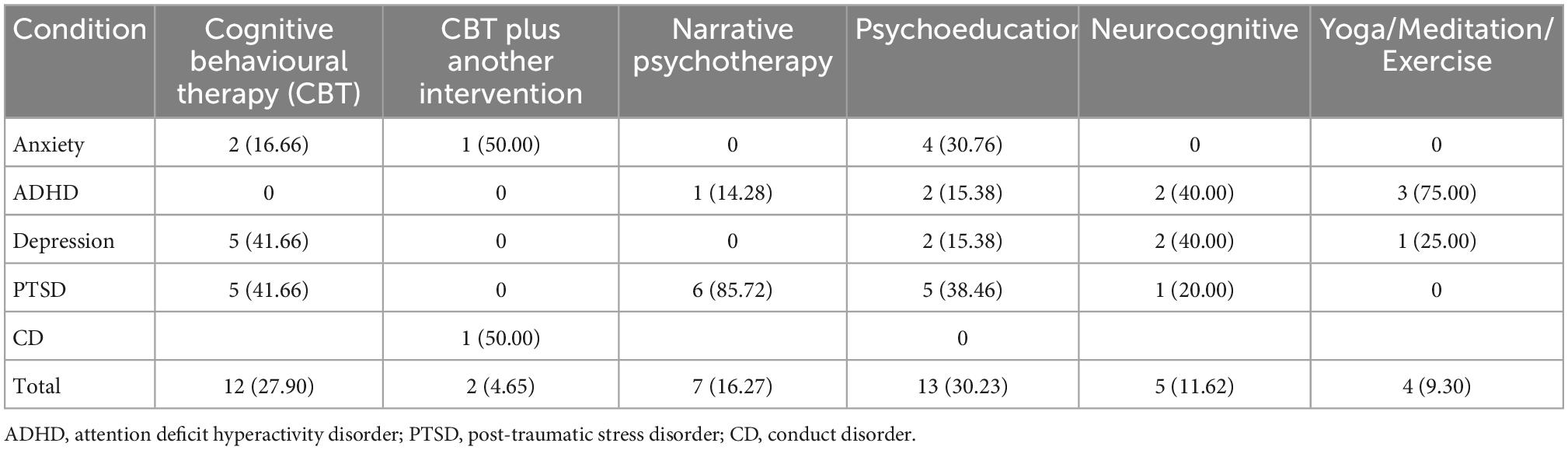
Interventions evaluated were: Cognitive behavioral therapy (CBT) (N = 12–27.90%) (24–27, 29–32, 34, 41, 44, 45), CBT combined with another intervention (N = 2–4.65%) (31, 58), Psychoeducation (N = 13–30.23%) (28, 29, 33, 37, 41, 50, 51, 56, 57, 59–62), Neurocognitive (N = 5–11.62%) (34, 37, 40, 54), Narrative psychotherapy (N = 7–16.27%) (35, 38, 39, 46–48, 55), Yoga/Meditation (N = 4–10%) (23, 31, 42, 49). Table 2 shows the synthesis of the studies included in the systematic review.
Table 3 shows the synthesis of the studies included in the systematic review and the risk of bias. There were 7 studies (17.94%) on ADHD (23, 36, 37, 39, 42, 53, 61), 14 studies (35.90%) on PTSD (28, 29, 33–35, 38, 41, 43, 46–48, 55, 57), 10 studies (25.64%) on depression (24, 27, 30, 32, 44, 45, 49, 50, 54, 56), and 7 studies (17.94%) on anxiety (25, 30, 31, 51, 59, 60, 62).
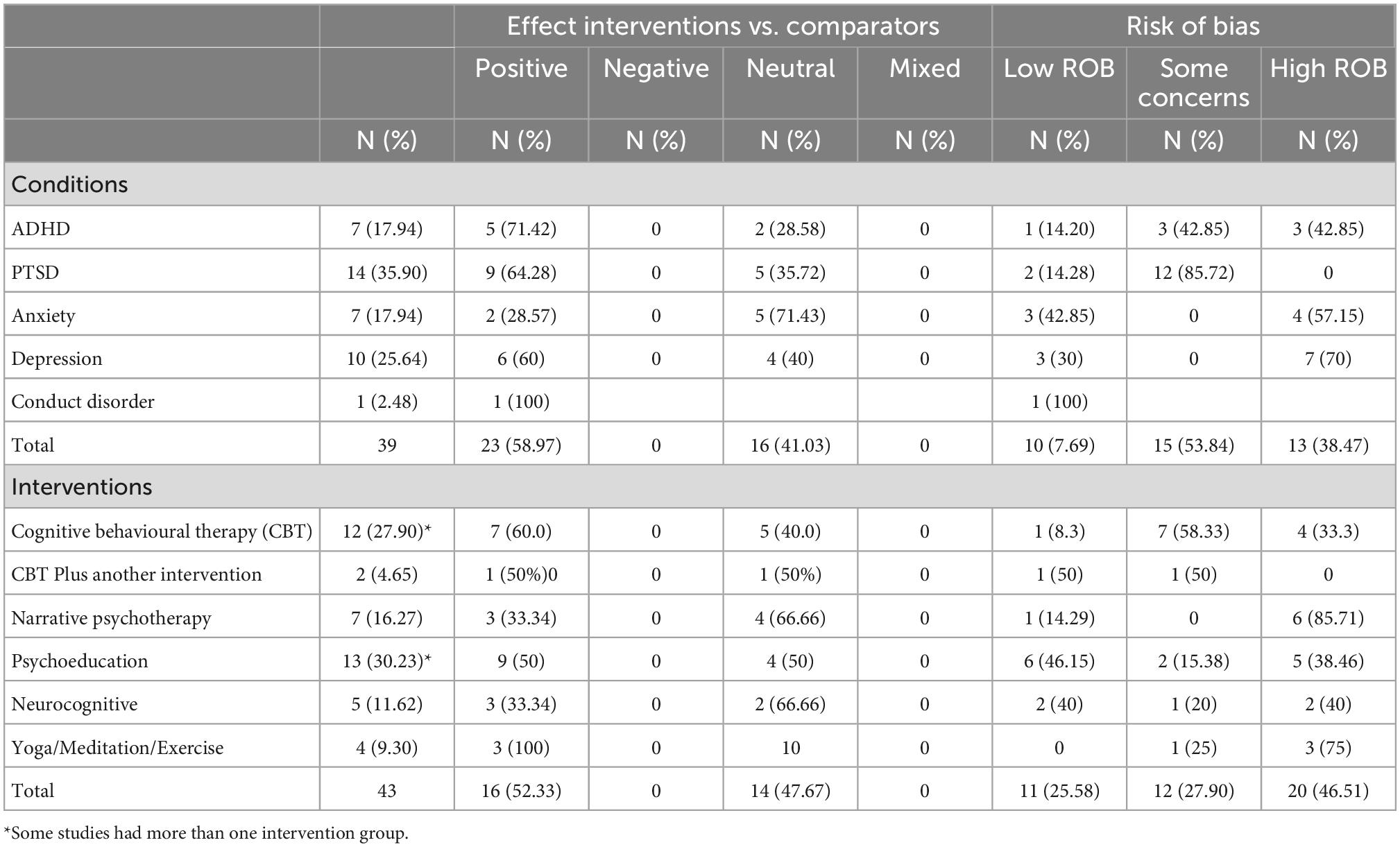
Table 3. Summary effect of interventions as compared to control/no intervention, and risk of bias classification by conditions and types of intervention.
Eleven studies presented low risk of bias. A total of 12 studies had some concerns and 20 studies had high risk of bias.
Cognitive behavioral therapy was used to treat all conditions, but ADHD (24–27, 29, 30, 32, 34, 41, 43–45) and CD (58). CBT Plus another intervention was only investigated for anxiety and CD (31, 58). Narrative psychotherapy were used in seven studies; ADHD and PTSD (35, 37, 38, 46–48, 55). Psychoeducation were used in 13 studies (28, 29, 33, 37, 41, 50, 51, 56, 57, 59–62) for PTSD, ADHD, depression, and anxiety. Yoga/meditation/exercise were used in four studies (23, 36, 42, 49) in ADHD and depressive symptoms. Neurocognitive therapy was used in five studies (34, 37, 39, 40, 54) for ADHD, PTSD anxiety, and depression. Table 4 shows the interventions investigated per condition.
Pairwise comparisons
In the 39 studies included in our review, we identified 43 different pairwise comparisons. We grouped interventions according to five types of mental health conditions based on the stated target of the intervention. Figure 2 show pooled SMD for all conditions, only PTSD (SMD = 0.61; 95% CI = 0.37–0.86) were statistically significant. Overall, interventions were superior to comparators SMD = 0.46 (0.18–0.74); not statistically significant for anxiety (SMD = 0.11; 95% CI = −0.13 to 0.36), ADHD (SMD = 0.36; 95% CI = −0.15 to 0.87), and for depression (SMD = 0.80; 95% CI = −0.47 to 2.07). For CD the sample size was very small, so the results are imprecise.
Discussion
Main results
In our review, we found 39 studies which assessed the efficacy/effectiveness of interventions for 6–18 years old child/adolescent to treat mental health problems in schools in LMICs. When stratified by conditions, pooled effects of interventions to treat anxiety, ADHD, depression were non-superior to comparators. For PTSD, significant effect was found. When SMD of all studies were pooled together, a significant effect was found, suggesting that, overall, interventions delivered in the school environment are effective in reducing mental health problems among children and adolescents.
Comparison to other reviews
Other systematic reviews published in the literature are mostly focussed on universal interventions on mental health disease prevention and wellness promotion (13, 15, 16), with conflicting results–some reviews have found, for example small to medium STD to prevent depression and anxiety symptoms (13, 14) and to promote wellbeing (16). In other review, however, found no evidence of effects on preventing depression, anxiety, and PTSD (16).
Anxiety and depression are being reported together in school-based mental health literature synthesis (14, 63, 64). However, as showed in our results, school-based interventions reach different results for each condition, thus requiring future studies to deal separately considering universal or target programs (65).
Regarding PTSD and childhood trauma there is a growing body of evidence from systematic reviews associating the importance of cognitive behavioural therapies for reducing the risk of psychotic symptoms, improve well-being (66, 67) which is in agreement with our interventions effectiveness found in the literature.
Regarding ADHD, multiple psychosocial have been developed and empirically tested to improve ADHD symptoms, according to CADDRA Guidelines Work GROUP the evidence supports Cognitive Behavioural Therapy and Caregiver interventions. Other interventions, such as Physical Exercise and Mind–Body, still lack strong evidence to be supported (68). Our review found that multiple school-based psychosocial interventions have been tested in LMIC and single studies shows promising effects.
Offering interventions to prevent mental disorders and to promote mental health in schools should[could] contribute to improve access to care among young people with mental health problems by adopting task-share approaches that propose that mild and moderate mental disorders can be treated in the community by no-specialist professionals. Therefore, identifying treatment programmes (universal or targeted) that are effective when delivered in schools is key for the scaling up of mental health care. Our review contributes to the literature by identifying interventions that have been delivered in schools and proven effective.
Additional reflection points
Most children and adolescents with mental health conditions do not receive evidence-based care or they are underdiagnosed, leading to chronicity of mental health symptoms and increased costs of care (69). The body of evidence applied in LMICS comes from HICs countries, however, different modes of living, social, cultural, and health system factors limit the generalisability and applicability of indirect evidence (70).
In our review, interventions were delivered by different professionals, for instance: teachers, researchers, community health workers, non-specialised health professionals, lay person. These professionals are well-recognised for educating and mobilising the community to increase demand for care (71). This is a valid strategy, and is in agreement with the literature (72–74), which suggests young people with mild and moderate symptoms can be treat in the community, and only more severe cases, which requires a greater level of care should be referral to specialised providers (75). Our results show that there is a potential for scaling up interventions to treat mental health problems in schools, helping to increase young people’s access to care in settings where health care professionals are scarce.
Quality of the evidence
GRADE approach assess five factors: risk of bias, inconsistency, indirectness, imprecision, and publication bias and factors that increase the quality of evidence (large magnitude of an effect, dose-response gradient, effect of plausible residual confounding). Thus, as seen in Table 1: The SMD varied across studies and group of conditions/interventions, we believe the intervention protocols being studied, many different conditions, and different stage of disease were the cause of serious downgraded (−1), due to inconsistency among studies and imprecision of estimates. Additionally, another serious downgrade (−1), the study limitations (risk of bias).
Considering the broad evidence synthesised for interventions and conditions, we would make weak recommendation/very low-quality evidence, which means caregivers will need to allocate more time to shared decision making including individual patient’s circumstances, preferences, and values.
Study limitations
The studies have limitations that should be highlighted. First, there are three main potential bias in the review process concerns: (1-) lack of reporting to allow us make judgement in the “Risk of bias 2.0” assessment; (2-) many conditions and many interventions were found, which increased clinical variability across the review, turning it in a more descriptive synthesis of the literature; (3-) lack of consistency of interventions protocols. Additionally, most trials were not registered, presenting another potential source of bias.
This review does not address comparison between effectiveness of interventions delivered in the school setting and other settings. It does show, however, that some interventions are effective for certain type of symptomatology. Once there is now evidence of interventions that could effectively treat mental health problems in school settings, additional studies should explore the feasibility of scalling up such intervention in the school system in different contexts and identify which factors would facilitate implementation in real world circumstances.
Implications and recommendations for future researchers
Implementation of school-based interventions is conditioned on school attendance of children and adolescents which can vary among and within LMICs (9). Additionally, other factors can influence engagement and delivery, as this may require appropriate training for teachers and other school personnel, impact on their routine and require additional supportive, such as supervision, as well as additional material/economic resources (76, 77). Thus, planning of mental health programs are complex and need to consider the factors raised above.
Low- and middle-income countries are diverse/heterogenous countries. Yet, most of the evidence in the review comes from Iran, in the Western Asia region, and may not be easily transferrable to other LMIC due to cultural, economic, and other contextual differences.
The methodological quality of studies called our attention, we found a considerable number of studies with methodological concerns and high risk of bias.
Future studies should examine and describe in more detail the effectiveness of intervention’s components, such as frequency, delivery methods, etc., as well as implementation aspects that could guide policy and decision making for better mental health care.
Conclusion
We presented a systematic review of school-based interventions for mental health problems in young people living in low- and middle-income countries. The evidence presented here is motivated by the uniqueness of school environment for such interventions, the fact that most children and adolescents in the world live in a LMIC context and no evidence synthesis have been previously organised.
The results indicated that school-based interventions for anxiety, PTSD, and ADHD in children and adolescents tested in LMICs showed a significant reduction of symptoms. The list of interventions from primary studies were: CBT was used to treat PTSD, anxiety, depression and CD. CBT Plus another intervention was only investigated for anxiety and CD. Narrative psychotherapies were used in ADHD and PTSD. Psychoeducation in PTSD, ADHD, depression, and anxiety. Yoga/meditation/exercise were used in ADHD and depressive symptoms. Neurocognitive therapy was used in ADHD, PTSD, anxiety, and depression.
Author contributions
AG conceived and designed the study, contributed to the definition of the search strategy, and wrote the first version of the manuscript. WR and MH conceived and designed the study and contributed to the definition of the search strategy and the writing up of the manuscript. CM and CT contributed to the study design and revision of the manuscript. DM and CZ contributed to the study design, definition of the search strategy, and revision of the manuscript. SE-L conceived and designed the study and contributed to the definition of the search strategy and revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the UK Medical Research Council (MRC), grant number MR/R022763/1, Fundação de Amparo à Pesquisa do Estado de Alagoas (FAPEAL), grant number 60030 000764/2018, and Fundação de Apoio ao Desenvolvimento do Ensino, Ciência e Tecnologia do Estado de Mato Grosso do Sul, grant number 71/700.071/2018. MH was a post-doctoral research fellow at UFRGS, supported by the National Institute of Mental Health (grant number R01MH120482). AG was also supported by the Academy of Medical Science, the Newton Fund NIFR7\1004, and the fellowship of research productivity (PQ) granted by the National Council for Scientific and Technological Development (CNPq).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Polanczyk G, Salum G, Sugaya L, Caye A, Rohde L. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. (2015) 56:345–65. doi: 10.1111/jcpp.12381
2. Caspi A, Houts R, Ambler A, Danese A, Elliott M, Hariri A, et al. Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin birth cohort study. JAMA Netw Open. (2020) 3:e203221. doi: 10.1001/jamanetworkopen.2020.3221
3. Thompson E, Richards M, Ploubidis G, Fonagy P, Patalay P. Changes in the adult consequences of adolescent mental health: findings from the 1958 and 1970 British birth cohorts. Epidemiology. (2020). Available online at: http://medrxiv.org/lookup/doi/10.1101/2020.07.17.20156042 (accessed July 25, 2022). doi: 10.1101/2020.07.17.20156042
4. Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry. (2015) 56:370–93. doi: 10.1111/jcpp.12372
5. Zhou W, Ouyang F, Nergui O, Bangura J, Acheampong K, Massey I, et al. Child and adolescent mental health policy in low- and middle-income countries: challenges and lessons for policy development and implementation. Front Psychiatry. (2020) 11:150. doi: 10.3389/fpsyt.2020.00150
6. Saxena S, Paraje G, Sharan P, Karam G, Sadana R. The 10/90 divide in mental health research: trends over a 10-year period. Br J Psychiatry. (2006) 188:81–2. doi: 10.1192/bjp.bp.105.011221
7. World Health Organization. Comprehensive Mental Health Action Plan 2013–2030. Geneva: World Health Organization (2021).
9. Local Burden of Disease Educational Attainment Collaborators. Mapping disparities in education across low- and middle-income countries. Nature. (2020) 577:235–8. doi: 10.1038/s41586-019-1872-1
10. Han S, Lee D. Children’ stress, depression, sleep, and internet use. Int J Psychol Educ Stud. (2021) 8:246–53. doi: 10.52380/ijpes.2021.8.4.671
11. Collishaw S, Goodman R, Ford T, Rabe-Hesketh S, Pickles A. How far are associations between child, family and community factors and child psychopathology informant-specific and informant-general? J Child Psychol Psychiatry. (2009) 50:571–80. doi: 10.1111/j.1469-7610.2008.02026.x
12. Sekhar D, Schaefer E, Waxmonsky J, Walker-Harding L, Pattison K, Molinari A, et al. Screening in high schools to identify, evaluate, and lower depression among adolescents: a randomized clinical trial. JAMA Netw Open. (2021) 4:e2131836. doi: 10.1001/jamanetworkopen.2021.31836
13. Caldwell D, Davies S, Thorn J, Palmer J, Caro P, Hetrick S, et al. School-Based Interventions to Prevent Anxiety, Depression and Conduct Disorder in Children and Young People: A Systematic Review and Network Meta-Analysis. Southampton: NIHR Journals Library (2021). doi: 10.3310/phr09080
14. Werner-Seidler A, Spanos S, Calear A, Perry Y, Torok M, O’Dea B, et al. School-based depression and anxiety prevention programs: an updated systematic review and meta-analysis. Clin Psychol Rev. (2021) 89:102079. doi: 10.1016/j.cpr.2021.102079
15. Bradshaw M, Gericke H, Coetzee B, Stallard P, Human S, Loades M. Universal school-based mental health programmes in low- and middle-income countries: a systematic review and narrative synthesis. Prev Med. (2021) 143:106317. doi: 10.1016/j.ypmed.2020.106317
16. Barry M, Clarke A, Jenkins R, Patel V. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health. (2013) 13:835. doi: 10.1186/1471-2458-13-835
17. UNICEF. On My Mind: Promoting, Protecting and Caring for Children’s Mental Health. New York, NY: UNICEF (2021). 259 p.
18. Grande A, Ribeiro W, Faustino C, de Miranda C, Mcdaid D, Fry A, et al. Effective/cost effective interventions of child mental health problems in low- and middle-income countries (LAMIC): systematic review. Medicine. (2020) 99:e18611. doi: 10.1097/MD.0000000000018611
19. Ribeiro WS, Grande AJ, Hoffmann MS, Ziebold C, McDaid D, Fry A, et al. A systematic review of evidence-based interventions for child and adolescent mental health problems in low- and middle-income countries. Compr Psychiatry. (2023) 121:152358. doi: 10.1016/j.comppsych.2022.152358
20. The World Bank. World Bank Country and Lending Groups – World Bank Data Help Desk. (2022). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed July 14, 2022).
21. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
22. Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
23. Abadi M, Madgaonkar J, Venkatesan S. Effect of yoga on children with attention deficit/hyperactivity disorder. Psychol Stud. (2008) 53:154–9. doi: 10.1007/978-1-4020-5614-7_196
24. Araya R, Fritsch R, Spears M, Rojas G, Martinez V, Barroilhet S, et al. School intervention to improve mental health of students in Santiago, Chile: a randomized clinical trial. JAMA Pediatr. (2013) 167:1004. doi: 10.1001/jamapediatrics.2013.2361
25. Aydin A, Tek S, Sor O. Evaluation of the effectiveness of a cognitive-behavioral therapy program for alleviating the symptoms of social anxiety in adolescents. Turk J Psychiatry. (2010) 21:1–11.
26. Barron I, Abdallah G, Smith P. Randomized control trial of a CBT trauma recovery program in Palestinian schools. J Loss Trauma. (2013) 18:306–21. doi: 10.1080/15325024.2012.688712
27. Bella-Awusah T, Ani C, Ajuwon A, Omigbodun O. Effectiveness of brief school-based, group cognitive behavioural therapy for depressed adolescents in south west Nigeria. Child Adolesc Mental Health. (2016) 21:44–50. doi: 10.1111/camh.12104
28. Berger R, Gelkopf M. School-based intervention for the treatment of tsunami-related distress in children: a quasi-randomized controlled trial. Psychother Psychosom. (2009) 78:364–71. doi: 10.1159/000235976
29. Chen Y, Shen W, Gao K, Lam C, Chang W, Deng H. Effectiveness RCT of a CBT intervention for youths who lost parents in the Sichuan, China, Earthquake. Psychiatr Serv. (2014) 65:259–62. doi: 10.1176/appi.ps.201200470
30. Ebesutani C, Helmi K, Fierstein M, Taghizadeh M, Chorpita BFA. Pilot study of modular cognitive-behavioral therapy and cognitive-behavioral hypnotherapy for treating anxiety in Iranian girls. Int J Cogn Ther. (2016) 9:13–37. doi: 10.1521/ijct_2016_09_01
31. Ebrahiminejad S, Poursharifi H, Bakhshiour Roodsari A, Zeinodini Z, Noorbakhsh S. The effectiveness of mindfulness-based cognitive therapy on Iranian female adolescents suffering from social anxiety. Irani Red Crescent Med J. (2016) 18:e25116. doi: 10.5812/ircmj.25116
32. Gaete J, Martinez V, Fritsch R, Rojas G, Montgomery A, Araya R. Indicated school-based intervention to improve depressive symptoms among at risk Chilean adolescents: a randomized controlled trial. BMC Psychiatry. (2016) 16:276. doi: 10.1186/s12888-016-0985-4
33. Hasanovi M, Hasanbaši E. Psychosocial assistance to students with posttraumatic stress disorder in primary and secondary schools in post-war Bosnia Herzegovina. Psychiatr Danub. (2009) 21:463–73.
34. Jaberghaderi N, Rezaei M, Kolivand M, Shokoohi A. Effectiveness of cognitive behavioral therapy and eye movement desensitization and reprocessing in child victims of domestic violence. Iran J Psychiatry. (2019) 14:67–75. doi: 10.18502/ijps.v14i1.425
35. Jordans M, Komproe I, Tol W, Kohrt B, Luitel N, Macy R, et al. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial: evaluation of a psychosocial intervention in Nepal. J Child Psychol Psychiatry. (2010) 51:818–26. doi: 10.1111/j.1469-7610.2010.02209.x
36. Kiani B, Hadianfard H, Mitchell J. The impact of mindfulness meditation training on executive functions and emotion dysregulation in an Iranian sample of female adolescents with elevated attention-deficit/hyperactivity disorder symptoms: mindfulness in adolescents with ADHD symptoms. Aust J Psychol. (2017) 69:273–82. doi: 10.1111/ajpy.12148
37. Lan Y, Liu X, Fang H. Randomized control study of the effects of executive function training on peer difficulties of children with attention-deficit/hyperactivity disorder C subtype. Appl Neuropsychol Child. (2018) 9:41–55. doi: 10.1080/21622965.2018.1509003
38. Layne C, Saltzman W, Poppleton L, Burlingame G, Pašalić A, Duraković E, et al. Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2008) 47:1048–62. doi: 10.1097/CHI.0b013e31817eecae
39. Looyeh M, Kamali K, Shafieian R. An exploratory study of the effectiveness of group narrative therapy on the school behavior of girls with attention-deficit/hyperactivity symptoms. Arch Psychiatr Nurs. (2012) 26:404–10. doi: 10.1016/j.apnu.2012.01.001
40. Neshat-Doost H, Dalgleish T, Yule W, Kalantari M, Ahmadi S, Dyregrov A, et al. Enhancing autobiographical memory specificity through cognitive training: an intervention for depression translated from basic science. Clin Psychol Sci. (2013) 1:84–92. doi: 10.1177/2167702612454613
41. O’Callaghan P, McMullen J. Comparing a trauma focused and non trauma focused intervention with war affected Congolese youth: a preliminary randomised trial. Intervention. (2014) 13:28–34. doi: 10.1097/WTF.0000000000000054
42. Pisacco N, Sperafico Y, Enricone J, Guimarães L, Rohde L, Dorneles B. Metacognitive interventions in text production and working memory in students with ADHD. Psicol Reflex Crít. (2018) 31:5. doi: 10.1186/s41155-017-0081-9
43. Qouta S, Palosaari E, Diab M, Punamäki R. Intervention effectiveness among war-affected children: a cluster randomized controlled trial on improving mental health. J Traum Stress. (2012) 25:288–98. doi: 10.1002/jts.21707
44. Saw J, Tam C, Bonn G. Development and validation of a school-based cognitive-behavioural therapy (CBT) intervention for Malaysian high school students with depressive symptoms. Asia Pac J Couns Psychother. (2019) 10:171–87. doi: 10.1080/21507686.2019.1629973
45. Singhal M, Munivenkatappa M, Kommu J, Philip M. Efficacy of an indicated intervention program for Indian adolescents with subclinical depression. Asian J Psychiatry. (2018) 33:99–104. doi: 10.1016/j.ajp.2018.03.007
46. Tol W, Komproe I, Jordans M, Ndayisaba A, Ntamutumba P, Sipsma H, et al. School-based mental health intervention for children in war-affected Burundi: a cluster randomized trial. BMC Med. (2014) 12:56. doi: 10.1186/1741-7015-12-56
47. Tol W, Komproe I, Jordans M, Vallipuram A, Sipsma H, Sivayokan S, et al. Outcomes and moderators of a preventive schoolbased mental health intervention for children affected by war in Sri Lanka: a cluster randomized trial. World Psychiatry. (2012) 11:114–22. doi: 10.1016/j.wpsyc.2012.05.008
48. Tol W, Komproe I, Susanty D, Jordans M, Macy R, De Jong J. School-based mental health intervention for children affected by political violence in indonesia: a cluster randomized trial. JAMA. (2008) 300:655. doi: 10.1001/jama.300.6.655
49. Lima R, Barros M, Bezerra J, Santos S, Monducci E, Rodriguez-Ayllon M, et al. Universal school-based intervention targeting depressive symptoms in adolescents: a cluster randomized trial. Scand Med Sci Sports. (2022) 32:622–31. doi: 10.1111/sms.14115
50. Byansi W, Ssewamala F, Neilands T, Sensoy Bahar O, Nabunya P, Namuwonge F, et al. The short-term impact of a combination intervention on depressive symptoms among school-going adolescent girls in Southwestern Uganda: the Suubi4Her cluster randomized trial. J Adolesc Health. (2022) 71:301–7. doi: 10.1016/j.jadohealth.2022.04.008
51. Venturo-Conerly K, Osborn T, Alemu R, Roe E, Rodriguez M, Gan J, et al. Single-session interventions for adolescent anxiety and depression symptoms in Kenya: a cluster-randomized controlled trial. Behav Res Ther. (2022) 151:104040. doi: 10.1016/j.brat.2022.104040
52. Hattabi S, Bouallegue M, Ben Yahya H, Bouden A. Rehabilitation of ADHD children by sport intervention: a Tunisian experience. Tunis Med. (2019) 97:874–81.
53. Lan Y, Liu X, Fang H. Randomized control study of the effects of executive function training on peer difficulties of children with attention-deficit/hyperactivity disorder C subtype. Appl Neuropsychol Child. (2020) 9:41–55.
54. Taghvaienia A, Zonobitabar A. Positive intervention for depression and teacher–student relationship in Iranian high school girl students with moderate/mild depression: a pilot randomized controlled trial. Child Adolesc Psychiatry Ment Health. (2020) 14:25. doi: 10.1186/s13034-020-00331-9
55. Rossouw J, Yadin E, Alexander D, Seedat S. Long-term follow-up of a randomised controlled trial of prolonged exposure therapy and supportive counselling for post-traumatic stress disorder in adolescents: a task-shifted intervention. Psychol Med. (2022) 52:1022–30. doi: 10.1017/S0033291720002731
56. Osborn T, Wasil A, Venturo-Conerly K, Schleider J, Weisz J. Group intervention for adolescent anxiety and depression: outcomes of a randomized trial with adolescents in Kenya. Behav Ther. (2020) 51:601–15. doi: 10.1016/j.beth.2019.09.005
57. Getanda EM, Vostanis P. Feasibility evaluation of psychosocial intervention for internally displaced youth in Kenya. J Ment Health. (2020) 1–9. doi: 10.1080/09638237.2020.1818702 [Epub ahead of print].
58. Kumuyi D, Akinnawo E, Akpunne B, Akintola A, Onisile D, Aniemeka O. Effectiveness of cognitive behavioural therapy and social skills training in management of conduct disorder. S Afr J Psychiatr. (2022) 28:1737. doi: 10.4102/sajpsychiatry.v28i0.1737
59. Osborn T, Venturo-Conerly K, Arango GS, Roe E, Rodriguez M, Alemu R, et al. Effect of Shamiri Layperson-provided intervention vs study skills control intervention for depression and anxiety symptoms in adolescents in Kenya: a randomized clinical trial. JAMA Psychiatry. (2021) 78:829. doi: 10.1001/jamapsychiatry.2021.1129
60. Ab Ghaffar S, Mohd Sidik S, Ibrahim N, Awang H, Gyanchand Rampal L. Effect of a school-based anxiety prevention program among primary school children. Int J Environ Res Public Health. (2019) 16:4913. doi: 10.3390/ijerph16244913
61. Haack L, Araujo E, Meza J, Friedman L, Spiess M, Alcaraz Beltrán D, et al. Can school mental health providers deliver psychosocial treatment improving youth attention and behavior in Mexico? A pilot randomized controlled trial of CLS-FUERTE. J Atten Disord. (2021) 25:2083–97. doi: 10.1177/1087054720959698
62. Maalouf F, Alrojolah L, Ghandour L, Afifi R, Dirani L, Barrett P, et al. Building emotional resilience in youth in Lebanon: a school-based randomized controlled trial of the FRIENDS intervention. Prev Sci. (2020) 21:650–60. doi: 10.1007/s11121-020-01123-5
63. Jones E, Mitra A, Bhuiyan A. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. (2021) 18:2470. doi: 10.3390/ijerph18052470
64. González-Valero G, Zurita-Ortega F, Ubago-Jiménez J, Puertas-Molero P. Use of meditation and cognitive behavioral therapies for the treatment of stress. depression and anxiety in students. A systematic review and meta-analysis. Int J Environ Res Public Health. (2019) 16:4394. doi: 10.3390/ijerph16224394
65. Werner-Seidler A, Perry Y, Calear A, Newby J, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev. (2017) 51:30–47. doi: 10.1016/j.cpr.2016.10.005
66. Stanton K, Denietolis B, Goodwin B, Dvir Y. Childhood trauma and psychosis. Child Adolesc Psychiatr Clin N Am. (2020) 29:115–29. doi: 10.1016/j.chc.2019.08.004
67. Price M, Hollinsaid N. Future directions in mental health treatment with stigmatized youth. J Clin Child Adolesc Psychol. (2022) 51:810–25. doi: 10.1080/15374416.2022.2109652
68. Tourjman V, Louis-Nascan G, Ahmed G, DuBow A, Côté H, Daly N, et al. Psychosocial interventions for attention deficit/hyperactivity disorder: a systematic review and meta-analysis by the CADDRA guidelines work GROUP. Brain Sci. (2022) 12:1023. doi: 10.3390/brainsci12081023
69. Le L, Esturas A, Mihalopoulos C, Chiotelis O, Bucholc J, Chatterton M, et al. Cost-effectiveness evidence of mental health prevention and promotion interventions: a systematic review of economic evaluations. PLoS Med. (2021) 18:e1003606. doi: 10.1371/journal.pmed.1003606
70. Patel V. The need for treatment evidence for common mental disorders in developing countries. Psychol Med. (2000) 30:743–6. doi: 10.1017/S0033291799002147
71. Shidhaye R, Murhar V, Gangale S, Aldridge L, Shastri R, Parikh R, et al. The effect of VISHRAM, a grass-roots community-based mental health programme, on the treatment gap for depression in rural communities in India: a population-based study. Lancet Psychiatry. (2017) 4:128–35. doi: 10.1016/S2215-0366(16)30424-2
72. McLaughlin C. International approaches to school-based mental health: intent of the special issue. School Psychol Int. (2017) 38:339–42. doi: 10.1177/0143034317714839
73. Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools in high-income countries. Lancet Psychiatry. (2014) 1:377–87. doi: 10.1016/S2215-0366(14)70312-8
74. Ghebreyesus T, Fore H, Birtanov Y, Jakab Z. Primary health care for the 21st century, universal health coverage, and the sustainable development goals. Lancet. (2018) 392:1371–2. doi: 10.1016/S0140-6736(18)32556-X
75. Patel V, Saxena S. Achieving universal health coverage for mental disorders. BMJ. (2019) 366:l4516. doi: 10.1136/bmj.l4516
76. Lai K, Hung S, Lee H, Leung P. School-based mental health initiative: potentials and challenges for child and adolescent mental health. Front Psychiatry. (2022) 13:866323. doi: 10.3389/fpsyt.2022.866323
77. Gee B, Wilson J, Clarke T, Farthing S, Carroll B, Jackson C, et al. Review: delivering mental health support within schools and colleges – A thematic synthesis of barriers and facilitators to implementation of indicated psychological interventions for adolescents. Child Adolesc Ment Health. (2021) 26:34–46. doi: 10.1111/camh.12381
Keywords: school, mental health, systematic reviews, adolescent, intervention
Citation: Grande AJ, Hoffmann MS, Evans-Lacko S, Ziebold C, de Miranda CT, Mcdaid D, Tomasi C and Ribeiro WS (2023) Efficacy of school-based interventions for mental health problems in children and adolescents in low and middle-income countries: A systematic review and meta-analysis. Front. Psychiatry 13:1012257. doi: 10.3389/fpsyt.2022.1012257
Received: 05 August 2022; Accepted: 14 December 2022;
Published: 06 January 2023.
Edited by:
Monika Raniti, The Royal Children’s Hospital, AustraliaReviewed by:
Lauren McGillivray, University of New South Wales, AustraliaRuth Aston, The University of Melbourne, Australia
Copyright © 2023 Grande, Hoffmann, Evans-Lacko, Ziebold, de Miranda, Mcdaid, Tomasi and Ribeiro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wagner Silva Ribeiro,  Vy5TaWx2YS1SaWJlaXJvQGxzZS5hYy51aw==
Vy5TaWx2YS1SaWJlaXJvQGxzZS5hYy51aw==
 Antonio Jose Grande
Antonio Jose Grande Mauricio Scopel Hoffmann
Mauricio Scopel Hoffmann Sara Evans-Lacko2
Sara Evans-Lacko2 Claudio Torres de Miranda
Claudio Torres de Miranda David Mcdaid
David Mcdaid Cristiane Tomasi
Cristiane Tomasi Wagner Silva Ribeiro
Wagner Silva Ribeiro